Abstract
Aim:
The aim of the study is to compare and evaluate the role of new dental adhesives to bond composite to the resinmodified glass inomer cement (RMGIC).
Materials and Methods:
Thirty specimens were prepared on acrylic blocks, with wells prepared in it by drilling holes, to retain the RMGIC. The specimens were randomly divided into three groups of ten specimens each. In Group a thin layer of selfetch adhesive (3M ESPE) was applied between the RMGIC and the composite resin FILTEK P60 (3M SPE). In Group II, total etch adhesive (Adeper Scotch bond 2, 3M ESPE) was applied, and in Group III, there was no application of any adhesive between RMGIC and the composite resin. After curing all the specimens, the shear bond strength was measured using an Instron universal testing machine.
Results:
The results were drawn and tabulated using ANOVA-fishers and Dunnet D statistical tests.The maximum shear bond strength values were recorded in Group I specimens with self-etch adhesive showing a mean value of 2.74 when compared to the Group II adhesive (Total etch) showing a mean shear strength of value 1.89, where no adhesive was used, showed a minimum mean shear bond strength of 1.42. There was a great and significant difference between Group I and Group II (P value 0.05) whereas, both Group I and Group II showed a vast and significant difference from Group III (P value = 0–001).
Conclusion:
Hence, this present study concludes that application of self-etch adhesive (3M ESPE, U.S.A) in between RMGIC and composite resin increases the shear bond strength between RMGIC and the resin composites, as compared to the total-etch type adhesive (Adeper Scotch bond 2,3M ESPE, U.S.A) as well as without application of the adhesive agent.
Keywords: Sandwich technique, self-etch adhesive, total-etch adhesive
Introduction
One of the major challenges in dentistry has been to find an ideal restorative material that has physical properties similar to those of tooth structure, adhesion to dentin and enamel, in addition to resistance to degradation in the oral cavity. In attempt to reach these characteristics, glass ionomer cement (GIC) was developed and first presented by Wilson and Kent[1] in 1972. A remarkable improvement of this class of material occurred approximately 15 years ago, with the introduction of the resin-modified glass ionomer cement (RM-GIC).[2] This material is characterized by the addition of photo-activated methacrylate, and a small amount of resin, such as 2-HEMA or bisphenol-A-glycidyl methacrylate (Bis-GMA), to the conventional glass ionomer cement (GIC) liquid or powder.
Presently, RM-GICs present two or three setting reactions: (a) acid-base reaction, typical of conventional GICs (initiated when the powder and liquid are mixed, occurring without light); (b) photo initiated setting reaction through the methacrylate groups (initiated when the powder/liquid mixture is exposed to light and occurs only where the light penetrates); (c) free-radical methacrylate curing without light (initiated when the powder and liquid are mixed without necessity of light.[3] A strong bond between RMGIC and the composite resin is an important factor for the quality of bilayered restoration. Etching of RMGIC is not required prior to the bonding of the composite resin.[4] However, application of resin bonding agents promotes the adhesion of the resin composite to both conventional GIC and RMGIC. There is limited literature on the bond strength of RMGIC to composite resin with adhesive agents in between. However, bonding agents have been seen to improve the wettability of GIC to help it adhere to the composite resin.[5]
Studies have shown that bonding agents who demonstrate a high degree of wettability, low viscosity, and low contact angle achieve a better union between GIC and the resin composite. Newer adhesive agents have undergone various modifications, such as, changes in viscosity, modification of primers, addition of nanofillers, and so on, to improve the bond strength between the tooth and composite resin.[6] Hence, the present study was conducted to evaluate and compare the shear bond strength of RMGIC to composite resin, using different generations of bonding systems applied on RMGIC.
Materials and Methods
Resin modified GIC (Vitrebond 3M ESPE, St. Paul USA) was bonded to a resin composite (Filtek™ F-60 3M ESPE, St.Paul USA) by using two different bonding agents, a total-etch adhesive (Adper™ Scotch Bond 2-3M ESPE, St.Paul USA) and a self-etch adhesive (Adper™ Prompt™ L Pop™ -3M ESPE, St. Paul USA) and followed the curing with blue (LED) curing light, Rotex, Taiwan.
Preparation of the specimens
The thirty specimens used in this investigation were prepared in 12 mm/25 mm dimensions, which was polished with 220, 320, and 400 grit carbide polishing paper. In each block, a well of 6 mm diameter and 2.5 mm depth was prepared by drilling holes in it to retain the RMGIC. Groove was placed on the walls for increasing the retention. The wells was then filled with light cure GIC by mixing it according to the manufacturer's instructions and covering them with glass plates to produce a smooth surface and to permit light for curing the material. It was then cured with a blue light-emitting diode (LED) curing light (Rotex, Taiwan) for 40 seconds, according to the manufacturer's recommendation, to produce a final set. The glass plate was carefully removed to ensure that the glass ionomer surface was smooth and not pitted.
Specimens were randomly divided into three groups of 10 specimens each, the groups were as follows.
Group A: To the light cure GIC (Vitrebond™) a thin layer of self-etch adhesive (3M ESPE) was applied according to the manufacturer's instructions and cured, and then a cylinder of composite resin (Filtek™ F60, 3M ESPE, St. Paul USA) was added and cured over the specimen.
Group B: Same as group A, but a thin layer of total-Etch adhesive (Adper Scotchbond 2) was applied and cured over RMGIC.
Group C: Acts as a control group, no adhesive agent was applied between the light cure GIC and resin composite.
Immediately after following this procedure, a transparent plastic ring, 5 mm in height, with a 3 mm internal diameter, was centered over the resin-treated GIC, in the templates. The composite resin was condensed into a transparent plastic ring, using an incremental curing technique, above the RMGIC substrate, and all sides of the specimen were cured to ensure complete curing of the material. Following the curing the plastic ring was removed.
All the procedures were conducted at room temperature. The bonded specimens were stored in distilled water at 37°C for 24 hours, to stimulate the conditions of oral cavity, until the specimens underwent the shear bonding test. The shear bond strength was measured by shearing of the bonded specimens on an Instron universal testing machine (model 4406), using a cross head speed of 3 mm/minute [Figure 1]. The shearing apparatus was constructed to grip the acrylic block, and a wedge blade system was designed to apply a shear force of approximately 0.1 mm on the adhesive interface. The readings were tabulated and subjected to statistical analysis using ANOVA, Dunnet D test. Mean and standard deviation were calculated for each group by using the ANOVA test and intergroup comparison was done by the multiple comparison test—Dunnet D test, which revealed a statistical significance among the groups.
Figure 1.

Instron Universal Testing machine
Results
The mean shear bond strength and standard deviations were calculated for each group [Table 1]; and analyzed using the ANOVA test.
Table 1.
Mean values ( Mpa) and standard deviation( SD) Of the shear bond strength of the RMGIC bond to the composite by using different adhesives
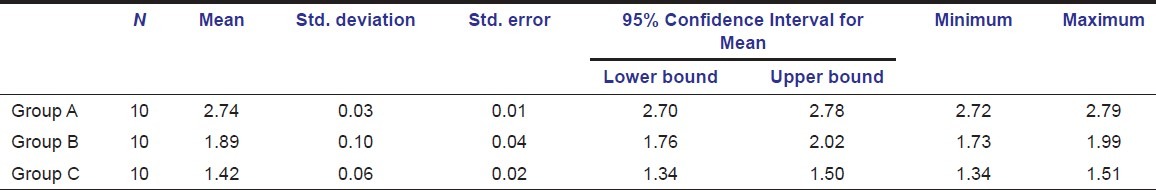
The maximum shear bond strength values were recorded for Group B, where the self-etch adhesive (Adper™ Prompt™ L Pop™) was used, with the mean value of 2.74 MPa and a standard deviation of 0.10. On the other hand, Group C (without any bonding agent) displayed minimum shear bond strength, with a mean of 1.42 MPa and standard deviatation of 0.64, and Group B, with the total-etch adhesive (Adper™ Scotch Bond 2 Adhesive) showed a mean shear bond strength of 1.89 MPa with a standard deviation of 0.03 [Figure 2].
Figure 2.
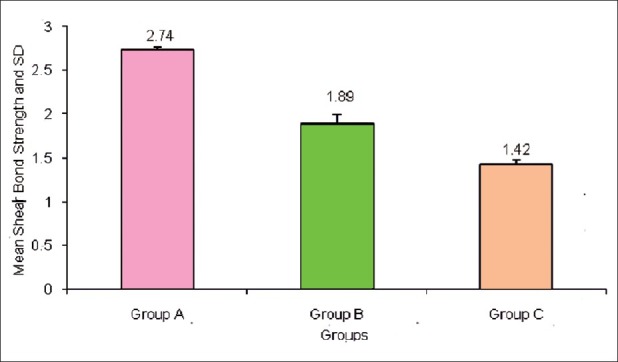
Bar diagram illustrates the mean bond strength between different groups
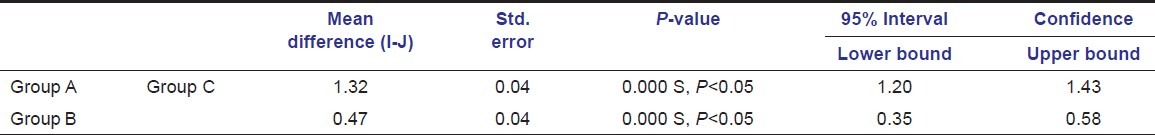
An intergroup comparison was conducted by using the multiple comparison test (Dunnet t test), which revealed a statistical significant difference among the groups, The Dunnet t test showed statistically high significant differences between Group A and Group C (P value 0.05), whereas Group B in comparison to Group C showed a very high significant difference (P value 0.05) [Table 2].
Table 2.
Intergroup comparison and its statistical significance
Discussion
The primary objective of restoring any vital tooth is the prevention of pulpal insults.[7] The possible sources for adverse pulpal inflammation have been identified as thermal stimuli, chemical stimuli, and bacterial endotoxins.
The result of the present study has concluded that a self-etch adhesive agent, Adper™ Prompt™ L Pop™, produces better shear bond strength to Vitrebond, a RMGIC, which is highly significant as compared to a Total-etch adhesive Adper™, Scotch Bond 2, and to the group without any bonding agent. This may be due to the acidic pH of the self-etch adhesive. The acidic nature of adhesive agents makes the superficial surface of the GIC dissolve, thereby improving the bonding of GIC to the composite resin. In addition to a low pH, the self-etch adhesive used in the present study has less viscosity compared to the Total-etch adhesive. A study by GJ Mount, 1989, has shown that a bonding agent having less viscosity shows a lesser contact angle to the surface, and results in better wettability, which helps in promoting a better bond between RMGIC and the resin composite.[8]
The present study is in agreement with other studies where the effect of surface treatments and storage methods on composite/GIC were evaluated, where it was established that an application of a silane coupling agent over a non-etched GIC surface, followed by application of a bonding agent, demonstrated maximum shear bond strength.[9,10]
In the present study, RMGIC was used over the conventional GIC under composite resin restoration because RMGIC sets by an acid-base reaction and exhibits a command set when activated by light or chemical agents via the methacrylate group. RMGIC has also demonstrated a better bonding to composite resin than the conventional GIC.[11,12] This is due to a similar chemistry between RMGIC and the composite resin, which allows the strong bonding of RMGIC to composite resin. Both RMGIC and the resin composite are cured by a free radical initiator system, which provides a potential for the chemical bonding between these two materials.
Conclusions
From the results of the present study it can be concluded that Application of bonding agents improves the wettability of glass ionomer cement to adhere to composite resin, thus promoting a strong shear bond between RMGIC and the resin composite.
Moreover, the application of the self-etch adhesive between RMGIC and the composite resin showed significantly higher shear bond strength compared to the total-etch adhesive.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
References
- 1.Wilson AD, Kent BE. A new translucent cement for dentistry: The glass ionomer cement. Br Dent J. 1972;15:133–5. doi: 10.1038/sj.bdj.4802810. [DOI] [PubMed] [Google Scholar]
- 2.Wilson AD. Resin-modified glass ionomer cements. Int J Prosthod. 1990;3:425–9. [PubMed] [Google Scholar]
- 3.Abdalla AI, Gracia-Godoy F. Bond strength of resin-modified glass inomers and polyacid-modified resin components to dentine. Am J Dent. 1997;10:291–4. [PubMed] [Google Scholar]
- 4.Smith GE. Surface deterioration of glass ionomer cement during acid etching: An SEM evaluation. Oper Dent. 1988;13:3–7. [PubMed] [Google Scholar]
- 5.Hinoura KO, Onose K, Moore K, Phillips RW. Effect of bonding agent on the bond strength between glass ionomer cement and composite resin. Quintessence Int. 1989;20:31–5. [PubMed] [Google Scholar]
- 6.Erickson RL, Glasspole EA. Bonding to tooth structure: A comparison of glass inomer and composite resin system. J Esthet Dent. 1994;6:227–44. doi: 10.1111/j.1708-8240.1994.tb00864.x. [DOI] [PubMed] [Google Scholar]
- 7.Tziafas D, Smith AJ, Lesot H. Designing new treatment strategies in vital pulp therapy. J Dent. 2000;28:77–92. doi: 10.1016/s0300-5712(99)00047-0. [DOI] [PubMed] [Google Scholar]
- 8.Mount GJ. The wettability of bonding resins used in the composite resin/glassionomer “sandwich technique”. Aust Dent J. 1989;34:32–5. doi: 10.1111/j.1834-7819.1989.tb03002.x. [DOI] [PubMed] [Google Scholar]
- 9.Aamin A-el-HM, Bakir NG, Faird MR. Effect of surface treatments and storage methods on the bond strength between composite/glass ionomer cement laminate. Egypt Dent J. 1994;40:871–7. [PubMed] [Google Scholar]
- 10.Noort R. Introduction to Dental Materials. 1st ed. Mosby: Elsevier Publishing; 1994. [Google Scholar]
- 11.Farah CS, Orton VG, Collard SM. Shear bond strength of chemical and light cured glass ionomer cements bonded to resin. Aust Dent J. 1998;43:81–6. doi: 10.1111/j.1834-7819.1998.tb06095.x. [DOI] [PubMed] [Google Scholar]
- 12.Barnes DM, Blank LW. A clinical evaluation of a resin modified glass–ionomer restorative material. J Am Dent Assoc. 1995;126:1245–53. doi: 10.14219/jada.archive.1995.0359. [DOI] [PubMed] [Google Scholar]


