Abstract
Chronic pain is a debilitating and pervasive health problem, particularly among older adults. Researchers and clinicians acknowledge that pain conditions do not occur in isolation, but rather exact a toll on the individual sufferer and the family system at large. No research, however, has explicitly explored the impact of older parents’ chronic pain symptoms on their adult children. In this article, we present relevant predictions from theoretical models that identify the interpersonal effects of chronic illness and pain on family relationships. Guided by theory and empirical research on these topics, we present a conceptual framework of hypothesized risk factors for adult children of parents with chronic pain. We conclude by offering an agenda for future research.
Keywords: Intergenerational relationships, adult children, pain, chronic illness
Over the past decade, researchers and health policy makers have focused increased attention on the problem of chronic pain and its management. This heightened interest is evidenced by a recently-issued report from United States Institute of Medicine, which calls for urgent attention to the disabling effects of chronic pain (Institute of Medicine, 2011). While arthritis and arthritis-related diseases (e.g., back pain) remain the most common causes of chronic pain in older adults (AGS Panel on the Pharmacological Management of Persistent Pain in Older Persons, 2009; Lawrence et al., 1998) other pain producing conditions also occur commonly in this age group, including neuropathies (e.g., diabetes, herpes zoster), vertebral compression fractures from osteoporosis, as well as cancer and cancer treatments (Schmader, 2004; Rao & Cohen, 2004). A growing body of evidence also indicates that diverse chronic illnesses such as advanced heart, lung and/or kidney disease are also common causes of later life pain (Potter, Hami, Bryan, & Quigley, 2003; Walke et al., 2007; Solano, Gomes, & Higginson, 2006). Chronic pain contributes to functional disability via several mechanisms including activity restriction, mobility impairment, social isolation, and depression (AGS Panel on the Pharmacological Management of Persistent Pain in Older Persons, 2009. Chronic physical pain is a common, costly, and often disabling condition and one that poses challenges for both health care providers and caregivers (AGS Panel of Persistent Pain in Older Persons, 2002), particularly among older adults.
Although estimates of prevalence vary from study to study, they suggest that up to 50% of all community-dwelling older people live with chronic pain (Helme & Gibson, 2001). The negative consequences of chronic pain include diminished quality of life, problems sleeping, cognitive and physical disability, immune dysfunction, depression, and social withdrawal (Jakobsson, Klevsgard, Westergren, & Hallberg, 2003; Karp, Reynolds, Butters, & al, 2006; Reid, Williams, & Gill, 2005; Tan, Jensen, Thornby, & Sloan, 2008; Zhu, Devine, Dick, & Prince, 2007). Indeed, the most frequently cited cause of impairment in activities of daily living in later life is pain (Leveille, Fried, & Guralnik, 2002).
Given the extent of chronic pain among older people, a surprising gap exists in the literature on the topic. Specifically, the impact of an older parent’s chronic pain on his or her adult children has not been explored. Adult children typically have extensive contact with older parents and many are engaged in the provision of support to parents in need of care (Fingerman, Pillemer, Silverstein, & Suitor, 2011; Suitor, Gilligan, & Pillemer, 2011). In addition, a growing literature has established the impact of a family members’ pain on spouses and on parents of young children and adolescents. Although this literature has not focused on later life, it suggests that the impact of chronic pain on family relations may extend to older parent – adult child relations.
To date, no studies have been conducted to address the effects of older parents’ chronic pain experience on relationships with adult children. Providing a systematic and comprehensive review of existing research is therefore not possible. The goal of this article is to shed light on this under-researched issue by setting forth a conceptual framework to guide future studies. We begin by reviewing literature relevant to this topic, asking: 1) Should we expect chronic pain in older parents to affect parent-child relationship quality? and 2) What factors may moderate the association between chronic pain and parent-child relations? We conclude with suggestions for a research agenda on this topic.
Chronic Pain: Should It Matter in the Older Parent – Adult Child Relationship?
Accumulating evidence has documented the association between the experience of chronic illness and family relationships (Martire, 2005). Both empirical research (Gallant, Spitze, & Grove, 2010; Turk, Flor, & Rudy, 1987) and clinical practice (see Martire, Lustig, Schulz, Miller, & Helgeson, 2004 for a review) have shown that the family plays an important role in an individual’s adjustment to and recovery from chronic illness. The attitudes and responses of family members to their ailing relative may contribute to the patient’s psychological adjustment, maintenance of health behaviors and overall symptomatology (Snelling, 1990).
However, the association between chronic illness and family relations also operates in the reverse direction, in that the patient’s symptoms, emotional distress, and need for physical and emotional assistance exacts a toll on the family system, leading to increased discord and diminished relationship quality (Leonard, Cano, & Johansen, 2006). In particular, there is consensus in both the empirical and the clinical literature that the experience of chronic pain has “spill-over” effects into individuals’ family relationships. Clinical evidence of the impact of chronic pain on family relationships (Kerns & Turk, 1984; Lewandowski, Palermo, Stinson, Handley, & Chambers, 2010) has since been supported by empirical documentation of the specific adverse effects on family functioning and interactions. A considerable body of research substantiates the link between chronic pain and family discord, revealing that chronic pain conditions may contribute to conflictual family environments and to negative relationship quality (see Leonard et al., 2006; Palermo & Chambers, 2005; Palermo & Eccleston, 2009 for a review).
Due to problems in communication and coping brought on by the patient’s pain condition, the family often experiences social, emotional and relational disruption. In particular, Palermo and colleagues (Palermo, 2000; Palermo & Eccleston, 2009) have reported that chronic pain in children affects not only parental well-being, but also family functioning more generally. Further, a recent systematic review of studies on the effect of adolescents’ pain on family function found that chronic pain among children was associated with lower family cohesion and higher levels of conflict (Lewandowski et al., 2010).
Such findings are echoed in studies of marital dyads. Compared with control groups, chronic pain sufferers and their spouses experience significantly lower family cohesion (Romano, Turner, & Jensen, 1997), and as with parents of young children in chronic pain, spouses also report problems in communication (Flor, Turk, & Scholz, 1987). In turn, poor communication may contribute compromised marital quality. Indeed, some estimates indicate that over half of both persons with pain and spouses exhibit high levels of marital dissatisfaction in the presence of chronic pain, with approximately one third reporting severe levels of dissatisfaction (Kerns & Turk, 1984).
Although, as noted, no studies have specifically addressed the effects of parental pain on intergenerational relations, recent work by Monin, Schulz, and colleagues (Monin & Schulz, 2010; Schulz & Sherwood, 2008) points toward a possible impact. They propose a potential source of adult children’s distress, beyond frequently cited stress of care provision or challenging behaviors by the care recipient: exposure to the suffering that results from chronic disease. In a series of studies, these researchers examined the impact of three forms of suffering on spousal caregivers: physical, emotional, and existential. Although not focused specifically on chronic pain, this program of research suggests that suffering makes a significant contribution to caregiver distress, beyond such previously established predictors as the relative’s disability, behavior problems, and the amount of care provided (Schulz et al., 2009; Schulz et al., 2008).
In summary, the literature on the effects of chronic pain on other family relationships (married couples and parents of young children and adolescents) indicates that the presence of chronic pain in the family negatively affects relationship quality among role partners. Further, research on the impact of suffering on a caregiver’s well-being supports this view. Based on this combined evidence, a major priority for researchers should be to systematically examine the impact of pain on relationships with adult children in the family.
Moderators of the link between chronic pain and parent-adult child relationship quality
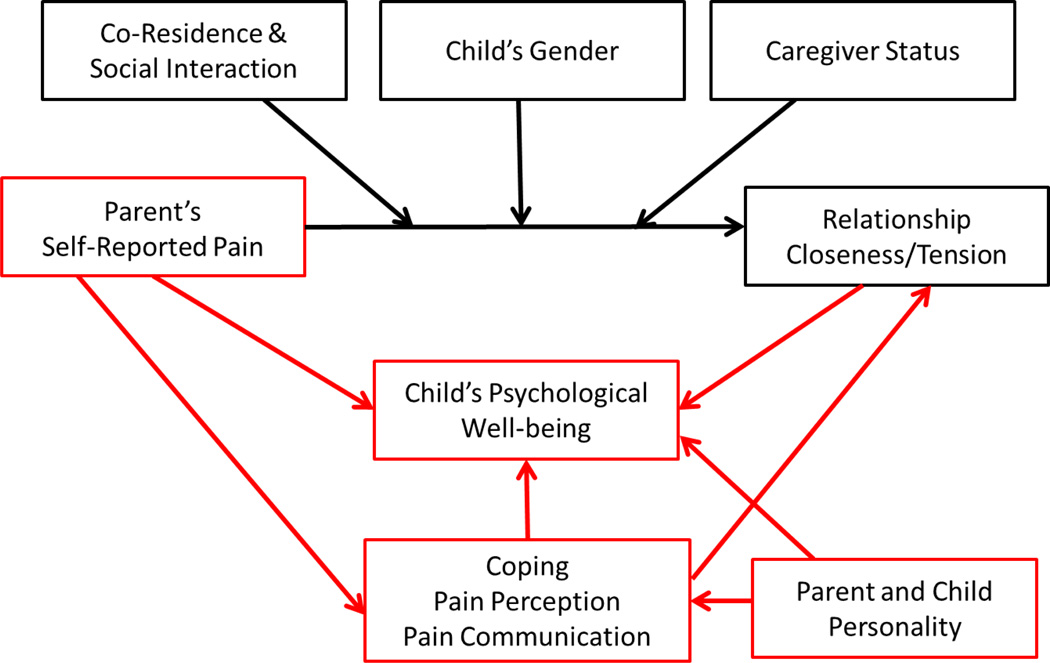
We have focused up to this point on the direct relationship between older parents’ pain and relationships with children. However, there are grounds to hypothesize that the effects on the parent-child relationship may vary considerably by characteristics of the parent and the adult child (e.g., gender), characteristics of the dyadic relationship (prior closeness and tension), and contextual factors (co-residence, frequency of interaction). As depicted in Figure 1, we propose that these variables will contribute to differences in an adult child’s relationship with his or her afflicted parent. Although there are other potential moderators, we have focused on these factors because evidence from both the literatures on intergenerational relations and on chronic pain in younger families suggest they may be related both to the impact of pain on family relationships.
Figure 1.
Proposed conceptual model of risk factors for adult children of parents in chronic pain
Moderators of the link between chronic pain and parent-adult child relationship quality
Co-residence, frequency and quality of contact
The research we have reviewed on pain and the family has focused on the consequences of chronic pain on spouses and parents of young children. However, these two contexts share a structural characteristic that is different from older parents and their adult children: the person experiencing chronic pain and the role partner reside with one another, thus exposing the role partner to the relative’s pain on a frequent, if not continual, basis. However, fewer than 10% of older parents live with their adult children, so such intensive direct exposure to the pain suffering of parents is much more limited. Although data are lacking on the impact of contact on chronic pain, it seems likely that adult children who have more frequent interaction would be more affected by the parent’s pain.
The chronic pain literature does not address this issue directly, but researchers advocate for examining the frequency of pain communication as a means of uncovering the relational aspects of the pain experience (Cano & Williams, 2010). Specifically, communication patterns between patients and their relatives may contribute to overall relationship quality and satisfaction. The patient, for example, may engage in overt pain expression, such as pain disclosure (i.e., verbal “social sharing” of the experience) or pain behavior (i.e., nonverbal actions conveying physical distress) (Stephens, Martire, Cremeans-Smith, Druley, & Wojno, 2006). In addition, patients may display catastrophizing (i.e., an intensified emotional reaction to the pain experience). Adult children who are in more frequent contact with parents may therefore be exposed to pain disclosure and behavior, which is often upsetting and stressful (Newton-John & Williams, 2006). Moreover, exploring not only the duration and frequency of interaction, but also the quality of contact within the pain context will help understand whether communication about pain leads to deleterious family outcomes.
Gender
Gender of the child is likely to be related to the impact of pain on parent-child relations. Research has demonstrated stronger affectional ties and greater confiding between older parents and daughters than with their sons. Mothers generally have closer relationships with their children than fathers, and children report feeling more closely attached to their mothers than to their fathers (Bengtson, 2001; Fingerman, 2001; Rossi & Rossi, 1990; Spitze, Logan, Deane, & Zerger, 1994; Suitor & Pillemer, 2006; Ward, 2008). Both sons and daughters interact more with their mothers than their fathers and report a higher quality of affect toward them than with fathers (Buist, Dekovic, Meeus, & van Aken, 2002). Further, daughters give disproportional support to the older generation (Chelsey & Poppie, 2009; Horowitz, 1985; Spitze & Logan, 1990; Suitor, Pillemer, & Sechrist, 2006). Indeed, not only do daughters provide more support than do sons, but daughters are typically both mothers’ and fathers’ preferred source of emotional support and help during illness (Suitor & Pillemer, 2006). Thus, the pattern of greater contact and closeness with daughters may make them more vulnerable to the effects of a parent’s pain.
Further, both the chronic pain and suffering literatures suggest that compassion and empathy are key factors in shaping relational outcomes for care recipients and their relatives (Goubert et al., 2005; Monin & Schulz, 2010). Notably, empathic responses to patient suffering may vary by caregiver gender. For example, compared with male caregivers, female caregivers not only tend to be more sensitive to their loved one’s emotions (Monin & Schulz, 2009), but also report a greater desire to meet others’ needs (Williamson & Schulz, 1990). In addition, men and women differ in their views of and reactions to the caregiving relationship. Whereas men report less emotional gratification when they perceive the relationship as less close, women display more resentment toward the care recipient (Williamson & Schulz, 1990).
Empirical evidence from the pain literature also documents gender differences in the caregiving relationship. Research indicates greater marital dissatisfaction among wives with a husband in chronic pain than vice versa (Bermas, Tucker, Winkelman, & Katz, 2000; Hafstrom & Schram, 1984). Also particular to the pain context, research suggests that satisfaction with pain-related communication may be lower among wives (Newton-John & Williams, 2006). Although some studies have failed to find gender differences (Geisser, Cano, & Leonard, 2005), in general, the literature portrays a consistent picture of lower relationship satisfaction among female caregivers. We therefore expect that adult daughters will experience greater disruptions in relationship quality than sons.
Caregiver status
Among adult children of older parents, it is possible that the effect of chronic pain on relationship quality depends in part on whether the offspring are providing care to his or her parent. Recent reviews of the caregiving literature suggest the detrimental impact of care provision on family relationships (Quinn, Clare, & Woods, 2009). Characterized by deterioration in overall communication (de Vugt et al., 2003) and relationship quality (Lyons, Zarit, Sayer, & Whitlatch, 2002), entrance into caregiving may lead to tension and strain in family life. Compared with non-caregivers, caregivers report less reciprocity in the relationship (Gallagher-Thompson, Dal Canto, Jacob, & Thompson, 2001) and greater levels of dependency in the patient (Jordan, Eccleston, & Osborn, 2007).
Among parents of young children in pain, research has found both feelings of strain and accentuated closeness within the dyad (Eccleston, Crombez, Scotford, Clinch, & Connell, 2004). Qualitative studies present a similar pattern of results, in which parents note that they “bonded more” with their child, creating an extremely close, but ever dependent relationship (Snelling, 1994). As proposed within the suffering literature, compassion and empathy are essential components in conditioning emotional reactions among caregiving relatives (Monin & Schulz, 2009). As such, increased emotional closeness may imply greater empathy between the members of the dyad (Olson, Portner & Lavee, 1985), and thus, allow both parent and child to share the burden of the pain. Given the stressful nature of the pain experience, heightened levels of strain also emerge as both partners contend with emotional anguish. It is therefore possible that providing care to an older parent with chronic pain may generate ambivalence rather than unambiguously positive or negative assessments of the relationship (Pillemer, Suitor, Pardo, & Henderson, 2010).
Summary
Despite the absence of studies testing whether parental pain affects intergenerational relationship quality, taken together these related literatures provide consistent suggestive evidence that chronic pain can make a strong, independent contribution to the quality of parent-adult child relations. The literature also provides supporting evidence that the effects of a parent’s chronic pain on relationship quality are likely to be moderated by: a) proximity and contact; b) child’s gender; and c) whether the child has provided care to his or her parent during a recent illness or injury.
Promising directions for future research
In previous sections of this paper, we raised a number of issues that merit further study regarding the impact of parent’s chronic pain on adult children, arguing that the experience of pain by the older parent is likely to affect both closeness and tension within the dyad. In support of that argument, we integrated literatures on family caregiving and suffering among older people with research on younger families with a member who is a pain sufferer.
We believe that this topic provides a very fertile area for future research. We propose several avenues for exploration, highlighting the need for rigorous methodological approaches to investigate the role of older parent pain in later life families. In guiding our suggestions for future work in this area, we again turn to literature on the effects of family members’ pain on spouses and parents of young children, but we also indicate how this literature may be adapted for the study of adult children of aging parents.
Pain perception
Accurate perception of the patient’s pain by family members is critical to a family member’s ability to provide appropriate care and assistance to the relative in pain (Goubert et al., 2005). Thus, one potential area for research may be the simultaneous exploration of pain perception by both patient and relative. Within the context of spousal relationships, the partner’s perception of the patient’s symptom severity may contribute to marital satisfaction and adjustment (Romano et al., 1991) as well as higher quality emotional support by the spouse (Manne & Zautra, 1989; Martire et al., 2006; Martire, Stephens, Druley, & Wojno, 2002). Similar associations have been documented among parents of children with chronic pain, such that worried parents tend to engage in more pain-promoting behaviors (e.g., encouraging excessive rest, providing physical assistance/taking over a task) (Guite, Logan, McCue, Sherry, & Rose, 2009).
Levels of agreement between the patient and relative about the pain experience have implications for the dyad. In general, when concordance rates are high, the overall relationship tends to fare better (Martire et al., 2006). Unfortunately, family members often are inaccurate judges, frequently overestimating the patient’s pain and disability (Beaupre et al., 1997; Cremeans-Smith et al., 2003; Redinbaugh, Baum, DeMoss, Fello, & Arnold, 2002; Riemsma, Taal, & Rasker, 2000), which in turn may have ramifications for the dyad (Goubert et al., 2005). Overestimation may contribute to greater depression (Cremeans-Smith et al., 2003) and disability among patients (Goubert, Eccleston, Vervoort, Jordan, & Crombez, 2006; Guite et al., 2009), as well as increased soliciting behavior among relatives (Guite et al., 2009).
Future studies of older parents and adult children can therefore shed light on concurrent and divergent assessments of the pain experience by the patient and family member. Within the context of later life families, we may expect to see similar outcomes for adult children with a parent in pain, where greater pain disclosure leads to greater relationship strain. Inquiry in this area may provide greater insight into the dynamics of the overall adult – child parent relationship.
Pain communication
Another topic for future study is investigation of overt pain communication among older parents and its effects on adult children. Although few studies have explicitly examined the effects of patient pain communication on family members (Newton-John, 2002), emerging evidence suggests that spouses’ frequent communication about severe pain may be associated with decreased emotional support from their partners (Stephens et al., 2006). Other research, however, provides a more favorable view, indicating that somatization among patients actually may not compromise marital adjustment in spouses (Feinauer & Steele, 1992; Newton-John & Williams, 2006). Gathering information from both members of the dyad may be essential in understanding the interwoven nature of the relationship. For instance, within parent-adolescent relationships, catastrophizing among parents may contribute to their own feelings of parenting stress, beyond the child’s pain intensity (Goubert et al., 2006). Future endeavors may benefit from exploring how simultaneous catastrophizing in both adult children and their parents may have ramifications for the overall quality of the relationship.
Thus, the growing body of empirical work argues for additional exploration of dyadic communication within the context of chronic pain. As such, theoretical models have begun to consider how emotional disclosure and validation may also predict relational outcomes. Moreover, it has been hypothesized that verbal and nonverbal communication fosters exaggerated concern for the afflicted individual (Leonard & Cano, 2006; Stephens et al., 2006), perhaps contributing to strained relationships. This body of research can provide a fruitful direction for research in later life families given that advanced age is linked with greater abilities in emotion regulation (Charles, 2010; Urry & Gross, 2010). Due to age-related changes in the ability to regulate one’s emotions, older adults may catastrophize less than individuals in earlier life stages, especially as they are more likely to employ selective strategies such as “thinking positively” to combat worries (Hunt, Wisocki, & Yanko, 2003). Studies exploring pain communication can be useful in understanding how families at different life stages cope with the pain experience.
Coping
Extending from research on pain communication, future inquiry into coping strategies may contribute additional insight into management of the pain experience. Although many studies portray a bleak picture for families with a member in chronic pain, other research reveals a more favorable view. In fact, there is some evidence to suggest that family members actually remain quite satisfied with their relationships, even when a relative experiences high levels of pain (Bermas et al., 2000).
One hypothesized element in distinguishing families in distress from those that are well-adjusted is coping behavior. Recent empirical work provides direct support for this association, revealing less marital satisfaction among spouses who engaged in more passive, rather than active, coping strategies (Bermas et al., 2000). Findings such as these extend earlier theoretical accounts, which propose the way in which a family approaches the pain experience may dictate relational outcomes. For instance, early frameworks posit that chronic pain may be “either a threat or a challenge” (Turk et al., 1987) and further, that familial adaptation to chronic illness will have repercussions for relationships and interactions among individual members. Building on this line of research, Berg and Upchruch (2007) recently proposed a developmental-contextual framework which highlights dyadic coping as an integral component of spousal adjustment to chronic illness. Empirical tests of this theory, however, have primarily focused on the patient’s experience rather than on outcomes for the relative.
Particular to later life families, coping behavior among parents in chronic pain may have implications for their adult children. As noted, because older adults tend to regulate their emotions more efficiently than younger adults (Charles, 2010) and worry less overall (Hunt et al., 2003), a divergent pattern of results from those in young families may emerge. Some studies suggest that coping styles among older adults in chronic pain mirror those of younger individuals in pain (Keefe & Williams, 1990), and but it remains to be seen whether these styles will have a distinct impact on offspring rather than on spouses.
Impact of pain and family relationships on family members’ well-being
The preceding discussion suggests that having a parent who suffers from chronic pain may have a negative impact on the parent – child relationship. It is also possible that older parents’ chronic pain and the disruption caused for families will negatively affect the psychological well-being of offspring. More specifically, the patient’s own symptoms, emotional distress, and need for physical and emotional assistance may elicit emotional reactions by family members (Kerns & Turk, 1984). Prior work has investigated this association in young families and spousal samples, providing a potential foundation for future research on the psychological health of adult children of parents in chronic pain.
The relationship between mood disturbance and chronic pain is well-documented; estimates suggest that 30–50% of all chronic pain patients suffer from depression (Banks & Kerns, 1996). Accruing research suggests that rates may be equally high for spouses and parents of young children with chronic pain. In fact, reports of significant spousal depressive symptomatology range from 20–50% (Ahern, Adams, & Follick, 1985; Kerns & Turk, 1984), with estimates for parents at approximately 40% (Eccleston, Crombez, Stcotford, Clinch, & Connell, 2004). Notably, prevalence surveys also reveal that both spouses (Comstock & Helsing, 1976) and parents (Cadman, Rosenbaum, Boyle, & Offord, 1991) of chronic illness patients exhibit higher levels of depressive symptoms and negative affect than community samples.
Evidence from earlier studies of spousal chronic pain and partner depression consistently documents the presence of psychological distress in both members of the dyad. For example, in an exploratory study of 30 male chronic pain patients and their wives, over one-half of both patients and spouses reported significant levels of depressed mood (Kerns & Turk, 1984). Later work (Flor, et al., 1987; Schwartz, Slater, Birchler, & Atkinson, 1991), however, provides more conservative estimates of spousal depression, with averages around one quarter of the spousal sample. Even these modest appraisals of psychological distress among spouses pose concern for scholars and practitioners, catalyzing a wave of psychosocial intervention plans incorporating close family members in the therapeutic approach to treatment (Martire, 2005).
Therapeutic interventions targeting adolescents and young children in chronic pain also advocate for family involvement. These initiatives echo the adult literature in suggesting that family participation in behavioral treatment may be a promising avenue in managing not only the sufferers’ symptoms, but also family members’ psychological distress (Eccleston, Malleson, Clinch, Connell, & Sourbut, 2003). Of note, parents may benefit in both the short- and long-term from such interventions: recent reports indicate significant improvements in parental depression and stress at immediate and three-month follow-up assessments (Eccleston, et al., 2003). Even with the assistance of therapeutic interventions, individual differences in psychological well-being among family members exist. Systematic reviews reveal considerable variability in the experiences and outcomes of caregivers (Pinquart & Sörensen, 2003). Whereas some caregiving relatives manage the stress and strain of assisting a loved one, others languish in the face of such trying circumstances. Individuals’ coping abilities and perception of caregiving demands may influence their health, well-being and response to the overall experience. Importantly, personality characteristics may play a role in shaping such reactions. For example, those high in the trait of neuroticism not only appraise the caregiving experience more negatively (Bookwala & Schulz, 1998), but also exhibit heightened reactivity to care-related stressors (Koerner, Kenyon, & Shirai, 2009. Moreover, these individuals suffer from depressive symptomatology (Bookwala & Schulz, 1998) as well as compromises in subjective physical health (Hooker, Monahan, Shifren, & Hutchinson (1992), This may be particularly salient within the chronic pain context where the relative must confront issues related to both emotional and physical anguish of the ailing family member.
In addition, relatives’ respective outcomes may hinge upon the patients’ own beliefs and behaviors toward intervention efforts and treatment planning. It is plausible that a compliant and amenable attitude toward treatment by the patient may lead to increased well-being among family members. On the other hand, oppositional or aversive behaviors could contribute not only to discord within the dyad, but also to heightened levels of anguish and strain by family members. The additional stressor of dealing with a noncompliant and combative patient may further contribute to deterioration in relatives’ health outcomes. Although speculation of this relationship has been documented in clinical reports (Groves, 1978), this prediction has yet to be tested in empirical research.
Although studies have not investigated this issue directly, some studies have explored the association between patients’ emotional distress and family members’ own psychological health (e.g., Cohen, Vowles, & Eccleston, 2010). A considerable body of research has demonstrated that exposure to other individuals in chronic pain elicits affective distress in the observer (Goubert, Craig, et al., 2005). In an integrative review, Craig (2009) highlights the social and interactive nature of pain, and the degree to which pain suffering and pain expression affect significant others. Both verbal and nonverbal expressions of pain lead can lead to concern and anxiety on the part of relatives.
Notably, personality may shape the way in which chronic pain patients disclose and communicate about their symptoms. The trait of neuroticism, for example, has been associated with more somatic complaints (Affleck, Tennen, Urrows, & Higgins, 1992), greater pain catastrophizing (Affleck, et al., 1992) and overall heightened levels of distress among chronic pain patients (BenDebba, Torgerson, & Long, 1997). In turn, these conditions have been implicated as risk factors for poorer psychological health among family members. Given this potential pathway by which patient communication may contribute to decrements in family members’ emotional well-being, assessments of both patient and relative personality should be a priority for future exploration.
Lumley and colleagues (2011) note that those in close relationships with affected individuals not only experience stress from seeing their loved ones in pain, but that they have difficulty determining what actions to take to best support the relative and can feel powerless toameliorate the situation. Feelings of powerlessness, in turn, lead to “torture…worse than frustration” for the relative, especially as the patient’s condition persists over time (Jordan, et al., 2007), Such qualitative reports underscore how parental distress is accentuated when parents feel helpless in assuaging their child’s pain. Furthermore, the cyclical and antagonistic relationship between powerlessness and distress may be difficult to sever, leaving family members in a depressed and helpless state as the patient’s symptoms worsen. Conversely, self-efficacy beliefs may buffer such deleterious outcomes, and have been linked with positive health and well-being among caregivers (Rabinowitz, Mausbach, Thompson, & Gallagher-Thompson, 2007).
Taken together, the findings presented above reveal potential pathways by which chronic pain may elicit compromised emotional well-being in both the afflicted individual and close relatives. Future research may thus provide practical benefits by including psychological distress as a clinical indicator of the negative impact chronic pain in older parents has on relationships with their offspring.
Methodological concerns
We have proposed several rich areas for future study; however, research on the dynamic nature of pain within families is not without methodological challenges. Lack of prospective data and a primary focus on cross-sectional studies limit our understanding of directionality of family functioning and pain (Eccleston et al., 2004). Causal directions for the impact of chronic pain on family members, even in early life, have yet to be established, and longitudinal assessments are necessary to illuminate outcomes over time. In addition to longitudinal research endeavors, smaller focus group studies may help clarify how older parents’ pain may impact their adult children’s emotional health. Further, qualitative data may unearth features unique to the adult child-parent relationship when a parent experiences chronic pain
Conclusion
In summary, the existing literature suggests several hypotheses regarding the potential impact of older parents’ chronic pain on their adult children. First, the large body of research on family caregiving has established that parental chronic disease and related problems matter for adult children in terms of perceived relationship quality. Second, the literature on the effects of chronic pain on other family relationships (married couples and parents of young children and adolescents) indicates that the chronic pain experience is likely to affect both closeness and tension within the dyad. Guided by these two sets of findings, we propose a conceptual model of hypothesized factors that may moderate the association between chronic pain and adult child-parent relations. Specifically, we conjecture that the adult child-parent relationship quality may vary by: a) proximity and contact; b) child’s gender; and c) whether the child is the primary caregiver.
The proposed model suggests a variety of avenues for future research, testing the hypothesized pathways between a parents’ pain experience and the quality of intergenerational relationships. After testing for direct effects of pain on relationship quality, we suggest that moderators be considered, and in particular co-residence and contact; gender, and whether or not the child is a caregiver. Another fruitful area for exploration is the degree to which a parent’s pain negatively affects the child’s psychological well-being, which in turn may affect relationship quality.
In this paper, we have highlighted three specific areas for future study that may moderate the association between pain and relationship quality: pain perception, pain communication, and coping within the dyad. We then suggest that the familial disruption caused by an older parents’ chronic pain may also contribute to compromises in adult children’s psychological health. Overall, we conclude that based on the evidence provided in this article, further exploration of the impact of chronic pain on older parent – adult child relations appears to be justified.
Finally, it is important to note the potential importance for practice and policy of establishing this topic as a priority for research. Family caregivers provide the majority of assistance impaired older persons receive, and the economic value of these services is very great (Houser & Gibson, 2008). Therefore, it is critically important to understand factors that facilitate or inhibit caregiving activities on the part of adult children. It is possible that difficulty coping with a parent’s pain may discourage some potential caregivers, given the disruption in family relationships sometimes caused by pain suffering. Further, caring for a parent in pain may potentiate caregiver stress and burden, leading to exhaustion and termination of care. Improving caregivers’ ability to understand parents’ pain and to help them manage it may therefore ultimately promote care at home and discourage use of institutional settings.
To this end, we suggest a focus both on acquiring additional basic knowledge about chronic pain and older parent – adult child relations and in developing interventions to improve coping with pain as a family. Within young families and spousal dyads, gains in treatment outcomes for both partners are most pronounced with family support and involvement (Martire et al., 2004). Pain-coping skills training (CST) interventions, for example, are most effective with spousal assistance. Compared to control groups, spouse-assisted CST not only attenuates patient pain symptoms, but also increases feelings of self-efficacy and marital adjustment among spouses (Keefe et al., 1996). In addition, interdisciplinary cognitive behavioral (ICBT) pain management programs involving family members simultaneously improves patient functioning while reducing parental distress and anxiety. Such therapies are easily transferrable to later life families and are likely to provide benefits to both older persons in need of assistance and their caregivers.
References
- Ahern DK, Adams AE, Follick MJ. Emotional and marital disturbance in spouses of chronic low back pain patients. Clinical Journal of Pain. 1985;1(2):69–74. [Google Scholar]
- AGS Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacologic management of persistent pain in older persons. Journal of the American Geriatriatrics Society. 2009;57:1331–1346. doi: 10.1111/j.1532-5415.2009.02376.x. [DOI] [PubMed] [Google Scholar]
- AGS Panel of Persistent Pain in Older Persons. The management of persistent pain in older persons. Journal of the American Geriatric Society. 2002;50:205–224. doi: 10.1046/j.1532-5415.50.6s.1.x. [DOI] [PubMed] [Google Scholar]
- Banks SM, Kerns RD. Explaining high rates of depression in chronic pain: A diathesis-stress framework. Psychological Bulletin. 1996;119(1):95–110. [Google Scholar]
- Beaupre P, Keefe FJ, Lester N, Affleck G, Frederickson B, Caldwell DS. A computer-assisted observational method for assessing spouses’ ratings of osteoarthritis patients’ pain. Psychology, Health, & Medicine. 1997;2:99–108. [Google Scholar]
- Bengtson VL. Beyond the nuclear family: The increasing importance of multigenerational bonds. Journal of Marriage and the Family. 2001;63:1–16. [Google Scholar]
- Berg CA, Upchurch R. A developmental–contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Bermas BL, Tucker JS, Winkelman DK, Katz JN. Marital satisfaction in couples with rheumatoid arthritis. Arthritis Care and Research. 2000;13:149–155. doi: 10.1002/1529-0131(200006)13:3<149::aid-anr4>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Bookwala J, Schulz R. A comparison of primary stressors, secondary stressors, and depressive symptoms between elderly caregiving husbands and wives: The caregiver health effects study. Psychology and Aging. 2000;15(4):607–616. doi: 10.1037//0882-7974.15.4.607. [DOI] [PubMed] [Google Scholar]
- Buist KL, Dekovic M, Meeus W, van Aken MAG. Developmental patterns in adolescent attachment to mother, father and sibling. Journal of Youth and Adolescence. 2002;31:167–176. [Google Scholar]
- Cadman D, Rosenbaum P, Boyle M, Offord DR. Children with chronic illness: Family and parent demographic characteristics and psychosocial adjustment. Pediatrics. 1991;87(6):884–895. [PubMed] [Google Scholar]
- Cano A, Williams ACdC. Social interaction in pain: Reinforcing pain behaviors or building intimacy? Pain. 2010;149(1):9–11. doi: 10.1016/j.pain.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles ST. Strength and vulnerability integration: A model of emotional well-being across adulthood. Psychological Bulletin. 2010;136:1068–1091. doi: 10.1037/a0021232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chelsey N, Poppie K. Assisting parents and in-laws: Gender, type of assistance, and couples’ employment. Journal of Marriage and Family. 2009;71:247–262. [Google Scholar]
- Cohen LL, Vowles KE, Eccleston C. Parenting an adolescent with chronic pain: An investigation of how a taxonomy of adolescent functioning relates to parent distress. Journal of Pediatric Psychology. 2010;35(7):748–757. doi: 10.1093/jpepsy/jsp103. Retrieved from http://www.pediatricsdigest.mobi/content/87/6/884.short. [DOI] [PubMed] [Google Scholar]
- Comstock GE, Helsing KJ. Symptoms of depression in two communities. Psychological Medicine. 1976;6:551–563. doi: 10.1017/s0033291700018171. Retrieved from http://journals.cambridge.org/action/displayJournal?jid=PSM. [DOI] [PubMed] [Google Scholar]
- Craig KD. The social communication model of pain. Canadian Psychology. 2009;50(1):22–32. [Google Scholar]
- Cremeans-Smith JK, Stephens MAP, Franks MM, Martire LM, Druley JA, Wojno WC. Spouses’ and physicians’ perceptions of pain severity in older women with osteoarthritis: Dyadic agreement and patients’ well-being. Pain. 2003;106:27–34. doi: 10.1016/s0304-3959(03)00268-9. [DOI] [PubMed] [Google Scholar]
- de Vugt ME, Stevens F, Aalten P, Lousberg R, Jaspers N, Winkens I, et al. Behavioural disturbances in dementia patients and quality of the marital relationship. International Journal of Geriatric Psychiatry. 2003;18:149–154. doi: 10.1002/gps.807. [DOI] [PubMed] [Google Scholar]
- Eccleston C, Crombez G, Scotford A, Clinch J, Connell H. Adolescent chronic pain: patterns and predictors of emotional distress in adolescents with chronic pain and their parents. Pain. 2004;108:221–229. doi: 10.1016/j.pain.2003.11.008. [DOI] [PubMed] [Google Scholar]
- Feinauer LL, Steele WR. Caretaker marriages: the impact of chronic pain syndrome on marital adjustment. American Journal of Family Therapy. 1992;20:218–226. [Google Scholar]
- Fingerman KL. Aging mothers and their adult daughters: A study in mixed emotions. New York: Springer; 2001. [Google Scholar]
- Fingerman KL, Pillemer KA, Silverstein M, Suitor JJ. The Baby Boomers' intergenerational relationships. The Gerontologist. 2011;52:199–209. doi: 10.1093/geront/gnr139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flor H, Turk DC, Scholz B. Impact of chronic pain on the spouse: Marital, emotional and physical consequences. Journal of Psychosomatic Research. 1987;31:63–71. doi: 10.1016/0022-3999(87)90099-7. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Dal Canto PG, Jacob T, Thompson LW. A comparison of marital interaction patterns between couples in which the husband does or does not have Alzheimer's Disease. The Journals of Gerontology: Psychological Sciences. 2001;56:S140–S150. doi: 10.1093/geronb/56.3.s140. [DOI] [PubMed] [Google Scholar]
- Gallant MP, Spitze G, Grove GJ. Chronic illness self-care and the family lives of older adults: A synthetic review across four ethnic groups. Journal of Cross-Cultural Social Sciences and Law. 2010;25:21–43. doi: 10.1007/s10823-010-9112-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisser ME, Cano A, Leonard MT. Factors associated with marital satisfaction and mood among spouses of persons in chronic back pain. The Journal of Pain. 2005;6:518–525. doi: 10.1016/j.jpain.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Goubert L, Caig KD, Vervoort T, Morley S, Sullivan MJL, Williams ACdC, et al. Facing other in pain: the effects of empathy. Pain. 2005;118:285–288. doi: 10.1016/j.pain.2005.10.025. [DOI] [PubMed] [Google Scholar]
- Goubert L, Eccleston C, Vervoort T, Jordan A, Crombez G. Parental catastrophizing about their child’s pain. The parent version of the Pain Catastrophizing Scale (PCS-P): A preliminary validation. Pain. 2006;123:254–263. doi: 10.1016/j.pain.2006.02.035. [DOI] [PubMed] [Google Scholar]
- Guite JW, Logan DE, McCue R, Sherry DD, Rose JB. Parental beliefs and worries regarding adolescent chronic pain. Clinical Journal of Pain. 2009;25:223–232. doi: 10.1097/AJP.0b013e31818a7467. [DOI] [PubMed] [Google Scholar]
- Hafstrom JL, Schram VR. Chronic illness in couples: Selected characteristics, including wife's satisfaction with and perception of marital relationships. Family Relations. 1984;33:195–203. Retrieved from http://www.jstor.org/stable/584605. [Google Scholar]
- Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clinical Geriatric Medicine. 2001;17:417–413. doi: 10.1016/s0749-0690(05)70078-1. [DOI] [PubMed] [Google Scholar]
- Hooker K, Monahan D, Shifren K, Hutchinson C. Mental and physical health of spouse caregivers - the role of personality. Psychology and Aging. 1992;7:367–375. doi: 10.1037//0882-7974.7.3.367. [DOI] [PubMed] [Google Scholar]
- Horowitz A. Family caregiving to the frail elderly. Annual Review of Gerontology and Geriatrics. 1985;6:194–246. [PubMed] [Google Scholar]
- Houser A, Gibson M. Valuing the invaluable: The economic value of family caregiving, 2008 update. Washington, DC: AARP Public Policy Institute; 2008. Retrieved from http://www.aarp.org/relationships/caregiving/info-11-2008/i13_caregiving.html. [PubMed] [Google Scholar]
- Hunt S, Wisocki P, Yanko J. Worry and use of coping strategies among older and younger adults. Anxiety Disorders. 2003;17:547–560. doi: 10.1016/s0887-6185(02)00229-3. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Relieving pain in America: A blueprint for transforming prevention, care, education, and research. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- Jakobsson U, Klevsgard R, Westergren A, Hallberg IR. Old people in pain: a comparative study. Journal of Pain Symptom Management. 2003;60:793–797. doi: 10.1016/s0885-3924(03)00145-3. [DOI] [PubMed] [Google Scholar]
- Jordan A, Eccleston C, Osborn M. Being a parent of the adolescent with complex chronic pain: An interpretative phenomenological analysis. European Journal of Pain. 2007;11:49–56. doi: 10.1016/j.ejpain.2005.12.012. [DOI] [PubMed] [Google Scholar]
- Karp JF, Reynolds CFr, Butters MA, et al. The relationship between pain and mental flexibility in older adult pain clinic patients. Pain Medicine. 2006;7:444–452. doi: 10.1111/j.1526-4637.2006.00212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe FJ, Williams DA. A comparison of coping strategies in chronic pain patients in different age groups. Journals of Gerontology. 1990;45:161–165. doi: 10.1093/geronj/45.4.p161. [DOI] [PubMed] [Google Scholar]
- Keefe F, Caldwell DS, Baucom D, Salley A, Robinson E, Timmons K, Beaupre P, Weisberg JN, Helms M. Spouse-assisted coping skills training in the management of osteoarthritic knee pain. Arthritis Care and Research. 1996;9(4):279–291. doi: 10.1002/1529-0131(199608)9:4<279::aid-anr1790090413>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Kerns RD, Turk DC. Depression and chronic pain: The mediating role of the spouse. Journal of Marriage and Family. 1984;46:845–852. Retrieved from http://www.jstor.org/stable/352532. [Google Scholar]
- Koerner SS, Kenyon DYB. Understanding “good days” and “bad days”: Emotional and physical reactivity among caregivers for elder relatives. Family Relations. 2007;56:1–11. [Google Scholar]
- Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, Heyse SP, Wolfe F. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis & Rheumatism. 1998;41:778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- Leonard MT, Cano A. Pain affects spouses too: Personal experience with pain and catastrophizing as correlates of spouse distress. Pain. 2006;126:139–146. doi: 10.1016/j.pain.2006.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard MT, Cano A, Johansen AB. Chronic pain in a couples context: A review and integration of theoretical models and empirical evidence. Journal of Pain. 2006;7:377–390. doi: 10.1016/j.jpain.2006.01.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leveille SG, Fried L, Guralnik JM. Disabling symptoms: What do older women report? Internal Medicine. 2002;17:766–773. doi: 10.1046/j.1525-1497.2002.20229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowski AS, Palermo TM, Stinson J, Handley S, Chambers CT. Systematic review of family functioning in families of children and adolescents with chronic pain. The Journal of Pain. 2010;11:1027–1038. doi: 10.1016/j.jpain.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan DE, Guite JW, Sherry DD, Rose JB. Adolescent-parent relationships in the context of adolescent chronic pain conditions. Pain. 2006;22:576–583. doi: 10.1097/01.ajp.0000210900.83096.ca. [DOI] [PubMed] [Google Scholar]
- Lumley MA, Cohen JL, Borszcz GS, Cano A, Radcliffe AM, Porter LS, et al. Pain and emotion: a biopsychosocial review of recent research. Journal of Clinical Psychology. 2011;67(9):942–968. doi: 10.1002/jclp.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons KS, Zarit SH, Sayer AG, Whitlatch CJ. Caregiving as a dyadic process: Perspectives from caregiver and receiver. Journal of Gerontology: Psychological Sciences. 2002;57:P195–P204. doi: 10.1093/geronb/57.3.p195. [DOI] [PubMed] [Google Scholar]
- Manne SL, Zautra AJ. Spouse criticism and support: Their association with coping and psychological adjustment among women with rheumatoid arthritis. Journal of Personality and Social Psychology. 1989;56:608–617. doi: 10.1037//0022-3514.56.4.608. [DOI] [PubMed] [Google Scholar]
- Martire LM. The "relative" efficacy of involving family in psychosocial interventions for chronic illness: Are there added benefits to patients and family members? Families, Systems, & Health. 2005;23:312–328. [Google Scholar]
- Martire LM, Keefe FJ, Schulz R, Ready R, Beach SR, Rudy TE, et al. Older spouses' perceptions of partners' chronic arthritis pain: Implications for spousal responses, support provision, and caregiving experiences. Psychology and Aging. 2006;21:222–230. doi: 10.1037/0882-7974.21.2.222. [DOI] [PubMed] [Google Scholar]
- Martire LM, Lustig AP, Schulz R, Miller GE, Helgeson VS. Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychology. 2004;23:599–611. doi: 10.1037/0278-6133.23.6.599. [DOI] [PubMed] [Google Scholar]
- Martire LM, Stephens MAP, Druley JA, Wojno WC. Negative reactions to received spousal care: Predictors and consequences of miscarried support. Health Psychology. 2002;21:167–176. [PubMed] [Google Scholar]
- Miaskowski C, Zimmer EF, Barrett KM, Dibble SL, Wallhagen M. Differences in patients’ and family caregivers’ perceptions of the pain experience influence patient and caregiver outcomes. Pain. 1997;72:217–226. doi: 10.1016/s0304-3959(97)00037-7. [DOI] [PubMed] [Google Scholar]
- Monin JK, Schulz R. Interpersonal effects of suffering in older adult caregiving relationships. Psychological Aging. 2009;24:681–695. doi: 10.1037/a0016355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin JK, Schulz R. The effects of suffering in chronically ill older adults on the health and well-being of family members involved in their care the role of emotion-related processes. GeroPsych. 2010;23:207–213. doi: 10.1024/1662-9647/a000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton-John TRO. Solicitousness and chronic pain: A critical review. Pain Reveiws. 2002;9:7–27. [Google Scholar]
- Newton-John TRO, Williams ACdC. Chronic pain couples: Perceived marital interactions and pain behaviours. Pain. 2006;123:53–63. doi: 10.1016/j.pain.2006.02.009. [DOI] [PubMed] [Google Scholar]
- Olson DH, Portner J, Lavee Y. FACES III. St. Paul MN: Family Social Science, University of Minnesota; 1985. [Google Scholar]
- Palermo TM. Impact of recurrent and chronic pain on child and family daily functioning: A critical review of the literature. Developmental and Behavioral Pediatrics. 2000;21:58–69. doi: 10.1097/00004703-200002000-00011. Retrieved from http://journals.lww.com/jrnldbp/Abstract/2000/02000/Impact_of_Recurrent_and_Chronic_Pain_on_Child_and.11.aspx. [DOI] [PubMed] [Google Scholar]
- Palermo TM, Chambers CT. Parent and family factors in pediatric chronic pain and disability: An integrative approach. Pain. 2005;119:1–4. doi: 10.1016/j.pain.2005.10.027. [DOI] [PubMed] [Google Scholar]
- Palermo TM, Eccleston C. Parents of children and adolescents with chronic pain. Pain. 2009;146:15–17. doi: 10.1016/j.pain.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillemer K, Suitor JJ, Pardo S, Henderson C. Mothers' differentiation and depressive symptoms among adult children. Journal of Marriage and Family. 2010;72:333–345. doi: 10.1111/j.1741-3737.2010.00703.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. Journal of Gerontology: Psychological Sciences. 2003;56B(2):P112–P128. doi: 10.1093/geronb/58.2.p112. [DOI] [PubMed] [Google Scholar]
- Potter J, Hami F, Bryan T, Quigley C. Symptoms in 400 patients referred to palliative care services: Prevalence and patterns. Palliative Medicine. 2003;17(4):310–314. doi: 10.1191/0269216303pm760oa. [DOI] [PubMed] [Google Scholar]
- Quinn C, Clare L, Woods B. The impact of the quality of relationship on the experiences and wellbeing of caregivers of people with dementia: A systematic review. Aging and Mental Health. 2009;13:143–154. doi: 10.1080/13607860802459799. [DOI] [PubMed] [Google Scholar]
- Rabinowitz YG, Mausbach BT, Thompson LW, Gallagher-Thompson D. The relationship self-efficacy and between cumulative health risk associated with health behavior patterns in female caregivers of elderly relatives with Alzheimer’s dementia. Journal of Aging and Health. 2007;19:946–964. doi: 10.1177/0898264307308559. [DOI] [PubMed] [Google Scholar]
- Rao A, Cohen HJ. Symptom management in the elderly cancer patient: Fatigue, pain, and depression. Journal of the National Cancer Institute Monographs. 2004;32:150–157. doi: 10.1093/jncimonographs/lgh031. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Byrk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed. Newbury Park, CA: Sage Publications; 2002. [Google Scholar]
- Redinbaugh EM, Baum A, DeMoss C, Fello M, Arnold R. Factors associated with the accuracy of family caregiver estimates of patient pain. Journal of Pain Symptom Management. 2002;23:31–38. doi: 10.1016/s0885-3924(01)00372-4. [DOI] [PubMed] [Google Scholar]
- Reid MC, Williams CS, Gill TM. Back pain and decline in lower extremity physical function among community-dwelling older persons. Journals of Gerontology: Medical Sciences. 2005;60:793–797. doi: 10.1093/gerona/60.6.793. [DOI] [PubMed] [Google Scholar]
- Riemsma RP, Taal E, Rasker JJ. Perceptions about perceived functional disabilities and pain of people with rheumatoid arthritis: Differences between patients and their spouses and correlates with well-being. Arthritis Care and Research. 2000;13:255–261. doi: 10.1002/1529-0131(200010)13:5<255::aid-anr3>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Romano JM, Turner JA, Friedman LS, Bulcroft RA, Jensen MP, Hops H. Observational assessment of chronic pain patient-spouse behavioral interactions. Behavior Therapy. 1991;11:549–567. [Google Scholar]
- Romano JM, Turner JA, Jensen MP. The family environment in chronic pain patients: Comparison to controls and relationship to patient functioning. Journal of Clinical Psychology in Medical Settings. 1997;4:383–395. [Google Scholar]
- Rossi AS, Rossi PH. Of human bonding: Parent child relations across the life course. New York: Aldine de Gruyter; 1990. [Google Scholar]
- Schmader KE. Epidemiology and impact on quality of life of postherpetic neuralgia and painful diabetic neuropathy. Clinical Journal of Pain. 2002;18(6):350–354. doi: 10.1097/00002508-200211000-00002. [DOI] [PubMed] [Google Scholar]
- Schwartz L, Slater MA, Birchler GR, Atkinson JH. Depression in spouses of chronic pain patients: the role of patient pain and anger, and marital satisfaction. Pain. 1991;44:61–67. doi: 10.1016/0304-3959(91)90148-Q. [DOI] [PubMed] [Google Scholar]
- Snelling J. The role of the family in relation to chronic pain: review of the literature. Journal of Advanced Nursing. 1990;15:771–776. doi: 10.1111/j.1365-2648.1990.tb01905.x. [DOI] [PubMed] [Google Scholar]
- Snelling J. The effect of chronic pain on the family unit. Journal of Advanced Nursing. 1994;19:543–551. doi: 10.1111/j.1365-2648.1994.tb01119.x. [DOI] [PubMed] [Google Scholar]
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. Journal of Pain Symptom Management. 2006;31(1):58–69. doi: 10.1016/j.jpainsymman.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Spitze G, Logan J. Sons, daughters and intergenerational social support. Journal of Marriage and Family. 1990;52:420–430. Retrieved from http://www.jstor.org/stable/353036. [Google Scholar]
- Spitze G, Logan JR, Deane G, Zerger S. Adult children's divorce and intergenerational relationships. Journal of Marriage and the Family. 1994;56:279–293. Retrieved from http://www.jstor.org/stable/353100. [Google Scholar]
- Stephens MAP, Martire LM, Cremeans-Smith JK, Druley JA, Wojno WC. Older women with osteoarthritis and their caregiving husbands: Effects of pain and pain expression on husbands' well-being and support. Rehabilitation Psychology. 2006;51(1):3–12. [Google Scholar]
- Suitor JJ, Gilligan M, Pillemer K. Conceptualizing and measuring intergenerational ambivalence in later life. The Journals of Gerontology: Psychological Sciences. 2011;66B:769–781. doi: 10.1093/geronb/gbr108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suitor JJ, Pillemer K. Choosing daughters: Exploring why mothers favor adult daughters over sons. Sociological Perspectives. 2006;49:139–161. [Google Scholar]
- Suitor JJ, Pillemer K, Sechrist J. Within-family differences in mothers’ support to adult children. Journal of Gerontology: Psychological Sciences. 2006;61B:S10–S17. doi: 10.1093/geronb/61.1.s10. Retrieved from http://psychsocgerontology.oxfordjournals.org/content/61/1/S10.short. [DOI] [PubMed] [Google Scholar]
- Tan G, Jensen MP, Thornby J, Sloan PA. Negative emotions, pain and functioning. Psychological Services. 2008;5:26–35. [Google Scholar]
- Turk DC, Flor H, Rudy TE. Pain and familes.I. Etiology, maintenance, and psychosocial impact. Pain. 1987;30:3–27. doi: 10.1016/0304-3959(87)90080-7. [DOI] [PubMed] [Google Scholar]
- Urry HL, Gross JJ. Emotion regulation in older age. Current Directions in Psychological Science. 2010;19:352–357. [Google Scholar]
- Walke LM, Byers AL, Tinetti ME, Dubin JA, McCorkle R, Fried MD. Range and severity of symptoms over time among older adults with chronic obstructive pulmonary disease and heart failure. Archives of Internal Medicine. 2007;167(22):2503–2508. doi: 10.1001/archinte.167.22.2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward R. Multiple parent-adult child relations and well-being in middle and later life. Journal of Gerontology: Psychological Sciences. 2008;63B:S239–S247. doi: 10.1093/geronb/63.4.s239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson GM, Schulz R. Relationship orientation, quality of prior relationship, and distress among caregivers of Alzheimer's patients. Psychology and Aging. 1990;3:502–509. doi: 10.1037//0882-7974.5.4.502. [DOI] [PubMed] [Google Scholar]
- Zhu K, Devine A, Dick IM, Prince RL. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine. 2007;32:2012–2018. doi: 10.1097/BRS.0b013e318133fb82. [DOI] [PubMed] [Google Scholar]