Abstract
Background
Causes of children’s asthma health disparities are complex. Parents’ asthma illness representations may play a role.
Purpose
The study aims to test a theoretically based, multi-factorial model for ethnic disparities in children’s acute asthma visits through parental illness representations.
Methods
Structural equation modeling investigated the association of parental asthma illness representations, sociodemographic characteristics, health care provider factors, and social–environmental context with children’s acute asthma visits among 309 White, Puerto Rican, and African American families was conducted.
Results
Forty-five percent of the variance in illness representations and 30% of the variance in acute visits were accounted for. Statistically significant differences in illness representations were observed by ethnic group. Approximately 30% of the variance in illness representations was explained for whites, 23% for African Americans, and 26% for Puerto Ricans. The model accounted for >30% of the variance in acute visits for African Americans and Puerto Ricans but only 19% for the whites.
Conclusion
The model provides preliminary support that ethnic heterogeneity in asthma illness representations affects children’s health outcomes.
Keywords: Asthma, Illness representation, Acute visits, Ethnicity, Disparities
Introduction
The causes of children’s asthma health outcomes disparities are complex and include genetic, environmental, health care system factors, and individual health and illness beliefs. Compared to white children, Black and Hispanic children are more likely to have a diagnosis of asthma, incur potentially avoidable asthma hospitalizations and asthma-related emergency department visits, exhibit lower adherence to the medication regimen, and are less likely to see a specialist [1–4]. There is emerging data demonstrating within-race heterogeneity in asthma outcomes [5, 6], which highlights the necessity of conducting subgroup analyses based on ethnic origin, not solely race. Earlier studies showed that Black children bear the largest burden of asthma [2], but when the Hispanic group was disaggregated into different subgroups, it was revealed that Puerto Rican children have the highest rates of morbidity and mortality [6].
Illness beliefs and behaviors may also differ by ethnicity and help to explain disparities. Pachter et al. [7] conducted a study that examined variations in asthma beliefs and practices among Mexican-American, Puerto Rican, Mexican, and Guatemalan families. The asthma belief systems differed significantly across the ethnic groups, although there was a small core set of beliefs common to all ethnic groups (causes of and susceptibility to asthma). Environmental triggers/irritants, weak lungs, inheritability, and imbalances in hot/cold elements were common across the ethnic subgroups. The most notable differences occurred for asthma symptoms and treatments. Of the 48 symptoms of asthma presented, all groups identified wheeze, cough chest noise, and difficulty breathing. In addition, the Mexican-Americans reported choking. Other symptoms described by the Puerto Rican sample were chest congestion, fast heartbeat, dark or red eyes, difficulty sleeping, weakness, paleness, visible ribs when breathing, and difficulty talking. Individuals from Mexico also reported agitation, hoarseness, thirst, fever/chills, and pneumonia. The sample from Guatemala reported many of the above symptoms and also others reflective of upper respiratory infections. Taking medications prescribed by the doctor, going to the hospital, and relaxation techniques were the only treatments reported by all groups of the 42 questions asked regarding treatment. The Mexican-American and Puerto Rican samples did not endorse the use of herbal and folk remedies, while the Guatemala sample believed in the use of many of these therapies. The Mexican sample also reported the use of antibiotics and sedatives [7].
Recent research into the psychological aspects of asthma has identified individual-level, lay behavioral approaches to asthma [8, 9], which differ from the professional model of asthma management. The professional model portrays asthma as a chronic illness effectively managed through early intervention and controller medications [10–12]. Lay models frequently depict asthma as episodic, acute, and not readily controllable [11, 13–15]. Research evaluating the discrepancies between lay and professional models on health care-seeking behaviors and treatment compliance in asthma and the role of illness representations in asthma health disparities is in its infancy. Yoos et al. [13] reported that parental illness representations congruent with the lay model led to increased probability of suboptimal medication regimens for children. Ethnic minority, low education, and poverty were associated with lay model beliefs. Illness representations among a sample of White and African American families had no association with health care-seeking behaviors [13]. Sidora-Arcoleo et al. [16, 17], among a sample of White, African American, and Puerto Rican families, found that illness representations aligned with the professional model were associated with increased probability of controller medication use, decreased probability of alternative medicine use, and fewer acute asthma visits.
While research continues to provide important information about racial and ethnic disparities in asthma, there is still much work to be done regarding how these factors interact to produce health disparities in these populations. The results of the present study expand the framework for assessing differences in health outcomes among a sample of children with asthma beyond socio-demographic (e.g., race/ethnicity, poverty, education) and health system factors (e.g., lack of a medical home and health insurance) [18] to a multi-factorial model encompassing not only the known socio-demographic risk factors for poor outcomes but also illness representations, socio-contextual factors, and aspects of the parent–health care provider relationship. Lack of a medical home and health insurance are two primary factors that have been identified in the literature as major contributors to disparities in health outcomes based on race, education, and poverty. A unique characteristic of this study sample is that all subjects had a medical home and health insurance as well as free medications for their children. Removing these barriers allows for examination of other factors potentially contributing to children’s asthma health disparities.
Theoretical Framework
The Common-Sense Model of Self-Regulation [19–22] provides the theoretical framework for these analyses. The Common Sense Model takes into account environmental, social, and cultural factors and individuals’ beliefs about health and illness [19–22]. Parents form a “lay theory” about the symptoms, diagnostic labels, cause, cure, timeline, and controllability of the illness. The three tenets of this model are that the parent is an active problem solver; the illness representation is the central cognitive construct that drives the parents’ health care seeking, treatment decisions and appraisal of the outcomes; and illness representations are individualized and may not be in agreement with medical facts [19]. The processes of illness representation, health care seeking, treatment decision, and appraisal of outcomes are shaped by the parent’s prior history managing their child’s asthma, personality traits, and social and cultural contexts.
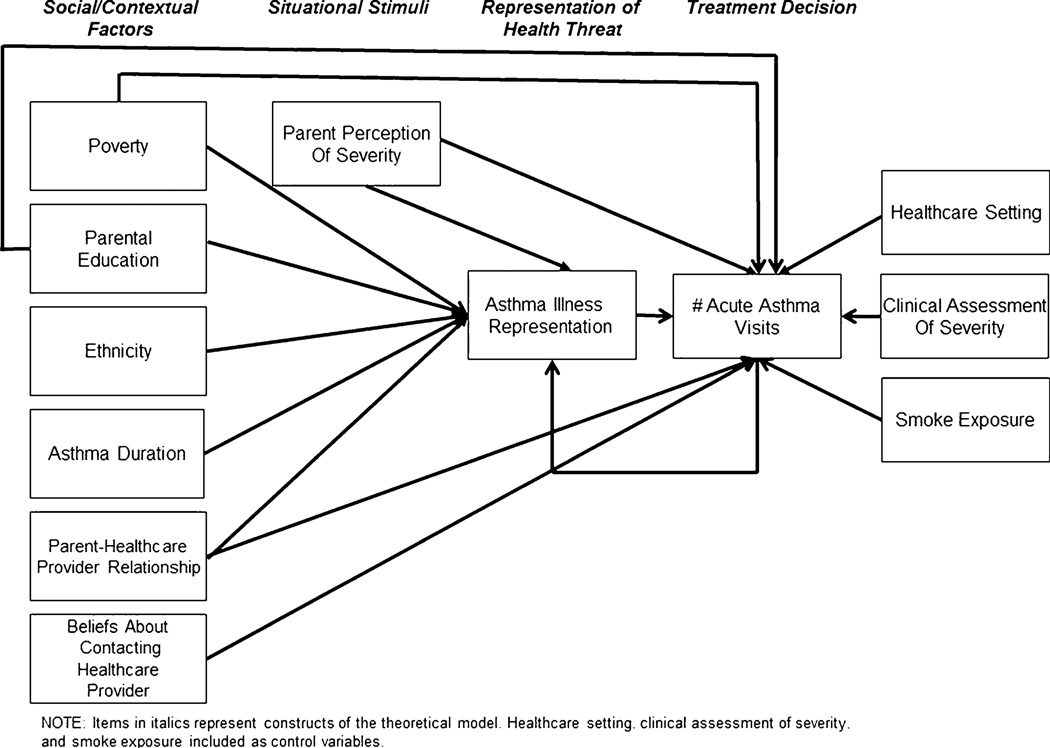
Figure 1 displays the conceptual model examining the relationship between illness representations and acute asthma visits. The parent’s perception of the child’s symptoms (situational stimuli) initiates illness representation formation. The parent’s social and contextual factors (ethnicity, poverty, and education) and their own experiential events (asthma duration, parent–health care provider relationship, and beliefs about contacting the health care provider) lead them to form their individual asthma illness representation (representation of the health threat), which is associated with the decision whether to make an asthma health care visit (treatment decision).
Fig. 1.
Conceptual model.
Two research questions were examined:
Do the sample data provide acceptable fit to the exploratory conceptual model for explaining the variance in illness representations and acute asthma visits?
Are there statistically significant differences by ethnic group in explaining the variance in illness representations and acute asthma visits?
Methods
Study Design
Secondary analyses of data derived from (1) a descriptive study investigating parental illness representations and adequacy of children’s treatment regimens among a primarily white and African American sample in Rochester, NY, USA and (2) a study on children’s asthma symptom perception and parental illness representations conducted in Bronx, NY, USA, among Puerto Rican, African American, and Afro-Caribbean families. The studies from which these data were derived were conducted in accordance with ethical standards for the responsible conduct of research in humans and the revised (2000) Declaration of Helsinki.
Sample and Procedures
Rochester Sample
Full details of the original study were previously published [13] but will be briefly summarized. Two hundred twenty-eight parents and their children with asthma were recruited from two hospital-based ambulatory pediatric clinics and four community pediatric private practices. Parents and children were invited to participate if they met the following criteria: (a) child 5–12 years old, (b) able to understand and complete the interview in English, (c) child diagnosed with asthma (verified through medical records), and (d) the child had at least two asthma-related health care visits (including well-child visits where asthma was discussed and acute visits) in the year prior to the interview. School-aged children with the diagnosis of asthma were identified in each of the clinical settings using the practices’ computerized data sets to extract demographic information, ICD-9 codes, and number of asthma-related visits. Eligible families were informed of the study by a letter from the primary care providers in each of the settings and could refuse further contact by notifying their health care provider. Potentially willing participants were contacted by the research staff and offered enrollment. After agreement to participate was obtained, a home visit was scheduled. Formal consent processes took place at the home visit with written permission for the interview and medical record review obtained from the parent and assent obtained from the child. Interviewers were experienced pediatric nurses trained in asthma care and the research protocol. The University of Rochester Institutional Review Board approved the protocol.
Bronx Sample
One hundred nine participants were recruited from a pediatric asthma/allergy clinic at a public hospital. Parents and children were invited to participate if: (a) child was 7–15 years, (b) able to understand and complete the interview in English, (c) child diagnosed with asthma confirmed by medical chart review, and (d) child had experienced breathing problems in the past year. Children were excluded for severe cognitive learning disabilities. Children with asthma and their primary caregivers were approached in the clinic by a member of the research team who described the study and administered informed consent/assent for families interested in participating. Two members of the research team conducted each session. One individual administered the parent questionnaires, while the other individual conducted the children’s interviews. The Albert Einstein College of Medicine Institutional Review Board approved this study; all parents signed informed consent, and children provided verbal assent.
At both sites, the parent with the most or equal responsibility for the child’s asthma management (self-reported) was asked to participate. Ninety-seven percent of the respondents were the child’s mother or step-mother. Children with all levels of asthma severity were eligible to participate. To provide a more heterogeneous analysis dataset (child’s age, asthma severity, geography, ethnicity, and site of care) as well as to increase the sample size in several of the ethnic groups, the data from Rochester and the Bronx were pooled [16]. The psychometric properties of the asthma illness representation instrument from the Bronx dataset were previously analyzed using standard psychometric techniques (item-total correlation analysis, internal reliability, factor analysis, and external validity). These analyses revealed that, with the exception of the Facts About Asthma subscale, the alphas were either consistent with or better than the original. The Cronbach’s alpha coefficients ranged from 0.62 to 0.83 compared to a range of 0.61–0.78 for the original subscales [16]. Additionally, examination of the demographic predictors of illness beliefs congruent with the professional model revealed that the findings among the Bronx sample were in agreement with those from the original study, demonstrating that parents who were white, non-poor, and had higher educational achievement held asthma illness beliefs congruent with the professional model [16]. The majority of the Puerto Rican sample was from the Bronx, while the majority of the white sample was from Rochester. Confounding between geographic location and ethnicity precluded having a variable for geographic location in the model but a variable for health care setting (clinic versus private practice) was included. Only cases with no missing data for the model variables were included yielding a final sample size for the analyses of 309.
Measures
Endogenous Variables
Asthma Illness Representation Scale
This 37-item instrument is designed for research and health care settings to identify barriers and risk factors for underutilization of controller medications. It was validated among an ethnically diverse sample [13, 16, 23]. The Cronbach’s alpha for the total score is 0.84 and is computed as the mean of items [13, 16]. The alpha for this analysis sample was 0.82. Items are scored on a 5-point Likert-type scale from 1 (strongly agree) to 5 (strongly disagree). Selected items are reverse-scored; higher values indicate alignment with the professional model. A sample of the items comprising each asthma illness representation subscale is provided below:
Treatment expectations: “Children with asthma can expect to have symptoms several times a week”; “I expect that asthma will not affect my child’s school attendance”; and “I believe that my child can be symptom-free most of the time.”
Attitudes toward medication use: “Children with asthma are taking too many inhaled steroids”; “I worry about the side effects of inhaled steroids”; and “Using inhaled steroids should be a last resort in treating asthma.”
Facts regarding asthma: “Inhaled steroids work by fighting inflammation in the lungs”; “Asthma is caused by weak lungs”; and “If albuterol controls symptoms then anti-inflammatory medications are not necessary.”
Nature of asthma symptoms: “Asthma symptoms are unpredictable”; “It is hard to figure out how bad an attack is”; and “Asthma cannot be controlled.”
Emotional aspects of medication use: “Taking daily medication makes a child feel different from other children”; “My child is reluctant to use an inhaler in front of other children”; and “My child does not like the taste of inhaled steroids.”
Number of Acute Asthma Visits
Total number of acute clinic visits, emergency room visits, and hospitalizations for asthma treatment (past year) were obtained from medical record review and parent report. Parent-reported visits not found in the medical record were included because the parent may have sought care at a site other than those where data were abstracted from.
Exogenous Variables
Ethnicity
Parents self-identified their ethnic group as white/Non-Hispanic, African American/Non-Hispanic, Hispanic, Afro-Caribbean, or Other. The number reporting “Other” was too small (n=3) and diverse to allow for meaningful group comparisons and was omitted.
Parental Education
Parental education is reported as years of completed education.
Poverty
Enrollment in Medicaid and/or State Children’s Health Insurance Program was used as a surrogate indicator for poverty. Poverty was coded as 0 (non-poor) or 1 (poor).
Illness Duration
Calculated by subtracting age at diagnosis from age at interview and converted to months. Three parents reported age at diagnosis as “since birth” (coded as 1 month).
Perception of Asthma Severity
Parents’ perception of children’s asthma severity (past 3 months) was rated on a 4-point Likert-type scale, ranging from 1 (very mild) to 4 (severe).
Clinical Assessment of Severity
The classification of asthma severity was based on criteria established by the National Asthma Education and Prevention Program’s Expert Panel Report [12]. There are four severity groups: mild intermittent, mild persistent, moderate persistent, and severe persistent. Study nurses assigned the child’s severity level based on the parent’s response to questions regarding daytime and nocturnal symptoms, activity limitations, exacerbations, and use of short-acting β2 agonists for the 3-month period prior to the interview.
Parent–Health Care Provider Relationship
Quality of the relationship was assessed by ten questions covering continuity of care provider, shared communication regarding worries about asthma and medications, understanding the effect of asthma on the child’s and family’s lives, and instructions about medication use. Items are scored on a 5- point Likert-type scale; responses range from 1 (strongly agree) to 5 (strongly disagree). Several items were reverse scored; higher scores represent a more favorable relationship with the health care provider. The total score was calculated as the mean. The scale was validated among an ethnically diverse sample, has good internal consistency (α=0.82) [16], and illness representations congruent with the professional model [13, 16, 23] and number of acute asthma visits in the past year [16]. The Cronbach’s alpha for this sample was 0.78.
Several additional variables were included as they were hypothesized to modify the relationship between social/contextual factors, parental illness representations, and acute visits.
Beliefs About Contacting the Health Care Provider
This scale contains items considered by the National Asthma Education and Prevention Program Expert Panel [12] to indicate inadequate symptom control and necessity for a health care visit. Parents were asked to rate agreement that they would contact the health care provider if each of these situations occurred. Responses ranged from 1 (strongly agree) to 5 (strongly disagree). Cronbach’s alpha for this scale was 0.76 in the original validation sample and this sample. [13, 16, 23] This variable is included as a control variable on acute visits because it could potentially affect parent’s health care seeking behavior.
Smoke Exposure
The Bronx study did not include an assessment of environmental triggers, only exposure to tobacco smoke; thus, smoke exposure was used as the indicator for triggers, a factor considered important by the Expert Panel [12]. Parents reported on the presence of smokers in the child’s home. Responses were coded as 0 (no) or 1 (yes). This variable is included as a control variable on acute visits because presence of smoke in the home could trigger an asthma exacerbation and lead directly to an acute visit.
Health Care Setting
Health care setting was coded as 0 (private practice) and 1(hospital-based ambulatory clinic).
Statistical Analysis
Descriptive statistics were computed for all variables (SAS V9.2). Following procedures described by Preacher et al. [24], multi-group structural equation modeling (SEM) examined within and between ethnic group differences in acute asthma visits as a function of variation in parental illness representations (MPlus V6.1). SEM estimates how well the sample data fit a model derived from a priori hypotheses of the relationship among the exogenous and endogenous variables. It is based on the covariance matrix of these variables using maximum likelihood estimation. The maximum likelihood estimators are assumed to be population values that maximize the likelihood that the data were drawn from the population. Multi-group analyses were specified to allow modeling of the heterogeneity based on ethnic group.
The distribution for acute visits was skewed; thus, two steps were taken to guard against misleading results due to violated statistical assumptions. First, all model tests were evaluated with adjusted standard errors and model fit indices computed using robust maximum likelihood estimation method. Second, parallel analyses using bias-corrected bootstrapped estimates and confidence intervals were run [24, 25], and the results are reported below.
To address research question 1, the criteria for assessing adequacy of fit of the overall model were the following: χ2/df ratio <2, comparative fit (CFI) and Tucker–Lewis (TLI) indices≥0.90, root mean square error approximation (RMSEA)≤0.05, and standardized root mean square residual (SRMR)<0.08 [26–29]. In this model, two equations were estimated simultaneously: (1) predictors of illness representations and (2) relationship between illness representations and number of acute visits. SEM yields an R2 value for each of these equations. Preacher and Coffman [30] developed software that calculates study power based on covariance structure modeling, and this is reported for all models evaluated during the trimming analyses. The standard assumptions were H0/ε=0.05, HA/ε=0.08, α=0.05, and N=309. Only the df changed from one model to the next.
To address whether differences in parental illness representations and acute visits were due to variations by ethnicity (research question 2), an SEM model was fitted including ethnic group as a covariate and the interactions of ethnic group with illness representation, parent–health care provider relationship, clinical assessment of severity, and parental perception of severity. Mediation analyses were conducted examining the simultaneous indirect effect of the exogenous variables on acute asthma visits through illness representations for each ethnic group. Two criteria should be met when testing mediation [24, 25, 31]. The first (joint test) requires statistically significant paths from exogenous variable to mediator and mediator to endogenous variable. The second is a statistically significant result of a test (e.g., asymmetric confidence limits test) that takes each path into account simultaneously. Both tests were used to examine mediation. MacKinnon et al. [31] demonstrated that tests of statistical significance of mediating variables tend to have low power, and it is not uncommon to set the criteria for statistical significance at p≤0.10. Ethnic group was specified as the grouping variable in order to obtain individualized results. Statistically significant paths and the R2 value for each of the equations for each ethnic group are presented.
Results
Table 1 displays the participants’ baseline characteristics by ethnic group. A greater proportion of the African American and Puerto Rican families was poor (73% and 60%, respectively) and received health care for their child at a hospital-based clinic (79% and 90%, respectively). White parents (14 years) had greater number of years of education than African American and Puerto Rican parents (12 years). Puerto Rican children were older, had longer duration of asthma, and more acute visits in the past year compared to White and African American children. African American families (43%) reported more smokers in the household compared to white (27%) and Puerto Rican (24%) families. Fewer white children (30%) had moderate to severe persistent asthma, based on clinical assessment, compared to African American (54%) and Puerto Rican (51%) children. Interestingly, Puerto Rican parents perceived their child’s asthma to be more severe than the clinical assessment classification. Seventy-four percent of parents rated their child’s asthma severity as moderate or severe compared to 51% classified as such by clinical assessment. African American and White parents tended to underestimate their child’s severity. Forty-one percent of African American children were rated as having moderate to severe asthma by their parents compared to 54% per clinical assessment. Twenty-three percent of white parents perceived their child as having moderate to severe asthma compared to 30% based on clinical assessment. Puerto Rican and African American parents had lower illness representation scores compared to White parents indicating closer alignment with the lay model. White parents reported the highest quality of their relationship with the health care provider, followed by African American parents, and Puerto Rican parents. There were no differences in beliefs about when to contact the child’s health care provider.
Table 1.
Baseline characteristics of study participants by ethnic group (N=309)
| Characteristic | White | African American | Puerto Rican |
|---|---|---|---|
| (N=125) | (N=114) | (N=70) | |
| No. (%) | No. (%) | No. (%) | |
| Poora*** | |||
| No | 100 (80.0) | 31 (27.2) | 28 (40.0) |
| Yes | 25 (20.0) | 83 (72.8) | 42 (60.0) |
| Smoker in house** | |||
| No | 91 (72.8) | 65 (57.0) | 53 (75.7) |
| Yes | 34 (27.2) | 49 (43.0) | 17 (24.3) |
| Parent perception of asthma severity*** | |||
| Very Mild | 75 (60.0) | 46 (40.7) | 8 (11.4) |
| Mild | 21 (16.8) | 21 (18.6) | 11 (15.7) |
| Moderate | 25 (20.0) | 31 (27.4) | 35 (50.0) |
| Severe | 4 (3.2) | 15 (13.3) | 16 (22.9) |
| Asthma severity per clinical assessment*** | |||
| Mild intermittent | 44 (35.2) | 12 (10.5) | 14 (20.0) |
| Mild persistent | 43 (34.4) | 40 (35.1) | 20 (28.6) |
| Moderate persistent | 25 (20.0) | 44 (38.6) | 30 (42.9) |
| Severe persistent | 13 (10.4) | 18 (15.8) | 6 (8.5) |
| Clinic settingb*** | |||
| No | 111 (88.8) | 24 (21.1) | 7 (10.0) |
| Yes | 14 (11.2) | 90 (78.9) | 63 (90.0) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Parent's highest grade completed (self-reported)*** | 14.4 (2.51) | 12.6 (1.99) | 12.0 (2.44) |
| Child's age (parent report)** | 9.0 (2.30) | 9.6 (2.49) | 10.2 (2.36) |
| Asthma duration (months)c*** | 63.9 (33.34) | 78.2 (40.02) | 88.1 (42.21) |
| Parent report of health care provider relationship *** | 4.1 (0.43) | 3.7 (0.53) | 3.3 (0.40) |
| Asthma illness representation scaled*** | 3.4 (0.33) | 3.1 (0.39) | 2.9 (0.33) |
| Number of fealth care visits (acute, emergency room, hospital) past yeare |
5.3 (5.24) | 5.8 (5.19) | 7.2 (7.26) |
Poor was coded as 1=yes if enrolled in Medicaid/SCHIP and 0=no.
Clinic setting was coded 0=private practice and 1=hospital-based ambulatory clinic.
Asthma duration was computed as age at interview (months)-age at diagnosis (months).
Items are scored on a 5-point Likert-type scale; responses range from 1 (strongly agree) to 5 (strongly disagree). Higher scores represent beliefs aligned with the professional model. The total score was calculated as the mean of the items.
Health care visits were abstracted from the medical record and obtained from parent report.
p<.05
p<.01
p<.001.
Model Fit (Research Question 1)
Table 2 presents the results of the model fit and trimming analyses. The first model analyzed included all variables as identified in the conceptual model (Fig. 1). Ethnicity was included in the analyses as a grouping variable, thus is not represented as a path variable in these analyses. Based on H0/ε=0.05, HA/ε=0.08, α=0.05, df=15, and N=309, power was 0.52 for rejecting the hypothesis of close fit. This model demonstrated good fit statistics (χ2/df=0.83, CFI=1.0, TLI=1.1, RMSEA<0.0001, and SRMR=0.02) but low power; thus, results were examined for non-significant paths that could be trimmed. Five subsequent model trimming analyses were conducted removing paths that were not statistically significant for any ethnic group or whose influence on the fit statistics was negligible. The final model for the illness representation equation was comprised of parental education, poverty, parent–health care provider relationship, asthma duration, and parental perception of severity. The equation for acute visits consisted of illness representation, parental perception of severity, clinical assessment of severity, smoke exposure, and health care setting. The final model exhibited almost identical fit statistics to the original model but the increase in df (from 15 to 21) resulted in an increase in power to 0.67.
Table 2.
Test of model fit for social/contextual factors, perception of severity, and parental illness representations on children’s acute visits.
| Path variables | χ2/df | CFI | TLI | RMSEA | SRMR | Powera |
|---|---|---|---|---|---|---|
| Model 1 | 0.83 | 1.0 | 1.1 | <0.0001 | 0.02 | 0.52 |
| Asthma illness representation on | ||||||
| Parental education | ||||||
| Poverty | ||||||
| Parental perception of severity | ||||||
| Child's asthma duration | ||||||
| Parent—health care provider relationship | ||||||
| Number of acute visits on | ||||||
| Asthma illness representation | ||||||
| Parental education | ||||||
| Poverty | ||||||
| Parental perception of severity | ||||||
| Parent-health care provider relationship | ||||||
| Smoke exposure | ||||||
| Beliefs about contacting health care provider | ||||||
| Clinical assessment of severity | ||||||
| Health care setting | ||||||
| Model 2: smoke exposure omitted from acute visits | 1.15 | 0.99 | 0.96 | 0.04 | 0.02 | 0.47 |
| Model 3: beliefs about contacting health care provider omitted from & smoke exposure added back to acute visits |
0.97 | 1.0 | 1.0 | <0.0001 | 0.02 | 0.47 |
| Model 4: beliefs about contacting health care provider+Health care provider relationship on acute visits ommitted |
1.06 | 1.0 | 0.98 | 0.02 | 0.02 | 0.52 |
| Model 5: beliefs about contacting health care provider+health care provider relationship+ education omitted from acute visits |
0.91 | 1.0 | 1.0 | <0.0001 | 0.02 | 0.60 |
| Model 6: beliefs about contacting health care provider+health care provider relationship + education+poverty omitted from acute visits |
0.84 | 1.0 | 1.0 | <0.0001 | 0.02 | 0.67 |
Ethnicity included as a grouping variable in the model, thus not represented as a path
Power based on RMSEA
Prior to conducting the SEM mediation analyses, regression analyses were run, which paralleled the model fitting analyses. The initial model contained all variables from the model fitting analyses plus interactions of ethnic group with each co-variate. Model trimming was carried out to maximize percent of variance accounted for and elimination of non-significant interactions. The final model retained the interaction of ethnic group with parent-health care provider relationship for the illness representation equation. The final equation for acute visits kept the interactions of ethnic group with illness representation, parental perception of severity, and clinical assessment of severity. This model accounted for 45% of the variance in asthma illness representations and 30% of the variance in acute visits. Table 3 presents the results for the final regression model, which are summarized below.
Table 3.
Regression results for differences in asthma illness representations and acute visits
| Variable | R2 | β (SE) | 95% CI | p value |
|---|---|---|---|---|
| Asthma illness representation | 0.45 | |||
| Ethnic group | −0.36 (0.17) | −0.65, −0.08 | 0.03 | |
| Poverty | −0.14 (0.04) | −0.21, −0.07 | 0.001 | |
| Parental perception of severity | −0.06 (0.02) | −0.09, −0.03 | 0.001 | |
| Parental education | 0.03 (0.01) | 0.02, 0.05 | <0.0001 | |
| Asthma duration | 0 (0) | −0.001, 0.001 | 0.58 | |
| Parent- health care provider relationship | 0.14 (0.09) | −0.01, 0.30 | 0.13 | |
| Ethnic group × parent- health care provider relationship |
0.09 (0.05) | 0.01, 0.17 | 0.06 | |
| Acute visits | 0.30 | |||
| Ethnic group | −0.56 (0.60) | −1.55, 0.42 | 0.35 | |
| Asthma illness representation | −0.64 (0.34) | −1.21,−0.08 | 0.06 | |
| Parental perception of severity | 0.24 (0.13) | 0.02, 0.46 | 0.07 | |
| Smoke exposure | 0.08 (0.10) | −.09, .25 | 0.45 | |
| Clinical assessment of asthma severity | 0.32 (0.15) | 0.07, 0.57 | 0.04 | |
| Health care setting | −0.47 (0.12) | −0.66, −0.27 | <0.0001 | |
| Ethnic group × asthma illness representation | 0.20 (0.17) | −0.09, 0.49 | 0.25 | |
| Ethnic group × perception of severity | 0.05 (0.07) | −0.07, 0.16 | 0.52 | |
| Ethnic group × clinical assessment of severity | −0.06 (0.08) | −0.18, 0.07 | 0.46 |
Effects on Asthma Illness Representations
Statistically significant differences in illness representations were observed for ethnicity(β=−0.36, SE=0.17, 95% CI=−0.65,−0.08, p=0.03), poverty(β=−0.14, SE=.04, 95% CI=−0.21,−0.07, p=0.001), parental perception of severity(β=−0.06, SE= 0.02, 95% CI=−0.09,−0.03, p=0.001), and parental education( β=0.03, SE=0.01, 95% CI=0.02, .05, p≤<0.0001). All of these relationships were consistent with previous results demonstrating that poor, lesser educated, ethnic minority parents who perceive greater disease severity in their children hold illness beliefs aligned with the lay model. The interaction of ethnic group and parent–health care provider relationship on illness representation demonstrated a trend towards statistical significance (β=0.09, SE=0.05, 95% CI=0.01, 0.17, p=0.06).
Effects on Acute Asthma Visits
There were only two statistically significant predictors of acute visits: clinical assessment of asthma severity (β=0.32, SE=0.15, 95% CI=0.07, 0.57, p=0.04) and health care setting (β=−0.47, SE=0.12, 95% CI=−0.66, −0.27, p≤0.0001). Greater asthma severity led to increased acute visits. Interestingly, children who received their asthma care at the hospital-based ambulatory clinics had fewer acute visits. There was a trend for asthma illness representation and parental perception of severity towards significance. None of the ethnic group interactions on acute visits was statistically significant.
Ethnic Group Differences in Asthma Illness
Representations and Acute Visits (research question 2)
Direct Effects on Asthma Illness Representations
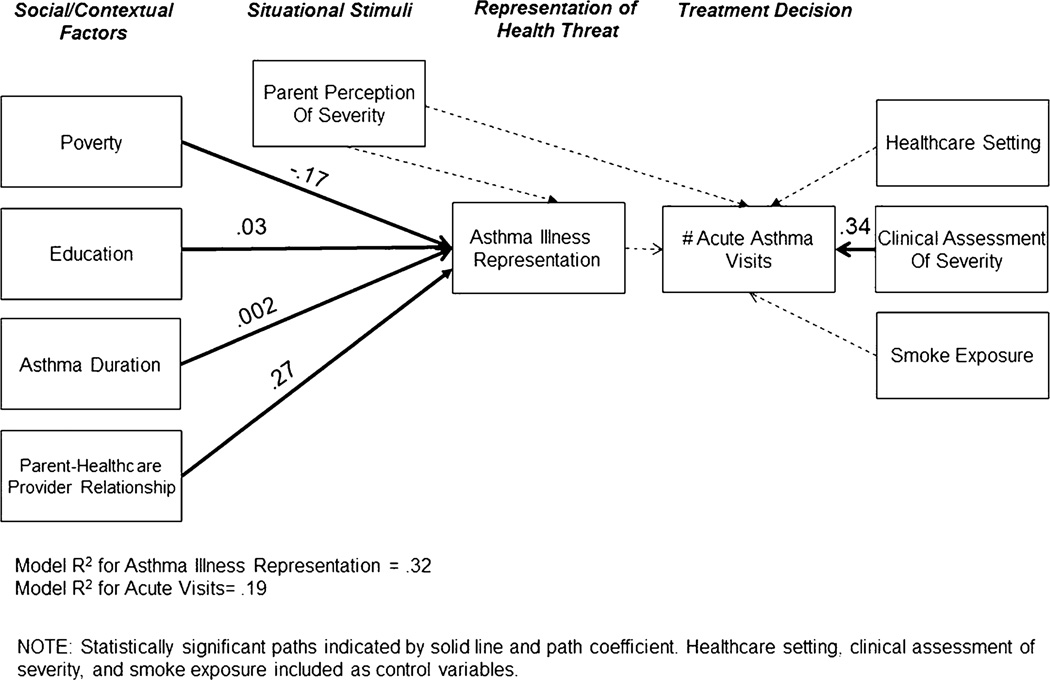
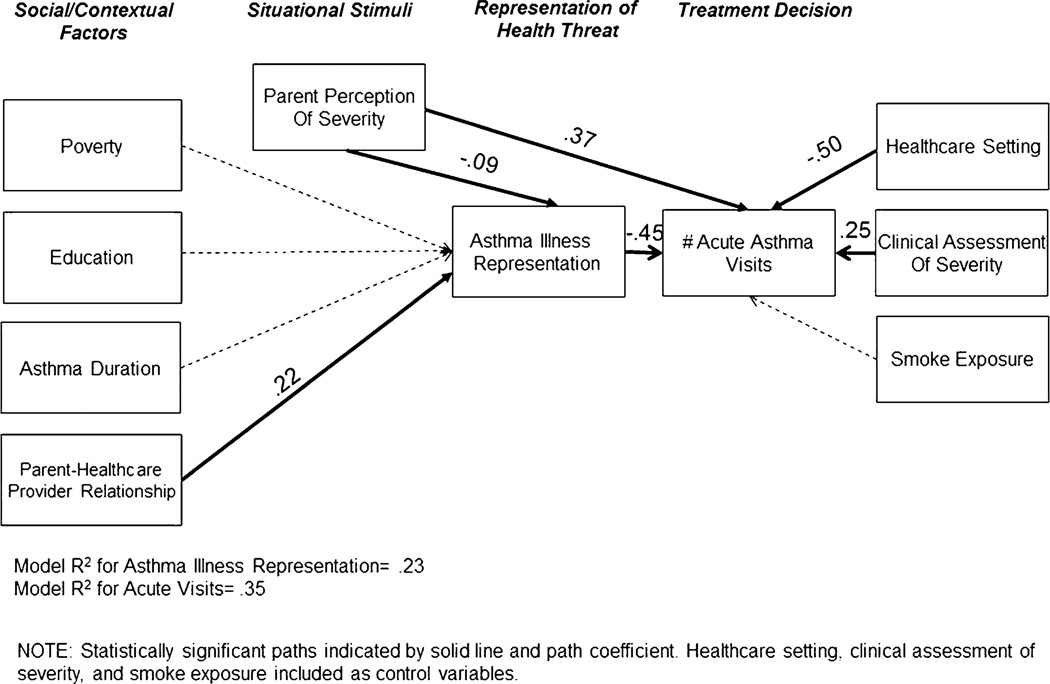
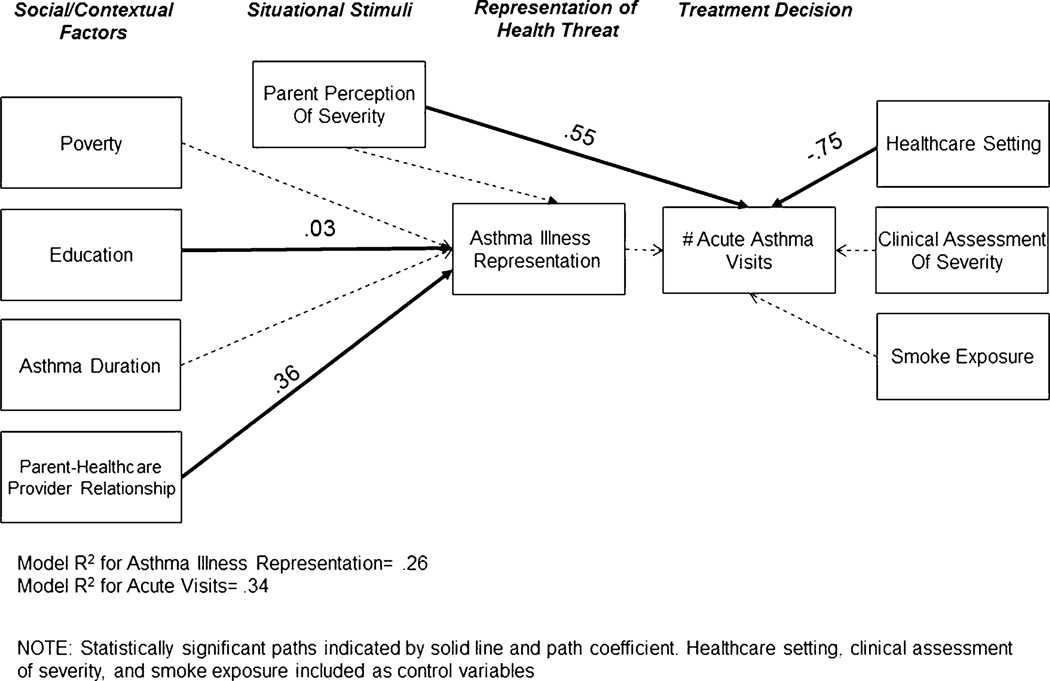
The final model accounted for a greater percentage of variance of illness representations for the white parents (32%) compared to African American (23%) and Puerto Rican (26%) parents (Table 4). As illustrated in Figs. 2, 3, and 4, differences in predictors of illness representations were observed by ethnic group. Examination of individual path coefficients revealed that only quality of the parent–health care provider relationship was a significant predictor of illness representations across all ethnic groups. Higher quality ratings were associated with higher illness representation scores, indicating alignment with the professional model. Higher education was indicative of higher illness representation scores for white and Puerto Rican parents; the African American parents demonstrated a trend towards significance in the same direction. Living in poverty and shorter asthma duration were associated with illness representation scores congruent with the lay model only for white parents. Parental perception of greater asthma severity resulted in lower illness representation scores, indicating alignment with the lay model only for the African American parents.
Table 4.
Model direct, indirect, and total effects of variables on illness representations and acute asthma visits by ethnic group
| Variables and their effect | White | African American | Puerto Rican | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R2 | β(SE) | 95% CI | p value | R2 | β(SE) | 95% CI | p value | R2 | β(SE) | 95% CI | p value | |
| Direct effect on illness representation | 0.32 | 0.23 | 0.26 | |||||||||
| Parent perception of severity | −0.02 (0.03) | −0.07, 0.03 | 0.53 | −0.09 (0.03) | −0.13, −0.03 | 0.01 | −0.02 (0.05) | −0.10, 0.06 | 0.73 | |||
| Parental education | 0.03 (0.01) | 0.01, 0.05 | 0.009 | 0.03 (0.02) | 0,0.05 | 0.06 | 0.03 (0.02) | 0, 0.05 | 0.05 | |||
| Poverty | −0.17 (0.07) | −0.29, −0.06 | 0.02 | −0.09 (0.08) | −0.20, 0.05 | 0.24 | −0.05 (0.07) | −0.17, 0.07 | 0.51 | |||
| Asthma Duration | 0.002 (0.001) | 0.001, 0.003 | 0.02 | 0 (0.001) | −0.002, 0.001 | 0.77 | −0.001 (0.001) | −0.002, 0.001 | 0.55 | |||
| Parent-health care provider relationship | 0.27 (0.06) | 0.18,0.39 | <0.0001 | 0.22 (0.07) | 0.11, 0.34 | 0.002 | 0.36 (0.13) | 0.12, 0.54 | 0.006 | |||
| Direct effect on acute visits | 0.19 | 0.35 | 0.34 | |||||||||
| Parental perception of severity | 0.07 (0.10) | −0.08, 0.24 | 0.50 | 0.37 (0.10) | 0.20, 0.53 | <0.0001 | 0.55 (0.11) | 0.40, 0.7 | <0.0001 | |||
| Illness representation | −0.08 (0.20) | −0.44, 0.20 | 0.67 | −0.45 (0.19) | −0.76, −0.11 | 0.02 | −0.14 (0.37) | −0.66, 0.54 | 0.70 | |||
| Smoke exposure | −0.13 (0.18) | −0.43, 0.15 | 0.46 | 0.20 (0.18) | −0.09, 0.50 | 0.25 | 0.32 (0.24) | −0.14, 0.69 | 0.19 | |||
| Clinical assessment of severity | 0.34 (0.09) | 0.19, 0.49 | <0.0001 | 0.25 (0.12) | 0.09, 0.46 | 0.03 | 0.15 (0.15) | −0.14, 0.36 | 0.34 | |||
| Health care setting | −0.34 (0.23) | −0.74, 0.03 | 0.14 | −0.50 (0.19) | −0.78, −0.20 | 0.008 | −0.75 (0.25) | −10.14, −0.34 | 0.002 | |||
| Indirect effect of illness representation on acute visits | ||||||||||||
| Poverty | 0.01 (0.04) | −0.03, 0.100.710 | 0.71 | 0.04 (0.04) | −0.005, 0.15 | 0.35 | 0.007 (0.03) | −0.03, 0.08 | 0.83 | |||
| Asthma duration | 0 (0) | −0.001, 0 | 0.68 | 0 (0) | −0.001, 0.001 | 0.79 | 0 (0) | 0, 0.001 | 0.86 | |||
| Parental perception of severity | 0.002 (0.008) | −0.004, 0.02 | 0.84 | 0.04 (0.02) | 0.008, 0.09 | 0.11 | 0.002 (0.02) | −0.02, 0.04 | 0.91 | |||
| Parental education | −0.002 (0.006) | −0.02, 0.005 | 0.69 | −0.01 (0.009) | −0.03, 0 | 0.18 | −0.004 (0.01) | −0.03, 0.01 | 0.74 | |||
| Parent-health care provider relationship | −0.02 (0.05) | −0.13, 0.05 | 0.68 | −0.10 (0.06) | −0.21,−0.02 | 0.09 | −0.05 (0.13) | −0.24, 0.17 | 0.69 | |||
Fig. 2.
Final path analysis: acute asthma visits on asthma illness representation score-White.
Fig. 3.
Final path analysis: acute asthma visits on asthma illness representation score- African American.
Fig. 4.
Final path analysis: acute asthma visits on asthma illness representation score-Puerto-Rican
Direct Effects on Acute Asthma Visits
Results for acute visits demonstrated that the final model accounted for a substantially larger proportion of the variance among African American (35%) and Puerto Rican (34%) parents than for white parents (19%) (Table 4). There were also ethnic group differences in predictors of acute asthma visits (Table 4 and Figs. 2, 3 and 4). Higher illness representation scores (congruent with the professional model) were associated with fewer acute visits but only for the African American sample. Parental perception of greater asthma severity was associated with more acute visits among the African American and Puerto Rican children only. Among white and African American children, greater asthma severity per clinical assessment was linked with more acute visits. African American and Puerto Rican families who received their child’s asthma care in a hospital-based clinic had fewer acute visits, but health care setting was not significantly related to acute visits for the white sample. Smoke exposure was not related to acute visits for any ethnic group.
Indirect Effects on Acute Asthma Visits
Among the African American sample, there was a trend toward significance for the mediating effect of illness representation on the relationship between parent–health care provider relationship and acute asthma visits (β=−0.10, SE=0.06, 95% CI=−0.21,−0.02, p=<0.09). Illness representations did not mediate the effect of any social/contextual variables on acute visits for the white or Puerto Rican samples (Table 4).
Discussion
This test of the Common Sense Model [19–21] for investigating disparities in children’s acute asthma visits as a function of ethnic differences in illness representations revealed preliminary support for the conceptual model. For all ethnic groups, higher quality of the relationship with the health care provider was associated with illness representations aligned with the professional model. If parents feel that they are part of the decision-making process regarding treatment of their children’s asthma, they may be more likely to adhere to the prescribed medication regimen resulting in better asthma health outcomes for their children. Higher parental education was also associated with beliefs congruent with the professional model (statistically significant for white and Puerto Rican parents). Research has shown that education relates to how an individual acquires and processes information [32, 33]. These skills are important as parents assimilate information obtained from health care providers, friends, and other sources regarding children’s asthma and management; negotiate the complex health care system; and decide how to treat their children. Parents living in poverty have been shown to form illness representations congruent with the lay model [13, 23, 34]. The current results do not fully support this. Living in poverty was associated with lower illness representations scores only for the white sample. Poverty and education were moderately correlated (r= 0.40), and because the influence of these variables was estimated simultaneously through SEM, it appears that education is a more powerful predictor in this sample for the African American and Puerto Rican samples. Parents’ experience dealing with children’s asthma, measured by the child’s asthma duration, is hypothesized to affect their illness representations. This relationship was only supported for the White parents even though the African American and Puerto Rican children experienced asthma for longer durations. If the minority children are truly sicker and have poorly controlled symptoms, it is possible that the parents’ beliefs are not influenced at all by how long or short a period of time the child has been diagnosed. The theoretical model describes a link between parental perception of severity and illness representation formation. In this sample, perception of greater severity led to beliefs aligned with the lay model, but this was statistically significant only for African American parents. This negative relationship may be attributable to lack of asthma control. If parents have been struggling with maintaining good control, then their beliefs surrounding medication use and disease control could be weakened.
The conceptual model accounted for a greater proportion of the variance in acute visits for African American and Puerto Rican parents compared to white parents and identified important differences in predictors of parents’ health care seeking behaviors. Previous analyses demonstrated mixed results for the relationship between illness representation and acute visits [13, 16]. In these analyses, illness representations congruent with the professional model led to fewer acute visits for African American sample only. For the white and Puerto Rican families, illness representation scores congruent with the professional model were not associated with fewer acute visits as we expected. Seventy-seven percent of white parents perceived their child’s asthma to be mild intermittent or mild persistent (70% were clinically assigned those designations). This suggests that although parents’ beliefs were congruent with the professional model, their child’s disease status did not warrant an acute visit. Interestingly, greater severity assessed by clinical exam was related to increased acute visits for these parents, even though the majority of children had mild symptoms. The absence of a relationship between illness representation and acute visits for the Puerto Rican families may be due to sample size limitations because these parents had the lowest illness representation scores, but their children had the highest number of acute visits. Among the Puerto Rican sample, parental perception of greater severity was associated with increased acute visits but clinically assessed severity demonstrated no relationship. Emerging findings are demonstrating that Puerto Ricans may over-perceive asthma symptoms [35, 36]. This may partially explain the observed relationship between parental perception and acute visits. Fifty percent of the parents rated their child’s symptom severity greater than that assigned by clinical assessment (data not shown).
An interesting finding for this group was that care received in the hospital-based clinic setting was related to fewer acute visits in spite of greater parental perception of severity, and actual worse disease severity based on clinical assessment. This is in contrast with findings by Galbraith et al. [37].who found that minority children with persistent asthma were less likely to be prescribed inhaled steroids by minority-serving providers who were in hospital clinics or community health centers.
Clinical Implications
We have demonstrated that parental education plays a significant role in variations in illness representation, above and beyond poverty. Several studies have suggested that parents with higher education were more likely to understand the role that anti-inflammatory medications play in managing their children’s asthma, had more knowledge about the disease, and were more likely to adhere to the prescribed medication regimen [32, 33]. It will be important for health care providers to have a basic understanding of the cognitive capacity of the parents when discussing the child’s asthma management strategies.
This study also provides insight into the role that illness beliefs play in health care-seeking behaviors. Health care providers, regardless of their practice setting, can best treat children with asthma if they understand what beliefs parents hold about what causes asthma, the nature of asthma symptoms, its course of action (chronic versus episodic), medications and alternative therapies used in treatment, and expectations for symptom resolution. If parents’ beliefs are discordant with the health care provider’s beliefs and are not addressed when devising the management plan, there is increased risk for non-adherence. Health care providers have an opportunity to intervene at the individual level to effect changes aimed at improving adherence to the prescribed treatment regimen through improved communication, education (both parents and themselves), and partnership with the families.
Limitations
Inherent with secondary analyses are study limitations. There was confound between geographic setting and ethnicity. The majority of the white sample was from Rochester and the Puerto Rican families were predominantly from the Bronx. Because the focus was on ethnic differences, not geographic differences, and health care setting was included in the model, we believe that we minimized the influence of this confound. The Rochester data did not include pulmonary lung function measures. Thus, asthma severity was assigned based on clinical assessment by the research nurse per National Asthma Education and Prevention Program guidelines regarding symptoms, activity limitations, and medication use [12]. The two studies from which these data were obtained were cross-sectional and therefore, a test of the feedback loop could not be carried out. Although the model trimming analyses resulted, in a 15% increase in study power, the study was still under-powered (0.67), which limited the ability to detect potentially meaningful pathways. Lastly, this is only one conceptual model that yielded good fit statistics. There may be alternative models that perform equally well or better than the model tested here.
Conclusions
These analyses took a unique approach to studying ethnic disparities in childhood asthma using a theoretically based, multifactorial model, which yielded several informative findings. Use of SEM analysis to examine between-group differences is more sophisticated than multiple regression because it allows the simultaneous estimation of model parameters, thus reducing standard errors of the parameters and yielding more precise estimates. SEM also provides a more powerful estimate of mediation than regression, a primary focus of these analyses. This model provides some preliminary support for the complex relationships that exist between ethnicity, experiential and health care provider factors, environmental context, and illness representations that affect health care seeking behaviors and, ultimately, children’s asthma health outcomes. Additional research is currently underway expanding this model and testing it in a multisite, 1-year longitudinal study. Knowledge gained from utilizing more complex models and SEM analytical methods will help identify key individual-level factors potentially leading to asthma health disparities and subsequently, fruitful targets for intervention.
Acknowledgment
This research was funded by the National Institute for Nursing Research (1RO1NR007905-01A2; PI: Yoos, H.) and the American Lung Association (SB-20474-N; PI: Feldman, J.) Dr. Sidora-Arcoleo is a faculty affiliate at the Arizona State University Southwest Interdisciplinary Research Center’s Center of Excellence for Health Disparities Research and Training. Data analysis and manuscript development were supported by funding from the National Institute on Minority Health and Health Disparities of the National Institutes of Health (NIMHD/NIH), award P20 MD002316-02,03 (F. Marsiglia, P.I.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMHD or the NIH. The authors would like to thank the families who participated in this study for their invaluable contributions, the research staff in Rochester and Bronx, NY for their work with these families, and April Hawthorne, MEd for her assistance in preparing and reviewing the manuscript.
Footnotes
Conflict of Interest Statement The authors have no conflicts of interest to declare.
Contributor Information
Kimberly Sidora-Arcoleo, Ohio State University College of Nursing, 1595 Neil Avenue, Columbus, OH 43210, USA, Arcoleo.1@osu.edu.
Jonathan M. Feldman, Ferkauf Graduate School of Psychology, Albert Einstein College of Medicine, Yeshiva University, Rousso Building 1300 Morris Park Avenue, Bronx, NY 10461, USA, jonathan.feldman@einstein.yu.edu
Denise Serebrisky, Jacobi Medical Center, Albert Einstein College of Medicine, Yeshiva University, 1400 Pelham Parkway, South Bronx, NY 10461, USA, dserebrisky@yahoo.com
Amanda Spray, Ferkauf Graduate School of Psychology, Yeshiva University, Rousso Building 1300 Morris Park Avenue, Bronx, NY 10461, USA amandaspray@gmail.com
References
- 1.Stewart KA, Higgins PC, McLaughlin CG, Williams TV, Granger E, Croghan TW. Differences in prevalence, treatment, and outcomes of asthma among a diverse population of children with equal access to care: Findings from a study in the military health system. Arch Pediatr Adolesc Med. 2010;164:720–726. doi: 10.1001/archpediatrics.2010.100. [DOI] [PubMed] [Google Scholar]
- 2.Akinbami LJ, Schoendorf KC. Trends in childhood asthma: Prevalence, health care utilization, and mortality. Pediatrics. 2002;110:315–322. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- 3.Akinbami LJ, LaFleur BJ, Schoendorf KC. Racial and income disparities in childhood asthma in the united states. Ambulatory Pediatrics. 2002;2:382–387. doi: 10.1367/1539-4409(2002)002<0382:raidic>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 4.Canino G, Koinis-Mitchell D, Ortega AN, McQuaid EL, Fritz GK, Alegria M. Asthma disparities in the prevalence, morbidity, and treatment of latino children. Soc Sci Med. 2006;63:2926–2937. doi: 10.1016/j.socscimed.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control. The state of childhood asthma, United States, 1980–2005. Advance Data. 2006;381:9. [PubMed] [Google Scholar]
- 6.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among hispanic children: Puerto rican children bear a disproportionate burden. Pediatrics. 2006;117:43–53. doi: 10.1542/peds.2004-1714. [DOI] [PubMed] [Google Scholar]
- 7.Pachter LM, Weller SC, Baer RD, et al. Variation in asthma beliefs and practices among mainland Puerto Ricans, Mexican-Americans, Mexicans, and Guatemalans. J Asthma. 2002;39:119–134. doi: 10.1081/jas-120002193. [DOI] [PubMed] [Google Scholar]
- 8.Kaptein AA, Hughes BM, Scharloo M, et al. Illness perceptions about asthma are determinants of outcome. J Asthma. 2008;45:459–464. doi: 10.1080/02770900802040043. [DOI] [PubMed] [Google Scholar]
- 9.Kaptein AA, Klok T, Moss-Morris R, Brand PL. Illness perceptions: Impact on self-management and control in asthma. Curr Opin Allergy Clin Immunol. 2010;10:194–199. doi: 10.1097/ACI.0b013e32833950c1. [DOI] [PubMed] [Google Scholar]
- 10.Global Initiative for Asthma. Global initiative for asthma: Global strategy for asthma management and prevention. Global Initiative for Asthma. 2006 GINA_WR2006:1-2-110 Accessed 09/03/08. [Google Scholar]
- 11.Insel KC, Meek PM, Leventhal H. Differences in illness representation among pulmonary patients and their providers. J Health Psychol. 2005;10:147–162. doi: 10.1177/1359105305048561. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Department of Health & Human Services: National Asthma Education Program. Expert Panel 3 Report: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: U.S. Department of Health & Human Services; 2007. [Google Scholar]
- 13.Yoos HL, Kitzman H, Henderson C, et al. The impact of the parental illness representation on disease management in childhood asthma. Nursing Research. 2007;56:167–174. doi: 10.1097/01.NNR.0000270023.44618.a7. [DOI] [PubMed] [Google Scholar]
- 14.van Dellen QM, van Aalderen WM, Bindels PJ, et al. Asthma beliefs among mothers and children from different ethnic origins living in Amsterdam, the Netherlands. BMC Public Health. 2008;8:380. doi: 10.1186/1471-2458-8-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halm EA, Mora P, Leventhal H. No symptoms, no asthma: The acute episodic disease belief is associated with poor self-management among inner-city adults with persistent asthma. Chest. 2006;129:573–580. doi: 10.1378/chest.129.3.573. [DOI] [PubMed] [Google Scholar]
- 16.Sidora-Arcoleo K, Feldman J, Serebrisky D, Spray A. Validation of the asthma illness representation scale (AIRS©) Journal of Asthma. 2010;47:33–40. doi: 10.3109/02770900903362668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sidora-Arcoleo K. Variations in Parental Illness Representations of Children with Asthma: The Impact on the Use of Complementary & Alternative Medicine and Symptom Severity. PhD thesis. Rochester: University of Rochester, School of Medicine & Dentistry; 2006. [Google Scholar]
- 18.Hill TD, Graham LM, Divgi V. Racial disparities in pediatric asthma: A review of the literature. Curr Allergy Asthma Rep. 2011;11:85–90. doi: 10.1007/s11882-010-0159-2. [DOI] [PubMed] [Google Scholar]
- 19.Diefenbach M, Leventhal H. The common-sense model of illness representations: Theoretical and practical considerations. Journal of social distress and the homeless. 1996;5:11–38. [Google Scholar]
- 20.Leventhal H, Diefenbach M, Leventhal EA. Illness cognition using common sense to understand treatment adherence and affect cognition interactions. Cognitive Therapy and Research. 1992;16:143–163. [Google Scholar]
- 21.Cameron LD, Leventhal H, editors. The Self-Regulation of Health and Illness Behavior. London, UK: Taylor & Francis; 2003. [Google Scholar]
- 22.Sutton S, Baum A, Johnston M, editors. Handbook of Health Psychology. London, UK: Sage Publications; 2004. [Google Scholar]
- 23.Peterson-Sweeney K, McMullen A, Yoos HL, Kitzman H. Parental perceptions of their child's asthma: Management and medication use. J Pediatr Health Care. 2003;17:118–125. doi: 10.1067/mph.2003.31. [DOI] [PubMed] [Google Scholar]
- 24.Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychol.Methods. 2010;15:209–233. doi: 10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- 25.Preacher KJ, Zhang Z, Zyphur MJ. Alternative methods for assessing mediation inn multilevel data: The advantages of multilevel SEM. Structural Equation Modeling. 2011;18:161–182. [Google Scholar]
- 26.Kline R. In: Structural models with Observed Variables and Path Analysis: I. Fundamentals, Recursive Models. Kenny DA, editor. New York: Guilford; 1998. pp. 95–154. [Google Scholar]
- 27.Kline R. Structural models with observed variables and path analysis: II nonrecursive models, multiple group analysis. In: Kenny DA, editor. Principles and Practice of Structural Equation. New York: Guilford; 1998. pp. 155–188. [Google Scholar]
- 28.Byrne BM. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- 29.Kenny D. [Accessed 06/13/2011];Measuring Model Fit. Available at: http://www.davidakenny.net/cm/fit.htm. [Google Scholar]
- 30.Preacher KJ, Coffman DL. [Accessed May 3, 2006];Computing power and minimum sample size for RMSEA [computer software] Available at: http://www.quantpsy.org. [Google Scholar]
- 31.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods [methods, mediation, intervening variable] 2002;7(1):83–84. 104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eviatar Z. Culture and brain organization. Brain and Cognition. Special Issue: Millennium issue. 2000;42:50–52. doi: 10.1006/brcg.1999.1159. [DOI] [PubMed] [Google Scholar]
- 33.Koriat A, Goldsmith M, Pansky A. Toward a psychology of memory accuracy. Annu Rev Psychol. 2000;51:481–537. doi: 10.1146/annurev.psych.51.1.481. [DOI] [PubMed] [Google Scholar]
- 34.Conn KM, Halterman JS, Fisher SG, Yoos HL, Chin NP, Szilagyi PG. Parental beliefs about medications and medication adherence among urban children with asthma. Ambul Pediatr. 2005;5:306–310. doi: 10.1367/A05-004R1.1. [DOI] [PubMed] [Google Scholar]
- 35.Feldman JM, McQuaid EL, Klein RB, et al. Symptom perception and functional morbidity across a one-year follow-up in pediatric asthma. Pediatr Pulmonol. 2007;42:339–347. doi: 10.1002/ppul.20584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Feldman JM, Eisenberg EJ, Oculato TM, Soto D, Serebrisky D, Crain EF. Asthma symptom perception and parental modeling among inner-city families. Paper presented at the annual meeting of the International Society for the Advancement of Respiratory Psychophysiology. 2006 [Google Scholar]
- 37.Galbraith AA, Smith LA, Bokhour B, et al. Asthma care quality for children with minority serving providers. Arch Pediatr Adolesc Med. 2010;164:38–45. doi: 10.1001/archpediatrics.2009.243. [DOI] [PMC free article] [PubMed] [Google Scholar]