Abstract
BACKGROUND
Regular use of aspirin after a diagnosis of colon cancer has been associated with a superior clinical outcome. Experimental evidence suggests that inhibition of prostaglandin-endoperoxide synthase 2 (PTGS2) (also known as cyclooxygenase-2) by aspirin down-regulates phosphatidylinositol 3-kinase (PI3K) signaling activity. We hypothesized that the effect of aspirin on survival and prognosis in patients with cancers characterized by mutated PIK3CA (the phosphatidylinositol-4,5-bisphosphonate 3-kinase, catalytic subunit alpha polypeptide gene) might differ from the effect among those with wild-type PIK3CA cancers.
METHODS
We obtained data on 964 patients with rectal or colon cancer from the Nurses’ Health Study and the Health Professionals Follow-up Study, including data on aspirin use after diagnosis and the presence or absence of PIK3CA mutation. We used a Cox proportional-hazards model to compute the multivariate hazard ratio for death. We examined tumor markers, including PTGS2, phosphorylated AKT, KRAS, BRAF, microsatellite instability, CpG island methylator phenotype, and methylation of long interspersed nucleotide element 1.
RESULTS
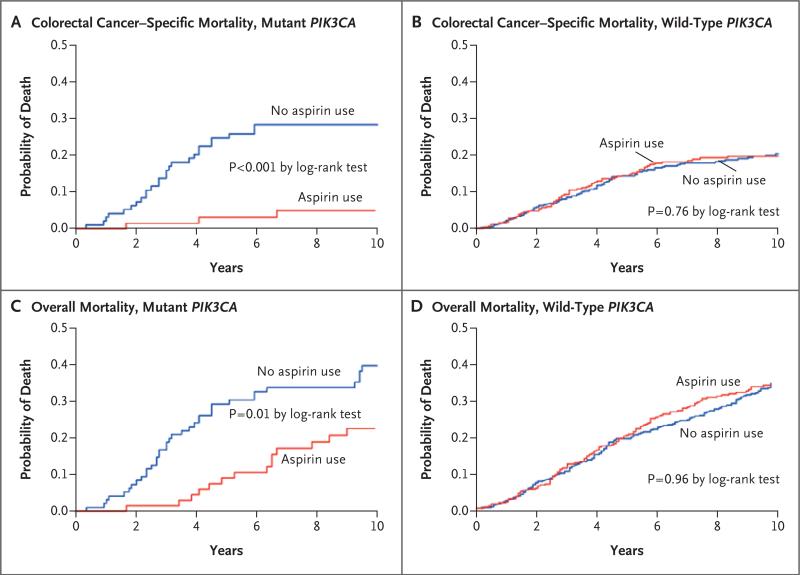
Among patients with mutated-PIK3CA colorectal cancers, regular use of aspirin after diagnosis was associated with superior colorectal cancer–specific survival (multivariate hazard ratio for cancer-related death, 0.18; 95% confidence interval [CI], 0.06 to 0.61; P<0.001 by the log-rank test) and overall survival (multivariate hazard ratio for death from any cause, 0.54; 95% CI, 0.31 to 0.94; P = 0.01 by the log-rank test). In contrast, among patients with wild-type PIK3CA, regular use of aspirin after diagnosis was not associated with colorectal cancer–specific survival (multivariate hazard ratio, 0.96; 95% CI, 0.69 to 1.32; P = 0.76 by the log-rank test; P = 0.009 for interaction between aspirin and PIK3CA variables) or overall survival (multivariate hazard ratio, 0.94; 95% CI, 0.75 to 1.17; P = 0.96 by the log-rank test; P = 0.07 for interaction).
CONCLUSIONS
Regular use of aspirin after diagnosis was associated with longer survival among patients with mutated-PIK3CA colorectal cancer, but not among patients with wild-type PIK3CA cancer. The findings from this molecular pathological epidemiology study suggest that the PIK3CA mutation in colorectal cancer may serve as a predictive molecular biomarker for adjuvant aspirin therapy. (Funded by The National Institutes of Health and others.)
Numerous observational and randomized, controlled studies have suggested a protective effect of regular use of aspirin on colorectal neoplasias.1-7 The favorable outcome that has been associated with aspirin use after colorectal cancer is diagnosed8-10 suggests that aspirin is a promising agent for adjuvant therapy. Accumulating data suggest that colorectal cancers are a heterogeneous group of diseases that potentially have differential responses to treatment.11 The effect of postdiagnosis aspirin use on survival appears to differ according to tumor expression of PTGS2 (HGNC:9605, the official symbol for prostaglandin-endoperoxide synthase 2, also known as cyclooxygenase-2) as assessed by immunohistochemical techniques.8 Considering the challenges in standardizing PTGS2 immunohistochemical assays across pathology laboratories, other molecular biomarkers — particularly those that can be assessed through a more standardized approach than immunohistochemistry — are needed to better identify patients with colorectal cancer who will derive a benefit from aspirin.
The phosphatidylinositol 3-kinase (PI3K) signaling pathway plays an important role in carcinogenesis.12 Mutations in PIK3CA (the gene encoding phosphatidylinositol-4,5-bisphospho nate 3-kinase, catalytic subunit alpha polypeptide) are present in approximately 15 to 20% of colorectal cancers.13-19 Up-regulation of PI3K enhances PTGS2 activity and prostaglandin E2 synthesis, resulting in inhibition of apoptosis in colon-cancer cells.20 Aspirin may suppress cancer-cell growth and induce apoptosis by blocking the PI3K pathway.21 We therefore hypothesized that the effect of aspirin on survival among patients with mutated-PIK3CA colorectal cancers might differ from the effect among those with wild-type PIK3CA tumors. To test this hypothesis, we used two U.S. nationwide prospective cohort studies with data on aspirin use, tumor molecular characteristics, and patient outcomes.
Methods
Study Design
We used data from two prospective cohort studies, the Nurses’ Health Study (NHS, involving 121,700 women who were enrolled in 1976) and the Health Professionals Follow-up Study (HPFS, involving 51,500 men who were enrolled in 1986).22,23 Every 2 years, participants were sent follow-up questionnaires to update information on lifestyle factors and to identify newly diagnosed cancers and other diseases. The National Death Index was used to ascertain deaths of study participants. The cause of death was assigned by study physicians. Paraffin-embedded tissue blocks were collected from hospitals where participants with colorectal cancer had undergone colorectal resection or endoscopic biopsy (for preoperatively treated rectal cancer). Tumor-tissue data, information on aspirin use, and survival data were available for 1097 patients with colorectal cancer that was diagnosed before July 1, 2006. Among these patients, we used data from 964 patients for whom information about the presence or absence of PIK3CA mutation, based on analysis of tumor tissue, was available. Patients were followed until death or January 2011, whichever came first.
Written informed consent was obtained from all study participants. Tissue collection and analyses were approved by the human subjects committees at the Harvard School of Public Health and Brigham and Women's Hospital. The last two authors were responsible for the study concept and design. All authors acquired, analyzed, and interpreted the data. The first two authors and the last two authors take responsibility for the integrity of the data and the accuracy of the data analysis and vouch for the fidelity of the study to the protocol.
Assessment of Aspirin Use
Assessment of aspirin use in the NHS and HPFS cohorts has been described in detail previously.8 In 1980, NHS participants were asked whether they regularly used aspirin in most weeks, as well as the dose and duration of use; thereafter, this information was updated biennially (except in 1986). Beginning in 1986, HPFS participants were asked whether they regularly used aspirin two or more times each week; after 1992, information on the average dose used each week was requested. In both cohorts, the use of standard-dose (325-mg) aspirin tablets was documented. After 1992, to reflect the increasing use of low-dose (81-mg) aspirin (baby aspirin), participants were asked to convert four low-dose tablets to one standard-dose tablet in their response. The reasons for aspirin use were documented, as described previously, and included headache, arthritis, and other musculoskeletal pain, as well as cardiovascular disease and its prevention.8 As described previously,8 aspirin use was defined as regular use of aspirin during most weeks, whereas nonuse of aspirin was defined as no regular use of aspirin during most weeks.
Analyses of PIK3CA, BRAF, KRAS, Microsatellite Instability, and DNA Methylation
DNA was extracted from paraffin-embedded tissues.15 Polymerase chain reaction and pyrosequencing of PIK3CA (exons 9 and 20),15,24KRAS (codons 12 and 13),25 and BRAF (codon 600)26 were performed as previously described. Microsatellite instability status was determined as previously described.27 Methylation analyses of long interspersed nucleotide element 1 (LINE-1) elements28,29 and of eight CpG island methylator phenotype–specific loci27 (CACNA1G, CDKN2A, CRABP1, IGF2 MLH1, NEUROG1, RUNX3, and SOCS1 with the use of the MethyLight technique30,31) were performed as previously described.
PTGS2 and Phosphorylated AKT Immunohistochemistry
Immunohistochemical analyses to detect PTGS2 and phosphorylated AKT (phospho-AKT) were performed as previously described,22,32 and details of the methods are described in the Supplementary Appendix, available with the full text of this article at NEJM.org.
Statistical Analysis
A detailed description of the statistical analysis is provided in the Supplementary Appendix. All reported P values are two-sided. There was no prespecified subgroup analysis. We performed 13 post hoc subgroup analyses (for two different end points); the results of 12 of these analyses are reported here (Table S1 in the Supplementary Appendix). Thus, up to two false positive findings would be expected by chance alone. The Kaplan–Meier method and log-rank test were performed for the survival analysis. In the analyses of colorectal cancer–specific mortality, data on deaths from causes other than colorectal cancer were censored. To control for confounding, we used Cox proportional-hazards models to calculate the hazard ratio for death according to aspirin use or nonuse and the presence or absence of tumor PIK3CA mutation. The significance of an interaction was assessed by means of the Wald test on the cross-product term of the aspirin and PIK3CA variables.
Results
Patients
Table 1 summarizes the baseline characteristics of the 964 patients with colorectal cancer, according to aspirin use or nonuse after diagnosis and the presence or absence of tumor PIK3CA mutation. KRAS mutations were associated with mutated-PIK3CA tumors, as previously described.15 As compared with patients who did not use aspirin before diagnosis, a higher proportion of patients who used aspirin before diagnosis also used it after diagnosis, as previously described.8 The proportion of mutated-PIK3CA tumors was 17% (in 70 of 413 patients) among patients who used aspirin before diagnosis and 17% (in 91 of 551 patients) among patients who did not use aspirin before diagnosis. There were 395 deaths overall, including 190 deaths from colorectal cancer. The median follow-up was 153 months (interquartile range, 104 to 195) among patients with data that were censored.
Table 1.
Baseline Characteristics of Patients with Colorectal Cancer, According to PIK3CA Mutation Status and Regular Use or Nonuse of Aspirin after Diagnosis.*
| Characteristic | All Patients (N = 964) | Wild-Type PIK3CA | Mutant PIK3CA | P Value | ||
|---|---|---|---|---|---|---|
| No Aspirin Use (N = 466) | Aspirin Use (N = 337) | No Aspirin Use (N = 95) | Aspirin Use (N = 66) | |||
| Sex — no. (%)† | 0.30 | |||||
| Male | 429 (44) | 195 (42) | 155 (46) | 44 (46) | 35 (53) | |
| Female | 535 (56) | 271 (58) | 182 (54) | 51 (54) | 31 (47) | |
| Age — yr | 68.0±8.6 | 67.5±8.4 | 69.1±8.5 | 69.1±8.0 | 69.1±10.1 | 0.12 |
| Year of diagnosis — no. (%) | 0.06 | |||||
| Before 1997 | 422 (44) | 224 (48) | 134 (40) | 40 (42) | 24 (36) | |
| 1997 or later | 542 (56) | 242 (52) | 203 (60) | 55 (58) | 42 (64) | |
| History of colorectal cancer in first-degree relative — no. (%) | 0.38 | |||||
| No | 777 (81) | 386 (83) | 266 (79) | 73 (77) | 52 (79) | |
| Yes | 187 (19) | 80 (17) | 71 (21) | 22 (23) | 14 (21) | |
| Body-mass index — no./total no. (%)‡ | 0.99 | |||||
| <30 | 788/963 (82) | 380/466 (82) | 276/337 (82) | 77/94 (82) | 55/66 (83) | |
| ≥30 | 175/963 (18) | 86/466 (18) | 61/337 (18) | 17/94 (18) | 11/66 (17) | |
| Aspirin use before diagnosis — no. (%) | <0.001 | |||||
| No | 551 (57) | 360 (77) | 100 (30) | 71 (75) | 20 (30) | |
| Yes | 413 (43) | 106 (23) | 237 (70) | 24 (25) | 46 (70) | |
| Tumor location — no./total no. (%) | 0.13 | |||||
| Rectum | 212/961 (22) | 118/465 (25) | 70/335 (21) | 14/95 (15) | 10/66 (15) | |
| Distal colon | 313/961 (33) | 148/465 (32) | 114/335 (34) | 29/95 (31) | 22/66 (33) | |
| Proximal colon | 436/961 (45) | 199/465 (43) | 151/335 (45) | 52/95 (55) | 34/66 (52) | |
| Disease stage — no. (%) | 0.01 | |||||
| I | 260 (27) | 112 (24) | 102 (30) | 19 (20) | 27 (41) | |
| II | 301 (31) | 159 (34) | 87 (26) | 36 (38) | 19 (29) | |
| III | 264 (27) | 128 (27) | 99 (29) | 23 (24) | 14 (21) | |
| IV | 64 (7) | 31 (7) | 18 (5) | 12 (13) | 3 (5) | |
| Unknown | 75 (8) | 36 (8) | 31 (9) | 5 (5) | 3 (5) | |
| Tumor differentiation — no./total no. (%) | 0.85 | |||||
| Well or moderately differentiated | 880/958 (92) | 422/461 (92) | 311/337 (92) | 85/94 (90) | 62/66 (94) | |
| Poorly differentiated | 78/958 (8) | 39/461 (8) | 26/337 (8) | 9/94 (10) | 4/66 (6) | |
| Microsatellite instability — no./total no. (%) | 0.84 | |||||
| None or low level | 800/952 (84) | 382/460 (83) | 283/332 (85) | 81/95 (85) | 54/65 (83) | |
| High level | 152/952 (16) | 78/460 (17) | 49/332 (15) | 14/95 (15) | 11/65 (17) | |
| CIMP — no./total no. (%) | 0.84 | |||||
| Low or negative | 755/916 (82) | 366/438 (84) | 264/323 (82) | 75/93 (81) | 50/62 (81) | |
| High | 161/916 (18) | 72/438 (16) | 59/323 (18) | 18/93 (19) | 12/62 (19) | |
| BRAF — no./total no. (%) | 0.94 | |||||
| Wild-type | 828/959 (86) | 400/464 (86) | 288/335 (86) | 84/95 (88) | 56/65 (86) | |
| Mutant | 131/959 (14) | 64/464 (14) | 47/335 (14) | 11/95 (12) | 9/65 (14) | |
| KRAS — no./total no. (%) | <0.001 | |||||
| Wild-type | 623/959 (65) | 317/463 (68) | 231/336 (69) | 44/95 (46) | 31/65 (48) | |
| Mutant | 336/959 (35) | 146/463 (32) | 105/336 (31) | 51/95 (54) | 34/65 (52) | |
| LINE-1 methylation level — % | 62.9±9.5 | 62.7±10.0 | 62.4±9.2 | 64.2±9.4 | 64.3±9.4 | 0.58 |
| PTGS2 expression — no./total no. (%) | 0.12 | |||||
| Negative | 315/798 (39) | 149/395 (38) | 104/276 (38) | 37/79 (47) | 25/48 (52) | |
| Positive | 483/798 (61) | 246/395 (62) | 172/276 (62) | 42/79 (53) | 23/48 (48) | |
| Phosphorylated AKT — no./total no. (%) | 0.02 | |||||
| Negative | 195/562 (35) | 102/266 (38) | 73/200 (36) | 11/58 (19) | 9/38 (24) | |
| Positive | 367/562 (65) | 164/266 (62) | 127/200 (63) | 47/58 (81) | 29/38 (76) | |
Plus–minus values are means ±SD. Aspirin use was defined as regular use of aspirin during most weeks, whereas aspirin nonuse was defined as no regular use of aspirin during most weeks. CIMP denotes CpG island methylator phenotype, and LINE-1 long interspersed nucleotide element 1.
Data for men were obtained from the Health Professionals Follow-up Study, and data for women were obtained from the Nurses’ Health Study.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Aspirin Use and Survival According to PIK3CA Mutation Status
We tested the hypothesis that the effect of post-diagnosis use of aspirin on survival might be stronger in mutated-PIK3CA colorectal cancer than in wild-type PIK3CA cancer (Fig. 1 and Table 2, and Table S2 in the Supplementary Appendix). Among patients with mutated-PIK3CA tumors, regular use of aspirin after diagnosis was associated with significantly longer cancer-specific survival (multivariate hazard ratio for cancer-related death, 0.18; 95% confidence interval [CI], 0.06 to 0.61; P<0.001 by the log-rank test). In contrast, among patients with wild-type PIK3CA tumors, regular use of aspirin after diagnosis was not associated with cancer-specific survival (multivariate hazard ratio for death, 0.96; 95% CI, 0.69 to 1.32; P = 0.76 by the log-rank test; P = 0.009 for the interaction). Although statistical power was limited, the effect of aspirin on survival among patients with mutated-PIK3CA tumors appeared consistent irrespective of the dose (data not shown).
Figure 1. Mortality among Patients with Colorectal Cancer, According to Regular Use or Nonuse of Aspirin after Diagnosis and PIK3CA Mutation Status.
Panels A and B show colorectal cancer–specific mortality among patients with mutant-PIK3CA tumors and those with wild-type PIK3CA tumors, respectively, and Panels C and D show overall mortality in the respective subgroups of patients.
Table 2.
Hazard Ratios for Death with Adjustment for Stage of Disease and Other Variables, According to Tumor PIK3CA Mutation Status and Use or Nonuse of Aspirin after Diagnosis.*
| PIK3CA | Total No. of Patients | Colorectal Cancer–Specific Mortality |
Overall Mortality |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Deaths | Univariate Hazard Ratio (95% CI) | P Value† | Hazard Ratio, Adjusted for Disease Stage (95% CI) | P Value† | Multivariate Hazard Ratio, Adjusted for Disease Stage (95% CI) | P Value† | No. of Deaths | Univariate Hazard Ratio (95% CI) | P Value† | Hazard Ratio, Adjusted for Disease Stage (95% CI) | P Value† | Multivariate Hazard Ratio, Adjusted for Disease Stage (95% CI) | P Value† | ||
| Wild-type | 0.003 | 0.01 | 0.009 | 0.02 | 0.06 | 0.07 | |||||||||
| No aspirin use | 466 | 96 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 196 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | ||||||
| Aspirin use | 337 | 65 | 0.95 (0.69–1.30) | 0.93 (0.68–1.28) | 0.96 (0.69–1.32) | 137 | 1.01 (0.81–1.25) | 1.01 (0.81–1.25) | 0.94 (0.75–1.17) | ||||||
| Mutant | |||||||||||||||
| No aspirin use | 95 | 26 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 44 | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | ||||||
| Aspirin use | 66 | 3 | 0.14 (0.04–0.47) | 0.18 (0.05–0.60) | 0.18 (0.06–0.61) | 18 | 0.49 (0.28–0.85) | 0.57 (0.33–0.98) | 0.54 (0.31–0.94) | ||||||
The multivariate Cox regression model, stratified according to and adjusted for disease stage, initially included age, sex, year of diagnosis, time from diagnosis to first measurement of aspirin use after diagnosis (in months), regular use or nonuse of aspirin before diagnosis, tumor location, tumor differentiation, body-mass index, microsatellite instability status, CpG island methylator phenotype, KRAS mutation, BRAF mutation, LINE-1 (long interspersed nucleotide element-1) methylation, and the presence or absence of PTGS2 expression. A backward-elimination model with a threshold of P = 0.05 was used to select variables in the final models. CI denotes confidence interval.
P values are for the interaction of aspirin use and PIK3CA mutation.
Because only three colorectal cancer–specific deaths occurred among 66 patients with mutated-PIK3CA tumors who used aspirin after diagnosis, the log-rank or Cox regression analysis may not have yielded a robust P value. We therefore used Fisher's exact test to examine the association between aspirin use after diagnosis and 5-year survival according to the presence or absence of tumor PIK3CA mutation (Table 3). Among patients with mutated-PIK3CA tumors, 23 of 90 patients who did not use aspirin after diagnosis (26%) died within 5 years after diagnosis, whereas only 2 of 62 regular users of aspirin after diagnosis (3%) died within 5 years after diagnosis (P<0.001). In contrast, among patients with wild-type PIK3CA tumors, the 5-year cumulative colorectal cancer–specific mortality was the same (15%) for users and nonusers of aspirin after diagnosis (P = 0.92).
Table 3.
Colorectal Cancer–Specific Survival at 5 Years, According to Tumor PIK3CA Mutation Status and Use or Nonuse of Aspirin after Diagnosis.*
| PIK3CA | No. of Patients | Dead at 5 Yr after Diagnosis | Alive at 5 Yr after Diagnosis | P Value |
|---|---|---|---|---|
| number (percent) | ||||
| Wild-type | 0.92 | |||
| No aspirin use | 440 | 65 (15) | 375 (85) | |
| Aspirin use | 319 | 48 (15) | 271 (85) | |
| Mutant | <0.001 | |||
| No aspirin use | 90 | 23 (26) | 67 (74) | |
| Aspirin use | 62 | 2 (3) | 60 (97) | |
P values were calculated with the use of Fisher's exact test.
We obtained information on aspirin use after diagnosis with the use of a biennial questionnaire, and some patients with stage IV disease did not survive long enough to be included in our analysis; this might have resulted in selection bias in favor of patients with indolent stage IV disease. Therefore, we performed a sensitivity analysis limited to patients with stage I, II, or III disease (excluding patients with stage IV disease), which yielded similar results (Table S3 in the Supplementary Appendix). Results of analyses limited to stage II or III disease and to stage III disease alone are included in Tables S4 and S5 in the Supplementary Appendix, respectively.
We performed an exploratory analysis to determine whether aspirin use before diagnosis might have modified the interactive prognostic association between aspirin use after diagnosis and tumor PIK3CA mutation (Table 4, and Table S6 in the Supplementary Appendix). Among patients with wild-type PIK3CA tumors, regular use of aspirin after diagnosis was not significantly associated with colorectal cancer–specific or overall survival, irrespective of aspirin use before diagnosis. The small number of deaths among patients with mutated-PIK3CA tumors who used aspirin after diagnosis precluded robust statistical assessments.
Table 4.
Colorectal-Cancer Mortality, According to Tumor PIK3CA Mutation Status and Aspirin Use or Nonuse before Diagnosis and after Diagnosis.*
| Variable | No. of Patients | Colorectal Cancer–Specific Mortality | Overall Mortality | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of Events | Univariate Hazard Ratio (95% CI) | Hazard Ratio, Adjusted for Disease Stage (95% CI) | Multivariate Hazard Ratio, Adjusted for Disease Stage (95% CI) | No. of Events | Univariate Hazard Ratio (95% CI) | Hazard Ratio, Adjusted for Disease Stage (95% CI) | Multivariate Hazard Ratio, Adjusted for Disease Stage (95% CI) | ||
| Wild-type PIK3CA | |||||||||
| No aspirin use before diagnosis | |||||||||
| No aspirin use after diagnosis | 360 | 71 | 1 (referent) | 1 (referent) | 1 (referent) | 147 | 1 (referent) | 1 (referent) | 1 (referent) |
| Aspirin use after diagnosis | 100 | 17 | 0.84 (0.49–1.43) | 0.82 (0.48–1.39) | 0.90 (0.53–1.54) | 41 | 0.99 (0.70–1.39) | 0.98 (0.69–1.39) | 0.97 (0.68–1.37) |
| Aspirin use before diagnosis | |||||||||
| No aspirin use after diagnosis | 106 | 25 | 1 (referent) | 1 (referent) | 1 (referent) | 49 | 1 (referent) | 1 (referent) | 1 (referent) |
| Aspirin use after diagnosis | 237 | 48 | 0.88 (0.54–1.43) | 0.93 (0.57–1.52) | 0.92 (0.56–1.51) | 96 | 0.92 (0.66–1.31) | 0.96 (0.68–1.36) | 0.85 (0.60–1.21) |
| Mutant PIK3CA | |||||||||
| No aspirin use before diagnosis | |||||||||
| No aspirin use after diagnosis | 71 | 20 | 1 (referent) | 1 (referent) | 1 (referent) | 34 | 1 (referent) | 1 (referent) | 1 (referent) |
| Aspirin use after diagnosis | 20 | 1 | 0.16 (0.02–1.17) | 0.20 (0.03–1.46) | 0.28 (0.04–2.10) | 6 | 0.57 (0.24–1.35) | 0.63 (0.26–1.51) | 0.59 (0.24–1.41) |
| Aspirin use before diagnosis | |||||||||
| No aspirin use after diagnosis | 24 | 6 | 1 (referent) | 1 (referent) | 1 (referent) | 10 | 1 (referent) | 1 (referent) | 1 (referent) |
| Aspirin use after diagnosis | 46 | 2 | 0.15 (0.03–0.74) | 0.22 (0.04–1.10) | 0.18 (0.04–0.92) | 12 | 0.54 (0.23–1.24) | 0.68 (0.29–1.58) | 0.60 (0.26–1.40) |
The multivariate Cox regression model, stratified according to and adjusted for disease stage, initially included age, sex, year of diagnosis, time from diagnosis to first measurement of aspirin use after diagnosis (in months), regular use or nonuse of aspirin before diagnosis, tumor location, tumor differentiation, body-mass index, microsatellite instability status, CpG island methylator phenotype, KRAS mutation, BRAF mutation, LINE-1 (long interspersed nucleotide element-1) methylation, and the presence or absence of PTGS2 expression. A backward-elimination model with a threshold of P=0.05 was used to select variables in the final models.
Aspirin Use and Survival According to PIK3CA Mutation and PTGS2 Expression Status
Our previous study8 showed that regular use of aspirin after diagnosis was associated with reduced mortality from colorectal cancer, especially among patients with PTGS2-positive tumors. Thus, as a further exploratory analysis, we examined the relationship between aspirin use after diagnosis and survival according to combined PTGS2 and PIK3CA status (Table S7 in the Supplementary Appendix). In patients with wild-type PIK3CA tumors, aspirin use after diagnosis, even among those with PTGS2-positive tumors, did not appear to be significantly associated with survival. However, the effect of aspirin appeared to be stronger among patients with both mutated-PIK3CA and PTGS2-positive tumors, although the number of events in patients with mutated-PIK3CA tumors was too small to perform a robust statistical analysis.
Aspirin Use and Survival According to PIK3CA Mutation Status and Other Selected Variables
We conducted exploratory analyses of aspirin use after diagnosis and patient survival according to PIK3CA mutation status and other selected variables, limiting these analyses to patients with microsatellite-stable cancer. The results (Table S8 in the Supplementary Appendix) are similar to the results of the primary analysis (Table 2).
Next, we performed an analysis stratified according to the status of phospho-AKT expression (Table S9 in the Supplementary Appendix). Also, because the frequency of PIK3CA mutation may gradually increase along colorectal subsites from the rectum to the ascending colon,33 we performed an analysis according to tumor location (Table S10 in the Supplementary Appendix). However, in both analyses, statistical power was limited because of the small number of deaths among patients with mutated-PIK3CA tumors.
NSAID Use and Survival According to PIK3CA Mutation Status
We considered the possibility that concurrent use of a nonsteroidal antiinflammatory drug (NSAID) may have confounded our associations. However, inclusion of regular use of NSAIDs in our multivariate models did not materially alter our effect estimates for the association between aspirin use after diagnosis and survival. In exploratory analyses of regular use of NSAIDs after diagnosis and survival according to the presence or absence of PIK3CA mutation (Table S11 in the Supplementary Appendix), there was no significant interaction between NSAID use and PIK3CA status (P = 0.48 for interaction).
Discussion
We found that tumor PIK3CA mutation and regular use of aspirin after diagnosis had a significant interactive effect on survival among patients with colorectal cancer. Specifically, among patients with mutated-PIK3CA tumors, regular use of aspirin after diagnosis was associated with significantly increased survival. In contrast, patients with wild-type PIK3CA tumors did not appear to derive a benefit from aspirin use after diagnosis. In addition, the effect of aspirin appeared to be most pronounced in patients who had tumors with both PIK3CA mutation and PTGS2 expression. Our data support the hypothesis that aspirin use after diagnosis may have a differential effect on survival, depending on the presence or absence of tumor PIK3CA mutation.
Our data suggest that regular use of aspirin is suitable for testing as an adjuvant treatment in patients with mutated-PIK3CA cancers and that PIK3CA mutation status may serve as a tumor biomarker that predicts the response to adjuvant aspirin treatment. Our data also suggest that even relatively low doses of aspirin may prolong survival among patients with mutated-PIK3CA cancer. Nevertheless, because of the small numbers of deaths in some subgroups, we must be cautious in interpreting our data. Furthermore, since our current analysis was not prespecified when the cohorts were initially enrolled, and testing of multiple hypotheses through subgroup analyses increases the possibility of a false positive result,34 our findings need to be confirmed by analyses of independent data sets.
A possible alternative explanation for our findings is that aspirin use before diagnosis, which is related to aspirin use after diagnosis, may be associated with the occurrence of indolent tumor subtypes, particularly among mutated-PIK3CA tumors. We previously reported that aspirin use before diagnosis by itself was not associated with prognosis among patients with colorectal cancer.8 In our current analysis, we analyzed the effect of aspirin use after diagnosis according to both PIK3CA mutation and aspirin use before diagnosis (Table 3). Although statistical power was limited, the results suggest that the association between aspirin use after diagnosis and increased survival is probably not explained by aspirin use before diagnosis. Colorectal cancers are a heterogenous group of complex diseases, as indicated by molecular pathological epidemiology35-37 and the unique tumor principle.11 Thus, it is not possible to explain tumor behavior on the basis of one or a few biomarkers alone. The interplay among inflammation, aspirin, and tumor molecular features is suggested by the current study and our previous studies.8,22
The proportion of mutated-PIK3CA tumors was the same (17%) among users and nonusers of aspirin before diagnosis, despite our main finding that aspirin use after diagnosis appeared to prevent progression of disease in patients with mutated-PIK3CA tumors. One reason for this apparent discrepancy may be related to tumor evolution. During tumor evolution, tumor cells are subject to changes in their own genome, epigenome, proteome, and metabolome and to changes in the local microenvironment.11 Thus, their dependence on an inflammatory microenvironment probably varies according to the specific phase of tumor evolution, which may result in the differential interaction of aspirin use and PIK3CA mutation in the early phase of evolution (before diagnosis) versus the late phase (after diagnosis).
Our previous data8 suggested that patients who use aspirin before diagnosis may not benefit from aspirin use after diagnosis. However, our current study provides evidence of a beneficial effect of aspirin use after diagnosis if the colorectal cancer has PIK3CA mutation, irrespective of aspirin use or nonuse before diagnosis. This finding may prove to have substantial implications for decisions about treatment.
In our current study, the strongest effect of aspirin use was in patients who had tumors with both PIK3CA mutation and PTGS2 expression. We must interpret these results with caution, however, because of the multiple subgroup analyses and limited statistical power. Nonetheless, our current findings are not inconsistent with those of our previous study,8 which showed a strong antitumor effect of aspirin on PTGS2-positive colorectal cancer. Experimental evidence supports cross-talk between the PI3K and PTGS2 pathways.20,21 In combination with the experimental observation that aspirin can induce cell apoptosis through PTGS2-independent pathways,38,39 our data may provide support for an antitumor effect of aspirin in addition to that of PTGS2 inhibition, although the exact mechanisms need to be clarified.
A “colorectal continuum” hypothesis that is distinctive from the long-standing “proximal versus distal colorectum” model has recently been proposed.33,40 The frequencies of molecular features such as a high level of microsatellite instability and extensive CpG island methylation, as well as BRAF and PIK3CA mutations, appear to increase continuously from the rectum to ascending colon.33 Considering a gradual transition of gut biogeography, the inhibitory effect of aspirin on cancer may differ according to both the specific site of the tumor and its molecular features. Our current study lacked statistical power to examine effect modification according to both PIK3CA mutation status and the specific tumor site, and larger studies should address this question.
Our study has several strengths. We collected data on aspirin use both before diagnosis and after diagnosis; this allowed us to examine the potential influence of the timing of aspirin use in relation to the cancer diagnosis. Since all study participants were health professionals with knowledge of medications, the accuracy of self-reported information on aspirin use was probably high. Furthermore, our comprehensive molecular pathological epidemiology database,35-37 with accumulated data on various lifestyle factors, tumor molecular features, and clinical outcomes, provided a unique opportunity to test our specific hypothesis of the interactive prognostic effect between aspirin use and PIK3CA mutation.
Our current study also has some limitations. Data on cancer treatment were limited. Given that all patients received a diagnosis before July 1, 2006, we assume that chemotherapy use did not differ substantially according to PIK3CA mutation status, information that was unavailable to the treating physicians. Moreover, our multivariable survival analysis was adjusted for cancer stage (I, II, III, or IV), and decision making for treatment was largely based on the stage of the cancer. In addition, we had limited information about cancer recurrence; nevertheless, with adequate follow-up time in the current study, colorectal cancer–specific survival served as a reasonable measure of the colorectal cancer–specific outcome.
In conclusion, this study suggests that regular use of aspirin after the diagnosis of colorectal cancer is significantly associated with increased survival among patients with mutated-PIK3CA tumors but not among patients with wild-type PIK3CA tumors. This relationship appeared to be independent of aspirin use before diagnosis. PIK3CA mutation may serve as a tumor biomarker that predicts the response to the initiation of aspirin therapy in patients with newly diagnosed colorectal cancer.
Supplementary Material
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Supported by grants from the National Institutes of Health (P01 CA87969 and P01 CA55075; P50 CA127003, to Dr. Fuchs; R01 CA149222, to Dr. Meyerhardt; R01 CA137178, to Dr. Chan; and R01 CA151993, to Dr. Ogino), the Bennett Family Fund for Targeted Therapies Research, and the Entertainment Industry Foundation through the National Colorectal Cancer Research Alliance; by the Frank Knox Memorial Fellowship at Harvard University and a fellowship from the Chief Scientist Office, Scotland (to Dr. Lochhead); and by a Damon Runyon Clinical Investigator Award (to Dr. Chan).
We thank the participants and staff of the Nurses’ Health Study and the Health Professionals Follow-up Study for their contributions and the participating state cancer registries for their help.
Footnotes
The following two groups of authors contributed equally to this article: Drs. Liao, Lochhead, and Nishihara and Drs. Fuchs, Chan, and Ogino.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Sandler RS, Halabi S, Baron JA, et al. A randomized trial of aspirin to prevent colorectal adenomas in patients with previous colorectal cancer. N Engl J Med. 2003;348:883–90. doi: 10.1056/NEJMoa021633. [Erratum, N Engl J Med 2003;348:1939.]
- 2.Burn J, Gerdes AM, Macrae F, et al. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomised controlled trial. Lancet. 2011;378:2081–7. doi: 10.1016/S0140-6736(11)61049-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Algra AM, Rothwell PM. Effects of regular aspirin on long-term cancer incidence and metastasis: a systematic comparison of evidence from observational studies versus randomised trials. Lancet Oncol. 2012;13:518–27. doi: 10.1016/S1470-2045(12)70112-2. [DOI] [PubMed] [Google Scholar]
- 4.Din FV, Theodoratou E, Farrington SM, et al. Effect of aspirin and NSAIDs on risk and survival from colorectal cancer. Gut. 2010;59:1670–9. doi: 10.1136/gut.2009.203000. [DOI] [PubMed] [Google Scholar]
- 5.Dubé C, Rostom A, Lewin G, et al. The use of aspirin for primary prevention of colorectal cancer: a systematic review prepared for the U.S. Preventive Services Task Force. Ann Intern Med. 2007;146:365–75. doi: 10.7326/0003-4819-146-5-200703060-00009. [DOI] [PubMed] [Google Scholar]
- 6.Flossmann E, Rothwell PM. Effect of aspirin on long-term risk of colorectal cancer: consistent evidence from randomised and observational studies. Lancet. 2007;369:1603–13. doi: 10.1016/S0140-6736(07)60747-8. [DOI] [PubMed] [Google Scholar]
- 7.Baron JA, Cole BF, Sandler RS, et al. A randomized trial of aspirin to prevent colorectal adenomas. N Engl J Med. 2003;348:891–9. doi: 10.1056/NEJMoa021735. [DOI] [PubMed] [Google Scholar]
- 8.Chan AT, Ogino S, Fuchs CS. Aspirin use and survival after diagnosis of colorectal cancer. JAMA. 2009;302:649–58. doi: 10.1001/jama.2009.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rothwell PM, Wilson M, Elwin CE, et al. Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet. 2010;376:1741–50. doi: 10.1016/S0140-6736(10)61543-7. [DOI] [PubMed] [Google Scholar]
- 10.Rothwell PM, Wilson M, Price JF, Belch JF, Meade TW, Mehta Z. Effect of daily aspirin on risk of cancer metastasis: a study of incident cancers during randomised controlled trials. Lancet. 2012;379:1591–601. doi: 10.1016/S0140-6736(12)60209-8. [DOI] [PubMed] [Google Scholar]
- 11.Ogino S, Fuchs CS, Giovannucci E. How many molecular subtypes? Implications of the unique tumor principle in personalized medicine. Expert Rev Mol Diagn. 2012;12:621–8. doi: 10.1586/erm.12.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samuels Y, Wang Z, Bardelli A, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science. 2004;304:554. doi: 10.1126/science.1096502. [DOI] [PubMed] [Google Scholar]
- 13.Lièvre A, Blons H. Laurent-Puig P. Oncogenic mutations as predictive factors in colorectal cancer. Oncogene. 2010;29:3033–43. doi: 10.1038/onc.2010.89. [DOI] [PubMed] [Google Scholar]
- 14.Barault L, Veyrie N, Jooste V, et al. Mutations in the RAS-MAPK, PI(3)K (phosphatidylinositol-3-OH kinase) signaling network correlate with poor survival in a population-based series of colon cancers. Int J Cancer. 2008;122:2255–9. doi: 10.1002/ijc.23388. [DOI] [PubMed] [Google Scholar]
- 15.Liao X, Morikawa T, Lochhead P, et al. Prognostic role of PIK3CA mutation in colorectal cancer: cohort study and literature review. Clin Cancer Res. 2012;18:2257–68. doi: 10.1158/1078-0432.CCR-11-2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mao C, Yang ZY, Hu XF, Chen Q, Tang JL. PIK3CA exon 20 mutations as a potential biomarker for resistance to anti-EGFR monoclonal antibodies in KRAS wild-type metastatic colorectal cancer: a systematic review and meta-analysis. Ann Oncol. 2012;23:1518–25. doi: 10.1093/annonc/mdr464. [DOI] [PubMed] [Google Scholar]
- 17.De Roock W, Claes B, Bernasconi D, et al. Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol. 2010;11:753–62. doi: 10.1016/S1470-2045(10)70130-3. [DOI] [PubMed] [Google Scholar]
- 18.Whitehall VL, Rickman C, Bond CE, et al. Oncogenic PIK3CA mutations in colorectal cancers and polyps. Int J Cancer. 2012;131:813–20. doi: 10.1002/ijc.26440. [DOI] [PubMed] [Google Scholar]
- 19.He Y, Van't Veer LJ, Mikolajewska-Hanclich I, et al. PIK3CA mutations pre dict local recurrences in rectal cancer patients. Clin Cancer Res. 2009;15:6956–62. doi: 10.1158/1078-0432.CCR-09-1165. [DOI] [PubMed] [Google Scholar]
- 20.Kaur J, Sanyal SN. PI3-kinase/Wnt association mediates COX-2/PGE(2) pathway to inhibit apoptosis in early stages of colon carcinogenesis: chemoprevention by diclofenac. Tumour Biol. 2010;31:623–31. doi: 10.1007/s13277-010-0078-9. [DOI] [PubMed] [Google Scholar]
- 21.Uddin S, Ahmed M, Hussain A, et al. Cyclooxygenase-2 inhibition inhibits PI3K/AKT kinase activity in epithelial ovarian cancer. Int J Cancer. 2010;126:382–94. doi: 10.1002/ijc.24757. [DOI] [PubMed] [Google Scholar]
- 22.Chan AT, Ogino S, Fuchs CS. Aspirin and the risk of colorectal cancer in relation to the expression of COX-2. N Engl J Med. 2007;356:2131–42. doi: 10.1056/NEJMoa067208. [DOI] [PubMed] [Google Scholar]
- 23.Morikawa T, Kuchiba A, Yamauchi M, et al. Association of CTNNB1 (beta-catenin) alterations, body mass index, and physical activity with survival in patients with colorectal cancer. JAMA. 2011;305:1685–94. doi: 10.1001/jama.2011.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nosho K, Kawasaki T, Ohnishi M, et al. PIK3CA mutation in colorectal cancer: relationship with genetic and epigenetic alterations. Neoplasia. 2008;10:534–41. doi: 10.1593/neo.08336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ogino S, Kawasaki T, Brahmandam M, et al. Sensitive sequencing method for KRAS mutation detection by pyrosequencing. J Mol Diagn. 2005;7:413–21. doi: 10.1016/S1525-1578(10)60571-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ogino S, Kawasaki T, Kirkner GJ, Loda M, Fuchs CS. CpG island methylator phenotype-low (CIMP-low) in colorectal cancer: possible associations with male sex and KRAS mutations. J Mol Diagn. 2006;8:582–8. doi: 10.2353/jmoldx.2006.060082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogino S, Nosho K, Kirkner GJ, et al. CpG island methylator phenotype, micro-satellite instability, BRAF mutation and clinical outcome in colon cancer. Gut. 2009;58:90–6. doi: 10.1136/gut.2008.155473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ogino S, Nosho K, Kirkner GJ, et al. A cohort study of tumoral LINE-1 hypomethylation and prognosis in colon cancer. J Natl Cancer Inst. 2008;100:1734–8. doi: 10.1093/jnci/djn359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Irahara N, Nosho K, Baba Y, et al. Precision of pyrosequencing assay to measure LINE-1 methylation in colon cancer, normal colonic mucosa, and peripheral blood cells. J Mol Diagn. 2010;12:177–83. doi: 10.2353/jmoldx.2010.090106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weisenberger DJ, Siegmund KD, Campan M, et al. CpG island methylator phenotype underlies sporadic microsatellite instability and is tightly associated with BRAF mutation in colorectal cancer. Nat Genet. 2006;38:787–93. doi: 10.1038/ng1834. [DOI] [PubMed] [Google Scholar]
- 31.Ogino S, Kawasaki T, Brahmandam M, et al. Precision and performance characteristics of bisulfite conversion and real-time PCR (MethyLight) for quantitative DNA methylation analysis. J Mol Diagn. 2006;8:209–17. doi: 10.2353/jmoldx.2006.050135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baba Y, Nosho K, Shima K, et al. Phosphorylated AKT expression is associated with PIK3CA mutation, low stage, and favorable outcome in 717 colorectal cancers. Cancer. 2011;117:1399–408. doi: 10.1002/cncr.25630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yamauchi M, Morikawa T, Kuchiba A, et al. Assessment of colorectal cancer molecular features along bowel subsites challenges the conception of distinct di chotomy of proximal versus distal colorectum. Gut. 2012;61:847–54. doi: 10.1136/gutjnl-2011-300865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang R, Lagakos SW, Ware JH, Hunter DJ, Drazen JM. Statistics in medicine — reporting of subgroup analyses in clinical trials. N Engl J Med. 2007;357:2189–94. doi: 10.1056/NEJMsr077003. [DOI] [PubMed] [Google Scholar]
- 35.Ogino S, Stampfer M. Lifestyle factors and microsatellite instability in colorectal cancer: the evolving field of molecular pathological epidemiology. J Natl Cancer Inst. 2010;102:365–7. doi: 10.1093/jnci/djq031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ogino S, Chan AT, Fuchs CS, Giovannucci E. Molecular pathological epidemiology of colorectal neoplasia: an emerging transdisciplinary and interdisciplinary field. Gut. 2011;60:397–411. doi: 10.1136/gut.2010.217182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ogino S, Galon J, Fuchs CS, Dranoff G. Cancer immunology — analysis of host and tumor factors for personalized medicine. Nat Rev Clin Oncol. 2011;8:711–9. doi: 10.1038/nrclinonc.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dikshit P, Chatterjee M, Goswami A, Mishra A, Jana NR. Aspirin induces apoptosis through the inhibition of protea-some function. J Biol Chem. 2006;281:29228–35. doi: 10.1074/jbc.M602629200. [DOI] [PubMed] [Google Scholar]
- 39.Lu M, Strohecker A, Chen F, et al. Aspirin sensitizes cancer cells to TRAIL-induced apoptosis by reducing survivin levels. Clin Cancer Res. 2008;14:3168–76. doi: 10.1158/1078-0432.CCR-07-4362. [DOI] [PubMed] [Google Scholar]
- 40.Yamauchi M, Lochhead P, Morikawa T, et al. Colorectal cancer: a tale of two sides or a continuum? Gut. 2012;61:794–7. doi: 10.1136/gutjnl-2012-302014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.