Abstract
Background
Hemodialysis(HD) access is considered a critical and actionable determinant of morbidity, with a growing literature suggesting that initial HD access type is an important marker of long term outcomes. Accordingly, we examined HD access during the incident dialysis period, focusing on infection risk and successful fistula creation over the first dialysis year.
Study Design
Longitudinal cohort
Setting & Participants
All United States adults admitted to Fresenius Medical Care North America facilities within 15 days of first maintenance dialysis session between January 1 and December 31, 2007.
Predictor
Vascular access type at HD initiation
Outcomes
Vascular access type at 90 days and at the end of the first year on HD, bloodstream infection within the first year by access type, and catheter complication rate.
Results
Amongst the 25,003 incident dialysis patients studied, 19,622(78.5%) initiated dialysis with a catheter, 4,151(16.6%) with a fistula, and 1,230(4.9%) with a graft. At 90 days, 14,105(69.7%) had a catheter, 4432(21.9%) patients had a fistula, and 1705(8.4%) had a graft. Functioning fistulas and grafts at dialysis initiation had first year failure rates of 10% and 15%, respectively. Grafts were seldom replaced by fistulas (3%), while 7,064 (47.6%) of all patients who initiated with a catheter alone still had only a catheter at 1 year. Overall, 3,327 (13.3%) patients had at least one positive blood culture during follow-up, with the risk being similar between fistula and graft groups, but approximately 3-fold higher in patients with a catheter (p<0.001 for either comparison). Nearly one in three catheters (32.5%) will require TPA use by median time of 41 days, with 59% requiring more than one TPA administration.
Limitations
Potential underestimation of bacteremia because follow-up blood culture results did not include samples sent to local laboratories.
Conclusions
Among a large and representative population of incident US dialysis patients, catheter use remains very high over the first year of hemodialysis care, and is associated with high mechanical complication and blood stream infection rates.
Vascular access in hemodialysis (HD) patients is generally regarded as a critical and actionable determinant of morbidity and mortality. Studies have consistently shown that, compared with arteriovenous grafts (AVGs), native arteriovenous fistulas (AVFs) are associated with enhanced survival, fewer occurrences of mechanical and infectious complications, longer patency and reduced health care costs (1–4), and that both are better than central venous catheters.(5, 6) With the advances made by the Fistula First (www.fistulafirst.org) national movement, the rate of AVF use in prevalent HD patients has increased substantially, but 82% of US patients still initiate HD by means of a catheter, and most of these (63.2% of all incident patients) have no concomitant arteriovenous access maturing when dialysis is begun.(7) Even among patients followed up by nephrologists for 6 months or more, 75% initiate HD with a catheter.
The high maturation failure rate for AVF, in particular, prolongs the duration of catheter exposure (8–10), which increases risk of catheter related infections and complications. (11, 12) Our recent work,(13) along with other published data(10, 14, 15), have suggested that initial HD access type is an important marker of long term morbidity and mortality, which warrants a closer examination of its impact during the incident dialysis period. Published studies examining vascular access during the incident dialysis period are hampered by small sample size (5, 16) or cross sectional design, or else are outdated. To add clarity to the contemporary literature in the era of the Fistula First initiative, we examined HD access type at the time of initiation, transitions in access type over the first year on HD, and how these issues are associated with infectious and non-infectious catheter related complications utilizing data from a contemporary national cohort of incident HD patients.
Methods
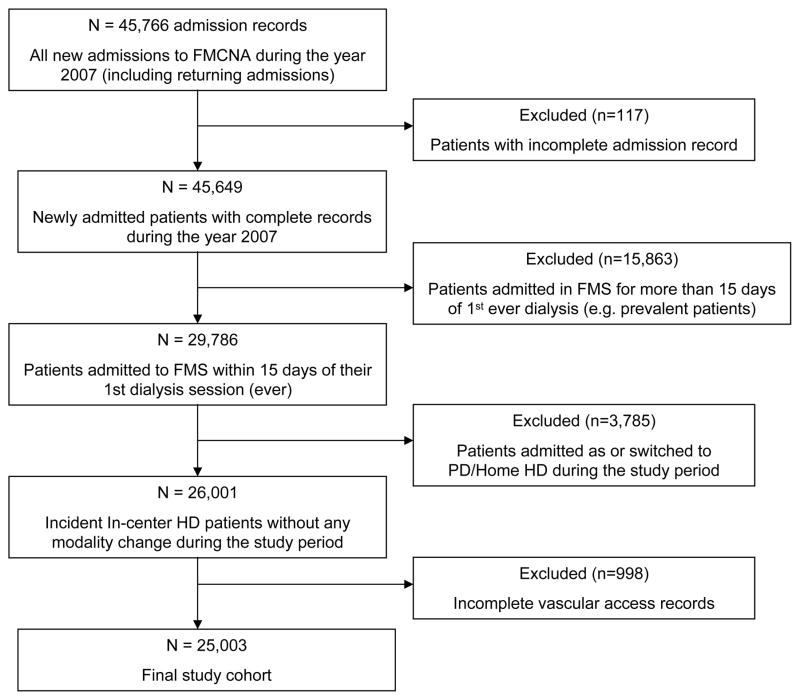
Arteriovenous access outcomes in the first year after dialysis initiation were analyzed among 25,003 incident HD patients who were admitted to Fresenius Medical Care North America (FMCNA) facilities between January 1 and December 31, 2007, and within 15 days of their first dialysis session after beginning maintenance HD (Figure 1). The 15-day inclusion period was used to delineate a well-defined incident population with newly utilized vascular accesses, which minimized the chances of missing antecedent access events or complications. The majority of patients excluded by this criterion were those who were new to FMCNA, but had previously undergone dialysis elsewhere.
Figure 1.
Cohort Selection. FMCNA, Fresenius Medical Care North America; FMS, ; HD, hemodialysis; PD, peritoneal dialysis.
Vascular access was recorded on admission and classified as AVF, AVG or catheter. The presence of any HD catheter was classified as “catheter,” even in instances when another maturing AV access was in place. Baseline demographic characteristics and comorbid medical conditions were recorded. Baseline values of albumin, hemoglobin, phosphorus, and equilibrated Kt/V were considered as the mean of observed values measured over the first 30 days following FMCNA admission for dialysis (Table 1).
Table 1.
Patient demographics of incident HD patients
| All Patients | Fistula | Graft | Catheter | ||||
|---|---|---|---|---|---|---|---|
| Total | Catheter Only | Catheter + Fistula | Catheter + Graft | ||||
| No. of Patients | 25,003 | 4,151 (16.6) | 1,230 (4.9) | 19,622 (78.5) | 14,836 (59.3) | 4,038 (16.2) | 748 (3.0) |
| Age (y) | 63.4 (15.3) | 63.6 (14.2) | 65.7 (13.8) | 63.3 (15.6) | 63.6 (15.8) | 61.9 (14.9) | 63.9 (14.5) |
| Male | 56.1 | 65.6 | 41.7 | 55.0 | 54.0 | 60.9 | 42.0 |
| Race | |||||||
| White | 64.8 | 66.2 | 52.5 | 65.3 | 66.4 | 63.2 | 53.9 |
| Black | 30.0 | 28.2 | 41.3 | 29.7 | 29.1 | 29.7 | 41.6 |
| Other | 5.2 | 5.5 | 6.2 | 5.0 | 4.5 | 7.1 | 4.5 |
| BMI (kg/m2) | 30.6 | 30.8 | 31.1 | 30.5 | 30.3 | 31.2 | 30.8 |
| Diabetes Mellitus | 55.1 | 51.3 | 57.3 | 55.7 | 54.4 | 59.7 | 61.6 |
| CAD) | 11.0 | 9.8 | 10.2 | 11.4 | 11.3 | 11.8 | 10.4 |
| PVD | 6.9 | 5.4 | 5.9 | 7.3 | 7.3 | 7.2 | 8.7 |
| CHF | 14.8 | 10.2 | 11.4 | 15.8 | 16.0 | 14.8 | 18.2 |
| Laboratory values | |||||||
| Albumin (g/dL) | 3.5 | 3.7 | 3.6 | 3.4 | 3.4 | 3.5 | 3.3 |
| Hemoglobin (g/dL) | 10.7 | 10.8 | 10.8 | 10.7 | 10.7 | 10.7 | 10.5 |
| Phosphorus (mg/dL) | 4.7 | 4.8 | 4.6 | 4.7 | 4.7 | 4.8 | 4.6 |
| eKt/V | 1.3 | 1.3 | 1.4 | 1.3 | 1.3 | 1.3 | 1.4 |
Note: Patients are from a US nationwide sample admitted to Fresenius Medical Care North America facilities between January 1 and December 31, 2007. Values for continuous variables given as mean or mean +/− SD; values for categorical variables, as percentage or number (percentage). Conversion factors for units: phosphorus in mg/dL to mmol/L, x 0.3229.
BMI, body mass index; CAD, coronary artery disease; HD, hemodialysis; PVD, peripheral vascular disease; CHF, congestive heart failure, eKt/V, equilibrated Kt/V.
Access status was updated for each patient whenever a new access was placed or used for the first time, or when a catheter was removed. Patients were followed for 365 days or until censoring for death, kidney transplantation, withdrawal from dialysis, or recovery of kidney function. Reasons for censoring for all patients are presented in Table S1, provided as online supplementary material. Episodes of failure to mature as well as failure of previously functional AV accesses were abstracted from the electronic medical record. Blood culture results during the study period were obtained solely from a central laboratory (Spectra Laboratory), which processes approximately 85% of all blood cultures drawn in all FMCNA facilities; remaining samples are those sent to local labs on the weekend or for results urgency. Positive blood culture results, antibiotic use, and hospitalization for infections were equated with the likely presence of bloodstream infections (BSI), absent collection of potentially corroborative clinical data in the database. Thrombotic access complications were abstracted from the database. The association between vascular access type and time to BSI was evaluated utilizing Cox models. Unadjusted, case-mix adjusted (CM; adjusted for age, gender, race, diabetes mellitus), and CM + Quality Indicator adjusted models (aforementioned plus baseline albumin, hemoglobin, phosphorus and equilibrated Kt/V) were estimated separately.
As it was not possible to distinguish between catheter removal resulting from mechanical complication versus that resulting from maturation of a concomitant AV access, mechanical complications and recombinant tissue plasminogen activator (TPA) use were considered in the restricted cohort of patients who initiated dialysis with a catheter and no other access. SAS 9.1 (SAS Institute) was used for all data analyses.
All patients consented for use of data for quality assessment and practice patterns at the time of HD enrollment, and institution review was waivered for quality improvement purposes. All FMCNA patients acknowledged receipt of Notice of Privacy Practices at HD enrollment, informing them of the use of clinical data for treatment, payment and healthcare operations, among other appropriate uses and disclosures. These provider initiated quality improvement studies are considered as being under the areas of treatment, payment, and healthcare operations and, therefore, do not require institutional review board approval or patient consent.
Results
Patient demographics
The mean age for the 25,003 HD patients studied was 63.4 ± 15.3 years; 56.1% were male, 64.8% were white, 30.0% were black, and 5.2% were of other races, and 55.1% of patients had diabetes (Table 1). Overall, the mean follow-up time was 277 ± 130 (median, 365; interquartile range, 166–365) days. The majority of patients, 78.5% initiated dialysis with a catheter, 16.6% with an AVF, and 4.9% with an AVG. Catheter patients tended to be younger than AVF patients, and both were younger than AVG patients. Male patients had more AVF and fewer AVG relative to catheters. Patients with diabetes were disproportionately represented among the AVG group, and underrepresented in the AVF group. Black patients were more likely to have an AVG than an AVF, whereas Caucasian patients were slightly more likely to have an AVF than an AVG. The catheter rate did not differ by race. In addition, CHF, CAD and PVD were more prevalent among catheter patients, particularly when compared to the AVF group.
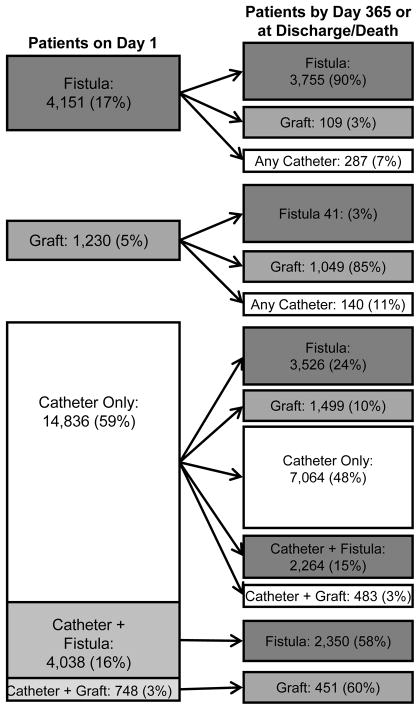
Access evolution within the first year of dialysis
At dialysis initiation, 4,151 (17%) patients had a functioning AVF, 1,230 (5%) had a functioning AVG, 14,836 (59%) had solely a catheter, 4,038 (16%) had a catheter and maturing AVF, and 748 (3%) had a catheter and maturing AVG. Among the 20,242 patients alive at day 90, 4,432 (21.9%) had an AVF (3,386 having had a mature/maturing AVF on day 1), 1,705 (8.4%) had an AVG (1,012 had a mature/maturing AVG on day 1), and 14,105 (69.7%) had a catheter (13,704 had a catheter alone on day 1) (Table S2).
As of 1 year on dialysis--or death or censoring for those who did not remain enrolled for 1 year-- 90.5% of those started with a functioning AVF continued with an AVF and 85.3% of those started with a functioning AVG continued with an AVG (Figure 2). Among the 14,836 (59%) patients who initiated HD with a catheter only, 3,526 (23.8%) were undergoing dialysis with an AVF at the end of one year, 1,499 (10.1%) had an AVG, 2,264 (15.3%) had both a catheter and a maturing AVF, 483 (3.3%) had a catheter and a maturing AVG, and 7,064 (47.6%) had a catheter only at end of follow up. Among the 4,038 patients who started HD with a catheter and a concomitant AVF, 2,350 (58.2%) had an AVF by the end of follow up. Among the 748 patients who initiated with a catheter and a concomitant AVG, 451 (60.3%) were undergoing dialysis with an AVG by the end of follow up. In a total of 2,639,039 treatments administered during this 365-day period for all patients, 873,418 (33.1%) were delivered via AVF; 300,321 (11.4%), via AVG; and 1,465,300 (55.5%), via catheter.
Figure 2.
Evolution of hemodialysis access in the first year in 25,003 incident HD patients sampled from across the US admitted to Fresenius Medical Care North America facilities between January 1 and December 31, 2007.
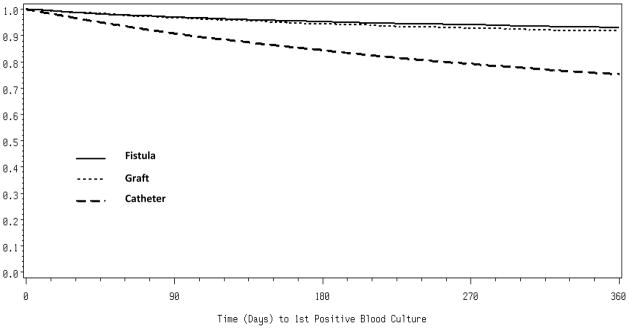
Blood stream infection within the first year
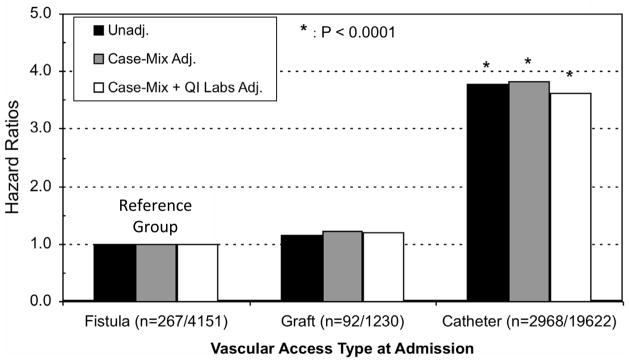
Overall, 3,327 (13.3%) patients had at least one positive blood culture result during follow-up. Kaplan-Meier curves for time to first BSI by access type are shown in Figure 3. Based on incident dialysis access type, catheter patients had a BSI event rate of 1.27/1000 catheter-days, which was ~3-fold higher than that of patients receiving dialysis through an AVF or AVG (p<0.001 for catheter to AVF or catheter to AVG comparison; Table 2). Additionally, among the subset of 3327 individuals who experienced a BSI during follow-up, the median time to first BSI was 85 days among patients with a catheter, 111 days among patients with an AVF, and 117 among patients with an AVG. The case mix and case mix plus quality indicator adjusted hazard ratios for BSI demonstrated hazard ratios for catheters vs. fistulas of 3.83 and 3.62, respectively (both p<0.001; Figure 4). The risk of BSI was not significantly different between individuals undergoing dialysis with fistulas vs. grafts (Figure 4). Post-hoc analysis of the actual access type at the time of BSI compared with baseline access type is shown in Table 3. The change in access type occurred in both directions such that results were unchanged compared to the primary analysis.
Figure 3.
Kaplan-Meier curves for time to first positive blood culture among incident hemodialysis patients, by initiating access type for all patients (N=25,003).
Table 2.
Blood stream infection in the first year on hemodialysis in incident HD patients
| All | Catheters | Fistulas | Grafts | |
|---|---|---|---|---|
| Patients with BSI/Total Patients | 3327/25003 (13.3%) | 2968/19622 (15.1%) | 267/4151 (6.4%) | 92/1230 (7.5%) |
| Total no. of BSI Episodes | 5441 | 4798 | 490 | 153 |
| Median Time to 1st BSI (d) * | 87 | 85 | 111 | 116.5 |
| BSI Rates/1000-days | 0.99 | 1.27 | 0.37* | 0.39** |
Note: Patients are from a US nationwide sample admitted to Fresenius Medical Care
North America facilities between January 1 and December 31, 2007.
BSI, bloodstream infection. HD, hemodialysis
in patients with BSI-positive blood culture results.
p<0.001 compared to catheters
Figure 4.
Vascular access type and associated risk of bloodstream infection in the first year in incident hemodialysis patients, separated by initiating dialysis access type. Case-mix Cox model adjusted for age, gender, race, diabetes status, body mass index, and comorbidities (diabetes, peripheral vascular disease, coronary artery disease, and congestive heart failure). Case-Mix + Quality Indicator (QI) adjusted for first 30-days include laboratory results for albumin, hemoglobin, phosphorous and eKt/V. BSI, bloodstream infection.
Table 3.
Misclassification of BSI attribution
| Baseline Access Type | Total | Access Type on Date of Positive Blood Culture Result | |||
|---|---|---|---|---|---|
| Catheter | Fistulas | Grafts | |||
| Catheter | 2968 | 2928 (99.4) | 25 (9.0) | 15 (14.8) | |
| Fistulas | 267 | 12 (0.4) | 254 (91.0) | 1 (1.0) | |
| Grafts | 92 | 7 (0.2) | 0 (0) | 85 (84.2) | |
| Total | 3327 | 2947 (100) | 279 (100) | 101 (100) | |
Note: Misclassification using intention-to-treat method (baseline vascular access type) compared with actual vascular access of record at the time of the blood draw for blood cultures with positive results. Values shown as number (percentage).
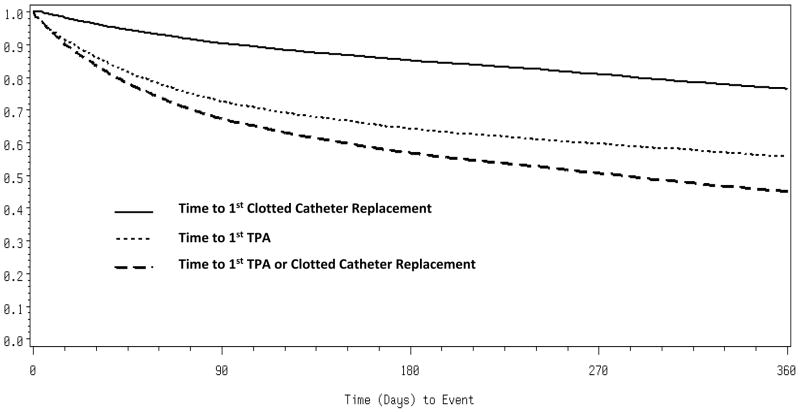
Catheter complications
Among the 19,622 (78.5%) patients with catheters at dialysis initiation, Kaplan-Meier event free survival curves for each outcome and their composite are presented in Figure 6. First-ever use of TPA by 4,829 (32.5% of the total) patients occurred during follow-up at a median of 41 days, and 2,860 (59.2%) of these had more than one TPA administration (Fig 5). Furthermore, 863 (17.9%) patients with catheters that had TPA instillation eventually had the catheter replaced for lack of usability (others may have had catheter removal as a result of infections or had the catheter removed with a new arteriovenous access in place). 2,169 catheters present on dialysis initiation (14.6%) were replaced for the first time because of dysfunction (absent infection) at a median of 75 days. The TPA use rate was 6.38/1000 catheter days, and the catheter replacement rate was 1.05/1000 catheter days.
Figure 5.
Kaplan-Meier Curve on time to first episode of intervention in hemodialysis patients who initiated dialysis with solely a tunneled catheter, separated by interventions performed. TPA, tissue plasminogen activator.
Discussion
In the era since the introduction of the Fistula First initiative, we studied 25,003 incident HD patients for a nationwide contemporary look at vascular access course and evolution during the first year on dialysis, with associated blood stream infection and catheter complication rates.
Functioning fistulas and grafts at dialysis initiation had failure rates of 10% and 15%, respectively, at 1 year. Grafts were seldom changed to fistulas (3%). Forty-eight percent of all patients who initiate with a catheter alone still had only a catheter at 1 year. Fistulas that were maturing at the time of admission were used as the sole source of dialysis access only 42% of the time at one year—findings consistent with other reports. (8) These data add to the accumulating body of evidence demonstrating that AVF and AVG maturation in dialysis patients frequently takes much longer than the conventional 3 months, 2 weeks (8–13), perhaps because of vessel health and surgical or cannulation techniques. Therefore, collaboration with surgical colleagues(7) and development of novel methods for identifying CKD patients at greatest risk for progression to ESRD, who are most likely to benefit from earlier permanent access referral, will be critical in increasing early permanent access use in incident HD patients. Although repeat attempts for permanent access can be made after the first year, patients are exposed to greater catheter use and attendant complications during the wait. Considered together with the high technical failure rate, additional studies focusing on permanent access referrals and access attempts in patients who are still undergoing dialysis via a central venous catheter at 1 year are necessary to identify reasons for continued catheter use, especially in those who are amenable to interventions.
As expected, most BSI events in the first year of dialysis were among patients with central venous catheters. It is surprising that among patients with AVFs and AVGs in whom BSIs developed, the median time to event was only approximately 30 days longer than among catheter users. However, these data must be interpreted in light of there being many fewer BSIs among patients with AVFs and AVGs. Additionally, infections in fistula or grafts are not often associated with bacteremia, therefore some of the observed BSI events in patients with AVFs and AVGs may have been unrelated to vascular access.
The main limitation of our study is the incomplete capture of BSIs. Approximately 15% of all culture specimens were sent to non-FMCNA laboratories. Although this may lead to a spuriously low event rate (and a spuriously high time-to-event value), the bias incurred is expected to be modest since approximately 85% of all events were likely to have been captured. Furthermore, because failure of data capture is unlike to be related to access type, comparative analyses should be reasonably free of bias. To guard against misattribution resulting from access crossover, we performed post-hoc analyses considering the actual access type in place at the time of BSI and observed no material change of results (Table 3 Another potential limitation is the uncertain validity of the source data related to vascular access. Although access data for these analyses were not formally validated, internal quality assurance testing done at FMCNA in other contexts indicates accuracy of about 90%–95%. Last, we acknowledge there is limited precision regarding when catheter-to-AV access conversion took place. Because the majority of morbidity seems to be related to the presence of an indwelling catheter, using the date of catheter extraction as a surrogate seems clinically grounded.
The observed data about TPA use and catheter replacements were obtained from patients who initiated dialysis with only a catheter access, excluding patients who had a concomitant catheter with a maturing AV access. This conservative approach may have lead to underestimation of the true utilization rate, as a result of omission of mechanical complications of catheters in patients with concomitant maturing accesses. However, such an approach was necessary, because the precise date of functional access transition is not reliably known in our dataset; the period between established function of AV access and catheter removal is variable, because only the date of catheter removal is reflected in the data during the study period. Nearly 1 in 3(32.5%) catheters will require TPA use by median time of 41 days, with 59% requiring more than one TPA administration. The presence of biofilm and partially dissolved intra/peri-lumen blood clots can function as a nidus for infection, potentially preventable by the development of a new antimicrobial catheter lock solution or more resistant catheters. Flow-related dysfunction requiring TPA and catheter replacement pose significant expense and burden on healthcare resource utilization, while potentially contributing to the high infection risk in this group.(14, 15, 17–20) In addition, future studies should evaluate whether differences in handling of catheters by dialysis providers may decrease nosocomial contamination of catheters.
A growing body of evidence has suggested the importance of the type of vascular access used at HD initiation in terms of infectious complications, central vein stenosis,(21) and mortality risk.(16) While the Fistula First initiative has significantly increased the total number of prevalent patients undergoing dialysis with an AVF,(22) our study illustrates that, within the first year on dialysis, catheter use remains the predominant access type, and that transition to a permanent access is often delayed. This confirms prior reports in single center experiences.(10) Although a fistula may not be the most appropriate type of dialysis access for select patients,(23) programs designed to increase functional arteriovenous accesses prior to the need for maintenance dialysis will be an important step in improving early morbidity and mortality during dialysis for most patients. In light of the significant risk posed by catheter use, arteriovenous access planning and pre-emptive access placement, in patients with rapidly progressing moderate to severe chronic kidney disease, should be a high priority.
Attendance in pre-dialysis education programs for patients with chronic kidney disease has been shown to improve the rate of arteriovenous access use during dialysis initiation.(24–26) It has been recommended that this pre-dialysis education should occur at or around a glomerular filtration rate (GFR) of 30 ml/min/1.73 m2, with access placement happening at a GFR of 20 ml/min/1.73 m2, so that a mature access is reasonably predicted to be in place by the time GFR is reduced to 10 ml/min/1.73 m2 – also referred to as the “30-20-10 rule.”(27, 28) It might also be reasonable to consider selective placement of AVF in patients who are undergoing peritoneal dialysis. (29) There are limitations for some patients with regards to lack of insurance coverage prior to dialysis initiation that may require innovative solutions and advocacy for changes to Medicare policies.(30) More innovative programs that provide incentives to both nephrologists and surgeons while increasing accountability, such as the accountable care organizations proposed by the Department of Health and Human Services (comprised of voluntary groups of physicians, hospitals, and other health care providers that agree to take responsibility for the care of a clearly delineated population of Medicare patients), (30, 31) also would be welcome.
In summary, among a large, contemporary and representative population of patients who initiated hemodialysis in the United States, catheter use remained very high over the first year of hemodialysis care, and was associated with high mechanical complication and blood stream infection rates. These findings highlight the need for multidisciplinary research and collaborative efforts to better identify patients at high risk of progression to ESRD, incentivize insurance coverage for prophylactic fistula placement, re-evaluate the role of AVG to minimize catheter exposure, improve processes to drive efficient catheter conversion into arteriovenous accesses, and increase technological innovations for catheter care in patients who require dialysis through a central venous catheter. Collaboration from outside the renal community, including regulators, payers, surgeons and hospitals, will be needed to effectively address the future of dialysis access care.
Supplementary Material
Table S1: Discharge breakdown of all study subjects at day 365.
Table S2: Access type at day 90.
Acknowledgments
Support: None.
Footnotes
Finanical Disclosure: As of this writing, WW, ML, RH, and EL were or remain as employees of Fresenius Medical Care, North America. Dr. Brunelli has served as an advisor to Amgen, C.B. Fleet Company and Proctor & Gamble. Dr. Brunelli has received speaking honoria from Fresenius Medical Care North America, and his spouse is employed by Astra Zeneca. HX and JI declare that they have no relevant financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bradbury BD, Fissell RB, Albert JM, Anthony MS, Critchlow CW, Pisoni RL, et al. Predictors of early mortality among incident US hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS) Clin J Am Soc Nephrol. 2007;2(1):89–99. doi: 10.2215/CJN.01170905. [DOI] [PubMed] [Google Scholar]
- 2.Astor BC, Eustace JA, Powe NR, Klag MJ, Fink NE, Coresh J. Type of vascular access and survival among incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. J Am Soc Nephrol. 2005;16(5):1449–55. doi: 10.1681/ASN.2004090748. [DOI] [PubMed] [Google Scholar]
- 3.Gulati S, Sahu KM, Avula S, Sharma RK, Ayyagiri A, Pandey CM. Role of vascular access as a risk factor for infections in hemodialysis. Ren Fail. 2003;25(6):967–73. doi: 10.1081/jdi-120026031. [DOI] [PubMed] [Google Scholar]
- 4.Powe NR, Jaar B, Furth SL, Hermann J, Briggs W. Septicemia in dialysis patients: incidence, risk factors, and prognosis. Kidney Int. 1999;55(3):1081–90. doi: 10.1046/j.1523-1755.1999.0550031081.x. [DOI] [PubMed] [Google Scholar]
- 5.Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK. Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int. 2001;60(4):1443–51. doi: 10.1046/j.1523-1755.2001.00947.x. [DOI] [PubMed] [Google Scholar]
- 6.Ishani A, Collins AJ, Herzog CA, Foley RN. Septicemia, access and cardiovascular disease in dialysis patients: the USRDS Wave 2 study. Kidney Int. 2005;68(1):311–8. doi: 10.1111/j.1523-1755.2005.00414.x. [DOI] [PubMed] [Google Scholar]
- 7.Goodkin DA, Pisoni RL, Locatelli F, Port FK, Saran R. Hemodialysis vascular access training and practices are key to improved access outcomes. Am J Kidney Dis. 2010;56(6):1032–42. doi: 10.1053/j.ajkd.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 8.Feldman HI, Joffe M, Rosas SE, Burns JE, Knauss J, Brayman K. Predictors of successful arteriovenous fistula maturation. Am J Kidney Dis. 2003;42(5):1000–12. doi: 10.1016/j.ajkd.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Lok CE, Allon M, Moist L, Oliver MJ, Shah H, Zimmerman D. Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas (REDUCE FTM I) J Am Soc Nephrol. 2006;17(11):3204–12. doi: 10.1681/ASN.2006030190. [DOI] [PubMed] [Google Scholar]
- 10.Lee T, Barker J, Allon M. Tunneled catheters in hemodialysis patients: reasons and subsequent outcomes. Am J Kidney Dis. 2005;46(3):501–8. doi: 10.1053/j.ajkd.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 11.Dember LM, Beck GJ, Allon M, Delmez JA, Dixon BS, Greenberg A, et al. Effect of clopidogrel on early failure of arteriovenous fistulas for hemodialysis: a randomized controlled trial. JAMA. 2008;299(18):2164–71. doi: 10.1001/jama.299.18.2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xue H, Lacson E, Jr, Wang W, Curhan GC, Brunelli SM. Choice of vascular access among incident hemodialysis patients: a decision and cost-utility analysis. Clin J Am Soc Nephrol. 2010;5(12):2289–96. doi: 10.2215/CJN.03210410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shingarev R, Maya ID, Barker-Finkel J, Allon M. Arteriovenous graft placement in predialysis patients: a potential catheter-sparing strategy. Am J Kidney Dis. 2011;58(2):243–7. doi: 10.1053/j.ajkd.2011.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Allon M. Dialysis catheter-related bacteremia: treatment and prophylaxis. Am J Kidney Dis. 2004;44(5):779–91. [PubMed] [Google Scholar]
- 15.Allon M, Daugirdas J, Depner TA, Greene T, Ornt D, Schwab SJ. Effect of change in vascular access on patient mortality in hemodialysis patients. Am J Kidney Dis. 2006;47(3):469–77. doi: 10.1053/j.ajkd.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 16.Bradbury BD, Chen F, Furniss A, Pisoni RL, Keen M, Mapes D, et al. Conversion of vascular access type among incident hemodialysis patients: description and association with mortality. Am J Kidney Dis. 2009;53(5):804–14. doi: 10.1053/j.ajkd.2008.11.031. [DOI] [PubMed] [Google Scholar]
- 17.Berns JS. That catheter is going to cost you! Semin Dial. 2006;19(5):440–2. doi: 10.1111/j.1525-139X.2006.00202.x. [DOI] [PubMed] [Google Scholar]
- 18.Al-Solaiman Y, Estrada E, Allon M. The Spectrum of Infections in Catheter-Dependent Hemodialysis Patients. Clin J Am Soc Nephrol. 2011 doi: 10.2215/CJN.03900411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lacson E, Jr, Wang W, Lazarus JM, Hakim RM. Change in vascular access and mortality in maintenance hemodialysis patients. Am J Kidney Dis. 2009;54(5):912–21. doi: 10.1053/j.ajkd.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Lacson E, Jr, Wang W, Lazarus JM, Hakim RM. Change in vascular access and hospitalization risk in long-term hemodialysis patients. Clin J Am Soc Nephrol. 2010;5(11):1996–2003. doi: 10.2215/CJN.08961209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agarwal AK, Patel BM, Haddad NJ. Central vein stenosis: a nephrologist’s perspective. Semin Dial. 2007;20(1):53–62. doi: 10.1111/j.1525-139X.2007.00242.x. [DOI] [PubMed] [Google Scholar]
- 22.Lacson E., Jr Epidemiology of hemodialysis vascular access in the United States. Clin Nephrol. 2011;75(6):497–505. [PubMed] [Google Scholar]
- 23.O’Hare AM, Allon M, Kaufman JS. Whether and when to refer patients for predialysis AV fistula creation: complex decision making in the face of uncertainty. Semin Dial. 2010;23(5):452–5. doi: 10.1111/j.1525-139X.2010.00783.x. [DOI] [PubMed] [Google Scholar]
- 24.Lacson E, Jr, Wang W, Devries C, Leste K, Hakim RM, Lazarus M, et al. Effects of a nationwide predialysis educational program on modality choice, vascular access, and patient outcomes. Am J Kidney Dis. 2011;58(2):235–42. doi: 10.1053/j.ajkd.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 25.Lopez-Vargas PA, Craig JC, Gallagher MP, Walker RG, Snelling PL, Pedagogos E, et al. Barriers to timely arteriovenous fistula creation: a study of providers and patients. Am J Kidney Dis. 2011;57(6):873–82. doi: 10.1053/j.ajkd.2010.12.020. [DOI] [PubMed] [Google Scholar]
- 26.Kulawik D, Sands JJ, Mayo K, Fenderson M, Hutchinson J, Woodward C, et al. Focused vascular access education to reduce the use of chronic tunneled hemodialysis catheters: results of a network quality improvement initiative. Semin Dial. 2009;22(6):692–7. doi: 10.1111/j.1525-139X.2009.00647.x. [DOI] [PubMed] [Google Scholar]
- 27.Levin A. Identification of patients and risk factors in chronic kidney disease--evaluating risk factors and therapeutic strategies. Nephrol Dial Transplant. 2001;16 (Suppl 7):57–60. doi: 10.1093/ndt/16.suppl_7.57. [DOI] [PubMed] [Google Scholar]
- 28.Lee D, Levin A, Roger SD, McMahon LP. Longitudinal analysis of performance of estimated glomerular filtration rate as renal function declines in chronic kidney disease. Nephrol Dial Transplant. 2009;24(1):109–16. doi: 10.1093/ndt/gfn477. [DOI] [PubMed] [Google Scholar]
- 29.Lacson E, Jr, Lazarus JM, Himmelfarb J, Ikizler TA, Hakim RM. Balancing Fistula First with Catheters Last. Am J Kidney Dis. 2007;50(3):379–95. doi: 10.1053/j.ajkd.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Allon M, Dinwiddie L, Lacson E, Jr, Latos DL, Lok CE, Steinman T, et al. Medicare reimbursement policies and hemodialysis vascular access outcomes: a need for change. J Am Soc Nephrol. 2011;22(3):426–30. doi: 10.1681/ASN.2010121219. [DOI] [PubMed] [Google Scholar]
- 31.Berwick DM. Making good on ACO’s Promise- the final fule for the medicare shared savings program. NEJM. 2011 doi: 10.1056/NEJMp1111671. e-press, Oct 20, 2011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Discharge breakdown of all study subjects at day 365.
Table S2: Access type at day 90.