Abstract
Objective
To determine the patient experience of using a simple telehealth strategy to manage hypertension in adults.
Design
As part of a pragmatic service evaluation, the acceptability of, satisfaction with and ease of use of a simple telehealth strategy was determined via text, cross-sectional questionnaire survey administered by telephone, case studies, discussion groups and informal feedback from practices. This simple telehealth approach required patients to take home blood pressure (BP) readings and text them to a secure server (‘Florence’) for immediate automatic analysis and individual healthcare professional review.
Participants
124 intervention patients who used the Florence system.
Setting
10 volunteer general practitioner's (GP) practices in Stoke on Trent, UK, with poor health and high levels of material deprivation took part.
Results
Patient satisfaction was high. In particular, patients found the system easy to use, were very satisfied about the feedback from their GP regarding their BP readings, found the advice sent via Florence useful and preferred to send BP readings using Florence rather than having to go to the practice monthly to get BP checked. Overall satisfaction with the system was 4.81/5.00 at week 13 of the programme. Other advantages of being enrolled with Florence were improved education about hypertension, a greater feeling of support and companionship and flexibility which allowed self-care to occur at a time that suited the patient rather than their practice.
Conclusions
This simple telehealth strategy for managing hypertension in the community was met with high levels of patient satisfaction and feelings of control and support. This management approach should thus be considered for widespread implementation for clinical management of hypertension and other long-term conditions involving monitoring of patients’ bodily measurements and symptoms as a large number of meaningful readings can be obtained from many patients in a prompt, efficient, interactive and acceptable way.
Keywords: Primary Care, Telehealth, Patient experience, Text message
Article summary.
Article focus
Home blood pressure (BP) readings are a valuable source of information upon which clinical management decisions can be made and are acceptable to patients.
Although studies have shown that patients are receptive to the idea of simple telehealth strategies for managing BP and that they respond well to text messages, details of the patient experience when actually using simple telehealth in this way is lacking.
This paper examines the experiences of and feedback from intervention patients who used an innovative interactive simple telehealth strategy to monitor and manage their hypertension.
Key messages
Patients find that simple telehealth is a flexible, convenient, easy to use and acceptable means of them jointly managing their hypertension with a responsible health professional.
The interactive nature of such a simple telehealth strategy provides support and companionship for some patients and builds their confidence in their health and well-being.
Patients are supportive of wider use of this technology in the future for hypertension and other long-term conditions.
Strengths and limitations of this study
As this is a service evaluation, the results obtained accurately reflect the actual use of the technology in the clinical setting.
Due to the fact that this was a service evaluation, not all patients provided feedback using all the means employed and data collection did not continue until it reached saturation, and therefore there may be some missing data.
Introduction
Hypertension is common and carries the risk of great morbidity and mortality. Current management strategies are not adequately controlling this significant problem and new and innovative means of diagnosing and managing hypertension are required. For the best part of the last century the concept of home blood pressure (BP) readings to improve the accuracy of measurement and prevent inappropriate treatment of white coat hypertension has been recognised. However, the early machines utilised were not reliable and useful readings were limited.1 Twenty years ago, Aylett1 outlined that patients became more actively involved in their care with self-BP monitoring, compared with ambulatory-BP monitoring. Ten years ago, a literature review concluded that home BP measurements using automated devices are equivalent to ambulatory readings taken into health settings.2 The programme evaluated here for patient acceptability and satisfaction brings these historic ideas about improving blood pressure management into the present day. Utilising an electronic sphygmomanometer, to obtain home BP readings, patients text their results into a secure server (‘Florence’) and receive immediate automated feedback regarding any required further actions, based upon the level of the reading. This is an innovative system that allows ‘closed loop’ management in the main, that is, automatic responses; however, individualised patient management is provided from the patient's own healthcare professional who reviews their BP recordings weekly, or more frequently if indicated. Clinically, this type of clinical management strategy has a number of benefits; it allows multiple readings, and thus meaningful averages to be calculated, from patients in their own environment, collected at any time of the day or night. Thus, personal, social or occupational factors need not be barriers to accessing prompt and effective care for hypertension.
Florence had not been used in this healthcare setting prior to undertaking this programme, although local pilot work for other conditions resulted in positive healthcare professional and patient anecdotal feedback. However, previous work by other groups has suggested that this innovative system was likely to be well accepted by patients. In 2003, when availability of home electronic sphygmomanometers was relatively new, Rickerby and Woodward3 reported that home BP measurements were easy to obtain with little or no formal training and are acceptable for certain patients, particularly those who wish to accept responsibility for the management of their hypertension as it facilitates more regular BP monitoring than could be realistically possible if measurements were only obtained in the clinical setting. Bostock et al4 investigated the acceptability of the concept of remote management of BP using mobile phones among healthcare professionals and patients and discovered that patients were generally welcoming to this approach provided that reassurances and action strategies were in place should high readings be returned. Further, Liew et al5 demonstrated that receipt of text messages resulted in behaviours equivalent to conventional (direct 1:1 telephone) reminder systems, thus supporting the use of interactive text message feedback both from Florence and the healthcare professionals reviewing the readings.
To improve satisfaction with this technology among patients it is important that they are positive about this method of service provision in addition to achieving good clinical outcomes. This paper reports the findings of a service evaluation undertaken in primary care to determine the acceptability and levels of patient satisfaction with the use of a simple telehealth intervention for monitoring BP.6
Method
This paper describes the feedback obtained as part of a service evaluation of the implementation of an innovative simple telehealth strategy for managing hypertension. Information about the service design, recruitment, patient characteristics and results with regard to the management of BP are described elsewhere.6 The telehealth strategy used was innovative as it employed the use of home electronic BP measurements and mobile phones so that patients could text their BP results to a secure server (‘Florence’) for automatic assessment and immediate response according to the level of BP received and personalised, human review of results at least weekly, by the patient's usual primary healthcare team for advice on further management and changes (eg, to medication) that are required. Patients were enrolled to use Florence for 3 months, or a shorter period if they became, or were found to be, normotensive. Data collection continued for 6 months after enrolment onto the programme.
Information on patient satisfaction, ease of use of Florence and acceptability of this management strategy was obtained using a variety of means. Patients received two questions monthly (weeks 4, 8 and 12) via text throughout their time using the system. These were ‘It is easy to use the Florence system to record my blood pressure’ and ‘I am satisfied with the feedback from my GP about my blood pressure as a result of using the system’. Patients were required to respond using a five-point Likert scale (1=strongly disagree, 2=disagree, 3=neither disagree/agree, 4=agree and 5=strongly agree). At week 13 patients were texted a further question to answer using a satisfaction score of 1–5, ‘how satisfied are you with your experience of using the Florence system to manage your blood pressure?’
At least two patients per practice were contacted by telephone by practice staff to complete a cross-sectional questionnaire survey which, using a Likert scale as above and a selection of attitude statements, enquired about the patients' attitudes towards and satisfaction with using Florence. Attitude statements included ‘The Florence (text messaging) system is easy to use’, ‘I am satisfied with the feedback from by GP about my blood pressure as a result of using the Florence system’, I find the advice/information I receive from Florence to be useful’ and ‘I prefer to send daily BP readings via Florence rather than having to go to my doctor's surgery to get my BP checked monthly’. Patients were selected by convenience sampling as some patients were not contactable by telephone. Only one questionnaire was administered to each patient but these data were collected at various time points after enrolment to Florence so they provide an overview of patient satisfaction at all stages of the programme.
When patients stopped using Florence they were contacted by telephone by practice staff to enquire about their reasons for stopping and/or any problems encountered, their experiences of using Florence and the likelihood that they would get involved in a similar project in the future should one be available for other health conditions. Patients had to respond to the same attitude statements detailed above. They were also asked to describe any problems encountered and to provide any further comments where they felt this to be appropriate and this supplementary information was recorded as free text. The length of time of using Florence was noted so that an average usage could be calculated.
Nine months after the start of the programme, an educational event was held for patients to learn about more about telehealth technology and its wider application. Discussion groups were held during this event for patients to provide feedback about their experiences of being involved in the intervention. Non-attendees were able to remotely provide feedback. The discussion groups were semistructured and patients were asked questions about using telehealth in general, ease of use of the technology in this specific programme and satisfaction with seeing healthcare professionals less frequently given the closer monitoring using telehealth.
Feedback from practice staff was a dynamic process. Comments from practice staff over the course of the programme were noted. During data collection, patients that appeared to be clinically interesting (eg, many readings in the middle of the night) were flagged and practices were asked to provide case studies on these patients. Further, practices provided case studies of patients they felt had particularly benefitted from being involved in the programme.
Patient feedback obtained via the Likert scales was summarised descriptively and average scores were calculated. An overview of the patient experience of using Florence obtained through free text feedback on the questionnaires, written and verbal feedback from practice staff and during the discussion groups was summarised according to topics as they emerged.
Results
This service evaluation analysed data from 124 intervention patients. At the point of final data collection, the 6-month follow-up period was not complete for five patients. Fifty-one patients stopped using the programme at 3 months, as per the protocol and an additional 37 patients continued using Florence after the 3-month programme period had ended. Of these 37 patients, 19 continued to submit BP readings to Florence 6 months postrecruitment.
In total, 95 patients were sent the monthly questions via Florence, of which, 76% responded to at least one question. Nine of these patients stopped using Florence before completing 3 months so did not get sent week 12 and 13 questions. Sixty-three patients provided feedback via the questionnaire administered by practice staff over the telephone. The average time between recruitment and administration of the questionnaire among these patients was 5.2 months (range 1–9 months). Twenty-four people participated in discussion groups.7
Feedback obtained using the telephone questionnaire at various time points during the data collection period was collected from 64 patients. Another 82 questionnaires were completed by patients who were contacted after leaving the programme. Forty of these patients left the programme by choice and 42 left because their BP was found to be, or became, controlled within the normotensive range. Of the 40 patients who were classified as leaving the programme by choice, 17 left because they had completed the allocated 3 months, 4 because they were unable to devote the required time or were not in the country to undertake the programme, 3 left due to struggling to use or having limited access to a mobile phone, 2 patients preferred review by the doctor face to face, 2 patients left their general practitioner (GP) practice, 2 felt unable to relax enough to take their own BP themselves, 1 patient only wanted to use it short term, 1 could not access Florence, 1 misunderstood that the programme should have continued and 1 was advised by secondary care to have their BP monitored at the hospital. Of the remaining six patients two patients reported that they did not want to continue with the programme anymore but gave no specific reasons and no explanation was provided for four patients.
Patients found Florence easy to use
The statement ‘It is easy to use the Florence system to record my blood pressure’ was posed on a number of occasions using a five-point Likert scale (1=strongly disagree, 3=neither disagree/agree and 5=strongly agree), and at each stage, results were favourable. Average scores out of a maximum of 5.00, from the text questions on months 1, 2 and 3 of the programme were 4.49, 4.77 and 4.78, respectively (see figure 1). In response to the attitude statement ‘The Florence (text messaging) system is easy to use’, an average score of 4.79 (median 5) was obtained from the telephone questionnaire during the programme period (see table 1) and, among patients who left the programme a score of 4.31 (median 5) was obtained from those leaving through choice and 4.73 (median 5) from those who left due to being normotensive. Further, a number of patients offered the free text feedback that the system was ‘easy to use’ and they had ‘no problems’ implementing it and the feedback from discussion groups was that it ‘seemed to be easy to use’.7
Figure 1.
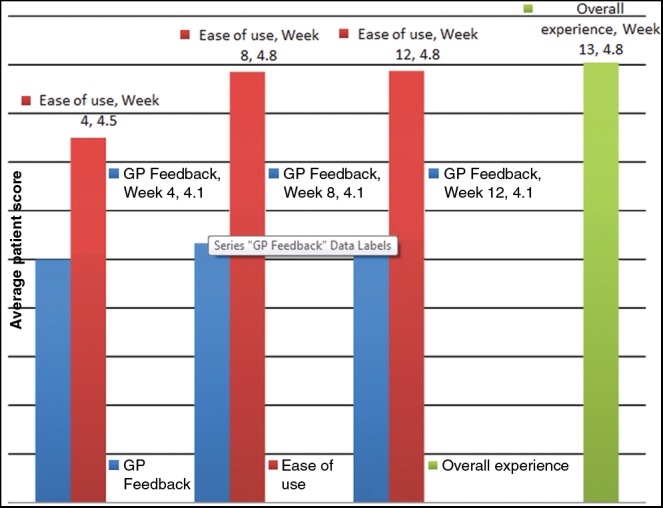
Average patient satisfaction scores for feedback from general practitioner/practice nurse, ease of use of the Florence system and the overall experience of using Florence (1=strongly disagree, 3=neither disagree/agree and 5=strongly agree).
Table 1.
Spread of responses to Likert statements from cross-sectional survey administered by telephone
| Strongly disagree | Disagree | Neither disagree/agree | Agree | Strongly agree | Average | Missing data | |
|---|---|---|---|---|---|---|---|
| The Florence system is easy to use | 1 | 0 | 2 | 5 | 55 | 4.79 | 3 |
| I am satisfied with the feedback from my GP about my blood pressure | 1 | 2 | 1 | 17 | 41 | 4.53 | 4 |
| ‘I prefer to send daily BP readings via Florence rather than having to go to my doctors surgery to get my BP checked monthly | 2 | 3 | 11 | 11 | 35 | 4.19 | 4 |
BP, blood pressure; GP, general practitioner.
Patients were satisfied with the feedback they obtained through Florence
The statement ‘I am satisfied with the feedback from my GP about my BP as a result of using the Florence system’ was also asked multiple times using a five-point Likert scale. Again, results were positive. Average scores out of a maximum of 5.00, from the text questions during months 1, 2 and 3 of the programme were 4.04 (median 5.00), 4.07 (median 5.00) and 4.05 (median 5.00), respectively (see figure 1). An average score of 4.53 (median 5.00) was obtained from the telephone questionnaire administered during the programme period (see table 1) and, among patients who left the programme, a score of 4.54 (median 5.00) was obtained from those who left through choice and 4.14 (median 5.00) from those who left due to being normotensive.
This level of satisfaction does not appear to be one sided. An indication that simple telehealth was also satisfactory to healthcare professionals and promoted efficiencies in care is highlighted by the following: “(A doctor involved recalls that she) had just finished texting her instructions to a patient informing him that he would need a prescription following his blood pressure result—she took the prescription out to reception within five minutes of sending the message, and he was already standing there waiting for the prescription, having jumped into his car and driving to collect it!”
‘Self-care’ that suits the patient rather than the surgery
A key benefit highlighted by patients and fed back by practices was the flexibility proffered by the Florence system. BP readings could be taken and submitted at any time of the day or night. This assisted patients who may be at risk of ‘white coat’ hypertension.8 One man, who exited the Florence system due to his BP becoming controlled, stated that home BP readings were beneficial as he was ‘less stressed, more disciplined’ and he ‘learned how BP was affected by...work and was much lower at weekends—he could then tell how to look after his BP better’. Similarly, one patient ‘was delighted by the fact that he could communicate with his GP without the necessity of travelling to the surgery…he often had to tackle rush hour traffic…to attend…his appointment and felt that he was not in a sufficiently relaxed state to have his BP taken when he'd completed that battle’. The theme of being more ‘relaxed’ or ‘less anxious’ when taking home BP and submitting them to Florence was repeated by a number of patients.
Further, Florence also suited patients whose lifestyles conflict with attending GP surgeries. For example, one patient who ‘doesn't get up until the afternoon’ sent in multiple readings in the middle of the night. Elderly patients who rely on others to transport them to the GP surgery were ‘delighted not to have the inconvenience of attending surgery for the blood pressures to be taken’. Carers benefited from this flexibility also; “a 59 year old male who lives with and cares for his 84 year old father…he felt very happy and felt that someone is looking after him...without him coming to the surgery…he hadn't been into the surgery [for over six months] and rarely comes in due to caring full time for his father.”
Florence provided reassurance for patients with uncertain diagnoses of hypertension
Although patients without confirmed hypertension did not meet our ‘specific’ inclusion criteria for this project, this was a service evaluation and these patients were recruited for clinically appropriate reasons and gained significant benefit from being involved. For example, 25 patients with high clinic systolic BP readings at recruitment used Florence and discovered they had normal home readings, without making any changes to their medication. These patients could be reassured and discharged from the system. This reassurance was welcomed by some of the patients who reported that “no treatment needed—reassuring…long term monitoring gives a better picture’, ‘reassuring to monitor in home environment’ and ‘reassured no problem.” Such use of Florence represents an extension to the current National Institute for Health and Clinical Excellence recommendations for 24 h ambulatory or home monitoring of BP to determine a diagnosis of hypertension.8
Reinforces care and advice from primary healthcare team
Florence was noted to reinforce health messages from the primary healthcare team and led to control of hypertension among patients who had previously been difficult to manage. Someone in the discussion group fed back “my partner was struggling with his blood pressure, and telehealth has made a world of difference.”7 Patients specifically commented on liking ‘to see BP reading and be aware that it is normal’. Another discussion group member commented that telehealth ‘helped me to learn to live with the disease and become more involved in monitoring my own health’.7 The enhanced involvement and knowledge about BP readings and the significance of the result obtained, promoted by the training and accompanying literature for the programme, led to a new attitude of compliance with management of their hypertension among certain patients. For example, one patient who had previously stopped his own medication had been strongly counselled about the dangers of his uncontrolled BP continued to have significant hypertension. He joined the Florence system and gained better control of his BP, practice staff reported that ‘he could take his BP at home, where the readings would be done in a less stressful situation…the process has helped his understanding of his condition...it does seem to be a combination of the nurse's firm advice, and Florence's routine readings that have combined to stabilise his condition’. A similar situation was noted in another patient ‘the system has highlighted just how high her BP actually is’. The intensive nature of Florence made one patient feel ‘he had a strong support from his GP and that it was a really worthwhile illustration of the quality of NHS service’.
A few patients fed back that being involved in the programme prompted them to find out more about ‘blood pressure’, educated them about the relevance and interpretation of the BP values and highlighted the importance of good BP control. “[A 25 year old male] found the scheme helped him to understand more about the importance of keeping his BP under control especially with regards to his ongoing kidney problems.” “A 73 yr old male…on the whole felt that [being involved in the programme] had helped him to understand his BP and control a bit better.” “[A 60 year old female] found that using this system helped her considerably as she was more relaxed plus she found the accompanying literature very helpful and it prompted her to research further about hypertension on the internet, therefore increasing her understanding.” However, one individual highlighted that despite improved understanding, patients remain free to exert their autonomy ‘once information became knowledge I understood my disease. Then I had a choice: should I do something about it or not—it was my choice’.
Florence also helped to promote more comprehensive management of high-risk patients, such as “a 25 year old male…noted to have proteinuria at his new patient check and…BP…145/84 mm Hg. Over time he was noted to have persisting proteinuria with mid stream urine samples negative for infection. He had a history of gout and associated anti-inflammatory drug use. [Blood tests revealed] creatinine 275, urea 11.7 and eGFR 25 [so he was diagnosed with] CKD Stage 4. Following referral to nephrology he was found to have small kidneys and signs of longstanding CKD…he was advised that he needed good BP control and was invited to join the Florence programme…He was not on any BP medication at baseline (the new patient check) but was started on amlodipine by nephrology soon afterwards. Having previously not self-monitored his BP, while involved in this programme he monitored it twice per week and found the texts useful as they reminded him to take his BP.”
Florence was a companion to patients
An unexpected role that Florence was found to fulfil was of companionship to the patients it serves. “A 67 year old lady was very happy with using Florence—she said that when she finished using the system she missed the contact and felt that she had ‘lost a friend.’” Other indicators of this role of Florence were from a patient who reported ‘that using the system gave her a sense of comfort to have the feedback from the GP to reassure her that she was managing her condition very well’ and another who reported that ‘getting texts from Flo has given him a break in his daily routine, as it feels that he has someone to talk to’.
Few problems were encountered
Problems using the simple telehealth system were identified among only a few patients. Among patients who chose to leave the programme by choice, six had problems sending or receiving text messages using Florence and one reported having a problem taking their own BP, but this was due to them being ‘too anxious’. Among the six patients who had problems sending or receiving text messages, one patient was texting in words, not numbers, got frustrated as submissions were not recognised and left the programme, one reported not being ‘a technical person’, two patients required other family members to text in readings, one reported not being able to access the Florence system and the final patient only had problems returning messages from survey questions, rather than BP readings. Among patients who left the programme with controlled BP, four reported problems sending or receiving text messages using Florence and one had a problem taking their own BP due the resultant effects of having a previous stroke. Of the four patients who reported problems sending or receiving text messages, two had problems initially transferring readings but after further advice had no problems thereafter, one patient reported having incongruous responses after submitting readings and one patient reported a problem but gave no explanation. Another patient also reported getting conflicting advice; they were ‘told by phone that BP's okay but had to contact surgery regarding medication’.
Some patients fed back that multiple messages a day prompting them to submit readings and providing advice was a little excessive. However, this was balanced by another patient who stated that they ‘felt at first that taking BP each day was a bit much but soon realised the benefits and could not fault it’.
Focus group discussions among patients also highlighted that this type of service would not be suitable for all patients, especially those with limited cognitive abilities. They also suggested that older people may not manage to use a mobile phone or other equipment; however, this is not a universal problem as patients up to the age of 86 years used the system.
Simple telehealth and the future
Among the 40 patients who left the programme by choice, an average score of 3.71 (median 4.00) of 5.00 was obtained in response to the statement ‘I would be interested in using this type of programme in the future for this or another type of health problem’. A score of 4.54 (median 5.00) was obtained (from a five-point Likert scale where 1=strongly disagree and 5=strongly agree) in relation to the same question among the 42 patients who left the programme with controlled BP.
Further evidence of a positive attitude towards future use of a similar programme was obtained when patients were asked to respond to the statement “I prefer to send daily BP readings via Florence rather than having to go to my doctors surgery to get my BP checked monthly,” an average score of 4.19 (median 5.00) was obtained (see table 1).
Positive attitudes among patients for the utility of simple telehealth in the future were underlined by feedback from the discussion groups. This highlighted the areas in which patients felt that telehealthcare may be of value in the future. Such uses include monitoring of other chronic conditions such as renal, heart, respiratory conditions and diabetes and certain ‘medium-term afflictions’ (eg, pre-eclampsia). However, patients also saw a role for telehealthcare as prompting service particularly for those with learning disabilities, dementia and carers, assisting patients to remember to take medications, fluids and food and managing patients preoperatively. Finally, patients imagined this type of intervention could help the ‘well’ to stay that way by monitoring health parameters to prevent illness.
Not only did patients see scope for this type of service provision in the future, feedback indicated that the lessons learned through the use of this system will be taken into the future by individual patients. For example, one man ‘is continuing to take his own blood pressure at home with a machine he has purchased and will continue to monitor himself accordingly so that he can bring the results into surgery on his review appointment’.
Discussion
This service evaluation demonstrates that patients found this simple telehealth strategy for managing hypertension easy to use, convenient and acceptable. Patients liked feeling increased levels of support and Florence had a role as a companion, in promoting patients to educate themselves further and providing reassurance about normotension in cases of white coat hypertension. As previously found,3 the skills and knowledge gained by patients from using Florence have led some patients to commence longer-term health behaviours such as self-directed ongoing monitoring and purchase of their own home machines.
The problems encountered with using the system were relatively minor and many could be eliminated by careful recruitment of patients (ensuring dexterity to use BP machine and mobile phone and access to equipment needed), through thorough counselling about what they will be expected to do (one patient reported it feeling ‘awkward’ initially but was ‘fine when got used to it’) and what they should expect to receive from the system before embarking on the programme and/or tailor the number of requests more precisely to the needs of the patient. For example, if, clinically, only once weekly readings are required then Florence can be ‘instructed’ to only send prompts at this regularity. Such down regulation in the frequency of prompts from Florence is expected to occur in all patients using the system as hypertension becomes controlled. Discussion groups raised the concern that “older people won't want to change, maybe they wouldn't manage the mobile phone or other equipment, they would need a lot of teaching about it so they were able to use it. If there wasn't confidence in being able to use the equipment, it would make them feel worse.”7 However, this concern did not affect the majority of Florence users as only three patients could not manage the mobile phone enough to continue with the programme. In line with previous experience,3 this management approach just does not seem to suit some patients’ preferences, who would rather see a doctor and/or are concerned about using home BP machines or mobile phones. However, this only appears to apply to a small minority of patients.
The results presented are from a pragmatic service evaluation. They are therefore valuable as they reflect patient experience in the actual clinical setting when the programme is delivered by the patients’ usual clinical staff. However, data were thus neither obtained systematically nor until the point of data saturation. Further, the number of patients included was not derived through calculation of required sample size but determined by the maximum number of patients that could be recruited in the given time period. Data regarding the number of patients approached to join the programme and thus how many declined are not available. The same question may have been asked of the same patient on multiple occasions and at varying time points throughout their use of the programme. Data are also missing from some patients who could not be contacted or if practice staff did not have capacity to contact all patients involved to obtain feedback. The effect on the data of this missing information is likely to be minimal as patients were not systematically excluded from providing feedback and the feedback from practice staff in all 10 participating practices ensured that overall patient experience was summarised. Predominantly, patient feedback was very positive. This finding may be due to the wording of the statements associated with the Likert scales which were all framed in a positive way, for example, ‘The Florence (text messaging) system is easy to use’ and ‘I find the advice/information I receive from Florence to be useful’. However, patients had an opportunity to disagree with these statements using the Likert scale and it could be argued that using both positive and negative statements may lead to confusion in giving responses. When thinking about other possible anomalous causes of the positive results found it is important to consider the risk of missing opposing views. It was clear if and when patients stopped using Florence as there were no further readings submitted to the server. If submissions of readings appeared to have ceased, practice staff were requested to contact the patient to establish if they were still using Florence and, if not, they completed the telephone questionnaire to find out the reasons why not and establish if any problems had been encountered. Of the 124 patients enrolled on the programme, 82 completed questionnaires upon cessation of their use of Florence. Of the remaining patients, 19 were still submitting BP readings to Florence after 6 months had elapsed since their enrolment. Therefore, it is unlikely that any significant negativity about the programme was missed unless dissatisfied patients were regularly using the programme and not feeding this dissatisfaction back to the team.
In line with the findings of McManus et al9 and Jones et al,10 intervention patients were supportive of home or self-monitoring in the future and, once the programme had finished, some wished to continue using Florence. Generally, there was no evidence that undertaking home readings increased anxiety. Only one patient specifically reported that they withdrew from the programme as she “would have preferred to send BP readings in monthly…(as daily readings) made her feel anxious (as) she knew each day when she got up she had to text in.” This is in accordance with the findings of previous studies investigating home BP readings by Little et al11 in 2002, McManus et al9 in 2005 and Ovaisi et al12 in 2011 which all found good levels of acceptability of home readings among patients and no evidence of detrimental effects of increased anxiety. In general, patients in this service evaluation found home readings to be beneficial as they were more relaxed and less anxious than they would be in the GP surgery. It may be for this reason that the patients investigated by Jones et al10 felt that home readings were more ‘natural’.
Patient concordance with jointly agreed management strategies between the patient and their responsible health professional is essential in maximising the health benefits obtained. Therefore, the ease of use of any intervention needs to be high to minimise barriers to use. This evaluation identified that this simple telehealth intervention was generally found to be easy to use, a finding which is supported by Clark et al.13 who undertook a systematic review of telemonitoring and structured telephone support programmes for patients with chronic heart failure. They reported generally high patient acceptance, satisfaction and ease of use scores among the studies they examined.
Utilising this simple telehealth strategy has benefits over patients taking home readings and reporting them to the GP for two reasons: BP readings are transmitted and recorded in real time, therefore there is no scope for missing or lost results at GP review; and one recent study of home BP readings among stroke patients identified that even though all patients understood the importance of having a high BP reading, when one was obtained, they did not all seek help or direction from their primary care team.12 The simple health strategy used in this service evaluation eliminates this barrier to seeking appropriate care as all results that are sent to Florence are reviewed on the dedicated server by the primary healthcare team at regular intervals. Further, due to the at least weekly review of BP readings by the patients’ usual primary care team, any persistently suboptimal readings that have not been recognised by the patient will be detected more quickly than they will have been had the patient been asked to record their blood pressure at home and return after a month or so.
In agreement with a previous systematic review of telemonitoring for heart failure,14 which concluded that telemonitoring was generally ‘favourable compared with usual care’, this service evaluation indicates that patients feel the same about simple telehealth monitoring of hypertension. The flexibility, control and education that Florence provides were well received and appear to have empowered patients who had previously been uncontrolled and/or non-compliant with usual care.
When used in clinical practice, there should be scope to continue using Florence for prolonged periods even after normotension is reached, albeit with readings at reduced intervals. Not only would this ensure enduring control it may help to allay patients’ concerns that arose during the discussion groups about ‘slipping through the net’ due to lack of face-to-face contact. Some patients within this service evaluation, and those who were interviewed by Jones et al10 following a similar intervention, were keen to continue self-monitoring in the same way. The number of BP readings requested by Florence each week or month can be adjusted down accordingly in these situations.
In summary, there is a clear need for new and improved clinically driven strategies for hypertension control in primary care to prevent morbidity and mortality. This pragmatic service evaluation indicates that simple telehealth strategies may not only be effective in doing this in actual clinical practice but do so in a way that is easy, flexible, affordable, acceptable and, in many cases, preferable, when compared with usual care. Not only does simple telehealth deliver a service that patients appreciated and believed in, it appeared to become a companion to some patients. Our results indicate that careful selection and counselling of patients is required at recruitment onto such a programme to ensure that they understand and agree with the nature and frequency of the processes involved and that they are physically and cognitively able to operate the simple equipment.
Supplementary Material
Acknowledgments
The authors thank John Blackburn, Chris Chambers, James Davies, Mike Dixon, Phil O'Connell, Dave Sanzeri, Diane Wilshaw who work for NHS Stoke on Trent CCG and were part of the programme steering group and/or data collection team.
Footnotes
Contributors: EC designed data collection tools, inputted and analysed data and drafted and revised the original paper. RC lead the programme of work and oversaw the processes of data collection, analysis and reporting, she also devised and revised this paper. KM collected data and revised the draft paper. EC, RC and KM are responsible for the overall content as guarantor(s). JB, CC, JD, MD, PO, DS and DW were all involved in running the programme and for data collection.
Funding: Funded by Health Foundation.
Competing interests: All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that (1) EC, KM and RC have support from NHS Stoke on Trent for the submitted work; (2) EC, KM and RC have no relationships with Mediaburst Limited that might have an interest in the submitted work in the previous 3 years (3) their spouses, partners, or children have no financial relationships that may be relevant to the submitted work; and (4) EC, KM and RC have no non-financial interests that may be relevant to the submitted work.
Ethics approval: This was a service evaluation.
Provenance and peer review : Not commissioned; externally peer reviewed.
Data sharing statement: No additional unpublished data are available. A linked paper has been submitted containing the design, recruitment, patient characteristics and results of the programme described.
References
- 1.Aylett MJ. Ambulatory or self blood pressure measurement? Improving the diagnosis of hypertension. Fam Pract 1994;11:197–200 [DOI] [PubMed] [Google Scholar]
- 2.Rickerby J. The role of home BP measurement in managing hypertension—an evidence based review. J Hum Hypertens 2002;16:469–72 [DOI] [PubMed] [Google Scholar]
- 3.Rickerby J, Woodward J. Patients’ experiences and opinions of home blood pressure measurement. J Hum Hypertens 2003;17:495–503 [DOI] [PubMed] [Google Scholar]
- 4.Bostock Y, Hanley J, McGown D, et al. The acceptability to patients and professionals of remote blood pressure monitoring using mobile phones. Prim Health Care Res Dev 2009;10:299–308 [Google Scholar]
- 5.Liew SM, Tong SF, Lee VKM, et al. Text messaging reminders to reduce non-attendance in chronic disease follow-up: a clinical trial. Br J Gen Pract 2009;59:916–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cottrell E, Chambers R, O'Connell P. Using simple telehealth in primary care to reduce blood pressure: a service evaluation. 2012. (In Press—bmjopen-2012–001391.R1) [DOI] [PMC free article] [PubMed]
- 7.Stoke on Trent Community Health Voice Telehealthcare event on 27th January 2012. Unpublished
- 8.National Institute of Health and Clincial Excellence Hypertension: clinical management of primary hypertension in adults. London: NICE, 2011 [Google Scholar]
- 9.McManus RJ, Mant J, Roalfe A, et al. Targets and self monitoring in hypertension: randomised controlled trial and cost effectiveness analysis. BMJ 2005;331:493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones MI, Greenfield SM, Bray EP, et al. Patients’ experiences of self-monitoring blood pressure and self-titration of medication: the TASMINH2 trial qualitative study. Br J Gen Pract 2012;62:e135–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Little P, Barnett J, Barnsley L, et al. Comparison of accepability of and preferences for different methods of measuring blood pressure in primary care. BMJ 2002;325:258–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ovaisi S, Ibison J, Leontowitsch M, et al. Stroke patients’ perceptions of home blood pressure monitoring: a qualitative study. Br J Gen Pract 2011;61:e604–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clark RA, Inglis SC, McAlister FA, et al. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ 2007;334:942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polisena J, Tran K, Cimon K, et al. Home telemonitoring for congestive heart failure: a systematic review and meta-analysis. J Telemed Telecare 2010;16:68–76 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


