Abstract
Background and objective
The increasing prevalence of childhood obesity has led to interest in its prevention, particularly through school-based and family-based interventions in the early years. Most evidence reviews, to date, have focused on individual behaviour change rather than the ‘obesogenic environment’.
Objective
This paper reviews the evidence on the influence of the food environment on overweight and obesity in children up to 8 years.
Data sources
Electronic databases (including MEDLINE, EMBASE, Cochrane Controlled Trials Register (CCTR), DARE, CINAHL and Psycho-Info) and reference lists of original studies and reviews were searched for all papers published up to 31 August 2011.
Study selection
Study designs included were either population-based intervention studies or a longitudinal study. Studies were included if the majority of the children studied were under 9 years, if they related to diet and if they focused on prevention rather than treatment in clinical settings.
Data extraction
Data included in the tables were characteristics of participants, aim, and key outcome results. Quality assessment of the selected studies was carried out to identify potential bias and an evidence ranking exercise carried out to prioritise areas for future public health interventions.
Data synthesis
Thirty-five studies (twenty-five intervention studies and ten longitudinal studies) were selected for the review. There was moderately strong evidence to support interventions on food promotion, large portion sizes and sugar-sweetened soft drinks.
Conclusions
Reducing food promotion to young children, increasing the availability of smaller portions and providing alternatives to sugar-sweetened soft drinks should be considered in obesity prevention programmes aimed at younger children. These environment-level interventions would support individual and family-level behaviour change.
Keywords: Preventive Medicine, Public Health
Article summary.
Article focus
Prevalence of childhood obesity remains high.
Interventions to reduce obesity appear to be shifting from an individual focus to a more societal approach.
This paper systematically reviews the evidence linking obesity and diet-related environmental factors.
Key messages
The three environmental exposures identified as having the most impact were the availability of sugar-sweetened beverages; portion sizes and food promotion.
Reduction of these three elements is likely to hold promise in obesity prevention among children.
Strengths and limitations of this study
There was an absence of evidence for a number of environmental factors.
Anthropometric outcome measures were not made in all the studies.
A number of the intervention studies included were of short duration with short follow-up periods.
Introduction
Childhood obesity is associated with health problems in childhood and an increased risk of obesity along with associated health risks in adulthood, particularly in children who have an obese parent.1 2 In 2010, over 43 million children under the age of 5 years were reported to be overweight worldwide.3 The need for obesity prevention in children has, therefore, become a priority for both governments and researchers. Many obesity interventions have focused on individual behaviour change to prevent excessive childhood weight gain, but this strategy has generally led to only short-term improvements in obesity and related risk factors if any.4 5 One reason for this is because it is difficult to make changes to behaviour in an environment which increasingly promotes a high energy intake and sedentary activity. This ‘obesogenic’ environment has been defined as ‘the sum of the influences that the surroundings, opportunities or conditions of life have on promoting obesity in individuals and populations’.6
According to Swinburn et al,7 individuals interact with the environment in multiple micro-(local) environments or settings, including schools, homes and neighbourhoods. These are, in turn, influenced by the broader macroenvironments (such as the education and health systems, government, the food industry and a society's attitudes and beliefs), which are less amenable to the control of individuals. Modifying the ‘obesogenic’ environment could produce a more lasting effect on behavioural change.7
Of a number of published evidence reviews on strategies for preventing childhood obesity,8–15 only one published in 2007 has focused on environmental influences of obesity-related dietary behaviours in children and young people (aged 3–18 years).15 It found consistent associations between parental influences (parental food intake and education) and obesity in this age group.15 The early years are a priority population for intervention strategies for two reasons. First, there are a greater number of potential settings for population-wide interventions for children than for adults, for example, schools, preschool institutions and after-school care services. Second, it is more difficult to reduce excessive weight in adolescents and adults once it becomes established; therefore, it may be helpful to initiate obesity prevention interventions during early childhood.16 There is a growing consensus that the appropriate period to target obesity prevention interventions is the early years in a child's life.17 The aim of the present review was, therefore, to examine the evidence for environmental influences on dietary determinants of obesity, focusing on younger children (birth to 8 years).
Methods
A workshop to identify environmental influences on diet, physical activity and obesity was held involving senior researchers from government and academia, health practitioners and policy professionals in Scotland. The areas which emerged from this workshop were then refined by the study team to nine areas of focus which are shown in box 1.
Box 1. Areas for dietary determinants of obesity, as derived from stakeholder workshops.
Desire for highly palatable foods
Demand for easy to prepare food and individual meals
Food promotion
Large portions
High-energy snack foods
Sugar-sweetened soft drinks
Food availability and access
Restaurants, fast food outlets and coffee bars
School and nursery catering
Search strategy and data sources
Key words used as part of the search strategy included obesity, body mass index (BMI), dietary intervention, obesity prevention, food promotion and food advertisements. The detailed search strategy for MEDLINE is provided in appendix I. One reviewer (GOA) searched electronic databases (including MEDLINE, EMBASE, Cochrane Controlled Trials Register (CCTR), DARE, CINAHL and Psycho-Info) and reference lists of other studies and reviews. Electronic searching was carried out for all papers published up to 31 August 2011. Studies identified from searching electronic databases were combined, duplicates removed and papers were screened for relevance to the review based on the information contained in the title and abstract by two reviewers (GOA and SD).
Inclusion/exclusion criteria
Studies were included if they fulfilled all the following criteria: 1) they involved exposure to one of the environmental influences on dietary determinants of obesity in children aged <9 years listed in box 1; 2) the study design was an intervention (either a population-based intervention or a short-term experimental study) or a longitudinal study; 3) the study reported outcomes including BMI/weight, skin-fold thickness, percentage body fat, per cent overweight/obesity or dietary behaviours linked to obesity. Studies designed specifically for the treatment of childhood obesity and those where the target population was predominantly overweight or obese were excluded as the focus of the review was on prevention in the whole child population.
Study selection and data synthesis
The full text of references identified as potentially relevant were obtained. Papers that could not be rejected with certainty were assessed independently by another reviewer (SD) using the inclusion criteria. Differences were resolved by discussion and consensus with other reviewers (GM and JM). Data were extracted regarding study design, sample size, participants, aim, intervention and outcomes/results by one reviewer (GOA) into table format. Each study was summarised and described with regard to characteristics of participants, aim, characteristics of interventions and key outcome results, and this was checked by another reviewer (SD). Two separate tables were created one for the intervention studies (table 1) and another for the longitudinal studies (table 2).
Table 1.
Details of included studies (intervention studies)
| Study and country | Design and duration | Population and age at time of outcome assessment | Aim | Results |
|---|---|---|---|---|
| Desire for highly palatable foods | ||||
| No studies | ||||
| Demand for easy to prepare and individual meals | ||||
| No studies | ||||
| Food promotion | ||||
| Goldberg et al23 the Netherlands | Randomised controlled trial (2 experiments) carried out in one day | Children aged 5–6 years (n=122) | To examine the effect of messages on TV on children's snack food selections. | Mean number of less-nutritious foods selected was less in those who watched nutrition education materials compared to those who watched food commercials (2.87 vs 8.70, p<0.05) |
| Ross et al24 the Netherlands | Randomised controlled trial duration one day | Children aged 6–9 years (n=100) | To assess accuracy of judgments of real fruit content in 3 sets of foods advertised on TV | Children exposed to intensive viewing of TV advertising of foods with artificial fruits were less accurate in judging fruit content of foods than those who were not exposed to these adverts (F(1, 87) =5.97, p<0.05). |
| Peterson et al 25 the USA | Pretest-post-test control group design 10 classroom days |
Children aged 5–6 years (n=106) | To assess how TV nutrition programmes affect children's dietary habits | Children exposed to pro-nutrition messages scored higher on nutrition knowledge (p<0.01) and a ‘Pretend Eating Test’ (p<0.01 for pro-nutrition foods) than those not exposed |
| Borzekowski et al 26 the USA | Randomised controlled trial 5 days |
Preschoolers aged 2–6 years (n=46) from low income families | To examine the influence of televised food commercials on children's food preferences | Children exposed to tape with advertisements were more likely to choose advertised foods than tape without ads (Cochran Q Statistic = 8.13, df=1, p=0.004) |
| Dovey et al27 the USA | Mixed methods design 3 months |
Children aged 5–7 years (n=66) | To investigate the impact of food neophobia, weight status and exposure to healthy and unhealthy food adverts on the amount of snack food consumed in children aged 5–7 years | Total kcal intake was higher following the unhealthy food adverts compared to both the healthy food adverts (p=0.005) and toy adverts (p<0.001). Children with low scores on food neophobia scale ate significantly more following the unhealthy food adverts compared to healthy food adverts (p=0.024) and toy adverts (p=0.001) |
| Robinson et al28 the USA | Non-randomised controlled trial duration 1 day | Preschoolers aged 3–5 years from low-income families (n=63) | To examine effects of food branding on young children's taste preferences | Increase in taste preference scores of foods (0.37±0.45, p<0.001) if children thought they were from McDonalds |
| Forman et al29 the USA | 2×2 Factorial design 4 visits of one day each |
Children aged 4–6 years (n=43): 20 overweight and 23 non-overweight | To assess the influence of branding on children's intake | Overweight children ate 40.7 kcal more in branded vs unbranded meals, while non-overweight children ate 45.3 kcal less (p=0.04) |
| Large portions | ||||
| Fisher et al30 the USA | Within subject crossover design 3 months |
Preschoolers aged 2–5 years (n=35) | To examine effects of exposure to large portion of an entrée on food intake and weight status | Doubling an age-appropriate portion of entrée increased the amount of entrée eaten by 25±7% (p<0.001) and total energy intake by 15±5% (p<0.01) at lunch |
| Rolls et al31 the USA | Non-randomised controlled trial 3 weeks |
Children aged 3–6 years (n=32) | To examine effects of portion size on children's food intake | Children aged 4.3–6.1 years had higher total energy intake when served larger portions (p<0.002) but this effect was not seen in children aged 3.0–4.3 years |
| Looney et al32 the USA | 2×2 crossover design 2 months |
Children aged 3–5 years (n=17) | To investigate the impact of portion size and energy density on intake, both grams and kilocalories of snacks in pre-school aged children | There was a significant impact of portion size on snack intake (small portion size 84.2±30.8 kcal, large portion size 99.0±52.5 kcal; p<0.05) |
| Spill et al33 the USA | Crossover design 4 weeks |
Children aged3–5 years (n=51) | To investigate whether increasing the portion size of vegetables served at the start of a meal leads to increased vegetable consumption and decreased meal energy intake in children | There was a significant increase in total vegetable consumption at the meals (p<0.0001). Doubling portion size of the first course increased carrot consumption by 47% (p<0.0001) |
| Sud et al34 the USA | A nested non-randomised controlled trial 4 visits of 1 day each |
Children aged 4–6 years (n=70) | To determine the associations between use of restrictive feeding practices and energy density (ED) and total energy consumed | Restrictive feeding practices were not associated with total energy intake (p=0.05). Total energy intake was positively associated with energy-dense food (r=0.4, p<0.05) |
| High-energy snack foods | ||||
| Fisher & Birch 36 the USA | Non-randomised controlled trial 2 years |
Girls at 5 and 7 years of age (n=192) | To evaluate whether eating in the absence of hunger was associated with increased risk of overweight | Girls who ate more snack foods in the absence of hunger (201–263 kcal) more likely to be overweight (OR 4.6, 95% CI 1.4 to 15.2) |
| Sugar sweetened soft drinks | ||||
| Mrdjenovicand Levitsky37 the USA | Non-randomised controlled trial ;Pretest/post-test 8 weeks |
Children aged 6–13 years (n=30) | To test effect of sweetened drink consumption on energy balance | Sweetened drink consumption of >12 oz/day was related to weight gain of 1.12±0.7 kg |
| Muckelbaur et al41 Germany | Non-RCT 12 months |
Children aged 6–8 years (n=2950) | To test whether promotion of consumption of water was effective in overweight prevention | Reduction in risk of overweight in intervention versus control (OR=0.69; 95% CI 0.48 to 0.98) |
| James et al42 the UK | Cluster RCT 12 months |
Children aged 8–9 years (n=644) | To test whether a programme to reduce soft drink consumption can prevent weight gain | Decrease in obesity in intervention compared to control group (−0.2% vs 7.5%: difference 7.7%; 95% CI 2.2% to 13.1%) |
| Karanja et al 40 the USA | RCT 2 years |
Children followed from birth to 2 years (n=178) | To prevent excess weight gain in American-Indian and Alaskan native toddlers by promoting breastfeeding and curtailment of sugar-sweetened beverage consumption | Significantly less increase in BMI z-scores was observed among the intervention group compared to the control group (p=0.016) |
| Restaurants, fast food outlets and coffee bars | ||||
| No studies | ||||
| School and nursery catering | ||||
| Himes et al45 the USA | RCT 3 years |
5–11-year-old American-Indian children (n=470) | To assess whether a school-based programme can decrease calories eaten as fat | Decrease in mean percent calories from total fat (3.6%) and saturated fat (2.1%) in intervention relative to controls (p<0.05) |
| Williams et al 46 the USA | Non-RCT 18 months |
Children aged 3–5 years (n=787) | To reduce saturated fat content of school meals by <10% of daily energy | Intake of saturated fat decreased from 11.0% to 8.0% in those with a change in the school meals vs increase of 10.2% to 11.4% in control (p<0.001) |
| Webber et al47 the Netherlands | RCT 30 months |
Children aged 7–9 years (n=4019) | To examine the impact of a school-based cardiovascular risk reduction programme on risk factors | There was no change in BMI between groups, but there was a change in total cholesterol in intervention and control groups (1.3 vs 0.9 mg/dl, respectively) p>0.05 |
| Bartholomew et al 48 the USA | RCT 12 weeks |
Children aged 5–11 years (n=1298) |
To examine the effect of an intervention to increase low fat entrees at school cafeterias | Low-fat and moderate-fat entrees were selected at a higher rate in the intervention (32.1% and 26.4%, respectively) than the control school (13.8% and 7.5%, respectively), p<0.01 |
| Ransley et al49 the UK | Non-RCT 7 months |
Children aged 4–6 years (n=703) | To evaluate the impact of daily provision of fruit and vegetables in schools | There was an increase in fruit intake in reception and year 1 pupils (0.4 portions; 95% CI: 0.2–0.5 and 0.6 portions; 95% CI 0.4 to 0.9, respectively) at 3 months. This reduced to 0.2 (95% CI 0.1 to 0.4) and 0.3 (95% CI 0.1 to 0.6) for reception and year 1 pupils respectively at 7 months. No significant changes were observed in energy, fat or sugar intake in intervention vs control schools at 7 months |
| Hendy et al 50 the USA | RCT 3 months |
Children 1st to 4th grade (n=382) | To examine the effectiveness of the Kids Choice Programme for increasing children's weight management behaviours and decreasing BMI percentile (BMI%) | There was a significant decrease in BMI% for both overweight (tcorr (111)= 3.49, p=0.001) and average weight (tcorr (199)= 2.16 p=0.032) children after 3 month application. Results were not sustained in either group at 6 months |
| Bayer et al 51 Germany | RCT 2 years |
Children aged 3–6 years (n=1340) | To assess the effects of a low-cost behavioural prevention programme in a preschool setting | There was a significant increase in the vegetable (OR=1.26, 95% CI 1.26 to 2.01) and fruit (OR=1.64, 95% CI 1.26 to 2.12) consumption and this was sustainable after 18 months |
| Marcus et al 52 Sweden | RCT 4 years |
Children aged 6–10 years (n=3135) | To assess the efficacy of a school-based intervention programme to reduce the prevalence of overweight in 6–10-year-old children. | There was a significant decrease in the prevalence of overweight and obesity in the intervention schools (3.2%) compared to the control schools (2.8%) (p<0.05). There were significant differences between the intervention and control school children for consumption of high-fat dairy products (p=0.001), sweetened cereals (p=0.02) and sweets (p=0.002) |
| Hollar et al 53 the USA | Quasiexperimental design 2 years (Non-RCT) |
Children aged 6–13 years (n=2494) | To determine whether an obesity prevention intervention can improve systolic and diastolic blood pressure and maintain healthy weight | There was a significant decrease in the BMI percentile score (mean (SD)) among girls in the intervention group (−1.73 (13.6) compared to the girls in the control group (-0.47 (12.1) (p=0.007) |
BMI, body mass index; RCT, randomised control trial.
Table 2 .
Details of included studies (cohort studies)
| Study and country | Design and duration | Population and age at the time of outcome assessment | Aim | Results |
|---|---|---|---|---|
| Desire for highly palatable foods | ||||
| Reilly et al19 the UK | Longitudinal 4 years |
Children aged 7 years (n=8234) | To identify risk factors in early life for obesity in children | Junk food dietary pattern at age 3 years was associated with obesity at 7 years though the effect was no longer significant when adjusted for other factors (p=0.083) |
| Demand for easy to prepare and individual meals | ||||
| Anderson et al 20 the USA | Longitudinal 6 years |
Children aged 11 years (n=4471) | To assess the effect of maternal employment on childhood obesity | 10 h increase in work/week by mother increased child overweight by 0.5–1% |
| Gable et al 21 the USA | Longitudinal 3 years |
Children aged 7–8 years (n=8459) | To identify eating and activity factors associated with overweight | Children who ate more family meals in early school years were less likely to become overweight by 3rd grade (OR 0.93; p<0.001) |
| Hawkins et al 22 the UK | Longitudinal 2 years 3 months | Children aged 3 years (n=13 113) | To examine risk factors for overweight in children | Children were more likely to be overweight for every 10 h a mother worked per week (OR=1.10, 95% CI 1.04 to 1.1.7) |
| Food promotion | ||||
| No studies | ||||
| Large portions | ||||
| No studies | ||||
| High-energy snack foods | ||||
| Francis et al 35 the USA | Longitudinal 4 years |
Caucasian girls at ages 5, 7 and 9 years (n=173) | To assess whether TV viewing was related to snacking frequency and obesity in children | Change in BMI from age 5–9 was significantly correlated with fat intake from snacks in children with overweight parents (0.26) but not in those with non-overweight parents (0.14) (p<0.05) |
| Sugar-sweetened soft drinks | ||||
| Welsh et al 38 the Netherlands | Longitudinal 35 months |
Children aged 2–3 years (n=10 904) | To examine whether sweet drink intake is associated with obesity risk in preschoolers | Children at risk of overweight and consumed 1-<2 drinks /day were 2.0 (95% CI 1.3 to 3.2) times likely to become overweight and this risk was dose-dependent |
| Alexy et al 39 Germany | Longitudinal 2 years |
Children aged 3–5 years (n=205) | To examine relation between fruit juice consumption and anthropometric indices | Neither the BMI (r=−0.117, p=0.095) nor growth velocity (r=−0.0977, p=0.163) correlated with the consumption of fruit juice |
| Restaurants, fast food outlets and coffee bars | ||||
| Thompson et al 43 the USA | Longitudinal median 6 years |
Girls aged 8–12 years (n=101) | To examine relation between eating food purchased away from home and change in BMI | Weekly consumption of quick-service food was positively associated with change in BMI z-score (F=3.37, p<0.05) |
| Galvez et al 44 the USA | Longitudinal 3 years |
Children aged 6–8 years (n=323) | To determine whether presence of convenience stores and fast food outlets near a child's home is associated with increased risk for childhood obesity | Children living in proximity of one or more convenience stores were more likely to have BMI percentile in the top tertile compared to children who had no convenience stores near their residence (OR=1.90, 95% CI 1.15 to 3.15) |
| School and nursery catering | ||||
| No studies | ||||
BMI, body mass index.
Quality assessment
All the papers included in the review were assessed for quality using the ‘Effective Public Health Practice Project quality assessment tool for quantitative studies’.18 The tool was modified to take into account the design of the included studies.
Evidence ranking exercise
Fourteen academic researchers and government agency staff were given the data-extraction tables to complete the ranking exercise for 1) the strength of the evidence for a causal association between the environmental factor and childhood overweight and 2) the likely effect size of public health actions on each factor on the prevalence of overweight in children. The strength of the evidence and the likely effect size of actions were rated on a scale of 0 (low) to 5 (high).
Results
Literature search
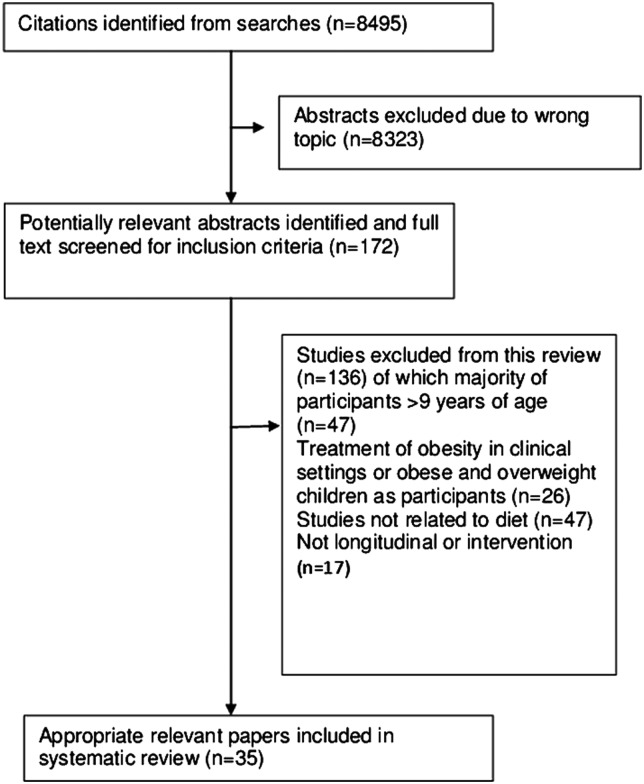
A total of 8495 references were identified from electronic databases and other publications. Initial screening of titles and abstracts produced 172 potentially relevant references. These references were further screened for their full text, and thirty-five studies met the inclusion criteria. Search results are summarised in the flow diagram (figure 1).
Figure 1.
Flow chart for the literature search.
Characteristics of included studies
Nineteen studies (54%) reported primary outcomes in anthropometric measures directly linked to obesity (eg, weight or BMI percentiles); seven (20%) reported dietary intake; seven (20%) reported food choice and two (6%) reported nutrition knowledge. Twenty-five (71%) studies were intervention studies, of which fifteen were short-term experiments (4 days–3 months) and ten were long-term interventions (7 months–4 years), and ten studies (29%) were longitudinal studies. Twenty-three (64%) of the studies were from the USA and the remainder (36%) were from Northern Europe (four from the Netherlands, one from Sweden, four from the UK and three from Germany). The date of publication of included studies was between 1978 and 2011, although only four (11%) were published prior to 2000.
Environmental determinants of dietary influences on obesity in children up to 8 years of age
Table 1 shows study characteristics and results of included studies, which were classified under the nine areas identified in box 1. Some studies were difficult to classify in these areas but were grouped within the area that best reflected the content of the study. There were no studies classed under ‘food availability and access’; for the eight remaining areas, there were between one and seven studies with most number of studies for ‘food promotion’. Because of heterogeneity of study designs and outcome measures, it was not possible to combine the results of the studies in meta-analysis.
Desire for highly palatable foods
The only study which related to this topic was a longitudinal study using data from the Avon Longitudinal Study of Parents and Children in the UK. In this study, Reilly and colleagues found that a ‘junk food’ dietary pattern (determined from diet questionnaire given at 38 months) was associated with an increased risk of overweight or obesity at 7 years in univariate analysis (p<0.001) though this effect was attenuated in the final multivariate model (p=0.083).19
Demand for easy-to-prepare food and individual meals
There were three studies relating to this topic, all of which were longitudinal studies. One study from the USA20 found that the children of mothers who worked more hours per week were more likely to be overweight, particularly among mothers of higher socioeconomic status. A more recent study from the UK supports this finding in children up to 3 years of age, with the effect again more marked in the higher income households.21 Another US study using the nationally representative ECLS-K cohort reported that the number of family meals eaten per week was inversely associated with overweight in the children up to age 7 years.22
Food promotion
Seven studies examined the role of food promotion in childhood obesity, all of which were short term experimental studies. Five studies explored the impact of TV advertising on children's food choice or food knowledge: three were from the USA, published in the late 1970s or early 1980s; two of which found evidence of an influence of TV food commercials on food preference or food understanding in school-age children,23 24 though another found that information from ‘pronutrition’ messages was retained but did not influence subsequent food choice.25 A recent study of 2–6 year olds found that even brief exposure to TV commercials altered the food preferences of the children.26 In a trial from the USA,27 researchers showed a significant increase in immediate energy intake following exposure to unhealthy food adverts. This study also found an association between food neophobia (described in the study as a reluctance to eat, or avoidance of, new foods) and the increase in intake following exposure to unhealthy food adverts. Two other studies of US children aged 3–6 years investigated whether branded packaging influenced food preferences: one found significant preference for foods when wrapped in branded packaging28 while the other found that overweight children overate in branded meals in comparison to the non-overweight group.29
Large portions
Five short-term experimental studies were identified which related to portion sizes: one US study found that the portion size of lunch items influenced the amount of food consumed by 5year-old but not by 3-year-old children, that is, older children ate more30 whereas, in another study from the same laboratory in children aged 3–5 years, doubling the portion size of the main dish served at lunchtime increased the food consumed by 25% and energy intake by 15%.31 A similar relationship between snack portion size and intake in US children was shown by Looney et al.32 Another US study found an increase in the portion size of vegetables resulted in an increase in consumption.33 Only one study explored the relationship between restrictive feeding practices (parental use of restriction over child's feeding) and energy intake and found no association.34
High-energy snack foods
One longitudinal study in US girls found that higher snacking frequency was associated with an increase in BMI from 5 to 9 years. This study also found that girls who watched more TV consumed more snacks in front of the TV.35
In an experimental study of 5-year-old to 7-year-old US girls, those who ate large amounts of snack foods in the absence of hunger were more likely to be overweight at both ages.36
Sugar-sweetened soft drinks
There were four longitudinal studies focusing on the consumption of sugar-sweetened soft drinks. A small study of US children aged 6–13 years attending a summer camp found that the children who consumed >16 oz/day of sugar-sweetened soft drinks had significantly higher total energy intake and a tendency to greater weight gain over the summer compared to children who consumed between 6oz and 16oz of sugar-sweetened soft drinks per day.37 A retrospective longitudinal study from Netherlands of over 10 000 children who had diet assessed at age 2 or 3 years and height and weight measured a year later found that the odds of becoming overweight was two times higher in children who were above the 85 centile at baseline and who had one or more ‘sweet drinks’ (fruit juices, juice drinks and non-diet carbonated drinks) per day.38 However, in this study and in a longitudinal study in Germany,39 no evidence was found for adverse effects of high fruit juice consumption on weight gain among the study participants. In a longitudinal study from the USA40 among toddlers (2 years of age), cutting back on sugar-sweetened beverages (limits not specified) resulted in a significantly lower increase in BMI z-scores.
Two intervention studies were also identified: one study in primary schools in deprived areas in Germany in which a reduction in overweight was found in intervention schools which received drinking water fountains with provision of drink bottles and related lessons compared to those in a neighbouring city which did not.41 A UK study of children aged 7–11 years from primary schools found that educational sessions and activities designed to reduce carbonated drink consumption led to a decrease in the percentage of overweight and obese children of 0.2%, compared to an increase of 7.5% in the control group over a follow-up period of 12 months.42
Restaurants, fast food outlets and coffee bars
Two longitudinal studies were found which related to this area, both from the USA. In girls aged 8–12 years, Thompson and colleagues found that those who ate fast food twice a week, or more, had a greater increase in BMI z-score over 3 years than those who ate fast food less frequently.43 Proximity to fast food outlets and convenience stores to a child's home was directly linked to BMI percentile in the other study by Galvez et al.44
School and nursery catering
Five intervention studies aimed to evaluate the potential role of school and nursery catering on children's diets and obesity. Results from two intervention studies to reduce the fat content of school meals by training the catering staff and parents led to a decrease in the intake of calories from total fat and saturated fat.45 46 In one of these studies in American-Indian children an intervention to reduce the fat content of school meals reduced the intake of energy and fat over the whole day in the intervention schools.45 Webber and colleagues found an increase in physical activity and a reduction in serum cholesterol in the intervention group after 2.5 years, though there was no significant difference in obesity between intervention and control groups.47 A fourth study examined the effect of modifying school lunch choices by always providing one low or moderate fat choice and only providing two high fat choices, and found an increase in the selection of the lower fat choices.48 A large-scale trial of introducing daily fruit in schools in the UK showed a modest increase in fruit intake but no effect on vegetable intake or on the intake of energy, fat or sugar after 12 months.49 A short trial from the USA where children were encouraged using reward tokens to choose fruit and vegetables and healthy drinks at school meals showed a reduction in BMI after 3 months but the results were not sustained after a 6-month period.50 A longitudinal study from Germany by Bayer et al51 observed an increase in the consumption of fruit and vegetables at school meals following a low-cost behavioural programme which was sustained after a period of 18 months. However, no change was observed in the weight status among normal weight and overweight children. Alteration to the school meals through promotion of low-fat dairy products, whole grain bread and elimination of all sweets and sweetened drinks resulted in a significant reduction in the prevalence of overweight and obesity in a longitudinal intervention study from Sweden.52 This was attributed to the possibility of healthy eating habits as a result of the intervention. In the Healthier Options for Public School children (HOPS) study from the USA, Hollar et al53 showed modification to school meals to include high fibre items such as whole grains and more fruit and vegetables and a reduction in the energy-dense products resulted in a significant decrease in BMI among girls.
Evidence ranking exercise results
Environmental factors related to diet that obtained mean ratings >3 for both strength of evidence and likely effect size were high energy-dense snacks, sugar-sweetened soft drinks, availability of high fat, sugar and salt foods and portion size of manufactured foods and of restaurant and cafeteria items.
Risk of bias and selection bias
More than half of the studies included in this review were intervention studies but only nine were randomised control trials (RCTs) and non-RCTs and other experimental designs (n=16) account for the rest. Study samples in these were sometimes convenience samples such children attending day care at university day-care centres. This affected in scoring the studies such that the smaller experimental study population was not always representative of the target population,33 and in some studies which fulfilled these criteria, the scores were low as a result of small percentage of selected individuals who agreed to participate.49
Outcome variables
Although within majority of the included studies outcome measures were BMI, BMI z-scores or changes in weight,40 50 53 other studies only reported the outcomes as changes in energy intakes, gain in health-related and nutrition-related knowledge and taste-preference scores.25 28 29 30
Measurement of data
Data measurements in some of the studies especially the longitudinal studies were based on self-reported/recall data43 in comparison to those experimental studies where data were recorded by trained personnel.33 50 Most of the studies where data were reported by the study participants or their parents valid assessment tools were used which may have helped reduce the risk of bias.
Short follow-up periods
More than half of the intervention studies were of a duration of less than 6 months with some lasting no more than a period of 4 weeks. The nature of some of the studies was such that the design determined the length of the intervention; however, it is necessary to examine whether the results could be replicated elsewhere to study their validity or over a longer intervention period.
Follow-up of participants
More than half of the studies had a high percentage of participants completing the study and this may be a reflection of number of factors such as small number of participants, short-study periods and nature of the intervention.
Discussion
Main findings of this study
Most of the evidence supported an influence of the food environment on children's food intake or weight, although some studies suggested that the effects might be restricted to older children or boys, or those who were overweight. There were seven studies supporting an effect of food promotion: a recent review on this topic concluded that most often the advertised foods contrasted strongly with the ones recommended by public health advisers, and with themes of fun and fantasy or taste, used to promote these to children, whereas recommended foods got little promotional support.54 There were five studies supporting an effect of large portion size on food intake, though some evidence that this effect might be stronger in boys and in children of school age rather than younger/preschool children. For sugar-sweetened soft drinks, three intervention and three longitudinal studies supported the possibility that reducing intake could decrease the risk of overweight: the one study, which did not support this, focused on fruit juice rather than sugar-sweetened soft drinks. For interventions designed to improve food offered in schools, there was some evidence that this improved the diet of the children for the selected foods or nutrients, though only one study showed a reduction in the intake of saturated fat;46 of the five studies where BMI was an outcome measure three reported a significant decrease in BMI among the intervention group.49 51 52 There was, however, an indication from several studies that the effects measured were not sustained long term, which may be an indication for the need of long-term interventions. For the other possible influences of the food environment (‘food availability and access’), there was an absence of evidence on which to base conclusions. The ranking exercise provided a structured approach for obtaining a consensus view on priorities for public health action using tables of evidence. Use of the ranking exercise approach with a larger number academics and policy makers from different sectors would be useful to assess whether the area of expertise and sector (academia vs policy) influences the rating of the evidence.
What this study adds
This review is the first to focus on the influence of the food environment on overweight and obesity in younger children. We used experts’ perceptions and practitioners’ perceptions of the different factors in the food environment to classify the studies under specific areas as defined at a workshop at which the participants were encouraged to offer all possible external influences on children's diet as it relates to obesity. Although it was necessary to interpret the focus of each area fairly broadly to allow the individual studies to be allocated, the approach was useful in grouping the studies into areas which could be identified for policy action.
Limitations of this study
For this review, we examined the obesogenic environment using topic headings generated by the stakeholders from a range of health professions and not restricted to academia alone. This may have led to broadening of the subject headings and may act as a limitation for the search strategy to encompass the ideas generated around obesity prevention. Publication bias (whereby positive studies are more likely to be published than negative studies) and selection bias (owing to our restriction to English language articles) have to be taken into account. The selected population may not always be representative of the target population especially in the case of small experimental designs as they tend to use convenient samples. Not all the evidence outcomes in this review were reported in anthropometric indices linked to obesity; the role of intermediary behaviour changes (such as changes in nutrient and energy intakes or nutrition and health knowledge) in obesity risk or its prevention, as reported by some of the studies, was included as these are a prerequisite for changes in weight. Reliability and validity of the data may be of concern in studies where data were based on recall or self report albeit using validated instruments. Duration of the study can be a limiting factor and majority of the intervention studies were short term so it is not clear as to whether the changes observed could be maintained over a longer period. Furthermore, the majority of the studies took place in the USA or northern Europe which limits the generalisability for the rest of the world, since the ‘obesogenic’ environment is supported by increasingly complex social, political and cultural environments which may be unique to a particular country.13 Out of the studies identified here, only one40 included children from birth to 2 years of age though this seems to be a group of interest in terms of targeting early year interventions.55
Conclusion
This review has identified three areas in which the evidence is growing to support interventions on the food environment of young children, that is, reducing promotion of high-fat, high-sugar foods, making smaller portion sizes available and providing alternatives to sugar-sweetened soft drinks. More research is needed to strengthen the evidence on interventions in these areas, for example, on the optimal design and delivery of the interventions, and the impact on body weight and BMI rather than food intake. For other areas, there was an absence of evidence which needs to be addressed.
Supplementary Material
Acknowledgments
This work was funded by Good Places Better Health (GPBH) initiative of the Scottish Government as part of the Environmental Determinants of Public Health in Scotland project. We thank the participants in the stakeholder workshops.
Appendix: Key word search terms
obesity
weight gain
weight loss
overweight or over weight
weight change
6. BMI or body mass index
body fat
family support
family therapy
behaviour therapy
behaviour modification
behaviour change
lifestyle change
lifestyle intervention
counselling
social support
peer support
Fat restricted diet
healthy eating
dietary therapy
dietary intervention
fruit or vegetable
high fat
low fat
fatty food
health promotion
health education
community intervention
school programme or community program
school intervention or community intervention
family intervention or parent intervention
health policy or school policy or food policy or nutrition policy
obesity prevention
primary prevention or secondary prevention
preventive measures
randomised controlled trial
randomisation
double-blind procedure
single-blind procedure
control group or comparison group
random
comparative study
evaluation
intervention trial
pre/post test
matched communities or matched schools or matched populations
matched pairs
quasiexperimental or pseudoexperimental
non-randomised or pseudorandomised or quasirandomised
prospective study
longitudinal study or longitudinal evaluation
observational study.
food promotion
snacking or snack foods
food portion size
restaurant
fast foods
school or nursery catering
sugar-sweetened drinks
fruit juice
fizzy drinks
carbonated drinks
soft drinks
family structure
children
preschoolers
infants
boys or girls
Footnotes
Contributors: HC, GM, JM, GOA and SD were responsible for the concept and design of the study. GOA and SD were responsible for the search strategy and data extraction and for the preparation of initial draft and the final version. JM, SS, JR, AE, HC and GM provided valuable input on the data extraction tables. All authors approved the final manuscript.
Funding: Funded by Good Places better Health Initiative of the Scottish Government. Grant number EV028 RGC 1880.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The ratings for the quality assessment exercise for individual studies are available from the authors on request.
References
- 1.Must A. Morbidity and mortality associated with elevated body weight in children and adolescents. Am J Clin Nutr 1996;63(3 Suppl):445S–7S [DOI] [PubMed] [Google Scholar]
- 2.Reilly JJ, Methven E, McDowell ZC, et al. Health consequences of obesity. Arch Dis Child 2003;88:748–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Obesity and overweight. Geneva, Switzerland: World Health Organization; 2011. http://www.who.int/mediacentre/factsheets/fs311/en/index.html(accessed 27 Oct 2011). [Google Scholar]
- 4.Flynn M, McNeil A, Maloff M, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with “best practice” recommendations. Obes Rev 2005;7(Suppl 1):7–66 [DOI] [PubMed] [Google Scholar]
- 5.Singh AS, Chin A, Paw MJ, et al. Short-term effects of school-based weight gain prevention among adolescents. Arch Pediatr Adoles Med 2007;161:565–71 [DOI] [PubMed] [Google Scholar]
- 6.Swinburn B, Egger G. Preventative strategies against weight gain and obesity. Obes Rev 2002;3:289–301 [DOI] [PubMed] [Google Scholar]
- 7.Swinburn B, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med 1999;29:563–70 [DOI] [PubMed] [Google Scholar]
- 8.Harris KC, Kuramoto LK, Schulzer M, et al. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ 2009;180:719–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foster GD, Sherman S, Borradaile KE, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics 2008;121:e794–802 [DOI] [PubMed] [Google Scholar]
- 10.Hawkins SS, Law C. A review of risk factors for overweight in preschool children: a policy perspective. Int J Pediatr Obes 2006;1:195–209 [DOI] [PubMed] [Google Scholar]
- 11.Dobbins M, De Corby K, Robeson P, et al. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6–18. Cochrane Database Syst Rev 2009;(1)CD007651. [DOI] [PubMed] [Google Scholar]
- 12.Canadian Institute for Health Research Addressing childhood obesity: the evidence for action. http://www.cihr-irsc.gc.ca/e/23293.html (accessed 14 Apr 2010).
- 13.Summerbell CD, Waters E, Edmunds L, et al. Interventions for preventing obesity in children. Cochrane Database Syst Revi 2005;(3)CD001871. [DOI] [PubMed] [Google Scholar]
- 14.Brown T, Summerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health Research and Clinical Excellence. Obes Rev 2009;10:110–41 [DOI] [PubMed] [Google Scholar]
- 15.van der Horst K, Oenema A, Ferreira I, et al. A systematic review of environmental correlates of obesity-related dietary behaviours in youth. Health Educ Res 2007;22:203–26 [DOI] [PubMed] [Google Scholar]
- 16.Dehghan M, Akhtar-Danesh N, Merchant AT. Childhood obesity: prevalence and prevention. Nutr J 2005;4:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harrington JW, Nguyen VQ, Paulson JF, et al. Identifying the “Tipping Point” age for overweight pediatric patients. Clin Pediatr 2010;49:638–43 [DOI] [PubMed] [Google Scholar]
- 18.Effective Public Health Practice Project. 1998. Quality Assessment Tool For Quantitative Studies. http://www.ephpp.ca/index.html (accessed Feb 2010).
- 19.Reilly JJ, Armstrong J, Dorosty AR, et al. for the Avon Longitudinal Study of Parents and Children Study Team Early life risk factors for obesity in childhood: cohort study. BMJ 2005;330:1357–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson PM, Butcher KF, Levine PB. Maternal employment and overweight children. J Health Econ 2003;22:477–504 [DOI] [PubMed] [Google Scholar]
- 21.Gable S, Chang Y, Crull JL. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-aged children. J Am Dietet Assoc 2007;107:53–61 [DOI] [PubMed] [Google Scholar]
- 22.Hawkins SS, Cole TJ, Law C. The Millennium Cohort Study Child Health group. Maternal employment and early childhood overweight: findings from the UK Millennium Cohort study. Int J Obes 2008;32:30–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldberg ME, Gorn GJ, Gibson W. The effects of TV messages for high and low nutritional foods on children's snack and breakfast food choices. In: Kent Hunt.ed. Advances in consumer research. Vol 5, Ann Abor: Association for Consumer Research, 1978:540–5 [Google Scholar]
- 24.Ross RP, Campbell T, Huston-Stein A, et al. Nutritional misinformation of children: a developmental and experimental analysis of the effects of televised food commercials. J Appl Dev Psychol 1981;1:329–47 [Google Scholar]
- 25.Peterson PE, Jeffrey DB, Bridgwater CA, et al. How pronutrition television programming affects children's dietary habits. Dev Psychol 1984;20:55–63 [Google Scholar]
- 26.Borzekowski DLG, Robinson RN. The 30-second effect: an experiment revealing the impact of television commercials on food preferences of preschoolers. J Am Diet Assoc 2001;101:42–6 [DOI] [PubMed] [Google Scholar]
- 27.Dovey TM, Taylor L, Stow R, et al. Responsiveness to healthy television (TV) food advertisements/ commercials is only evident in children under the age of seven with low food neophobia. Appetite 2011;56:440–6 [DOI] [PubMed] [Google Scholar]
- 28.Robinson TN, Borzekowski DLG, Matheson DM, et al. Effects of fast food branding on young children's taste preferences. Arch Pediatr Adolesc Med 2007;161:792–7 [DOI] [PubMed] [Google Scholar]
- 29.Forman J, Halford JCG, Summe H, et al. Food branding influences ad libitum intake differently in children depending on weight status. Results of a pilot study. Appetite 2009;53:76–83 [DOI] [PubMed] [Google Scholar]
- 30.Fisher JO, Rolls BJ, Birch LL. Children's bite size and intake of an entrée are greater with large portions than with age-appropriate or self-selected portions. Am J Clin Nutr 2003;77:1164–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rolls BJ, Engell D, Birch LL. Serving portion size influences 5-year old but not 3-year old children's food intakes. J Am Diet Assoc 2000;100:232–4 [DOI] [PubMed] [Google Scholar]
- 32.Looney SM, Raynor HA. Impact of portion size and energy density on snack intake in preschool-aged children. J Am Diet Assoc 2011;111:414–18 [DOI] [PubMed] [Google Scholar]
- 33.Spill MK, Birch LL, Roe LS, et al. Eating vegetables first: the use of portion size to increase vegetable intake in preschool children. Am J Clin Nutr 2010;91:1237–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sud S, Tamayo NC, Faith MS, et al. Increased restrictive feeding practices are associated with reduced energy density in 4–6 year old, multi-ethnic children at ad libitum laboratory test-meals. Appetite 2010;55:201–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Francis LA, Lee Y, Birch LL. Parental weight status and girls’ television viewing, snacking, and body mass indexes. Obes Res 2002;11:143–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. Am J Clin Nutr 2002;76:226–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mrdjenovic G, Levitsky D. Nutritional and energetic consequences of sweetened drink consumption in 6 to 13 year-old children. Pediatrics 2003;142:604–10 [DOI] [PubMed] [Google Scholar]
- 38.Welsh JA, Cogswell ME, Rogers S, et al. Overweight among low-income preschool children associated with the consumption of sweet drinks: Missouri, 1999–2002. Pediatrics 2005;115;e223–9 [DOI] [PubMed] [Google Scholar]
- 39.Alexy U, Sichert-Hellert W, Kersting M, et al. Fruit juice consumption and the prevalence of obesity and short stature in German preschool children: results of the DONALD study. J Pediatr Gastroenterol Nutr 1999;29:343–9 [DOI] [PubMed] [Google Scholar]
- 40.Karanja N, Lutz T, Ritenbaugh C, et al. The TOTS community intervention to prevent overweight in American Indian toddlers beginning at birth: a feasibility and efficacy study. J Community Health 2010;35:667–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muckelbauer R, Libuda L, Clausen K, et al. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics 2009;123;e661–7 [DOI] [PubMed] [Google Scholar]
- 42.James J, Thomas P, Cavan D, et al. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ 2004;328:1237–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thompson OM, Ballew C, Resnicow CK, et al. Food purchased away from home as a predictor of change in BMI z-score among girls. Int J Obes 2004;28:282–9 [DOI] [PubMed] [Google Scholar]
- 44.Galvez MP, Hong L, Choi E, et al. Childhood obesity and neighbourhood food store availability in an inner city community. Acad Pediatr 2009;9:339–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Himes JH, Ring K, Gittelsohn J, et al. Impact of the pathways intervention on dietary intakes of American Indian school children. Prev Med 2003;37:S55–61 [DOI] [PubMed] [Google Scholar]
- 46.Williams CL, Bollella MC, Strobino BA, et al. ‘Healthy-Start’: outcome of an intervention to promote a heart healthy diet in preschool children. J Am Coll Nutr 2002;21:62–71 [DOI] [PubMed] [Google Scholar]
- 47.Webber LS, Osganian SK, Feldman HA, et al. Cardiovascular risk factors among children after a 2 -year intervention—the CATCH study. Prev Med 1996;25:432–41 [DOI] [PubMed] [Google Scholar]
- 48.Bartholomew JB, Jowers EM. Increasing frequency of lower-fat entrees offered at school lunch: an environmental change strategy to increase healthful selections. J Am Diet Assoc 2006;106:248–52 [DOI] [PubMed] [Google Scholar]
- 49.Ransley JK, Greenwood DC, Cade JE, et al. Does the school fruit and vegetable scheme improve children's diet? A non-randomised controlled trial. J Epidemiol Community Health 2007;61:699–703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hendy HM, Williams KE, Camise TS. Kid's choice program improves weight management behaviours and weight status in school children. Appetite 2011;56:484–94 [DOI] [PubMed] [Google Scholar]
- 51.Bayer O, von Kries R, Strauss A, et al. Short and mid term effects of a setting based prevention program to reduce obesity risk factors in children: a cluster-randomized trial. Clin Nutr 2009;28:122–8 [DOI] [PubMed] [Google Scholar]
- 52.Marcus C, Nyberg G, Nordenfelt A, et al. A 4-year cluster- randomized, controlled childhood obesity prevention study: STOPP. Int J Obes 2009;33:408–17 [DOI] [PubMed] [Google Scholar]
- 53.Hollar D, Lombardo M, Lopez-Mitnik G, et al. Effective multi-level, multi-sector, school-based obesity prevention programming improves weight, blood pressure and academic performance, especially among low-income, minority children. J Health Care Poor Underserved 2010;21:93–108 [DOI] [PubMed] [Google Scholar]
- 54.Hastings G, Stead M, McDermott L, et al. Review of research on the effects of food promotion to children. Final report prepared for the Food Standards Agency. www.food.gov.uk/multimedia/pdfs/foodpromotiontochildren1.pdf
- 55.Rolland-Cachera MF, Peneau S. Stabilization in the prevalence of childhood obesity: a role for early nutrition? Int J Obes 2010;34:1524–5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.