Abstract
Objectives
In Bangladesh, private healthcare is common and popular, regardless of income or area of residence, making the private sector an important player in health service provision. Although the private sector offers a good range of health services, tuberculosis (TB) care in the private sector is poor. We conducted research in Dhaka, between 2004 and 2008, to develop and evaluate a public–private partnership (PPP) model to involve private medical practitioners (PMPs) within the National TB Control Programme (NTP)'s activities. Since 2008, this PPP model has been scaled up in two other big cities, Chittagong and Sylhet. This paper reports the results of this development, evaluation and scale-up.
Design
Mixed method, observational study design. We used NTP service statistics to compare the TB control outcomes between intervention and control areas. To capture detailed insights of PMPs and TB managers about the process and outcomes of the study, we conducted in-depth interviews, focus group discussions and workshops.
Setting
Urban setting, piloted in four areas in Dhaka city; later scaled up in other areas of Dhaka and in two major cities.
Findings
The partnership with PMPs yielded significantly increased case finding of sputum smear-positive TB cases. Between 2004 and 2010, 703 participating PMPs referred 3959 sputum smear-positive TB cases to the designated Directly Observed Treatment, Short-course (DOTS) centres, contributing about 36% of all TB cases in the project areas. There was a steady increase in case notification rates in the project areas following implementation of the partnership.
Conclusions
The PPP model was highly effective in improving access and quality of TB care in urban settings.
Keywords: Public Health
Article summary.
Article focus
To assess the effectiveness of a public–private partnership (PPP) model to involve the private medical sector in tuberculosis (TB) control.
To ascertain whether scaling-up of the PPP model approach to engage private medical practitioners is feasible and has an effect on case notification rates.
Key messages
This study demonstrated the feasibility and effectiveness of providing TB care through involving the private medical sector providers.
The PPP substantially improved access to and quality of TB care in urban settings, as evidenced by increased TB case notification rates and increased treatment success rates.
Our results show that it is feasible to scale up a public–private partnership within the national TB control programme.
Strengths and limitations of this study
As TB continues to be a major threat to public health in low-income and middle-income countries, and is re-emerging as an issue for concern in high-income countries, the findings of this study provide evidence for national and international scale-up of such partnerships.
By using both quantitative and qualitative methods, this study has permitted more in-depth analysis of the effectiveness of this PPP model.
From the beginning, the study was guided by a vision of nationwide scale-up.
Introduction
Despite the availability of effective treatment, the ability to control tuberculosis (TB) remains uncertain. Current estimates suggest that globally there are over 8.8 million new TB cases, and nearly 1.5 million people die from TB yearly: 98% of these cases and deaths occur in developing countries.1 The WHO predicts that 36 million people will die of TB between 2002 and 2020 if control measures do not improve.2–4 Bangladesh is among the top-10 high TB burden countries; for all forms of TB, the prevalence is 411/100 000 and the incidence is 225/100 000 population per year.1 To reduce this burden, the National TB Control Programme (NTP) has adopted the Directly Observed Treatment, Short-course (DOTS) strategy, delivered primarily through government-run health facilities.5 However, major obstacles to implementation remain, primarily owing to insufficient infrastructure and shortage of appropriately trained health personnel.6 7 These limitations mean many people with the signs and symptoms of TB, must travel considerable distances to obtain TB care, have lengthy waits to be seen when they arrive, and may not be dealt with appropriately. Health facility opening times that are inconvenient for working people also limit access to and acceptability of direct observation of treatment (DOT), a central component of DOTS. Furthermore, there is considerable stigma associated with TB, both in its own right and because of its association with HIV/AIDS. These factors combine to limit patients’ desire and ability to seek early diagnosis and treatment from public services. Consequently, large numbers of people with chest symptoms initially seek care from private healthcare providers.
Private healthcare is common in Bangladesh and popular among all, regardless of income or location. Private sector healthcare providers are generally medically trained providers working for profit and located outside the government health system. The private sector also incorporates a large number of privately managed auxiliary health services such as diagnostic laboratories, ambulance services and pharmacies/drugstores.8 These private healthcare providers are available in abundance in urban areas.9–11 There are countless untrained or non-qualified providers in Bangladesh who offer a combination of traditional (eg, Unani, ayurvedic) and western (allopathic) types of medicine but they are primarily found in rural areas.8 Although the private sector offers a range of good-quality health services, as in many other countries the care they provide for TB is poor with over-reliance on radiology (eg, x-ray) for diagnosis, use of inappropriate treatment regimens, and poor case holding, leading to incomplete treatment and potentially to multidrug-resistant TB.12–15 Moreover, non-existent linkages with the public sector means TB cases managed by private sector providers are neither recorded nor reported, so that routine cohort reporting is impossible, and outcomes are not consolidated into national data. Given this context, the task of increasing access to and quality of TB care as well as increasing the case detection rate is enormous. To achieve this task, the NTP has identified the need for collaboration between the public and private health sector providers.
In this context, we conducted research to develop and evaluate a public–private partnership (PPP) model to involve private medical practitioners (PMPs) in the NTP's urban TB control activities, and to measure to what extent the outcomes of this partnership affect access to and quality of TB care. The development and piloting of the PPP model took place in four selected research sites in Dhaka city during the period 2004–2008. Since 2008, this PPP model has been scaled up in two other cities, Chittagong and Sylhet, in addition to scaling up in other areas of Dhaka City. This paper reports the outcomes from this development, evaluation and scale-up.
Methods
Considering the research objectives and intended outcome of a change in policy and practice, an operational research methodology was thought to be appropriate based on a set of criteria underpinning the broader scope of operations research.16 17 This approach was employed to make the implementation process more participative and resource-effective, and to facilitate scale-up. Specific techniques and approaches drawn from both quantitative and qualitative research methods were used to collect multiple kinds of data for the study.18 19
The study was set within the policy environment of a government–non-governmental organizations (NGO) collaboration, enabling participation of the Society for Empowerment, Education and Development (SEED) and three other NGOs, Bangladesh Rural Advancement Committee (BRAC), Progoti Samaj Kallyan Protisthan (PSKP) and Population Services Training Centre (PSTC), which were undertaking TB control activities jointly with the NTP.
Four areas of Dhaka City—Mirpur, Rampura, Dokkhinkhan, and Kamrangirchar—were selected as study sites. Selection was purposeful, based on where the selected partner NGOs were located and had a DOTS centre, and where PMPs were major providers of health services. These study sites generally represent the geographic catchment areas of the selected NGOs covering a population of nearly 1 million.
Within this partnership, SEED was the lead research partner; BRAC, PSKP and PSTC provided TB services (diagnosis, treatment and follow-up) through designated health centres, and the NTP provided overall policy guidelines and supported the organisation and management of the research activities. In Mirpur, PSKP provided TB services through two DOTS centres and PSTC had one DOTS centre in Rampura; whereas BRAC covered both Dokkhinkhan, and Kamrangirchar through one DOTS centre in each area. PMPs agreed to refer TB suspects and patients to these designated DOTS centres following the NTP guidelines. A technical committee was formed with representation from the NTP, partner NGOs and PMPs to advise on operational issues and to support the smooth running of the partnership. A local project coordinator coordinated the project activities.
We developed and implemented the PPP model in three phases:
- Preparation phase
- Formation of a technical working group committee (TWGC);
- Collection of pre-intervention baseline data and
- Identification of tasks/service components within the partnership, based on partners’ diverse strengths.
- Intervention phase
- Strengthening DOTS centres to provide the PPP service components;
- Orientation and training of PMPs on NTP guidelines/protocols;
- Adaptation of TB forms and registers to incorporate PPP components;
- Development of diagnostic, referral and treatment protocols and linkages;
- Development and organisation of advocacy, communication and social mobilisation (ACSM) initiatives involving all stakeholders;
- Monitoring and supervision of the partnership activities and
- Evaluation of pilot phase.
- Scale-up phase
- Identification and orientation of new partners and
- Scale-up.
To evaluate the PPP, we compared TB outcomes in the intervention and control (non-PPP) areas using service statistics from the NTP and the five NGO DOTS centres involved in this project. We also collected additional baseline data from the selected PMPs (see ref. 12 for details), and used in-depth interviews, focus group discussions (FGDs) and workshops to capture PMPs’ and TB managers’ insights of the process and outcomes of the study (table 1).
Table 1.
Evaluation methods, participants, tools and focus
| Phase | Method (n) | Participants (n) | Tools | Focus |
|---|---|---|---|---|
| Preparation | ▸ Survey (1) | ▸ PMPs (60) | ▸ Semistructured questionnaire | ▸ Process |
| ▸ In-depth interviews (42) | ▸ NTP managers (12) ▸ NGO managers (6) ▸ PMPs (24) |
▸ Semistructured questionnaire | ▸ Process ▸ Outcomes |
|
| ▸ FGDs (4) | ▸ PMPs (24) | ▸ FGD guidelines | ▸ Process | |
| Evaluation | ▸ Workshops (2) | ▸ PMPs (60: 30 per workshop) | ▸ Agenda ▸ Workshop guidelines |
▸ Process ▸ Outcomes |
| ▸ Follow-up interviews (12) | ▸ PMPs (12) | ▸ Semistructured questionnaire | ▸ Process ▸ Outcomes |
FGD, focus group discussion; NGO, non-govenmental organisation; NTP, National Tuberculosis Control Programme; PMP, private medical practitioners.
Analysis of quantitative data was primarily by tabulation and graphs, and of qualitative data by thematic analysis.
Ethical approval was obtained from the University of Leeds, UK and also from appropriate in-country institutions including the Directorate General of Health Services, and the Bangladesh National TB Control Programme (NTP). All personal data have been anonymised and have remained confidential. Written informed consent was obtained from each participant of the in-depth interviews and FGDs.
Findings
Pilot implementation (2004–2008)
At inception in 2004, the PPP included 97 PMPs, but by the end of 2009, this had risen to 703. There was continuous enrolment of PMPs: although numbers fluctuated due to retirement and relocation, no PMPs chose to leave the PPP for any other reason. The male : female ratio was 6:1, reflecting the ratio among urban private health service providers.
All 703 PMPs were trained to provide quality TB care. As PMPs made it clear they were unwilling to set aside more than 2 days for training, we tailor-made a 2-day training module (based on a training-needs assessment) that included technical aspects of TB care, operational aspects of the PPP and TB record-keeping.
We used a participatory approach involving all stakeholders including PMPs to develop and revise the tools and forms. National recording and reporting forms and registers were revised to incorporate PPP elements, and to maintain records of the referrals from PMPs. These were field-tested and reviewed before use. We revised the NTP's TB treatment algorithm to incorporate a flexible referral mechanism, which allowed the DOTS centres to refer TB suspects/patients back to their respective PMPs, if the PMPs wished. We also used a participatory approach to develop ACSM materials, which were made context-specific using baseline survey data. These advocacy activities had a major role in influencing policy makers to endorse the PPP model for country-wide scale-up.
PMPs initially expected financial support from the NTP as a partnership component. This expectation was discussed with all stakeholders and it was agreed that any financial incentive would jeopardise the partnership and could prove unsustainable in the long run. At the beginning of the partnership, PMPs also expressed a lack of confidence about the quality of public sector TB services, especially of diagnosis using sputum microscopy and the NTP-recommended treatment regimen. This study addressed these issues through joint development and monitoring of partnership activities, and strong advocacy and communication campaigns.
Quantitative findings
Within the project period (2004–2008), a total of 3585 sputum-smear positive (SS+) TB patients were registered in the five DOTS centres in the project areas; of these, 647 were referred by PMPs. Numbers referred rose progressively over the period (table 2).
Table 2.
Sputum-smear positive (SS+) tuberculosis (TB) cases registered in the public -private partnership (PPP) areas
| 2004 | 2005 | 2006 | 2007 | 2008 | Total | |
|---|---|---|---|---|---|---|
| Total SS+ TB cases in the PPP areas | 533 | 673 | 800 | 830 | 749 | 3585 |
| Total SS+ TB cases referred by PMPs | 11 | 54 | 143 | 164 | 275 | 647 |
| PMPs’ contribution (%) | 2 | 8 | 18 | 20 | 37 | 18 |
PMP, private medical practitioners.
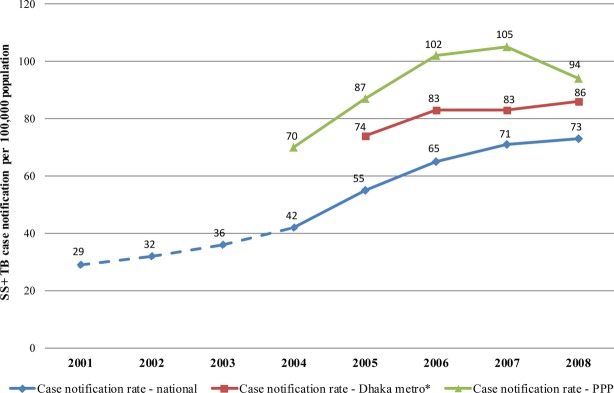
The case notification rate for new SS+ TB cases in the study areas increased steadily over the project period, and was consistently higher than the national average. By 2008, the rate in the study areas was 94/100 000 whereas the national rate was 73/100 000 (figure 1). The study rate was also consistently higher than that in Dhaka metropolitan city, which encloses the study sites (figure 1).
Figure 1.
Case notification rates of new SS+ TB (sputum-smear positive tuberculosis) cases in Dhaka metropolitan city* and the public–private partnership (PPP) project areas. *Data for Dhaka metropolitan city available only from 2005, when the National TB Control Programme started reporting for Metropolitan areas.
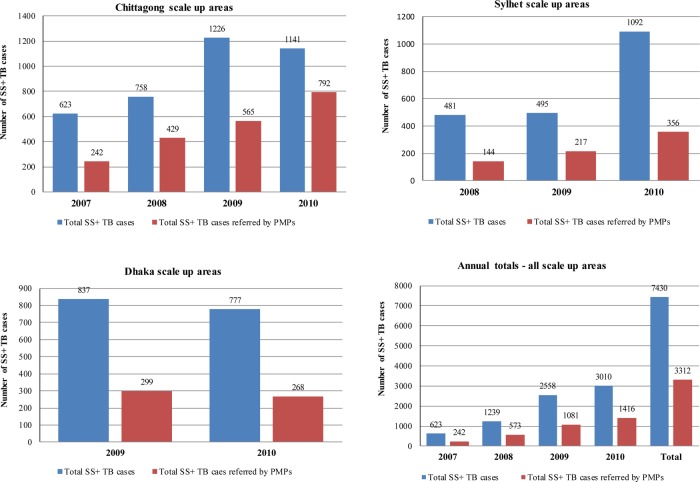
The presence of BRAC's extensive community network influenced the total number of new SS+ cases identified in the PPP areas (figure 2). In Dokkhinkhan and Kamrangirchar areas, the number of new SS+ TB cases was higher than in Mirpur and Rampura areas where BRAC's community health workers (known as Shasthya Sebika) work closely with the community to identify persons with chest complaints and advise them to go for a sputum test from a designated DOTS centre.
Figure 2.
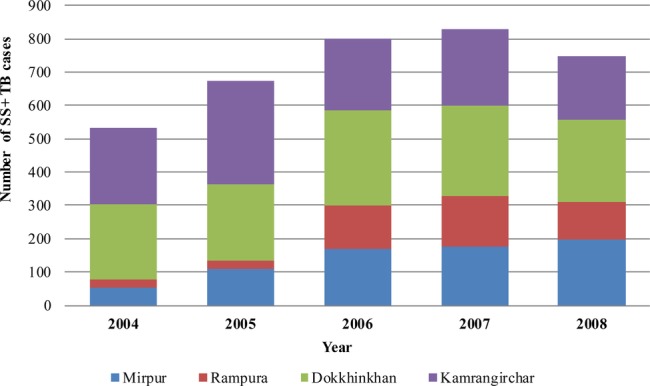
Area-wise case notification of SS+ TB (sputum-smear positive tuberculosis) in the public–private partnership (PPP) project areas: 2004–2008.
Another noticeable impact of the PPP was a large increase in the numbers of cases of extrapulmonary TB registered over time (figure 3).
Figure 3.
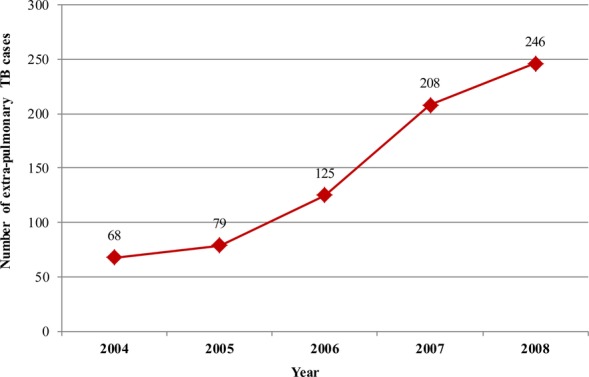
Numbers of extra-pulmonary tuberculosis (TB) cases registered in the public–private partnership (PPP) DOTS Centres.
Almost three-quarters of the reported TB cases were between 15 and 54 years of age: most male cases were detected in the 35–44 age-group, whereas the peak in females was observed in the 15–24 year age-group. The number of male cases was always higher than females cases, except in children in the 0–14 age group. Only one-third of new SS+ TB cases were female. This reflects the national distribution and trend observed by the NTP and other collaborating NGOs (figure 4).
Figure 4.
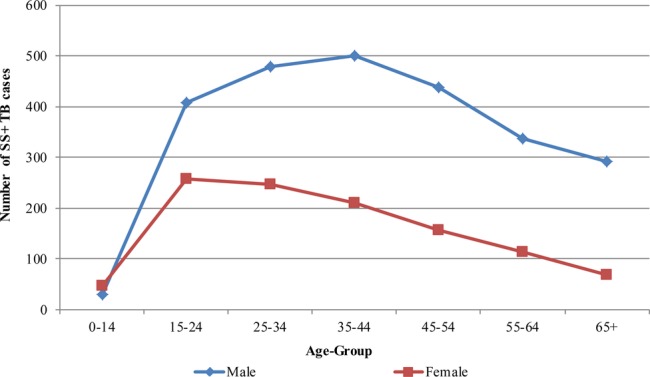
Distribution of new SS+ TB (sputum-smear positive tuberculosis) cases by age group and gender in the public–private partnership (PPP) project areas.
PMPs made a significant contribution to the numbers of TB suspects examined in the designated labs in the four PPP areas: in total, 2756 of the 24 678 TB suspects examined were referred by PMPs, with a steady rise over the study period (figure 5).
Figure 5.
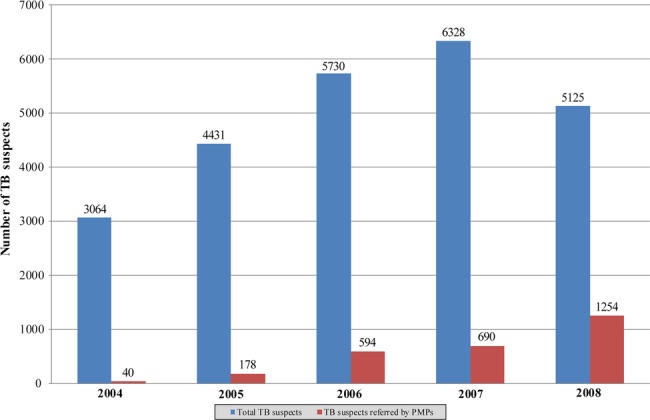
Numbers of tuberculosis (TB) suspects receiving sputum microscopy in the public–private partnership (PPP) project areas.
Scaling up and getting research into policy and practice
On the basis of the PPP pilot results, the NTP started implementing the PPP model in other cities—Chittagong (from 2007), Sylhet (2008), and other areas of Dhaka (2009)—covering more than 15 million people. In Chittagong, five NGO partners collaborated with the NTP to support the PPP; in Sylhet, BRAC was the only NGO service provider, but two medical college hospitals were also involved. In the scale-up areas, PMPs have made a substantial contribution to the NTP's effort to control TB in Bangladesh (figure 6 and table 3).
Figure 6.
SS+ TB (sputum-smear positive tuberculosis) patients registered in public–private partnership (PPP) scale-up areas and private medical practitioners’ (PMPs’) contribution, 2007–2010.
Table 3.
Total sputum-smear positive tuberculosis (SS+) tuberculosis (TB) patients in all public–private partnership (PPP) areas and private medical practitioners' (PMP) contribution, 2004–2010
| Dhaka | Chittagong | Sylhet | Total | |
|---|---|---|---|---|
| Total SS+ TB cases in the PPP areas | 5199 | 3748 | 2068 | 11 015 |
| Total SS+ TB cases referred by PMPs | 1214 | 2028 | 717 | 3959 |
| PMPs’ contribution % | 23 | 54 | 35 | 36 |
Overall impact of the PPP on TB control
The involvement of PMPs substantially increased the case finding of SS+ TB cases, a key TB control indicator. The partnership made a significant contribution in identifying SS+ TB cases: from the inception of the PPP in 2004 until 2010, 703 participating PMPs referred almost 19 000 TB suspects and 3959 SS+ TB cases to the designated DOTS centres (figure 7). Overall, almost 36% of all SS+ TB cases were attributable to involvement of the private sector providers (table 3).
Figure 7.
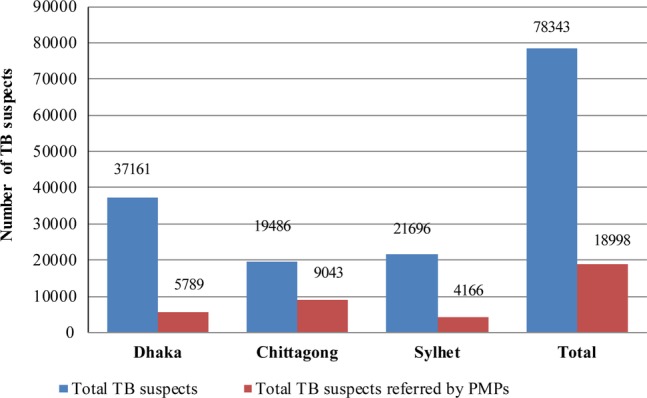
Overall private medical practitioners (PMP) contribution to identifying tuberculosis (TB) suspects in all public–private partnership (PPP) areas, 2004–2010.
Qualitative findings
The qualitative evaluation revealed that the participatory approach of planning and designing the PPP, including involvement of all stakeholders in the process of selecting service components, selecting partners and monitoring of the PPP, played a crucial part in securing commitment and ownership from all parties involved. Virtually all the PMPs interviewed (96%) mentioned having a positive experience with regard to the monitoring and support mechanism of the project, which was key to the success of the project implementation, and paved the way for scale-up. Specifically, they valued the monthly field visit by the project field staff. In reply to the question, “Do you own this project?”, a popular PMP spontaneously replied “Oh, yes. No doubt about it.” He went on to say “I have been consulted throughout the planning process of the project, and later we have jointly implemented it. So, this is our project. I am part of it.”
The quarterly review meetings were organised in rotation by the NTP and the partner NGOs either in the NTP's conference room or in one of the NGO's working locations. When asked about these arrangements, both the NTP and NGOs expressed their satisfaction and expressed their commitment to maintaining this practice in future collaborations.
All PMPs interviewed (n=24) said that they had no problems using the referral and other forms. “The (TB related) registers and referral forms are quite simple and user-friendly, and easy to maintain” said a busy practitioner. The NTP managers said they were amazed by the fact that most PMPs were keeping records. The PMPs also liked the system of referral back to the referring practitioners, which preserved their professional and commercial interests. However, a few PMPs were unhappy as they felt they did not get sufficient feedback about the patients they had referred, even though feedback was regularly given to PMPs through monthly field visits and during quarterly review meetings.
The evaluation revealed major challenges in managing the PPP. It was difficult to bring such a heterogeneous group under one umbrella, especially in the early stages of the partnership process.
Another important finding was that the public, NGO and private sector providers showed strong commitment and willingness to work together to achieve the common goal of TB control, although PMPs were initially sceptical about the motive of the public sector regarding this partnership, and the public sector and NGOs were initially doubtful whether PMPs would sacrifice their time to participate in such partnerships.
In the absence of a regulatory mechanism, the PPP was primarily based on good relationships and dialogue. Both NTP and NGO respondents stated that they were sometimes overburdened with the extra work needed to implement the partnership activities. The NTP was hit harder than the partner NGOs, because there was a shortage of staff within the NTP management. Other key challenges encountered during implementation were to maintain the progress of the partnership as it evolved, and to ensure joint ownership of decisions and collective responsibility for the direction and activities of the partnership. One senior PMP said “Initially, I thought this partnership would fail because I had serious reservations about negative attitudes of government officials. They [government officials] don't know how to give respect to anybody other than their bosses. But after getting the chance to work with the NTP, I have now changed my mind. I have found the government officials now behave much better than they used to do in the past.”
Discussion and conclusion
The PPP model was highly effective in improving access to and quality of TB care in urban settings, as evidenced by a steady increase in case notification since implementation of the partnership, exceeding internationally agreed targets, and consistently maintaining much higher rates than the national average.
Systematic implementation of the PPP led to greater and effective involvement of PMPs, resulting in increased access to quality TB care. However, needs-based training is necessary for PMPs to enhance their knowledge on the NTP guidelines with regard to appropriate diagnosis, treatment and follow-up to guarantee the continuity and quality of TB care.
The tools, protocols and ACSM materials proved vital to facilitating the partnership. The lessons learned from this partnership formed the basis of the National PPM (Public–Private Mix) guidelines. The revised tools and guidelines considerably improved the quality of TB reporting, thus strengthening the health information available. The revised protocol for referrals gave PMPs confidence that they would not lose their patients, which greatly increased their motivation to remain in the partnership.
The key challenges encountered during implementation were to maintain momentum as the partnership evolved, and to ensure joint ownership of decisions and collective responsibility for the direction and activities of the partnership. The NTP's and other partners’ commitment and nurturing of an atmosphere where all stakeholders could feel involved in the partnership were critical to overcoming these challenges.
It was possible to bring the public, NGOs and private sector health providers together to work towards achieving a common public health goal, despite perceived barriers between public and private sector providers, initial scepticism about forming the partnership and challenges during implementation of the PPP. The participatory development of the partnership and maintenance of close linkages with the PMPs helped them to gain confidence and trust in the public sector services, which in turn, facilitated the development of a close relationship with the NTP and NGO partners. However, in order to develop and sustain such a partnership, roles and responsibilities of participating agencies and individuals must be defined. These findings are consistent with the outcomes of other much smaller operational research projects implemented elsewhere.15 20–25
The selected study sites were drawn from urban DOTS areas in Bangladesh and the research was deliberately embedded within the NTP programme activities. The PPP service components were aligned with the NTP guidelines and were implemented through the NTP/NGOs' designated DOTS centres. The health system elements, particularly the type of health facilities, structure of health staffing and organisation of the TB control activities through government–NGO collaboration were similar in the study areas and in other urban areas of Bangladesh. Moreover, the type and characteristics of urban healthcare provided by private sector providers follow a similar pattern in all urban areas of the country. Therefore, the PPP can be scaled up in other urban DOTS areas as long as that human and financial resources are provided for the partnership activities.
In summary, this study demonstrated that TB control outcomes could be achieved by combining the diverse strengths and advantages of the public and private sectors, NGOs and a group of selected PMPs. High rates of case detection were attained without involving all private practitioners in the area, thus making the PPP technically attractive to national programmes in other countries in terms of the feasibility of implementation and wider scale-up.
Supplementary Material
Acknowledgments
We thank the patients, PMPs and NGOs involved in this study, and the Bangladesh NTP for permission to carry out the study. We also thank an anonymous professional colleague who reviewed the revised manuscript.
Footnotes
Contributors: ZU conceived and designed the study and led the data collection and analysis, and preparation of the manuscript; RH participated in the data analysis and in the preparation of the manuscript; AH participated in data collection and analysis; SA coordinated the study implementation and data collection; AI participated in data collection; JNN participated in the design of the study, advised on data collection and analysis and participated in the preparation of the manuscript.
Funding: This document is an output from a project funded by UK Aid from the UK Department for International Development (DFID) for the benefit of developing countries. However, the views expressed and information contained in it are not necessarily those of or endorsed by DFID, which can accept no responsibility for such views or information or for any reliance placed on them.
Competing interests: None.
Ethics approval: University of Leeds, UK and Ministry of Health and Family Welfare, Bangladesh.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.World Health Organisation Global tuberculosis control: World Health Organisation report. Geneva: World Health Organisation, 2011 [Google Scholar]
- 2.World Health Organisation Tuberculosis factsheet 2002, factsheet number 104, revised August 2002 Geneva: World Health Organisation, 2002 [Google Scholar]
- 3.Grange JM, Zumla A. The global emergency of tuberculosis: what is the cause? J R Soc Health 2002;122:78–81 [DOI] [PubMed] [Google Scholar]
- 4.Benatar S, Brock G. Global health and global health ethics, Cambridge: Cambridge University Press, 2011 [Google Scholar]
- 5.Guda DR, Khandaker IU, Parveen SD, et al. NGO and public sector tuberculosis service delivery—rapid assessment results; published for the United States Agency for International Development by the Quality Assurance Project, December 2004
- 6.World Health Organisation Tuberculosis and health sector reforms in Bangladesh—a concept paper. New Delhi: World Health Organisation, Regional Office for South-East Asia, 2004 [Google Scholar]
- 7.The National Tuberculosis Control Programme (NTP) Annual report. Dhaka: Government of Bangladesh, 2007 [Google Scholar]
- 8.Barkat A, Maksud AKM. Private sector health services in Bangladesh: an exploratory study, prepared for Engender health. Dhaka: Human Development Research Centre (HDRC), 2003 [Google Scholar]
- 9.UNICEF Public-private partnership in the social sector-part two: country experiences. Dhaka: UNICEF Bangladesh, 1999:219–91 [Google Scholar]
- 10.Zafar Ullah AN, Lubben M, Newell JN. A model for effective involvement of private medical practitioners in TB care. Int J Health Plann Manag 2004;19:227–45 [DOI] [PubMed] [Google Scholar]
- 11.World Bank Comparative advantages of public and private health care providers in Bangladesh; Bangladesh development series paper no. 4. South Asia Human Development Unit, Dhaka: The World Bank Office, 2005 [Google Scholar]
- 12.Zafar Ullah AN, Huque R, Begum V, et al. Public-private partnership for TB control in Bangladesh: role of private medical practitioners in the management of TB patients. World Med Health Policy 2010;2: Article 13:217–34. [Google Scholar]
- 13.Uplekar MW, Juvekar SK, Monarkar S, et al. Tuberculosis patients and practitioners in private clinics in India. Int J Tuberc Lung Dis 1998;2:324–9 [PubMed] [Google Scholar]
- 14.World Health Organisation Involving private medical practitioners in TB and STI control. New Delhi: World Health Organisation, 2001 [Google Scholar]
- 15.Newell JN, Pande SB, Baral SC, et al. Control of Tuberculosis in an urban setting in Nepal: public-private partnership. Bull World Health Organ 2004;82:92–8 [PMC free article] [PubMed] [Google Scholar]
- 16.Walley J, Graham K, Wei X, et al. Getting research into practice: primary care management of noncommunicable diseases in low-and middle income countries. Bull World Health Organ 2012;90:402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zachariah R, Harries AD, Ishikawa N, et al. Operational research in low-income countries: what, why, and how? Lancet Infect Dis 2009;9:711–17 [DOI] [PubMed] [Google Scholar]
- 18.Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educ Res 2004;33:14–26 [Google Scholar]
- 19.Patton MQ. Qualitative research & evaluation methods. 3rd edn London: Sage Publications, 2002 [Google Scholar]
- 20.Newell JN, Pande SB, Baral SC, et al. Leadership, management and technical lessons learnt from a successful public-private partnership for TB control in Nepal. Int J Tuberc Lung Dis 2005;9:1013–17 [PubMed] [Google Scholar]
- 21.Porter JD, Ogden JA, Rao PV, et al. Introducing operations research into management and policy practices of a non-governmental organization (NGO): a partnership between an Indian leprosy NGO and an international academic institution. Health Policy Plan 2004;19:80–7 [DOI] [PubMed] [Google Scholar]
- 22.Rangan S. The public-private mix in India's Revised National Tuberculosis Control Programme: an update. J Indian Med Assoc 2003;101:161–3 [PubMed] [Google Scholar]
- 23.Rangan S, Rasalpurkar SB, Morankar SN, et al. Tuberculosis control in rural India: lessons from public-private collaboration. Int J Tuberc Lung Dis 2004;8:552. [PubMed] [Google Scholar]
- 24.Dewan P, Lal SS, Lonnroth K, et al. Improving tuberculosis control through public-private collaboration in India. Literature review. BMJ 2006;332:574–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dreesch N, Nyoni J, Mokopakgosi O, et al. Public-private options for expanding access to human resources for HIV/AIDS in Botswana. Hum Res Health 2007;5:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.