Abstract
Objective
Magnesium (Mg) is thought to be an important element in the pathogenesis of acute asthma attacks. We hypothesized that erythrocytic Mg would be decreased during an acute asthma exacerbation. We aimed at investigating plasma and erythrocytic Mg in acute asthmatic children.
Methods
This case-control study included 30 Egyptian outpatients with acute asthma. Thirty healthy matched children were included as controls. All candidates had measurements of plasma and erythrocytic Mg levels before and after treatment.
Findings
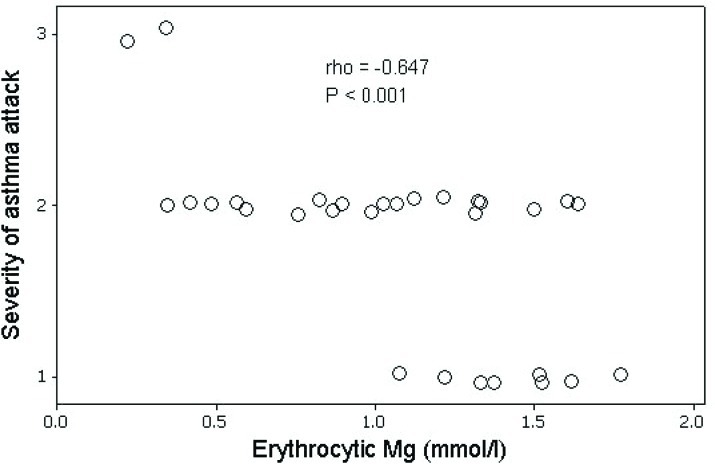
No significant differences were detected in plasma Mg levels between cases and controls (1.53±0.33 mmol/L versus 1.67±0.50 mmol/L respectively, P =0.2). However, erythrocytic Mg levels were significantly reduced in cases when compared to controls (1.06±0.43 mmol/L versus 2.57±0.59 mmol/L respectively, P<0.001). Plasma Mg levels did not significantly change in acute asthmatics before and after their rescue treatment (1.53±0.33 mmol/L versus 1.68±0.31mmol/L respectively, P=0.07). In contrast, the study detected a significant increase in erythrocytic Mg levels in cases after their treatment from acute attacks (1.06±0.43 mmol/L versus 1.56±0.23 mmol/L respectively, P<0.001), with significant negative correlation with severity of attack (Spearman's rho = -0.647, P<0.001).
Conclusion
Erythrocytic Mg levels were significantly lower during the acute asthma, and were negatively correlated with severity of exacerbation, while plasma Mg did not significantly change. Only erythrocytic Mg levels were significantly elevated after receiving rescue treatment.
Keywords: Asthma, Children, Erythrocytes, Magnesium
Introduction
Asthma continues to be the most prevalent chronic disease in childhood[1]. Continuous efforts are still exerted to understand the natural history and pathogenesis of this disease in order to alleviate its burden on children and their families[2]. Magnesium (Mg) is an abundant intracellular cation. It is involved in numerous physiological functions, including protein folding, intracellular signaling, enzymatic reactions involving protein and nucleic acid metabolisms and enzyme catalysis[3]. Mg is involved in pathophysiological reactions related to asthma; it has been shown to relax bronchial smooth muscles in vitro and to dilate asthmatic airways in vivo[4]. Inhibition of release of acetylcholine from cholinergic nerve terminals and of histamine from mast cells, promotion of nitric oxide synthesis and prostacycline generation are all associated with changes in intracellular Mg concentrations. It has been shown that intravenous administration or inhalation of Mg could alleviate symptoms in acute asthma[5].
Our study hypothesized that erythrocytic (intracellular) Mg would be decreased during an acute asthma exacerbation. Low intracellular Mg concentrations in adults[6] and children[7] with acute asthma have been previously reported. However, published works addressing this issue are relatively few. More efforts need to be conducted in order to build stronger evidence.
The present study aimed at measuring Mg concentrations in plasma and erythrocytes of children with acute asthma exacerbations, comparing them to matched healthy controls.
Subjects and Methods
Study Design
This is a case-control study that was conducted at University Children's Hospital, Faculty of Medicine, Cairo University and Heliopolis Hospital in Cairo, Egypt, in the period from November, 2009 to November, 2010. Thirty Egyptian patients were included as cases. They were outpatients suffering from acute asthma attack and treated in the emergency departments. Thirty healthy age-and sex-matched non-asthmatic children were included in this study as controls. Sample size was calculated using Power and Sample Size Calculator version 3.0.34 [Freeware] based on the following parameters: power = 0.82, case/control ratio = 1, standard deviation = 0.05 and type-I error = 0.5.
Inclusion and Exclusion Criteria
Cases fulfilled the following inclusion criteria: Aged 2 to 16 years, diagnosed as asthmatics according to Global Initiative for Asthma (GINA) guidelines[8] and had acute asthma attack (mild, moderate or severe) according to GINA Guidelines[8] at the time of inclusion. Patients were excluded if they had chest infection/chest disease other than asthma, if they had diseases known to cause hypomagnesemia, if they had received Mg-containing drugs or drugs that might affect the hydration and/or Mg status of the body, if they received any rescue treatment for acute asthma within 24 hours before inclusion or if they refused to participate in the study. Short-acting bronchodilators given were in the form of nebulized salbutamol sessions of 5 minutes each for a maximum of 2 sessions 15 minutes apart, systemic steroids were added to severe cases. Those who needed more treatment were excluded to avoid the effect of therapy on Mg concentrations.
Ethical Considerations
The study design conformed to the Revised Helsinki Declaration of Bioethics[9], and was approved by the Research Ethics Committee of Department of Pediatrics, Faculty of Medicine of Cairo University. Participant's anonymity was preserved and an informed written consent was obtained from parents and/or surrogates of all study candidates before enrollment.
All candidates were subjected to a complete clinical study (thorough history and physical examination). The following investigations were performed: complete blood counts (CBC) and measurement of plasma and erythrocytic Mg levels immediately before taking any bronchodilator therapy and within half an hour after that. No Mg-containing medications were used in this study. Venous blood samples were withdrawn without tourniquet into heparinized metal-free test tubes and a CBC was performed immediately. Samples were centrifuged at 650g for 10 minutes and plasma and erythrocytes were separated, then 100 microliters of erythrocytes were lysed by addition of 1.5 ml of double-distilled water. Hemolysed samples were excluded from the study. Both plasma and lysed erythrocytes were stored at -20°C until the time of analysis. Erythrocytic and plasma Mg levels were analyzed using atomic absorption spectrophotometery.
Statistical Analysis
This was performed using Minitab 16 software (Minitab Inc. USA). The following tests were used: Frequency distributions, means±standard deviation, t-test, chi-square test and tests of correlation. P-values <0.05 were considered significant. The 95% confidence intervals (95% CI) were calculated when appropriate.
Findings
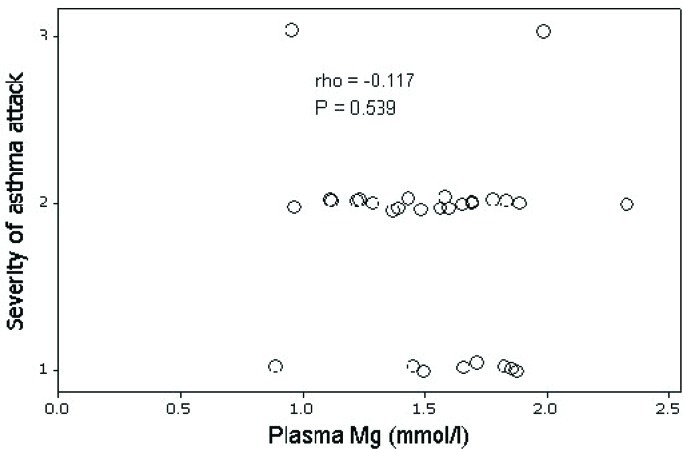
Groups were matched as regards age and sex. Acute asthmatics were significantly higher in vital signs, total leucocytic and eosinophilic counts (P<0.001). There was no significant difference between groups as regards plasma Mg levels. However, erythrocytic Mg levels were significantly reduced in cases when compared to controls (P<0.001). About 26% of patients had mild attack, while nearly 67% had moderate attack and 6.6% had severe attack (Table 1). There was a significant improvement of vital signs of patients after treatment (P<0.001) but no significant change in leucocytic or eosinophilic counts. Plasma Mg levels did not significantly change in acute asthmatics before and after their rescue treatment. In contrast, the study detected a significant increase in erythrocytic Mg levels in patients after their treatment (P<0.001) (Table 2). There was no significant correlation between plasma Mg and severity of attack (Fig. 1). However, there was a significant negative correlation between erythrocytic Mg and severity of attack (P<0.001) (Fig. 2).
Table 1.
Comparison between cases and controls
| Cases (30) a | Controls (30) a | 95% CI | P-value | |
|---|---|---|---|---|
| Age (years) | 8.23(3.02) | 8.36 (3.164) | -1.61; 1.63 | 0.997 |
| Sex (male/female) | 15.15 | 15/15 | - | 0.998 |
| Heart rate (per minute) | 98.90 (6.58) | 91.87(6.12) | 3.75; 10.32 | < 0.001 |
| Respiratory rate (per minute) | 38.73 (3.34) | 31.80(4.29) | 4.94; 8.92 | < 0.001 |
| Temperature (°C) | 37.14 (0.22) | 36.97(0.185) | 0.07; 0.28 | 0.001 |
| Cough (present/absent) | 21.9 | - | - | - |
| Severity of acute attackb | 8.20.2 | - | - | - |
| RBCs (106/cmm) | 4.36 (0.57) | 4.28 (0.48) | -0.71; 0.87 | 0.819 |
| TLC (1000/cmm) | 7.46(2.32) | 5.40 (1.35) | 1.08; 3.05 | < 0.001 |
| Eosinophils (cells/cmm) | 361.5 (132.7)8 | 174.7 (76.83) | 130.40; 243.20 | < 0.001 |
| Plasma Mg (mmol/L) | 1.53 (0.33) | 1.67 (0.50) | - 0.36; 0.07 | 0.193 |
| Erythrocytic Mg (mmol/L) | 1.06(0.43) | 2.57 (0.59) | -1.77; -1.24 | < 0.001 |
mean (standard deviation) or frequency
mild, moderate and severe attacks
CI, confidence intervals; RBCs, red blood cells; TLC, total leucocytic count
Table 2.
Comparison of cases before and after attack treatment
| Cases (30) | Before treatment a | After treatment a | 95% CI | P-value |
|---|---|---|---|---|
| Heart rate (per minute) | 98.90 (6.58) | 89.50 (3.36) | 6.68 – 12.12 | <0.001 |
| Respiratory rate (per minute) | 38.73 (3.34) | 30.33 (2.19) | 6.93 – 9.86 | <0.001 |
| Plasma Mg (mmol/L) | 1.53 (0.33) | 1.68 (0.31) | - 0.32 – 0.01 | 0.07 |
| Erythrocytic Mg (mmol/L) | 1.06 (0.43) | 1.56 (0.23) | - 0.67 – (- 0.31) | <0.001 |
Mean (standard deviation); CI, confidence intervals
Fig. 1.
Correlation between plasma Mg and severity of asthma attack
Fig. 2.
Correlation between erythrocytic Mg and severity of asthma attack
Discussion
Plasma levels of Mg were not significantly different between acute asthmatic children and controls. This agrees with the results of previous similar works; Sedighi et al[7] conducted a study that reported no significant differences in plasma Mg (P=0.06). Again, Aggarwal et al[10] reported that plasma Mg levels remained within normal. Emelyanov et al[11] reported similar results. In contrast to plasma Mg, our study detected that erythrocytic Mg levels were significantly lower during acute asthmatic episodes when compared to controls and there was a significant negative correlation between erythrocytic Mg and severity of asthma attack. These findings support the study's hypothesis. It is suggested that reduced intracellular Mg might have partly precipitated acute asthma attack. Zervas et al[6] reported similar results in adults during acute asthma; they concluded that acute asthma was associated with lower erythrocyte Mg content while plasma levels remained unchanged. Sedighi et al[7] reported significantly reduced erythrocytic Mg in acute asthmatic children compared to controls.
Our study attempted to further investigate the intracellular and extracellular Mg concentrations of the same group of acute asthmatics before and after receiving rescue treatment (no Mg treatment was given). It was found that plasma Mg levels did not differ significantly. However, erythrocytic Mg concentration was found to increase significantly after receiving treatment for acute asthma. This reflects that Mg content of the body - measured intracellularly in erythrocytes - was deficient at the onset of acute asthma attack, that it started to increase after the attack, and that this change could not have been detected if we relied on plasma Mg measurement. Low erythrocytic Mg reflects relative Mg deficiency in other cell types pertinent to asthma, like inflammatory cells, smooth and skeletal muscle cells. This agrees with the findings of Hashimoto et al[12] who reported that 40% of asthmatic patients demonstrated Mg deficiency, and that the low Mg concentration in erythrocytes reflected decreased Mg stores in patients with bronchial asthma. Some studies, however, did not find any significant difference in Mg concentrations (both intracellular and extracellular) between asthmatics and normal subjects. This includes the studies of Kazaks et al[13] and de Valk et al[14]. Although these studies do not agree with our results, yet they were conducted on adults and focused mainly on milder degrees of exacerbations, which might explain the different findings.
Our study added to the relatively few works conducted on children and it did find a significant negative correlation between intracellular Mg andconducted on children and it did find a significant negative correlation between intracellular Mg and severity of attack. However, there were points of weakness: the small sample size, the use of erythrocytes instead of other cells more relevant to asthmatic inflammation and the lack of pulmonary function testing. It is recommended to repeat this study on a larger scale with a longitudinal design to allow for follow up.
Conclusion
Erythrocytic Mg levels in asthmatics were significantly lower than in normal controls during the acute asthma attacks in children, and were negatively correlated with severity of the attack, while plasma Mg did not significantly change. Moreover, only erythrocytic Mg was significantly elevated after receiving rescue treatment.
Acknowledgment
Authors wish to thank Mr. Abdu El Nayeh MSc, researcher at the National Institute of Research (NRC) in Cairo, Egypt for his contribution in the laboratory part of this study.
Conflict of Interest
None
References
- 1.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005-2009. Natl Health Stat Report. 2011;32:1–14. [PubMed] [Google Scholar]
- 2.Szefler SJ. Advances in pediatric asthma in 2010: addressing the major issues. J Allergy Clin Immunol. 2011;127(1):102–15. doi: 10.1016/j.jaci.2010.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rowe BH, Camargo CA., Jr The role of magnesium sulfate in the acute and chronic management of asthma. Curr Opin Pulm Med. 2008;14(1):70–6. doi: 10.1097/MCP.0b013e3282f19867. [DOI] [PubMed] [Google Scholar]
- 4.Kowal A, Panaszek B, Barg W, et al. The use of magnesium in bronchial asthma: a new approach to an old problem. Arch Immunol Ther Exp (Warsz) 2007;55(1):35–9. doi: 10.1007/s00005-007-0008-8. [DOI] [PubMed] [Google Scholar]
- 5.Bichara MD, Goldman RD. Magnesium for treatment of asthma in children. Can Fam Physician. 2009;55(9):887–9. [PMC free article] [PubMed] [Google Scholar]
- 6.Zervas E, Papatheodorou G, Psathakis K, et al. Reduced intracellular Mg concentrations in patients with acute asthma. Chest. 2003;123(1):113–8. doi: 10.1378/chest.123.1.113. [DOI] [PubMed] [Google Scholar]
- 7.Sedighi M, Pourpak Z, Bavarian B, et al. Low magnesium concentration in erythrocytes of children with acute asthma. Iran J Allergy Asthma Immunol. 2006;5(4):183–6. [PubMed] [Google Scholar]
- 8.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention NIH Pub. No 02-3659, January 1995. Updated 2008. Available from: www.ginasthma.com.Access date: Nov 3, 2009.
- 9.World Medical Association Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects. Revised by the 59th WMA General Assembly. Available from: http://www.wma.net/en/30publications/10policies/b3/index.html.Access date: Nov 3, 2009.
- 10.Aggarwal P, Sharad S, Handa R, et al. Comparison of nebulized magnesium sulphate and salbutamol combined with salbutamol alone in the treatment of acute bronchial asthma: a randomized study. Emerg Med J. 2006;23(5):358–62. doi: 10.1136/emj.2005.026203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emelyanov A, Fedoseev G, Barnes PJ. Reduced intracellular magnesium concentrations in asthmatic patients. Eur Respir J. 1999;13(1):38–40. doi: 10.1183/09031936.99.13103899. [DOI] [PubMed] [Google Scholar]
- 12.Hashimoto Y, Nishimura Y, Maeda H, Yokoyama M. Assessment of magnesium status in patients with bronchial asthma. J Asthma. 2000;37(6):489–96. doi: 10.3109/02770900009055475. [DOI] [PubMed] [Google Scholar]
- 13.Kazaks AG, Uriu-Adams JY, Albertson TE, Stern JS. Multiple measures of magnesium status are comparable in mild asthma and control subjects. J Asthma. 2006;43(10):783–8. doi: 10.1080/02770900601031870. [DOI] [PubMed] [Google Scholar]
- 14.de Valk HW, Kok PT, Struyvenberg A, et al. Extracellular and intracellular magnesium concentrations in asthmatic patients. Eur Respir J. 1993;6(8):1122–5. [PubMed] [Google Scholar]
- 15.Britton J, Pavord I, Richards K, et al. Dietary magnesium, lung function, wheezing, and airway hyperreactivity in a random adult population sample. Lancet. 1994;344(8919):357–62. doi: 10.1016/s0140-6736(94)91399-4. [DOI] [PubMed] [Google Scholar]
- 16.Fox C, Ramsoomair D, Carter C. Magnesium: its proven and potential clinical significance. South Med J. 2001;94(12):1195–201. [PubMed] [Google Scholar]