Abstract
Objective
Cow's milk allergy has different presentations in children and can cause functional bowel symptoms such as chronic constipation. The aims of this study were to investigate the role of cow's milk allergy as a cause of chronic constipation and effect of cow's milk free diet (CMFD) on its treatment in children.
Methods
We performed a randomized clinical study comparing CMFD with cow's milk diet (CMD) in two groups each consisting of 70 patients (age range, 1-13 years) with chronic functional constipation (defined as Rome III criteria). All subjects had been referred to a pediatric gastroenterology clinic and had previously been treated with laxatives for at least 3 months without success; also all 140 patients performed skin prick test. The case group received CMFD for 4 weeks. After that they received CMD for 2 extra weeks. The control group received CMD for whole 6 weeks. A response was defined as decreased in signs and symptoms that not fulfilled Rome III criteria after 4 weeks of CMFD and came back to Rome III criteria after 2 weeks of CMD challenge.
Findings
After 4 weeks 56 (80%) patients of the case group responded in comparison to 33 (47.1%) patients in the control group (P=0.0001). In the case group after 2 weeks challenge 24 out of 56 (42.8%) responders developed constipation according to Rome III criteria. With other words, the frequency of cow's milk allergy among constipated patients was 80%. Only one patient had positive skin prick test.
Conclusion
In children, chronic constipation can be a manifestation of cow's milk allergy. At present, although several aspects must be further investigated, a therapeutic attempt with elimination diet is advisable in all children with constipation unresponsive to correct laxative treatment.
Keywords: Cow's Milk, Milk Allergy, Allergy, Chronic Constipation, Children
Introduction
As a gastrointestinal (GI) disease chronic constipation is very common in the general population with a prevalence of nearly 20%[1]. It is also very common in children with a frequency between 3% and 16%[2]. In dealing with this disease, it is important to be sure that it is not secondary to other conditions, like thyroid disease or congenital anomaly of GI tract. Life style modification can be the first management in chronic functional constipation. Then, if no response is achieved, a therapeutic trial with fiber and/or simple laxatives is suggested. In spite of these modalities many patients do not respond. It has been reported that at the end of a 5-year follow-up study, no improvement was seen in 35-45% of the patients[3].
In children with chronic constipation not responding to laxative treatment the symptom may be due to other causes, one of them being cow's milk allergy[4–6].
Association between cow's milk allergy and chronic constipation has been reported by Buisseret in 1978[7]. In an open but not placebo-controlled study by Iacono et al, was shown that 21 of 27 patients with refractory constipation responded to a cow's milk free diet (CMFD)[5].
Many reports showed the relationship between chronic constipation and cow's milk allergy, but some were against[6, 8–15]. Loening-Baucke reported no improvement of the symptom in children with chronic constipation who had a history of cow's milk allergy and have been on CMFD[3]. Yimyaem et al reviewed the results of 10 cow's milk allergy patients studied from 1997 to 2001 and did not find any relation with constipation[16].
In order to clarify these apparently conflicting results we decided to check the effect of CMFD on our patients with chronic constipation.
Subjects and Methods
In this randomized clinical trial all consecutive patients less than 14 years of age with chronic constipation referred to Pediatric Gastroentero-logy Clinic affiliated with Shiraz University of Medical Sciences between April 2009 and April 2010 were evaluated. We used Rome III criteria for definition of functional constipation[17], i.e. two or more of the following in a child with a developmental age of at least 4 years with insufficient criteria for diagnosis of inflammatory bowel syndrome:
Two or fewer defecations in the toilet per week.
At least 1 episode of fecal incontinence per week.
History of retentive posturing or excessive volitional stool retention.
History of painful or hard bowel movements.
Presence of a large fecal mass in the rectum.
History of large diameter stools that may obstruct the toilet.
Criteria fulfilled at least once per week for at least 2 months before diagnosis, and one month of at least two of the following in infants up to 4 years of age:
Two or fewer defecations per week.
At least one episode/week of incontinence after the acquisition of toileting skills.
History of excessive stool retention.
History of painful or hard bowel movements.
Presence of a large fecal mass in the rectum.
History of large diameter stools which may obstruct the toilet[17].
The exclusion criteria were anatomical causes of constipation (eg, Hirschsprung's disease, spinal disease), constipation due to other disorders (eg, hypothyroidism, psychomotor retardation), prior anal surgery, and use of medications that can cause constipation.
140 children were enrolled: 73 boys and 67 girls (52.1% and 47.9%, respectively), age range, 1-13 years; (mean, 4.6±2.7 years). They all fed cow's milk, dairy products, or commercial formulas derived from cow's milk. Previous treatment with different laxatives such as lactulose, Mg(OH)2, paraffin, and PEG for at least three months had been unsuccessful in all patients. When the patient was first seen, complete physical examination including rectal examination was done and a detailed chart was compiled containing the results of the physical examination and medical history information such as breast feeding during the first months of life, acceptance of formula at weaning, and especially the presence or absence of Rome III criteria. Next day the patient received Skin Prick Test.
Diagnosis of cow's milk allergy induced constipation was based on increased frequency of defecation or decreased number of signs and symptoms after 4 weeks CMFD and coming back to Rome III criteria after 2 weeks of challenge with CMD in comparison to the control group. We define CMFD as a diet free of any dairy products made of cow's milk.
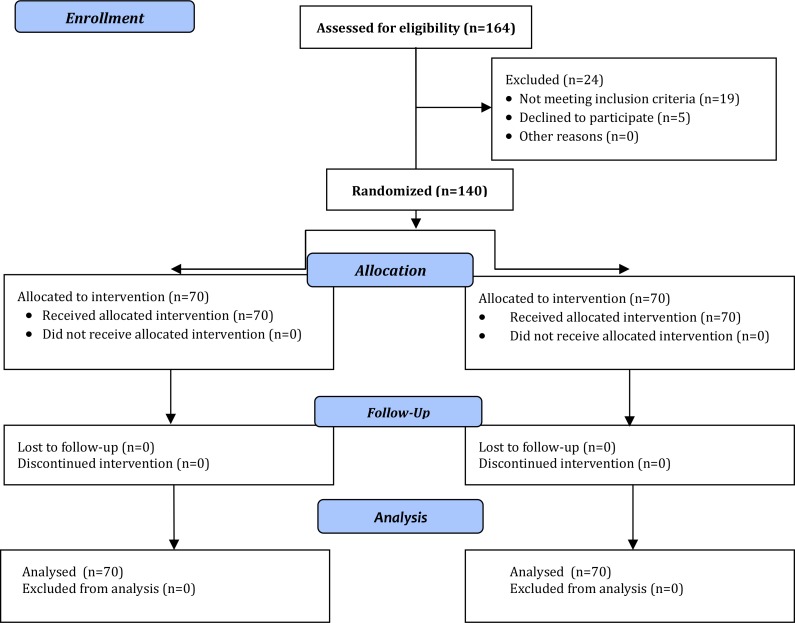
Fig. 1.
Flow diagram of patients
At the first visit, the parents were asked to record the child's signs and symptoms, and all medications were discontinued. Then the patient was assigned to receive PEG solution 0.5 gram/Kg/day and CMFD or PEG solution with the same dose and CMD for the next 4 weeks. PEG was prescribed by pediatric gastroenterologist to all patients. The order of dietary treatment was randomly assigned by a computer generated method with the individual patient as the unit of randomization and according to this randomization the patients were recommended to receive CMFD or CMD by a pediatric allergist. At the end of the treatment, the protocols were evaluated again by pediatric gastroenterologist who was blinded to the type of diet. At baseline and at the end of the first study periods, the children were examined by a researcher. During the study period, the parents recorded the number of bowel movements, as well as the appearance of the stools and the child's difficulty in passing them. To ensure that the children did not receive any other kind of milk or milk-containing foods during the study, the parents were given a list of the most common milk-containing foods to be avoided. During the study period, they were asked to record the amount and type of food their child had eaten each day. At the end of the study, we analyzed these diaries to evaluate adherence to the diet and the quantity of milk consumed. The parents were able to contact us whenever necessary, and telephone contacts helped to ensure adherence to the diet. After the first study period, the children who were on the CMFD were given the CMD for another two weeks. During the two week challenge period, the parents recorded any clinical symptoms, and the patients were reexamined in the hospital for any adverse reaction, and at the end of the challenge period they were evaluated for presence of constipation again. Informed consent was obtained from the parents of all the patients involved in the study. The study was approved by Institutional Review Board of Shiraz University of Medical Sciences. Frequency analysis was performed with Fisher's exact test. The Pearson Chi-Square and McNemar tests were used to compare the Rome criteria, and Student's t-test for parametric analysis. All P-values were two-tailed, and P-values less than 0.05 were considered to indicate statistical significance.
Findings
Two groups were matched for age, sex, duration of illness, frequency of breast feeding at birth and signs and symptoms of constipation at the time of entry to study. The base-line characteristics of the 140 patients are shown in Tables 1 and 2. Eighty-four (60%) children had abdominal pain and only 7 (5%) patients had anal fissures. After 4 weeks 56 (80%) patients of the case group responded in comparison to 33 (47.1%) patients in control group (P=0.0001). The comparison of Rome criteria in the case group before trial and 4 weeks after CMFD are shown in Table 3. Table 4 shows the comparison of these criteria between case and control group. All patients in case group underwent a challenge with CMD for two weeks. The comparison of Rome criteria in case group before trial and at the end of trial are shown in Table 5. None of the patients who received CMD had an acute reaction. After this period 24 out of 56 (42.8%) responders developed constipation according to Rome III criteria. With other words, the frequency of cow's milk allergy among constipated patients was 80% but the frequency of cow's milk allergy induced constipation based on our definition (increased frequency of defecation or decreased number of signs and symptoms after 4 weeks CMFD and coming back to Rome III criteria after 2 weeks of challenge with CMD) was 34.3%.
Table 1.
Clinical characteristics of children with chronic constipation before trial
| Parameter | Patients on Cow's Milk Free Diet (n = 70) | Patients on Cow's Milk Diet (n = 70) | P-value |
|---|---|---|---|
| Age [mean (SD)](months) | 54.7 (32.2) | 55.5 (34.1) | 0.887 |
| Sex (Male/Female) | 39/31 | 34/36 | 0.501 |
| Breast feeding at birth (%) | 23 (32.9) | 17 (24.3) | 0.348 |
| Duration of illness [mean (SD)](months) | 26.3 (22.7) | 26.1 (19.3) | 0.955 |
| Abdominal pain | 40 | 44 | 0.606 |
| Anal fissure | 5 | 2 | 0.447 |
Table 2.
Comparison of Rome criteria in children with chronic constipation before trial
| Parameter | Patients on Cow's Milk Free Diet (n = 70) | Patients on Cow's Milk Diet (n = 70) | P-value |
|---|---|---|---|
| ≤ 2 defecations per week | 56 | 63 | 0.2 |
| ≥ 1episode/week of incontinence after the acquisition of toileting skills | 28 | 25 | 0.7 |
| History of retentive posturing or excessive volitional stool retention | 61 | 58 | 0.6 |
| History of painful or hard bowel movements | 69 | 66 | 0.4 |
| Presence of a large fecal mass in the rectum | 40 | 63 | 0.0001 |
| History of large diameter stools | 69 | 66 | 0.4 |
Table 3.
Comparison of Rome criteria in children with chronic constipation before trial and 4 weeks after cow's milk free diet
| Parameter | Patients on Cow's Milk Free Diet before Trial (n = 70) | Patient on Cow's Milk Free Diet after 4 Weeks (n = 70) | P-value |
|---|---|---|---|
| ≤ 2 defecations per week | 56 | 3 | 0.000 |
| ≥ 1 episode/week of incontinence after the acquisition of toileting skills | 28 | 2 | 0.000 |
| History of retentive posturing or excessive volitional stool retention | 61 | 7 | 0.000 |
| History of painful or hard bowel movements | 69 | 9 | 0.000 |
| Presence of a large fecal mass in the rectum | 40 | 2 | 0.000 |
| History of large diameter stools | 69 | 9 | 0.000 |
Table 4.
Comparison of Rome criteria in children with chronic constipation on cow's milk free diet and cow's milk diet after 4 weeks
| Parameter | Patients on Cow's Milk Free Diet (n = 70) | Patients on Cow's Milk Diet (n = 70) | P-value |
|---|---|---|---|
| ≤ 2 defecations per week | 3 | 20 | 0.0003 |
| ≥ 1 episode/week of incontinence after the acquisition of toileting skills | 2 | 15 | 0.002 |
| History of retentive posturing or excessive volitional stool retention | 7 | 19 | 0.02 |
| History of painful or hard bowel movements | 9 | 32 | 0.0001 |
| Presence of a large fecal mass in the rectum | 2 | 20 | 0.0001 |
| History of large diameter stools | 9 | 32 | 0.0001 |
Table 5.
Comparison of Rome criteria in children with chronic constipation on cow's milk free diet before trial and 2 weeks after cow's milk diet challenge
| Parameter | Patients on Cow's Milk Free Diet before Trial (n = 70) | Patient on Cow's Milk Free Diet 2 Weeks after Cow's Milk Diet Challenge (n = 70) | P-value |
|---|---|---|---|
| ≤ 2 defecations per week | 56 | 11 | <0.001 |
| ≥ 1 episode/week of incontinence after the acquisition of toileting skills | 28 | 7 | <0.001 |
| History of retentive posturing or excessive volitional stool retention | 61 | 10 | <0.001 |
| History of painful or hard bowel movements | 69 | 20 | <0.001 |
| Presence of a large fecal mass in the rectum | 40 | 7 | <0.001 |
| History of large diameter stools | 69 | 20 | <0.001 |
At beginning of the study there was a trend towards a high frequency of negative skin prick test among the patients with functional constipation, and in only one child with cow's milk allergy induced constipation it was positive.
Discussion
Cow's milk allergy has many signs and symptoms. Some studies showed that chronic diarrhea is the mostly encountered GI symptom of cow's milk allergy in children[6], constipation being another but not too frequent symptom. It is not yet confirmed that allergy to cow's milk could cause refractory chronic constipation.
Several clinical studies have been done in pediatric cow's milk allergy with inconsistent results. Recently it is agreed that constipation seems to be the result of hypersensitivity to cow's milk proteins[4–12, 18]. In a recent study the role of allergy in the etiology of constipation in children was investigated. Nighty-nine out of 136 (72.8%) constipated children less than 3 years of age had allergy to cow's milk protein as a cause of constipation and after introduction of the elimination diet clinical improvement was observed in all children. The authors concluded that cow's milk allergy is the most common cause of constipation in the first three years of life[19].
Syrigou EI et al in Greece showed that constipation was improved in 28/32 constipated children with positive atopy patch test (APT) after withdrawing the APT-positive foods for an 8-week period[20]. We found a relation between the intake of cow's milk products and constipation in about one third (34.3%) of the patients. In a study in Spain 35 of the 69 constipated children (51%) improved during the first CMFD period, 8 of these did not develop constipation when CM was reintroduced, and other 27 children (39%) developed constipation during the CM challenge and improved during the second CMFD phase, which is consistent with our study[21].
Only one patient had positive skin prick test. Positive skin prick test response indicates the possible association between the food tested and the patient's reaction to that specific food. Although positive skin prick test response only “suggests” the presence of symptomatic allergy, the negative skin prick test response is an excellent means of excluding IgE-mediated food allergy. In this regard Irastorza I et al did not find an IgE-mediated immunologic mechanism in children with chronic constipation[21], but for approving this, further study is needed. The present study showed that excluding cow's milk products from children's diet with chronic constipation is associated with improvement of the signs and symptoms in 80% of patients. This percent of responding to elimination diet was the same as in other studies[4–6, 18]. In one study, of 27 children with chronic functional constipation who did not respond to 2 months of laxative therapy, 21 (77.7%) were responsive to elimination of cow's milk and dairy products for a 1 month period[22], this is comparable with our results.
We found that CMD has a meaningful effect on making signs and symptoms of constipation, and other factors may have effect on these signs and symptoms like other proteins in other diets, and compliance of patients and their parents during the study. It is not completely agreed that 2 weeks of challenge test is enough for coming back of all signs and symptoms of CMD dependent constipation, and if it was longer, further signs and symptoms might recur.
Furthermore, clinical examination of the children in our study showed a low frequency (5%) of severe anal fissures. Because in some studies[4, 7, 11], these lesions reappeared after the reintroduction of cow's milk and before the onset of constipation, it is hypothesized that these are one of the mechanisms causing constipation. But in our study, we found no cause and effect relationship between anal fissure and constipation.
This study has some limitations. Our pediatric gastroenterology department is a referral center, the pediatricians who referred patients, may have preselected the patients. Also, we could not totally rule out psychological factors, which are frequently suggested as the cause of chronic constipation. In most previous studies, like ours, all the patients had been previously treated unsuccessfully with laxatives; so, the high frequency of cow's milk allergy in constipated children in these studies may have been due in part to their inclusion criteria.
Conclusion
Chronic constipation can be a manifestation of cow's milk allergy in children. At present, although many questions exist that have no answer, but a therapeutic trial with elimination diet is advisable in all children with constipation unresponsive to correct laxative treatment.
Acknowledgment
Local Research Ethics Committee of Shiraz University of Medical Sciences has approved this research.
Conflict of Interest
None
References
- 1.Locke GR, III, Pemberton JH, Phillips SF. American Gastroenterology Association medical position statement: guidelines on constipation. Gastroenterology. 2000;119(6):1761–78. doi: 10.1053/gast.2000.20390. [DOI] [PubMed] [Google Scholar]
- 2.Loening-Baucke V. Constipation in early childhood: patient characteristics, treatment and long-term follow-up. Gut. 1993;34(10):1400–4. doi: 10.1136/gut.34.10.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loening-Baucke V. Controversies in the management of chronic constipation. J Pediatr Gastroenterol Nutr. 2001;32(Suppl 1):S38–9. doi: 10.1097/00005176-200104001-00017. [DOI] [PubMed] [Google Scholar]
- 4.van Ginkel R, Reitsma JB, Buller HA, et al. Childhood constipation: longitudinal follow-up beyond puberty. Gastroenterology. 2003;125(2):357–63. doi: 10.1016/s0016-5085(03)00888-6. [DOI] [PubMed] [Google Scholar]
- 5.Iacono G, Carroccio A, Cavataio F, et al. Chronic constipation as a symptom of cow milk allergy. J Pediatr. 1995;126(1):34–9. doi: 10.1016/s0022-3476(95)70496-5. [DOI] [PubMed] [Google Scholar]
- 6.Iacono G, Cavataio F, Montalto G, et al. Intolerance of cow's milk and chronic constipation in children. N Engl J Med. 1998;339(16):1100–4. doi: 10.1056/NEJM199810153391602. [DOI] [PubMed] [Google Scholar]
- 7.Buisseret PD. Common manifestations of cow's milk allergy in children. Lancet. 1978;1(8059):504–5. doi: 10.1016/s0140-6736(78)90072-7. [DOI] [PubMed] [Google Scholar]
- 8.Chin KC, Tarlow MJ, Allfree AJ. Allergy to cow's milk presenting as a chronic constipation. Br Med J (Clin Res Ed) 1983;287(6405):1593. doi: 10.1136/bmj.287.6405.1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGrath J. Allergy to cow's milk presenting as a chronic constipation. BMJ. 1984;288(6412):236. doi: 10.1136/bmj.288.6412.236-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davidson M, Kugler MM, Baue CH. Diagnosis and management in children with severe and protracted constipation and obstipation. J Pediatr. 1963;62:261–75. doi: 10.1016/s0022-3476(63)80404-7. [DOI] [PubMed] [Google Scholar]
- 11.Shah N, Lindley K, Milla P. Cow's milk and chronic constipation in children. N Engl J Med. 1999;340(11):891–2. [PubMed] [Google Scholar]
- 12.Daher S, Soleé D, de Morais MB. Cow's milk and chronic constipation in children. N Engl J Med. 1999;340(11):891. doi: 10.1056/NEJM199903183401114. [DOI] [PubMed] [Google Scholar]
- 13.Daher S, Tahan S, Solé D, et al. Cow's milk protein intolerance and chronic constipation in children. Pediatr Allergy Immunol. 2001;12(6):339–42. doi: 10.1034/j.1399-3038.2001.0o057.x. [DOI] [PubMed] [Google Scholar]
- 14.Vanderhoof JA, Perry D, Hanner TL, et al. Allergic constipation; association with infantile milk allergy. Clin Pediatr. 2001;40(7):399–402. doi: 10.1177/000992280104000707. [DOI] [PubMed] [Google Scholar]
- 15.Turunen S, Karttunen TJ, Kokkonen J. Lymphoid nodular hyperplasia and cow's milk hypersensitivity in children with chronic constipation. J Pediatr. 2004;145(5):606–11. doi: 10.1016/j.jpeds.2004.06.067. [DOI] [PubMed] [Google Scholar]
- 16.Yimyaem P, Chongsrisawat V, Vivatvakin B, et al. Gastrointestinal manifestations of cow's milk protein allergy during the first year of life. J Med Assoc Thai. 2003;86(2):116–23. [PubMed] [Google Scholar]
- 17.Rasquin A, Di Lorenzo C, Forbes D, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130(5):1527–37. doi: 10.1053/j.gastro.2005.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carroccio A, Montalto G, Custro N, et al. Evidence of very delayed clinical reactions to cow's milk in cow's milk intolerant patients. Allergy. 2000;55(6):574–9. doi: 10.1034/j.1398-9995.2000.00417.x. [DOI] [PubMed] [Google Scholar]
- 19.Kamer B, Dólka E, Pyziak K, et al. Food allergy as a cause of constipation in children in the first three years of life - own observations. Med Wieku Rozwoj. 2011;15(2):157–61. [PubMed] [Google Scholar]
- 20.Syrigou EI, Pitsios C, Panagiotou I, et al. Food allergy-related paediatric constipation: the usefulness of atopy patch test. Eur J Pediatr. 2011;170(9):1173–8. doi: 10.1007/s00431-011-1417-6. [DOI] [PubMed] [Google Scholar]
- 21.Irastorza I, Ibañez B, Delgado-Sanzonetti L, et al. Cow's-milk-free diet as a therapeutic option in childhood chronic constipation. J Pediatr Gastroenterol Nutr. 2010;51(2):171–6. doi: 10.1097/MPG.0b013e3181cd2653. [DOI] [PubMed] [Google Scholar]
- 22.El-Hodhod MA, Younis NT, Zaitoun YA, Daoud SD. Cow's milk allergy related pediatric constipation: appropriate time of milk tolerance. Pediatr Allergy Immunol. 2010;21(2 Pt 2):e407–1. doi: 10.1111/j.1399-3038.2009.00898.x. [DOI] [PubMed] [Google Scholar]