Abstract
Brown adipose tissue (BAT) is known to function in the dissipation of chemical energy in response to cold or excess feeding, and also has the capacity to modulate energy balance. To test the hypothesis that BAT is fundamental to the regulation of glucose homeostasis, we transplanted BAT from male donor mice into the visceral cavity of age- and sex-matched recipient mice. By 8–12 weeks following transplantation, recipient mice had improved glucose tolerance, increased insulin sensitivity, lower body weight, decreased fat mass, and a complete reversal of high-fat diet–induced insulin resistance. Increasing the quantity of BAT transplanted into recipient mice further improved the metabolic effects of transplantation. BAT transplantation increased insulin-stimulated glucose uptake in vivo into endogenous BAT, white adipose tissue (WAT), and heart muscle but, surprisingly, not skeletal muscle. The improved metabolic profile was lost when the BAT used for transplantation was obtained from Il6–knockout mice, demonstrating that BAT-derived IL-6 is required for the profound effects of BAT transplantation on glucose homeostasis and insulin sensitivity. These findings reveal a previously under-appreciated role for BAT in glucose metabolism.
Introduction
The increased prevalence of obesity worldwide has been paralleled by an alarming increase in the rate of type 2 diabetes (1), and this growing epidemic has underscored the need to elucidate the molecular basis for obesity as well as develop novel treatments for this condition. Obesity is characterized by an expansion of adipose tissue mass. However, of the major adipose tissue depots, only brown adipose tissue (BAT) is inversely correlated with BMI in humans (2, 3), and it consumes large amounts of energy for thermogenesis (4). BAT is a highly energetic organ that not only utilizes its unique expression of uncoupling protein 1 (UCP1) for uncoupling of respiration (i.e., cold or diet-induced thermogenesis), but is also a mitochondrially rich tissue that uses glucose and fatty acids as a fuel (5–8). Adult humans have substantial depots of metabolically active BAT (2, 3, 7, 9), suggesting that BAT may play a fundamental role in the maintenance of a leaner and more metabolically healthy phenotype.
These factors have led to the concept that BAT transplantation could be used as a therapeutic tool to combat obesity and metabolic disease (10–14). Nonetheless, these efforts have been hampered by the limited success in developing BAT transplantation models that can be sustained for more than 3–4 weeks (15–17). Consequently, the effects of BAT transplantation on metabolic homeostasis have not been established. In the current study, we examined whether increasing BAT mass by transplantation would improve whole-body and tissue-specific metabolism and, if so, the mechanism for this effect. We found that BAT transplantation, in both chow-fed and high-fat diet–fed mice, significantly decreased body weight and improved glucose metabolism and insulin sensitivity. The mechanism for this effect involves BAT-derived IL-6, as transplantation of BAT from Il6-knockout mice failed to significantly improve glucose homeostasis and insulin sensitivity.
Results
Transplantation of BAT improves glucose tolerance and insulin sensitivity.
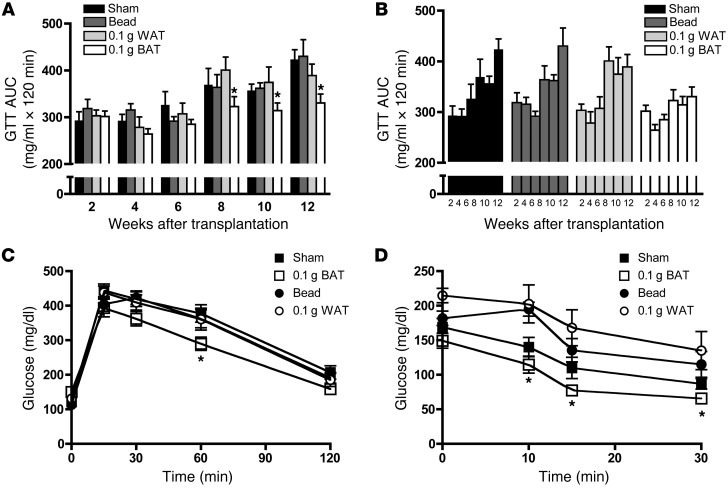
To determine whether increased BAT mass improves metabolic homeostasis, we studied the effects of BAT transplantation on glucose tolerance, insulin sensitivity, and changes in body composition in mice. BAT (0.1 g) from 12-week-old C57BL/6 donor male mice was transplanted into the visceral cavity of age-matched male mice by placing the tissue superior to the epididymal fat pad. There was no initial effect of BAT transplantation on glucose tolerance; however, by 8 weeks after transplantation, there was a significant improvement in glucose tolerance compared with 3 control groups: sham-operated mice, mice transplanted with a 0.15-g glass bead, and mice transplanted with 0.1 g visceral WAT (Figure 1, A–C). The 3 control groups showed a steady decrease in glucose tolerance over time, demonstrating progressive insulin resistance with increasing age (Figure 1B). Strikingly, from 6 weeks after transplantation, there was no decline in glucose tolerance in the mice transplanted with BAT (Figure 1B).
Figure 1. BAT transplantation improves glucose tolerance and increases whole body insulin sensitivity.
(A–C) Mice received transplants of 0.1 g BAT, a 0.15-g glass bead, or 0.1 g WAT or were sham operated. For glucose tolerance tests (GTT), mice were injected with 2 g glucose/kg body weight, i.p. (A and B) Glucose AUC and (C) GTT curve at 12 weeks after transplantation. (D) For ITTs, mice were injected with 1 U insulin/kg i.p. and data expressed as absolute glucose. Data are mean ± SEM. n = 5–8/group. *P < 0.05 between BAT-transplanted mice and all control groups.
To assess whole-body insulin sensitivity, we performed insulin tolerance tests (ITTs) 12 weeks after transplantation of BAT into the visceral cavity. There was a significant increase in insulin sensitivity in mice receiving BAT transplants compared with control groups (Figure 1D). These data demonstrate that transplantation of BAT into the visceral cavity of mice results in a dramatic improvement in whole-body glucose homeostasis and insulin sensitivity.
The improved insulin sensitivity in the mice receiving BAT transplants was associated with a reduction in body weight and fat mass at 12 weeks after transplantation, while total lean mass was unaltered (Supplemental Figure 1, A–C; supplemental material available online with this article; doi: 10.1172/JCI62308DS1). Food intake (Supplemental Figure 1D) was not changed, whereas energy expenditure was significantly increased (Supplemental Figure 1E). There was no effect of BAT transplantation on spontaneous activity or respiratory exchange rate (RER) (Supplemental Figure 1, F and G). Mice that received 0.1 g BAT had an overall increase in carbohydrate and fatty acid oxidation, resulting in no change in RER. Triglyceride concentrations in skeletal muscle and liver, and cardiovascular parameters including heart rate and blood pressure (Supplemental Tables 1 and 2), were also unaffected by BAT transplantation. Thus, the improved glucose homeostasis with BAT transplantation into the visceral cavity is accompanied by decreased body weight and fat mass, and increased energy expenditure.
In contrast to these beneficial effects of BAT transplantation into the visceral cavity, transplantation of BAT into the subcutaneous cavity of mice did not result in changes in glucose tolerance (Supplemental Figure 1H). The lack of effect of BAT transplantation into the subcutaneous cavity was not likely due to a lack of vascularization, since the two transplantation procedures resulted in similar CD31 protein expression (Supplemental Figure 1I). However, BAT transplantation into the visceral cavity resulted in significantly more tyrosine hydroxylase (TH) protein expression (Supplemental Figure 1J), suggesting that lack of innervation with subcutaneous transplantation may account for the ineffectiveness of BAT transplantation on glucose tolerance in this location. To determine whether autonomous transplantation of BAT would improve glucose tolerance, we studied an additional cohort of mice. Interscapular BAT was removed and transplanted into the visceral cavity of the same mice. These mice with autonomous BAT transplantation had a significant improvement in glucose tolerance test compared with sham-operated controls, however, not to the extent of mice transplanted with BAT from donor mice (Supplemental Figure 1K). The mice that underwent autonomous BAT transplantation did not show decreases in body weight (37 ± 5 g in sham vs. 35 ± 3 g in mice receiving autonomous BAT transplantation) or percent fat mass (31% ± 3% in sham vs. 21% ± 10% in mice receiving autonomous BAT transplantation). All subsequent experiments were done using transplantation of BAT into the visceral cavity.
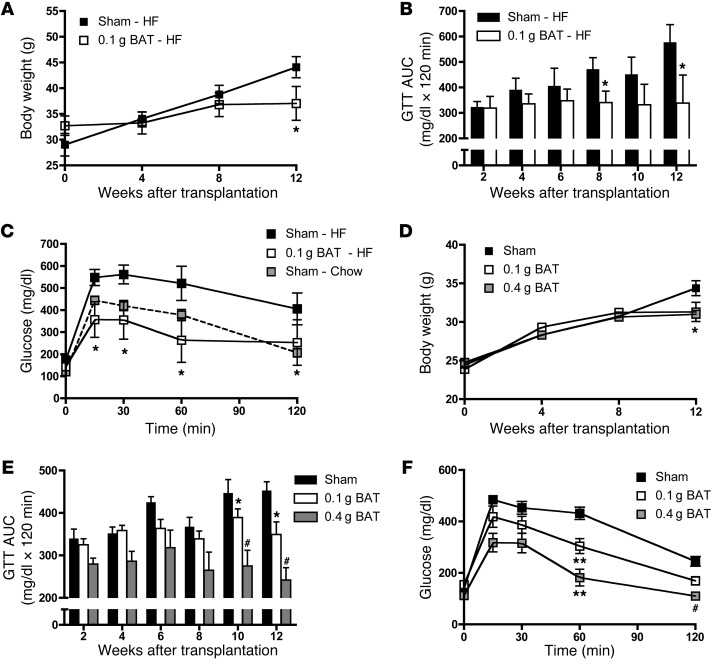
After observing the beneficial effects of BAT transplantation into the visceral cavity in mice on a chow diet, we hypothesized that increasing BAT in mice would ameliorate the well-established effects of high-fat feeding to impair glucose homeostasis. Mice at 6 weeks of age were fed a high-fat diet for 6 weeks, underwent transplantation of 0.1 g BAT from chow-fed donors, and were maintained on the high-fat diet for an additional 12 weeks. High-fat feeding increased body weights, an effect partially attenuated with BAT transplantation (Figure 2A). Remarkably, high-fat feeding did not impair glucose tolerance in mice receiving BAT (Figure 2, B and C).
Figure 2. BAT transplantation ameliorates high-fat diet–induced insulin resistance and has dose-dependent effects on glucose tolerance.
(A–C) Mice were fed a high-fat diet (HF) for 18 weeks, with BAT transplanted after 6 weeks. (A) Body weight, (B) GTT AUC, and (C) GTT curve at 12 weeks after transplantation. Data are mean ± SEM. n = 6/group; *P < 0.05. For comparison, chow-fed, sham-operated mice from a separate cohort of animals are indicated with a dashed line (n = 17). (D–F) Mice received transplants of 0.1 g BAT or 0.4 g BAT or were sham operated. (D) Body weight, (E) GTT AUC, and (F) GTT curve at 12 weeks after transplantation. Data are mean ± SEM. n = 13–14/group; *P < 0.05, **P < 0.01, #P < 0.001 compared with sham.
To determine whether the effects of BAT transplantation on glucose homeostasis were dose dependent, we studied mice maintained on a chow diet following transplantation with 0.1 g or 0.4 g BAT or sham operation. Body weights at 12 weeks after transplantation were similarly decreased in mice receiving 0.1 or 0.4 g BAT (Figure 2D). Mice receiving 0.4 g BAT had a significant improvement in glucose tolerance compared with both sham-operated mice and mice receiving 0.1 g BAT at 12 weeks after transplantation (Figure 2, E and F), demonstrating a dose-dependent effect of BAT transplantation. BAT transplantation also resulted in a more favorable circulating lipid and hormonal profile (Supplemental Table 3), with decreases in plasma insulin, cholesterol, and leptin concentrations and a tendency toward a decrease in free fatty acids, albeit with no difference between mice receiving 0.1 or 0.4 g BAT. Taken together, these data conclusively demonstrate that transplantation of BAT into mice results in a significantly improved metabolic profile.
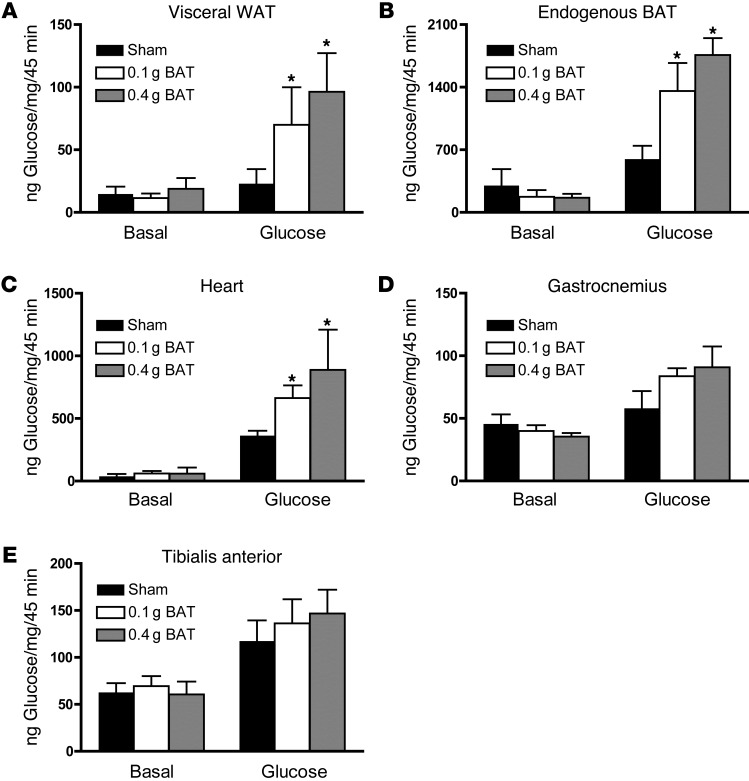
BAT transplantation increases glucose uptake in endogenous BAT and WAT, but not skeletal muscle.
To establish which tissues were responsible for the increased glucose disposal with BAT transplantation, mice were injected with labeled [3H]2-deoxyglucose in combination with saline or a 20% glucose bolus that results in a physiological increase in plasma insulin concentrations (18). Basal rates of glucose uptake in all tissues were not different among groups (Figure 3, A–E), and glucose injection increased glucose uptake in all adipose tissues. Unexpectedly, BAT transplantation resulted in higher rates of glucose uptake in visceral WAT, endogenous BAT, and heart, but not in skeletal muscle. The lack of effect in skeletal muscle is surprising given that under normal physiological conditions, skeletal muscle accounts for approximately 80% of systemic glucose clearance (19); however, it is consistent with a study in rats where increasing endogenous BAT mass by treatment with a β3-specific adrenoceptor agonist increased glucose uptake in epididymal adipose tissue without an increase in skeletal muscle (20). These results provide evidence that the transplanted BAT exerts paracrine and/or endocrine effects to modify other tissues.
Figure 3. BAT transplantation increases glucose uptake into WAT, BAT, and heart.
(A–E) Mice received transplants of 0.1 g BAT or 0.4 g BAT or were sham operated, and were studied 12 weeks after transplantation. Mice were fasted overnight and anesthetized, and [3H]2-deoxyglucose/g body weight was administered via retro-orbital injection in the presence of saline (Basal) or 1 mg/kg body weight glucose (Glucose); glucose uptake was measured in (A) visceral WAT, (B) endogenous BAT, (C) heart, (D) gastrocnemius muscle, (E) tibialis anterior muscle. Data are mean ± SEM. *P < 0.05 compared with sham mice (n = 6/group).
To investigate the mechanism underlying the increase in glucose uptake in WAT, heart, and endogenous BAT, we determined the expression of several key proteins involved in glucose and lipid metabolism (Supplemental Tables 4–7). BAT transplantation did not affect expression or activity of these proteins in endogenous BAT (Supplemental Table 4). In contrast, there was a significant increase in expression of the glucose transporter 1 (GLUT1) protein in WAT (Supplemental Table 5 and Supplemental Figure 2A), a significant increase in adipose tissue basal glycogen content (expressed per milligram WAT weight) (Supplemental Figure 2B), a tendency toward an increase in glycogen per total adipose tissue mass (P = 0.07) (Supplemental Figure 2C), and a marked decrease in WAT cell size (Supplemental Figure 2, D–F). Significant increases in GLUT1 were also observed in the heart of BAT-transplanted mice (Supplemental Table 6). There were no morphological or histological changes observed in the heart (Supplemental Figure 2G).
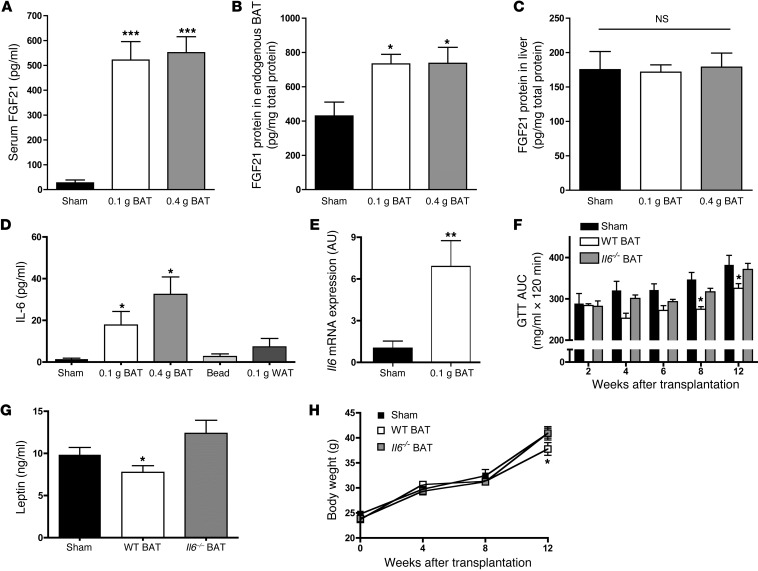
BAT transplantation increases norepinephrine, FGF21, and IL-6 concentrations.
Mice receiving BAT transplants had a significant increase in circulating norepinephrine concentrations (Supplemental Table 3). Norepinephrine can increase BAT-derived FGF21, a protein that has been shown to regulate glucose homeostasis and insulin sensitivity upon thermogenic activation (21, 22). Compared with sham-treated control mice, mice receiving BAT transplants had a 5-fold increase in serum FGF21 concentrations (Figure 4A). Since BAT and liver are major sources of FGF21 (21, 22), we measured FGF21 protein levels in these tissues. There was a 2-fold increase in FGF21 protein concentrations in endogenous BAT (Figure 4B), but no effect of BAT transplantation on FGF21 concentrations in the liver (Figure 4C). Taken together, these data raise the possibility that BAT transplantation leads to adaptations to endogenous BAT that result in an increase in BAT-derived FGF21, which may contribute to the observed metabolic improvements.
Figure 4. BAT transplantation increases circulating IL-6 and FGF21 concentrations, and Il6–/– mice do not show beneficial effects of BAT transplantation.
(A–E) Mice underwent sham operation or transplantation with 0.1 or 0.4 g BAT and were studied 12 weeks after transplantation. (A) Serum FGF21 and (B) FGF21 protein levels in endogenous BAT, (C) FGF21 protein levels in liver, (D) serum IL-6, (E) and Il6 measured by qPCR in endogenous BAT. Data are mean ± SEM. n = 6–17/group; *P < 0.05 compared with sham. **P < 0.01. ***P < 0.001. (F–H) Mice underwent sham operation or transplantation with 0.1 g BAT from Il6–/– or Il6+/+ mice. (F) GTT AUC, (G) serum leptin, and (H) body weight. Data are mean ± SEM. *P < 0.05 compared with sham and mice receiving 0.1 g Il6–/– BAT. n = 4–8/group.
Given the putative paracrine or endocrine effects of the transplanted BAT, another salient characteristic of the transplanted mice was an increase in circulating IL-6 concentrations (Figure 4D). There was also an increase in Il6 mRNA in endogenous BAT from mice receiving 0.1 g BAT compared with endogenous BAT from sham-operated mice (Figure 4E). Although increased circulating IL-6 concentrations can be indicative of an inflammatory response, this is unlikely with the current model of BAT transplantation. First, IL-6 concentrations were not increased in mice receiving transplants of beads or WAT (Figure 4D). Second, TNF-α, another inflammatory cytokine, was not increased with BAT transplantation (Supplemental Table 3). Finally, there was no change in basal temperature in mice receiving transplants of BAT compared with sham-operated mice (Supplemental Figure 4, A and B). Instead of an inflammatory response — given that FGF21 concentrations are increased by BAT transplantation, that norepinephrine treatment of BAT in culture can result in secretion of IL-6 (23, 24), and that mice overexpressing IL-6 have an improved metabolic profile (25) — we hypothesize that IL-6 and FGF21 work together to regulate glucose metabolism.
BAT-derived IL-6 is necessary for improvement in glucose homeostasis.
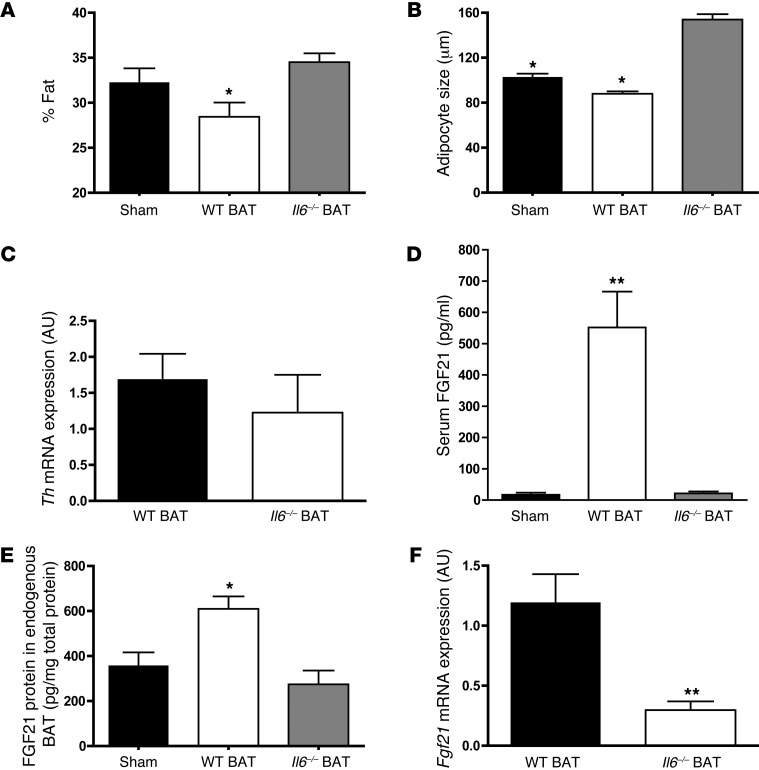
We next tested the novel hypothesis that BAT transplantation results in increased IL-6 concentrations that in turn are responsible for improved glucose homeostasis. For this purpose, BAT (0.1 g) from Il6–/– and Il6+/+ (WT) mice was transplanted into WT animals. Twelve weeks after surgery, mice receiving BAT from WT animals showed the characteristic improvement in glucose tolerance, but this effect was not present in the mice receiving BAT from Il6–/– mice (Figure 4F). Mice receiving BAT from Il6–/– mice failed to show the same increase in circulating IL-6, norepinephrine (Supplemental Table 8), and leptin (Figure 4G) or decrease in body weight (Figure 4H). The decrease in fat mass (Figure 5A) and white adipocyte cell size (Figure 5B) was also not observed in mice receiving transplants of Il6–/– BAT, whereas it was observed in mice receiving WT BAT. Mice receiving Il6–/– BAT did, however, have similar levels of tyrosine hydroxylase mRNA compared with mice receiving WT BAT (Figure 5C), demonstrating that the presence of IL-6 in the innervated BAT, and not the innervation per se, was necessary for the effects of BAT on glucose homeostasis.
Figure 5. Transplantation of Il6–/– BAT does not alter fat mass or adipocyte size of serum FGF21.
(A–F) Mice underwent sham operation or transplantation with 0.1 g BAT from Il6–/– or Il6+/+mice. (A) Percent fat mass, (B) visceral WAT cell size at 12 weeks after transplantation, (C) qPCR of tyrosine hydroxylase in transplanted BAT, (D) serum FGF21, (E) endogenous BAT FGF21 protein, and (F) qPCR of Fgf21. Data are mean ± SEM. *P < 0.05 compared with sham and mice receiving 0.1 g Il6–/– BAT. **P < 0.01. n = 4–8/group.
Another important finding was that transplantation of BAT from Il6–/– mice did not result in a significant increase in serum FGF21 concentrations (Figure 5D) compared with mice receiving WT BAT. In addition, mice receiving BAT from Il6–/– mice did not have an increase in FGF21 protein in their endogenous BAT (Figure 5E). Furthermore, the transplanted BAT from the WT compared with the Il-6–/– mice had significantly higher expression of Fgf21 mRNA (Figure 5F). These data suggest that IL-6 regulates FGF21, which is further supported by data showing that Il6–/– mice have lower liver FGF21 protein levels at room temperature and lower serum FGF21 concentrations in response to 24-hour cold exposure (4°C) (Supplemental Figure 3, A and B).
Transplanted BAT maintains BAT-like characteristics.
The transplanted BAT has some, but not all, characteristics of endogenous BAT. Markers of a brown adipocyte phenotype such as UCP1, PRDM-16, and citrate synthase activity were present in the transplanted BAT, albeit at reduced levels compared with endogenous BAT (Supplemental Table 4). Histological analysis revealed that the BAT transplants had a progressively decreased multilocular appearance over time, and the remaining multilocular cells were surrounded by unilocular cells (Supplemental Figure 4, C and D). These findings are similar to those of previous studies in which transplants of BAT into the kidney capsule of mice (15, 16) or transplants of BAT-engineered myoblastic precursors (26) resulted in multilocular cells surrounded by unilocular cells. We also performed cold-exposure studies to determine whether the transplanted BAT maintained thermogenic properties. Mice receiving BAT did not differ in basal body temperature compared with sham-operated mice, demonstrating that the increase in IL-6 was not eliciting a “fever” response. However, mice receiving BAT had a striking capacity to maintain body temperature when exposed to cold (4°C) (Supplemental Figure 4, A and B), suggesting that the transplanted tissues retained the ability to thermoregulate in response to cold exposure. Tyrosine hydroxylase (Th) mRNA expression was similar in transplanted and endogenous BAT (Supplemental Figure 4E), and immunofluorescence revealed the presence of TH and UCP1 (Supplemental Figure 4, F and G) in the transplanted tissue, further establishing the functionality of the transplanted BAT. Finally, although rates were lower compared with endogenous BAT, the transplanted tissue actively took up glucose upon stimulation (Supplemental Figure 4H), consistent with what has been reported for engineered brown adipocyte transplants (26). The lower rates of glucose uptake in transplanted BAT suggest that the transplanted tissue does not directly contribute to the increased whole-body glucose disposal; rather, the finding further supports the concept that the transplanted BAT functions in an endocrine manner to improve the metabolic profile.
Discussion
The advances in brown adipose cell biology during the last decade have increased our understanding of the cellular origin (27–29), function (8, 13, 29), and adult human tissue distribution (2, 3, 7, 9) of BAT. The current study establishes that increasing BAT has advantageous effects on body composition and insulin sensitivity and suggests that BAT is an endocrine organ that can function to improve whole-body and tissue glucose homeostasis. Mice receiving transplanted BAT showed a significant decrease in body weight and an improvement in insulin sensitivity and glucose metabolism. The transplantation of BAT also ameliorated the harmful effects of a high-fat diet, reducing body weights and improving glucose tolerance in the BAT-transplanted mice beyond that of the sham-operated, chow-fed mice. The improvements in whole-body metabolism can be attributed to both paracrine and endocrine effects of the transplanted BAT on other tissues (specifically visceral WAT, heart, and endogenous BAT). While the transplanted BAT is actively taking up glucose, this effect may be relatively small compared with the larger effects observed in other tissues. These beneficial effects were due solely to the implantation of BAT, as mice transplanted with the same amount of WAT or with a glass bead did not show the same reduction in body weight or improvement in glucose metabolism.
To our knowledge, this is the first study to show improved metabolic parameters in mice receiving BAT transplants. Past studies differed from the current study in terms of location of transplantation, time course of study, and success of transplantation (15–17, 30–32), and none of these previous studies reported the effects of transplantation on whole-body glucose metabolism or insulin sensitivity (15–17, 30–32). The transplants from the current study were successful out to 12 weeks after transplantation, as indicated by the presence of innervation and vascular markers in the transplanted tissue. The tissue was also metabolically active, as it actively took up glucose upon stimulation, and mice receiving this tissue had a significant improvement in cold tolerance. Thus, our results demonstrate that transplantation of BAT to a location where it successfully reestablishes innervation results in an improved metabolic profile in the recipient mouse.
A remarkable finding from the current study was the ability of the BAT transplants to normalize glucose tolerance in the high-fat diet–fed mice. This demonstrates that the BAT transplants originating from the chow-fed donors maintain the characteristics of lean, healthy BAT and do not take on the characteristics of the insulin-resistant, high-fat diet–fed recipient mice. In contrast, in a study of the obese, insulin resistant ob/ob mouse, transplantation of BAT from lean mice into ob/ob mice resulted in the transplanted BAT taking on the characteristics of the ob/ob mouse (18). These data imply that the transplantation of BAT into mice on a high-fat diet ameliorates the effect of the high-fat feeding and results in beneficial effects on glucose metabolism.
Multiple findings from the current study, including the increases in circulating norepinephrine, IL-6, and FGF21, led us to postulate that the metabolic effects of the transplanted BAT originated from a paracrine or endocrine action. Indeed, another important finding of the current study was that transplanted BAT could exert its effect over whole-body metabolism through an IL-6–dependent mechanism, as mice receiving BAT transplants from Il6–/– mice showed no improvement in glucose tolerance and no increase in circulating IL-6. These findings suggest that IL-6 functions as a brown adipokine, or “batokine,” in vivo and is critical for the beneficial effects of BAT transplantation on metabolic homeostasis. Interestingly, the phenotype of the mice transplanted with BAT in the current study is similar to that observed in transgenic mice in which IL-6 was overexpressed (Il6tg). Il6tg mice had decreased fat mass and adipocyte cell size when compared with WT controls, effects that were amplified when these mice were placed on a high-fat diet (25). An additional study showed that an i.c.v. injection of IL-6 resulted in increased energy expenditure, decreased body weight, decreased adiposity, and decreased circulating leptin in rats (33). There has been much contradictory data on the effects of IL-6 on glucose tolerance and obesity, but our data support the concept that an increase in circulating IL-6 increases energy expenditure, reduces adiposity, decreases circulating insulin, and improves glucose tolerance.
Based on the evidence that epinephrine treatment of cultured brown adipocytes in culture media increases IL-6 (23, 24), and the well-established effects of IL-6 in promoting lipolysis in WAT (34, 35), we propose a model whereby BAT-derived IL-6 promotes lipolysis, resulting in the observed reduction in adipocyte size. Another potential mechanism through which IL-6 could promote increased insulin sensitivity and glucose metabolism is an increase in GLUT1 expression, which is observed in the WAT and hearts of mice receiving BAT. The increase in GLUT1 could be stimulated by the increase in IL-6 and/or FGF21, as IL-6 (24, 33, 36–38) and FGF21 (21, 22, 39) have been shown to increase GLUT1 expression in cultured brown adipocytes and 3T3-L1 cells, respectively.
BAT-derived IL-6 may contribute to the increases in circulating FGF21 and BAT FGF21 concentrations that occurred with BAT transplantation. This concept is supported by the findings that there are significant increases in circulating FGF21 and FGF21 protein in BAT from mice receiving transplants of WT BAT, but no such increase was observed in BAT of mice receiving Il6–/– BAT. FGF21-transgenic mice have increased insulin sensitivity, improved glucose tolerance, resistance to diet-induced obesity, and an increase in GLUT1 in peripheral tissues (21, 22), similar to the mice in the current study that were transplanted with BAT. Whether this increase in FGF21 is a direct or indirect result of the increase in IL-6 has yet to be determined, but these finding suggest that in addition to IL-6, IL-6-stimulated FGF21 could contribute to the improved metabolic phenotype of the mice receivingt BATtransplants.
In conclusion, we have demonstrated that transplanted BAT can have beneficial effects on control of body composition and metabolism. These effects appear to be due to circulating IL-6, which is increased in these mice. The increase in IL-6 is linked to an improvement in glucose metabolism and provides another indication that BAT could be targeted for treatment of obesity-related diseases such as insulin resistance, metabolic syndrome, and diabetes. This is the first study to our knowledge to demonstrate that an increase in BAT significantly increases circulating IL-6, suggesting that an increase in BAT-derived IL-6 improves systemic glucose metabolism. This work reveals a previously underappreciated role of BAT in glucose metabolism and underscores the role for BAT to combat obesity-related diseases.
Methods
Mice and fat transplantation.
Twelve-week-old male C57BL/6 mice from Charles River Laboratories were used as recipient mice for transplantation. Tissue for transplantation was obtained from 12-week-old male C57BL/6 mice from Charles River Laboratories or The Jackson Laboratory (Il6–/– mice and C57BL/6 controls). All animals were maintained on a standard 12-hour light/12-hour dark cycle. Mice were maintained on a standard mouse diet (21% kcal from fat) (9F 5020 Lab Diet, PharmaServ Inc.), unless otherwise indicated. A separate cohort of mice was maintained on a high-fat diet (60% kcal from fat) (Research Diets Inc.).
BAT transplantation.
Transplantation was performed using BAT removed from the intrascapular region of 12-week-old male C57BL/6 mice. After euthanasia of donor mice by cervical dislocation, BAT was removed and incubated in 10 ml saline at 37°C for 20–30 minutes. Twelve-week-old C57BL/6 recipient mice were anesthetized by i.p. injection of 85–100 mg/kg body weight pentobarbital. For each recipient mouse, 0.1 or 0.4 g donor BAT, a 0.15-g glass bead, or 0.1 g WAT from the epididymal fat pad (also from 12-week-old C57BL/6 mice) was transplanted into the visceral cavity. The transplant was carefully lodged deep between folds within the endogenous epididymal fat of the recipient (40). Mice that were sham operated underwent the same procedure, but instead of receiving BAT, their epididymal fat pad was located, exposed, and then replaced.
Glucose and ITTs.
For glucose tolerance tests, animals were fasted for 11 hours (22:00–9:00) with free access to drinking water. A baseline blood sample was collected from the tail of fully conscious mice, followed by i.p. injection of glucose (2.0 g/kg body weight), and blood was taken from the tail at 15, 30, 60, 90, and 120 minutes after injection. ITTs were performed at 12 weeks after transplantation. Animals were fasted for 2 hours (12:00–14:00), and baseline blood samples were collected from the tail of fully conscious mice. Insulin (1 U/kg body weight) (Humulin; Eli Lilly) was administered by i.p. injection, and blood samples were taken from the tail at 10, 15, 30, 45, and 60 minutes after injection. Glucose concentrations were determined from blood using a OneTouch Ultra portable glucometer (LifeScan).
Glucose uptake in vivo.
Glucose uptake in vivo was measured as previously described (19). Briefly, mice were fasted overnight (22:00– 9:00) and then anesthetized with sodium pentobarbital (85–100 mg/kg mouse body weight, i.p. injection). After 30 minutes, blood was taken from the tail to assess basal glucose concentrations and background radioactivity levels. Mice were injected with either saline or 1 mg glucose in combination with 0.33 μCi [3H]2-deoxyglucose/g mouse body weight administered via the retro-orbital sinus, and blood samples were taken 5, 10, 15, 25, 35, and 45 minutes later for the determination of glucose and [3H] levels. After the last blood draw, animals were sacrificed by cervical dislocation, and endogenous and transplanted BAT, visceral WAT, heart, liver, tibialis anterior, and gastrocnemius were harvested and immediately frozen in liquid nitrogen. Accumulation of [3H]2-deoxyglucose was assessed in tissues using a perchloric acid/Ba(OH)2/ZnSO4 precipitation procedure modified from previous work (41).
Biochemical and physiological methods.
Adipose tissue was removed from recipient mice and prepared in paraffin after fixation in 10% phosphate-buffered formalin, and then hematoxylin and eosin stains were performed. To measure the size of the adipocytes, we analyzed at least 300 cells per sample using NIH ImageJ software ( http://rsb.info.nih.gov/ij/). Fat and lean mass were measured by dual-energy X-ray absorptiometry (DEXA) scanning with a Lunar PIXImus2 mouse densitometer. The Comprehensive Lab Animal Monitoring System (CLAMS) (Oxymax OPTO-M3 system, Columbus Instruments) was used to measure activity level, food and water intake, volume of O2 consumption, volume of CO2 production, and heat production 12 weeks after transplantation or sham operation. Total energy expenditure of mice was calculated as described previously (42). Retro-orbital sinus bleeds were performed after an overnight fast (22:00–9:00), and plasma levels of hormones and metabolites were assessed. Plasma insulin, leptin, triglyceride, cholesterol, total adiponectin, free fatty acid, IL-6, TNF-α, and FGF21 were measured with mouse ELISA kits (Crystal Chem Inc., Alpco Diagnostics, and BioVendor R&D).
To determine the effects of cold exposure on body temperature, mice were fasted overnight, and body temperature was determined using an animal rectal probe thermometer (Physitemp). Basal temperature was determined, and then animals were then placed at 4°C, and body temperature was measured at 15, 30, 60, 90, and 120 minutes.
Tissue processing and immunoblotting were performed as previously described (43, 44). Antibodies used were GLUT1 (AB1340) and GLUT4 (AB1346) (Millipore), UCP1 (sc-6528), and FATP1 (sc-25541, Santa Cruz Biotechnology Inc.), PRDM16 (NB100-1088, Novus), CD36 (ABM-5525, Cascade Biosciences), ACC (07-439, Upstate), COXIV (no. 4844), STAT3 (no. 9132), p-STAT3 (no. 9131) (Cell Signaling Technology), and CD31 (no. 28364) (Abcam). Citrate synthase activity was determined in adipose tissue lysates as previously described (45) and was calculated as nanomoles per minute per milligram of protein.
Immunofluorescence.
For immunofluorescence, UCP1 (1:50; AnaSpec) and tyrosine hydroxylase (1:100; Millipore) antibodies were used. Sections were analyzed by confocal microscopy on a Zeiss LSM-410 Inverted Laser Scanning Microscope.
Statistics.
The data are presented as mean ± SEM. Statistical significance was defined as P < 0.05 and determined by 2-tailed Student t tests or ANOVA, with Tukey and Bonferroni post hoc analysis. The number of animals used for each experiment is indicated in the figure legends.
Study approval.
All experiments were performed in accordance with a protocol approved by the Institutional Animal Care and Use Committee of the Joslin Diabetes Center and the NIH guidelines for the care and use of laboratory animals.
Supplementary Material
Acknowledgments
The authors thank Margarette Adelman, Allen Clermont, Alevtina Pinkhasov, and Geetha Sankaranarayan of the Joslin Diabetes Center DERC Physiology, Histology, and Complex Assay cores for technical assistance; Julie A. Ripley for editorial contributions; and Aaron Cypess and Hans Lauritzen for critical discussions. This work was supported by NIH grants R01-DK068626 and R01-AR45670 (to L.J. Goodyear), F32-DK091048-01 and T32 DK07260-33 (to K.I. Stanford), and 5P30 DK36836 (Joslin Diabetes Center DERC). R.J.W. Middelbeek was supported by a mentor-based fellowship awarded to L.J. Goodyear from the American Diabetes Association.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2013;123(1):215–223. doi:10.1172/JCI62308.
References
- 1. International Association for the Study of Obesity. International Obesity Task Force. IASO web site http://www.iotf.org/ . Accessed October 30, 2012.
- 2.Saito M, et al. High incidence of metabolically active brown adipose tissue in healthy adult humans: effects of cold exposure and adiposity. Diabetes. . 2009;58(7):1526–1531. doi: 10.2337/db09-0530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cypess AM, et al. Identification and importance of brown adipose tissue in adult humans. N Engl J Med. 2009;360(15):1509–1517. doi: 10.1056/NEJMoa0810780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lowell BB, Spiegelman BM. Towards a molecular understanding of adaptive thermogenesis. Nature. 2000;404(6778):652–660. doi: 10.1038/35007527. [DOI] [PubMed] [Google Scholar]
- 5.Rothwell NJ, Stock MJ. Effects of age on diet-induced thermogenesis and brown adipose tissue metabolism in the rat. Int J Obes. 1983;7(6):583–589. [PubMed] [Google Scholar]
- 6.Gesta S, Tseng YH, Kahn CR. Developmental origin of fat: tracking obesity to its source. Cell. 2007;131(2):242–256. doi: 10.1016/j.cell.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 7.van Marken Lichtenbelt WD, et al. Cold-activated brown adipose tissue in healthy men. N Engl J Med. 2009;360(15):1500–1508. doi: 10.1056/NEJMoa0808718. [DOI] [PubMed] [Google Scholar]
- 8.Bartelt A, et al. Brown adipose tissue activity controls triglyceride clearance. Nat Med. 2011;17(2):200–205. doi: 10.1038/nm.2297. [DOI] [PubMed] [Google Scholar]
- 9.Virtanen KA, et al. Functional brown adipose tissue in healthy adults. N Engl J Med. 2009;360(15):1518–1525. doi: 10.1056/NEJMoa0808949. [DOI] [PubMed] [Google Scholar]
- 10.Dulloo AG, Miller DS. Thermogenic drugs for the treatment of obesity: sympathetic stimulants in animal models. Br J Nutr. 1984;52(2):179–196. doi: 10.1079/BJN19840087. [DOI] [PubMed] [Google Scholar]
- 11.Lowell BB, et al. Development of obesity in transgenic mice after genetic ablation of brown adipose tissue. Nature. 1993;366(6457):740–742. doi: 10.1038/366740a0. [DOI] [PubMed] [Google Scholar]
- 12.Guerra C, Koza RA, Yamashita H, Walsh K, Kozak LP. Emergence of brown adipocytes in white fat in mice is under genetic control. Effects on body weight and adiposity. J Clin Invest. 1998;102(2):412–420. doi: 10.1172/JCI3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tseng YH, Cypess AM, Kahn CR. Cellular bioenergetics as a target for obesity therapy. Nat Rev Drug Discov. 2010;9(6):465–482. doi: 10.1038/nrd3138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whittle AJ, López M, Vidal-Puig A. Using brown adipose tissue to treat obesity — the central issue. Trends Mol Med. 2011;17(8):405–411. doi: 10.1016/j.molmed.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 15.Ferren L. Morphological differentiation of implanted brown and white fats. Trans Kans Acad Sci. 1966;69(1):350–353. [PubMed] [Google Scholar]
- 16.Ashwell M, Wells C, Dunnett SB. Brown adipose tissue: contributions of nature and nurture to the obesity of an obese mutant mouse (ob/ob). Int J Obes. 1986;10(5):355–373. [PubMed] [Google Scholar]
- 17.Nechad M, Olson L. Development of interscapular brown adipose tissue in the hamster. II — Differentiation of transplants in the anterior chamber of the eye: role of the sympathetic innervation. Biol Cell. 1983;48(2–3):167–174. doi: 10.1111/j.1768-322X.1984.tb00211.x. [DOI] [PubMed] [Google Scholar]
- 18.Ho RC, Alcazar O, Fujii N, Hirshman MF, Goodyear LJ. p38gamma MAPK regulation of glucose transporter expression and glucose uptake in L6 myotubes and mouse skeletal muscle. Am J Physiol Regul Integr Comp Physiol. 2004;286(2):R342–R349. doi: 10.1152/ajpregu.00563.2003. [DOI] [PubMed] [Google Scholar]
- 19.Bonadonna RC, et al. Transmembrane glucose transport in skeletal muscle of patients with non-insulin dependent diabetes. J Clin Invest. 1993;92(1):486–494. doi: 10.1172/JCI116592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Souza CJ, Hirshman MF, Horton ES. CL-316,243, a beta3-specific adrenoceptor agonist enhances insulin-stimulated glucose disposal in nonobese rats. Diabetes. 1997;46(8):1257–1263. doi: 10.2337/diabetes.46.8.1257. [DOI] [PubMed] [Google Scholar]
- 21.Kharitonenkov A, et al. FGF21 as a novel metabolic regulator. J Clin Invest. 2005;115(6):1627–1635. doi: 10.1172/JCI23606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hondares E, et al. Thermogenic activation induces FGF21 expression and release in brown adipose tissue. J Biol Chem. 2011;286(15):12983–12990. doi: 10.1074/jbc.M110.215889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cannon B, Houstek J, Nedergaard J. Brown adipose tissue. More than an effector of thermogenesis? Ann N Y Acad Sci. 1998;856:171–187. doi: 10.1111/j.1749-6632.1998.tb08325.x. [DOI] [PubMed] [Google Scholar]
- 24.Burýsek L, Houstek J. β-Adrenergic stimulation of interleukin-1α and interleukin-6 expression in mouse brown adipocytes. FEBS Lett. 1997;411(1):83–86. doi: 10.1016/S0014-5793(97)00671-6. [DOI] [PubMed] [Google Scholar]
- 25.Sadagurski M, Norquay L, Farhang J, D’Aquino K, Copps K, White MF. Human IL6 enhances leptin action in mice. Diabetologia. 2010;53(3):525–535. doi: 10.1007/s00125-009-1580-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kajimura S, et al. Initiation of myoblast/brown fat switch through a PRDM16-C/EBP-β transcriptional complex. Nature. 2009;460(7259):1154–1158. doi: 10.1038/nature08262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farmer SR. Transcriptional control of adipocyte formation. Cell Metab. 2006;4(4):263–273. doi: 10.1016/j.cmet.2006.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seale P, et al. Transcriptional control of brown fat determination by PRDM16. Cell Metab. 2007;6(1):38–54. doi: 10.1016/j.cmet.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tseng YH, et al. New role of bone morphogenetic protein 7 in brown adipogenesis and energy expenditure. Nature. 2008;454(7207):1000–1004. doi: 10.1038/nature07221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roberts JL, Ashwell M, Enser M. Brown adipose tissue triacylglycerol fatty acids of obese and lean mice: in situ and in transplants. Lipids. 1986;21(3):195–201. doi: 10.1007/BF02534821. [DOI] [PubMed] [Google Scholar]
- 31.Dellagiacoma G, et al. Brown adipose tissue: magnetic resonance imaging and ultrastructural studies after transplantation in syngeneic rats. Transplant Proc. 1992;24(6):2986. [PubMed] [Google Scholar]
- 32.Smahel J. Experimental implantation of adipose tissue fragments. Br J Plast Surg. 1989;42(2):207–211. doi: 10.1016/0007-1226(89)90205-1. [DOI] [PubMed] [Google Scholar]
- 33.Li G, Klein RL, Matheny M, King MA, Meyer EM, Scarpace PJ. Induction of uncoupling protein 1 by central interleukin-6 gene delivery is dependent on sympathetic innervation of brown adipose tissue and underlies one mechanism of body weight reduction in rats. Neuroscience. 2002;115(3):879–889. doi: 10.1016/S0306-4522(02)00447-5. [DOI] [PubMed] [Google Scholar]
- 34.Pedersen BK, et al. The metabolic role of IL-6 produced during exercise: is IL-6 an exercise factor? Proc Nutr Soc. 2004;63(2):263–267. doi: 10.1079/PNS2004338. [DOI] [PubMed] [Google Scholar]
- 35.Hoene M, Weigert C. The role of interleukin-6 in insulin resistance, body fat distribution, and energy balance. Obes Rev. 2008;9(1):20–29. doi: 10.1111/j.1467-789X.2007.00410.x. [DOI] [PubMed] [Google Scholar]
- 36.Shimizu Y, Kielar D, Minokoshi Y, Shimazu T. Noradrenaline increases glucose transport into brown adipocytes in culture by a mechanism different from that of insulin. Biochem J. 1996;314(pt 2):485–490. doi: 10.1042/bj3140485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wernstadt I, et al. Reduced stress- and cold-induced increase in energy expenditure in interleukin-6-deficient mice. Am J Physiol Regul Integr Comp Physiol. 2006;291(3):R551–R557. doi: 10.1152/ajpregu.00514.2005. [DOI] [PubMed] [Google Scholar]
- 38.Wallenius V, et al. Interleukin-6-deficient mice develop mature-onset obesity. Nat Med. 2002;8(1):75–79. doi: 10.1038/nm0102-75. [DOI] [PubMed] [Google Scholar]
- 39.Ge X, Chen C, Hui X, Wang Y, Lam KS, Xu A. Fibroblast growth factor 21 induces glucose transporter-1 expression through activation of the serum response factor/Ets-like protein-1 in adipocytes. J Biol Chem. 2011;286(40):34533–34541. doi: 10.1074/jbc.M111.248591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tran TT, Yamamoto Y, Gesta S, Kahn CR. Beneficial effects of subcutaneous fat transplantation on metabolism. Cell Metab. 2008;7(5):410–420. doi: 10.1016/j.cmet.2008.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferré P, Leturque A, Burnol AF, Penicaud L, Girard J. A method to quantify glucose utilization in vivo in skeletal muscle and white adipose tissue of the anaesthetized rat. Biochem J. 1985;228(1):103–110. doi: 10.1042/bj2280103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Albarado DC, et al. Impaired coordination of nutrient intake and substrate oxidation in melanocortin-4 receptor knockout mice. Endocrinology. 2004;145(1):243–252. doi: 10.1210/en.2003-0452. [DOI] [PubMed] [Google Scholar]
- 43.Bradford MM. A rapid and sensitive method for quantitation of microgram quantifites of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 44.Towbin H, Staehelin T, Gordon J. Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheets: procedure and some applications. Proc Natl Acad Sci U S A. 1979;76(9):4350–4354. doi: 10.1073/pnas.76.9.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Srere PA. Citrate synthase. Methods Enzymol. 1969;13:3–11. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.