Abstract
Psychosocial stress has been shown to be a contributing factor in the development of atherosclerosis. Although the underlying mechanisms have not been elucidated entirely, it has been shown previously that the transcription factor nuclear factor-κB (NF-κB) is an important component of stress-activated signaling pathway. In this study, we aimed to decipher the mechanisms of stress-induced NF-κB-mediated gene expression, using an in vitro and in vivo model of psychosocial stress. Induction of stress led to NF-κB-dependent expression of proinflammatory (tissue factor, intracellular adhesive molecule 1 [ICAM-1]) and protective genes (manganese superoxide dismutase [MnSOD]) via p50, p65 or cRel. Selective inhibition of the different subunits and the respective kinases showed that inhibition of cRel leads to the reduction of atherosclerotic lesions in apolipoprotein−/− (ApoE−/−) mice via suppression of proinflammatory gene expression. This observation may therefore provide a possible explanation for ineffectiveness of antioxidant therapies and suggests that selective targeting of cRel activation may provide a novel approach for the treatment of stress-related inflammatory vascular disease.
INTRODUCTION
Atherosclerosis, despite intensive research efforts, remains a major health burden in the postmodern Western society. The treatment and/or prevention of atherosclerotic lesions have focused on well-established risk factors such as lipids, blood pressure or diabetes. Psychosocial stress has been shown to be an independent risk factor for cardiovascular disease (1) amendable by intervention (2), but the underlying mechanisms which lead to atherosclerosis remain unclear. Activation of the redox-sensitive transcriptional factor nuclear factor-κB (NF-κB) is believed to be an important component of the cascade of events triggered by psychosocial stress, leading to inflammation, thrombosis and vascular damage (3–11). NF-κB subunits are expressed ubiquitously and can be activated by a wide range of stimuli, such as reactive oxygen species (ROS), cytokines, infection and DNA damage; however, their actions are regulated in a cell- and stimulus-specific manner, leading to a diverse spectrum of effects (12).
As most inducers of NF-κB trigger the release of ROS (10,13,14), antioxidants have been studied as a therapeutic option for reducing atherothrombosis (13–15). While there is experimental and clinical evidence suggesting a role for redox-mediated cellular dysfunction in atherosclerosis, there is still a large discrepancy between the expected effect of reducing cellular redox responses and the clinical benefit of currently available therapies (16–19). A potential explanation for this discrepancy might be provided by the observation that members of the NF-κB family also orchestrate gene clusters required for the resolution of inflammation (20–23), for instance, inhibition of NF-κB activation by a macrophage-restricted deletion of inhibitor of κB (IκB)-kinase-2 (IKK-2) increases atherosclerosis in mice (24).
A study (12), which investigated the gene network controlled by the canonical NF-κB pathway, revealed that this pathway regulates expression of noncontiguous, functionally discrete groups of genes (regulons), whose temporal expression occurs in waves. Moreover, its mode of activation (oscillatory or monophasic) plays an important role in determining the spectrum of target genes (12). Consistent with this are the findings that there is a biphasic clustered pattern of NF-κB subunit expression, characterized by the nuclear translocation of the NF-κB subunit cRel at early time points and later formation of NF-κB p50/p65-heterodimers and NF-κB p50/p50-homodimers during resolution (25). Inhibition of the latter at later time points therefore results in sustained, rather than self-limited inflammation (22). A shift in NF-κB subunit composition might therefore have a profound effect on the balance of pro- and antiatherogenic gene expression, particularly as specific combinations of NF-κB subunits can distinguish between variant κB sites in different promoters (26–30).
Psychosocial stress and catecholamine-mediated vascular dysfunction are important contributors to vascular disease (31–36). In our previous work, we have demonstrated that psychosocial stress triggers the activation of NF-κB (32). In the present study, our goal was to further characterize the involvement of different NF-κB subunits in the stress-dependent signaling and to analyze their respective effects, not only on the expression of proinflammatory and proatherogenic genes, but also on cell-protective genes. Therefore, catecholamine-induced NF-κB activation and subsequent gene expression were studied in vitro and in vivo in a mouse model of stress-induced atherosclerosis.
MATERIALS AND METHODS
Reagents
Norepinephrine, phentolamine, propranolol, GF109203, wortmannin, SB202190, pyrolidinedithiocarbamate (pDTC), acetylcysteine (AcCys), α-tocopherol, ascorbic acid, human tumor necrosis factor-α (TNF-α), lipopolysaccharide, oil red O, Alcian blue, scarlet fuchsin, hematoxylin, phosphotungstic acid, orcein and Spanish saffron were from Sigma (Deisenhofen, Germany). Oxidized low density lipoprotein was from Biomedical Technologies Inc. (Stoughton, MA, USA). [γ-32P]ATP (3000 Ci/mmol at 10 Ci/mL), ECL-nitrocellulose membranes, ECL detection reagents and Hyperfilm-X-ray-films were from Amersham (Braun-schweig, Germany). NuPageBis-Tris gels were Invitrogen products (Life Technologies, Carlsbad, CA, USA). Poly dI/dC was from Pharmacia (Freiburg, Germany). Peroxidase (POD) staining reagent, ABC-peroxidase staining kit, 3,3′-diaminobenzidine (DAB) and hematoxylin were from Vector Laboratories (Burlinghame, CA, USA).
Animal Experiments
Procedures in this study were approved by the Animal Care and Use Committee at the Regierungspräsidium Karlsruhe, Germany. ApoE−/− mice, 8-wk old, (Charles River Laboratories, Wilmington, MA, USA) were used throughout the study. The animals were bred in the Central Animal Facility of Heidelberg University. They were exposed to 12-h light-dark (L:D) cycles (6:18 h L:D) and had ad libitum access to food and water.
Induction of Acute and Chronic Restraint Stress
ApoE−/− mice (8-wk old; female) were used throughout the experiments. All experiments were started at the same time of day, and mice were separated in single cages 24 h prior to the experiments. For the induction of acute stress, mice were subjected to a 20-min immobilization by being placed in a well-ventilated tube without the possibility to move. The immobilization was repeated once after 4 h of relaxation. Retro-orbital blood samples were taken before euthanization. Mice were then divided into groups and either left untreated or subjected to continued immobilization in the absence or presence of either a combination of α- and β-adrenergic receptor antagonists (phentolamine, 2 mg/kg + propranolol, 0.8 mg/kg) or one of the following inhibitors: protein kinase C (PKC) inhibitor GF109203 × (2 μg/kg), p38 mitogen-activated protein kinase (p38MAPK) inhibitor SB202190 (5 mg/kg), PI3/Akt inhibitor wortmannin (1.5 mg/kg), small interfering ribonucleic acid (siRNA) for p50, p65 and cRel (1.5 μg/g), respectively. Adrenergic antagonists and inhibitors were given intraperitoneally (IP), 12 h prior to the first restraint and the untreated mice received the equal volume of phosphate-buffered saline (PBS).
For the induction of chronic stress, mice were exposed to repeated episodes of immobilization (as described above), twice per week during a 4-wk treatment period. Mice were separated in single cages 24 h before the experiments. Inhibitors were given IP and siRNAs were given intravenously (IV) 12 h prior to the first immobilization of the day.
The scheme of all experimental procedures is depicted in Supplementary Figure S1. Norepinephrine (NE) plasma levels were determined using the Catcombi Elisa Kit (IBL, Hamburg, Germany) according to the manufacturer’s instructions.
Bone Marrow Transplantation
Bone marrow was obtained aseptically from femurs and tibias of male Apo E−/−, C57Bl/6-wild-type and cRel−/− mice (on the C57Bl/6 background) (37), 10 to 12 wks old, after euthanizing animals by cervical dislocation as described previously in detail (38). Unfractionated bone marrow (BM) cells were resuspended in sterile PBS (5 × 106 cells/0.2 mL) and injected retro-orbitally into 6- to 8-wk old Apo E−/− mice that had been lethally irradiated (10 Gy) 1 d before. Six weeks after BM reconstitution, animals were divided into the respective groups and either left untreated or subjected to the repeated episodes of the immobilization stress during 4 wks as described above. The efficiency of engraftment was confirmed by reverse transcriptase–PCR (RT-PCR) for NF-κB cRel in peripheral blood mononuclear cells (pBMC). Twenty three percent of animals subjected to the transplantation died within 2 wks after the procedure.
Cell Culture
THP-1 cells (cell culture collection, DKFZ, Heidelberg, Germany) were maintained in RPMI 1640 medium containing 2 mmol l-glutamine and 100 U/mL penicillin, 100 μg/mL streptomycin (BioWhittaker, Walkerville, MD, USA) and 20% fetal calf serum (Gibco; Life Technologies) at 37°C and seeded 1 d before experiments.
Isolation of Murine pBMC
Whole blood from five mice/group was pooled and pBMC were isolated as described previously (39).
Western Blot Analysis
Cells were harvested and nuclear protein extracts were obtained as described previously (4,40). Membranes were incubated with anti-NF-κB p50 (Epitomics, Burlingame, CA, USA), anti-NF-κB p65 and anti-NF-κB cRel (Rockland Im-munochemicals, Gilbertsville, PA, USA) antibodies (1:500 dilution). Thereafter, the membranes were stripped and incubated with Histone-1 antibody (Santa Cruz, Heidelberg, Germany), which served as a loading control (1:300 dilution).
Electrophoretic Mobility Shift Assay (EMSA)
Nuclear proteins were prepared and assayed for transcription factor binding activity using oligonucleotides specific for the NF-κB binding sites in the tissue factor (TF) and ICAM-1-promoters and the intronic NF-κB binding site in the MnSOD gene (see Supplementary Table S1) as described (4,40,41).
Chromatin Immunoprecipitation (ChIP)
Total chromatin (TCh) was isolated as described in detail (42), including sonication (5 × 7 s; Bandelin Sonoplus, Berlin, Germany) and immunoprecipitation with antibodies to NF-κB p50 (Epitomics), NF-κB p65 (Rockland Immunochemicals, Gilbertsville, PA, USA), NF-κB cRel (Rockland Immunochemicals and Santa Cruz) or an anti-rabbit immunoglobulin G (IgG) serving as negative control (Cell Signaling Technology Inc., Beverly, MA, USA). ICAM-1- and TF-promoter fragment or the fragment of the intronic NF-κB binding site in the MnSOD gene was amplified by PCR (primer sequences in Supplementary Table S1) using the following conditions: 94°C 120 s, 30 × (94°C 20 s, 54°C 45 s, 72°C 30 s), 72°C 120 s for THP-1 cells or 94°C 120 s, 34 × (94°C 20 s, 57°C 45 s, 72°C 15 s), 72°C 120 s for murine pBMC. PCR products were visualized on 1.7% agarose gels.
RT-PCR
RT-PCR was performed using 1 μg total RNA as starting material. Primers shown in Supplementary Table S2 and the following conditions were used for human (THP-1) and murine (pBMC) samples: human ICAM-1: 94°C 120 s, 30 × (94°C 60 s, 54°C 45 s, 72°C 30 s), 72°C 120 s; murine ICAM-1: 94°C 120 s, 28 × (94°C 20 s, 56°C 45 s, 72°C 15 s), 72°C 120 s; human and murine TF: 94°C 120 s, 32 × (94°C 20 s, 56°C 60 s, 72°C 30 s), 72 C° 120 s; human MnSOD: 95°C 90 s, 30 × (95°C 30 s, 55°C 30 s, 72°C 30 s), 72°C 120 s: murine MnSOD: 94°C 120 s, 27 × (94°C 20 s, 55°C 45 s, 72°C 20 s), 72°C 120 s; murine NF-κB p50: 94°C 120 s, 32 × (94°C 20 s, 55°C 45 s, 72°C 30 s), 72°C 120 s; murine NF-κB p65: 94°C 180 s, 33 × (94°C 30 s, 60°C 30 s, 72°C 30 s), 72°C 360 s; murine NF-κB cRel: 94°C 120 s, 28 × (94°C 20 s, 60°C 45 s, 72°C 20 s), 72°C 120 s and murine PI3K: 94°C 120 s, 32 × (94°C 20 s, 56°C 30 s, 72°C 15 s), 72°C 120 s. The signal was normalized using the housekeeping gene β-actin for both, human and murine samples with the following conditions: 94°C 300 s, (94°C 60 s, 55°C 180 s, 72°C 90 s), 2 × (94°C 45 s, 60°C 45 s, 72°C 90 s), 25 × (94°C 45 s, 65°C 45 s, 72°C 90 s), 72°C 360 s. The PCR-products were separated onto 1.7% agarose gels and visualized by ethidium bromide staining. β-actin served as control for sample loading. Reactions lacking template RNA or AMV-reverse transcriptase served as internal controls.
Antisense Experiments
Phosphothioate oligonucleotide (PTO)-modified antisense oligonucleotides (asODNs) for silencing NF-κB subunits spanned bp 468 to bp 492 for NF-κB p50 (acc. no. NM_003998), bp 73–bp 97 for NF-κB p65 (NM_021975) and bp 225–bp 249 for NF-κB cRel (NM_002908) (Supplementary Table S3). Scrambled oligonucleotides were designed as controls. THP-1 cells were preincubated with 0.2 μmol/L asODNs for 48 h prior to induction and were renewed every 24 h. The efficiency of silencing was confirmed by RT-PCR.
RT2 Profiler PCR Arrays
THP-1 cells were preincubated with 0.2 μmol/L as ODNs for NF-κBp 50 and NF-κB cRel for 48 h and/or either induced with NE for 1 h or left untreated. After RNA isolation and complementary deoxyribinocleic acid (cDNA) synthesis, predesigned PCR microarrays for oxidative stress and antioxidant defense; NF-κB pathway and atherosclerosis pathway (SABioscience, Frederick, MD, USA) were performed according to the manufacturer instructions. Quantitative real-time PCR was performed with 500 ng RNA using Chromo 4 Real-time Detector (Bio-Rad, Munich, Germany) and the acquired data were analyzed using the manufacturer’s analyzing template.
Immunohistochemistry
Aortae were cleaned from surrounding tissue and cut transversally with a cryostat (Microm, Walldorf, Germany). Sections (8 μm) were air dried and incubated with antibodies for activated NF-κB p65 (1 μg/mL Chemicon, Temecula, CA, USA), NF-κB p50 (1 μg/mL; Epitomics), NF-κB cRel (1 μg/mL; Santa Cruz), ICAM-1 (1 μg/mL; R&D Systems, Minneapolis, MN, USA), MnSOD (1 μg/mL; Biozol, Eching, Germany) or nitrotyrosine (1.5 μg/mL, Upstate, Lake Placid, NY, USA). Sections were fixed with 2% paraformaldehyde for 15 min at room temperature, stained using the POD reaction with ABC peroxidase and DAB staining kits, and counterstained with hematoxylin. For the immunostaining for TF, 5-μm-thick paraffin-embedded sections were stained using the antibody for TF (2 μg/mL; Calbiochem, Darmstadt, Germany), ABC peroxidase and DAB staining kits, and hematoxylin as counterstain. Immunofluorescence was performed on frozen sections using antibodies for murine CD11b (2 μg/mL; Acris, Herford, Germany), ICAM-1 (1 μg/mL; R&D Systems, Minneapolis, MN, USA), TF (2 μg/mL; Calbiochem) MnSOD (1 μg/mL; Biozol), CD14 (2 μg/mL; Abcam, Cambridge, UK), FITC-labeled CD3 (2.5 μg/mL Santa Cruz), CD45 receptor (1.5 μg/mL; Santa Cruz), α-smooth muscle cell actin (1 μg/mL; Abcam), thrombomodulin (10 μg/mL, R&D Systems, Wiesbaden, Germany), FITC-labeled anti-rat (1 μg/mL; Acris) and anti-rabbit (1 μg/mL; Santa Cruz), Texas-Red labeled anti-rabbit, anti-goat, anti-rat and anti-mouse IgG (1 μg/mL; Santa Cruz). All slides were visualized with Olympus AX70 microscope and visualizing software Cell F (Olympus, Hamburg, Germany).
Staining of Aortic Tissue with Oil Red O
Mice were anesthetized with 2-methyl-2-buthanol-tert-amylalcohol and 2,2,2-tribromethanol (Sigma) before intracardiac perfusion was performed with 15 mL PBS followed by 15 mL of 78% methanol (43,44). Aortae were separated from surrounding tissue, extracted, fixated and stained as described previously (43–45). Pictures were taken with a Motic 1000 Digital Camera (Special Application Products Ltd, Ipswich, UK). The stained area was quantified using ImageJ software (NIH, Bethesda, MD, USA; http://rsb.info.nih.gov/ij/index.html) Where indicated, 8 μm sections were air dried and incubated with 0.5% oil red O dissolved in 60% isopropanol for 30 min. Sections were visualized using Olympus AX70 microscope and the pictures were inverted into the dark background using visualizing software Cell F (Olympus, Hamburg, Germany).
Movat Staining
Frozen sections (8 μm) of aortic tissue were stained with Movat pentachrome stain (44,46). Sections were photo -graphed and analyzed with Image Pro software (Media Cybernetics, Bethesda, MD, USA) and the extent of the necrotic cores, extracellular matrix and thickness of the fibrous caps was quantified.
Statistical Analysis
All values are given as mean ± standard deviation. Statistical analysis was performed using SPSS software, version 11.0. Groups were compared using the one-factor analysis of variance (ANOVA) for multiple comparisons and analyzed using post hoc Games-Howell test for unequal variances or Fisher least significant differences (LSD) test. p < 0.05 was considered to be statistically significant. Correlation analysis was performed using Spearman rank correlation. Correlation coefficient R > 0.4 was considered significant.
All supplementary materials are available online at www.molmed.org.
RESULTS
Psychosocial Stress and Norepinephrine Induces Atherosclerosis via Differential Activation of NF-κB Subunits
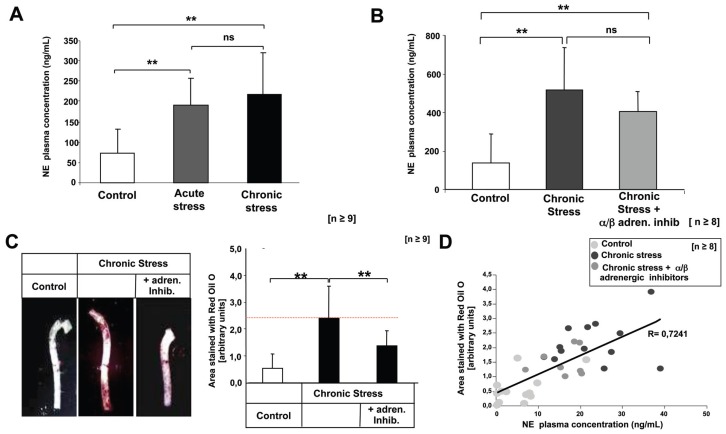
ApoE−/− mice were subjected to either acute or chronic immobilization stress for a period of 4 wks. Both models of stress induced significant increases in the plasma levels of NE, which correlated positively with the extent of atherosclerotic lesion formation, indicating a direct effect of catecholamines. Inhibition of α/β-adrenergic receptors in mice undergoing chronic stress significantly reduced the formation of atherosclerotic lesions without affecting plasma levels of NE (Figure 1). There were no differences in the number of B-lymphocytes (CD45-R+), smooth muscle cells (αSMA+) or endothelial cells (thrombomodulin+) between the two stress models (Supplementary Figure S2A), however, mice undergoing chronic stress did show increased aortic monocytes/macrophages (CD14+) and T-lymphocytes (CD3+). The proinflammatory markers, ICAM-1 and TF (6,40), as well as antiinflammatory marker MnSOD (23) also were increased in CD11-positive macrophages, and were reduced by inhibition of α/β-adrenergic receptors (Supplementary Figure S2B).
Figure 1.
Exposure to chronic stress and subsequent catecholamine release leads to the formation of atherosclerotic lesions. (A) Plasma NE levels in ApoE−/− mice left untreated or subjected to acute or repeated stress. Statistically significant differences are indicated (**p < 0.01). (B) Plasma NE levels in ApoE−/− mice either left untreated or subjected to repeated stress. Where indicated mice received a combination of α-adrenergic and β-adrenergic receptor antagonists. Statistically significant differences are indicated (**p < 0.01). (C) ApoE−/− mice were exposed to repeated stress episodes as described in methods. Representative aortae stained with oil red O and quantification of positive covered are shown. Aortic tissue was evaluated by one investigator blinded for the identities of the experimental groups. Statistically significant differences are indicated (**p < 0.01). Data represent the mean ± SD (n ≥ 8). (D) Diagram showing correlation analysis performed between NE plasma levels and oil red O staining intensity using Spearman rank correlation.
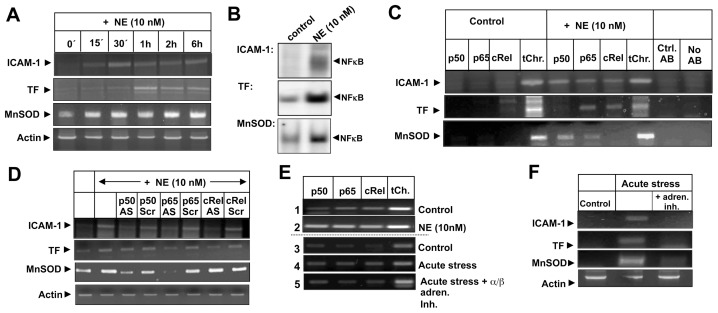
Stimulation of THP-1 cells with NE increased expression of ICAM-1, TF and MnSOD in a time-dependent manner (Figure 2A). In silico analysis of the promoter regions of these genes showed that each of them contained NF-κB binding sites, which showed increased binding activity upon stimulation with NE (Figure 2B). Chromatin immunoprecipitation showed that, upon stimulation, the ICAM-1 promoter was occupied by p50, p65 and cRel, the TF promoter by p65 and cRel and the MnSOD binding site by p50/p65 heterodimers (Figure 2C). Pretreatment with the respective antisense-oligodeoxynucleotides confirmed that a differential pattern of NF-κB subunit activation is induced by NE (Figure 2D). Similar results also were observed for ICAM-1 in peripheral blood mononuclear cells isolated from healthy wild type (C57Bl/6) mice stimulated ex vivo with NE (Figure 2E), as well in the mononuclear cells isolated from ApoE−/− mice subjected to acute stress (Figure 2F). Inhibition of α/β-adrenergic receptors in these mice reduced activation of all NF-κB subunits and respective gene expression, indicating the dependence of stress-induced catecholamine release.
Figure 2.
Norepinephrine and exposure to stress induced NF-κB activation in vitro and ex vivo. NE induced NF-κB activation and subsequent gene expression is mediated by differential composition of NF-κB heterodimers. (A) THP-1-cells were incubated with NE for the indicated times and RT-PCR was performed to determine three types of transcription: ICAM-1, TF and MnSOD. (B) NF-κB binding activity at binding sites of ICAM-1, TF and MnSOD genes measured by EMSA with nuclear extracts from THP-1 cells incubated with NE for 15 min (Control = unstimulated; NE = norepinephrine). (C) Chromatin immunoprecipitation with antibodies to p50, p65, cRel was performed as described in Methods using unstimulated and NE-induced THP-1 cellsan was followed by PCR amplification of NF-κB binding sites in ICAM-1, TF and MnSOD genes. (D) THP-1 cells were left untreated or incubated with antisense or scrambled ODNs for NF-κB p50, p65 or cRel as described in Materials and Methods. Four mRNA levels—ICAM-1, TF, MnSOD and β-actin—were analyzed using RT-PCR. All experiments were repeated at least three times with identical results. (E) pBMC were either isolated from pooled total blood from two C57Bl/6 mice/measure and cultured for 24 h before either left untreated or stimulated with 10 nmol/L NE for 15 min or (1,2) from total blood of five ApoE−/− mice/group, whereas part of the mice were untreated (3) or underwent a 20 min immobilization stress in the absence (4) or presence of adrenergic inhibitors (5). Chromatin immunoprecipitation was performed followed by PCR amplification of NF-κB binding site in the murine ICAM-1 promoter. Total chromatin served as positive control. The experiment was repeated twice with identical results. (F) pBMC were isolated from pooled total blood derived from five ApoE−/− mice/group and analyzed for ICAM-1, TF, MnSOD and β-actin mRNA levels using RT-PCR. The experiment was repeated twice with identical results.
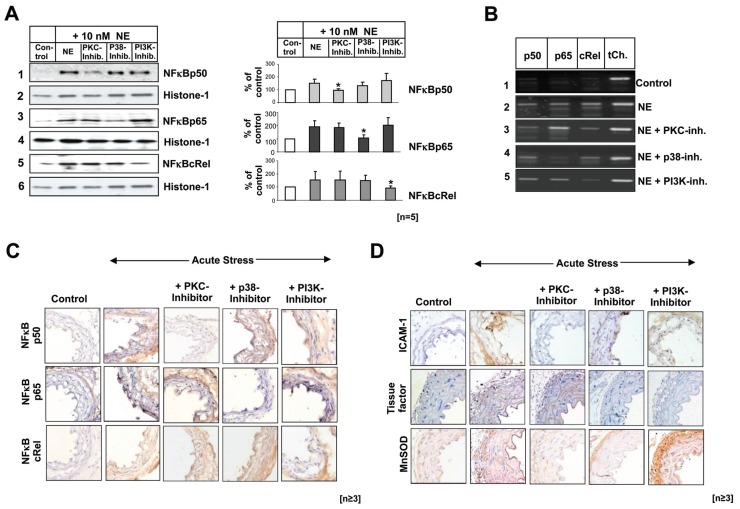
Stress-Induced Differentiation Activation of NF-κB Requires Different Signaling Pathways
Inhibition of PKC in NE stimulated THP-1 cells, reduced p50 nuclear translocation and DNA binding to ICAM-1 promoter, whereas inhibition of p38MAPK decreased p65 activity. cRel nuclear translocation and DNA binding was reduced by inhibition of phosphoinositide-3-kinase (PI3K) (Figures 3A,B). PKC inhibition also reduced cRel binding, without affecting nuclear translocation, suggesting that not only the availability of nuclear NF-κB subunits, but also the presence of specific subunits at a given promoter, might influence the binding of other subunits required to form transcriptionally active heterodimers.
Figure 3.
Effects of PKC, p38MAPK or PI3K pathway inhibition on NF-κB subunits nuclear translocation in vitro: THP-1 cells were preincubated for 45 min in the absence or presence of the PKC, p38MAPK or PI3K inhibitor before treatment with NE for 15 min. (A) Nuclear extracts of THP-1 cells were immunoblotted with antibodies to p50, p65, cRel and histone-1. The signal intensity was evaluated and is summarized in the bargraphs. Statistical significant differences are indicated (*p < 0.05). Data represent the mean ± SD (n = 5). (B) The recruitment of p50, p65 and cRel-subunits to the ICAM-1 promoter was determined using ChIP-assays. (C) NF-κB subunit activation in vivo. ApoE−/− mice were either untreated or underwent immobilization as described in Materials and Methods, in the absence or presence of the inhibitors of PKC, p38 MAPK or PI3K. Aortic sections were stained with antibodies to p50, p65and cRel (magnification: 20×). The experiment was repeated three times with identical results. (D) Target gene expression in aortic tissue: Frozen (top, bottom) or paraffin-embedded (middle) aortic sections were stained for ICAM-1, TF and MnSOD using magnification 20×. The experiment was repeated three times with identical results.
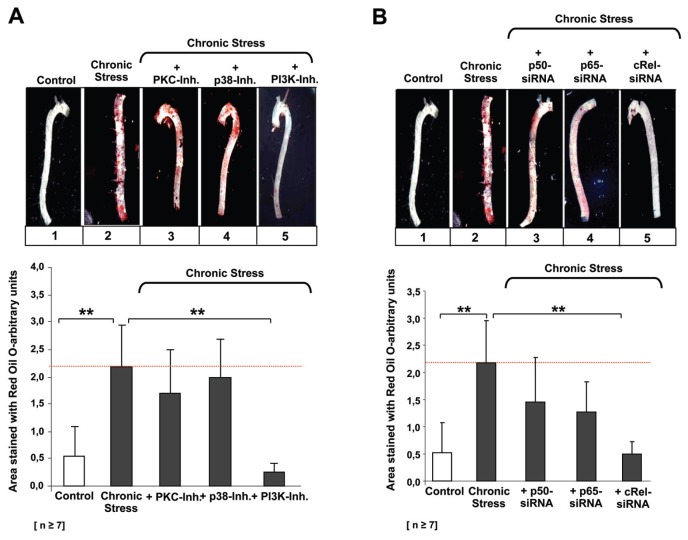
cRel Activation Plays a Key Role in Psychosocial Stress-Induced Atherosclerosis
ApoE−/− mice subjected to acute stress showed significant increases in p50, p65 and cRel positivity in inflammatory and endothelial cells of the aortic root (Figure 3C). Consistent with the in vitro findings (Figures 3A,B), pretreatment of the mice with the inhibitors of PKC, p38MAPK and PI3K resulted in a reduction of ICAM-1 expression, while TF expression was reduced when either p65 or cRel were inhibited by p38MAPKi-nase or PI3K, respectively. MnSOD expression was reduced when p50 or p65 and PKC or p38MAPK were inhibited (Figure 3D). With respect to the formation of atherosclerotic lesions, it was observed that lesion formation was not affected substantively by inhibition of either p50 or p65 signaling pathways, whereas inhibition of cRel resulted in significant reduction in lesion formation, suggesting a key role of cRel activation in atherosclerosis (Figure 4A). These results were confirmed subsequently in acutely stressed ApoE−/− mice treated with NF-κB subunit–specific siRNAs (Figure 4B). Neither stress-induced aortic lesions nor extracellular matrix composition were affected significantly by inhibition of p50 (Supplementary Figure S4). Although inhibition of p65 only caused a moderate reduction of aortic lesions, it resulted in a significant reduction of aortic proteoglycan content and elastic fiber thickness (Supplementary Figure S4). By contrast, inhibition of cRel significantly reduced both aortic lesions and intimal thickening, consistent with the changes in the extracellular matrix composition in mice pretreated with siRNA targeting PI3K.
Figure 4.
Selective inhibition of PI3K pathway and cRel leads to the decrease of atherosclerotic lesions in aortas of ApoE−/− mice exposed to the repeated transient stress. (A) ApoE−/− mice were exposed to repeated stress episodes as described in methods. Thereafter, total aortae from at least four ApoE−/− mice, untreated; stressed; pretreated with PKC, p38MAPK or PI3K inhibitor; were stained with oil red O and evaluated by one investigator blinded to the identities of the experimental groups. Statistically significant differences are indicated (**p < 0.01). (B) Untreated (same staining as in Figure 5A) or stressed ApoE−/− mice (same staining as in Figure 5A) were pretreated with siRNA for p50, p65, cRel. Aortae were stained with oil red O and evaluated by one investigator blinded to the identities of the experimental groups. Statistically significant differences are indicated (**p < 0.01).
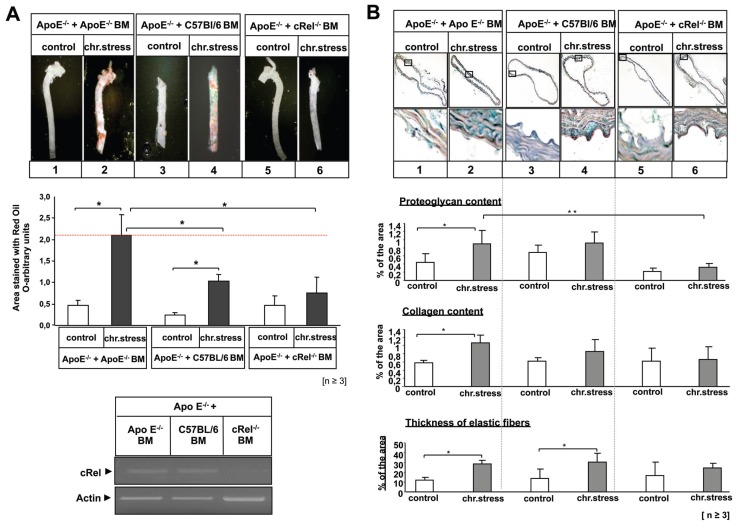
These results suggest that with respect to psychosocial stress, cRel activation indeed plays a key role in the development of atherosclerosis. To confirm this concept, ApoE−/− mice were transplanted with either ApoE−/− BM, C57BL/6-BM or BM from cRel−/− mice (37)(35) devoid of mononuclear cRel-expression. Stress-induced lesion formation was not altered in ApoE−/− mice transplanted with ApoE−/−BM and, as expected, was reduced in ApoE−/− mice transplanted with C57Bl/6-BM (Figure 5A). Stress-induced atherosclerotic lesions, however, were abrogated completely in ApoE−/− mice transplanted with cRel−/− BM. The extracellular matrix also was decreased in cRel−/−/ApoE−/−chimera, consistent with cRel-mediated sustained inflammation (Figure 5B).
Figure 5.
cRel deficiency reduces atherosclerotic lesions and extracellular matrix changes in response to repeated transient stress. Apo E−/− mice underwent BM transplantation, receiving BM from either male Apo E−/−, C57Bl/6-wild-type or cRel−/− mice-donor mice. After 6 wks of reconstitution, mice either left untreated or subjected to repeated episodes of immobilization stress for 4 wks as described above. (A) Aortae of untreated and stressed ApoE−/− mice that had received BM from either ApoE−/− mice (lane 1, 2), C57BL6 mice (lane 3, 4) or cRel−/− mice (lane 5, 6) were stained with oil red O. The positive area was quantified using ImageJ software and is summarized in the bar graphs. Aortas from at least 3 mice per group were stained and quantified. Statistically significant differences are indicated by (*p < 0.05). Data represent the mean ± SD (n ≥ 3). The RT PCR at the bottom demonstrates the efficiency of the BM engraftment; RNA was isolated from the pBMC of the animals that underwent BM transplantation and assayed for NF-κB cRel transcripts. (B) Frozen aortic sections were stained with Movat pentachrome stain as described in methods. Magnification: 4×, 20×. Sections were analyzed with Image Pro software as described. The results are summarized in the bargraphs and statistical significant differences are indicated by (*p < 0.05; **p < 0.01). Data represent the mean ± SD (n = 3).
Suppression of Antioxidant Defenses by cRel
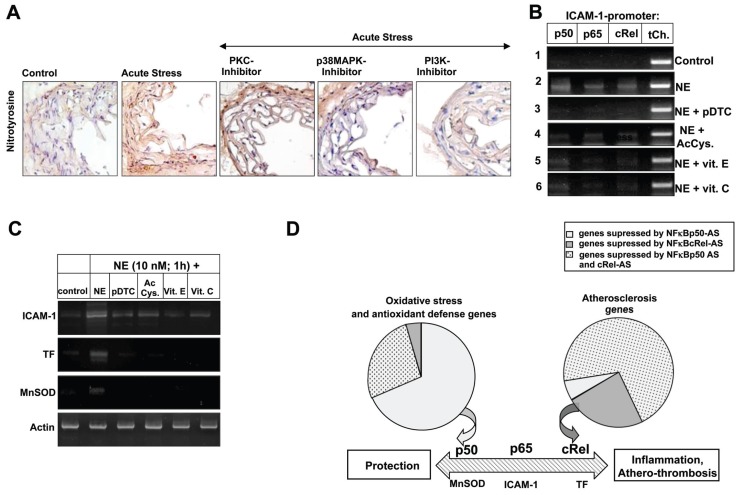
Oxidative stress has been proposed as an underlying mechanism for the development of atherosclerotic lesions. Consistent with this, ApoE−/−mice subjected to acute stress showed significant increases in oxidative stress as indicated by the formation of nitrotyrosine in vascular cells of the aortic root (Figure 6A). Nitrotyrosine levels were not reduced when either p50 or p65 signaling pathways were inhibited, but were reduced significantly by inhibition of cRel-dependent PI3K. As the expression of the antioxidant MnSOD is regulated in part by p50/p65 heterodimers, it would have been expected that inhibition of these subunits and, in turn, MnSOD expression would have led to increased oxidative stress. This result would suggest that although p50 and p65 are activated during stress, the presence of cRel forces the induction of proinflammatory genes such as ICAM-1 and TF, rather than induction of antioxidant genes such as MnSOD.
Figure 6.
(A) Suppression of cellular antioxidative defense is dependent on PI3K and cRel. ApoE−/− mice were either untreated or underwent 20 min immobilization in the absence or presence of PKC, p38MAPK or PI3K inhibitors as described. Frozen aortic sections were stained for nitrotyrosine (Magnification: 20×). (B, C) Treatment with antioxidant leads to nonselective inhibition of NF-κB. THP-1 cells were preincubated for 6 h in the absence or presence of pDTC (10 μmol/L), AcCys (5 mmol/L), vitamin E (600 U/mL) or vitamin C (2 mmol/L) before exposure to NE for 15 min or 1 h. (B) Recruitment of the NF-κB subunits p50, p65 and cRel to the NF-κB site of the ICAM-1 promoter, assayed by ChIP, following treatment with antioxidants. (C) RT-PCR for ICAM-1, TF and MnSOD transcription. The experiment was repeated twice with identical results. (D) NF-κB complexes differentially regulate multiple gene products. THP-1 cells were stimulated with 10 nmol/L NE for 1 h after being pretreated with asODN for either p50, cRel or both for 48 h before quantitative RT-PCR profiling arrays for the expression of genes involved in, the antioxidative defense or atherosclerosis were performed. Diagrams are showing the distribution of genes suppressed by respective asODN (See Supplementary Table S5 for complete list of the respective genes).
Treatment with Antioxidants Leads to General Inhibition of NF-κB Subunits and Subsequent NF-κB-Regulated Gene Expression
It was observed that treatment of THP-1 cells with a selection of antioxidants prior to stimulation by NE led to the suppressed nuclear translocation of p50, p65 and cRel (Figure 6B) and the expression of ICAM-1, TF and MnSOD (Figure 6C). Quantitative real-time PCR microarray analysis of cells treated with NF-κB-specific antisense-oligodeoxynucleotides prior to NE stimulation, showed that the majority of the genes involved in antioxidative defenses were suppressed by inhibition of p50, while suppression of cRel inhibited gene products involved in atherosclerosis (Figure 6D, Supplementary Table S5). Inhibition of p50 also was found to reduce genes involved in NF-κB signaling, suggesting that a general inhibition of NF-κB, as is the case with antioxidants, not only may inhibit NF-κB-dependent anti-oxidant defense systems, such as MnSOD, but also may disrupt the NF-κB network required to ensure normal cellular functioning. This is further supported by in silico analysis of NF-κB subunit recruitment to the promoters of the various genes involved either in atherosclerosis or antioxidant defense, thereby confirming diverging roles of cRel versus p50. Selective inhibition of cRel activation might therefore preserve the proresolution and antioxidant effects of NF-κB, while limiting the proinflammatory effects of NF-κB.
DISCUSSION
A model of stress-induced atherosclerosis was established to investigate post-receptor signaling leading to NF-κB activation. The model of acute stress was used to describe the instantaneous and acute changes in NF-κB activation and mRNA transcription. The chronic stress model was used to show the long-term effects on vascular integrity. It has been demonstrated that emotional stress can trigger cardiovascular events and, while the exposure to acute stressors, such as earthquakes, has been associated with an increased risk of acute coronary syndrome, arrhythmia, pulmonary embolism and transient left ventricular apical ballooning (“Takotsubo” cardiomyopathy) (47), exposure to chronic stressors has been linked to the increased blood pressure (48) as well as increased levels of the proinflammatory and procoagulant markers (49). The physiology of the stress response is very complex, involving not only heightened sympathetic nervous system activity, which is associated with the activation of α and β adrenergic receptors, but also reduced parasympathetic activity. Studies have shown an important role of vagal withdrawal in stress response, suggesting that parasympathetic inhibition can lead to reduced heart rate variability and promote endothelial dysfunction via mechanisms independent of adrenergic receptors, and therefore are not amendable by action of β blockers (50). Furthermore, during exposure to chronic stress, several molecular cascades are activated, modifying the immune state of the organisms and further promoting inflammation (51).
Apo E-deficient mice are widely used in atherosclerosis research. The ApoE- deficient mouse model is the only genetically engineered model that develops extensive atherosclerotic lesions on a chow diet and is also the model in which the lesions have been characterized most thoroughly (8). Utilizing these mice, we were able to show that induction of stress leads to increased circulation of NE, leading to differential activation of the NF-κB subunits p50, p65 and cRel. Selective inhibition of the NF-κB subunits and their respective signaling pathways demonstrated that the formation of stress-induced atherosclerotic lesions can be reduced either by inhibition of the PI3K pathway or by direct inhibition of cRel. These findings indicate that differential activation of NF-κB subunits can predict the gene expression program in response to a given stimulus and thus defines single NF-κB subunits as a specific target for therapeutic intervention.
It has been shown that inhibition of the NF-κB pathway with a macrophage-restricted deletion of IκB kinase 2 (IKK2) promotes severe atherosclerosis in LDL-receptor-deficient mice due to an imbalance of pro- and antithrombotic mechanisms (24). The present study extends these observations and identifies cRel as an essential mediator of atherothrombotic gene expression. The function of cRel was investigated mainly in hematopoietic cell lineages, revealing the defects in lymphocyte proliferation and humeral immunity in mice lacking cRel (52,53). The cRel−/− mice used in this study were viable and healthy throughout the experimental procedure. Several studies have demonstrated that cRel plays an important role in different pathways contributing to the inflammatory response, such as induction of cytokines, autoimmunity and infection diseases (54–57).
Regulation of cRel is controlled by key residues in the binding motifs present in the respective promoter sequences (58). The specificity-determining region of cRel increases its affinity for binding sites that diverge from the canonical NF-κB consensus sequence. As a consequence, p65 and cRel appear to regulate largely distinct sets of genes despite high structural homologies (58,59). NF-κB sites that contain three consecutive G nucleotides at positions 1–3 of the half-site in the NF-κB binding motif preferentially bind p50/p65-heterodimers, whereas sites that contain a T or C at position 1 selectively bind p65/cRel-heterodimers and preclude p50/p65 (60,61). Therefore, the presence of selective recognition motifs in promoters of different NF-κB- controlled genes predicts subunit binding. Our findings suggest that the genes involved in inflammation and atherosclerosis are modulated predominantly by cRel. Dominant nuclear translocation of cRel has been observed at early time points of inflammation (25). Recent work investigating the underlying molecular mechanisms of cardiac hypertrophy has demonstrated the pivotal role for cRel as a positive regulator of cardiac hypertrophy and remodeling and has suggested that disease-related shifts in balance from NF-κB p50 toward cRel-dependent signaling has a positive influence on the expression of genes controlling the adaptive response of the stressed heart (62). Consistent with these observations, our findings show that cRel is a potential target for the development of a specific treatment for mitigating the atherosclerotic response in humans. Future studies are needed to delineate the correlation between the extent of cRel activation and onset and/or progress of atherosclerosis. Nevertheless, given that cRel activation elicits atherosclerotic response, whereas p50 and p65 participate in the resolution of inflammation, a global antioxidant strategy is likely to fail. The results of some clinical studies (16–19) support this concept. Psychological strategies aimed at reducing the stress burden also should be investigated with respect to their impact on cRel activation, compared with the activation of p65 and p50. In addition, future research is necessary to find out whether the reduction of psychosocial stress has an effect on the kinases regulating the activation of respective NF-κB subunits.
Our findings demonstrate that activation and/or induction of cRel is mediated largely by the PI3K pathway. Inhibition of PI3K reduced cRel activation and translocation as well as cRel-mediated expression of ICAM-1 and TF expression, but it neither affected p65 or p50 binding to DNA, nor significantly reduced MnSOD expression in vitro or in vivo. The latter supports a concept in which cRel-dependent inflammation as well as p50/65-triggered resolution of inflammation (22) are, at least in part, controlled by turning off PI3K and activating cellular antioxidant defense mechanisms. This is consistent with a described mechanism of inhibition of NF-κB activation by statins (63). An integrative genomic approach demonstrated the role of PI3K–NF-κB signaling in the survival of breast cancer cell lines, further implying that turning off PI3K is a central step in the regulation and termination of inflammation (64).
CONCLUSION
In the present study, we have described distinctive signaling pathways leading to the activation of NF-κB subunits p50, p65 and cRel in response to stress and/or NE and have shown the physiological significance of these pathways by identifying cRel as a main differentiator responsible for the expression of proatherogenic and prothrombotic genes. These findings point to the selective targeting of cRel activation and maintaining p50/p65-controlled protective pathways as the basis for an NF-κB subunit-based novel therapeutic strategy, which would limit the proinflammatory effects of NF-κB, while preserving the antiinflammatory and antioxidant functions.
Supplemental Data
ACKNOWLEDGMENTS
The authors cordially thank Frank Autschbach, Institute for Pathology, University of Heidelberg, for his help and advice in performing the immunohistochemistry, and Hsiou C Liou, Department of Medicine, The New York Presbyterian Hospital, for the cRel−/− mice. In addition, the authors are grateful to Anja Buhl, Katja Heeb and Axel Erhardt for excellent technical assistance. This study was supported by the Dietmar-Hopp-Stiftung (PP Nawroth), the Deutsche Forschungsgemeinschaft (SFB938 to PP Nawroth; IS67/5–1 to B Isermann), the Network Aging Research (NAR; to A Bierhaus), and a grant from the German Society for Thrombosis and Haemostasis (GTH; to A Bierhaus and PP Nawroth).
Footnotes
Online address: http://www.molmed.org
DISCLOSURE
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
REFERENCES
- 1.Yusuf S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 2.Blumenthal JA, et al. Effects of exercise and stress management training on markers of cardiovascular risk in patients with ischemic heart disease: a randomized controlled trial. JAMA. 2005;293:1626–34. doi: 10.1001/jama.293.13.1626. [DOI] [PubMed] [Google Scholar]
- 3.Bierhaus A, Nawroth PP. Multiple levels of regulation determine the role of the receptor for AGE (RAGE) as common soil in inflammation, immune responses and diabetes mellitus and its complications. Diabetologia. 2009;52:2251–63. doi: 10.1007/s00125-009-1458-9. [DOI] [PubMed] [Google Scholar]
- 4.Bierhaus A, et al. Diabetes-associated sustained activation of the transcription factor nuclear factor-kappaB. Diabetes. 2001;50:2792–808. doi: 10.2337/diabetes.50.12.2792. [DOI] [PubMed] [Google Scholar]
- 5.Collins T, Cybulsky MI. NFkappaB: pivotal mediator or innocent bystander in atherogenesis? J Clin Invest. 2001;107:255–64. doi: 10.1172/JCI10373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Winther MP, Kanters E, Kraal G, Hofker MH. Nuclear factor kappaB signaling in atherogenesis. Arterioscler Thromb Vasc Biol. 2005;25:904–14. doi: 10.1161/01.ATV.0000160340.72641.87. [DOI] [PubMed] [Google Scholar]
- 7.Jawien J, et al. Inhibition of nuclear factor-kappaB attenuates artherosclerosis in apoE/LDLR - double knockout mice. J Physiol Pharmacol. 2005;56:483–9. [PubMed] [Google Scholar]
- 8.Jawien J, Nastalek P, Korbut R. Mouse models of experimental atherosclerosis. J Physiol Pharmacol. 2004;55:503–17. [PubMed] [Google Scholar]
- 9.Olszanecki R, et al. Effect of curcumin on atherosclerosis in apoE/LDLR-double knockout mice. J Physiol Pharmacol. 2005;56:627–35. [PubMed] [Google Scholar]
- 10.Hammes HP, et al. Benfotiamine blocks three major pathways of hyperglycemic damage and prevents experimental diabetic retinopathy. Nat Med. 2003;9:294–9. doi: 10.1038/nm834. [DOI] [PubMed] [Google Scholar]
- 11.Isermann B, et al. Activated protein C protects against diabetic nephropathy by inhibiting endothelial and podocyte apoptosis. Nat Med. 2007;13:1349–58. doi: 10.1038/nm1667. [DOI] [PubMed] [Google Scholar]
- 12.Brasier AR. The NFkappaB regulatory network. Cardiovasc Toxicol. 2006;6:111–30. doi: 10.1385/ct:6:2:111. [DOI] [PubMed] [Google Scholar]
- 13.Gloire G, Legrand-Poels S, Piette J. NFkappaB activation by reactive oxygen species: fifteen years later. Biochem Pharmacol. 2006;72:1493–505. doi: 10.1016/j.bcp.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 14.Li N, Karin M. Is NFkappaB the sensor of oxidative stress? FASEB J. 1999;13:1137–43. [PubMed] [Google Scholar]
- 15.Rojas A, Figueroa H, Morales MA, Re L. Facing up the ROS labyrinth—Where to go? Curr Vasc Pharmacol. 2006;4:277–89. doi: 10.2174/157016106777698441. [DOI] [PubMed] [Google Scholar]
- 16.Devaraj S, et al. Effect of high-dose alpha-tocopherol supplementation on biomarkers of oxidative stress and inflammation and carotid atherosclerosis in patients with coronary artery disease. Am J Clin Nutr. 2007;86:1392–8. doi: 10.1093/ajcn/86.5.1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maxwell S, Greig L. Antioxidants—a protective role in cardiovascular disease? Expert Opin Pharmacother. 2001;2:1737–50. doi: 10.1517/14656566.2.11.1737. [DOI] [PubMed] [Google Scholar]
- 18.Singh U, et al. High-dose alpha-tocopherol therapy does not affect HDL subfractions in patients with coronary artery disease on statin therapy. Clin Chem. 2007;53:525–8. doi: 10.1373/clinchem.2006.078865. [DOI] [PubMed] [Google Scholar]
- 19.Vivekananthan DP, Penn MS, Sapp SK, Hsu A, Topol EJ. Use of antioxidant vitamins for the prevention of cardiovascular disease: meta-analysis of randomised trials. Lancet. 2003;361:2017–23. doi: 10.1016/S0140-6736(03)13637-9. [DOI] [PubMed] [Google Scholar]
- 20.Hancock WW, Buelow R, Sayegh MH, Turka LA. Antibody-induced transplant arteriosclerosis is prevented by graft expression of anti- oxidant and anti-apoptotic genes. Nat Med. 1998;4:1392–6. doi: 10.1038/3982. [DOI] [PubMed] [Google Scholar]
- 21.Karin M, Yamamoto Y, Wang QM. The IKK NFkappa B system: a treasure trove for drug development. Nat Rev Drug Discov. 2004;3:17–26. doi: 10.1038/nrd1279. [DOI] [PubMed] [Google Scholar]
- 22.Lawrence T, Gilroy DW, Colville-Nash PR, Willoughby DA. Possible new role for NFkappaB in the resolution of inflammation. Nat Med. 2001;7:1291–7. doi: 10.1038/nm1201-1291. [DOI] [PubMed] [Google Scholar]
- 23.Sompol P, Xu Y, Ittarat W, Daosukho C, St Clair D. NFkappaB-associated MnSOD induction protects against beta-amyloid-induced neuronal apoptosis. J Mol Neurosci. 2006;29:279–88. [PubMed] [Google Scholar]
- 24.Kanters E, et al. Inhibition of NFkappaB activation in macrophages increases atherosclerosis in LDL receptor-deficient mice. J Clin Invest. 2003;112:1176–85. doi: 10.1172/JCI18580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adhikari N, Charles N, Lehmann U, Hall JL. Transcription factor and kinase-mediated signaling in atherosclerosis and vascular injury. Curr Atheroscler Rep. 2006;8:252–60. doi: 10.1007/s11883-006-0081-1. [DOI] [PubMed] [Google Scholar]
- 26.Di Santo A, et al. Resveratrol and quercetin down-regulate tissue factor expression by human stimulated vascular cells. J Thromb Haemost. 2003;1:1089–95. doi: 10.1046/j.1538-7836.2003.00217.x. [DOI] [PubMed] [Google Scholar]
- 27.Joyce DE, Gelbert L, Ciaccia A, DeHoff B, Grinnell BW. Gene expression profile of antithrombotic protein c defines new mechanisms modulating inflammation and apoptosis. J Biol Chem. 2001;276:11199–203. doi: 10.1074/jbc.C100017200. [DOI] [PubMed] [Google Scholar]
- 28.Lindner V. The NFkappaB and IkappaB system in injured arteries. Pathobiology. 1998;66:311–20. doi: 10.1159/000028039. [DOI] [PubMed] [Google Scholar]
- 29.Pendurthi UR, Williams JT, Rao LV. Resveratrol, a polyphenolic compound found in wine, inhibits tissue factor expression in vascular cells: A possible mechanism for the cardiovascular benefits associated with moderate consumption of wine. Arterioscler Thromb Vasc Biol. 1999;19:419–26. doi: 10.1161/01.atv.19.2.419. [DOI] [PubMed] [Google Scholar]
- 30.Weih F, et al. p50-NFkappaB complexes partially compensate for the absence of RelB: severely increased pathology in p50(−/−)relB(−/−) double-knockout mice. J Exp Med. 1997;185:1359–70. doi: 10.1084/jem.185.7.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bierhaus A, Humpert PM, Nawroth PP. Linking stress to inflammation. Anesthesiol Clin. 2006;24:325–40. doi: 10.1016/j.atc.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 32.Bierhaus A, et al. A mechanism converting psychosocial stress into mononuclear cell activation. Proc Natl Acad Sci U S A. 2003;100:1920–5. doi: 10.1073/pnas.0438019100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bluher M. Adipose tissue dysfunction in obesity. Exp Clin Endocrinol Diabetes. 2009;117:241–50. doi: 10.1055/s-0029-1192044. [DOI] [PubMed] [Google Scholar]
- 34.Brett JG, Steinberg SF, deGroot PG, Nawroth PP, Stern DM. Norepinephrine down-regulates the activity of protein S on endothelial cells. J Cell Biol. 1988;106:2109–18. doi: 10.1083/jcb.106.6.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fu JH, et al. The combination of a high-fat diet and chronic stress aggravates insulin resistance in Wistar male rats. Exp. Clin. Endocrinol Diabetes. 2009;117:354–60. doi: 10.1055/s-0028-1119406. [DOI] [PubMed] [Google Scholar]
- 36.von Känel R, et al. Effect of acute psychological stress on the hypercoagulable state in subjects (spousal caregivers of patients with Alzheimer’s disease) with coronary or cerebrovascular disease and/or systemic hypertension. Am J Cardiol. 2001;87:1405–8. doi: 10.1016/s0002-9149(01)01564-8. [DOI] [PubMed] [Google Scholar]
- 37.Boffa DJ, et al. Selective loss of c-Rel compromises dendritic cell activation of T lymphocytes. Cell Immunol. 2003;222:105–15. doi: 10.1016/s0008-8749(03)00114-x. [DOI] [PubMed] [Google Scholar]
- 38.Muhammad S, et al. The HMGB1 receptor RAGE mediates ischemic brain damage. J Neurosci. 2008;28:12023–31. doi: 10.1523/JNEUROSCI.2435-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hofmann MA, et al. Peripheral blood mononuclear cells isolated from patients with diabetic nephropathy show increased activation of the oxidative-stress sensitive transcription factor NFkappaB. Diabetologia. 1999;42:222–32. doi: 10.1007/s001250051142. [DOI] [PubMed] [Google Scholar]
- 40.Bierhaus A, et al. Antiparasitic treatment of patients with P. falciparum malaria reduces the ability of patient serum to induce tissue factor by decreasing NFkappa B activation. Thromb Haemost. 1995;73:39–48. [PubMed] [Google Scholar]
- 41.Mao X, Moerman-Herzog AM, Wang W, Barger SW. Differential transcriptional control of the superoxide dismutase-2 kappaB element in neurons and astrocytes. J Biol Chem. 2006;281:35863–72. doi: 10.1074/jbc.M604166200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nowak DE, Tian B, Brasier AR. Two-step cross-linking method for identification of NFkappaB gene network by chromatin immunoprecipitation. Biotechniques. 2005;39:715–25. doi: 10.2144/000112014. [DOI] [PubMed] [Google Scholar]
- 43.Beattie JH, Duthie SJ, Kwun IS, Ha TY, Gordon MJ. Rapid quantification of aortic lesions in apoE(−/−) mice. J Vasc Res. 2009;46:347–52. doi: 10.1159/000189795. [DOI] [PubMed] [Google Scholar]
- 44.Seehaus S, et al. Hypercoagulability inhibits monocyte transendothelial migration through protease-activated receptor-1-, phospholipase-Cbeta-, phosphoinositide 3-kinase-, and nitric oxide-dependent signaling in monocytes and promotes plaque stability. Circulation. 2009;120:774–84. doi: 10.1161/CIRCULATIONAHA.109.849539. [DOI] [PubMed] [Google Scholar]
- 45.Fredrikson GN, et al. Inhibition of atherosclerosis in apoE-null mice by immunization with apoB-100 peptide sequences. Arterioscler Thromb Vasc Biol. 2003;23:879–84. doi: 10.1161/01.ATV.0000067937.93716.DB. [DOI] [PubMed] [Google Scholar]
- 46.Movat HZ. Demonstration of all connective tissue elements in a single section; pentachrome stains. AMA Arch Pathol. 1955;60:289–295. [PubMed] [Google Scholar]
- 47.Hata S. Cardiovascular disease caused by earthquake-induced stress: psychological stress and cardiovascular disease. Circ J. 2009;73:1195–1196. doi: 10.1253/circj.cj-09-0305. [DOI] [PubMed] [Google Scholar]
- 48.Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008;51:1237–46. doi: 10.1016/j.jacc.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jain S, Mills PJ, von Kanel R, Hong S, Dimsdale JE. Effects of perceived stress and uplifts on inflammation and coagulability. Psychophysiology. 2007;44:154–60. doi: 10.1111/j.1469-8986.2006.00480.x. [DOI] [PubMed] [Google Scholar]
- 50.Burg MM, Soufer A, Lampert R, Collins D, Soufer R. Autonomic contribution to endothelin-1 increase during laboratory anger- recall stress in patients with coronary artery disease. Mol Med. 2011;17:495–501. doi: 10.2119/molmed.2010.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vale S. Psychosocial stress and cardiovascular diseases. Postgrad Med J. 2005;81:429–35. doi: 10.1136/pgmj.2004.028977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liou HC, Hsia CY. Distinctions between c-Rel and other NFkappaB proteins in immunity and disease. Bioessays. 2003;25:767–80. doi: 10.1002/bies.10306. [DOI] [PubMed] [Google Scholar]
- 53.Kontgen F, et al. Mice lacking the c-rel proto-oncogene exhibit defects in lymphocyte proliferation, humoral immunity, and interleukin-2 expression. Genes Dev. 1995;9:1965–77. doi: 10.1101/gad.9.16.1965. [DOI] [PubMed] [Google Scholar]
- 54.Lu YC, et al. Differential role for c-Rel and C/EBPbeta/delta in TLR-mediated induction of proinflammatory cytokines. J Immunol. 2009;182:7212–21. doi: 10.4049/jimmunol.0802971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sanjabi S, Hoffmann A, Liou HC, Baltimore D, Smale ST. Selective requirement for c-Rel during IL-12 P40 gene induction in macrophages. Proc Natl Acad Sci U S A. 2000;97:12705–10. doi: 10.1073/pnas.230436397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Campbell IK, Gerondakis S, O’Donnell K, Wicks IP. Distinct roles for the NFkappaB1 (p50) and c-Rel transcription factors in inflammatory arthritis. J Clin Inv. 2000;105:1799–806. doi: 10.1172/JCI8298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harling-McNabb L, et al. Mice lacking the transcription factor subunit Rel can clear an influenza infection and have functional anti-viral cytotoxic T cells but do not develop an optimal antibody response. Int Immunol. 1999;11:1431–9. doi: 10.1093/intimm/11.9.1431. [DOI] [PubMed] [Google Scholar]
- 58.Hoffmann A, Leung TH, Baltimore D. Genetic analysis of NFkappaB/Rel transcription factors defines functional specificities. EMBO J. 2003;22:5530–9. doi: 10.1093/emboj/cdg534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Natoli G. Tuning up inflammation: how DNA sequence and chromatin organization control the induction of inflammatory genes by NFkappaB. FEBS Lett. 2006;580:2843–9. doi: 10.1016/j.febslet.2006.02.072. [DOI] [PubMed] [Google Scholar]
- 60.Mackman N. Regulation of the tissue factor gene. FASEB J. 1995;9:883–9. doi: 10.1096/fasebj.9.10.7615158. [DOI] [PubMed] [Google Scholar]
- 61.Parry GC, Mackman N. A set of inducible genes expressed by activated human monocytic and endothelial cells contain kappa B-like sites that specifically bind c-Rel-p65 heterodimers. J Biol Chem. 1994;269:20823–5. [PubMed] [Google Scholar]
- 62.Gaspar-Pereira S, et al. The NFkappaB subunit c-Rel stimulates cardiac hypertrophy and fibrosis. Am J Pathol. 2012;180:929–39. doi: 10.1016/j.ajpath.2011.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Holschermann H, et al. Statins prevent NFkappaB transactivation independently of the IKK-pathway in human endothelial cells. Atherosclerosis. 2006;185:240–5. doi: 10.1016/j.atherosclerosis.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 64.Boehm JS, et al. Integrative genomic approaches identify IKBKE as a breast cancer oncogene. Cell. 2007;129:1065–79. doi: 10.1016/j.cell.2007.03.052. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.