Abstract
Introduction
Recent advancements in the management of colorectal liver metastases have resulted in an improvement in survival. Novel biomarkers such as KRAS, and their mutations potentially predict the response of biological therapies such as cetuximab (Erbitux). This paper evaluates the use of cetuximab in the first-line management of colorectal liver metastases.
Methods
An electronic literature search was performed of publications within the past 6 years. The following key words, singly or in combination, were used: KRAS, cetuximab, metastatic colorectal cancer and colorectal liver metastases. All randomized controlled trials and cohort studies were included.
Results
Fifteen prospective studies reviewed the clinical application of cetuximab. Seven studies included sub-group analysis of KRAS mutational status, with only one study performed prospectively. Until the MRC COIN trial, the evidence consistently demonstrated cetuximab significantly improved progression-free survival, overall survival and surgical resection rates, especially in KRAS wild-type tumours. However, the MRC COIN trial found cetuximab had no additional benefit when combined with standard chemotherapy.
Conclusions
The literature does not support the routine use of cetuximab as the standard first-line treatment of colorectal liver metastases, rather highlighting the need for the optimization of treatment on an individual basis, especially depending on tumour KRAS status.
Introduction
Metastatic colorectal cancer (mCRC) and its management pose a dilemma worldwide. Around 110 new cases of colorectal cancer are diagnosed daily, and 39 991 new cases were registered in the UK in 2008.1 In total, 30–40% of these patients will re-present with recurrent disease, often within the first 2 years of the initial treatment, with the common site for metastatic spread being the liver.2
The management of mCRC is multi-modal, and recent advancements in oncological and surgical management, with new-targeted therapies available, have resulted in an overall improvement in survival in this subgroup of patients. The widely used chemotherapy agents for the treatment of colorectal cancer include 5-fluorouracil (5-FU) in combination with folinic acid (FA) and oxaliplatin. In the setting of metastatic disease, 5-FU in combination with folinic acid has been shown to prolong survival by up to 12 months.3
In the last decade new targets have been identified for the treatment of colorectal cancer and their subsequent metastases. Novel candidate biomarkers are thought to be of both prognostic and diagnostic value. One such biomarker, v-Ki-ras2Kirsten rat sarcoma viral oncogene homologue (KRAS), a GTPase protein, may prove vital in determining a patient's response to certain chemotherapy/biological agents in the setting of metastatic colorectal cancer.4 Activated KRAS mutations have a role in oncogenic transformation during the development of colorectal cancer, and data would suggest they have a prevalence of 30–40% in colorectal cancer patients. The KRAS gene may be normal (wild type) or mutated, in the mutated form unregulated proliferation and impaired differentiation is promoted. These mutations are thought to potentially predict the response of biological therapies such as cetuximab (Erbitux, Merck Serono, Geneva, Switzerland), as those patients harbouring KRAS mutations may not benefit from these drugs.
Cetuximab is a recombinant monoclonal antibody that blocks the human epidermal growth factor receptor (EGFR) and therefore inhibits the proliferation of cells that depend on EGFR activation for growth. The BOND trial investigated patients' refractory to irinotecan, and found cetuximab in isolation was associated with a response rate of 10.8% and a median survival of 6.9 months. When combined with other treatments, the response rate improved to 22.9% and a median survival of 8.6 months.5 This resulted in the approval of the use of cetuximab in refractory metastatic colorectal cancer by the European Medicines Agency (EMEA) in June 2004. Studies have subsequently concentrated on the use of cetuximab as a first-line treatment combined with chemotherapy.
At present, there is a wide variation of practice with regard to colorectal liver metastases. This extended literature review, therefore, aimed to evaluate the clinical role of cetuximab when used as the first-line treatment of colorectal liver metastases and to determine its role in clinical practice within the setting of colorectal liver metastases.
Methods
An up-to-date computer-aided literature search was performed using the following databases:
PubMed/MEDLINE (1966 to date; National Library of Medicine, Bethesda, MD, USA);
Athens;
Embase (1980 to date; Elsevier Science, New York, NY, USA);
The Cochrane Central Register of Controlled Trials (Central);
Ovid.
The following key words were used: KRAS, cetuximab, erbitux, metastatic colorectal cancer, colorectal liver metastases, singly or in combination. To ensure an up-to-date literature search, the search was initially restricted to the last 6 years (2006–2011). To maximize this search, backward chaining of reference lists from retrieved papers was also undertaken. To ensure all possible literature was included, both published and unpublished, contact was made with the manufacturers of cetuximab, Merck Serono. However, in spite of their reply no further data were added to this review, and they had no input into the literature review.
All randomized controlled trials and cohort studies over the defined time period were included. It was limited to papers only published in the English language, involving human participants and studies that used cetuximab as a first-line treatment for colorectal liver metastases. A total of 15 studies relating to the clinical application of cetuximab as a first-line treatment of colorectal liver metastases were included. (Fig. 1: QUORUM flowchart)
Figure 1.
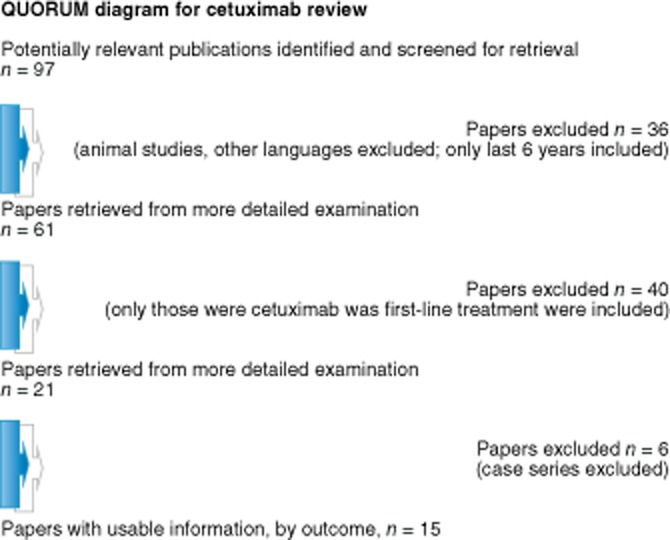
QUORUM diagram for cetuximab review
Literature review
Cetuximab as a first-line treatment for colorectal liver metastases
Many studies have assessed the role of cetuximab when combined with various chemotherapy agents. One of the most common chemotherapy regimens is FOLFOX, a combination of folinic acid (leucovorin), fluorouracil and oxaliplatin; along with FOLFIRI, a combination of folinic acid (FA), fluorouracil (5-FU) and irinotecan. Other described combinations include the use of capecitabine and bevacizumab. This review will assess the role and efficacy of cetuximab when combined with these various chemotherapy agents.
Cetuximab in combination with FOLFOX, FOLFIRI or both
When considering any potential new treatment, it is of prime importance to first establish the safety of such a treatment for human subjects. Folprecht et al. 20066 aimed to investigate safety when cetuximab was used in combination with irinotecan, 5-FU and FA. This was investigated using a prospective phase I/II trial, with no control group for comparison or power calculations to validate the findings. Although 27 patients were recruited, only 21 were included. Documented side effects included an acne-like rash, asthenia, diarrhoea, hypersensitivity, infection, leucopenia, mucositis, and nausea and vomiting. They found that cetuximab did not result in any life-threatening complications, and it was the increasing dose of 5FU that increased the side effect profile rather than cetuximab.
This small study provides level 2 evidence to suggest cetuximab does not alter the pharmokinetics of the chemotherapy agents used, and the increasing side effect profile is potentially as a result of an increased dose of 5FU rather than the addition of cetuximab.
Tabernero et al. 20077 further evaluated the safety and efficacy of cetuximab with FOLFOX-4 (oxaliplatin, FU, and LV) using a multicentre, non-controlled, open-label phase II study, with reproducible methodology. The lack of a control reduces its rigour. An adequately powered sample size of 62 patients enhanced the validity of the findings. An overall response of 72% was described, with a median progression-free survival of 12.3 months, and an overall survival of 30 months. Adverse events included diarrhoea, neutropenia and paraesthesia.
Overall, this study provides level 2 evidence to suggest the cetuximab is safe in clinical practice. However, in isolation and without comparison it cannot provide adequate evidence to support the addition of cetuximab in clinical practice.
Several large studies have been published in recent years to assess the role of cetuximab in the first-line management of metastatic colorectal cancer.
The OPUS study by Bokemeyer et al. in 20098 aimed to assess the best overall response of cetuximab combined with oxaliplatin, leucovorin and fluorouracil (FOLFOX-4) and compare with FOLFOX-4 alone as the first-line treatment of colorectal liver metastases. The strengths of this open-label, randomized multi-centre phase II study include the large adequately powered sample size, true randomization and the subsequent updated publication in 2011, all increasing the rigour of the study and its subsequent validity.9
Overall, the addition of cetuximab improved the overall response from 36% to 46%; however, this was not statistically significant. In the KRAS subgroup, in KRAS wild-type patients the overall response increased from 37% to 61% (P = 0.011) by adding cetuximab. In the updated analysis published in 2011, the overall response increased from 34% to 57% (P = 0.0027). In the entire study cohort, the progression-free survival was the same in both groups, whereas in the KRAS wild-type group, it was higher in those who received cetuximab (P = 0.0163). In the updated analysis, in the cetuximab group, survival was significantly better in those patients who were KRAS wild type (22.8 versus 13.4 months), and in all KRAS wild-type patients, those who received cetuximab had a higher chance of surgical intervention (12% versus 3%, P = 0.02).
In summary, the OPUS study provides level 1 evidence to demonstrate an increased response to treatment when cetuximab was added to the standard chemotherapy regimen, especially in those patients who were found to be KRAS wild type. The more recent 2011 publication enhances the validity of the OPUS study findings, adding strength to the theory that KRAS wild-type tumours have a better response to cetuximab. This, therefore, provides evidence that in clinical practice cetuximab may not be the most appropriate to all patients, but only those who are KRAS wild type further highlighting the need for an individual approach to cancer treatment to optimize the response.
When considering treatment, the overall aim in colorectal liver metastases is to first make unresectable disease resectable. The CELIM study aimed to assess the effectiveness of cetuximab in combination with chemotherapy for unresectable CRLM to downsize tumours for curative resection in the form of a prospective randomized trial.10 However, the methodology had several inherent weaknesses: 17 centres recruited participants introducing undeclared selection bias, the groups were not truly randomized and funding was provided by the drug company reducing the overall rigour of the methodology. The lack of a control group makes it difficult to draw any meaningful, valid conclusions regarding cetuximab.
Comparing cetuximab plus FOLFIRI with cetuximab plus FOLFOX-6, overall response rates were 68% compared with 59% and not statistically significant. The tumour response was higher in the KRAS wild-type group (70%) compared with the mutant group (41%; P = 0.008). The R0 resection rate was 38% in group A and 30% in group B. In those patients who did have a resection, the median time to intervention was noted to be 5.1 months. At the time of publication, disease-free and overall survival data are not yet matured; these are important parameters, which would further enhance the findings of this study and have important implications regarding whether cetuximab should be introduced into clinical practice. The adverse effects associated with these treatment options include 34% skin reactions and 23% neutropenia.
This study provided level 1 evidence that compared with historical controls, chemotherapy with cetuximab yielded a higher response rate and therefore increased resectability. On the basis of this study alone, as a result of the highly selective group with no control group or long-term outcome data, no conclusion can be drawn regarding the role of cetuximab in clinical practice. The variation in outcome depending on KRAS status does, however, further strengthen the argument for the introduction of KRAS testing routinely in metastatic colorectal cancer.
The CRYSTAL study, reported by Van Cutsem et al. in 2009,11 aimed to investigate the efficacy of cetuximab plus irinotecan, fluorouracil and leucovonin (FOLFIRI) as the first-line treatment for metastatic colorectal cancer, and sought to find an association between the mutation status of KRAS and clinical response to cetuximab It prospectively compared FOLFIRI with cetuximab and FOLFIRI in which both groups were truly randomized. This was an adequately powered study in which, 2020 patients were screened, of which 1217 patients underwent randomization, with 1198 subsequently treated (599 in each group).
It found cetuximab plus FOLFIRI reduced the risk of disease progression by 15% compared with FOLFIRI alone (P = 0.048). The response was higher in the cetuximab group (46.9% versus 38.7%), as was the rate of surgical resection (7% versus 3.7%). KRAS wild-type patients had a higher median survival and a higher response rate to cetuximab at 59.3%. This study should be interpreted with caution as two-thirds of patients had further chemotherapy regimens introducing a confounding variable.
The CRYSTAL study provided level 1 evidence demonstrating that cetuximab reduces the risk of progression in metastatic colorectal cancer when used in combination with FOLFIRI as first-line treatment, and is of particular benefit in patients with KRAS wild-type tumours.
The validity of these results is further strengthened by a more recent publication of follow-up data by Van Cutsem et al. 2011,12 which described a definite survival benefit from adding cetuximab. In KRAS wild-type patients, those who received cetuximab had a reduction in disease progression. To date, cetuximab consistently has demonstrated an increased response rate and better overall survival especially in those patients who are KRAS wild type; however, it still remains that these findings are in a highly selective sub group of patients which may not be representative of routine practice.
The CECOG trial is a prospective study of cetuximab and FOLFOX-6 or FOLFIRI by Ocvirk et al. 2010,13 aimed to assess the efficacy and safety of cetuximab combined with two chemotherapy regimens in patients with unresectable metastatic colorectal cancer, with robust methodology and an adequately powered sample size, which found no statistical difference in the outcome of both groups The combination of cetuximab and FOLFOX6 had a superior outcome in KRAS wild-type patients. KRAS wild type had a longer median survival of 22.5 months as compared with 15.2 months of the KRAS mutant (P = 0.02). With regard to survival rates, the KRAS wild-type survival rate at 24 months was 43% compared with 14% in the KRAS mutant group.
Although this is a smaller study when compared with studies such as the CRYSTAL study, it provides level 1 evidence the support the use of cetuximab when combined with chemotherapy, either FOLFIRI or FOLFOX6, in terms of clinical outcome especially progression-free survival. No significant differences were found for cetuximab with FOLFOX6 or FOLFIRI in the first-line treatment of metastatic colorectal cancer. In relation to clinical practice, the validity of these results is significantly reduced by the absence of a control arm, chemotherapy alone. When considering the role of KRAS testing, superior outcomes were only found when cetuximab was combined with FOLFOX6. This has potential implications to clinical practice, challenging the previous data to suggest cetuximab improves outcome in KRAS wild-type tumours, whereas it may also be dependent on what chemotherapy regimen cetuximab is combined with.
In the POCHER trial, by Garufi et al. 2010,14 the effectiveness of cetuximab and chronomodulated irinotecan, 5FU, FA and oxaliplatin administered as neoadjuvant chemotherapy to increase the respectability of colorectal liver metastases was assessed, using a phase II prospective trial involving 2 centres over a 2-year period.
A partial response was obtained in 34 patients, with an objective response rate of 79.1%. Twenty-six patients underwent radical liver surgery with a 60% rate of a R0 resection; 2 had R1 resections whereas 145 (n = 6) were unresectable at laparoscopy. Overall, only two had a complete pathological response.
After a median follow-up of 22 months, 16% were alive without recurrence, 39.5% were alive with recurrence, 2 were lost to follow-up and 39.5% died as a result of disease progression. Of the seven without recurrence, five were KRAS wild-type. The overall progression-free survival was 14 months, 15 months in resectable patients and 9 months in those with unresectable disease.
This study provides level 2 + evidence regarding the benefit of surgical resection of colorectal liver metastases in appropriately selected patients, with a statistically significant improvement in overall survival in those patients who were deemed resectable after resection. Weaknesses include a lack of a control group and a small sample; however, it is not highly selective. As only two patients had a complete pathological response, this study may suggest that the use of chemotherapy in addition to cetuximab is not in isolation but used as a method of down staging the disease. Further randomized controlled studies are required to validate this further.
The MRC COIN trial is the largest prospective randomized phase 3 trial of cetuximab combined with chemotherapy, with the population representative of clinical practice within the UK along with the added advantage of prospective KRAS testing.15 Maughan et al. aimed to assess the effect on overall survival of adding cetuximab to standard chemotherapy in the first-line treatment of advanced colorectal cancer, with robust methodology in which there was reduced selection bias. It involved three arms: arm A consisted of oxaliplatin plus fluoropyrimidine chemotherapy; arm B consisted of arm A plus cetuximab; and arm C was intermittent chemotherapy alone. This study solely compared arm A with B, in which the primary outcome is overall survival in patients with KRAS wild-type tumours. Progression-free survival, response and toxic effects were all evaluated.
In KRAS wild-type patients, the median survival in both groups was similar; however, there was a higher response in the cetuximab group in spite of no increase in curative resection. Irrespective of the treatment undertaken, the median overall survival was shorter in patients with mutations of any three of the KRAS oncogenes studied (n = 706, 13.6 months) compared with wild-type tumours [n = 581; 20.1 months (P < 0.0001)]. Fifty-seven per cent (n = 209) of patients with KRAS wild-type lesions in the control group had a partial or complete response versus 64% (n = 232) in the cetuximab group (P = 0.049). No increase in potential curative liver resection was noted; 13% in the KRAS wild-type control group compared with 15% in the cetuximab group (P = 0.74). Cetuximab was also noted to have a higher incidence of skin, gastrointestinal and other toxic effects.
This large robust study, in contradiction with previously published studies, provides level 1 evidence suggesting there may not be any overall benefit from cetuximab in a population representative of UK clinical practice.
Using the same data set, Adams et al.,16 aimed to compare intermittent versus continuous combination chemotherapy in advanced colorectal cancer, along with the assessment of the effect of the addition of cetuximab to continuous oxaliplatin and fluoropyrimidine combination chemotherapy, which were described previously.
This study, provides level 1 evidence to demonstrate that intermittent chemotherapy when combined with cetuximab is associated with an improved quality of life, shortened time on chemotherapy, a reduction in the number of hospital visits required and a minimal difference in overall survival. Interestingly, this study reported a shorter survival than other reported trials, which may be as a result of more advanced disease at the time of presentation along with the inclusion of a larger number of centres with different confounding approaches to management. Overall, the COIN trial questions the efficacy of cetuximab in a validated study with a clinically relevant cohort of patients.
Cetuximab in combination with oxaliplatin and capecitabine (XELOX)
Borner et al.17 aimed to determine the activity and tolerability of adding cetuximab to oxaliplatin and capecitabine (XELOX) in the first-line treatment of metastatic colorectal cancer. Using robust methodology it concluded this combination improves overall outcome.
Partial response rates were higher with cetuximab (arm B) (arm B 41% versus arm A 14%). The reviewed partial response rates, which were determined independently, were 21.6% in arm A compared with 43.2% in arm B, whereas retrospective overall response rates were 35.1% versus 54%. The median time to treatment failure was 5.7 months in arm A compared with 7.2 months in arm B. The median survival was 16.5 months in arm A and 20.5 months in arm B.
This study, however, provided level 1 evidence to suggest that by combining cetuximab with oxaliplatin and capecitabine (XELOX) improves the overall outcome. As a result of patient drop out, the sample size did not reach an adequate size to power the study significantly, and therefore any findings should be interpreted with caution. In isolation, the findings of the study would not be sufficient to change clinical practice; however, it would suggest the need for further randomized phase III trials to validate these findings.
Cetuximab in combination with capecitabine, oxaliplatin and bevacizumab
The CARIO2 trial assessed cetuximab in combination with capecitabine, oxaliplatin and bevacizumab.18 Although the methodology was not entirely robust, as a result of the entire sample not being included; this publication provides level 2 evidence that this is a safe drug, which can be given to patients without a major risk of severe side effects.
A more recent publication by Tol et al.19 aimed to assess the effect of adding the anti-epidermal growth factor receptor (EGFR) antibody cetuximab to a combination of capecitabine, oxaliplatin and bevacizumab for the first-line treatment of metastatic colorectal cancer.
This study provides level 1 evidence to contradict many previous studies, in which it demonstrated with statistically significance that cetuximab when combined with capecitabine, oxaliplatin and bevacizumab did not improve progression-free survival. In fact it actually decreased progression-free survival and resulted in a poorer quality of life. This was a large study with rigorous, robust methodology. Unlike other studies, it does demonstrate that KRAS wild-type tumours respond more favourably than KRAS mutant tumours when cetuximab was used. However, neither group given cetuximab had a better outcome than those just received capecitabine, oxaliplatin and bevacizumab alone. This however may not be relevant to clinical practice owing to the multi-centred nature of this study in which practice may not be representative of UK clinical practice.
Survival
Finally a large observational study from two eminent academic centres in United States performed from 1996 to 2006 found significant improvement in the survival of patients in colorectal liver metastases in recent years.20 Kopetz et al. aimed to evaluate the changes in survival of patients with metastatic colorectal cancer using both multi-institutional and population-based databases and to associate these changes to hepatic resection utilization and temporal trends in improvements in chemotherapy.
No significant difference in median survival was noted from 1990 to 1997 with a median survival of 14.2 months; however, a significant improvement was seen over later years to a maximum of 29.2 months by 2004 to 2006 (P < 0.05). Five-year survival increased from 9.1% in 1990–1997, to 19.2% in 2001–2003, with proportional hazard modelling of survival predicting a 5-year survival of 32% from 2004–2006.
To establish the impact of chemotherapy and to exclude the influence of hepatic resections, overall survival was repeated after censoring patients with hepatic resections at the time of surgery. When reviewing chemotherapy agents in isolation, patients diagnosed in 2004–2006 had a significant improvement in their overall survival, with a hazard ratio of 0.53 (95% CI, 0.45 to 0.62; P < 0.001). The one noticeable difference during this time period was the introduction of cetuximab and becavizumab.
Advances in chemotherapy along with the introduction of cetuximab and bevacizumab have been attributed to this significant overall improvement. Although it may not be possible to isolate cetuximab, it does provide evidence that changes in clinical practice have substantially improved outcome. In reference to current clinical practice, it would suggest that optimization of current chemotherapy agents and the development of novel agents has improved survival overall; however, by excluding those patients with poor performance status this may in fact be an overestimation of survival.
Discussion
In summary, the management of colorectal liver metastases has significantly advanced within the last decade. Many changes are now established routine practice including the role of PET-CT scanning in pre-operative scanning, laparoscopic surgical resection and more aggressive resection with the definition of resectable disease being redefined.
Fifteen studies reviewed the clinical application of cetuximab in the first-line treatment of unresectable colorectal liver metastases, all of which were prospective. The main findings are summarised in Table 1. Seven studies also included sub-group analysis depending on KRAS mutational status, with only one study performing KRAS mutational status prospectively.
Table 1.
Summary of clinical findings of referenced papers
| Study | Description | Overall response | R0 resection | PFS (months) | OS (months) |
|---|---|---|---|---|---|
| OPUS (n = 337) Bokemeyer 2009 | Cetuximab | 46% | Not available | 7.2 | Not available |
| Without cetuximab | 36% | 7.2 | |||
| OPUS 2011 | Cetuximab | 46% | Not available | 7.2 | 18.3 |
| Without cetuximab | 36% | 7.2 | 18.0 | ||
| CELIM (n = 114) Folprecht 2010 | FOLFOX6 + Cetuximab | 68% | 38% | Not available | Not available |
| FOLFIRI + cetuximab | 59% | 30% | |||
| CRYSTAL (n = 1198) Van Cutsem 2009 | Cetuximab | 46.9% | 4.8% | 8.9 | 19.9 |
| Without cetuximab | 38.7% | 1.7% | 8.0 | 18.6 | |
| CRYSTAL Van Cutsem 2011 | Cetuximab | 57.3% | Not available | 9.9 | 23.5 |
| Without cetuximab | 39.7% | 8.4 | 20.0 | ||
| CECOG (n = 115) Ocvirk 2010 | Cetuximab | 40% | Not available | 8.6 | 17.4 |
| Without cetuximab | 36% | 8.3 | 18.9 | ||
| POCHER (n = 43) Garufi 2010 | Cetuximab | 79.1% | 60% | 14 | 37 |
| Without cetuximab | |||||
| MRC COIN (n = 1630) Maughan 2011 | Cetuximab | 64% | 15% | 8.6 | 17.9 |
| Without cetuximab | 57% | 13% | 8.6 | 17 | |
| MRC COIN (n = 1630) Adams 2011 | Cetuximab | Not available | Not available | 7.4 | 14.4 |
| Without cetuximab | 8.4 | 15.8 | |||
| Borner 2008 (n = 64) | Cetuximab | 54% | Not available | Not available | 20.5 |
| Without cetuximab | 35.1% | 16.5 | |||
| Tol 2009 (n = 755) | Cetuximab | 52.7% | Not available | 9.4 | 19.4 |
| Without cetuximab | 50% | 10.7 | 20.3 | ||
Studies such as OPUS and CRYSTAL have consistently demonstrated that the addition of cetuximab to standard first-line chemotherapy agents (FOLFOX and FOLFIRI) significantly improved progression-free survival, overall survival and surgical resection rates (grade B evidence), especially in the setting of KRAS wild-type tumours. Tumour response rates have been shown to be directly related to increased surgical resection rates. Although the absolute numbers of tumours that convert from unresectable to resectable remain low, there is a statistically significant increase, resulting in an increasing role for liver surgeons in the management of these patients.
However, the MRC COIN trial, the largest prospective trial performed in the UK, has cast doubt on the conclusions drawn from the previous evidence. With its robust methodology it found cetuximab did not have any additional benefit when combined with standard chemotherapy regimens (grade B evidence). The chemotherapy regimen used however largely differs to previously published studies, with XELOX being most commonly used; and this may in part explain the difference to previously published data. In addition to this, the study participants were largely palliative care patients with multiple sites of metastatic disease. The findings are therefore not representative of patients with liver only disease and cannot be directly applied to this subgroup. On further sub-analysis, it did however report that progression-free survival was more likely to be superior in patients with one site of metastatic spread only.
The majority of evidence suggested an overall benefit in adding cetuximab to standard chemotherapy treatment. This has usually been performed in a highly selected group of patients, especially those with one metastatic site, with the potential of making previously unresectable disease resectable.
To date, the clinical benefit of cetuximab has been studied extensively; however, in this modern era of economic decline it is also imperative to consider the cost effectiveness of such treatment in the NHS. The evidence reinforces the importance of optimizing treatment on an individual basis, especially depending on their tumour biology.
In conclusion, therefore, in the era of evidence-based medicine the literature does not support the routine use of cetuximab in the treatment of colorectal liver metastases. It does however highlight the need for the optimization of treatment on an individual basis, especially the use of cetuximab in KRAS wild-type tumours only. With the increasing response rates associated with cetuximab and the subsequent opportunity to make unresectable liver metastases resectable, this will potentially increase the role of liver surgeons in the management of these previously unresectable patients. Prior to a change in clinical practice, the cost-effectiveness of this treatment needs to be considered in more detail. At present the evidence is not robust enough to change routine clinical practice, and establish guidelines to include the use of cetuximab.
Conflicts of interest
None declared.
References
- 1.Office for National Statistics. Cancer registrations in England 2008. 21 October 2010. Available at: http://www.statistics.gov.uk/statbase/Product.asp?vlnk=8843 (last accessed 18 June 2011)
- 2.Geoghegan JG, Scheele J. Treatment of colorectal liver metastases. Br J Surg. 1999;86:158–169. doi: 10.1046/j.1365-2168.1999.01013.x. [DOI] [PubMed] [Google Scholar]
- 3.Giacchetti S, Itzhaki M, Gruia G, Adam R, Zidani R, Kunstlinger F, et al. Long-term survival of patients with unresectable colorectal cancer liver metastases following infusional chemotherapy with 5-fluorouracil, leucovorin, oxaliplatin and surgery. Ann Oncol. 1999;10:663–669. doi: 10.1023/a:1008347829017. [DOI] [PubMed] [Google Scholar]
- 4.McGrath JP, Capon DJ, Smith DH, Chen EY, Seeburg PH, Goeddel DV, et al. Structure and organization of the human Ki-ras proto-oncogene and a related processed pseudogene. Nature. 1999;304:501–506. doi: 10.1038/304501a0. [DOI] [PubMed] [Google Scholar]
- 5.Satlz LB, Lenz HJ, Kindler HL, Hochster HS, Wadler S, Hoff PM, et al. Randomised phase II trial of cetuximab, bevacizumab and irinotecan compared with cetuximab and bevacizumab alone in irinotecan-refractory colorectal cancer: the BOND-2 study. J Clin Oncol. 2007;25:4557–4561. doi: 10.1200/JCO.2007.12.0949. [DOI] [PubMed] [Google Scholar]
- 6.Folprecht G, Lutz MP, Schoffski P, Seufferlein T, Nolting A, Pollert P, et al. Cetuximab and irinotecan/5-fluorouracil/folinic acid is a safe combination for the first-line treatment of patients with epidermal growth factor receptor expressing metastatic colorectal carcinoma. Ann Oncol. 2006;17:450–456. doi: 10.1093/annonc/mdj084. [DOI] [PubMed] [Google Scholar]
- 7.Tabernero J, Van Cutsem E, Diaz-Rubio E, Cervantes A, Humblet Y, Andre T, et al. Phase II trial of cetuximab in combination with fluorouracil, leucovorin, and oxaliplatin in the first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2007;25:5225–5232. doi: 10.1200/JCO.2007.13.2183. [DOI] [PubMed] [Google Scholar]
- 8.Bokemeyer C, Bondarenko I, Makhson A, Hartmann JT, Aparicio J, de Braud F, et al. Fluorouracil, leucovorin and oxaliplatin with or without cetuximab in the first line treatment of metastatic colorectal cancer. J Clin Oncol. 2009;27:663–671. doi: 10.1200/JCO.2008.20.8397. [DOI] [PubMed] [Google Scholar]
- 9.Bokemeyer C, Bondarenko I, Hartmann JT, de Braud F, Schuch G, Zubel A, et al. Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann Oncol. 2011;22:1535–1546. doi: 10.1093/annonc/mdq632. [DOI] [PubMed] [Google Scholar]
- 10.Folprecht G, Gruenberger T, Bechstein WO, Raab HR, Lordick F, Hartmann JT, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomized phase 2 trial. Lancet Oncology. 2010;11:38–47. doi: 10.1016/S1470-2045(09)70330-4. [DOI] [PubMed] [Google Scholar]
- 11.Van Cutsem E, Kohne CH, Hitre E, Zaluski J, Chang Chien CR, Makhson A, et al. Cetuximab and chemotherapy as an initial treatment of metastatic colorectal cancer. NEJM. 2009;360:1408–1417. doi: 10.1056/NEJMoa0805019. [DOI] [PubMed] [Google Scholar]
- 12.Van Cutsem E, Kohne CH, Lang I, Folpreht G, Nowacki MP, Cascinu S, et al. Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumour KRAS and BRAF mutation status. J Clin Oncol. 2011;29:2011–2019. doi: 10.1200/JCO.2010.33.5091. [DOI] [PubMed] [Google Scholar]
- 13.Ocvirk J, Brodowicz T, Wrba F, Ciuleanu TE, Kurteva G, Beslija S, et al. Cetuximab and FOLFOX 6 or FOLFIRI in metastatic colorectal cancer: CECOG trial. World J Gastroenterol. 2010;16:3133–3143. doi: 10.3748/wjg.v16.i25.3133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garufi C, Torsello A, Tumolo S, Ettorre GM, Zeuli M, Campanella C, et al. Cetuximab plus chronomodulated irinotecan, 5-fluorouracil, leucovorin and oxaliplatin as neoadjuvant chemotherapy in colorectal liver metastases: POCHER trial. Br J Cancer. 2010;103:1542–1547. doi: 10.1038/sj.bjc.6605940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maughan TS, Adams RA, Smith CG, Meade AM, Seymour MT, Wilson RH, et al. Addition of cetuximab to oxaliplatin-basec first line combination chemotherapy for the treatment of advanced colorectal cancer: results of a randomized phase 3 MRC COIN trial. Lancet. 2011;377:2103–2114. doi: 10.1016/S0140-6736(11)60613-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adams R, Meade AM, Seymour MT, Wilson RH, Madi A, Fisher D, et al. Intermittent versus continuous oxaliplatin and fluoropyrimidine combination chemotherapy for first-line treatment of advanced colorectal cancer: results of the randomized phase 3 MRC COIN trial. Lancet Oncology. 2011;12:642–653. doi: 10.1016/S1470-2045(11)70102-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Borner M, Koeberle D, Von Moos R, Saletti P, Rauch D, Hess V, et al. Adding cetuximab to capecitabine plus oxaliplatin (XELOX) in first-line treatment of metastatic colorectal cancer: a randomized phase II trial of the Swiss group for clinical cancer research SAKK. Ann Oncol. 2008;19:1288–1292. doi: 10.1093/annonc/mdn058. [DOI] [PubMed] [Google Scholar]
- 18.Tol J, Koopman M, Rodenburg CJ, Cats A, Creemers GJ, Schrama JG, et al. A randomized phase III study on capecitabine, oxaliplatin and bevacizumab with or without cetuximab in first-line advanced colorectal cancer, the CAIRO2 study of the Dutch Colorectal Cancer Group (DCCG). An interim analysis of toxicity. Ann Oncol. 2008;19:734–738. doi: 10.1093/annonc/mdm607. [DOI] [PubMed] [Google Scholar]
- 19.Tol J, Koopman M, Cats A, Rodenburg CJ, Creemers GJ, Schrama JG, et al. Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. NEJM. 2009;360:563–572. doi: 10.1056/NEJMoa0808268. [DOI] [PubMed] [Google Scholar]
- 20.Kopetz S, Cahng GJ, Overman MJ, Eng C, Sargent DJ, Larson DW, et al. Improved survival in metastatic colorectal cancer is associated with the adoption of hepatic resection and improved chemotherapy. Journal of Clin Oncology. 2009;27:3677–3683. doi: 10.1200/JCO.2008.20.5278. [DOI] [PMC free article] [PubMed] [Google Scholar]


