Abstract
Objective: The purpose of this study was to compare optical coherence tomography (OCT) with the existing technologies, to assess its accuracy and utility in detecting vertical root fractures of extracted human teeth. Background data: The detection of root fractures in teeth that have undergone root canal treatment is challenging because of the great difficulty in differentiating these fractures from morphologic or radiographic anomalies. OCT methods are based on depth-resolved optical reflectivity and have been developed to reduce the invasiveness and radiation exposure inherent to other techniques. Methods: Twelve extracted human mandibular teeth (totaling 25 roots) that were free of caries, calculus, and root treatment were used, and assessed by microfocus computed tomography, the current gold standard for fracture detection. The ability of appropriately trained observers to detect root fractures using visual, microscopic, and swept-source OCT (SS-OCT) techniques were compared. micro-CT and SS-OCT produce three-dimensional images of the tooth from which to diagnose fractures, but CT scanning involves radiation exposure that is not required in SS-OCT. Results: Seventeen of the 25 roots were found to have fractures by microfocus CT. These findings were replicated by SS-OCT, which revealed fractures exhibiting identical origin, size, and angulation within the root. We found that SS-OCT gave results compatible to the gold standard technique, and that SS-OCT and microscopy were more effective for identifying root fractures than was visual observation alone. Conclusions: SS-OCT may represent a novel, noninvasive, noncontact and nonexposure alternative to the conventional methods used for assessing root fractures in teeth.
Introduction
Diagnosis of vertical root fractures (VRF) in endodontically treated teeth has long been very challenging.1 The clinical signs, symptoms, and radiographic appearances of VRF frequently resemble periapical and marginal periodontitis, and the diagnosis of VRF can be made only by the observation of a fracture line by direct visual, dental loupe, or dental microscope inspection with or without surgical exploration.1,2 Existing diagnostic techniques such as the discovery of a periapical “halo” lesion in dental radiographs or localized deep periodontal pocketing are often rather subjective.3–6 Radiographic images reveal root fractures only if the X-ray beam is parallel to the fracture line, and the array of patterns of radiolucencies around affected roots that can arise from VRF makes diagnosis very difficult.7,8
Cone-beam computed tomography (CBCT) is a useful option for the detection of root fractures. The use of high resolution has been recommended for suspected cases of longitudinal root fracture.9 However, this increases scanning times and, therefore, patient radiation exposure.10 Moreover, the presence of metal posts or filling materials reduces its diagnostic capacity because these artifacts may appear in a radial fashion.11 Therefore, the narrow fractures are difficult to detect by CBCT in clinical practice.
In conventional endodontics, much information can be gleaned by applying methylene blue dye to the root canal and observing it under a microscope. However, because the dentin cannot be evaluated in depth, it is difficult to distinguish between a true VRF and nonpathologic root morphologies such as fins, grooves, and isthmuses. Surgical diagnosis is performed when a fracture is suspected in prosthetic teeth after root canal treatment, but the diagnosis and area identification of incomplete fractures remain challenging.12
Optical coherence tomography (OCT) is a new diagnostic method for creating high-resolution cross-sectional imaging of the internal biological structures based on depth-resolved optical reflectivity.13 OCT exploits the coherent behaviors of light. The light is split into two arms, the sample arm and a reference mirror, and these couple a low coherence light into a Michelson interferometer. When reflections from the reference mirror and backscattered light from the sample are recoupling, an interference signal is detected within the coherence length of the source. Swept-source optical coherence tomography (SS-OCT) was developed as an extension of OCT. SS-OCT combines a narrow line-width laser rapidly sweeping through a broad optical bandwidth with an immediate depth scan calculation using the Fourier transform with reduced noise.14
In endodontics, OCT is a proven and reliable method for nondestructively assessing intracanal anatomy, cleanliness of the root canal after preparation, root perforations, and, importantly, VRF caused by vertical pressure exerted by, for example, overzealous use of the spreader.7,15 The aim of this study was to evaluate the accuracy of SS-OCT in comparison with direct visual and dental microscopic inspection in detecting VRFs of extracted human teeth.
Materials and Methods
All experiments in this study complied with the guidelines of the Ethical Review Board of Tokyo Medical and Dental University.
Tooth selection
Twelve extracted human mandibular molars with no caries, dental calculus, or root canal treatment were used in this study. The teeth were stored in water containing a few crystals of thymol at room temperature. Twenty-five roots were evaluated (one tooth had three roots). The observation area defined for this study was the root surface (excluding the bifurcation side) from the apex to the cervical line.
Determination of VRF by gold standard technology
The presence of root fractures was determined by two observers using microfocus CT scanning (inspeXio SMX100CT®, Shimadzu, Kyoto, Japan) with exposure parameters set at 100 kV and 40 μA. The resolution was increased until the observers reached a consensus. Seventeen roots were determined as fractured and eight roots were shown intact. Voxel size of the microfocus CT scan image was 5–20 μm.
Diagnosis of VRF
The examiners in the present study were three clinicians trained in microscope-assisted root canal treatment at Tokyo Medical and Dental University Dental Hospital. Teeth were diagnosed by visual judgment (VJ), microscope (MS) and OCT. For VJ, after drying the tooth surface with a paper towel, direct visual inspection was performed under artificial light, without dyeing, probing, or magnification, and at a distance of at least 20 cm. For MS, the tooth surface was dried with a paper towel and observed using a dental microscope (OPMI® pico, Carl Zeiss, Germany) under halogen light at 12 V and 100 W, and the total magnification (eye lens×objective lens) was set to be 13.6 times. For OCT, we used the SS-OCT (Santec OCT-2000®, Santec, Komaki, Japan; Fig. 1) with a light source that repetitively sweeps the wavelengths from 1260 to 1360 nm at a 20 kHz sweep rate. Laser power was<10 mW within the American National Standards Institute limit. Axial resolution of the system was 11 μm in air, which corresponds to 8 μm in soft tissue and 6.8 μm in enamel. A 240×240×400 pixel three-dimensional (3D) image (4×4×3.2 mm) could be acquired within 4 sec, including data acquisition and process time. 3D scans were performed using the SS-OCT to a maximum of six times per tooth. 3D image processing software (Amira5.3®, Visage Imaging, Austria) was used for 3D formulation imaging and cross-sectional imaging of the teeth. The diagnosis of each tooth was made with this software on a liquid crystal display (Pro Lite E2710HDS; IIYAMA) at 1920×1080 pixel resolution on a desktop computer (MDV-ADG9160X2, MouseComputer, Tokyo, Japan). Examiners were trained for the system using the software to diagnose five extracted teeth that were not included in the main study.
FIG. 1.
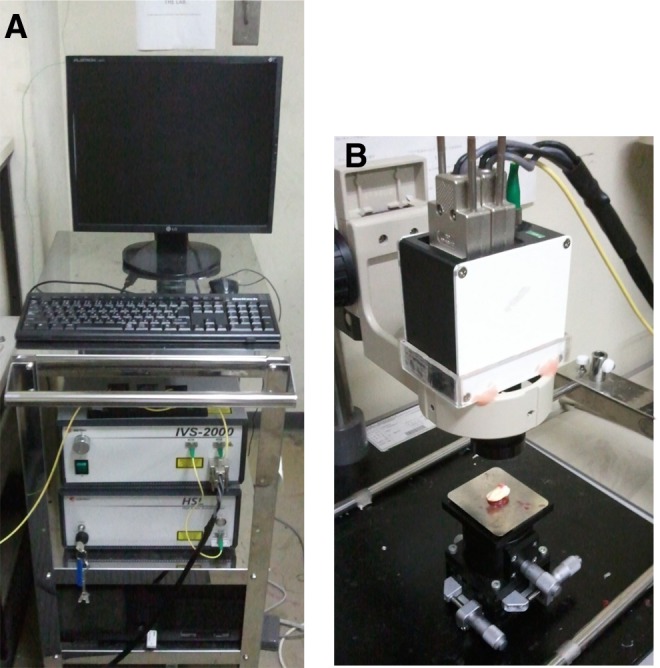
(A) Optical coherence tomography (OCT) system including screen, Mach-Zehnder interferometer, scanning laser source and data processing PC. (B) Sample arm incorporating scanning laser and manually adjustable stage to facilitate scanning of the sample.
Statistical analysis
Statistical analysis was performed using SPSS STATICS v17.0 software (SPSS Inc, Chicago, IL). Sensitivity, specificity, accuracy rate, and positive (PPV) and negative (NPV) predictive values were determined. Analysis of variance test, Tukey's HSD test and χ2 test were performed at a significance level of 5%. For each diagnosis, inter-examiner agreement was assessed by κ statistics.
Results
OCT detected fracture lines at the same location, angle, and line of development as the microfocus CT scan (Figs. 2 and 3). The root canal presented as a dark round area (Fig. 2B), whereas the fracture line was observed as a bright line falling short of the root canal (Fig. 2A). Fracture lines also appeared as bright bifurcating lines that terminated within the dentin (Fig. 3A). Values for the sensitivity, specificity, accuracy rate, PPV, NPV, and κ values are shown in Table 1. The sensitivity, accuracy rates and NPV of OCT and MS were significantly higher than those of VJ. No statistically significant differences were found for specificity, PPV, or κ value among the three groups.
FIG. 2.
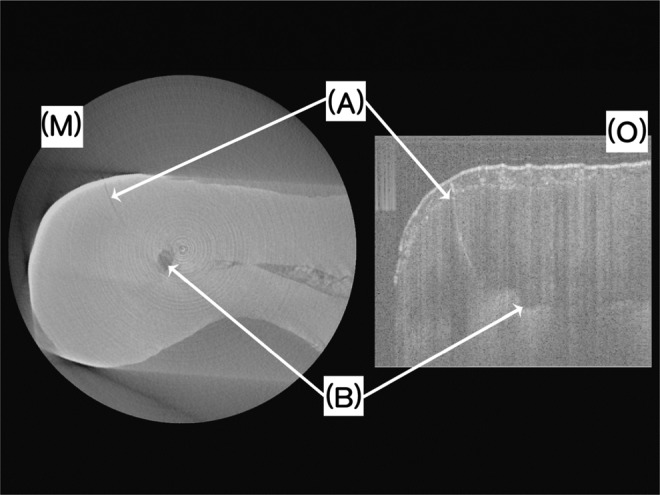
Fracture line (A) and root canal (B) observed by microfocus CT scan (M) and optical coherence tomography (OCT) (O), respectively.
FIG. 3.
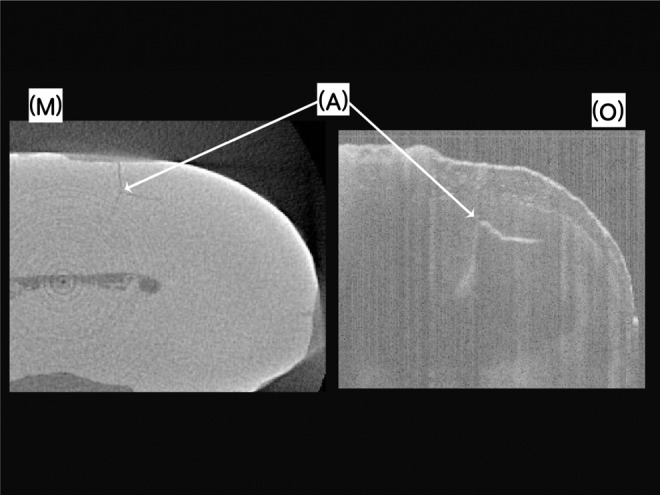
Bifurcate fracture line (A) observed by microfocus CT scan (M) and optical coherence tomography (OCT) (O), respectively.
Table 1.
Measurement Parameters for Three Analysis Techniques
| |
|
|
|
|
|
κ Value (each pair of examiners) |
||
|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | Accuracy rate | PPV | NPV | 1 vs 2 | 1 vs 3 | 2 vs 3 | |
| VJ | 0.49a | 0.92 | 0.63c | 0.93 | 0.63 | 0.58 | 0.50 | 0.46 |
| MS | 0.86b | 0.88 | 0.87d | 0.94 | 0.75 | 0.50 | 0.65 | 0.55 |
| OCT | 0.90b | 0.88 | 0.89d | 0.94 | 0.81 | 0.77 | 0.62 | 0.53 |
Different letters indicate a statistically significant difference at the 5% level.
VJ, visual judgment; MS, microscope; OCT, optical coherence tomography; PPV, positive predictive value; NPV, negative predictive value.
Discussion
In medical fields, OCT is used in ophthalmology to image the retina, in cardiovascular medicine to visualize the inner wall of a blood vessel, in digestive surgery to view the gastric mucosa, and in dermatology to assess basal cell carcinoma.16–18 The use of OCT in retinal imaging is its most successful clinical application because it enables the real-time, in situ visualization of tissue microstructure without the need to excise and process specimens as in conventional biopsy and histopathology.19 In cardiovascular internal medicine, atherosclerosis of the coronary artery can be diagnosed by OCT with a resolution 10 times higher than that of intravascular ultrasound.20
In dentistry, SS-OCT can evaluate the presence of bubbles within the resin-based composite restorations, and detect gaps in the restoration–tooth interface and failures in the adaptation of restorations.21 The combination of SS-OCT and a contrast agent enabled the detection of microgaps at the tooth–restoration interface with high sensitivity.14 SS-OCT is a promising diagnostic modality for the detection of early occlusal caries and interior defects in dentures.22,23 SS-OCT enables visualization and segmentation of the lower labial glands for diagnosis of Sjögren's syndrome and xerostomia and oral vascular lesions, for selection of the most appropriate treatment.24,25 OCT imaging of suspicious oral lesions could improve the accuracy of diagnoses of oral dysplasia, and clarify the distinction between cancerous and noncancerous lesions.26 OCT was shown to be able to prevent iatrogenic exposures of the pulp, complementing other existing methods and permitting a more predictive prognosis of treatment. OCT can also be used to monitor dentin bridge formation, thus yielding extra information on the success of pulp capping therapy.27
Previously, diagnostic imaging has been used to demonstrate the existence of wide fracture lines in teeth, which were concluded to have been caused by the application of physical pressure during endodontic treatment.28,29 However, in the present study, we have found that narrower fracture lines can be detected by microfocus CT in teeth that have not been subjected to endodontic treatment. It is unknown when these fractures were occurred (e.g., before extraction, caused by procedures of extraction, or arose during storage). Seventeen of 25 roots in 12 extracted teeth, to which no intentional force had been applied, showed confirmed fracture lines. These teeth would have been included in previous experiments using extracted teeth as a “non-fractured” sample and would have adversely affected the results. Therefore, for the future, we recommend that extracted teeth should be checked for narrower fractures by OCT or microfocus CT scan when teeth are used for in vitro study.
The teeth that were diagnosed as fractured were almost extracted, so PPV is an important value in this study. The specificity and PPV of three diagnosis methods had very high accuracy. The sensitivity and NPV of VJ were lower than those of MS and OCT, in other words, the fractures were often overlooked by VJ. In this study, fracture lines were observed by OCT in an in vitro setting, and the observation area was limited to the root surface. Therefore, the expected clinical condition is that root observation depends on root exposure caused either by gingival recession or by surgical intervention raising a flap. If the development area of the fracture is confirmable by OCT, correct treatment could be decided. The usefulness of OCT must be confirmed in clinical practice in vivo. The clinical advantages of OCT are that it is a noncontact, noninvasive, real-time display and nonexposure technique; therefore, OCT can be repeated as many times as desired. It is suggested to perform OCT before the prosthesis as a screening of root fracture. OCT is an objective diagnostic method, but frequently shows artifacts parallel to the direction of the laser radiation that can resemble fracture lines.30 However, continuous slice images were able to distinguish between these artifacts and true fracture lines. OCT is able to generate a detailed evaluation of the internal structure of the tooth and the extent of the fracture line within the dentin boundaries (i.e., the root surface and the canal wall). The training was conducted in advance, but the diagnosis of this study was the first diagnosis using OCT by the three examiners. If they gain experience, the accuracy rate will increase.
Conclusions
Within the limitations of this in vitro study, we conclude that the validity and reliability of OCT for detecting the presence of root fracture is comparable to that with a dental microscope.
Acknowledgments
This work was supported by a Research Grant for Longevity Sciences (23-20) from the Ministry of Health, Labour and Welfare and a Grant-in-Aid for Scientific Research (B) (No. 23390432) from the Japan Society for the Promotion of Science.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Tamse A. Iatrogenic vertical root fractures in endodontically treated teeth. Endod. Dent. Traumatol. 1988;4:190–196. doi: 10.1111/j.1600-9657.1988.tb00321.x. [DOI] [PubMed] [Google Scholar]
- 2.Kawamura-Hagiya Y. Yoshioka T. Suda H. Logistic regression equation to screen for vertical root fractures using periapical radiographs. Dentomaxillofac. Radiol. 2008;37:28–33. doi: 10.1259/dmfr/25198672. [DOI] [PubMed] [Google Scholar]
- 3.Nicopoulou-Karayianni K. Bragger U. Patrikiou A. Stassinakis A. Lang N.P. Image processing for enhanced observer agreement in the evaluation of periapical bone changes. Int. Endod. J. 2002;35:615–622. doi: 10.1046/j.1365-2591.2002.00526.x. [DOI] [PubMed] [Google Scholar]
- 4.Gelfand M. Sunderman E.J. Goldman M. Reliability of radiographic interpretations. J. Endod. 1983;9:71–75. doi: 10.1016/S0099-2399(83)80079-X. [DOI] [PubMed] [Google Scholar]
- 5.Goldman M. Pearson A.H. Darzenta N. Endodontic success – who's reading the radiograph? Oral Surg. Oral Med. Oral Pathol. 1972;33:432–437. doi: 10.1016/0030-4220(72)90473-2. [DOI] [PubMed] [Google Scholar]
- 6.Reit C. Gröndahl H.G. Endodontic retreatment decision-making among a group of general practitioners. Scand. J. Dent. Res. 1988;96:112–117. doi: 10.1111/j.1600-0722.1988.tb01416.x. [DOI] [PubMed] [Google Scholar]
- 7.Shemesh H. Van Soest G. Wu M.K. Wesselink P.R. Diagnosis of vertical root fractures with optical coherence tomography. J. Endod. 2008;34:739–742. doi: 10.1016/j.joen.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Tamse A. Fuss Z. Lustig J. Ganor Y. Kaffe I. Radiographic features of vertically fractured, endodontically treated maxillary premolars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999;88:348–352. doi: 10.1016/s1079-2104(99)70041-7. [DOI] [PubMed] [Google Scholar]
- 9.Melo S.L. Bortoluzzi E.A. Abreu M., Jr Corrêa L.R. Corrêa M. Diagnostic ability of a cone-beam computed tomography scan to assess longitudinal root fractures in prosthetically treated teeth. J. Endod. 2010;36:1879–1882. doi: 10.1016/j.joen.2010.08.025. [DOI] [PubMed] [Google Scholar]
- 10.Liedke G.S. Silveira H.E.D. Silveira H.L.D. Dutra V. Figueiredo J.A.P. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J. Endod. 2009;35:233–235. doi: 10.1016/j.joen.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 11.Youssefzadeh S. Gahleitner A. Dorffner R. Bernhart T. Kainberger F.M. Dental vertical root fractures: value of CT in detection. Radiology. 1999;210:545–549. doi: 10.1148/radiology.210.2.r99ja20545. [DOI] [PubMed] [Google Scholar]
- 12.Tamse A. Zilburg I. Halpern J. Vertical root fractures in adjacent maxillary premolars: an endodontic-prosthetic perplexity. Int. Endod. J. 1998;31:127–132. doi: 10.1046/j.1365-2591.1998.00129.x. [DOI] [PubMed] [Google Scholar]
- 13.Huang D. Swanson E.A. Lin C.P., et al. Optical coherence tomography. Science. 1991;254:1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Makishi P. Shimada Y. Sadr A. Tagami J. Sumi Y. Non-destructive 3D imaging of composite restorations using optical coherence tomography. J. Dent. 2011;39:316–325. doi: 10.1016/j.jdent.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Shemesh H. van Soest G. Wu M.K. van der Sluis L.W. Wesselink P.R. The ability of optical coherence tomography to characterize the root canal walls. J. Endod. 2007;33:1369–1373. doi: 10.1016/j.joen.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 16.Zuccaro G. Gladkova N. Vargo J., et al. Optical coherence tomography of the esophagus and proximal stomach in health and disease. Am. J. Gastroenterol. 2001;96:2633–2639. doi: 10.1111/j.1572-0241.2001.04119.x. [DOI] [PubMed] [Google Scholar]
- 17.Cunha D. Richardson T. Sheth N. Orchard G. Coleman A. Mallipeddi R. Comparison of ex vivo optical coherence tomography with conventional frozen-section histology for visualizing basal cell carcinoma during Mohs micrographic surgery. Br. J. Dermatol. 2011;165:576–580. doi: 10.1111/j.1365-2133.2011.10461.x. [DOI] [PubMed] [Google Scholar]
- 18.Pomerantz R. Zell D. McKenzie G. Siegel D.M. Optical coherence tomography used as a modality to delineate basal cell carcinoma prior to Mohs micrographic surgery. Case. Rep. Dermatol. 2011;3:212–218. doi: 10.1159/000333000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fujimoto J.G. Optical coherence tomography for ultrahigh resolution in vivo imaging. Nat. Biotechnol. 2003;21:1361–1367. doi: 10.1038/nbt892. [DOI] [PubMed] [Google Scholar]
- 20.Kang S.J. Mintz G.S. Akasaka T., et al. Optical coherence tomographic analysis of in-stent neoatherosclerosis after drug–eluting stent implantation. Circulation. 2011;123:2954–2963. doi: 10.1161/CIRCULATIONAHA.110.988436. [DOI] [PubMed] [Google Scholar]
- 21.Ishibashi K. Ozawa N. Tagami J. Sumi Y. Swept-source optical coherence tomography as a new tool to evaluate defects of resin-based composite restorations. J. Dent. 2011;39:543–548. doi: 10.1016/j.jdent.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 22.Shimada Y. Sadr A. Burrow M.F. Tagami J. Ozawa N. Sumi Y. Validation of swept-source optical coherence tomography (SS-OCT) for the diagnosis of occlusal caries. J. Dent. 2010;38:655–665. doi: 10.1016/j.jdent.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 23.Sumi Y. Ozawa N. Nagaosa S. Minakuchi S. Umemura O. Application of optical coherence tomography to nondestructive inspection of dentures. Arch. Gerontol. Geriatr. 2011;53:237–241. doi: 10.1016/j.archger.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 24.Ozawa N. Sumi Y. Shimozato K. Chong C. Kurabayashi T. In vivo imaging of human labial glands using advanced optical coherence tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009;108:425–429. doi: 10.1016/j.tripleo.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 25.Ozawa N. Sumi Y. Chong C. Kurabayashi T. Evaluation of oral vascular anomalies using OCT imaging. Br. J. Oral Maxillofac. Surg. 2009;47:622–626. doi: 10.1016/j.bjoms.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 26.Jerjes W. Upile T. Conne B., et al. In vitro examination of suspicious oral lesions using optical coherence tomography. Br. J. Oral Maxillofac. Surg. 2010;48:18–25. doi: 10.1016/j.bjoms.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 27.Braz A.K. Kyotoku B.C. Gomes A.S. In vitro tomographic image of human pulp-dentin complex: optical coherence tomography and histology. J. Endod. 2009;35:1218–1221. doi: 10.1016/j.joen.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 28.Ozer S.Y. Detection of vertical root fractures of different thicknesses in endodontically enlarged teeth by cone beam computed tomography versus digital radiography. J. Endod. 2010;36:1245–1249. doi: 10.1016/j.joen.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 29.Hassan B. Metska M.E. Ozok A.R. van der Stelt P. Wesselink P.R. Detection of vertical root fractures in endodontically treated teeth by a cone beam computed tomography scan. J. Endod. 2009;35:719–722. doi: 10.1016/j.joen.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 30.Antony B. Abràmoff M.D. Tang L., et al. Automated 3-D method for the correction of axial artifacts in spectral-domain optical coherence tomography images. Biomed. Opt. Express. 2011;2:2403–2416. doi: 10.1364/BOE.2.002403. [DOI] [PMC free article] [PubMed] [Google Scholar]


