Abstract
Following the Five Year Measles Elimination Program, measles has been declared eliminated from the Republic of Korea since 2006. However, there remain challenges related to the surveillance of measles in the postelimination phase. Even though the routine surveillance system has revealed a gradual decrease in the number of reported cases since 2002, 4 resurgences have occurred, notably due to outbreaks. Because vaccine-modified measles is becoming widespread due to high vaccination coverage, conducting laboratory confirmation in each case becomes important. Moreover, susceptible individuals with measles have been identified through seroprevalence studies. Lastly, the efforts to improve the timeliness of measles reporting have led to the establishment of an active laboratory-based surveillance network, which has shortened the interval between diagnosis and notification. In these circumstances, searching for more sensitive and effective surveillance measures is important for maintaining the elimination status and preventing future outbreaks of measles in Korea.
Keywords: Measles, Epidemiology, Korea
Background
Measles is a highly contagious disease that causes substantial disease burden in children worldwide. Although it is rare in South Korea presently, hospitalization for measles and its complications was common before the widespread use of the vaccine1-3). Furthermore, severe complications of measles can occur in susceptible subjects; in the 1960s, measles was one of the 10 leading causes of death in Korean children4). At the time of the installation of the national surveillance system in 1955, the annual number of reported measles cases ranged from 9,400 to 30,000; the number has been decreasing since the 1960s5). The introduction of measles monovalent vaccine in 1965 and the measles-mumps-rubella (MMR) vaccine in 1980 has played an important role in the decline in the number of reported cases. However, occasional outbreaks in cyclic patterns continued to occur every 3 to 4 years, due to poor routine vaccination coverage6,7). Although 1 dose of MMR vaccine given at 15 months of age was partly introduced into the National Immunization Program in 1985, the outbreak in 1989-1990, which affected approximately 5,000 patients, prompted the government and academia to take action8). During the outbreak, the peak incidence occurred among young children; therefore, since 1994, the Korean Pediatric Society has recommended that a second dose of MMR vaccine should be given at 6 years of age, and the same recommendation was issued by the government 3 years later8-10). Following the recommendation, the number of reported cases had decreased to less than 100 cases annually by the late 1990s. However, an unexpected nationwide outbreak involving 55,707 cases and 7 deaths occurred in 2000-200111). In response, the government instituted the Five Year Measles Elimination Program, which included the following: 1) a catch-up campaign targeting approximately 5 million school-aged children; 2) a keep-up vaccination program that required children to be certified as having received 2 doses of MMR vaccine before they could enter elementary school; and 3) an enhanced case- and laboratory-based measles surveillance system12,13). Following the installation of these programs, the annual measles incidence has declined to less than 1/100,000 of the population, and in 2006, the Republic of Korea became the first country in the Western Pacific Region (as defined by the World Health Organization) to declare measles as eliminated.
Despite this achievement, sporadic cases and outbreaks have been detected by the measles surveillance system. With the reduction in the number of children affected by measles, changes in the epidemiology of the disease are to be expected, as has been experienced in other countries14,15). To maintain the elimination status of measles in Korea, ongoing efforts are needed to meet the goals of: 1) high vaccination coverage for 2 doses of MMR vaccine, and 2) building effective measles surveillance strategies16,17). In this review, we have focused on the challenges related to the surveillance of measles during the post-elimination phase in Korea. Further, we have described the public health approaches that have provided the framework for the surveillance of measles that has been operating in Korea for the last 10 years.
Summary of measles case-based surveillance results (2002-2011)
Korea's routine surveillance system is an important tool for monitoring and interpreting the country's measles control measures. Since 1995, the mandatory reporting of suspected measles cases (those with fever, rash, and 1 of cough, coryza, and conjunctivitis [3C]) was required from physicians. A suspected case of measles must be reported to the public health centers or directly to the Korea Centers for Disease Control and Prevention (KCDC) through the electronic reporting system. The electronic reporting system was established in 2001 to enable timely reporting of suspected cases18). In general, the Korean National Notifiable Disease Surveillance System operates a passive surveillance scheme with supplementary case-based investigation performed for all reported cases of measles.
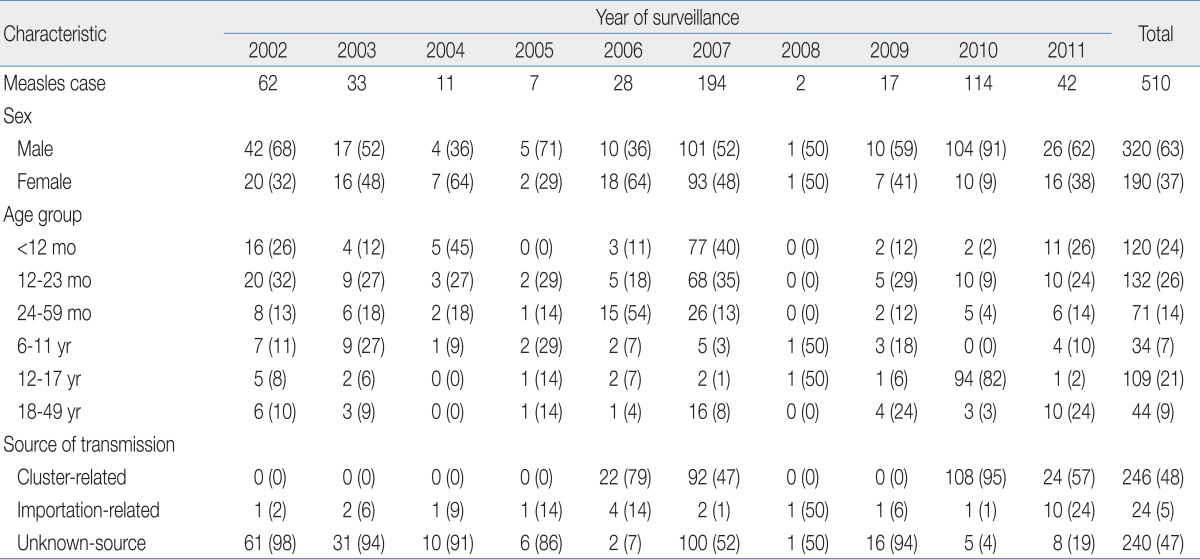
From 2002 to 2011, a total of 510 suspected measles cases were reported to the KCDC (Table 1). There was a gradual decrease from 2002 to 2005; however, resurgence was observed in 2006, 2007, 2010, and 2011. The increase in reported cases in each of these 4 years mainly resulted from measles outbreaks.
Table 1.
Demographic and Epidemiologic Characteristics of Measles Case-Patients, by Surveillance Year, Republic of Korea, 2002-2011
Values are presented as number (%).
Adapted from Korea Centers for Disease Control and Prevention (unpublished data).
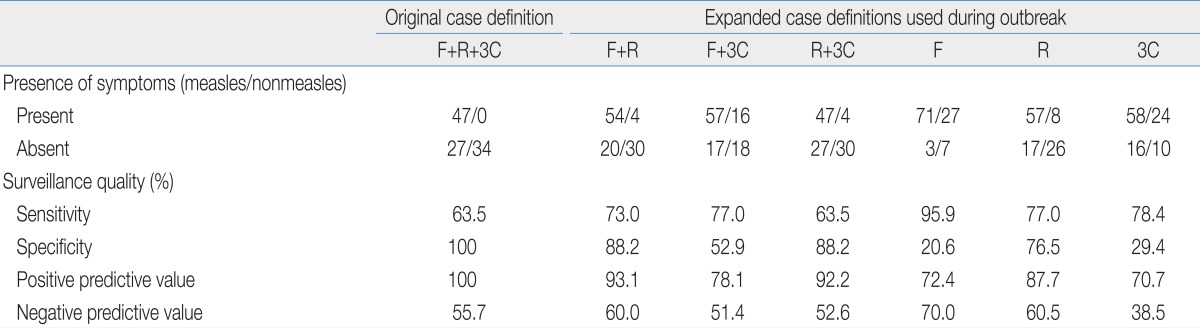
The first outbreak occurred in a preschool in Incheon and involved 15 confirmed cases from 152 exposed students. Among those 15 patients, 14 had received fewer than 2 doses of MMR vaccine, and measles affected 100% of children with no vaccination history19). Following the outbreak, the importance of maintaining high 2-dose MMR vaccination coverage and keeping accurate vaccination status records was emphasized. The second incident occurred in 2007, when multiple transmission chains of measles were identified, mainly in hospital settings20). Among 180 confirmed measles cases, 81 (45%) resulted from nosocomial transmission in 6 hospitals, mostly located in Seoul and its metropolitan area. More importantly, 124 cases (69%) did not have a history of MMR vaccination. This incident helped to improve the understanding of measles transmission in healthcare settings and how it is related to community transmission; the implication was that nosocomial transmission of measles may precipitate the ongoing spread in the community setting. Thirdly, a school outbreak in Incheon in 2010 involved 127 suspected cases from 878 exposed students (unpublished data, KCDC). Through the evaluation of symptoms and signs of affected students who had received MMR vaccination, the magnitude of vaccine-modified measles was recognized (Table 2). Among 74 vaccine-modified measles cases, only 64% met the original measles case definition; nearly 23% of patients did not present any signs of rash during the surveillance period. Lastly, in 2011, Gyeongnam Province reported multiple measles transmissions in hospitals and preschools, resulting in 32 confirmed measles cases (unpublished data, KCDC). Molecular analysis of measles virus isolates from 11 patients revealed the same D9 genotype in each, and these were the first of this genotype to be reported in Korea (the genotype is prevalent in neighboring Asian countries)21,22). The role of virological assessment in measles surveillance activities was consequently emphasized.
Table 2.
Sensitivity, Specificity, Positive Predictive Value, and Negative Predictive Value of Different Combination of Signs and Symptoms for Vaccine-Modified Measles Cases Identified in a School Outbreak in Incheon, Republic of Korea, 2010
F, fever; R, rash; 3C, more than one of cough, coryza, or conjunctivitis.
Adapted from Korea Centers for Disease Control and Prevention (unpublished data).
Although shifts in the epidemiology of infectious diseases are observed following an increase in vaccination coverage, our surveillance data did not show a noticeable age-related-shift among reported cases during the last 10 years. However, there were small differences in the proportions of certain age groups being infected in certain years. For example, 82% of cases in 2010, among subjects aged 12 to 17 years, were mostly reported from a junior high school-based outbreak (Table 1). The proportion of cases with an unidentified source of transmission has decreased from 98% in 2002 to 19% in 2012. This suggests an improvement in the power to detect the transmission linkage of individual cases. Nonetheless, further efforts to improve measles surveillance will allow earlier detection of sporadic measles cases and may eventually prevent the occurrence of outbreaks in Korea.
Modified measles: importance of laboratory confirmation
The success of measles surveillance is largely dependent on laboratory confirmation of suspected cases. With the low incidence of measles in Korea, suspecting the disease and making a clear diagnosis in patients with morbilliform rash is more difficult than it was 15 years ago, because recently trained pediatricians have had fewer opportunities to observe measles patients during their training periods. Therefore, the clinical diagnosis of measles has become unreliable in the postelimination era in Korea, as has been the case in other countries23). Moreover, understanding the magnitude of vaccine-modified measles is important because high vaccination coverage may result in disease burden in patients with primary or secondary vaccine failure. The current measles surveillance system defines a suspected measles case as an illness characterized by the presence of all the following features: morbilliform rash; fever above 38.0℃; and 1 or more of 3C. However, it is possible that this definition is inadequately sensitive for capturing all cases of measles, especially vaccine-modified cases. An outbreak that occurred in a school in 2010 has provided us with an opportunity to examine the performance of the original case definition, and highlights the importance of laboratory confirmation in individual cases.
The outbreak occurred in an all-male junior high school located in Incheon, and involved nearly 15% of the 878 students. Using a standardized questionnaire, an epidemiologic investigation using a retrospective cohort design was conducted, and the study described the sensitivity, specificity, positive predictive value, and negative predictive value of different combinations of signs and symptoms for vaccine-modified measles. All suspected cases had serum and throat swab specimens taken for laboratory confirmation.
Among the 74 vaccine-modified measles cases, the original case definition showed overall sensitivity of 63.5% and specificity of 100.0% (Table 2). An expanded case definition combining fever and rash showed higher sensitivity than the original case definition (72.9%), but lower specificity (88.2%). The presence of fever and 1 or more of 3C had the highest sensitivity among the combinations of signs and symptoms (77.0%), but it had the lowest specificity (52.9%).
These findings suggest that Korean physicians who encounter vaccine-modified measles may not diagnose or report the case as measles, because not all cases meet the definition for suspected measles. This implication is not dissimilar to that of reports from the United States and other countries24,25). Therefore, conducting laboratory confirmation in each case is necessary in Korea during the post-elimination phase.
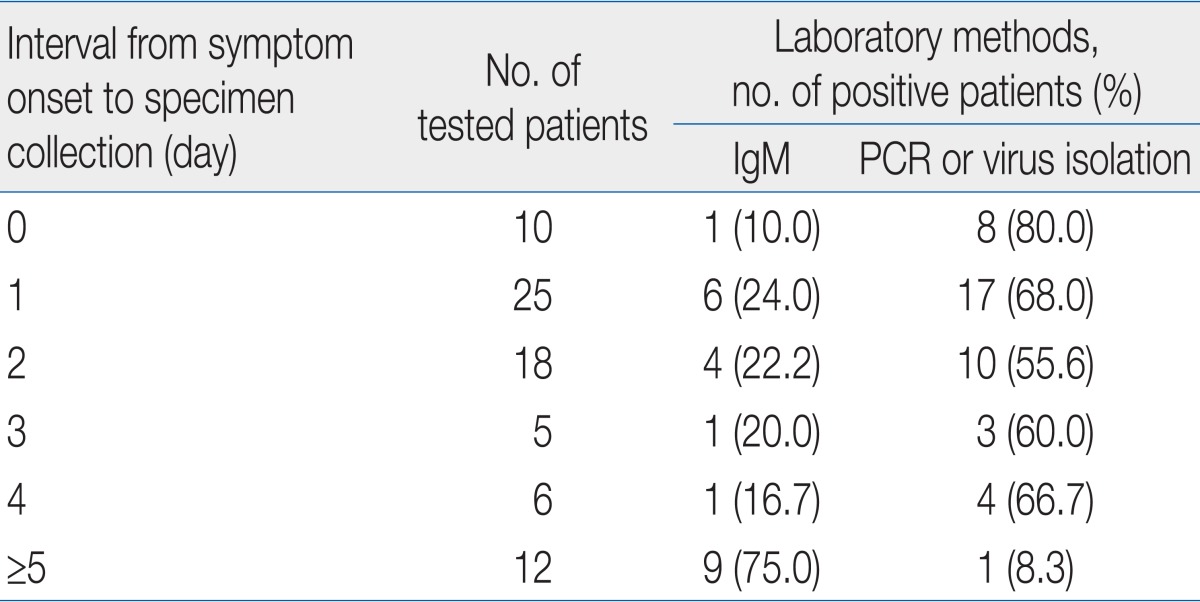
Two laboratory methods are used to confirm measles in Korea: serological and virological. Serologically confirmed measles requires a positive test for measles-specific immunoglobulin (Ig) M and/or a 4-fold rise in measles-specific IgG; virologically confirmed measles requires the virus to be isolated from culture and/or a positive result by reverse transcription polymerase chain reaction (RT-PCR). As described in Table 3, the positive predictive value for IgM is low during the first 5 days, whereas the positive predictive value for PCR or virus isolation is low after the first 4-5 days. Since 2011, the KCDC has emphasized to public health officers the importance of obtaining a serum specimen 3 days after the onset of rash and a throat swab specimen as early as possible after the onset of rash.
Table 3.
Comparative Interval from Symptom Onset to Specimen Collection in Measles Case-Patients, by Two Different Laboratory Methods Identified in a School Outbreak in Incheon, Republic of Korea, 2010
IgM, immunoglobulin M; PCR, polymerase chain reaction.
Adapted from Korea Centers for Disease Control and Prevention (unpublished data).
Seroepidemiology as a tool for screening susceptible population
Susceptible individuals with measles should be identified through public health measures beyond those used for routine surveillance. Because the vaccination program during the last 10 years has been stratified by age, determining the age-specific seroprevalence may help in identifying such populations. The Five Year National Measles Elimination Program that included a catch-up immunization program targeting school-aged children (8 to 16 years of age; those who were born between March 1985 and February 1994), and a keep-up program that requires, since 2001, all children entering elementary school to be certified by the physician as having received 2 doses of MMR vaccine. Therefore, comparing seroprevalence between different age cohorts, vaccinated according to different immunization strategies, would be useful in evaluating age-related susceptibility in the Korean population.
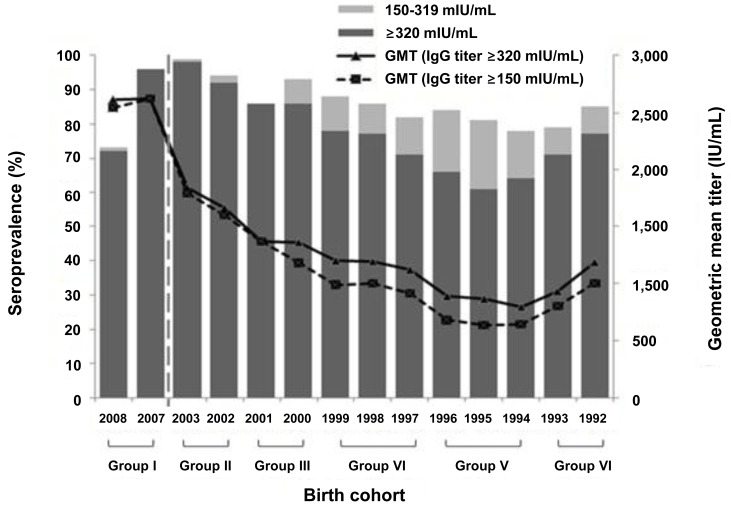
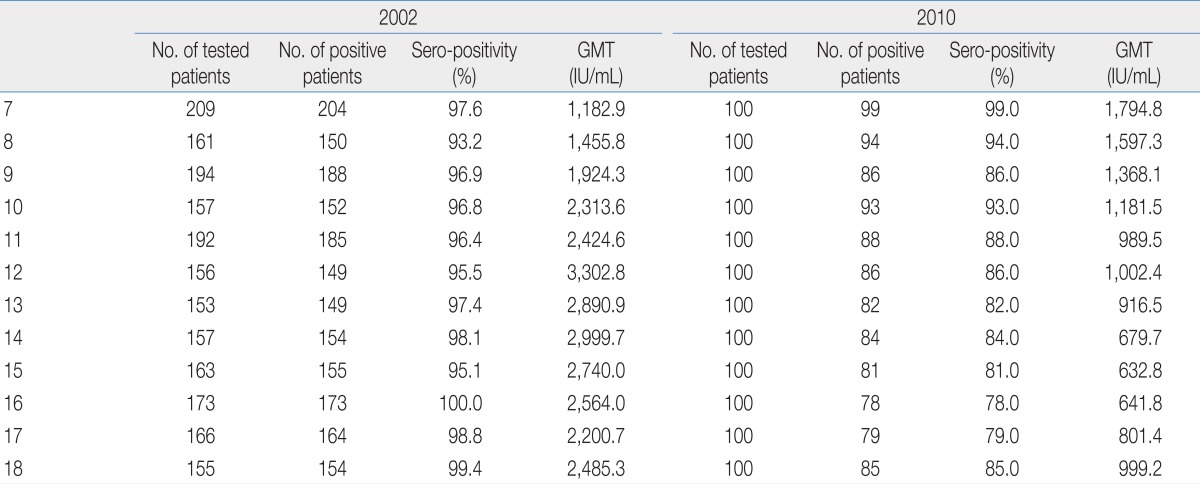
The seroprevalence study conducted in 2010 used residual serum specimens from a private diagnostic laboratory and measured measles seropositivity and anti-measles antibody geometric mean titer (GMT) for the following birth cohorts: group I, subjects aged 24 to 47 months (2007-2008 birth cohort) who had been targeted for receiving their first dose of MMR vaccine during 2008-2009; group II, subjects aged 7 to 8 years (2002-2003 birth cohort) who were subject to the keep-up MMR2 program during 2008-2009; group III, subjects aged 9 to 10 years (2000-2001 birth cohort) who were subject to the keep-up MMR2 program during 2006-2007; group IV, subjects aged 11 to 13 years (1997-1999 birth cohort) who were subject to the keep-up MMR2 program during 2003-2005; group V, subjects aged 14 to 16 years (1994-1996 birth cohort) who were subject to the keep-up MMR2 program during 2002; and group VI, subjects aged 17 to 18 years (1992-1993 birth cohort) who were subject to the catch-up campaign in 200126).
Overall, seropositivity gradually decreased from 99.0% in subjects aged 7 years to 78.0% in subjects aged 16 years (Fig. 1). The GMT showed a half U-shaped curve pattern, with the highest GMT in subjects aged 36 to 47 months (2,619.9 mIU/mL) and the lowest GMT in subjects aged 15 years (632.8 mIU/mL). In general, GMTs in 2010 were lower than those measured in a seroepidemiological study in 2002 (Table 4)27). Moreover, seropositivity among school-aged children in 2010 was lower than that of children in 2002, who had been recently vaccinated during the 2001 catch-up vaccination campaign. These data show a "pocket" of low seropositivity among adolescents aged 14 to 16 years (1994-1996 birth cohort), who were the target population for the earliest stage of the keep-up program in 2002. In addition, these data may indicate that the keep-up program failed to achieve its goals for a brief period during its early implementation. The 2010 outbreak among junior high school students described previously corresponded to the same "pocket" birth cohort identified in this seroprevalence study (1994-1996 birth cohort). Alternatively, the lower seroprevalence in older adolescents might be the result of secondary vaccine failure or waning immunity. There was a slight increase in the seropositivity in the 17 to 18 years cohort compared to that in the 14 to 16 years cohort that led to the half U-shaped pattern of the curve. This finding could be explained by the following hypothesis: 1) the catch-up immunization campaign in 2001 was more effective in maintaining the population's immunity than the keep-up program in 2002, and 2) this age cohort had a higher chance than younger groups of acquiring natural measles infection during the nationwide outbreak in 2000-2001.
Fig. 1.
Quantitative comparison of seroprevalence of measles by different age and age groups, Republic of Korea, 2010. GMT, geometric mean titer; IgG, immunoglobulin G.
Table 4.
Comparative Seropositivity from Measles Serosurveillance Data, between Years 2002 and 2010, Republic of Korea
While routine immunization and school-entry requirements have been in place for 10 years in Korea, timely immunization and coverage may remain suboptimal. There have been outbreaks in certain groups, primarily in those aged 1 to 2 and 14 to 16 years. Since pockets of susceptible people are at risk of sparking or being involved in a future outbreak and may promote the spread the infection in the community, consideration of follow-up vaccination for those with suboptimal immunization is needed. Moreover, because missed opportunities may contribute to these pockets of susceptibility, the importance of timely vaccination of young children aged 12 to 15 months should be highlighted.
Future directions: improving the performance of measles surveillance
To sustain the elimination of measles, sensitive surveillance and timely notification of suspected cases is essential. Efforts to improve the timeliness of reporting must, therefore, be part of the continuous process to improve the quality of the measles surveillance system28,29). Delay in notification can occur when physicians are inexperienced in diagnosing measles without laboratory confirmation. Therefore, immediate mandatory reporting from laboratories to the government could help to minimize delays.
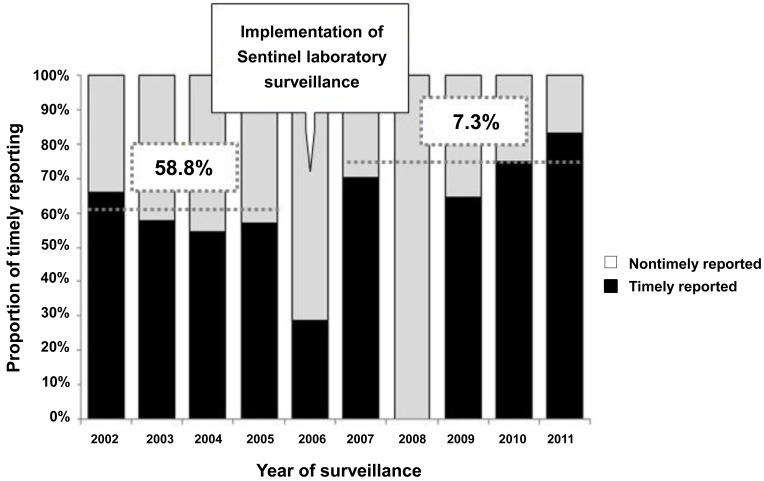
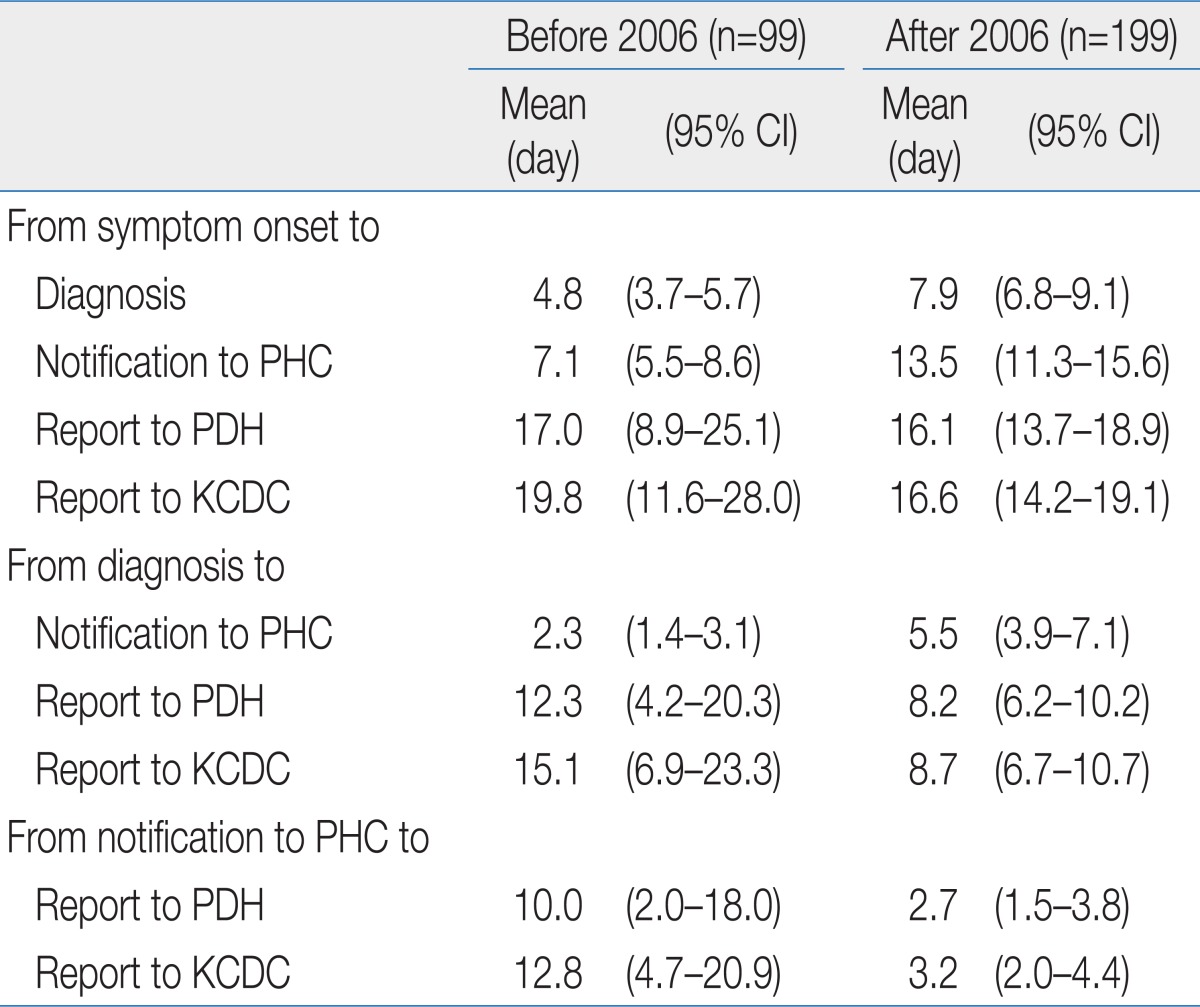
In Korea, active laboratory-based surveillance of measles, which started in 2006, has resulted in timely reporting of measles cases (Fig. 2). Moreover, when classified according to the 2 periods (before and after 2006), the interval between patient presentation and notification to a public health center and then to the KCDC has reduced from 12.8 days to 3.2 days (Table 5).
Fig. 2.
Timely reporting of sporadic measles cases before and after the implementation of sentinel laboratory surveillance in Republic of Korea, 2002-2011.
Table 5.
Timeliness of Measles Surveillance Activities, by Mode of Surveillance, Republic of Korea, 2002-2011
PHC, public health center; PDH, provincial department of health; KCDC, Korea Centers for Disease Control and Prevention.
Adapted from KCDC (unpublished data).
The conclusions to be drawn from the measles surveillance results in Korea are clear. To some extent, the efforts mentioned above have contributed to the maintenance of measles elimination. Finding more sensitive and effective surveillance measures are important for maintaining the elimination and preventing future outbreaks of measles.
References
- 1.Sohn KC, Cho SS, Doh KC, Choi Y, Chung KS, Kum DH, et al. Statistical observation for pediatric inpatients. J Korean Pediatr Soc. 1984;27:1–8. [Google Scholar]
- 2.Lee KS, Chung KS, Ryoo KY, Lee WG, Kang SJ, Lee SB, et al. Statistical analysis of pediatric diseases in Korea(1987) J Korean Pediatr Soc. 1989;32:885–896. [Google Scholar]
- 3.Ahn YH, Ma TY, Lee JS, Sun H. Statistical studies on pediatric emergency room patients. J Korean Pediatr Soc. 1977;20:751–756. [Google Scholar]
- 4.Kim IS, Lee DW. Recent mortality trends in Korea. Korean J Prev Med. 1969;2:61–76. [Google Scholar]
- 5.Oh SH. Trend in viral infectious diseases in children. Infect Chemother. 2011;43:435–442. [Google Scholar]
- 6.Korea Centers for Disease Control and Prevention. National notifiable infectious diseases reports [Internet] Cheongwon: Korea Centers for Disease Control and Prevention; c2012. [cited 2012 Jul 25]. Available from: http://www.cdc.go.kr. [Google Scholar]
- 7.Lee YH. Measles infections and measles vaccinations rates for the past 10 years in Kang Wha: a Cohort observation. Korean J Prev Med. 1981;14:43–51. [Google Scholar]
- 8.The Korean Pediatric Society. Measles-Mumps-Rubella vaccine. In: Lee HJ, editor. Immunization guideline. 7th ed. Seoul: The Korean Pediatric Society; 2012. pp. 92–108. [Google Scholar]
- 9.Kim SK, Yi IK, Han SK, Park JH, Chang YJ, Choi JW, et al. Epidemiologic study during 1993 measles outbreaks in Seongnam area. J Korean Pediatr Soc. 1995;38:180–188. [Google Scholar]
- 10.Yi IK, Choi JW, Kim SK, Son BK, Kim JG, Yu SK, et al. Epidemiologic study of measles outbreak in school-aged children in East KyongGi-Do area. J Korean Pediatr Soc. 1996;39:63–71. [Google Scholar]
- 11.Elimination of measles in the Republic of Korea, 2001-2006. Wkly Epidemiol Rec. 2007;82:118–124. [PubMed] [Google Scholar]
- 12.Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. National measels elimination 5 year program a white book. Seoul: Korea Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 13.Korea Centers for Disease Control and Prevention. Guidelines for the confirmation of second measles vaccination of elementary school students at their entry to school in 2006. Seoul: Korea Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 14.Wiesen E, Wannemuehler K, Goodson JL, Anand A, Mach O, Thapa A, et al. Stability of the age distribution of measles cases over time during outbreaks in Bangladesh, 2004-2006. J Infect Dis. 2011;204(Suppl 1):S414–S420. doi: 10.1093/infdis/jir146. [DOI] [PubMed] [Google Scholar]
- 15.Siedler A, Mankertz A, Feil F, Ahlemeyer G, Hornig A, Kirchner M, et al. Closer to the goal: efforts in measles elimination in Germany 2010. J Infect Dis. 2011;204(Suppl 1):S373–S380. doi: 10.1093/infdis/jir068. [DOI] [PubMed] [Google Scholar]
- 16.Sniadack DH, Mendoza-Aldana J, Jee Y, Bayutas B, Lorenzo-Mariano KM. Progress and challenges for measles elimination by 2012 in the Western Pacific Region. J Infect Dis. 2011;204(Suppl 1):S439–S446. doi: 10.1093/infdis/jir148. [DOI] [PubMed] [Google Scholar]
- 17.Gidding HF, Wood J, MacIntyre CR, Kelly H, Lambert SB, Gilbert GL, et al. Sustained measles elimination in Australia and priorities for long term maintenance. Vaccine. 2007;25:3574–3580. doi: 10.1016/j.vaccine.2007.01.090. [DOI] [PubMed] [Google Scholar]
- 18.Park O, Choi BY. Introduction and evaluation of communicable disease surveillance in the republic of Korea. J Prev Med Public Health. 2007;40:259–264. doi: 10.3961/jpmph.2007.40.4.259. [DOI] [PubMed] [Google Scholar]
- 19.So JS, Go UY, Lee DH, Park KS, Lee JK. Epidemiological investigation of a measles outbreak in a preschool in Incheon, Korea, 2006. J Prev Med Public Health. 2008;41:153–158. doi: 10.3961/jpmph.2008.41.3.153. [DOI] [PubMed] [Google Scholar]
- 20.Choi WS, Sniadack DH, Jee Y, Go UY, So JS, Cho H, et al. Outbreak of measles in the Republic of Korea, 2007: importance of nosocomial transmission. J Infect Dis. 2011;204(Suppl 1):S483–S490. doi: 10.1093/infdis/jir087. [DOI] [PubMed] [Google Scholar]
- 21.Pattamadilok S, Incomserb P, Primsirikunawut A, Lukebua A, Rota PA, Sawanpanyalert P. Genetic characterization of measles viruses that circulated in Thailand from 1998 to 2008. J Med Virol. 2012;84:804–813. doi: 10.1002/jmv.23249. [DOI] [PubMed] [Google Scholar]
- 22.Aoki Y, Mizuta K, Suto A, Ikeda T, Abiko C, Yamaguchi I, et al. Importation of the evolving measles virus genotype d9 to yamagata, Japan from Thailand in 2009. Jpn J Infect Dis. 2009;62:481–482. [PubMed] [Google Scholar]
- 23.Ferson MJ, Young LC, Robertson PW, Whybin LR. Difficulties in clinical diagnosis of measles: proposal for modified clinical case definition. Med J Aust. 1995;163:364–366. doi: 10.5694/j.1326-5377.1995.tb124630.x. [DOI] [PubMed] [Google Scholar]
- 24.Hyde TB, Nandy R, Hickman CJ, Langidrik JR, Strebel PM, Papania MJ, et al. Laboratory confirmation of measles in elimination settings: experience from the Republic of the Marshall Islands, 2003. Bull World Health Organ. 2009;87:93–98. doi: 10.2471/BLT.07.045484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riddell MA, Kelly HA, Featherstone D, Rota P. Laboratory testing and confirmation of suspected measles infection crucial in countries that have eliminated measles. Ann Emerg Med. 2009;54:639–640. doi: 10.1016/j.annemergmed.2009.03.035. author reply 640. [DOI] [PubMed] [Google Scholar]
- 26.Kim ES, Choe YJ, Cho H, Kim YJ, Yoon HS, Yang JS, et al. Seroprevalence of measles among children affected by national measles elimination program in Korea, 2010. Vaccine. 2012;30:3355–3359. doi: 10.1016/j.vaccine.2012.03.073. [DOI] [PubMed] [Google Scholar]
- 27.Kim SS, Han HW, Go U, Chung HW. Sero-epidemiology of measles and mumps in Korea: impact of the catch-up campaign on measles immunity. Vaccine. 2004;23:290–297. doi: 10.1016/j.vaccine.2004.07.030. [DOI] [PubMed] [Google Scholar]
- 28.Richard JL, Vidondo B, Mausezahl M. A 5-year comparison of performance of sentinel and mandatory notification surveillance systems for measles in Switzerland. Eur J Epidemiol. 2008;23:55–65. doi: 10.1007/s10654-007-9187-1. [DOI] [PubMed] [Google Scholar]
- 29.Lee MS, King CC, Chen CJ, Yang SY, Ho MS. Epidemiology of measles in Taiwan: dynamics of transmission and timeliness of reporting during an epidemic in 1988-9. Epidemiol Infect. 1995;114:345–359. doi: 10.1017/s0950268800057988. [DOI] [PMC free article] [PubMed] [Google Scholar]