Abstract
To evaluate the dosimetric impact of respiratory breast motion and daily setup error on whole breast irradiation (WBI) using three irradiation techniques; conventional wedge (CW), field-in-field (FIF) and irregular surface compensator (ISC). WBI was planned for 16 breast cancer patients. The dose indices for evaluated clinical target volume (CTVevl), lung, and body were evaluated. For the anterior-posterior (AP) respiratory motion and setup error of a single fraction, the isocenter was moved according to a sine function, and the dose indices were averaged over one period. Furthermore, the dose indices were weighted according to setup error frequencies that have a normal distribution to model systematic and random setup error for the entire treatment course. In all irradiation techniques, AP movement has a significant impact on dose distribution. CTVevlD95 (the minimum relative dose that covers 95 % volume) and V95 (the relative volume receiving 95 % of the prescribed dose) were observed to significantly decrease from the original ISC plan when simulated for the entire treatment course. In contrast, the D95, V95 and dose homogeneity index did not significantly differ from those of the original plans for FIF and CW. With regard to lung dose, the effect of motion was very similar among all three techniques. The dosimetric impact of AP respiratory breast motion and setup error was largest for the ISC technique, and the second greatest effect was observed with the FIF technique. However, these variations are relatively small.
Keywords: respiratory motion, setup error, field-in-field, electronic compensator, whole breast irradiation
INTRODUCTION
Patients with early stage breast cancer are usually treated with a combination of conservative surgery and post-operative radiotherapy with or without systemic therapy. In such cases, whole breast irradiation (WBI) is standard care. From conventional radiotherapy principles, the hot spot regions, which receive a higher dose than prescribed, may have adverse effects [1]. Furthermore, recent randomized controlled trials have demonstrated that there is no difference in clinical outcome between conventional treatment with fractionated doses of 2.0 Gy and hypofractionated treatment with 2.66 Gy [2]. However, the high-dose regions which occur in hypofractionated treatment are likely to suffer more severe adverse effects due to the larger fractionated dose compared to the dose used in conventional treatment. Consequently, in patients receiving hypofractionated treatment it is important to deliver a homogenous dose distribution throughout the breast to minimize hot spots.
In conventional WBI, the two parallel-opposed wedged tangential irradiation technique (conventional wedge, CW) is widely used. However, this technique results in significant dose heterogeneity [3]. Therefore, new dose delivery techniques, such as forward-planning segmented intensity-modulated radiation therapy (IMRT) [3, 4], electronic compensation, and IMRT [5] have been developed to improve dose uniformity.
Several studies on the dosimetric impact of respiratory motion and patient setup error have been performed in various ways. Some of these have discussed the dosimetric impact of respiratory motion on whole breast irradiation using breath-hold or four-dimensional computed tomography (CT) image sets [6-8]. They concluded that the planned dose based on CT images taken during a certain respiratory phase differed from the actual patient dose. However, the dosimetric impact of respiratory motion was clinically insignificant for the CW technique and segmental IMRT. In contrast, for dynamic IMRT, which delivers small discrete ‘beamlets’ or subfield intensity patterns, simulation results indicated that target dose coverage decreased when treatment was planned using end-of-inspiration-phase image sets [7].
Prabhakar et al. [9] have previously reported the dosimetric impact of setup error. They point out that the setup error in the isocenter should be kept strictly below 0.3 cm.
As summarized above, the effect of respiratory motion and setup errors on the actual delivered dose has been evaluated in previous studies. However, there has been no study taking both factors into account simultaneously. The purpose of our study was to evaluate the dosimetric impact of respiratory motion and daily setup error in patients using three different irradiation techniques: conventional wedge technique (CW), field-in-field (FIF), and irregular surface compensator (ISC). This study was approved by the Institutional Review Board.
MATERIALS AND METHODS
Patients
A total of 16 consecutive patients with early-stage breast cancer who received WBI were chosen for this study. Right breasts were treated in 8 patients and left breasts were treated in the other 8. For all patients, the prescribed dose was 50 Gy in 25 fractions.
All patients underwent helical CT under free-breathing conditions using a GE Highspeed RT scanner (GE Healthcare, Rydalmere, NSW, Australia) at 5.0 mm intervals to encompass both breasts and the entire thoracic cavity including both lungs.
A breast board (Bionix Radiation Therapy, Toledo, OH, USA) was used to immobilize patients in the supine position. A radio-opaque flexible marker was placed on the patient's midline.
Target volume and critical structure definition
CT image sets were transferred to the Eclipse treatment planning system (Varian Medical Systems, Palo Alto, CA, USA) for contouring and treatment planning. The patient outline, clinical target volume (CTV), planning target volume (PTV) and whole lung were contoured on each CT slice. The CTV was defined as the entire breast tissue including glandular breast and surrounding soft tissue. The PTV was defined as the CTV plus an expansion of 5 mm in all directions except for the external skin surface. The lung volume was automatically generated using the auto-contouring tool of the treatment planning system. The evaluated CTV (CTVevl) was defined as the volume of the CTV enclosed by contours drawn 5 mm below the skin surface to eliminate the region of dose build-up [6].
Planning
We performed treatment planning using two tangential fields for breast irradiation with three different techniques: CW, FIF and ISC.
For each patient, the same isocenter and gantry angle were used for each irradiation technique. All open tangential fields included a 1.5–2.0 cm flash beyond the patient skin surface to take the patient's breathing and setup error into account. A 4 MV photon beam was used for all tangential fields. The medial field border was defined along the radio-opaque flexible marker on the midline.
The planned dose was normalized to the dose at a point which was 0.5–2.0 cm superficial to the chest wall–lung interface. For each patient, this normalization point was set to the same location for all techniques and positioned so as not to be blocked by beam modifiers. Anisotropic Analytical Algorithm (ver. 8.6.14) [10] with inhomogeneity correction was used to calculate the dose for each plan.
Conventional wedge plan
For conventional wedge (CW) plan, the wedge angle and field weight were adjusted to evenly distribute hot spots in the medial, lateral and superficial regions.
Field-in-field plan
For field-in-field (FIF), we followed the procedures reported by Kestin et al. [3]. The monitor unit (MU) weights of the open radiation field and those of the sub-fields were adjusted to remove hot spots in each plan. Taking into account dose output stability, we selected sub-fields with more than 6 MU.
Irregular surface compensator plan
Irregular surface compensator (ISC), a type of electronic compensator, is a feature installed in Eclipse which enables improved dose homogeneity for irregular surface shapes. The X-ray fluence distribution required to produce an isodose surface perpendicular to the central axis at a specified depth is calculated by Eclipse and then delivered using a dynamic multileaf collimator (MLC). If the dose is not sufficiently homogenous, painting the fluence map can modify fluence distribution to achieve better dose homogeneity. The region enclosed by the 107 % isodose contours is erased by manual fluence painting. The fluence value of the superficial region is also applied in the flash region in order to ease MLC movement in the flash region.
Plan evaluation
A dose–volume histogram (DVH) analysis was performed for all regions of interest. The following dose indices were used to evaluate the plan quality where relative dose means the ratio of the received to the prescribed dose, and relative volume shows the fraction of the whole contoured volume of each region of interest.
mean dose of CTVevl,
CTVevl D95; the minimum relative dose that covers 95% of the volume of the CTVevl [11],
CTVevl V95; the relative volume of CTVevl that receives at least 95% of the prescribed dose [11],
- CTVevl dose homogeneity index (DHI); this index represents the homogeneity of the dose in CTVevl. Several definitions of DHI have previously been proposed [12, 13]. Here this index, which was defined by Ding et al. [14], is described as follows:
where D20 and D80 are the minimum doses covering 20% and 80% of the volume of the CTVevl, respectively, and Dprescription is the prescription dose.
(1) Lung V20: the relative volume of normal lung receiving more than 20 Gy [15],
Body V105: the absolute volume of the body, including CTVevl and other structures, that receives more than 105% of the prescribed dose.
Dose variation by isocenter shift
Based on the CT image set of each patient, an ‘original plan’ was created using the usual clinical planning technique of our Institution. Our approach for the evaluation of dose variation was to shift the isocenter of each original plan in every direction and estimate the variation of each dose index with isocenter shift.
Kinoshita et al. [16] published a report of their study on the 3D intrafractional motion of 17 Japanese breast cancer patients during tangential breast irradiation. In their study, the ranges of respiratory motion were 1.0 ± 0.6 mm, 1.3 ± 0.5 mm, and 2.6 ± 1.4 mm for the right-left, superior-inferior (SI), and anterior-posterior (AP) direction, respectively. Therefore, in our study, the isocenter of each plan was shifted by displacing the isocenter by 0.5 cm in all directions. Because the largest respiratory movement occurred in the AP direction as mentioned above, we also simulated dose variation by a 1.0 cm shift in this direction. These eight plans were defined as the ‘isocenter-shift plan’. We employed the same MU number as the original plan to the isocenter-shift plan so as not to change any delivery conditions except for the isocenter position. Each dose index was obtained for all isocenter-shift plans.
Dose variation with respiratory motion and setup error in a single fraction
To analyze movement in the AP direction, the variation of dose indices caused by respiratory motion and setup error were calculated for a single fraction using the method described below.
First, the dose index was obtained as a function of the amount of isocenter shift from the isocenter-shift plans. Next, the average of the dose index throughout the respiratory cycle ( ) was calculated using the assumption that the patient's respiratory cycle represented a sine curve in the AP direction. With a setup error E, this can be described as follows:
) was calculated using the assumption that the patient's respiratory cycle represented a sine curve in the AP direction. With a setup error E, this can be described as follows:
| (2) |
where A is the amplitude of respiratory movement, and T is the respiratory cycle. P is the dose index as a function of the amount of isocenter shift, which was obtained from the isocenter-shift plan. The amplitude A in the AP direction used in this study was 0.3 cm based on the study by Kinoshita et al. [16].
 was simulated with setup errors of −0.5, −0.3, 0.0, 0.3 and 0.5 cm, where negative and positive signs indicate the posterior and anterior direction, respectively.
was simulated with setup errors of −0.5, −0.3, 0.0, 0.3 and 0.5 cm, where negative and positive signs indicate the posterior and anterior direction, respectively.
Dose variation by respiratory motion and setup error in entire treatment course
Assuming that daily setup error has a normal distribution for systematic and random error, the dose indices after all fractions ( ) are calculated using
) are calculated using  , as follows;
, as follows;
| (3) |
where  is the normal distribution function of the systematic setup error E. M indicates the overall mean error and Σ is the standard deviation (SD) of systematic setup error. The normal distribution function of the random setup error e is defined as
is the normal distribution function of the systematic setup error E. M indicates the overall mean error and Σ is the standard deviation (SD) of systematic setup error. The normal distribution function of the random setup error e is defined as  where σ is the SD of the random setup error [17].
where σ is the SD of the random setup error [17].
Topolnjak et al. [18] studied setup error from measurements with cone-beam CT in breast treatments and reported that parameters for setup errors in the AP direction were M = 2.0 mm, Σ = 2.5 mm and σ = 2.6 mm. We adopted these values in our analysis.
Statistical analysis
All patient data were used in the statistical calculation. Student's t-test or Welch's t-test (two-tailed) was applied to compare each dose index between irradiation techniques and to investigate the effects of respiratory motion and setup error (i.e. comparing the dose indices on original and isocenter-shift plans,  and
and  ). A P value of ≤0.05 was considered statistically significant.
). A P value of ≤0.05 was considered statistically significant.
RESULTS
Plan evaluation
Table 1 summarizes the mean value and 1 SD of each dose index obtained from the original plan.
Table 1:
Summary of the dose indices on original plan for CTVevl, lung and body
| Mean ± 1SD | Range | |||
|---|---|---|---|---|
| Volume (cm3) | 293.3 ± 125.1 | (47.9–530.8) | ||
| CTVevl | Mean (%) | CW | 102.0 ± 1.3 | (99.9–105.8) |
| FIF | 100.2 ± 0.8 | (98.7–101.8) | ||
| ISC | 100.3 ± 0.8 | (98.8–101.9) | ||
| D95 (%) | CW | 97.6 ± 1.5 | (93.8–100.3) | |
| FIF | 95.8 ± 1.9 | (91.7–98.0) | ||
| ISC | 97.3 ± 1.0 | (95.6–98.9) | ||
| V95 (%) | CW | 98.8 ± 2.7 | (89.3–100.0) | |
| FIF | 96.2 ± 4.0 | (86.0–99.8) | ||
| ISC | 99.2 ± 1.1 | (95.7–100.0) | ||
| DHI (%) | CW | 4.9 ± 1.3 | (3.2–7.9) | |
| FIF | 3.9 ± 1.2 | (2.5–6.5) | ||
| ISC | 2.9 ± 0.7 | (2.0–4.3) | ||
| Lung | V20 (%) | CW | 7.20 ± 2.13 | (3.34–10.56) |
| FIF | 6.77 ± 2.08 | (2.86–9.93) | ||
| ISC | 6.23 ± 2.07 | (1.90–8.83) | ||
| Body | V105 (cm3) | CW | 114.66 ± 130.98 | (12.19–581.74) |
| FIF | 5.04 ± 13.43 | (0.00–54.70) | ||
| ISC | 0.29 ± 0.87 | (0.00–3.46) |
CW = conventional wedge, FIF = field in field, ISC = irregular surface compensator, CTVevl = CTV for evaluation (see the detail in text), Mean = mean dose, D95 = dose covering ≥ 95% volume. V95 = volume receiving ≥ 95% prescribed dose, DHI = dose homogeneity index, V20 = volume receiving ≥ 20 Gy, V105 = volume receiving ≥ 105% prescribed dose.
The value of the mean dose relative to the prescribed dose was 102.0% for CW, 100.2% for FIF and 100.3% for ISC. Due to the large hot spot region in CTVevl, which was indicated by the body V105, the mean dose of CTVevl in the CW plan was slightly higher than the other techniques.
D95s were 97.6% for CW, 95.8% for FIF and 97.3% for ISC. Although the D95s and V95s did not differ significantly between CW and ISC, those of FIF were statistically lower than the other techniques. This was because the widths of FIF sub-fields were narrow in the superior-inferior direction, and therefore the dose coverage on the superior and inferior target volume was slightly degraded. For the same reason, the DHI of the CTVevl for the FIF technique was slightly larger than for the ISC technique.
The body V105, including CTVevl and other structures, in the CW technique showed significantly larger values than in the FIF or ISC techniques. The reason was that the physical wedge was a one-dimension dose compensator, and it cannot compensate the dose sufficiently in the superior-inferior direction. Consequently, the DHI of the CTVevl was largest for the CW technique.
The lung V20 showed no significant difference between the three techniques.
Dose variation by isocenter shift
Table 2 shows the dose indices for CTVevl, lung and body with isocenter shift in the lateral and SI directions. For all techniques, isocenter shifts of 0.5 cm along these axes showed no significant variation from the original plans for most of the indices. However, for the lateral shift in ISC, which indicates a lateral shift away from the midline, V95 significantly decreased from 99.2% to 96.9% and D95 also decreased from 97.3% to 96.0%. The reason is that if a patient shifts away from the midline, the target moves into the flash region (see Fig. 1), where the fluence intensity is small to ensure a smooth movement of MLC, and not sufficient to give the prescribed dose to the target.
Table 2:
Summary of the dose indices on isocenter-shift plan for the lateral and superior-inferior directions
| Original 0 cm | Laterally toward midlinea 0.5 cm | Laterally away from midlinea 0.5 cm | Foota 0.5 cm | Heada 0.5 cm | |||
|---|---|---|---|---|---|---|---|
| CTVevl | Mean (%) | CW | 102.0 | 102.2 | 101.6 | 101.8 | 102.0 |
| FIF | 100.2 | 100.5 | 99.6 | 100.1 | 100.2 | ||
| ISC | 100.3 | 101.1 | 99.7 | 100.5 | 100.4 | ||
| D95 (%) | CW | 97.6 | 97.8 | 97.2 | 97.4 | 97.6 | |
| FIF | 95.8 | 95.4 | 95.7 | 95.5 | 95.8 | ||
| ISC | 97.3 | 97.3 | 96.0* | 96.8 | 97.1 | ||
| V95 (%) | CW | 98.8 | 98.8 | 98.5 | 98.7 | 98.5 | |
| FIF | 96.2 | 95.5 | 96.3 | 95.9 | 96.2 | ||
| ISC | 99.2 | 98.7 | 96.9* | 98.7 | 99.0 | ||
| DHI (%) | CW | 4.9 | 4.9 | 5.0 | 5.0 | 5.0 | |
| FIF | 3.9 | 4.8 | 3.5 | 4.2 | 3.7 | ||
| ISC | 2.9 | 3.4 | 3.2 | 3.3 | 2.9 | ||
| Lung | V20 (%) | CW | 7.20 | 6.08 | 8.53 | 6.73 | 7.67 |
| FIF | 6.77 | 5.55 | 8.07 | 6.31 | 7.23 | ||
| ISC | 6.23 | 5.04 | 7.50 | 5.79 | 6.68 | ||
| Body | V105 (cm3) | CW | 114.66 | 112.80 | 117.50 | 108.64 | 122.36 |
| FIF | 5.04 | 16.65 | 5.42 | 6.66 | 6.26 | ||
| ISC | 0.29 | 5.41 | 2.73 | 1.13 | 1.13 |
CW = conventional wedge, FIF = field in field, ISC = irregular surface compensator, CTVevl = CTV for evaluation (see the detail in text), Mean = mean dose, D95 = dose covering ≥ 95% volume, V95 = volume receiving ≥ 95% prescribed dose, DHI = dose homogeneity index, V20 = volume receiving ≥ 20 Gy, V105 = volume receiving ≥ 105% prescribed dose, Original = original plan. aThe planning CT image (patient) movement direction. *Statistically significant difference from original plan.
Figure 1:
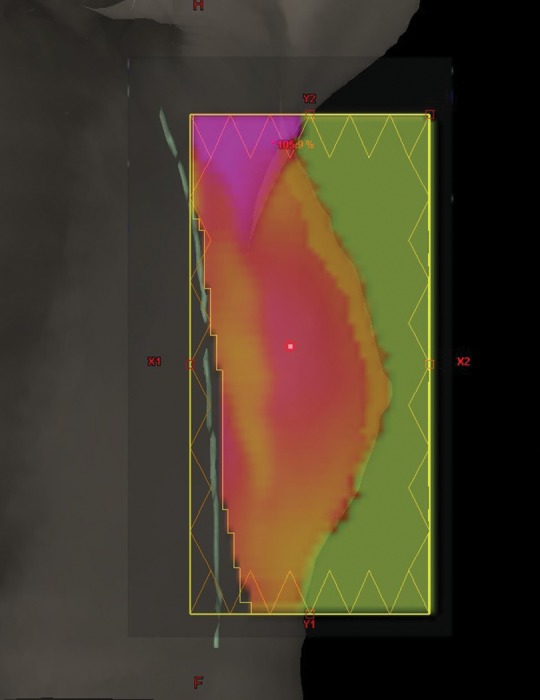
The X-ray optimal fluence map for the ISC field. The yellow rectangular represents the field edges defined by the jaws. Gray and light green colors indicate the patient body outline and midline, respectively.
The change in each dose index with isocenter movement in the AP direction is shown in Table 3. For the FIF and ISC techniques, there were significant differences in the mean dose and DHI even for a 0.5-cm isocenter shift. Regarding the DHI and V95 of the ISC technique, all isocenter shifts in the AP direction resulted in a significant difference from their values in the original plan. In contrast, for CW, a significant difference was found only in V95 of the CTVevl from 98.8% to 95.8%, when the isocenter was shifted 1.0 cm to the anterior, i.e. the patient shifted in the posterior direction.
Table 3:
Summary of the dose indices on the isocenter-shift plan for the anterior-posterior direction
| Original 0 cm | Posta 1.0 cm | Posta 0.5 cm | Anta 0.5 cm | Anta 1.0 cm | |||
|---|---|---|---|---|---|---|---|
| CTVevl | Mean (%) | CW | 102.0 | 101.6 | 102.2 | 101.5 | 101.0 |
| FIF | 100.2 | 99.3 | 100.3 | 99.4* | 98.5* | ||
| ISC | 100.3 | 100.1 | 101.1 | 99.3* | 97.2* | ||
| D95 (%) | CW | 97.6 | 93.0 | 96.8 | 97.1 | 96.6 | |
| FIF | 95.8 | 88.2 | 93.8 | 95.7 | 94.3* | ||
| ISC | 97.3 | 87.7* | 95.8 | 94.9* | 90.2* | ||
| V95 (%) | CW | 98.8 | 95.8* | 98.3 | 98.4 | 97.6 | |
| FIF | 96.2 | 87.5* | 93.8 | 96.1 | 87.9* | ||
| ISC | 99.2 | 91.9* | 97.6* | 93.1* | 71.2* | ||
| DHI (%) | CW | 4.9 | 5.7 | 5.0 | 5.0 | 5.0 | |
| FIF | 3.9 | 7.8* | 5.5* | 3.6 | 4.4 | ||
| ISC | 2.9 | 6.4* | 4.2* | 3.5* | 5.8* | ||
| Lung | V20 (%) | CW | 7.20 | 3.49* | 5.24* | 9.20* | 11.34* |
| FIF | 6.77 | 3.15* | 4.84* | 8.74* | 10.85* | ||
| ISC | 6.23 | 2.77* | 4.37* | 8.16* | 10.25* | ||
| Body | V105 (cm3) | CW | 114.66 | 121.34 | 115.21 | 115.79 | 123.69 |
| FIF | 5.04 | 70.25* | 30.89* | 7.50 | 15.42 | ||
| ISC | 0.29 | 64.96* | 18.17* | 3.14 | 14.40* |
CW = conventional wedge, FIF = field in field, ISC = irregular surface compensator, CTVevl = CTV for evaluation (see the detail in text), Mean = mean dose, D95 = dose covering ≥ 95% volume, V95 = volume receiving ≥ 95% prescribed dose, DHI = dose homogeneity index, V20 = volume receiving ≥ 20 Gy, V105 = volume receiving ≥ 105% prescribed dose, Post = posterior, Ant = anterior, Original = original plan. aThe planning CT image (patient) movement direction. *Statistically significant difference from original plan.
For V20 of the entire lung, shifting the isocenter in the AP direction resulted in a change of about 4% from the original plan in all three techniques. For the anterior isocenter shifts, body V105 for the FIF and ISC techniques increased significantly from the original plan value. In contrast, CW caused no changes in body V105 with AP movement.
Dose variation with respiratory motion and setup error in a single fraction
Table 4 shows the dose indices, taking respiratory motion into account for a single fraction treatment ( ). Because we confirmed that the dose indices were unaffected by isocenter shifts in the lateral and SI directions (Table 2), both respiratory motion and setup error were considered only in the AP direction for the dose index calculations.
). Because we confirmed that the dose indices were unaffected by isocenter shifts in the lateral and SI directions (Table 2), both respiratory motion and setup error were considered only in the AP direction for the dose index calculations.
Table 4:
The dose indices with consideration of respiratory motion and setup error in the anterior-posterior direction in single fraction (P̄ (E))
| Setup error (E) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Original | Posta 0.5 cm | Posta 0.3 cm | 0.0 cm | Anta 0.3 cm | Anta 0.5 cm | |||
| CTVevl | Mean (%) | CW | 102.0 ± 1.3 | 102.0 ± 1.5 | 102.1 ± 1.3 | 101.9 ± 1.3 | 101.7 ± 1.3 | 101.5 ± 1.3 |
| FIF | 100.2 ± 0.8 | 100.1 ± 1.1 | 100.2 ± 0.8 | 100.1 ± 0.8 | 99.7 ± 0.9 | 99.4 ± 0.9* | ||
| ISC | 100.3 ± 0.8 | 100.7 ± 1.8 | 100.7 ± 1.3 | 100.3 ± 0.9 | 99.7 ± 1.1 | 99.1 ± 1.5* | ||
| D95 (%) | CW | 97.6 ± 1.5 | 96.3 ± 5.8 | 97.0 ± 3.1 | 97.4 ± 1.6 | 97.3 ± 1.5 | 97.1 ± 1.6 | |
| FIF | 95.8 ± 1.9 | 93.1 ± 6.24 | 94.5 ± 3.7 | 95.4 ± 2.1 | 95.7 ± 1.6 | 95.4 ± 1.5 | ||
| ISC | 97.3 ± 1.0 | 94.5 ± 6.3 | 96.1 ± 3.4 | 96.5 ± 1.4 | 95.8 ± 1.2* | 94.5 ± 1.5* | ||
| V95 (%) | CW | 98.8 ± 2.7 | 97.9 ± 2.9 | 98.4 ± 2.6 | 98.6 ± 2.7 | 98.5 ± 3.2 | 98.3 ± 3.5 | |
| FIF | 96.2 ± 4.0 | 93.1 ± 4.8 | 94.6 ± 4.4 | 95.7 ± 4.0 | 95.9 ± 3.9 | 94.6 ± 4.3 | ||
| ISC | 99.2 ± 1.1 | 96.8 ± 2.7* | 98.1 ± 2.0 | 97.7 ± 1.8* | 95.0 ± 4.4* | 90.1 ± 7.1* | ||
| DHI (%) | CW | 4.9 ± 1.3 | 5.1 ± 1.2 | 5.0 ± 1.2 | 5.0 ± 1.3 | 5.0 ± 1.3 | 5.0 ± 1.3 | |
| FIF | 3.9 ± 1.2 | 5.7 ± 1.7* | 4.9 ± 1.5 | 4.2 ± 1.1 | 3.8 ± 0.8 | 3.8 ± 0.7 | ||
| ISC | 2.9 ± 0.7 | 4.3 ± 0.9* | 3.7 ± 0.8* | 3.3 ± 0.6 | 3.3 ± 0.6 | 3.8 ± 0.8* | ||
| Lung | V20 (%) | CW | 7.20 ± 2.13 | 5.28 ± 1.95* | 6.03 ± 2.02 | 7.21 ± 2.1 | 8.40 ± 2.15 | 9.22 ± 2.18* |
| FIF | 6.77 ± 2.08 | 4.89 ± 1.87* | 5.62 ± 1.96 | 6.78 ± 2.05 | 7.96 ± 2.11 | 8.77 ± 2.14* | ||
| ISC | 6.23 ± 2.07 | 4.42 ± 1.82* | 5.12 ± 1.92 | 6.24 ± 2.03 | 7.39 ± 2.09 | 8.19 ± 2.12* | ||
| Body | V105 (cm3) | CW | 114.66 ± 130.98 | 116.27 ± 118.84 | 115.19 ± 123.36 | 114.98 ± 130.12 | 115.58 ± 136.53 | 117.08 ± 141.27 |
| FIF | 5.04 ± 13.43 | 33.47 ± 29.18* | 21.03 ± 22.83 | 10.45 ± 15.98 | 6.71 ± 14.04 | 8.54 ± 16.22 | ||
| ISC | 0.29 ± 0.87 | 23.69 ± 23.58* | 12.04 ± 14.76* | 4.25 ± 6.09 | 2.29 ± 4.61 | 4.74 ± 8.19 | ||
CW = conventional wedge, FIF = field in field, ISC = irregular surface compensator, CTVevl = CTV for evaluation (see the detail in text), Mean = mean dose, D95 = dose covering ≥ 95% volume, V95 = volume receiving ≥ 95% prescribed dose, DHI = dose homogeneity index, V20 = volume receiving ≥ 20 Gy, V105 = volume receiving ≥ 105% prescribed dose; Post = posterior; Ant = anterior; Original = original plan. aEach direction shows the planning CT image (patient) movement direction. *Statistically significant difference from original plan.
When only respiratory motion was taken into consideration, as in the simulation with zero setup error, only V95 of ISC changed significantly from 99.2% ± 1.1% to 97.7% ± 1.8%.
In ISC, with setup errors of 0.3 cm in both directions, D95 decreased by 1.5% (in the anterior direction), V95 by 4.2% (in the anterior direction), and whole body V105 increased to 11.75 cm3 (in the posterior direction) from the values originally planned. The other two techniques were not influenced by E = ± 0.3 cm in all indices.
Furthermore, when E = ± 0.5 cm was adopted for ISC, significant variations of dose indices from the original plan were observed for D95, V95, DHI and whole body V105. In the case of FIF, DHI and whole body V105 differed from the original plan.
There were no significant changes in the dose indices of CTVevl, even when setup errors of 0.5 cm were applied for CW planning.
Regarding the lung, for all irradiation techniques, V20 tended to decrease as posterior setup error increased, and increase with increasing anterior setup error. In addition, the variations of lung V20 were almost the same for all techniques. The V20 decreased by 1.8% with 0.5-cm setup error in the posterior direction, and increased by 2.0% in the anterior direction.
Dose variation by respiratory motion and setup error in the entire treatment course
Table 5 demonstrates the dose indices of all treatment fractions considering respiratory motion and setup error ( ). Although the original plans always degrade with respiratory motion and setup error, the sizes of the dose index variations are smaller than the results of single fraction simulation. Significant degradation of 2.1%, 5.8%, 0.8% and 6.41 cm3 were observed for CTVevl D95, V95, DHI and whole body V105, respectively in ISC. While ISC produced better dose indices than FIF in the original plans, the difference of
). Although the original plans always degrade with respiratory motion and setup error, the sizes of the dose index variations are smaller than the results of single fraction simulation. Significant degradation of 2.1%, 5.8%, 0.8% and 6.41 cm3 were observed for CTVevl D95, V95, DHI and whole body V105, respectively in ISC. While ISC produced better dose indices than FIF in the original plans, the difference of  between ISC and FIF was not significant under our simulations.
between ISC and FIF was not significant under our simulations.
Table 5:
The dose indices with consideration of respiratory motion and setup error in the anterior-posterior direction in whole fractions (P̄̄)
| Original | P̄̄ | |||
|---|---|---|---|---|
| CTVevl | Mean (%) | CW | 102.0 ± 1.3 | 101.6 ± 1.3 |
| FIF | 100.2 ± 0.8 | 99.6 ± 0.8 | ||
| ISC | 100.3 ± 0.8 | 99.6 ± 1.2 | ||
| D95 (%) | CW | 97.6 ± 1.5 | 97.0 ± 1.6 | |
| FIF | 95.8 ± 1.9 | 95.1 ± 1.9 | ||
| ISC | 97.3 ± 1.0 | 95.2 ± 1.5* | ||
| V95 (%) | CW | 98.8 ± 2.7 | 98.3 ± 3.0 | |
| FIF | 96.2 ± 4.0 | 94.6 ± 4.0 | ||
| ISC | 99.2 ± 1.1 | 93.4 ± 4.2* | ||
| DHI (%) | CW | 4.9 ± 1.3 | 5.0 ± 1.3 | |
| FIF | 3.9 ± 1.2 | 4.2 ± 0.9 | ||
| ISC | 2.9 ± 0.7 | 3.7 ± 0.5* | ||
| Lung | V20 (%) | CW | 7.20 ± 2.13 | 8.02 ± 2.1 |
| FIF | 6.77 ± 2.08 | 7.58 ± 2.07 | ||
| ISC | 6.23 ± 2.07 | 7.03 ± 2.04 | ||
| Body | V105 (cm3) | CW | 114.66 ± 130.98 | 116.19 ± 134.4 |
| FIF | 5.04 ± 13.43 | 12.06 ± 16.97 | ||
| ISC | 0.29 ± 0.87 | 6.70 ± 8.50* |
CW = conventional wedge, FIF = field in field, ISC = irregular surface compensator, CTVevl = CTV for evaluation (see the detail in text), Mean = mean dose, D95 = dose covering ≥ 95% volume, V95 = volume receiving ≥ 95% prescribed dose, DHI = dose homogeneity index, V20 = volume receiving ≥ 20 Gy, V105 = volume receiving ≥ 105% prescribed dose, Original = original plan. *Statistically significant difference from original plan.
DISCUSSION
Patient respiratory breast motion and setup error modeling
In this study, we investigated the dosimetric impact of respiratory breast motion and daily setup error using CT data sets of Asian patients. The mean CTV volume for the 16 patients studied was 433.5 ± 142.7 cm3 (range, 174.8–710.5 cm3). In our study, CTV volumes in whole breast irradiation differ by more than 35% compared to other reports [8, 19].
It has been reported that anterior chest wall respiratory movements are 0.2–0.8 cm in Caucasian and African individuals [6, 8, 20]. Meanwhile, Kinoshita et al. [16] reported that the amplitude of respiratory breast motion in Asian patients was 0.3 cm in the AP direction. The respiratory movement of Asian breast patients is thus almost 1/3 of the results reported from the United States. Therefore, comparing Asian and American patients is worthwhile because not only does the extent of variation in breast volume differ, but there is a large difference in the respiratory motions.
Dose variation with respiratory motion and setup error in a single fraction
The dose indices of CTVevl are degraded in ISC and FIF simulations where the setup error increases. For ISC in particular, the target dose coverage was sensitive to the setup error in the anterior direction. This is because the CTV moves into the flash region of the radiation field. As shown in Fig. 1, the radiation fluence in the flash region is adjusted to be lower than the CTV region in our Institution because the MLC speed would reach the limit if the flash region had the same fluence in the CTV region. This is why ISC is sensitive to patient movement in the anterior direction. In contrast to ISC, FIF has an insignificant impact on the target dose coverage of CTVevl D95 and V95, as shown in Table 3. This is because about 90% of the prescribed dose is delivered with open fields. The CW technique is less sensitive to respiratory and setup movement, as shown in Table 4, because all MU are delivered only through the open field. These results are consistent with Cao and Vicini's results [7, 21].
In all three techniques, the setup error in the posterior direction significantly affected the lung V20, as well as target coverage. This is because the overlap between tangential fields and the lung becomes smaller, if the patient moves in a posterior direction.
Dose variation with respiratory motion and setup error in the entire treatment course
The main purpose of this study was to estimate the dosimetric impact of respiratory breast motion and daily setup error on target coverage and normal tissue dose over the entire treatment course. Thus, we calculated the dose indices, considering the effect of respiratory motion throughout the entire course of treatments ( ) by weighting the normally-distributed frequencies for systematic and random setup errors.
) by weighting the normally-distributed frequencies for systematic and random setup errors.
We found that  for ISC showed the largest variation in target coverage and DHI from the original plan. However, the present study suggested that ISC and FIF could achieve the same degree of target coverage and dose uniformity for actual patients, taking into consideration the effects of respiratory motion and setup error (Table 5).
for ISC showed the largest variation in target coverage and DHI from the original plan. However, the present study suggested that ISC and FIF could achieve the same degree of target coverage and dose uniformity for actual patients, taking into consideration the effects of respiratory motion and setup error (Table 5).
The dose distribution obtained with the CW technique is less sensitive to patient position displacement compared to FIF and ISC. However, it is known that the dose inhomogeneities that occur when using the standard wedge technique for WBI results in a significant increase in acute and chronic toxicity compared to IMRT [22]. Therefore, in terms of the grade and frequency of expected adverse effects, a patient-specific compensation technique, such as FIF or ISC could reduce toxicity and benefit the patient. Moreover, FIF and ISC would be suitable for hypofractionated treatment, a technique that requires a more homogenous dose distribution than conventional fractionation. In this study, we have shown that FIF and ISC irradiation techniques in WBI are more sensitive to respiratory breast motion and setup error than the CW technique. However, the dosimetric impacts of breast motions and daily setup errors for FIF and ISC in the whole fraction are relatively small and thus clinically acceptable.
We did not consider beam-on timing with respect to the respiratory phase. With regard to this point, Ding et al. [14] reported that target dose coverage and uniformity is more sensitive to radiation beam-on timing for respiratory motion with a cycle of longer than 6 s and an amplitude larger than 7 mm. In this study, the respiratory cycle was not considered to be a long respiratory cycle. Furthermore, it is rare for Asian patients to exhibit respiration amplitudes larger than 7 mm [16]. Thus, the parameters used in our simulation are reasonable for evaluating the effect of respiratory motion in this population.
Van Mourik et al. [23] evaluated the effects of setup errors and shape changes on breast radiation therapy. They concluded that the influences of patient and breast errors on the dose distributions are dependent on the irradiation techniques for the WBI plans. Therefore, the effect of breast shape changes during treatment should be investigated in more detail. In addition to that, we should investigate dosimetric effects of the lung expansion and contraction, and changing the separation between the breast and heart due to respiratory motion in our future work.
When using any irradiation techniques for WBI, it should be noted that the dose distributions calculated using a treatment planning system with 3D CT image data sets, defined as the original plan in this study, are not always the same as the dose distributions of actual patients due to the existence of respiratory motion and setup errors.
CONCLUSION
In this study, we evaluated the dosimetric impact of respiratory motion and setup error on whole breast tangential irradiation by numerical simulation. We found that the dosimetric impact of AP respiratory breast motion and setup error was largest on ISC, and the averaging variations of CTVevl V95 were about 6.0%. The second largest dosimetric effect was observed in the FIF technique. However, the deviation of target dose coverage from the original plan for ISC and FIF are relatively small, and hot spot regions represented by body V105 are significantly reduced by ISC and FIF compared to the CW technique.
REFERENCES
- 1.Yarnold J, Bentzen SM, Coles C, et al. Hypofractionated whole-breast radiotherapy for women with early breast cancer: myths and realities. Int J Radiat Oncol Biol Phys. 2011;79:1–9. doi: 10.1016/j.ijrobp.2010.08.035. [DOI] [PubMed] [Google Scholar]
- 2.Whelan TJ, Pignol JP, Levine MN, et al. Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med. 2010;362:513–20. doi: 10.1056/NEJMoa0906260. [DOI] [PubMed] [Google Scholar]
- 3.Kestin LL, Sharpe MB, Frazier RC, et al. Intensity modulation to improve dose uniformity with tangential breast radiotherapy: initial clinical experience. Int J Radiat Oncol Biol Phys. 2000;48:1559–68. doi: 10.1016/s0360-3016(00)01396-1. [DOI] [PubMed] [Google Scholar]
- 4.Lee JW, Hong S, Choi KS, et al. Performance evaluation of field-in-field technique for tangential breast irradiation. Jpn J Clin Oncol. 2008;38:158–63. doi: 10.1093/jjco/hym167. [DOI] [PubMed] [Google Scholar]
- 5.Strom EA. Breast IMRT: new tools leading to new vision. Int J Radiat Oncol Biol Phys. 2002;54:1297–8. doi: 10.1016/s0360-3016(02)03744-6. [DOI] [PubMed] [Google Scholar]
- 6.Frazier RC, Vicini FA, Sharpe MB, et al. Impact of breathing motion on whole breast radiotherapy: a dosimetric analysis using active breathing control. Int J Radiat Oncol Biol Phys. 2004;58:1041–7. doi: 10.1016/j.ijrobp.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Cao J, Roeske JC, Chmura SJ, et al. Calculation and prediction of the effect of respiratory motion on whole breast irradiation dose distributions. Med Dosim. 2009;34:126–32. doi: 10.1016/j.meddos.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Qi XS, White J, Rabinovitch R, et al. Respiratory organ motion and dosimetric impact on breast and nodal irradiation. Int J Radiat Oncol Biol Phys. 2010;78:609–17. doi: 10.1016/j.ijrobp.2009.11.053. [DOI] [PubMed] [Google Scholar]
- 9.Prabhakar R, Rath GK, Julka PK, et al. Simulation of dose to surrounding normal structures in tangential breast radiotherapy due to setup error. Med Dosim. 2008;33:81–5. doi: 10.1016/j.meddos.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Tillikainen L, Helminen H, Torsti T, et al. A 3D pencil-beam-based superposition algorithm for photon dose calculation in heterogeneous media. Phys Med Biol. 2008;53:3821–39. doi: 10.1088/0031-9155/53/14/008. [DOI] [PubMed] [Google Scholar]
- 11.Gregoire V, Mackie TR, Neve WD, et al. ICRU Report 83: Prescribing, recording, and reporting photon-beam Intensity-Modulated Radiation Therapy (IMRT) J ICRU. 2010;10:1–112. [Google Scholar]
- 12.Holder A. Designing radiotherapy plans with elastic constraints and interior point methods. Health Care Manag Sci. 2003;6:5–16. doi: 10.1023/a:1021970819104. [DOI] [PubMed] [Google Scholar]
- 13.Yoon M, Park SY, Shin D, et al. A new homogeneity index based on statistical analysis of the dose-volume histogram. J Appl Clin Med Phys. 2007;8:9–17. doi: 10.1120/jacmp.v8i2.2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ding C, Li X, Huq S, et al. The effect of respiratory cycle and radiation beam-on timing on the dose distribution of free-breathing breast treatment using dynamic IMRT. Med Phys. 2007;34:3500–9. doi: 10.1118/1.2760308. [DOI] [PubMed] [Google Scholar]
- 15.Graham MV, Purdy JA, Emami B, et al. Clinical dose-volume histogram analysis for pneumonitis after 3D treatment for non-small cell lung cancer (NSCLC) Int J Radiat Oncol Biol Phys. 1999;45:323–9. doi: 10.1016/s0360-3016(99)00183-2. [DOI] [PubMed] [Google Scholar]
- 16.Kinoshita R, Shimizu S, Taguchi H, et al. Three-dimensional intrafractional motion of breast during tangential breast irradiation monitored with high-sampling frequency using a real-time tumor-tracking radiotherapy system. Int J Radiat Oncol Biol Phys. 2008;70:931–4. doi: 10.1016/j.ijrobp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 17.van Herk M. Errors and margins in radiotherapy. Semin Radiat Oncol. 2004;14:52–64. doi: 10.1053/j.semradonc.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Topolnjak R, Sonke JJ, Nijkamp J, et al. Breast patient setup error assessment: comparison of electronic portal image devices and cone-beam computed tomography matching results. Int J Radiat Oncol Biol Phys. 2010;78:1235–43. doi: 10.1016/j.ijrobp.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 19.George R, Keall PJ, Kini VR, et al. Quantifying the effect of intrafraction motion during breast IMRT planning and dose delivery. Med Phys. 2003;30:552–62. doi: 10.1118/1.1543151. [DOI] [PubMed] [Google Scholar]
- 20.Kubo HD, Hill BC. Respiration gated radiotherapy treatment: a technical study. Phys Med Biol. 1996;41:83–91. doi: 10.1088/0031-9155/41/1/007. [DOI] [PubMed] [Google Scholar]
- 21.Vicini FA, Sharpe M, Kestin L, et al. Optimizing breast cancer treatment efficacy with intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2002;54:1336–44. doi: 10.1016/s0360-3016(02)03746-x. [DOI] [PubMed] [Google Scholar]
- 22.Harsolia A, Kestin L, Grills I, et al. Intensity-modulated radiotherapy results in significant decrease in clinical toxicities compared with conventional wedge-based breast radiotherapy. Int J Radiat Oncol Biol Phys. 2007;68:1375–80. doi: 10.1016/j.ijrobp.2007.02.044. [DOI] [PubMed] [Google Scholar]
- 23.van Mourik A, van Kranen S, den Hollander S, et al. Effects of setup errors and shape changes on breast radiotherapy. Int J Radiat Oncol Biol Phys. 2011;79:1557–64. doi: 10.1016/j.ijrobp.2010.07.032. [DOI] [PubMed] [Google Scholar]


