Abstract
An 85-year-old lady presented to our institution following multiple episodes of transient loss of consciousness. Her admission ECG revealed a junctional bradycardia with significant QT prolongation. Telemetry captured a torsades de pointes arrhythmia. Possible offending drugs (digoxin and hydroxychloroquine) were stopped and she was given intravenous magnesium and potassium. Despite this, she continued to have runs of torsades. An isoprenaline infusion was commenced to increase her resting heart rate. Her QT interval shortened and she had no further arrhythmia. Investigation into the cause of her bradycardia and prolonged QT revealed profound hypothyroidism. Levothyroxine was commenced but the patient remained bradycardia and required a permanent pacemaker. She had no further arrhythmia and was discharged home safely. This is a very rare case of severe primary hypothyroidism presenting with torsades de pointes.
Background
This case report describes the initial assessment and management of a patient presenting with torsades de pointes. It is a reminder that torsades is due to QT prolongation, which may be related to bradycardia. Following appropriate resuscitation, treatment should therefore be targeted towards correction of the QT interval. An isoprenaline infusion or temporary pacing may be required to increase the resting heart rate.
The case also highlights the importance of looking extensively for a cause of the QT prolongation, of which there are many. Drug induced QT prolongation and electrolyte abnormalities are most common and must be considered initially but it is also important to think about other rare causes. This case is a reminder that in patients presenting with bradycardia, prolonged QT and torsades de pointes arrhythmia, hypothyroidism should be considered in the differential diagnosis.
Case presentation
An 85-year-old lady presented to our emergency department with a 24-h history of lightheadedness and multiple brief episodes of loss of consciousness.
Her medical history includes a previous myocardial infarction, atrial fibrillation, systemic lupus erythematosus and osteoporosis. She was noted to be on warfarin, furosemide, digoxin, isosorbide mononitrate, rabeprazole, hydroxychloroquine, prednisolone, folic acid, calcium tables and co-dydramol.
On admission, she was haemodynamically stable with a blood pressure of 160/70. There was no postural drop. Clinical examination was unremarkable.
Her 12 lead ECG is shown in figure 1. It demonstrates a junctional bradycardia of 50 bpm with a significantly prolonged QT interval of 670 ms (QTc 650 ms). There were multiple premature ventricular complexes, with R waves occurring at the end of the prolonged QT interval (R on T phenomenon). During a further episode of transient loss of consciousness, telemetry captured a torsades de pointes type arrhythmia (figure 2).
Figure 1.
Admission ECG demonstrating a junctional bradycardia with significant QT prolongation and ventricular extrasystoles occurring on the T wave.
Figure 2.
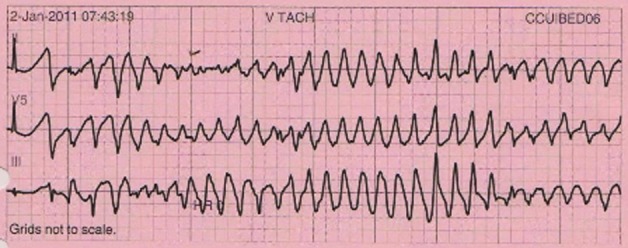
Torsades do pointes arrhythmia captured on telemetry.
The working diagnosis was torsades de pointes secondary to long QT. She was given intravenous magnesium and potassium. Digoxin and hydroxychloroquine was stopped. She was transferred to the coronary care unit for close monitoring.
Over the next 24 h, the patient had three further episodes of torsades de pointes. Each episode was associated with presyncope but settled spontaneously. She remained bradycardic with QT prolongation. An isoprenaline infusion was eventually commenced to achieve a resting heart rate of more than 70 bpm. Her QT interval shortened as predicted and she had no further arrhythmia. A temporary pacing wire was considered but was not required.
Investigations
Admission blood tests showed a normal full blood count, renal profile, liver function tests and inflammatory markers. Her magnesium level was 0.82 and potassium 4.0. This was supplemented. Her digoxin level was 0.9 (within the normal range) and troponin 0.04 (borderline elevated).
The next day, thyroid function tests revealed that the patient was profoundly hypothyroid with a significantly elevated thyroid stimulating hormone of 90.4 (0.2–5.5).
Her chest radiograph showed a normal cardiac silhouette with no evidence of pulmonary oedema. An echocardiogram demonstrated good left ventricular systolic function and no significant valve disease.
Differential diagnosis
This patient had multiple episodes of loss of consciousness secondary to a torsades de pointes type arrhythmia precipitated by an acquired long QT syndrome. Her QT prolongation was related to an underlying bradycardia and eventually found to be a rare manifestation of profound hypothyroidism. Hydroxychloroquine has also been implicated in causing QT prolongation.1
Treatment
The patient was commenced on 50 mcg of levothyroxine. Despite this she remained bradycardic and was dependent on isoprenaline to maintain a satisfactory heart rate.
Although there is an argument to withhold permanent pacing until the patient is fully replaced with thyroxine, this can take up to 8 weeks. From a practical perspective we felt that allowing a patient to stay in hospital for such a prolonged duration with torsade-related syncopal events, dependent on either isoprenaline or a temporary pacing system carried more risks than benefits. In view of this a DDDR permanent pacemaker was implanted 7 days later.
The pacemaker was programmed to provide overdrive atrial pacing at 80 bpm. This reduced the frequency of ventricular extrasystoles and shortened her QT interval as expected, removing the trigger for further episodes of torsades.
Outcome and follow-up
The patient was discharged home safely with advice to her general practitioner to uptitrate her levothyroxine dose. Follow-up was arranged with endocrinology and in the pacing clinic.
Discussion
Hypothyroidism has a variety of cardiac manifestations. The major cardiovascular changes that occur in hypothyroidism include a decrease in cardiac output and contractility, a reduction in heart rate and an increase in peripheral vascular resistance.2 3 In addition, hypothyroidism also affects atherosclerotic risk factors causing hypercholesterolaemia and diastolic hypertension.2 3
These changes can lead to a variety of clinical manifestations, ECG changes and abnormal biochemistry.2 4 5 These features are summarised in table 1. Although clearly important, cardiac symptoms and signs are generally not common or prominent in hypothyroidism.
Table 1.
Cardiac manifestations of hypothyroidism
| Symptoms and signs |
| Exertional dyspnoea, reduced exercise tolerance |
| Bradycardia |
| Hypertension |
| Oedema (often non-pitting) |
| Cardiac dysfunction with poor contractility, dilatation or pericardial effusion |
| Pericardial and pleural effusions |
| Electrocardiographic changes |
| Sinus bradycardia |
| Low voltage complexes |
| Long QT – predisposing to torsade de pointes |
| Biochemical changes |
| Dyslipidaemia (high total cholesterol and LDL) |
| Elevated serum homocysteine |
| Elevated serum creatine kinase |
LDL, low-density lipoprotein.
Occurrence of torsade de pointes as the first manifestation of hypothyroidism is very rare. There are few published case reports. Shojaie and Eshraghian described a 50-year-old woman who presented with syncope, prolongation of the QT interval and polymorphic ventricular tachycardia.6 She was initially treated with phenytoin and only found to have severe hypothyroidism on day 3 of admission following a neurology opinion for positional vertigo and hypotension. Treatment with levothyroxine was commenced and led to normalisation of her QT interval. No further arrhythmia was seen 2 months later. Schenck et al described a very similar presentation of severe hypothyroidism manifesting with symptomatic torsade de pointes tachycardia. This patient also responded well to treatment with levothyroxine.7
Our case highlights the initial assessment and management of a patient presenting with torsades de pointes. The arrhythmia is precipitated by prolongation of the QT interval. Therefore, initial assessment and management following appropriate resuscitation should be targeted towards identifying the cause of and correcting the QT prolongation.
Drugs and electrolyte abnormalities (hypokalemia, hypomagnesemia and hypocalcaemia) are the most common offending agents in acquired long QT syndrome. A very detailed drug history (including recent antibiotic therapy) must be taken and offending drugs stopped. A useful online list of QT-prolonging drugs can be found at www.qtdrugs.org. Electrolyte abnormalities must clearly be addressed but even if within normal limits, supplementation of magnesium and potassium is beneficial. Intravenous magnesium is the cornerstone of initial treatment as it suppresses ‘early afterdepolarisations’, the triggering event for torsades.
Bradycardia may be a significant contributory factor in acquired long QT as highlighted in this case. Acceleration of the heart rate shortens the QT interval. This can be achieved using β 1 adrenergic agonists such as isoprenaline or overdrive electrical pacing.8 Isoprenaline is administered as a continuous infusion titrated to heart rate and acts by accelerating AV conduction. As predicted, this shortened the QT interval in our case and prevented further episodes of torsades. β-adrenergic agonists are contra-indicated in the congenital form of long QT syndrome.
Following the initial period of stabilisation it is important to look for other causes of long QT, of which there are many. This case is a reminder that in a patient presenting with bradycardia, prolonged QT and torsades de pointes arrhythmia, hypothyroidism should be considered in the differential diagnosis.
Learning points.
-
▶
Torsades de pointes arrhythmia is a medical emergency precipitated by QT prolongation. In a patient presenting with torsades, the mainstay of treatment following initial resuscitation is intravenous magnesium and correction of the QT prolongation.
-
▶
The cause of QT prolongation should be extensively investigated. Drug induced causes and electrolyte abnormalities are most common and must be considered initially but other rare causes should be thought about.
-
▶
In bradycardia related torsades, it is vital to increase the resting heart rate to shorten the QT interval. This can be achieved with intravenous isoprenaline or overdrive electrical pacing.
-
▶
In patients presenting with bradycardia, prolonged QT and torsades de pointes arrhythmia, hypothyroidism should be considered in the differential diagnosis.
Footnotes
Competing interests: None.
Patient consent: Obtained.
References
- 1.Chen CY, Wang FL, Lin CC. Chronic hydroxychloroquine use associated with QT prolongation and refractory ventricular arrhythmia. Clin Toxicol (Phila) 2006;44:173–5. [DOI] [PubMed] [Google Scholar]
- 2.Taddei S, Caraccio N, Virdis A, et al. Impaired endothelium-dependent vasodilatation in subclinical hypothyroidism: beneficial effect of levothyroxine therapy. J Clin Endocrinol Metab 2003;88:3731–7. [DOI] [PubMed] [Google Scholar]
- 3.Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med 2001;344:501–9. [DOI] [PubMed] [Google Scholar]
- 4.Klein I, Danzi S. Thyroid disease and the heart. Circulation 2007;116:1725–35. [DOI] [PubMed] [Google Scholar]
- 5.Klein I. Endocrine Disorders and Cardiovascular Disease. In: Libby P, Bonow RO, Mann D, Zipes DP,eds. Heart Disease. Textbook of Cardiovascular Medicine. Eighth Edition Philadelphia, PA: WB Saunders; 2005. [Google Scholar]
- 6.Shojaie M, Eshraghian A. Primary hypothyroidism presenting with Torsades de pointes type tachycardia: a case report. Cases J 2008;1:298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schenck JB, Rizvi AA, Lin T. Severe primary hypothyroidism manifesting with torsades de pointes. Am J Med Sci 2006;331:154–6. [DOI] [PubMed] [Google Scholar]
- 8.Camm AJ, Luscher TF, Serruys PW. ESC Textbook of Cardiovascular Medicine. Second Edition Oxford: Oxford University Press; 2009. [Google Scholar]



