Abstract
Objectives
To compare the effects of a tailored and targeted print intervention in promoting dilated fundus examinations (DFEs) in older African Americans, and to determine if other factors are associated with getting a DFE.
Methods
African Americans, 65 years of age or older, who had not had a DFE in at least two years were recruited from community settings. Participants were randomized to receive either a tailored or targeted newsletter. Telephone follow-up was conducted at one, three, and six months to ascertain eye examination status. All self-reported DFEs were confirmed by contacting their eye doctor by telephone.
Main outcome measure
Doctor-confirmed DFE at six months.
Results
Of the 329 participants enrolled, 128 (38.9%) had a doctor-confirmed DFE. There was no difference in doctor-confirmed DFEs by intervention group (RR=1.07, 0.82–1.40 CI), with 66 participants in the tailored group (40.2%) and 62 (37.6%) participants in the targeted group having a doctor-confirmed DFE. Based on logistic regression analysis, reading the newsletter (OR=1.76, 1.08–2.87 CI) and planning on making an appointment for a DFE (OR=2.46, 1.42–4.26 CI) were significant predictors for getting a DFE.
Conclusion
The tailored and targeted interventions were equally effective in promoting doctor-confirmed DFEs at six months. Given the increases cost and effort associated with tailoring, our results suggest that well-designed targeted print messages can motivate older African Americans to get DFEs.
Dilated fundus examinations (DFEs) have been demonstrated to be an important strategy to diagnose treatable causes of visual impairment, such as glaucoma and diabetic retinopathy. However, the reluctance of people to undergo such examinations continues to be an important public health problem.1 This problem will continue to grow as the U.S. population ages, with a resultant increase in age-related eye disease. Despite public and professional educational programs to increase awareness about eye health,1–3 there is still a lack of knowledge and misconceptions about DFEs and eye disease.4 Interventions to increase the proportion of people who undergo DFEs at the recommended schedule can have a major public health impact, and affect people’s vision-related and general health-related quality of life.
This paper reports on a randomized clinical trial comparing tailored and targeted print interventions designed to promote eye examination behavior in older African Americans. Generic, targeted, and tailored health education material can be considered as being on a continuum, with increasing degrees of customization and audience segmentation.5 Generic messages provide the same information to all people, targeted messages are designed for a specific subgroup, while tailored messages are individualized based on each person’s characteristics.6 Information processing theory postulates that tailoring provides information that is more personally relevant than other messages so people pay more attention to the information, which eventually leads to behavior change.7 Although tailored messages have been shown to influence the adoption and maintenance of various health-related behaviors,7–10 this health communication strategy has had limited application regarding eye examination behavior.11–13
We investigated the hypothesis that the doctor-confirmed DFE rate would be higher in the tailored compared to the targeted intervention group. Constructs from the Health Belief Model,14 Transtheoretical Model (TTM),15 and Precaution Adoption Process Model (PAPM)16 guided intervention development. To better understand the reasons why people get DFEs, we examined the associations between demographics, preventive health practices, health literacy score, behavioral intentions, and DFE rates.
Methods
Community-dwelling African Americans, 65 years of age or older, who had not had a DFE in at least two years were recruited for the study. We conducted presentations at sites frequented by older African-Americans, such as senior centers and church groups, networked with community organizations, placed ads on the radio and in newspapers, and attended health fairs. Details of the recruitment process have been previously described.17 This research was approved by the Institutional Review Board of the University of Maryland School of Medicine.
Interested participants were screened for eligibility based on self-report, signed consent forms, and provided the research team with contact information. The health literacy skills of our participants were assessed by trained interviewers who administered the REALM-R,18 a shortened version of the REALM word recognition test. We administered a questionnaire to collect baseline demographic information and information about behavioral intention, perceived barriers and benefits to getting DFEs, and preventive health behaviors. We adapted questions from the mammography,9, 19 ophthalmology,20–22 and health behavior theory literature,16, 23 as well as information from focus groups,4 to design the questionnaire. Participants were paid $25 to compensate them for their time.
Participants were randomly assigned to the tailored or targeted intervention groups, with both groups receiving a four page newsletter designed to have a Flesch-Kincaid reading level of less than 6th grade. As shown in Table 1, the newsletter consisted of six sections, including a testimonial designed to model eye examination behavior and a barrier table to convey specific ideas to overcome barriers. Each section of the tailored newsletter was tailored on specific variables. We also included information about Medicare coverage of eye exams.
Table 1.
Tailoring variables based on participants responses, by newsletter section
| Sections | Intro | Facts | Testimonial | Ask the Doctor | Barrier table | Conclusion | ||
|---|---|---|---|---|---|---|---|---|
| Variables | 1 | 2 | 3 | |||||
| Stage of change | X | X | X | |||||
| Disease status | X | X | X | X | ||||
| Family history of glaucoma | X | |||||||
| Gender | X | |||||||
| Cues to action | X | X | ||||||
| Preventive care | X | |||||||
| Barriers | X | X | X | |||||
| Benefits | X | |||||||
| Knowledge | X | |||||||
All participants randomized to the targeted group received the same newsletter with the same messages. Each participant randomized to the tailored group received a unique newsletter, with the same sections and pictures as the targeted newsletter but with specific messages based on his/her responses to selected questions from the baseline questionnaire. For example, the “ask the doctor” section had five different messages in the message library, with a predetermined ranking to determine the order the messages would be used. People in the tailored arm received one of these five messages, depending on their questionnaire responses. One of these messages was pre-selected for the targeted newsletter. Newsletters were mailed within three weeks of study enrollment.
Participants were followed by telephone at one, three, and six months. We ascertained whether they made an appointment for or had an eye exam during the previous period, or what their intentions were regarding getting a DFE in the future. At the one-month follow-up participants were asked whether they read the newsletter. If a participant reported having a DFE, no subsequent calls were made. If a person could not be reached by telephone after eight attempts at different times and days, we called their contacts. If they could still not be reached, we mailed a brief questionnaire requesting it be completed and mailed back. Lastly, we sent a certified letter asking the participant to contact us. If we were unable to contact a participant at a follow-up period, we attempted to contact them at subsequent follow-up periods.
All self-reported DFEs, as well as reports of making an appointment at the six-month follow-up, were confirmed by contacting their eye care professional by telephone. Information about the date of the appointment and whether the appointment included dilation was reported by office staff. Participants who withdrew before follow-up or could not be contacted were considered as not having had a DFE.
Measures
We asked several questions to categorize participants according to their intention to get a DFE, based on the TTM and PAPM models. For our analysis, participants who never thought about getting a DFE were classified as stage 1. Respondents who decided they did not want to get a DFE were in stage 2, and those who had not decided yet were in stage 3. Respondents who wanted to get a DFE were asked about their future plans. Those planning on making an appointment in the next 6 months were assigned stage 4, and those planning on making an appointment in the next month were in stage 5. Participants planning on making an appointment someday but not very soon were considered as still deciding and classified as stage 3. Based on these definitions, people in stages 1–3 would be considered in the precontemplation stage of the TTM model, stage 4 corresponds to the contemplation stage and stage 5 corresponds to the preparation stage.
The questionnaire asked when participants last had a routine medical exam, had their eyes checked for glasses, and had a mammogram for women or prostate-specific antigen blood test for men. We created a variable based on the number of preventive care activities they received in the last two years, with scores ranging from 0 to 3.
To calculate a health literary score, 1 point was given for each of the 8 test words on the REALM-R that was pronounced correctly. Scores between 0 and 6 were considered poor literacy and scores of 7 or 8 were considered adequate literacy.18
We classified participants as having read the newsletter if they reported having read all or some of it. Some participants were not asked the newsletter questions because they were deceased, dropped out before their first follow-up, were lost to follow-up, or received a version of the follow-up questionnaire that did not have the newsletter questions. Participants were considered as not having read the newsletter if they were not asked the newsletter questions, did not remember receiving it, had not read any of it, or did not know if they read it.
There were four points in time that interaction with the study participants could affect eye examination behavior – after enrollment, after the newsletter was sent, and after the first and second follow-up phone calls. Timing was first calculated by determining where on the timeline the DFE occurred. If a DFE occurred either before or within three days of the newsletter being mailed we classified the timing as before receipt of the intervention. If, at the first or second phone call, a person reported having an appointment scheduled, and the DFE occurred within six weeks of the call date, we reasoned that the phone call did not affect the decision to have an eye exam and adjusted the timing. If the DFE occurred before the first follow-up or after the third phone call no adjustments were made.
Sample size and statistical methods
Based on sample size calculations, we needed 130 people in the tailored and targeted groups to give us 90% power to detect a minimum difference in eye examination rates of 20% between the groups. We felt differences less than 20% would not justify the added time, expense, and complexity of using tailored rather than targeted messages. Assuming an 80% follow-up rate, our goal was to enroll 165 people in each group, for a total of 330 people enrolled in the study. Because our follow-up rates were higher than 80%, our final sample size yielded 95% power to detect a 20% difference between groups.
For the analysis, we first compared participants by intervention group for key baseline demographic variables. Also selected were independent variables from the baseline questionnaire that could have an impact on eye examination behavior, including health-related variables, literacy score, and behavioral intention. To examine our primary outcome measure, we compared doctor-confirmed DFE rates at 6 months between those randomized to the tailored and targeted groups, based on intent-to-treat analysis. We also compared demographic variables and DFE status for participants with complete, partial, and no follow-up. To determine if other factors were associated with getting a DFE, we compared those who did and did not have a doctor-confirmed DFE by demographic and other variables.
Pearson’s chi square was used to compare dichotomous variables and Mantel-Haenszel chi-square was used for ordinal response variables. For small cell size, Fisher’s exact test was used. Relative risks and 95% confidence intervals were calculated to assess the strength of the association between covariates and getting a DFE. Analyses were performed using SAS 9.1 (SAS Institute, Gary, NC).
We conducted logistic regression analyses, using a doctor-confirmed DFE as the outcome variable, and calculated odd ratios and 95% confidence intervals. Covariates considered in the logistic regression analysis included those variables that were statistically significant, or approached significance (P values <.25), in the univariate analysis. Intervention group was also included in the model.
Results
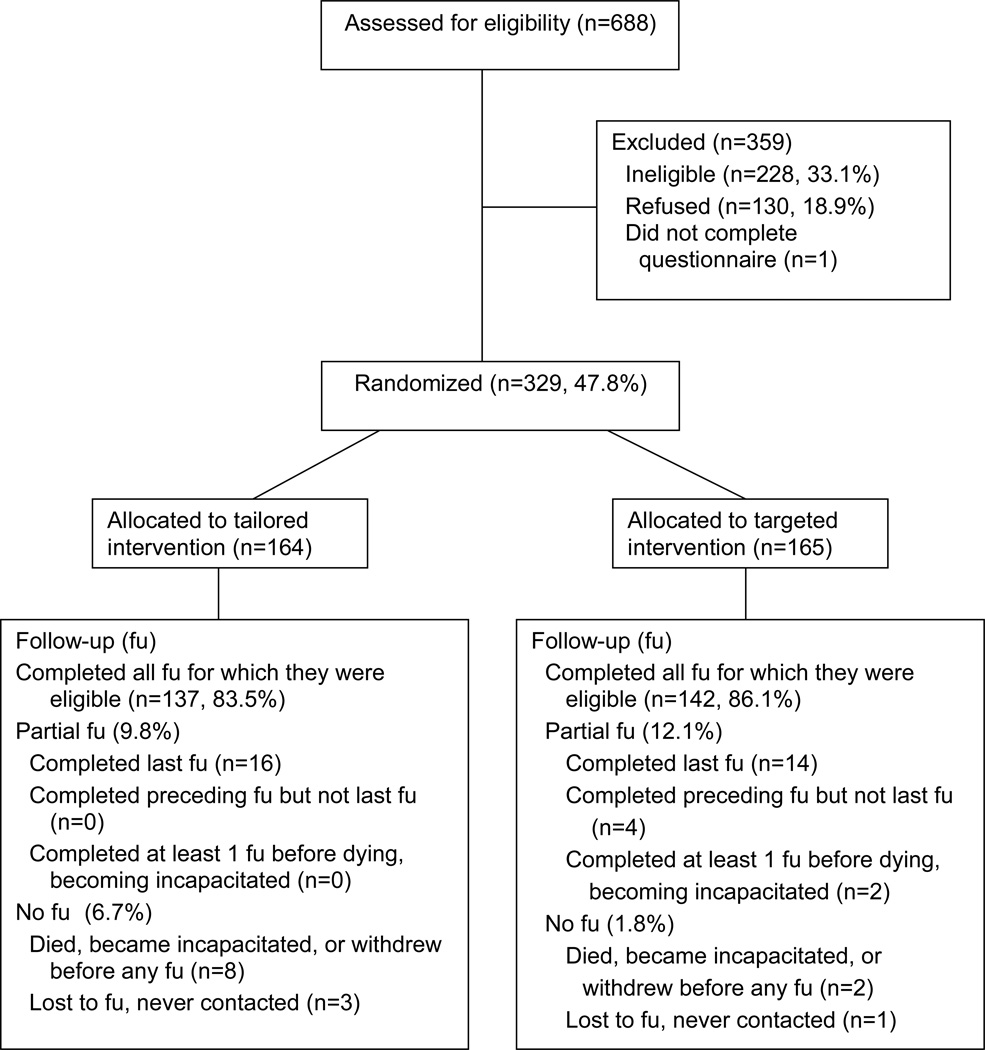
We enrolled 329 participants between June, 2007 and September, 2008, with 164 randomized to receive the tailored newsletter and 165 randomized to receive the targeted newsletter, as shown in Figure 1. One person signed a consent form but did not complete the questionnaire and was never randomized. Of the 329 participants randomized, 279 (84.8%) completed all follow-up calls for which they were eligible, 14 (4.3%) had no follow-up information, and 36 (10.9%) had partial follow-up. There was no difference in follow-up rates between the two intervention groups (χ2=5.1 P=.08).
Figure 1.
Follow-up status of 329 study participants
As shown in Table 2, at baseline the intervention groups were comparable in terms of demographic and other variables. We then compared these variables by follow-up status and found a statistically significant association between follow-up status and age, gender, health status, and preventive care. Participants who were 80 or older, males, those who reported poor health, and those with no preventive care in the past two years were less likely to have complete follow-up.
Table 2.
Comparison of demographic and other variables by intervention groups
| Tailored No. (%) |
Targeted No. (%) |
Total % |
χ2 value (P-value) | |
|---|---|---|---|---|
| Age | ||||
| 65–69 | 65 (39.6) | 70 (42.4) | 41.0 | |
| 70–79 | 72 (43.9) | 75 (45.5) | 44.7 | |
| ≥ 80 | 27 (16.5) | 20 (12.1) | 14.3 | 1.12 (0.29) |
| Gender | ||||
| male | 43 (26.2) | 57 (34.6) | 30.4 | |
| female | 121 (73.8) | 108(65.4) | 69.6 | 2.70 (0.10) |
| Education | ||||
| < h.s. | 66 (40.5) | 76 (46.1) | 43.3 | |
| h.s. grad | 56 (34.4) | 49 (29.7) | 32.0 | |
| some college | 27 (16.6) | 27 (16.4) | 16.5 | |
| college grad | 14 (8.6) | 13 (7.9) | 8.2 | 0.46 (0.50) |
| Incomea | ||||
| < $20,000 | 110 (79.7) | 107 (73.3) | 76.4 | |
| $20,000–29,999 | 16 (11.6) | 25 (17.1) | 14.4 | |
| ≥ $30,000 | 12 (8.7) | 14 (9.6) | 9.2 | 1.23 (0.27) |
| General health | ||||
| excellent | 20 (12.2) | 25 (15.2) | 13.7 | |
| good | 84 (51.2) | 86 (52.1) | 51.7 | |
| fair | 55 (33.5) | 49 (29.7) | 31.6 | |
| poor | 5 (3.1) | 5 (3.0) | 3.0 | 0.74 (0.39) |
| Preventive care | ||||
| 0 | 10 (6.1) | 10 (6.1) | 6.1 | |
| 1 | 29 (17.7) | 36 (21.8) | 19.8 | |
| 2 | 75 (45.7) | 71 (43.0) | 44.4 | |
| 3 | 50 (30.5) | 48 (29.1) | 29.8 | 0.33 (0.56) |
| Has glaucoma | ||||
| yes | 11 (6.7) | 19 (11.6) | 9.2 | |
| no | 153 (93.3) | 145 (88.4) | 90.8 | 2.35 (0.12) |
| Has diabetes | ||||
| yes | 39 (23.9) | 33 (20.0) | 22.0 | |
| no | 124 (76.1) | 132 (80.0) | 78.0 | 0.74 (0.39) |
| Has retinopathy | ||||
| yes | 3 (7.7) | 8 (25.0) | 15.5 | |
| no | 36 (92.3) | 24 (75.0) | 84.5 | FETb (0.06) |
| Last DFE | ||||
| < 5 years | 74 (46.5) | 79 (48.8) | 47.7 | |
| > 5 years | 49 (30.8) | 47 (29.0) | 29.1 | |
| never | 36 (22.6) | 36 (22.2) | 22.4 | 0.09 (0.77) |
| Literacy score | ||||
| adequate | 60 (36.8) | 61 (37.0) | 36.9 | |
| poor | 103 (63.2) | 104 (63.0) | 63.1 | 0.00 (0.98) |
| Read newsletter | ||||
| yes | 85 (51.8) | 78 (47.3) | 49.5 | |
| no | 79 (48.2) | 87 (52.7) | 50.5 | 0.68 (0.41) |
| Behavioral intention | ||||
| 1-never thought about | 27 (16.5) | 20 (12.1) | 14.3 | |
| 2-decided no | 3 (1.8) | 4 (2.4) | 2.1 | |
| 3-still deciding | 20 (12.2) | 38 (23.0) | 17.6 | |
| 4-plan in 6 months | 40 (24.4) | 42 (25.4) | 24.9 | |
| 5-plan in 1 month | 74 (45.1) | 61 (37.0) | 41.0 | 8.07 (0.09) |
excludes 45 people who refused to answer or were not sure
Fisher’s exact test
We compared participants who reported reading the newsletter with those who did not and found statistically significant differences for age (χ2MH=15.98, P<.0001), income (χ2MH=12.97, P=.0003) and literacy score (χ2=4.47, P=.0345). Participants 80 years and older and those with income less than $20,000 were less likely to read the newsletter. Among those with adequate literacy scores 57.0% read the newsletter compared to 44.9% with poor literacy. Although we found a statistically significant association between behavioral intention and last DFE (χ2=19.2, P=.01), no clear pattern emerged.
Dilated fundus exams
One hundred forty one participants reported having a DFE and an additional 14 people reported making an appointment at the six-month call. Of these 155 self-reports, 128 (82.6%) were confirmed by the doctor’s office as being dilated. Nine self-reports were reported to be non-dilated, two people did not show up for their appointment, and there was no record of an exam for 16 people. To assess the accuracy of the exam dates, we compared the month and year reported by the participant to the date given by the confirming doctor’s office. Of the 135 records with both dates, 79.3% had exact agreement and 95.6% were off by one month.
Based on 128 doctor-confirmed DFEs, 38.9% of the study participants had a DFE. As shown in Table 3, there was no difference in doctor-confirmed DFEs by intervention group (RR=1.07, 0.82–1.40 CI), with 40.2% of participants in the tailored group and 37.6% of participants in the targeted group having a doctor-confirmed DFE. Excluding the 20 people without last or any follow-up did not change the results. We further explored DFE rates by examining the timing of the exam in relation to the follow-up calls. As shown in Table 4, there was no difference in timing of DFEs by intervention group (χ2=1.2, P=.76).
Table 3.
Association between demographic and other variables and doctor-confirmed DFE
| DFE No. (%) |
No DFE No. (%) |
Relative risk (95% CI) | |
|---|---|---|---|
| Intervention group | |||
| tailored | 66 (40.2) | 98 (59.8) | 1.07 (0.82–1.40) |
| targeted | 62 (37.6) | 103 (62.4) | |
| Age | |||
| 65–69 | 51 (37.8) | 84 (62.2) | 1.18 (0.74–1.89) |
| 70–79 | 62 (42.2) | 85 (57.8) | 1.32 (0.84–2.09) |
| ≥ 80 | 15 (31.9) | 32 (68.1) | referent |
| Gender | |||
| male | 33 (33.0) | 67 (97.0) | 0.80 (0.58–1.09) |
| female | 95 (41.5) | 134 (58.5) | |
| Education | |||
| < h.s. | 55 (38.7) | 87 (61.3) | referent |
| h.s. grad | 40 (38.1) | 65 (61.9) | 0.98 (0.71–1.35) |
| some college | 18 (33.3) | 36 (66.7) | 0.86 (0.56–1.32) |
| college grad | 15 (55.6) | 12 (44.4) | 1.43 (0.96–2.13) |
| Incomea | |||
| < $20,000 | 87 (40.1) | 130 (59.9) | referent |
| $20,000–29,999 | 12 (29.3) | 29 (70.7) | 0.73 (0.44–1.21) |
| ≥ $30,000 | 14 (53.8) | 12 (46.2) | 1.34 (0.91–1.99) |
| General health | |||
| excellent | 17 (37.8) | 28 (62.2) | 1.89 (0.52–6.90) |
| good | 71 (41.8) | 99 (58.2) | 2.09 (0.59–7.30) |
| fair | 38 (36.5) | 66 (63.5) | 1.82 (0.52–6.47) |
| poor | 2 (20.0) | 8 (80.0) | referent |
| Preventive care | |||
| 0 | 5 (25.0) | 15 (75.0) | referent |
| 1 | 21 (32.3) | 44 (67.7) | 1.29 (0.56–2.98) |
| 2 | 57 (39.0) | 89 (61.0) | 1.56 (0.71–3.43) |
| 3 | 45 (45.9) | 53 (54.1) | 1.84 (0.83–4.04) |
| Has glaucoma | 12 (40.0) | 18 (60.0) | 1.03 (0.65–1.63) |
| Has diabetes | 32 (44.4) | 40 (55.6) | 1.19 (0.88–1.61) |
| Has retinopathy | 5 (45.4) | 6 (54.6) | 1.17 (0.61–2.28) |
| Last DFE | |||
| < 5 years | 66 (43.1) | 87 (56.9) | 1.55 (1.03–2.35) |
| > 5 years | 37 (38.5) | 59 (61.5) | 1.39 (0.88–2.18) |
| never | 20 (27.8) | 52 (72.2) | referent |
| Literacy score | |||
| adequate | 59 (48.8) | 62 (51.2) | 1.46 (1.12–1.91) |
| poor | 69 (33.3) | 138 (66.7) | |
| Read newsletter | |||
| yes | 76 (46.6) | 87 (53.4) | 1.49 (1.13–1.97) |
| no | 52 (31.3) | 114 (68.7) | |
| Behavioral intention | |||
| 1-never thought about | 15 (31.9) | 32 (68.1) | 1.54 (0.80–2.97) |
| 2-decided no | 1 (14.3) | 6 (85.7) | 0.60 (0.10–4.54) |
| 3-still deciding | 12 (20.7) | 46 (79.3) | referent |
| 4-plan in 6 months | 39 (47.6) | 43 (52.4) | 2.30 (1.32–4.00) |
| 5-plan in 1 month | 61 (45.2) | 74 (54.8) | 2.18 (1.28–3.74) |
excludes 45 people who refused to answer or were not sure
Table 4.
Timing of dilated fundus exams by intervention groups
| Timing of DFE | Tailored No. (%) |
Targeted No. (%) |
Total % |
χ2 value (P-value) |
|---|---|---|---|---|
| Before receipt of intervention | 5 (7.6) | 5 (8.1) | 7.8 | |
| Before 1st phone call | 28 (42.4) | 21 (33.9) | 38.3 | |
| After 1st phone call | 19 (28.8) | 19 (30.6) | 29.7 | |
| After 2nd phone call | 14 (21.2) | 17 (27.4) | 24.2 | 1.17 (0.76) |
To determine if other factors were associated with getting a DFE, we calculated the relative risk for getting a DFE for select variables, as shown in Table 3. We found no association between any of the demographic variables and getting a DFE. However, there was a statistically significant association between getting a DFE and timing of previous DFE, literacy score, reading the newsletter, and behavioral intention. Compared to participants who never had a DFE, participants whose last DFE was 2–5 years ago were 1.5 times as likely to have a doctor-confirmed DFE. People with an adequate health literacy score were 1.5 times as likely to have a DFE compared to participants with poor literacy, and participants who read the newsletter were 1.5 times as likely to have a DFE compared to those who did not read it. We also found that those planning on making an appointment for a DFE in the next month or 6 months were twice as likely to have a DFE as participants who had not decided yet about getting a DFE. We found similar results after excluding participants who withdrew or were lost to follow-up.
Table 5 presents results of logistic regression analysis for predictors of getting a DFE. Reading the newsletter and planning on making an appointment for a DFE remained significant predictors.
Table 5.
Predictors for getting dilated fundus exams
| Odds ratio (95% CI) | |
|---|---|
| Intervention group | |
| tailored vs. targeted | 0.95 (0.59, 1.54) |
| Gender | |
| female vs. male | 1.34 (0.77, 2.34) |
| Preventive care | |
| 0 | referent |
| 1 | 1.04 (0.28, 3.85) |
| 2 | 1.59 (0.47, 5.44) |
| 3 | 1.96 (0.56, 6.91) |
| Read newsletter | 1.76 (1.08, 2.87) |
| Last DFE | |
| < 5 years | 1.62 (0.85, 3.09) |
| > 5 years | 1.58 (0.79, 3.18) |
| never | referent |
| Literacy score | |
| adequate vs. poor | 1.61 (0.97, 2.66) |
| Behavioral intention | |
| planning (stage 4, 5) vs. | 2.46 (1.42, 4.26) |
| precontemplation (stage 1,2,3) |
Discussion
Our hypothesis that older African Americans receiving the tailored intervention would have higher rates of doctor-confirmed DFEs than participants receiving the targeted newsletter was not confirmed. Both approaches were equally effective in promoting DFEs at six months; 40% of participants who received the tailored newsletter and 38% who received the targeted newsletter had DFEs. Although these rates may not seem high, they are comparable to a recent study comparing a tailored telephone intervention to a generic print intervention in a population of diabetics, where 34% of participants receiving tailored phone messages had a confirmed DFE within 6 months.13
The impact of the intervention on DFE rates is complicated by the additional contacts we had with participants, although this should not have affected our primary comparison because follow-up procedures were the same for both groups and project staff were unaware of group assignment. Although 38% of the DFEs occurred before the first phone call and after the intervention was received, an additional 54% occurred after at least one phone call. For the 8% of DFEs occurring before receipt of the newsletter, the enrollment process may have been a motivating factor. Although some of our study participants may have gotten a DFE without any intervention, it is unlikely that we would have achieved a 39% DFE rate in these previously noncompliant participants.
Most studies examining the effectiveness of tailored messages have shown small but significant changes in health behavior when compared to non-tailored messages, although there have been other studies where no differences were observed.24, 25 As the degree of customization of health messages increases, and as audience segmentation increases, cost and effort also increase. Our study confirms that targeted messages that meet the specific needs of their audience can be as effective as tailored messages for promoting eye examination behavior, and questions whether the added cost of tailored interventions is justified.26, 27 Therefore, these results suggest that well-designed targeted print messages delivered in a community-setting with a moderate degree of customization and segmentation can motivate older African Americans to get DFEs.
In our population, behavioral intention was the strongest predictor of getting a DFE. Participants in the contemplation or preparation stage were 2.5 times more likely to get a DFE than participants in the precontemplation stage, with 46% having a doctor-confirmed DFE. DFE rates were higher among participants who had never thought about getting a DFE compared to those still deciding or those who had decided not to get one, suggesting that an intervention may be more successful among those who never thought about the behavior than among those who had given the behavior some thought but had not taken any action.
Reading the newsletter, which measures compliance with the intervention, was also a predictor of getting a DFE. The odds of having a DFE were 1.8 times higher among those who read the newsletter than those who did not. Participants with poor health literacy were significantly less likely to read the newsletter compared to those with adequate literacy. Even an intervention written at a 6th grade reading level may not appropriate for all members of the intended audience, suggesting the need to identify other intervention approaches which may be more effective with individuals having poor health literacy.
Our finding that this older African American population was actively engaged in preventive health practices, as evidenced by 94% having some contact with the health care system in the past two years, suggests the need for the eye care community to work more closely with primary care physicians and other health professionals to encourage discussions about eye care with their patients who are at increased risk of eye disease. Recommendations by primary care professionals to get eye examinations may be important to augment the delivery of the message to undergo DFEs.
Study participants were relatively reliable in reporting DFEs, with 82% of self-reports confirmed, and with 96% of the dates given for the exam within one month of the actual date. Although confirmation of self-reported DFEs remains the gold standard, it is reassuring that self-reports can give a reasonable estimate if they cannot be confirmed because of cost or time limitations that arise in both research and clinical settings.
Our study had several limitations. We conservatively estimated that only half the study participants read the newsletter. Although we had some loss to follow-up, we completed all follow-up calls or the last follow-up call for 94% of our study population. A third limitation was the use of self-reported DFE utilization as an eligibility criterion. Reporting errors may have resulted in people being included who were actually ineligible or excluded although they were in fact eligible. Another limitation was that confirmation of eye examination status was by office staff rather than medical record abstraction. To encourage office staff to access the medical information rather than simply agree or disagree with our information, we asked them to report the date and type of exam. Twenty-seven (17%) of the self-reported DFEs that were not confirmed were not included in the analysis.
Although results from this study may not be generalizable to the U.S. population 65 years and older, the proportion of participants who graduated from high school or had some college was similar to the U.S. general population.28 Our participants were similar to the U.S. population of blacks, 65 and older, in terms of self-reported health, with 35% in our study reporting fair or poor health compared to 39% in the U.S. overall. Perhaps as a reflection of self-selection, our study participants were more likely to report having trouble seeing even with glasses, with 35% of males and 31% of females reporting this, compared to 14% and 19% respectively in the U.S. population 65 and older.29
Our findings support the effectiveness of both targeted and tailored health messages for promoting DFEs among individuals 65 years and older who are at increased risk of glaucoma. Given the additional time and cost needed to develop tailored messages, our results have important implications for developing health communication strategies to promote eye-care seeking behavior in adults at increased risk of eye disease that can be disseminated in a variety of settings.
Acknowledgements
This study was supported by grant R01EY15899, National Institutes of Health, Bethesda, MD. Dr. Nancy Ellish had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Contributor Information
Nancy J. Ellish, University of Maryland School of Medicine Department of Ophthalmology and Visual Sciences, Baltimore, MD
Renee Royak-Schaler, University of Maryland School of Medicine, Department of Epidemiology and Preventive Medicine, Baltimore, MD
Eve J. Higginbotham, Howard University, Washington, DC
References
- 1.U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2nd ed. U.S. Government Printing Office; 2000. [Google Scholar]
- 2.National Health Education Program. National Eye Institute; 1991. Communication plan: a diabetic eye disease education program for people with diabetes. Report. [Google Scholar]
- 3.National Health Education Program. National Eye Institute; 1994. Communication plan: a glaucoma public education program. Report. [Google Scholar]
- 4.Ellish NJ, Royak-Schaler R, Passmore SR, et al. Knowledge, attitudes, and beliefs about dilated eye examinations among African-Americans. Invest Ophthalmol Vis Sci. 2007;48:1989–1994. doi: 10.1167/iovs.06-0934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawkins RP, Kreuter M, Resnicow K, et al. Understanding tailoring in communicating about health. Health Educ Res. 2008;23:454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kreuter MW, Farrell D, Olevitch L, Brennan L. Tailoring health messages Customizing communication with computer technology. Mahway, New Jersey: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 7.Kreuter MW, Bull FC, Clark EM, et al. Understanding how people process health information: a comparison of tailored and nontailored weight-loss materials. Health Psychol. 1999;18:487–494. doi: 10.1037//0278-6133.18.5.487. [DOI] [PubMed] [Google Scholar]
- 8.Brug J, Campbell M, van AP. The application and impact of computer-generated personalized nutrition education: a review of the literature. Patient Education & Counseling. 1999;36:145–156. doi: 10.1016/s0738-3991(98)00131-1. [DOI] [PubMed] [Google Scholar]
- 9.Skinner CS, Strecher VJ, Hospers H. Physicians Recommendations for Mammography - do Tailored Messages Make A Difference. Am J Public Health. 1994;84:43–49. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strecher VJ. Computer-tailored smoking cessation materials: a review and discussion. Patient Education & Counseling. 1999;36:107–117. doi: 10.1016/s0738-3991(98)00128-1. [DOI] [PubMed] [Google Scholar]
- 11.Basch CE, Walker EA, Howard CJ, et al. The effect of health education on the rate of ophthalmic examinations among African Americans with diabetes mellitus. Am J Public Health. 1999;89:1878–1882. doi: 10.2105/ajph.89.12.1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Legorreta AP, Hasan MM, Peters AL, et al. An intervention for enhancing compliance with screening recommendations for diabetic retinopathy. A bicoastal experience. Diabetes Care. 1997;20:520–523. doi: 10.2337/diacare.20.4.520. [DOI] [PubMed] [Google Scholar]
- 13.Walker EA, Schechter CB, Caban A, et al. Telephone intervention to promote diabetic retinopathy screening among the urban poor. Am J Prev Med. 2008;34:185–191. doi: 10.1016/j.amepre.2007.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strecher VJ, Rosenstock IM. The health belief model. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education. Theory, research, and practice. 2nd ed. San Francisco: Jossey-Bass Publishers; 1997. pp. 41–59. [Google Scholar]
- 15.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 16.Weinstein ND, Sandman PM. A Model of the Precaution Adoption Process - Evidence from Home Radon Testing. Health Psychol. 1992;11:170–180. doi: 10.1037//0278-6133.11.3.170. [DOI] [PubMed] [Google Scholar]
- 17.Ellish NJ, Scott D, Royak-Schaler R, et al. Community-based strategies for recruiting older, African Americans into a behavioral intervention study. J Natl Med Assoc. 2009;101:1104–1111. doi: 10.1016/s0027-9684(15)31105-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bass PF, III, Wilson JF, Griffith CH. A shortened instrument for literacy screening. J Gen Intern Med. 2003;18:1036–1038. doi: 10.1111/j.1525-1497.2003.10651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rakowski W, Ehrich B, Dube CE, et al. Screening mammography and constructs from the Transtheoretical Model: Associations using two definitions of the stages-of-adoption. Ann Behav Med. 1996;18:91–100. doi: 10.1007/BF02909581. [DOI] [PubMed] [Google Scholar]
- 20.Glaucoma Eye-Q test. National Eye Institute Website. 2010
- 21.Diabetic eye disease Eye-Q test. National Eye Institute Website. 2010
- 22.Pasagian-Macaulay A, Basch CE, Zybert P, et al. Ophthalmic knowledge and beliefs among women with diabetes. Diabetes Educ. 1997;23:433–437. doi: 10.1177/014572179702300408. [DOI] [PubMed] [Google Scholar]
- 23.National Institutes of Health. National Cancer Institute; 1997. Theory at a glance. A guide for health promotion practice. Report. [Google Scholar]
- 24.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- 25.Sohl SJ, Moyer A. Tailored interventions to promote mammography screening: a meta-analytic review. Prev Med. 2007;45:252–261. doi: 10.1016/j.ypmed.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kreuter MW, Oswald DL, Bull FC, et al. Are tailored health education materials always more effective than non-tailored materials? Health Educ Res. 2000;15:305–315. doi: 10.1093/her/15.3.305. [DOI] [PubMed] [Google Scholar]
- 27.Lairson DR, DiCarlo M, Myers RE, et al. Cost-effectiveness of targeted and tailored interventions on colorectal cancer screening use. Cancer. 2008;112:779–788. doi: 10.1002/cncr.23232. [DOI] [PubMed] [Google Scholar]
- 28.U.S. Census Bureau. Census 2000, Summary File 1; generated by Nancy Ellish; using American Factfinder. [20 July 2006]; < http://factfinder.census.gov>.
- 29.Older Americans Update 2006: Key indicators of well-being. Washington, DC: U.S. Government Printing Office; 2006. May, Federal Agency Forum on Aging-Related Statistics. [Google Scholar]