Abstract
Purpose
To describe community-based strategies that were effective in recruiting older, African-Americans into a behavioral intervention study designed to increase eye examination behavior.
Methods
Sites were identified that targeted older African-Americans, including senior centers, senior housing, and church groups. We conducted presentations at these sites, networked with community organizations, placed ads on the radio and in newspapers, and attended health fairs. Potential participants also called us in response to flyers and through word of mouth.
Results
We conducted 147 activities at 118 sites. A total of 688 potential participants were screened, with 330 (48%) enrolling, 33% ineligible, and 19% not interested. Highest enrollment rates were for word of mouth (69%), flyers (67%), and senior centers (66%). Barriers to participation included hesitancy of seniors to leave their apartments to attend presentations and competing health issues taking precedence over eye concerns.
Conclusions
A multi-faceted recruitment approach, incorporating both direct and indirect activities at a variety of sites, should be used to recruit older African Americans into a behavioral intervention study. Establishing relationships in the community, both prior to initiating recruitment activities and as an ongoing process, was important to the study’s success.
Keywords: recruitment, African-Americans, seniors, community-based
Background
With the 1984 NIH directive requiring the inclusion of women and minorities in clinical trials,1 research related to increasing participation by these groups has increased. In particular, studies have discussed barriers to recruiting African-Americans into clinical research studies, and strategies to address these barriers. Some of these studies have focused on recruitment for prevention or health promotion studies,2–4 where recruitment can be more difficult compared to treatment trials5 or observational studies.6 Studies have also addressed strategies for recruiting older participants,7, 8 as well as older, African-American participants.9–12
For African-Americans, a history of racial discrimination and exploitation, including the use of slaves for medical experimentation, continues to be an impediment to participation in clinical research.6, 13–17 In particular, the Tuskegee syphilis experiment has come to exemplify exploitation and misconduct in medical research.16 Mistrust of the medical community, including mistrust of doctors, researchers, and medical and academic institutions, as well as negative personal experience with the health care system, are also barriers to participation.2, 13, 15, 17–21 Lack of information about the disease being studied,19, 22 lack of support from family members or their church,18 and an ongoing need to prioritize other social requirements, such as paying for housing and food versus health needs,20 also serve as barriers to recruitment.
To address distrust issues, many studies recommend establishing relationships with the community, especially with both formal and informal community leaders.6, 14, 19, 23, 24 Direct contact with potential participants improves recruitment of African-Americans8 and older people.25 Other strategies to increase participation include matching the gender and race of the research staff to the target population,4, 10, 26 and being flexible to the needs of potential participants.27
Information is still limited, however, in applying and evaluating recruitment strategies in disease prevention and health promotion studies for African-Americans, 65 years and older. Therefore, the purpose of this paper is to describe our recruitment process, focusing on the strategies we successfully used in conducting a behavioral intervention study to increase eye examination behavior in a community-dwelling urban population of older African-Americans. This study addressed two Healthy People 2010 objectives: 1. To increase the proportion of persons who have a dilated eye examination (DEE) at appropriate intervals, and 2. To increase the proportion of adults with diabetes who have an annual DEE.28
Materials and Methods
The E.Y.E. (Examine Your Eyes) Project, a NIH-funded randomized clinical trial, was designed to test the efficacy of tailored versus targeted messages in a behavioral intervention to encourage African Americans 65 and older to have DEEs. We focused on this population because African-Americans are at increased risk of developing glaucoma, experience more serious consequences of glaucoma, and tend to have fewer eye examinations than their Caucasian counterparts. In addition, those 65 and older have Medicare coverage for annual eye exams for glaucoma, which is currently underutilized.
The study consisted of four components: (1) an interviewer-administered questionnaire to collect baseline demographic information and information about behavioral intention, knowledge about eye exams, glaucoma, diabetes, and diabetic retinopathy, barriers and benefits to getting DEEs, and doctor-patient communication; (2) the intervention mailed in the form of a newsletter with either tailored or targeted messages; (3) telephone follow-up of study participants at one-, three, and six-months to ascertain their eye-examination status; and (4) confirmation of self-reported DEEs with their doctors.
Recruitment
After developing a study logo to create an identity for the project, we then identified sites throughout Baltimore City that targeted African-American seniors. This was based on contacts already established by our community outreach worker, internet searches for senior centers and senior housing in Baltimore city, contacting city organizations, and networking. For most of the sites, we first called or visited in person. After this initial contact we usually met with the managers of senior housing complexes, coordinators at senior centers, officers of senior organizations, and lay leaders or health ministers at churches.
Some sites requested that we send flyers and information about the project before agreeing to a meeting. After these contacts, we scheduled presentations for potential participants at the sites. Some presentations were held during already scheduled activities, such as residents’ meetings, “Eating Together” programs, and senior group meetings. Other presentations were scheduled specifically for our project. At a few sites, we recruited participants by approaching older African-Americans directly to tell them about the project and ask if they were interested in participating.
We also attended meetings of various community organizations, such as tenant councils representing numerous senior housing complexes and neighborhood community associations, and met with representatives from several Baltimore City agencies. We attended small health fairs sponsored by churches and senior centers, as well as large, city-wide festivals. For the health fairs, we were contacted and asked to participate by community sources as well as through University of Maryland contacts. Ads were run on two radio stations which were selected because of their large African-American and older audience, and we had a story about the project reported on a local television station during National Glaucoma month. We also placed ads in a local African-American newspaper, and had two papers for seniors pick up the story and run ads and stories for free. In addition, we conducted a letter writing campaign with area churches, and then followed up by phone with some of the churches. People also heard about the E.Y.E. project through word-of-mouth, mostly from study participants. Our recruitment process was approved by the University of Maryland Institutional Review Board.
As part of our data collection, we recorded the number of people who attended our recruitment events, the number of people we screened for eligibility, if ineligible the reason for ineligibility, and the number of refusals. For some of the larger events, particularly the health fairs, the number of people who attended was estimated. In addition, when we recruited people by approaching them directly, the number of people who we approached was often not recorded. Therefore, the number of people we screened is not accurate for this activity.
Enrollment
During our presentations in community settings, or at the health fairs, potential participants could sign up if they were interested in participating in the project. Some sites used our flyers or made up their own posters to advertise the date and time of our presentation. If the presentations were small enough, we tried to enroll potential participants at that time. If not, potential participants were called to schedule appointments for enrollment. Potential participants also called us in response to our advertisements, flyers, and word of mouth referrals. People who called about the study were asked how they heard about the project.
All interested individuals were screened for eligibility, based on self-reports. To be eligible to participate in the E.Y.E. project an individual had to be 65 years of age or older, African American, not having a DEE for two years prior to enrollment, and not having an appointment for a DEE scheduled within a month of enrollment.
Research staff enrolled participants and conducted interviews primarily at the recruitment sites, although some interviews were conducted at private residences or at our office. Once deemed eligible, consenting of the participant was completed along with supplemental paperwork to collect personal and alternative contact information. This was followed by the administration of the questionnaire by a trained interviewer. The enrollment process took about 45 minutes, and participants were paid $25 for their time. In addition, several give-aways pertinent to the overall objectives of the study were distributed to the participants at the completion of their enrollment process.
Statistical analysis
We categorized recruitment sites by region and type of venue. Baltimore City zip codes were combined into nine geographic regions based on Baltimore City planning and police districts. We then estimated the distribution of African Americans 65 and older in these nine regions, using data from the 2000 census.29 After grouping the 55 community statistical areas of Baltimore City to correspond to the nine geographic regions, we multiplied the number of people 65 and older in the region by the percent of African-Americans in that region.
Venues were classified as churches, community organizations, health fairs, newspaper and other print media, radio or TV ads, senior centers, senior housing, and senior organizations. Included in the “other” category were government organizations, sororities, and adult day care centers. Activities were grouped into direct and indirect recruitment methods. Direct activities, where we interacted face-to-face with potential participants, included presentations, health fairs, and directly approaching people. Indirect activities, which required potential participants to contact us, included newspaper, radio, and television ads, flyers, and word of mouth.
To evaluate our recruitment effectiveness, we calculated two different enrollment proportions. The enrollment yield among those screened was calculated by dividing the number of people who enrolled by the total number of people screened, while the enrollment yield among those eligible used the same numerator but used the number of people eligible as the denominator.
Frequency distributions were used to summarize the data. We compared enrollment yields by type of activity and type of venue, using chi-squared analysis. We also compared enrollment yields for health fairs and presentations by type of venue, using either the chi-square test or Fisher’s exact test if expected cell frequencies were less than five. All statistical analysis was performed using SAS 9.1.
Results
Our recruitment phase occurred between January, 2006 and September, 2007. During the first six months of recruitment, our efforts primarily consisted of establishing community partnerships by providing information to possible sites, staffing tables at health fairs, and meeting with the staff of various groups. We started enrolling participants in June, 2006.
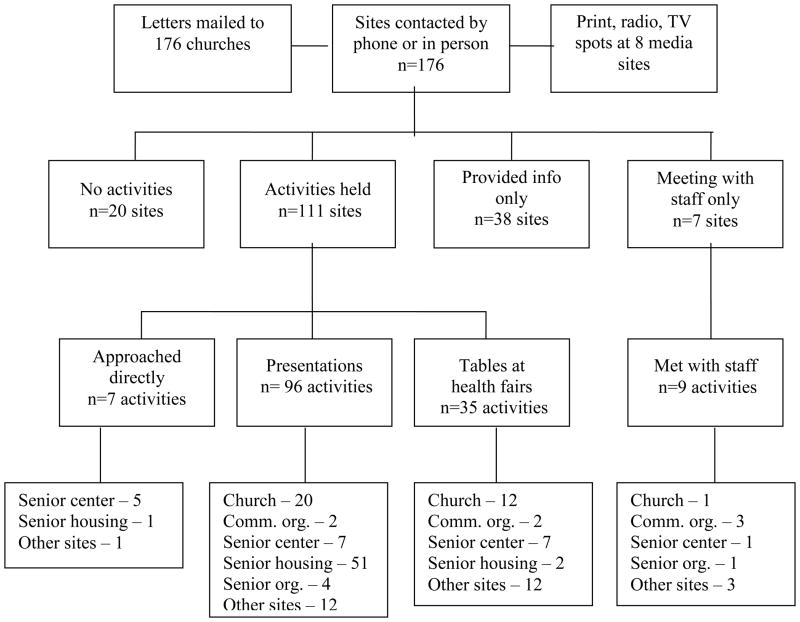
An overview of our recruitment strategies is shown in Figure 1. In addition to the letters mailed to churches and the media campaign, we contacted sites by phone or in person. Of the 176 sites contacted by phone or in person, 20 did not have any recruitment activities because they were either not interested or did not have an African-American clientele. For 38 sites we only provided information and for seven sites we just met with staff. We conducted presentations, recruited directly, or worked at health fairs at the remaining 111 sites. The major focus of our recruitment activities was presentations, which represented 65.3% of our activities. Additional activities included staffing tables at health fairs (23.8%), meeting with staff (6.1%) and directly approaching people without having a presentation (4.8%). Overall, 37% of our activities were held at senior housing locations, and an additional 22% were held at churches. The majority of the presentations took place at senior housing sites (53%), with churches accounting for an additional 21% of the presentations. Thirty-four percent of the health fairs were held at churches and another 34% occurred at other sites. Two thirds of our meetings with staff occurred at either community organizations or other sites. Because some sites had multiple activities, we held these 147 activities at 118 sites, as presented in Table 1.
Figure 1.
Flow diagram of recruitment activities
Table 1.
Enrollment status of 688 potential participants by recruitment venue and activity
| Recruitment venue and activity | Enrolled | Ineligible | Not interested | Screened | Sites no. | ||||
|---|---|---|---|---|---|---|---|---|---|
| no. | % | no. | % | no. | % | no. | % | ||
| Church | 38 | 11.5 | 34 | 14.9 | 14 | 10.8 | 86 | 12.5 | 31 |
| Health fair | 6 | 21 | 9 | ||||||
| Presentation | 32 | 13 | 5 | ||||||
| Directly approach | 0 | 0 | 0 | ||||||
| Senior center | 46 | 13.9 | 13 | 5.7 | 11 | 8.5 | 70 | 10.2 | 10 |
| Health fair | 13 | 8 | 7 | ||||||
| Presentation | 13 | 4 | 4 | ||||||
| Directly approach | 20 | 1 | 0 | ||||||
| Senior housing | 140 | 42.4 | 72 | 31.6 | 60 | 46.2 | 272 | 39.5 | 45 |
| Health fair | 1 | 1 | 1 | ||||||
| Presentation | 131 | 68 | 57 | ||||||
| Directly approach | 8 | 3 | 2 | ||||||
| Senior organization | 12 | 3.6 | 6 | 2.6 | 17 | 13.1 | 35 | 5.1 | 4 |
| Health fair | 0 | 0 | 0 | ||||||
| Presentation | 12 | 6 | 17 | ||||||
| Directly approach | 0 | 0 | 0 | ||||||
| Other sites | 22 | 6.7 | 39 | 17.1 | 18 | 13.8 | 79 | 11.5 | 23 |
| Health fair | 5 | 15 | 6 | ||||||
| Presentation | 13 | 13 | 10 | ||||||
| Directly approach | 4 | 11 | 2 | ||||||
| Community org. | 0 | 0.0 | 1 | 0.4 | 1 | 0.8 | 2 | 0.3 | 5 |
| Newspaper | 6 | 1.8 | 10 | 4.4 | 1 | 0.8 | 17 | 2.5 | |
| Radio/TV | 6 | 1.8 | 30 | 13.2 | 2 | 1.5 | 38 | 5.5 | |
| Saw flyer | 22 | 6.7 | 9 | 4.0 | 2 | 1.5 | 33 | 4.8 | |
| Word of mouth | 36 | 10.9 | 14 | 6.1 | 2 | 1.5 | 52 | 7.6 | |
| Unknown | 2 | 0.6 | 0 | 0.0 | 2 | 1.5 | 4 | 0.6 | |
| Total | 330 | 228 | 130 | 18.9 | 688 | 118 | |||
We screened a total of 688 potential participants from our various recruitment venues. As shown in Table 1, 330 people (48.0%) enrolled, representing 71.7% of those eligible, 228 (33.1%) were deemed ineligible, and 130 (18.9%) either refused to participate or could not be contacted to schedule an enrollment appointment. Senior housing accounted for 40% of the people screened, while churches, senior centers, and ‘other sites’ each accounted for approximately 10% of the people screened.
In terms of enrollment, senior housing facilities accounted for 42% of the people who enrolled, with presentations at senior housing the predominant activity. We did not enroll any people from community organizations because those sites were primarily for presenting information about the project rather than for recruitment. We found low rates of uninterested people for our media campaign (5%), flyers (6%), and word of mouth (4%).
Approximately 80% of the people screened in response to our radio and television ads were ineligible, and more than half the people screened in response to our newspaper ads were ineligible. Almost half of those deemed ineligible had a DEE within two years (49.6%), and an additional 32.9% were younger than 65 years. Other reasons for ineligibility included not being African-American (4.8%), having an appointment for a DEE already scheduled (6.6%), and miscellaneous reasons (6.1%).
We then examined enrollment yields among those screened and among those eligible, for activity and venue separately, as shown in Table 2. The highest enrollment rates for activities were for word of mouth and flyers, with rates among those screened of 69% and 67%, respectively. Although the enrollment rate for directly approaching people was high, because the number of people we approached was not always recorded, this rate may not be accurate. Lowest enrollment rates were for health fairs (27%) and print and radio ads (22%). For venues, the highest enrollment rate among those screened was 66% for senior centers, and the lowest rate was for ‘other sites’ (28%). There was a statistically significant association between activity and enrollment among those screened (χ2=51.18, P<.0001) and among those eligible (χ2=24.68, P=.0002). We also found statistically significant associations between venue and enrollment among those screened (χ2=26.09, P<.0001) and among those eligible (χ2=17.82, P=.0013).
Table 2.
Enrollment yields among screened and eligible by activity and venue
| Enrollment yield | ||
|---|---|---|
| Among those screened | Among those eligible | |
| Activities | ||
| Health fair | 26.9 | 52.1 |
| Presentation | 50.5 | 68.4 |
| Directly approach | 62.8 | 88.9 |
| Print/radio | 21.8 | 80.0 |
| Word of mouth | 69.2 | 94.7 |
| Flyer | 66.7 | 91.7 |
| χ2=51.18, P<.0001 | χ2=31.35, P<.0001 | |
| Venues | ||
| Church | 44.2 | 73.1 |
| Senior center | 65.7 | 80.7 |
| Senior housing | 51.5 | 70.0 |
| Senior organization | 34.3 | 41.4 |
| Other sites | 27.8 | 55.0 |
| χ2=26.09, P<.0001 | χ2=17.82, P=.0013 | |
Enrollment yields were also examined for direct and indirect recruitment activities. Among those screened, 48% of participants recruited by direct activities enrolled compared to 50% recruited by indirect activities (χ2=0.26, P=.61). However, among those eligible, 68% were recruited by direct activities compared to 91% recruited by indirect activities, a difference that was statistically significant (χ2=16.3, P<.0001).
We then compared enrollment rates for health fairs and presentations, controlling for venue. We did not include directly approaching people because the numbers were too small to stratify by venue. Enrollment yields were higher for presentations than for health fairs for all venues, although this difference was only statistically significant for churches.
Efforts were made to recruit a geographic representation of senior African Americans from all regions of Baltimore City by holding events at sites throughout the city, as shown in Table 3. The distribution of sites we contacted was similar to the distribution of African Americans 65 and older living in Baltimore City. We also compared the demographics of the 330 people who enrolled with Baltimore City data. Our enrolled population was somewhat younger and more educated than Baltimore City residents. Among the 65 and older population in Baltimore City, 26% were 65–69, 48% were 70–79, and 26% were 80 years and older, whereas for our enrolled population 41% were 65–69, 45% were 70–79, and 14% were 80 years or older. Our study population was 70% female compared to 62% of the 65 and older residents of Baltimore City. Although the proportion of people with at least some college was similar between the two groups, 43% of our enrolled population had less than a high school education and 32% were high school graduates compared to 57% and 20%, respectively, of Baltimore City residents 65 and older.
Table 3.
Frequency distribution of sites contacted, activities conducted, participants recruited, and population of African Americans 65 and older, by region of Baltimore City
| Region | Sites contacted | Activities conducted | Participants recruited | AA population 65 and older |
|---|---|---|---|---|
| C | 10.2 | 12.9 | 9.6 | 4.4 |
| E | 6.8 | 4.8 | 13.7 | 10.2 |
| N | 9.1 | 8.2 | 12.1 | 7.4 |
| NE | 14.2 | 10.2 | 9.2 | 19.0 |
| NW | 22.7 | 24.5 | 30.9 | 22.0 |
| S | 5.7 | 4.8 | 1.6 | 3.7 |
| SE | 2.8 | 2.0 | 0.6 | 2.8 |
| SW | 12.5 | 11.6 | 6.7 | 13.9 |
| W | 15.9 | 21.1 | 15.6 | 17.5 |
Discussion
We utilized a multi-faceted recruitment strategy, primarily conducting direct activities at numerous venues, but supplemented by indirect activities, to successfully recruit our sample of older, African-Americans. A multi-faceted approach has been reported to generate better results than using a single recruitment strategy.4, 11 The majority of our recruitment efforts were through face-to face presentations, where we were able to interact directly with potential participants. This activity allowed us to answer questions about the project and explain the inclusion criteria. Presentations were also an efficient use of staff time. Health fairs required staffing for several hours, or for the entire day for large fairs, with no enrollment taking place on that day. When we directly approached people we also spent several hours at a site, but were often able to enroll people the same day. Putting up flyers and word of mouth required little staff time and were not costly, whereas the media campaign was the most expensive recruitment method. Direct interaction has been reported as better at reaching minorities,8 and the preferred approach of older people.25 Although one health promotion study of minority women reported higher recruitment rates for “passive” methods compared to “active” methods3, their definition included direct mailing as active and speaking at groups as passive.
The association we found between activity type and enrollment was due to a number of factors. People recruited through indirect activities, which included word of mouth and seeing our flyers, as well as through media activities, had low refusal rates since they had to call us if they were interested. However, this was offset by the large rate of ineligibles who responded to our media campaign, even though we specified the inclusion criteria in our radio, television and newspaper ads. Therefore, our enrollment yield from the radio, television, and newspapers was relatively low, while enrollment yield from word of mouth and flyers was high. Presentations yielded consistently higher enrollment rates than health fairs for all venues because ineligibility rates for health fairs were always higher than for presentations. Two health promotion studies reported higher rates of ineligibility among potential participants recruited through the media, and a higher proportion of eligible participants from face-to-face interactions. 5, 12 A clinical trial of older women found that senior centers and mass mailings yielded higher enrollment rates than churches.30
Some barriers to participation are specific to the elderly. Through our meetings with site managers and coordinators, we learned that seniors living in their housing complexes might be hesitant to attend on-site presentations regardless of the topic because they were selective about which causes drew them from their apartments. Seniors can feel socially isolated,31 and are concerned about being victims of crime or identity theft. 10, 31 Memory issues were occasionally a problem during recruitment, especially related to eligibility criteria. In several instances, a potential participant was deemed eligible after our meeting at a presentation, only to find at a subsequent phone call to schedule the interview that the information they had given us regarding their age or date of last eye examination had changed. Although some researchers report transportation as a barrier to recruitment,19, 25 this was less of an issue in our study because we only required one face-to-face encounter, which usually took place at the original recruitment site. Focus groups with this same urban population did not find transportation to be an issue.32
In some instances we encountered resistance on the part of relatives, particularly related to time constraints and uncertainty about how we would use the personal information we collected. Sometimes competing health issues took precedence over eye concerns. Although we used colorful, easy to read posters, we found that many potential participants thought they would be receiving a free eye examination. This misunderstanding was reported in another behavioral intervention study of African-American adults.24
We encountered barriers in gaining access to some of our venues. Although some churches have health ministries to address the health concerns of their senior parishioners, for some church officials the E.Y.E. Project was a low priority. One study suggests that church-based recruitment may not be cost-effective because of differing agendas and the low priority placed on research by some pastors.10 We also found that the hierarchy of leadership in many churches created a maze of approval levels that had to be charted before engaging in any degree of collaboration. With the senior housing facilities, some of the on-site managers were not responsive to our requests for access to their sites. However, we were able to seek the approval of a Tenant’s Council, an organization whose members represented most of the larger senior housing complexes in Baltimore City, to gain access to the sites. Although it has been suggested to work from the bottom up, starting with the service providers who know their clientele well rather than high level administrators,10, 26 which is what we tried to do, sometimes it was necessary to go over the heads of the service providers.
With the senior centers, the issue was not access, but rather that their event calendars filled quickly. Therefore, it was sometimes necessary to schedule presentations several months in advance. We found that scheduling our presentations to coincide with specific programs worked well. For example, the “Eating Together” programs and Golden Age clubs sponsored by Baltimore City served as great opportunities to have a significant number of interested seniors gathered together for the dual purposes of networking and hearing about the E.Y.E. Project. Health fairs, while not suitable for offering privacy during the informed consent and interview process, are useful venues for disbursing study literature and building community goodwill.
We employed several strategies suggested in the literature to increase recruitment among African-Americans. Establishing relationships with the community is frequently cited as a way to overcome distrust, especially prior to recruitment.3, 9, 14, 23, 24 We spent the first six months of our recruitment phase working with previously established contacts, and meeting with managers, coordinators, and church leaders to establish relationships in the community. This provided us with names of specific venues that targeted older African Americans, and facilitated the scheduling of presentations at specific sites by making the E.Y.E Project known in the community. These meetings with informal and formal community leaders, and providing information to sites, continued throughout the study. In addition, although health fairs may be less effective for enrolling participants than other activities, we found them to be important in building relationships within the community.
The importance of the research staff should also be considered. Three of the four staff members of the E.Y.E Project who interacted in the community were African-American women, as suggested by several researchers.4, 10, 26 Sometimes what may be considered minor points can impact recruitment, such as the personal attributes of the staff,27 showing respect by addressing this older population by their formal name,9, 23, 33 or allowing for social interaction and conversation before starting the research protocol.9 Our staff was respectful to the potential participants, and was flexible both with the timing and location of our presentations and enrollment interviews. We attended evening and weekend events, and went to the target population to conduct interviews instead of having them come to us.
Although we were successful in enrolling 330 senior African Americans, this study had several limitations. Because we focused our efforts on presentations, some potential recruitment opportunities were not fully developed. Although we obtained a list of beauty and barber shops in the region, we only provided information to a few of these sites. Likewise, we did not recruit in food stores or pharmacies, although these strategies were discussed. While we recruited from a variety of settings and geographic areas, the enrolled sample was younger and more educated than the elderly population of Baltimore city. Low literacy and poor health status in this population may lead to selection bias.12 Also contributing to selection bias may be that people who chose to attend our presentations may already have an interest in the project and possess a level of understanding regarding eye disease that differs from those who chose not to attend.30 Although part of our procedures manual, at some of the larger recruitment activities we did not keep an accurate count of the number of people who attended the event, which can affect the calculation of the proportion of people screened.
Conclusion
We successfully recruited 330 older African Americans into a behavioral intervention study using a multi-faceted approach. Direct recruitment activities, such as presentations, should be the focus of efforts to recruit African Americans and seniors. However, these efforts should be supplemented with indirect methods, like posting flyers at venues frequented by seniors and having current participants tell their friends and relatives about the study, which do not involve much time or effort, yet have high enrollment yields. We found it important to establish relationships in the community, both prior to initiating recruitment activities and as an ongoing process, by working with both formal and informal community leaders. This can include networking with both old and new contacts and attending community organizational meetings. Health fairs are another good way to build community rapport. Also keep in mind some of the smaller issues which can impact successful recruitment, such as scheduling presentations during already scheduled activities, which provides you with a ready-made audience, or spending a few minutes talking with potential participants prior to the research activities.
Footnotes
Financial disclosure statement: Supported by a grant from the National Institutes of Health, R01EY15899, Bethesda, MD
Contributor Information
Nancy J. Ellish, Email: nellish@umaryland.edu, Department of Ophthalmology and Visual Sciences, University of Maryland School of Medicine, Baltimore
Deborah Scott, Email: peony55567@yahoo.com, Department of Ophthalmology and Visual Sciences, University of Maryland School of Medicine; Baltimore.
Renee Royak-Schaler, Email: rroyak@som.umaryland.edu, Department of Epidemiology and Preventive Medicine, University of Maryland School of Medicine, Baltimore.
Eve J. Higginbotham, Email: ejhigginbotham@msm.edu, Morehouse School of Medicine, Atlanta
References
- 1.NIH guidelines on the inclusion of women and minorities as subjects in clinical research. Federal Register. 1994;59:14508. [Google Scholar]
- 2.El-Khorazaty MN, Johnson AA, Kiely M, et al. Recruitment and retention of low-income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. BMC public health. 2007;7:233. doi: 10.1186/1471-2458-7-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee RE, McGinnis KA, Sallis JF, et al. Active vs. passive methods of recruiting ethnic minority women to a health promotion program. Ann Behav Med. 1997;19:378–384. doi: 10.1007/BF02895157. [DOI] [PubMed] [Google Scholar]
- 4.Wilbur J, McDevitt J, Wang E, et al. Recruitment of African American women to a walking program: eligibility, ineligibility, and attrition during screening. Res Nurs Health. 2006;29:176–189. doi: 10.1002/nur.20136. [DOI] [PubMed] [Google Scholar]
- 5.Gilliss CL, Lee KA, Gutierrez Y, et al. Recruitment and retention of healthy minority women into community-based longitudinal research. J Womens Health Gend Based Med. 2001;10:77–85. doi: 10.1089/152460901750067142. [DOI] [PubMed] [Google Scholar]
- 6.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 7.Greaney ML, Lees FD, Nigg CR, et al. Recruiting and retaining older adults for health promotion research: the experience of the SENIOR Project. Journal of Nutrition for the Elderly. 2006;25:3–22. doi: 10.1300/j052v25n03_02. [DOI] [PubMed] [Google Scholar]
- 8.MacEntee MI, Wyatt C, Kiyak HA, et al. Response to direct and indirect recruitment for a randomised dental clinical trial in a multicultural population of elders. Community Dent Oral Epidemiol. 2002;30:377–381. doi: 10.1034/j.1600-0528.2002.00003.x. [DOI] [PubMed] [Google Scholar]
- 9.Dennis BP, Neese JB. Recruitment and retention of African American elders into community-based research: lessons learned. Arch Psychiatr Nurs. 2000;14:3–11. doi: 10.1016/s0883-9417(00)80003-5. [DOI] [PubMed] [Google Scholar]
- 10.Levkoff S, Sanchez H. Lessons learned about minority recruitment and retention from the Centers on Minority Aging and Health Promotion. Gerontologist. 2003;43:18–26. doi: 10.1093/geront/43.1.18. [DOI] [PubMed] [Google Scholar]
- 11.Qualls CD. Recruitment of African American adults as research participants for a language in aging study: example of a principled, creative, and culture-based approach. J Allied Health. 2002;31:241–246. [PubMed] [Google Scholar]
- 12.Warren-Findlow J, Prohaska TR, Freedman D. Challenges and opportunities in recruiting and retaining underrepresented populations into health promotion research. Gerontologist. 2003;43:37–46. doi: 10.1093/geront/43.suppl_1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dancy BL, Wilbur J, Talashek M, et al. Community-based research: barriers to recruitment of African Americans. Nurs Outlook. 2004;52:234–240. doi: 10.1016/j.outlook.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 14.Killien M, Bigby JA, Champion V, et al. Involving minority and underrepresented women in clinical trials: the National Centers of Excellence in Women’s Health. J Womens Health Gend Based Med. 2000;9:1061–1070. doi: 10.1089/152460900445974. [DOI] [PubMed] [Google Scholar]
- 15.Corbie-Smith G, Thomas SB, St George DM. Distrust, race, and research. Arch Intern Med. 2002;162:2458–2463. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- 16.Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87:1773–1778. doi: 10.2105/ajph.87.11.1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moreno-John G, Gachie A, Fleming CM, et al. Ethnic minority older adults participating in clinical research: developing trust. J Aging Health. 2004;16:93S–123S. doi: 10.1177/0898264304268151. [DOI] [PubMed] [Google Scholar]
- 18.Farmer DF, Jackson SA, Camacho F, et al. Attitudes of African American and low socioeconomic status white women toward medical research. J Health Care Poor Underserved. 2007;18:85–99. doi: 10.1353/hpu.2007.0008. [DOI] [PubMed] [Google Scholar]
- 19.Arean PA, Gallagher-Thompson D. Issues and recommendations for the recruitment and retention of older ethnic minority adults into clinical research. J Consult Clin Psychol. 1996;64:875–880. doi: 10.1037//0022-006x.64.5.875. [DOI] [PubMed] [Google Scholar]
- 20.Napoles-Springer AM, Santoyo J, Stewart AL. Recruiting ethnically diverse general internal medicine patients for a telephone survey on physician-patient communication. J Gen Intern Med. 2005;20:438–443. doi: 10.1111/j.1525-1497.2005.0078.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shavers VL, Lynch CF, Burmeister LF. Racial differences in factors that influence the willingness to participate in medical research studies. Ann Epidemiol. 2002;12:248–256. doi: 10.1016/s1047-2797(01)00265-4. [DOI] [PubMed] [Google Scholar]
- 22.Smith YR, Johnson AM, Newman LA, et al. Perceptions of clinical research participation among African American women. J Womens Health (Larchmt) 2007;16:423–428. doi: 10.1089/jwh.2006.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adderley-Kelly B, Green PM. Strategies for successful conduct of research with low-income African American populations. Nurs Outlook. 2005;53:147–152. doi: 10.1016/j.outlook.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 24.Russell KM, Maraj MS, Wilson LR, et al. Barriers to recruiting urban African American women into research studies in community settings. Appl Nurs Res. 2008;21:90–97. doi: 10.1016/j.apnr.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Witham MD, McMurdo ME. How to get older people included in clinical studies. Drugs Aging. 2007;24:187–196. doi: 10.2165/00002512-200724030-00002. [DOI] [PubMed] [Google Scholar]
- 26.Alvarez RA, Vasquez E, Mayorga CC, et al. Increasing minority research participation through community organization outreach. West J Nurs Res. 2006;28:541–560. doi: 10.1177/0193945906287215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Julion W, Gross D, Barclay-McLaughlin G. Recruiting families of color from the inner city: insights from the recruiters. Nurs Outlook. 2000;48:230–237. doi: 10.1067/mno.2000.102992. [DOI] [PubMed] [Google Scholar]
- 28.U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2. U.S. Government Printing Office; 2000. [Google Scholar]
- 29.2000 Census Summary File One (SF1) - Maryland Population Characteristics. [Accessed December 23, 2008];Baltimore Neighborhood Indicators Alliance. 2002 Aug; Available at: URL: www.mdp.state.md.us/msdc/BNIA/bnia_idx.htm.
- 30.Unson CG, Ohannessian C, Kenyon L, et al. Barriers to eligibility and enrollment among older women in a clinical trial on osteoporosis: effects of ethnicity and SES. J Aging Health. 2004;16:426–443. doi: 10.1177/0898264304264211. [DOI] [PubMed] [Google Scholar]
- 31.Stahl SM, Vasquez L. Approaches to improving recruitment and retention of minority elders participating in research: examples from selected research groups including the National Institute on Aging’s Resource Centers for Minority Aging Research. J Aging Health. 2004;16:9S–17S. doi: 10.1177/0898264304268146. [DOI] [PubMed] [Google Scholar]
- 32.Ellish NJ, Royak-Schaler R, Passmore SR, et al. Knowledge, attitudes, and beliefs about dilated eye examinations among African-Americans. Invest Ophthalmol Vis Sci. 2007;48:1989–1994. doi: 10.1167/iovs.06-0934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Topp R, Newman JL, Jones VF. Including African Americans in health care research. West J Nurs Res. 2008;30:197–203. doi: 10.1177/0193945907303063. [DOI] [PubMed] [Google Scholar]