Abstract
Background
The initial graft tension applied at the time of anterior cruciate ligament (ACL) reconstruction alters joint contact and may influence cartilage health. The objective was to compare outcomes between two commonly used “laxity-based” initial graft tension protocols.
Hypothesis
We hypothesized that; 1) the high-tension group would have less knee laxity, improved clinical and patient-oriented outcomes, and less cartilage damage than the low-tension group after 36-months of healing, and 2) the outcomes of the high-tension group would be equivalent to those of a matched control group.
Study Design
Randomized controlled clinical trial.
Methods
Ninety patients with isolated unilateral ACL injuries were randomized to undergo ACL reconstruction using one of two initial graft tension protocols; 1) autografts tensioned to restore normal anteroposterior (AP) laxity at the time of surgery (i.e., “low-tension”; n=46) and 2) autografts tensioned to over-constrain AP laxity by 2 mm (i.e., “high-tension”; n=44). Sixty matched healthy subjects formed the control group. Outcomes were assessed pre-operatively, intra-operatively, and at 6-, 12- and 36-months after surgery.
Results
No significant differences were found between the two initial graft tension protocols for any of the outcome measures at 36-months. However, there were differences when comparing the two treatment groups to the control group. On average, AP laxity was 2 mm greater in the ACL reconstructed groups than in the control group (p<.007). IKDC knee evaluation scores (p<0.001), peak isokinetic knee extension torques (p<.027), and 4 out of 5 of the Knee Osteoarthritis Outcome Scores (KOOS; p<.05) were significantly worse than the control group. SF-36 scores and re-injury rates were similar between groups at 36-months. Although there were significant radiographic and MRI changes present in the ACL reconstructed knees of both treatment groups, the magnitude was relatively small and likely clinically insignificant at 36-months.
Conclusions
Both laxity-based initial graft tension protocols produced similar outcomes without fully restoring joint function and KOOS scores when compared to the control group. There was minimal evidence of cartilage damage 36-months after surgery.
Keywords: anterior cruciate ligament (ACL), autograft, reconstruction, tension, outcomes
INTRODUCTION
ACL reconstruction is commonly performed to restore joint function and to decrease the risk of post-traumatic osteoarthritis (OA) in the ACL-injured knee. The initial tension applied to the graft affects knee laxity and joint contact forces, and hence may be responsible for OA.6 Although recommendations for initial graft tension have been reported,4,8 the optimal tension to restore native knee stability while minimizing the risk of degenerative joint disease is unknown. There are two “laxity-based” graft tension approaches that are commonly used in practice.2 The first is to set the tension such that the anteroposterior (AP) laxity of reconstructed knee is equal to the contralateral uninjured knee at time of fixation. The second is to tension the graft to initially over-constrain the joint so that normal AP laxity is achieved when the graft stretches out during rehabilitation. The advantage of a laxity-based protocol over a force-based approach (e.g., 80N for all patients) is that the tension can be individualized to a patient by matching the laxity of the uninjured leg.11 Although several prospective clinical studies have been performed to evaluate the effects of initial graft tension, all evaluated force-based protocols, and none focused on the integrity of articular cartilage.4,14,17,27,31,33
The objective of this study was to compare clinical, functional, patient-oriented, and OA imaging outcome measures of two common initial graft tension protocols following ACL reconstruction with 36-months follow-up in a randomized double-blind controlled trial. The two laxity-based tension protocols under investigation were; 1) to restore normal AP laxity at the time of surgery relative to the contralateral uninjured knee (i.e., the “low-tension” group), or 2) to constrain AP laxity by 2 mm (i.e., the “high-tension” group). We hypothesized that; 1) the high-tension group would have less AP laxity, improved functional and patient-oriented outcomes, and less cartilage damage than the low-tension group after 36-months, and 2) the outcomes for the high-tension group would be equivalent to a gender-, race-, and age-matched control group.
MATERIAL AND METHODS
Trial Design
The Institutional Review Boards of Rhode Island Hospital, Miriam Hospital, Memorial Hospital and Brown University approved the study. All subjects granted their informed consent. The prospective randomized controlled trial was based on an intent-to-treat analysis of the two laxity-based initial graft tension protocols. The statistician (GJB) performed the randomization, which was disclosed to the surgeon via a sealed envelope intra-operatively. Although designed as a double-blind trial, the operating surgeon (PDF, MJH, or RMS) was informed of the randomization assignment at time of graft implantation. No investigators were allowed to review the assignments during the post-operative follow-up period and remained blinded until after all of the 36-month visits were completed.
Prior to initiating the study, a power analysis determined that 45 subjects per group would be necessary to detect a mean change in joint space width of 5% (1 − β=0.80; α=0.05) when assuming half of the subjects would exhibit OA changes.12,18 Based on this sample size, the study was powered to detect a 16% change in AP laxity, 12% change in International Knee Documentation Committee (IKDC) score, 12% change in peak isokinetic torque, and 10% change in the Knee Osteoarthritis Outcome Scores (KOOS).
Participants and Entry Criteria
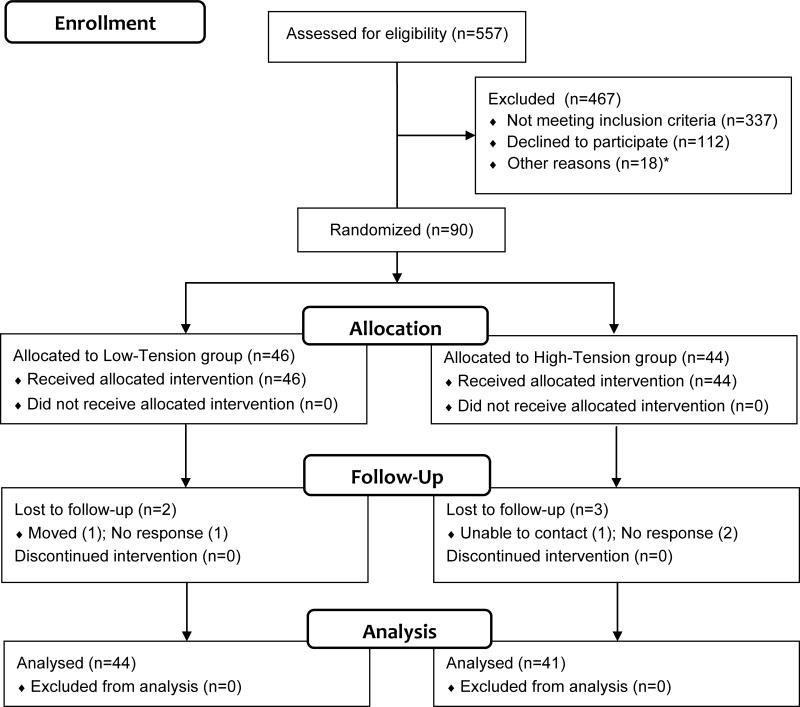
All patients who presented with a unilateral ACL injury in the clinics of three surgeons over three years (02/2004 to 02/2007) were assessed for eligibility (Table 1). Of the 557 patients screened (Fig. 1), 337 of them were excluded; due to ineligible graft type (allograft; 95 patients), previous knee injuries (78 patients), chronic knee injuries (66 patients), concomitant injuries (48 patients), age restrictions (30 patients), contralateral knee injuries (7 patients), partial ACL tears (3 patients), and other reasons (10 patients). Of the remaining 220 patients, 112 declined to participate and 108 were enrolled into the study. Of these 108 patients, 15 were disqualified due to intra-operative findings and 3 opted out of the study just prior to surgery. Of the 90 patients randomized between the two groups (low-tension, n=46; high-tension, n=44), only five (5.5%) were lost to follow-up. Of these, 86% filled out the questionnaires, and 79% returned for the on-site follow-up examination. It was also our intent to establish an independent control group that matched the characteristics of the population at risk. Sixty control subjects were recruited from the local area, and selected to match the frequency of individuals by age, gender, race (african american, hispanic, caucasian, other), and activity level (Table 1).
Table 1.
Inclusion/exclusion criteria for subject enrollment.
| Treatment Groups (High- and Low-tension) | |
| Inclusion Criteria | Male or female subjects between the ages of 15 and 50 years with unilateral ACL injury |
| Candidates for ACL reconstruction using bone-patellar tendon-bone or four- stranded hamstring tendon autograft | |
| A Tegner activity score ≥ 2 | |
| Meniscal tears involving <1/3 of the meniscus | |
| Exclusion Criteria | An ACL tear occurring more than 12-months prior to the 1st office visit |
| Previous injury to either knee | |
| Increased clinical laxity of the MCL, LCL, or PCL as compared to the control knee | |
| Evidence of degenerative arthritis on radiographs | |
| Pregnancy | |
| Diseases that predispose a patient for articular cartilage damage | |
| Moderate sized fissures or lesions in articular cartilage | |
| Meniscal tears involving more than 1/3 of meniscus | |
| Control Group | |
| Inclusion Criteria | Male or female subjects between the ages of 18 and 50 years |
| A Tegner activity score ≥ 2 | |
| Exclusion Criteria | Previous injury to either knee |
| Increased laxity of the MCL, LCL, or PCL compared to the control knee | |
| Evidence of degenerative arthritis on radiographs | |
| Pregnancy | |
| Diseases that predispose a patient to articular cartilage damage | |
Fig. 1.
CONSORT Flow Diagram (Adapted from Schulz et al).24 A sex, age, and activity level matched control group was also recruited (n=60) of which 48 remained in the study at 36-months.
ACL Reconstruction/Initial Graft Tension Protocols
Patients were reconstructed either with a bone-patellar tendon-bone autograft obtained from the central third of the ipsilateral patellar tendon, or a four-stranded autograft created from the semitendinosis and gracilis tendons. Graft type was selected by the patient. All surgeons followed the same operative procedures using the same transtibial drill guide system (Smith & Nephew; Andover MA) and anatomic landmarks to select graft insertion sites at the center of the native ACL insertions. Grafts were preconditioned with 20 manual tension cycles before placing them in the joint. For the patellar tendon grafts, the bone blocks were secured using titanium interference screws. The hamstring tendon grafts were fixed with a button on the femur and a biodegradable interference screw on the tibia backed up at the surgeon’s discretion with a screw and spiked soft tissue washer to capture the graft. For those patients receiving the low-tension assignment, the grafts were tensioned by firmly pulling on the distal graft with the knee at 0° of knee flexion.11 For those receiving the high-tension assignment, the grafts were firmly tensioned with the knee at 30° of knee flexion.11 Tibial fixation was partially engaged and AP laxity at 20° of flexion was checked using the KT-1000S (MEDmetrics Inc; San Diego CA) and compared to that of the contralateral knee under anesthesia. A sterilizable goniometer was used to verify the knee angle before testing. If the desired laxity value was not achieved to less than 1 mm of the desired value, the fixation was released, and the procedure repeated. Post-operatively, all subjects followed a standardized rehabilitation program designed to get them back to sport within 6 months.5
Clinical Outcomes
AP laxity values for both knees were measured using the KT-1000 Knee Arthrometer (MEDMetric Corporation, San Diego CA) pre-operatively and at all post-operative time points. Posterior and anterior directed shear loads were applied in succession to find the neutral position of the knee. Three manual maximum tests were performed and the displacement readings averaged. The difference between legs was reported. One examiner (HLO), with more than six years of experience, performed all of the KT-1000/KT-1000S measurements.
Clinical outcome was assessed using the 2000 IKDC Knee Examination Score (http://www.sportsmed.org).13 The IKDC scores evaluate four categories: 1) function, 2) symptoms, 3) range of knee motion, and 4) clinical examination. The IKDC score rates knees as normal (A), nearly normal (B), abnormal (C), and severely abnormal (D), with the final IKDC rating based on the score of the worst category.13 Subsequent surgical procedures on the ipsilateral or contralateral knee during follow-up were determined by patient questioning and medical record review. A trained sports physical therapist (HLO) administered all clinical and functional examinations.
Functional Outcomes
Subjects performed the 1-leg hop test for distance independently three times and the trials were averaged.22 The mean hop distance of the injured knee was normalized to that of the uninjured contralateral knee. Isokinetic strength testing (Biodex 3; Biodex Medical Systems, Inc. Shirley NY) was performed at 60°/sec to assess the strength of the extensor muscles of each knee.20 Peak torques for five repetitions were averaged and normalized with respect to bodyweight and height.
Patient-Oriented Outcomes
The KOOS23 and the SF-36v228 were implemented to assess patient-oriented outcomes. The KOOS evaluates five domains: 1) knee related quality of life, 2) sports and recreation function, 3) activity of daily living, 4) symptoms, and 5) pain.23 The SF-36 evaluates general health related to physical function, role limitations, bodily pain, vitality, social functioning, mental health, and health transition.28 Activity levels were monitored using the Tegner activity scale.26 Questionnaires were administered pre-operatively and at all follow-up visits.
OA Imaging Outcomes
Medial joint space width measurements were obtained from radiographs pre- and postoperatively using the semi-flexed metatarsophalangeal (MTP) view.7 Radiographs were taken of each knee, and the medial compartment joint space width was measured at the midline of the compartment in the coronal plane using a validated computer algorithm.19 The overall condition of the joint was assessed pre- and post-operatively using a modified Osteoarthritis Research Society International (OARSI) radiographic grading scale.1 Posterior-anterior and lateral radiographs of both knees were taken before surgery and at the 12- and 36-month follow-up visits. A grade of 0 (normal) to 4 (severe) was assigned to two different radiographic features: osteophyte formation and joint space narrowing. In addition, sclerosis, attrition, and ligament calcification were assessed on a dichotomous scale. The maximum possible score was 47. An experienced musculoskeletal radiologist (GAT) scored all films blinded.
The OA status of the knee was assessed using the semi-quantitative Whole Organ Magnetic Imaging Score (WORMS).21 The score utilizes MRI sequences to grade 14 independent features; cartilage signal and morphology, sub-articular bone marrow abnormality, sub-articular cysts, sub-articular bone attrition, marginal osteophytes evaluated in 15 regions. The condition of the menisci, cruciate and collateral ligaments, synovitis, loose bodies, and periarticular cysts were also included for a total possible score of 332 points. WORMS were performed by the experienced musculoskeletal radiologist (GAT) who was blinded. MRI was added to the protocol after half of the subjects were recruited into the study and were thus performed on a subset of the patients (n=28, n=25, and n=13 for the low-tension, high-tension and control groups, respectively).
Statistical Methods
Repeated measures ANOVA were used to evaluate differences among treatment groups with respect to temporal changes in the outcome variables. The statistical models included fixed factors representing treatment group (low-tension, high-tension and control) and time. The limb serving as the “operated knee” for the control subjects was randomly selected to match the proportion of left/right knees in the injured groups. If significant interactions were detected, F-tests corresponding to simple effects were examined. Pairwise comparisons were performed using Fisher’s LSD. Chi-square tests were utilized to compare the frequency of subsequent surgeries between groups, and to compare the distributions of IKDC score between groups at each assessment. All means presented represent least square means and their associated 95% confidence intervals (CI). P-values less than .05 were considered significant.
RESULTS
Patient Characteristics/Intra-Operative Findings
At the 36-month visit, 2 low-tension, 3 high-tension and 12 control subjects were lost to follow-up. Gender, age, weight, time between injury and index surgery, the ratio of patients receiving patellar tendon to hamstring tendon grafts, and the percentages of patients with minor meniscal injuries or minor chondral lesions were similar between the two initial graft tension groups (Table 2). Pre-operatively, the AP laxity values between the two tension groups were not significantly different (p=.437) but significantly greater than the control group (p<.001; Table 3). The Tegner Activity Scores were also not significantly different between the two treatment groups (p=.987), though, the control group was 1.1±0.8 points lower (p<.006; Table 3).
Table 2.
Subject data for participants in the low-tension, high-tension, and control groups (Sx=surgery).
| Low -tension | High-tension | Control | P-value | |
|---|---|---|---|---|
| Subjects randomized | 46 | 44 | 60 | - |
| Dropouts | 2 | 3 | 12 | - |
| # of subjects @36-months | 44 | 41 | 48 | - |
| Age in years, mean ± 95% CI | 24±2.7 | 23±2.1 | 25±1.6 | .028 |
| Weight in Kg, mean ± 95% CI | 73±5.0 | 69±4.9 | 72±3.6 | .586 |
| Days to surgery, mean ± 95% CI | 114±23.2 | 105±20.0 | - | .679 |
| Gender | ||||
| Males, # (%) | 24 (52.2) | 18 ( 40.9) | 34 (56.7) | .275 |
| Females, # (%) | 22 (47.8) | 26 (59.1) | 26 (43.3) | |
| Graft type | ||||
| B-PT-B, # (%) | 31 (67.4) | 27 (61.4) | - | .550 |
| Hamstring, # (%) | 15 (32.6) | 17 (38.6) | - | |
| Meniscal lesions at Sx* | ||||
| Medial, # (%) | 11 (23.9) | 11 (25.0) | - | .905 |
| Lateral, # (%) | 8 (17.4) | 7 (15.9) | - | .850 |
| Chondral lesions at Sx** | ||||
| Medial, # (%) | 3 (6.5) | 1 (2.2) | - | .328 |
| Lateral, # (%) | 5 (10.9) | 9 (20.4) | - | .210 |
Minor debridement or repair
Grade II or less (small), no treatment necessary
Table 3.
AP Laxity difference (injured - contralateral uninjured), Tegner Activity Score, hop distance (% contralateral), and peak extension torque (% contralateral) data for the two initial graft tension groups and the control groups over time. All data are presented as the mean ± 95% CI.
| Test | Time | Low-tension | High-tension | Control |
|---|---|---|---|---|
| AP laxity | Pre-op | 4.5±0.76 | 4.2±0.62 | 0.0±0.34 |
| Intra- | 0.0±0.18 | −2.2±0.24 | - | |
| 6-months | 1.7±0.94 | 0.8±0.83 | - | |
| 12-months | 2.3±0.94 | 2.1±0.80 | −0.1±0.31 | |
| 36-months | 1.7±0.31 | 2.3±0.73 | 0.3±0.65 | |
| Tegner | Pre-op | 7.6±0.57 | 7.6±0.56 | 6.5±0.51 |
| 12-months | 6.1±0.61 | 6.7±0.61 | 6.4±0.57 | |
| 36-months | 5.5±0.62 | 5.9±0.64 | 5.7±0.61 | |
| Hopdistance | Pre-op | 77.7±3.67 | 77.0±3.82 | 99.8±3.18 |
| 12-months | 92.1±4.96 | 91.4±4.04 | 100.8±3.51 | |
| 36-months | 94.6±4.20 | 95.6±4.27 | 100.7±3.98 | |
| Peak Torque | 12-months | 87±5.6 | 83±5.7 | 100±3.3 |
| 36-months | 95±5.1 | 95±5.3 | 105±8.9 |
Clinical Outcomes
Immediately after graft fixation, the mean ± 95% CI of the AP laxity differences for the high-tension and low-tension treatments were −2.0 ± 0.24 mm, and 0.0 ± 0.18 mm, respectively (p<.001; Table 3). The AP laxity values for both initial graft tension groups increased with time and were not significantly different between groups at 6- (p=.111), 12- (p=.806) or 36-months (p=.205). At 36-months, the pooled mean AP laxity value across the initial graft tension groups was 2 mm, and significantly greater than the control group (p<.007). There was no temporal change in AP laxity in the control group (p=.318).
Pre-operatively, the distributions of the IKDC examination scores between the two initial graft tension groups ranged from B (“Nearly normal”) to D (“Severely Abnormal) while the control group ranged from A (“Normal”) to B (“Nearly normal”) (Table 4). There was no significant difference in the distributions of the IKDC scores between the two initial graft tension groups (p=.683), however, they were significantly different from the control group (p<.001). After surgery, the distributions between the two initial graft tension groups equally shifted towards normal, though they remained significantly worse than the control group (p=.009 and p=.047 for the high-tension and low-tension cohorts, respectively).
Table 4.
IKDC examination scores for the three experimental groups.
| IKDC Score | Low-tension | High-tension | Controls |
|---|---|---|---|
| Pre-operative | |||
| A | 0 (0.0%) | 0 (0.0%) | 58 (96.7%) |
| B | 27 (60.0%) | 27 (64.3%) | 2 (3.3%) |
| C | 17 (37.8%) | 13 (30.9%) | 0 (0.0%) |
| D | 1 (2.2%) | 2 (4.8%) | 0 (0.0%) |
| 6-month | |||
| A | 22 (56.4%) | 19 (51.4%) | - |
| B | 15 (38.5%) | 17 (45.9%) | - |
| C | 2 (5.1%) | 1 (2.7%) | - |
| D | 0 (0.0%) | 0 (0.0%) | - |
| 12-months | |||
| A | 19 (52.8%) | 16 (45.7%) | 46 (95.8%) |
| B | 13 (36.1%) | 15 (42.9%) | 2 (4.2%) |
| C | 4 (11.1%) | 4 (11.4%) | 0 (0.0%) |
| D | 0 (0.0%) | 0 (0.0%) | 0 (0%) |
| 36-months | |||
| A | 20 (60.6%) | 17 (53.1%) | 32 (86.5%) |
| B | 10 (30.3%) | 11 (34.4%) | 4 (10.8%) |
| C | 3 (9.1%) | 4 (12.5) | 1 (2.7%) |
| D | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
There were no significant differences in the number of subsequent knee surgical procedures between groups (p=.160). In the ACL reconstructed knees, there were 2 revisions and 1 partial meniscectomy in the low-tension group, and 2 revisions and 2 partial meniscectomies in the high-tension group. In the contralateral knee, there was one primary ACL reconstruction performed in the low-tension group and two performed in the high-tension group. In the control group, 1 subject tore an ACL, which was surgically reconstructed, while another underwent partial meniscectomy after recruitment.
Functional Outcomes
Pre-operatively, the hop distances were not significantly different between the two initial graft tension groups (p=.806) but both were significantly less than the control group (p<.001; Table 3). After 36-months of healing, hop distances between the two initial graft tension groups were not significantly different from each other (p>.751). However, hop distance of the low-tension group was significantly different from the control (p=.038) while there was a trend in the high-tension group (p=.083). There were no temporal changes in hop distances within control subjects (p=.627). The mean peak extension torques in the two graft tension cohorts were not significantly different from each other at 12- and 36-months (p>.358; Table 3). At 36-months, the peak torque for both initial graft tension groups remained significantly less than the control at 36-months (p<.03).
Patient-Oriented Outcomes
For the two initial graft tension groups, there was a significant reduction in the mean Tegner Activity Scores over time (p<.0001; Table 3). There were no significant differences between the two initial graft tension groups at any time point (p>.242). Furthermore, the scores for the two initial graft tension groups were not significantly different from the control group at any post-operative time point (p>.523).
Pre-operatively, all KOOS values for the graft tension groups were significantly different from the control group (p<.001; Table 5). However, there were no differences between mean KOOS between the high- and low-tension groups (p>.470), and all scores improved with time. All KOOS, except that associated with activities of daily living, were significantly less than the control group after 36-months of graft healing. Pre-operatively, seven out of eight SF-36 scores were significantly less than the control group (p<.001; Appendix, Table A). All of the scores improved with time and were not significantly different from the control by 36-months.
Table 5.
Mean ± 95% CI for the five KOOS subscales; quality of life, sports, activities of daily living, symptoms & pain. There were no significant differences between the two initial graft tension groups at any time point. However, there were significant differences between the two initial graft tension groups and the control group at most time points
| Subscale | Time | Low-tension | High-tension | Control |
|---|---|---|---|---|
| Quality of Life (Tension treatment effect: p=.41; Tension time effect: p<.0001) | ||||
| Pre-surgery | 36.0±5.00# | 37.8±5.10# | 97.6±4.33 | |
| 6-months | 61.8±5.33 | 57.6±5.41 | - | |
| 12-months | 74.1±5.35# | 67.8±5.14# | 94.9±4.74 | |
| 36-months | 78.9±5.33# | 76.9±5.53# | 93.3±5.17 | |
| Sports& Recreation (Tension treatment effect: p=.95; Tension time effect: p<.0001) | ||||
| Pre-surgery | 55.9±4.98# | 57.3±5.02# | 98.3±4.19 | |
| 6-months | 75.2±5.21 | 74.1±5.27 | - | |
| 12-months | 79.6±5.15# | 80.5±5.06# | 95.5±4.65 | |
| 36-months | 83.6±5.19* | 83.1±5.39# | 93.1±5.06 | |
| Activities of Daily Living (Tension treatment effect: p=.51; Tension time effect: p<.0001) | ||||
| Pre-surgery | 85.8±2.76# | 84.4±2.80# | 98.9±2.82 | |
| 6-months | 94.3±2.94 | 90.4±3.04 | - | |
| 12-months | 94.5±2.90* | 95.0±3.04# | 97.9±3.08 | |
| 36-months | 94.6±2.92ns | 95.0±3.04ns | 96.2±3.35 | |
| Symptoms (Tension treatment effect: p=.26; Tension time effect: p<.0001) | ||||
| Pre-surgery | 70.4±3.74# | 70.9±3.82# | 96.8±3.25 | |
| 6-months | 80.7±3.98 | 77.8±4.04 | - | |
| 12-months | 85.1±3.94# | 79.6±3.88# | 95.9±3.53 | |
| 36-months | 86.2±3.96# | 82.3±4.11# | 93.7±3.82 | |
| Pain (Tension treatment effect: p=.97; Tension time effect: p<.0001) | ||||
| Pre-surgery | 75.2±3.23# | 76.8±3.31# | 98.9±2.81 | |
| 6-months | 86.5±3.45 | 86.0±3.49 | - | |
| 12-months | 90.2±3.41# | 88.3±3.37# | 97.9±3.08 | |
| 36-months | 90.5±3.45* | 91.1±3.57* | 96.2±3.35 | |
p<.01,
p<.05,
= not significant
Imaging Outcomes
The mean medial joint space widths of the injured knee were not affected by group (p=.273) or time (p=.946) within 36-months (Appendix; Fig. A). All changes were within the resolution of the method for measuring joint space width.19 The mean modified OARSI radiographic scores at 36-month follow-up were less than 2 (Appendix; Fig. B). The mean differences in the OARSI scores of the injured (index) knee minus the contralateral (uninjured) between groups were not significant but there was a strong trend (p=.072). The mean scores in the two initial tension groups significantly increased over time (p<.001) but not in the control group (p=.681).
The mean WORMS for the injured knee were greater than those of the control group both pre-operatively and after 36-months (Appendix; Fig. C). Although the mean differences (injured–contralateral knee) were not significantly different between the two initial graft tension groups (p=.229) pre-operatively, they were significantly greater than the control knee (p<.011). After 36-months, the mean difference in WORMS tended to be greater than the control group (p=.056).
DISCUSSION
The results of this study do not support the hypothesis that the high-tension group would have less AP laxity, improved functional and patient-oriented outcomes, and less cartilage damage than the low-tension group after 36-months of healing. The results also disprove the second hypothesis that the outcomes for the high-tension group would be equivalent to a gender-, race-, and age-matched control group since significant differences for many of the outcome measures (AP laxity, IKDC scores, hop for distance, isokinetic extension torque, four of five KOOS, and the pre-operative WORMS) were found between the initial graft tension groups and the matched control group at 36-months.
It has been shown that the graft tension immediately after fixation is dependent on the knee angle and magnitude of tension applied immediately prior to fixation.9 AP laxity values are significantly less when the graft is tensioned at 30° in comparison to full extension (0°).11 Thus, a graft tension protocol based on AP laxity at the time of graft fixation was possible and selected for this trial. The two laxity-based protocols under investigation bracketed the AP translation values a clinician would reasonably accept at the time of surgery (−2 mm to 0 mm). The mean ± 95% CI difference between legs in AP laxity for the high-tension and low-tension treatments at the time of graft fixation were −2.0 ± 0.24 mm, and 0.0 ± 0.18 mm, respectively, demonstrating that we were able to achieve the desired AP translation values for each group. Furthermore, these data suggest that the application of firm tension to the graft with the knee at 30° or 0° of flexion initially produces a joint that is either over-constrained by 2 mm or equal to that of the contralateral uninjured knee, respectively, though the long-term implications seem moot considering the study results. Thus, the need to directly perform instrumented intra-operative laxity measurement using the KT-1000S may not be required in the surgical setting if the knee flexion angle at the time of graft tensioning is controlled.
Cadaver experiments have been performed to better understand the relationship between graft tension, tibiofemoral compressive force, and AP laxity.6,11 An increase in initial graft tension increases the tibiofemoral compressive force and initially shifts the tibiofemoral contact point posteriorly.6 In the current study, the two laxity-based protocols initially produced significantly different AP laxity values and hence tibiofemoral compressive forces at the time of graft fixation. Although these AP laxity differences were not maintained over time, further study of long-term cartilage health is warranted since the higher tibiofemoral compressive forces immediately following graft fixation could alter cartilage metabolism in the initial healing phase when the cartilage is at highest risk for damage.3
A unique aspect of this study was the evaluation of cartilage integrity between the two initial graft tension groups as compared to the matched control group. Although some minor radiographic and MRI changes were observed in the ACL reconstructed knees, they were relatively small and likely clinically irrelevant within this time frame. No significant differences between the three groups were found in joint space width measurements at 36-months (Appendix; Fig. A). The mean modified OARSI radiographic scores were less than 2. Despite the small magnitude of these scores, the difference relative to the contralateral leg were significantly increasing with time within the two initial graft tension groups as compared to the control group (p<.0001)(Appendix; Fig. B). The pre-operative WORMS were significantly greater in the ACL reconstructed knees relative to the control knees. The higher WORMS were due to the sub-scores related to bone marrow edema, meniscus, and ACL integrity; factors commonly associated with the initial ACL injury. At 36-months, there was still a strong trend (p=.056) indicating that the WORMS remained elevated in the ACL reconstructed knees compared to the control knees (Appendix; Fig. C). How these imaging outcomes progress in the long-term will be the subject of future work.
Several randomized controlled trials of initial graft tension have been reported.4 Yasuda et al 31 evaluated the effects of 20, 40, and 80N on double stranded hamstring grafts connected in series with polyester tape. The high-tension group had significantly less AP laxity than the low-tension group after 2 years. Kim et al compared three initial graft tension levels (78, 117, 147N) on hamstring tendon autografts, and reported no significant differences in outcomes, including AP laxity, 1 to 2.8 years after surgery.14 Clinical trials have compared initial graft tensions of 20 versus 40 N,27 25 versus 50 N,33 and 45 versus 90 N of patellar tendon autografts.17 No significant differences in AP laxity were seen between tension groups after two years of healing in two studies, though the initial graft tension difference may be suspect because neither of the tensions produced a difference in AP laxity at the time of surgery.27,33 Nicholas et al reported a side-to-side difference in AP laxity of 3.0±2.2 versus 2.2±1.6 mm for the initial graft tension levels of 45 N and 90 N, respectively.17 Similar to our study, both tension conditions resulted in higher AP laxity values than the contralateral leg after 20 months of healing. However, it should be noted that the side-to-side difference for the low-tension (45N) condition was 2.4±2.4 mm one week after surgery suggesting that the low-tension level may not have been enough to restore normal AP laxity even immediately following graft fixation. In an evidence based review, it was suggested that these force-based tension studies were underpowered (average sample size of 21 patients per group).4 Our study is the first to evaluate a laxity-based approach for setting initial graft tension with appropriate power. The resultant intra-operative laxity values were measured for both initial graft tension groups and spanned those that would be acceptable at the time of graft fixation. Despite the initial differences in AP laxity, no differences in clinical, functional, patient-oriented, and imaging outcome measures were found between the two laxity-based graft tension protocols at the 36-month follow-up.
The randomized control study design was selected to minimize bias and the effects of confounding factors. The inclusion/exclusion criteria removed patients that would be at high risk for arthritis due to factors not related to their ACL injury, and to remove those with severe meniscal or chondral lesions that would increase their risk of OA.10,18 All patients with meniscal tears involving more than 1/3 of the meniscus and/or Grade II chondral lesions (as determined pre-operatively by MRI or arthroscopic examination) were excluded. Patients with minor meniscal and chondral damage were only included in an effort to expand our recruitment base because the incidence of concomitant minor meniscal/chondral damage is high.32
Patients were included if they were candidates for reconstruction with bone-patellar tendon-bone or 4-stranded hamstring tendon autografts. Both autografts were included to extend the recruitment base and to generalize our results. The assumption that both graft types would respond similarly was justified because biomechanical studies have shown that the graft structural properties, in situ graft forces, and dynamic joint kinematics are nearly equivalent,25,29,30 and because many randomized clinical trials have shown that the clinical, functional, patient-oriented and imaging outcomes are also equal.12,15,16 In our study, the patellar tendon autografts produced AP laxity values of −2.1 ± 0.55 mm and 0.1 ± 0.83 mm for the high- and low-tension groups, respectively, at the time of surgery. The 4-stranded hamstring tendon autograft AP laxity values were −2.2 ± 0.71 and 0.1 ± 0.87 mm, respectively.
In an effort to reduce variability, graft position, fixation, and the post-operative rehabilitation protocol were standardized across patients. All surgeons utilized the same drill guide system and anatomical landmarks to position the graft. Tibial aperture fixation was used to secure the patellar and hamstring tendon grafts. Finally, the rehabilitation program was standardized across subjects. Deviations from the prescribed program was not of great concern since recent data has shown that rehabilitation with either an “accelerated” or “non-accelerated” program would result in equivalent clinical, functional and patient-oriented outcomes.5
Eligible patients were stratified into the two initial graft tension groups to ensure balance in age, race, and gender. It was our intent to create a matched control group. However, the mean control group age was approximately one and a half years older than the initial graft tension groups. This difference was a result of our recruitment criteria since we were unable to include controls under the age of 18 due to IRB concerns related to radiographic exposure of healthy children. We also intended to match the activity level of the control group to that of the initial graft tension group. Unfortunately, the mean Tegner score was 1.1 point lower than that of the treatment groups. This is another limitation.
The study design included a separate control group whereas most studies of outcome following ACL reconstruction utilize the contralateral knee as the control. It is possible that the contralateral knee is also affected by changes in joint kinematics of the injured knee (e.g., patients may protect their knee), which is an important consideration particularly for studies addressing cartilage damage. The control group enabled us to gauge how the treated patients fared relative to a matched uninjured population. From this study, we learned that many of the outcome measures do not return to normal. For example, all of the mean KOOS for the control subjects were diminishing with time. These data suggest that other factors (e.g., aging, weight) may affect these patient-oriented outcome scores in long term studies. Also of note, two subjects in the control group injured their knees and required surgery during the 36-month study period, another consideration when interpreting failure data (based on subsequent surgeries) in cohort studies of ACL reconstruction. A matched control group is therefore an important addition to any outcome study following treatment of ACL injuries.
In conclusion, the results of this randomized controlled trial found that the two laxity-based initial graft tension protocols produce similar clinical, functional, patient-oriented and OA imaging outcomes at 36-months post-surgery. Even after 36-months of healing, many of the outcomes from the two initial graft tension cohorts were not completely restored.
Supplementary Material
Acknowledgments
This study was funded by grants from the National Institutes of Health (RO1-AR047910; RO1-AR047910S1). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. This trial is registered with ClinicalTrials.gov (NCT00434837). The authors thank Dr. Kurt Spindler (Vanderbilt University) for serving as the Data Safety Officer for the study. The MR images were acquired at the MRI Research Facility (Brown University, Providence RI) and the Osteoarthritis Initiative MRI Facility (Southeastern Medical Center, Memorial Hospital, Pawtucket RI). The authors gratefully acknowledge the assistance of Daniel Acuri (MRI technician, Rhode Island Hospital), Lynn Fanella (MRI technician, Brown University), David Dimascio (MRI technician, Memorial Hospital), Arlene Garcia (Clinical Coordinator, Rhode Island Hospital) and Alison Biercevicz (Graduate student, Brown University).
References
- 1.Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15:A1–A56. doi: 10.1016/j.joca.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 2.Amis AA, Jakob RP. Anterior cruciate ligament graft positioning, tensioning, and twisting. Knee Surg Sports Traumatol Arthrosc. 1998;6:S2–S12. doi: 10.1007/s001670050215. [DOI] [PubMed] [Google Scholar]
- 3.Anderson DD, Chubinskaya S, Guilak F, et al. Post-traumatic osteoarthritis: Improved understanding and opportunities for early intervention. J Orthop Res. 2011;29:802–809. doi: 10.1002/jor.21359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arneja S, McConkey MO, Mulpuri K, et al. Graft tensioning in anterior cruciate ligament reconstruction: a systematic review of randomized controlled trials. Arthroscopy. 2009;25:200–207. doi: 10.1016/j.arthro.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Beynnon BD, Uh BS, Fleming BC, et al. Rehabilitation following anterior cruciate ligament reconstruction; A prospective, randomized, double-blind comparison of accelerated versus non-accelerated rehabilitation. Am J Sports Med. 2005;33:347–359. doi: 10.1177/0363546504268406. [DOI] [PubMed] [Google Scholar]
- 6.Brady MF, Fleming BC, Bradley MP, Banerjee R, Fadale PD, Hulstyn MJ. Effects of initial graft tension on the tibiofemoral compressive forces and joint position following ACL reconstruction. Am J Sports Med. 2007;35:395–403. doi: 10.1177/0363546506294363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buckland-Wright JC, Wolfe F, Ward RJ. Substantial superiority of semiflexed (MTP) views in knee osteoarthritis: a comparative radiographic study, without fluoroscopy, of standing extended, semiflexed (MTP), and schuss views. J Rheumatol. 1999;26:2664–2674. [PubMed] [Google Scholar]
- 8.Burks RT, Leland R. Determination of graft tension before fixation in anterior cruciate ligament reconstruction. Arthroscopy. 1988;4:260–266. doi: 10.1016/s0749-8063(88)80041-0. [DOI] [PubMed] [Google Scholar]
- 9.Bylski-Austrow DI, Grood ES, Hefzy MS, Holden JP, Butler DL. Anterior cruciate ligament replacements: A mechanical study of femoral attachment location, flexion angle at tensioning, and initial tension. J Orthop Res. 1990;8:522–531. doi: 10.1002/jor.1100080408. [DOI] [PubMed] [Google Scholar]
- 10.Englund M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: Influence of type of meniscal tear and size of resection. Rheumatol. 2001;40:631–639. doi: 10.1093/rheumatology/40.6.631. [DOI] [PubMed] [Google Scholar]
- 11.Fleming BC, Brady MF, Bradley MP, Banerjee R, Hulstyn MJ, Fadale PD. Tibiofemoral compression force differences using laxity- and force-based initial graft tensioning techniques in the anterior cruciate ligament-reconstructed cadaveric knee. Arthroscopy. 2008;24:1052–1060. doi: 10.1016/j.arthro.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38:448–454. doi: 10.1177/0363546509350301. [DOI] [PubMed] [Google Scholar]
- 13.Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee Guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107–114. doi: 10.1007/s001670050082. [DOI] [PubMed] [Google Scholar]
- 14.Kim SG, Kurosawa H, Sakuraba K, Ikeda H, Takazawa S. The effect of initial graft tension on postoperative clinical outcome in anterior cruciate ligament reconstruction with semitendinosus tendon. Arch Orthop Trauma Surg. 2006;126:260–264. doi: 10.1007/s00402-005-0045-x. [DOI] [PubMed] [Google Scholar]
- 15.Magnussen RA, Carey JL, Spindler KP. Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2011;19:462–472. doi: 10.1007/s00167-010-1277-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011:CD005960. doi: 10.1002/14651858.CD005960.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nicholas SJ, D’Amato MJ, Mullaney MJ, Tyler TF, Kolstad K, McHugh MP. A prospectively randomized double-blind study on the effect of initial graft tension on knee stability after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:1881–1886. doi: 10.1177/0363546504265924. [DOI] [PubMed] [Google Scholar]
- 18.Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: A prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38:2201–2210. doi: 10.1177/0363546510373876. [DOI] [PubMed] [Google Scholar]
- 19.Oksendahl HL, Gomez N, Thomas CS, et al. Digital radiographic assessment of tibiofemoral joint space width: a variance component analysis. J Knee Surg. 2009;22:205–212. doi: 10.1055/s-0030-1247750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel RR, Hurwitz DE, Bush-Joseph CA, Bach BR, Andriacchi TP. Comparison of clinical and dynamic knee function in patients with anterior cruciate ligament deficiency. Am J Sports Med. 2003;31:68–74. doi: 10.1177/03635465030310012301. [DOI] [PubMed] [Google Scholar]
- 21.Peterfy CG, Guermazi A, Zaim S, et al. Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12:177–190. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 22.Reinke EK, Spindler KP, Lorring D, et al. Hop tests correlate with IKDC and KOOS at minimum of 2 years after primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1806–1816. doi: 10.1007/s00167-011-1473-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 24.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152:726–732. doi: 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 25.Tashman S, Kolowich P, Collon D, Anderson K, Anderst W. Dynamic function of the ACL-reconstructed knee during running. Clin Orthop. 2007;454:66–73. doi: 10.1097/BLO.0b013e31802bab3e. [DOI] [PubMed] [Google Scholar]
- 26.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop. 1985;198:43–49. [PubMed] [Google Scholar]
- 27.van Kampen A, Wymenga AB, van der Heide HJL. The effect of different graft tensioning in anterior cruciate ligament reconstruction: A prospective randomized study. Arthroscopy. 1998;14:845–850. doi: 10.1016/s0749-8063(98)70022-2. [DOI] [PubMed] [Google Scholar]
- 28.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 29.Wilson TW, Zafuta MP, Zobitz M. A biomechanical analysis of matched bone-patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am J Sports Med. 1999;27:202–207. doi: 10.1177/03635465990270021501. [DOI] [PubMed] [Google Scholar]
- 30.Woo SL-Y, Kanamori A, Zeminski J, Yagi M, Papageorgiou CD, Fu FH. The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon - A cadaveric study comparing anterior tibial and rotational loads. J Bone Joint Surg Am. 2002;84:907–914. doi: 10.2106/00004623-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Yasuda K, Tsujino J, Tanabe Y, Kaneda K. Effects of initial graft tension on clinical outcome after anterior cruciate ligament reconstruction - Autogenous doubled hamstring tendons connected in series with polyester tapes. Am J Sports Med. 1997;25:99–106. doi: 10.1177/036354659702500120. [DOI] [PubMed] [Google Scholar]
- 32.Yoon KH, Yoo JH, Kim KI. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am. 2011;93:1510–1518. doi: 10.2106/JBJS.J.01320. [DOI] [PubMed] [Google Scholar]
- 33.Yoshiya S, Kurosaka M, Ouchi K, Kuroda R, Mizuno K. Graft tension and knee stability after anterior cruciate ligament reconstruction. Clin Orthop. 2002;394:154–160. doi: 10.1097/00003086-200201000-00018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.