Abstract
Youth with elevated conduct disorder (CD) symptoms who also have callous-unemotional (CU) traits exhibit more antisocial behavior than youth without CU traits. However, evidence regarding whether CU traits increase risk of substance use over and above CD symptoms, and whether these associations differ for boys and girls, is scarce. Using the Developmental Pathways Project sample of 521 middle school students, we examined whether adolescent- and parent-reported CU traits measured in 6th grade prospectively predicted the onset and recurrence of substance use and use-related impairment by 9th grade. We also examined the degree to which CU traits uniquely predicted substance use and impairment over and above CD symptoms, as well as whether gender moderated these associations. Results indicated that adolescent-reported CU traits increased the likelihood of substance use and impairment onset and recurrence by 9th grade. Analyses revealed that CD symptoms accounted for prospective associations between adolescent-reported CU and substance use, but gender moderated these associations. Boys with elevated CU traits and CD symptoms were not more likely to report alcohol use onset or recurrence, but they were at highest risk of recurrent marijuana use, use of both alcohol and marijuana, and use-related impairment by 9th grade. Girls with low CU traits and high CD symptoms were most likely to report onset and recurrent use of alcohol, as well as recurrent marijuana use, use of both substances and impairment. Study findings highlight the importance of accounting for CD symptoms and gender when examining links between CU traits and substance use in early adolescence.
Keywords: Callous-unemotional traits, conduct disorder, substance use, early adolescence
Callous-unemotional (CU) traits, including lack of empathy or guilt for wrong doing, appear to identify a subset of children with conduct disorder (CD) who are most likely to exhibit severe and persistent antisocial behavior (Frick & Moffitt, 2010). Children with elevated CU traits exhibit high levels of psychopathy and delinquency as adolescents (Frick, Stickle, Dandreaux, Farrell, & Kimonis, 2005; Lynam et al., 2009; Obradovic, Pardini, Long, & Loeber, 2007) and as adults (Gretton, Hare, & Catchpole, 2004; Lynam, Caspi, Moffitt, Loeber, & Stouthamer-Loeber, 2007; McMahon, Witkiewitz, Kotler, & the Conduct Problems Prevention Research Group, 2010). At the same time, surprisingly little is known regarding associations between CU traits and correlates of delinquency, including behaviors that may contribute to the development of antisociality. Substance use, particularly early in adolescence, is considered to be part of the broader “externalizing behaviors spectrum” (Krueger et al., 2002) and may be one factor that escalates antisocial behavior among youth with elevated CU traits.
In the context of problem behavior theory (Jessor, 1987), children with elevated CU traits appear at risk of early substance use owing to how they respond to environmental influences. Youth with elevated CU traits seem insensitive to punishment, tending to behave inappropriately regardless of the negative consequences they may experience (for review, see Frick & White, 2008). This is concerning in light of data suggesting that responsiveness to environmental deterrents and social norms is associated with lower levels of adolescent substance use (Johnson & Gerstein, 2000; Keyes et al., 2011). Additionally, relative to those with lower CU traits, children with elevated CU traits are also more likely to respond favorably to rewarding stimuli (Frick, Cornell, Bodin et al., 2003) and to value positive qualities of deviant behavior (e.g., social dominance gained via aggression; Pardini, Lochman & Frick, 2003). These tendencies may increase their risk of substance use in adolescence since research underscores associations between positive expectancies and substance use initiation and problems (Cable & Sacker, 2007; Skenderian, Siegel, Crano, Alvaro, & Lac, 2008). Taken together, adolescents who are relatively unresponsive to negative consequences and view the outcomes of deviant behavior favorably, such as those with elevated CU traits, may engage in early and problematic substance use.
A number of studies have examined associations between psychopathy and substance use in adolescence. Adolescents from inpatient or incarceration settings with elevated psychopathic traits have been shown to be more likely to use drugs at earlier ages, to abuse alcohol and drugs, and to be diagnosed with substance use disorders than those without psychopathy (Harvey, Stokes, Lord, & Pogge, 1996; Mailloux, Forth, & Kroner, 1997; Murrie & Cornell, 2000; Roussy & Toupin, 2000). Though these investigations underscore psychopathy as a risk factor for substance use in adolescence, the degree to which CU traits specifically increased risk of substance use is unclear. This is because the construct of psychopathy tested in these studies was comprised of items assessing impulsivity and antisocial behavior in addition to CU traits. To our knowledge, only one study has examined CU traits as a unique risk factor for substance use. Hillege, Das, and de Ruiter (2010) found that non-referred adolescents with elevated CU traits used alcohol and drugs more frequently than those without CU traits. However, relations between CU traits and substance use onset or problems were untested. These outcomes are important to assess, especially in early adolescence, given that initiation of substance use prior to high school is non-normative and predicts heavier use throughout adolescence, more serious long-term substance use problems, and adult substance dependence (King & Chassin, 2007; Sung, Erkanli, Angold, & Costello, 2004). Moreover, all prior studies of the association between psychopathy/CU traits and substance use have been cross-sectional, which makes it impossible to ascertain the degree to which CU traits contribute to the subsequent development of substance use. Thus, one goal of the present study was to examine CU traits as a unique prospective risk factor for the onset and recurrence of substance use and impairment in adolescence.
Additional methodological limitations of existing studies raise important questions about the purported link between CU and substance use. As noted above, CU traits are associated with more severe and persistent conduct problems and antisociality. CD symptoms, and externalizing symptoms more broadly, are perhaps the most robust predictors of substance use among adolescents (Armstrong & Costello, 2002; Chassin, Ritter, Trim & King, 2003). Yet, no prior studies have controlled for CD symptoms when testing associations between CU and substance use. It may be that CU traits increase risk of substance use regardless of CD symptoms. Indeed, there is some evidence to suggest that elevated CU traits-only (without elevated conduct problems) increases risk of delinquency (Frick et al., 2005). Alternatively, it may be that CU predicts later substance use only because CU traits are a marker for youth with elevated CD symptoms who are most likely to engage in substance use. As such, this study investigated whether CU traits contribute unique risk for substance use over and above CD symptoms, and whether adolescents with elevated CU and CD are at greater risk of substance use and use-related problems in early adolescence relative to youth with elevated CD-alone.
Furthermore, little is known about whether the association between CU traits and substance use varies between adolescent boys and girls. Though three of the five studies investigating associations between psychopathic traits and substance use included girls in their samples, only one of these examined whether relations differed between boys and girls, and even that study did not test for gender moderation explicitly. Hillege and colleagues (2010) found that CU traits were positively correlated with drug use frequency among non-referred boys and girls, but found that CU traits were positively correlated with alcohol use frequency for boys only. The dearth of examinations on whether gender moderates links between CU traits and substance use is surprising in light of evidence suggesting that associations between CU traits and a variety of outcomes may vary by gender. For example, studies have found stronger associations between CU traits and relevant biomarkers (e.g., cortisol reactivity; Loney, Butler, Lima, Counts, & Eckel, 2006), deficits in affective empathy (Dadds et al., 2009), and genetic influences (Fontaine, Rijsdijk, McCrory, & Viding, 2010; Viding, Frick, & Plomin, 2007) in boys than girls. Conversely, research has also indicated that boys and girls both evince links between CU traits and antisociality (Dadds, Fraser, Frost, & Hawes, 2005; Frick, Cornell, Barry, Bodin, & Dane, 2003; Viding, Simmonds, Petrides, & Frederickson, 2009), while other work has shown significant relations between CU traits and aggression in girls but not boys (e.g., relational aggression; Marsee, Silverthorn, & Frick, 2005). Only two studies have examined whether CU traits and CD symptoms interact to predict different behavioral outcomes in boys and girls. Frick, Cornell, Barry and colleagues (2003) found that boys with elevated CU traits and CD symptoms were most likely to self-report delinquency, while girls with elevated CU traits and low CD symptoms were most likely to report delinquent behavior. Dadds and colleagues (2005) reported that boys exhibiting elevated CU traits and conduct problems subsequently demonstrated the most severe externalizing symptoms, while neither CU traits nor conduct problems prospectively predicted externalizing symptoms in girls. To extend the limited research on CU traits in girls, especially with regards to predicting substance use outcomes, we tested gender as a moderator of the interaction between CU and CD in the prediction of substance use onset and recurrence.
The current study sought to investigate several unanswered questions related to links between CU traits and substance use in early adolescence. We hypothesized that adolescents with elevated CU traits in 6th grade would be more likely than those with lower levels of CU traits to report onset and recurrent use of alcohol and/or marijuana, as well as impairment due to use, by 9th grade. Next, because CU traits have been shown to moderate links between CD symptoms and delinquency (Frick & Moffitt, 2010), we hypothesized that youth with elevated CU traits and CD symptoms would be more likely than those with elevated CD-only to report onset and recurrence of substance use and use-related impairment. Finally, because CU traits are more common among non-referred boys than among non-referred girls (Frick, Bodin & Barry, 2000; Frick et al., 2005), and because boys with elevated CU traits and CD symptoms appear to be at risk for worse outcomes than girls (Dadds et al., 2005; Frick, Cornell, Barry et al., 2003), we hypothesized that CU traits would be more likely to interact with CD symptoms in the prediction of substance use outcomes among boys than girls.
Method
Sample
The sample for this study was drawn from the Developmental Pathways Project (DPP; Vander Stoep et al., 2005), which is a community-based prospective cohort study designed to examine the antecedents and outcomes of depression and conduct problems in early adolescence. DPP participants were recruited from four Seattle-area public schools located in distinct areas within the city, and together have a racial/ethnic distribution that is nearly identical to the total enrolled student population of the school district. Universal emotional health screening was carried out with sixth grade students at these schools in four consecutive years (2001–2004); details of the screening procedure have been described elsewhere (Vander Stoep et al., 2005).
Students eligible for screening included 6th graders who had a 3rd grade reading comprehension level or higher. Of the 2920 eligible students, 2187 (74.9%) were screened. Each year following screening, a random sample of students, stratified by their scores on the Mood and Feelings Questionnaire (MFQ) for depression (Costello & Angold, 1988) and Youth Self Report (YSR) externalizing scale for conduct problems (Achenbach & Rescorla, 2001), were identified for participation in the longitudinal study. Students were first assigned to one of four groups based on their screening results: high depression and conduct problem score (comorbid; CM), high depression and low conduct problem score (DP), low depression and high conduct problem score (CD), and low depression and low conduct problem score (NE). These groups were formed using a cutoff of 0.5 SD above the screening sample mean on the MFQ and YSR.
Students who had been screened, who had at least one parent who could speak English, and who were still residing in the district were eligible for recruitment into the longitudinal study. A stratified random sample of 807 students was selected for longitudinal follow-up with students scoring high on depressive and/or conduct problem scores over-sampled according to a ratio of 1:1:1:2 from the four psychopathology screening groups (CM, DP, CD, NE). Since in the general school population, the ratio is approximately 1 CM: 1 DP: 1 CD: 6 NE, this sample selection approach yielded an over-representation of children in the CM, DP, and CD groups relative to their distribution in the general population. Of those selected, 521 (64.6%) students and their parents/guardians consented to participate in the DPP. At baseline, participants were 12.0 years-old on average (range 11–13.6), 51.6% male and included 1.4 % Native Americans, 24.9% Black, 24.1 % Asian/Pacific Islanders, and 10.1% Hispanics; the remaining 39.5% were Caucasian. Nearly half (48.1%) were raised in households with a total income under $50,000.
In-home interviews were conducted with participating students and parents/guardians (76% biological mothers, 15% biological fathers, 9% other relatives) by two trained research interviewers. Interviewers were blind to the psychopathology risk group status of the students. Baseline interviews were conducted within 3 months of screening (Fall 6th Grade), and in-person follow-up interviews were conducted 6, 12, 18, 24 and 36 months afterward (Fall 9th grade). Of the participants originally enrolled in DPP, between 86% and 90% were retained in each of the first four follow-up interviews, including over 80% in each psychopathology risk category.
Measures
CU traits
Adolescent CU traits were measured at baseline (6th grade) using self- and parent-report versions of the Antisocial Process Screening Device (APSD; Frick & Hare, 2001). The APSD has well-established inter-rater and test-retest reliability as well as discriminant and predictive validity (Frick & Hare, 2001). For the purpose of this study, only the 6 APSD-CU items were used. Each item was rated on a Likert-Scale ranging from 0 (not at all true), to 1 (sometimes true), to 2 (definitely true), and relevant items were reverse-coded such that higher scores indicated more CU traits. We submitted the CU items to a confirmatory factor analyses (CFA) to test the factor structure of the 6-item scale. Although self-report data fit the model [χ2 (9) = 21.72, p <.01, RMSEA=.05, CFI=.95], factor loadings for the last two items (“Does not show feelings or emotions” and “Keeps the same friends”) were not significant, suggesting that they were unrelated to the latent factor representing the common variance across CU items. Indeed, item-total correlations indicated that neither item was strongly correlated with the remaining CU items (rs = .05, .10, respectively). Prior studies have reported similar difficulties with the last two items (for review, see Poythress et al., 2006). Another CFA was conducted with a 4-item CU scale with self-report data, excluding the two underperforming items. Model fit was significantly better than the 6-item version [Δ χ2 (7) = 16.67, p <.05] and the internal consistency of the 4-item CU scale (α = .56) was better than the 6-item scale (α = .46). Though the alpha remained low, it is consistent with those reported in previous research with the 4-item self-report CU scale (α = .50 – .73; Poythress et al., 2006). CFAs also indicated that the 4-item CU scale fit the parent data well [χ2 (2) = 3.57, p =.16, RMSEA=.04, CFI=1.00], though not significantly better than the 6-item scale [Δ χ2 (7) = 10.45, p =.18]. Still, internal consistency was stronger for the 4-item scale than the 6-item scale (α = .66 vs. .63). For this reason, and to allow for study findings to be compared across self and parent reports, the 4-item CU scale was used for parent-report data. Items included in the 4-item scale were: “Concerned about how well he/she does at school/work,” “Good at keeping promises,” “Feels bad or guilty when he/she does something wrong,” and “Concerned about the feelings of others.”
CD symptoms
CD symptom counts were measured using the Diagnostic Interview Schedule for Children (DISC; Schaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) administered at baseline (6th grade). The DISC is designed to make psychiatric diagnoses by applying DSM IV criteria, and has well-established psychometrics, including good test-retest agreement (κ = .66) and concurrent validity (κ = .70) for parent- and youth-reported CD (Schwab-Stone, Shaffer, Dulcan, Jensen, & Fisher, 1996). Adolescents and parents in the study independently completed the DISC. Symptoms endorsed as occurring within the past year were summed to form adolescent- and parent-reported CD symptom counts, ranging from 0 to 26.
Substance use
The Customary Drinking and Drug Use Record (CDDR; Brown et al., 1998) was administered at each visit up to 9th grade to assess self-reported age of onset and frequency of alcohol and marijuana use during the prior six months. Participants were ensured their responses would be kept strictly confidential. The CDDR was originally validated in a community sample of adolescents, demonstrating high test-retest reliability over 1 week (rs = .83 and .93 for alcohol and drugs, respectively), strong convergent validity (rs = .68 and .74) and high inter-rater reliability (rs = .99 and 1.00; Brown et al., 1998). Additional studies have underscored the reliability and validity of adolescent self-reported lifetime use of alcohol and marijuana (Bailey, Flewelling, & Rachal, 1992; Shillington & Clapp, 2000). For the purpose of this study, binary use onset variables were created to indicate whether adolescents reported using alcohol, marijuana or both alcohol and marijuana by 9th grade. The number of assessments (out of 6) adolescents reported using alcohol, marijuana, or both alcohol and marijuana was also computed to identify adolescents reporting recurrent use by 9th grade.
Substance use impairment
The Rutgers Alcohol Problem Inventory (White & Labouvie, 1989) is a 23-item self-administered measure of negative drug and alcohol-related consequences. Again, participants were ensured their responses would be kept strictly confidential. Using a 5-point Likert-type scale ranging from 0 = "never" to 4 = "more than 10 times,” adolescents rated the occurrence of impairment in personal, social and academic functioning over the past 6 months due to alcohol and/or marijuana use. The sum total of these ratings is the index for use-related impairment. The RAPI has well-established test-retest reliability as well as discriminant and construct validity in both general and clinical samples of adolescents (Miller et al., 2002; White & Labouvie, 1989), and has shown good internal consistency and convergent validity when assessing consequences of adolescents using substances other than alcohol (Ginzler, Garrett, Baer, & Peterson, 2007). For study purposes, a binary onset variable was created to indicate if participants reported any use-related impairment by 9th grade. The number of assessments (out of 6) adolescents reported any impairment due to substance use was computed as a measure of recurrent impairment by 9th grade.
Covariates
Participant gender, age, depressive symptoms and family history of substance use were covariates in this study. Data collected at baseline were used for each variable. Gender was included given interest in testing it as a moderator of relations between CU and outcomes. Adolescent-reported depression symptom counts on the DISC (M=6.63, SD=4.70) were controlled in analyses with adolescent-rated CU and CD, while parent-reported DISC depression symptom counts (M=4.16, SD=3.52) were covaried in analyses with parent-rated CU and CD. The Family History Screen (Weissman et al., 2000) was administered to parents who reported on whether 1st and 2nd degree relatives ever had an alcohol or drug problem. A binary variable was computed to indicate whether or not participants had a family history of substance abuse (55% had such a history).
Analytical Plan
We utilized sampling weights based on depression/conduct problem status, gender, race/ethnicity, and educational program in all analyses to ensure the generalizability of study findings to the screened population of Seattle Public School students. We calculated descriptive statistics for adolescent- and parent-reported CU and CD, as well as adolescent-reported substance use variables, and tested intercorrelations among variables in the regression analyses. We utilized hierarchical regression to examine whether CU uniquely predicted onset and recurrence of substance use and impairment over and above CD, and to investigate whether the prediction varied for girls and boys. Covariates and the main effect of CU were entered in Step 1. In Step 2, the main effect of CD and the CU × CD interaction were added. Finally, gender × CU, gender × CD, and gender × CU × CD interactions were included in Step 3 to test for gender moderation. Logistic regression tested for unique predictors of substance use and impairment onset while ordinary least squares regression was used to assess for unique predictors of recurrent use and impairment
Results
Preliminary Analyses
Descriptive statistics for the predictors and outcomes are displayed in Table 1. Across self- and parent-reports, males reported more CU traits and CD symptoms than females. Relative to boys, girls were more likely to report having no CU traits (35.77% vs. 21.80, χ2 [512] = 12.23, p < .01) and less likely to report CU traits and CD symptoms (32.51% vs. 59.00%, χ2 [504] = 35.53, p < .01). Parents of girls were also more likely than parents of boys to report that their child exhibited no CU traits (30.40% vs. 21.76, χ2 [512] = 4.97, p < .05) and less likely to report that their child exhibited CU traits and CD symptoms (36.55% vs. 58.78%, χ2 [511] = 25.28, p < .01). Rates of substance use and impairment onset did not differ between males and females. On the other hand, girls were more likely to report recurrent alcohol use than boys. Girls and boys did not differ in the number of times they reported marijuana use, use of both alcohol and marijuana, or impairment due to use. As shown in Table 2, correlations between CU traits and CD symptoms were higher among boys (rs .38–.47) than girls (rs .12–.15) across informant.
Table 1.
Descriptives for Predictor and Outcome Variables
| Males (n=266) |
Females (n=250) |
||
|---|---|---|---|
| Adolescent Ratings in 6th Grade | M (SD) | M (SD) | p |
| CU | 1.99 (1.70) | 1.28 (1.30) | < .01 |
| CD | 2.92 (3.67) | 1.35 (2.20) | < .01 |
| Parent Ratings in 6th Grade | M (SD) | M (SD) | p |
| CU | 2.09 (1.72) | 1.68 (1.65) | < .01 |
| CD | 2.00 (2.50) | 1.36 (2.05) | < .01 |
| % Endorsing Use by 9th Grade | % | % | p |
| Alcohol Use | 37.55 | 40.87 | 0.44 |
| Marijuana Use | 18.96 | 18.65 | 0.93 |
| Alcohol and Marijuana Use | 17.1 | 15.87 | 0.71 |
| Impairment | 22.3 | 25.4 | 0.41 |
| Number of Visits Reporting Use by 9th Grade | M (SD) | M (SD) | p |
| Alcohol Use | .40 (.77) | .58 (1.02) | < .05 |
| Marijuana Use | .25 (.65) | .24 (.64) | 0.94 |
| Alcohol and Marijuana Use | .16 (.47) | .20 (.60) | 0.44 |
| Impairment | .34 (.73) | .39 (.85) | 0.51 |
Note: CU = Sum of 4-item Callous-Unemotional scale, with item scores ranging from 0-Not at all true to 2-Definitely true (Frick & Hare, 2001); CD = Conduct disorder symptom count from DISC (Shaffer et al., 2000). Use = Any use in last 6 mo; Impairment = Any impairment in last 6 mo; Number of visits = frequency of assessments when any use or impairment was endorsed.
Table 2.
Correlations among Covariates, Predictors and Substance Use Outcomes Included in Regression Analyses
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | - | −.08 | .18** | −.02 | .17** | .22** | .23** | .25** | .03 | .07 | .07 | .12 | .12 | .09 |
| 2. Family History | .01 | - | .01 | .15* | −.02 | .06 | −.25** | .11 | .06 | .20** | .18** | .12 | .14* | .14* |
| 3. Dep-Adol | .09 | .12 | - | .25** | .27** | .37** | .14* | .12 | .25** | .22** | .17** | .26** | .25** | .23** |
| 4. Dep-Par | .04 | .23** | .26** | - | .08 | .14* | .02 | .40** | .15* | .19** | .11 | .16** | .14* | .17** |
| 5. CU-Adol | .10 | −.02 | .22** | .04 | - | .15* | .24** | .04 | .13* | .13* | .08 | .10 | .08 | .11 |
| 6. CD-Adol | .26** | −.02 | .40** | .06 | .47** | - | .18** | .34** | .28** | .28** | .38** | .35** | .37** | .42** |
| 7. CU-Par | .15* | .01 | .11 | .12 | .31** | .43** | - | .12 | .05 | −.01 | .13* | .06 | .03 | .12 |
| 8. CD-Par | .20** | .14* | .15* | .29** | .26** | .43** | .38** | - | .09 | .15* | .07 | .09 | .09 | .09 |
| 9. Alcohol-Ons | .11 | .05 | .03 | .19** | .16** | .17** | .08 | .11 | - | .43** | .63** | .68** | .36** | .51** |
| 10. Marijuana-Ons | .19** | −.01 | .09 | .04 | .15* | .30** | .14* | .19** | .53** | - | .53** | .52** | .80** | .58** |
| 11. Impairment-Ons | .14* | −.05 | .13* | .08 | .20** | .28** | .09 | .10 | .62** | .79** | - | .62** | .52** | .79** |
| 12. Alcohol- | .13* | .01 | .20** | .18** | .26** | .29** | .08 | .09 | .66** | .46** | .62** | - | .63** | .79** |
| 13. Marijuana-Rec | .16** | .00 | .10 | .07 | .29** | .42** | .14* | .25** | .45** | .79** | .69** | .53** | - | .76** |
| 14. Impairment-Rec | .13* | −.07 | .15* | .09 | .31** | .36** | .11 | .15 | .56** | .71** | .88** | .69** | .78** | - |
Notes: Boys below diagonal, girls above diagonal; Family History = Family history of substance use across 1st and 2nd degree relatives (0=no, 1=yes); Dep = DISC depression symptom count from 6th grade; CU = APSD Callous-Unemotional scale administered in 6th grade; CD = DISC Conduct Disorder symptom count from 6th grade; Adol = Adolescent-report; Par = Parent-report; Ons = Onset of substance use or impairment by 9th grade? (0=no, 1=yes); Rec = number of visits (up to 9th grade) when any use or impairment was endorsed.
p < .05,
p < .01
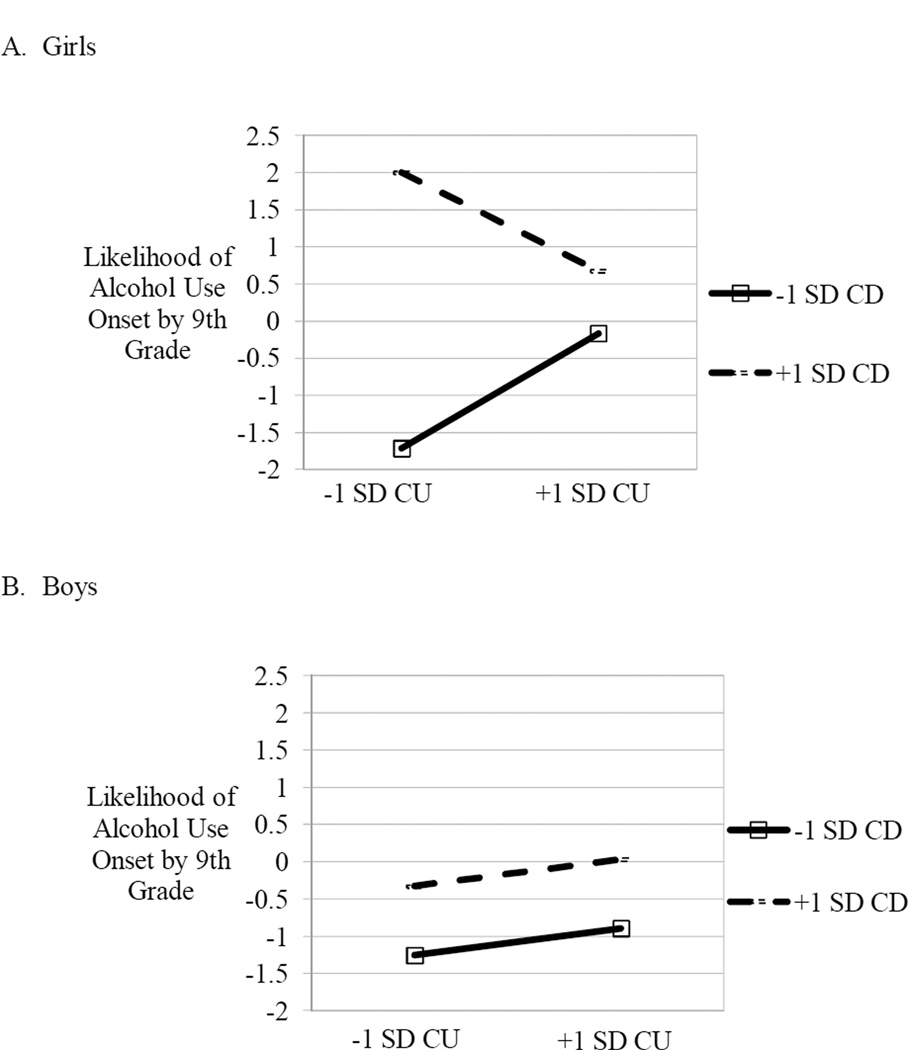
Predicting Onset of Substance Use and Impairment
Step 1 analyses with adolescent ratings indicated that, over and above the covariates, CU predicted the onset of alcohol use (b = .21, SE = .07, p < .01), marijuana use (b = .19, SE = .08, p < .05), use of both alcohol and marijuana (b = .21, SE = .08, p < .05), and use-related impairment (b = .18, SE = .07, p < .05). Adolescents reporting elevated CU traits in 6th grade were more likely than those reporting low CU traits to have used alcohol, marijuana, or both substances and to have been impaired due to use by 9th grade. However, when 6th grade CD symptoms were added to the model in Step 2, CU no longer significantly predicted onset of alcohol use (b = .14, SE = .07, p = .07), marijuana use (b = .04, SE = .09, p = .67), use of alcohol and marijuana (b = .06, SE = .10, p = .55), or use-related impairment (b = .05, SE = .09, p = .57). Conversely, CD symptoms increased the likelihood of alcohol use (b = .23, SE = .05, p < .01), marijuana use (b = .22, SE = .06, p < .01), use of alcohol and marijuana (b = .24, SE = .06, p < .01), and impairment due to use (b = .30, SE = .06, p < .01). As shown in Table 3, gender was found to moderate the effect of the interaction between CU and CD on alcohol use onset in Step 3. Follow-up regression analyses conducted for boys and girls separately found that the CU × CD interaction was a significant predictor of alcohol use onset for girls (b = .14, SE = .07, p < .05), with no interaction found for boys (b = .00, SE = .02, p = .91). As shown in Figure 1, girls reporting low CU and high CD in 6th grade were more likely to have used alcohol by 9th grade than girls reporting high CU and high CD or girls reporting low CD and low/high CU traits. The main effect of CD (b = .16, SE = .07, p < .05), but not CU (b = .12, SE = .10, p = .22), on 9th grade alcohol use was significant in boys. Gender was not found to moderate CU × CD prediction of the onset of marijuana use, use of alcohol and marijuana, or use-related impairment.
Table 3.
Adolescent-Reported Risk Factors for Onset of Substance Use and Impairment by 9th Grade
| Predictors | Alcohol | Marijuana | Alcohol and Marijuana | Impairment |
|---|---|---|---|---|
| Age | .04 (.27) | .44 (.33) | .42 (.34) | .15 (.31) |
| Family History | .12 (.21) | .62 (.27)* | .64 (.28)* | .30 (.25) |
| Dep-Adol | .02 (.02) | .03 (.03) | .01 (.03) | .01 (.03) |
| Gender | −.81 (.24)** | −.66 (.27)* | −.53 (.28) | −.90 (.26)** |
| CU-Adol | .04 (.14) | .14 (.14) | .14 (.15) | −.01 (.14) |
| CD-Adol | .36 (.10)** | .31 (.09)** | .36 (.10)** | .51 (.10)** |
| CU×CD | −.15 (.07)* | −.08 (.07) | −.12 (.07) | −.11 (.07)* |
| Gender×CU | .08 (.17) | −.26 (.19) | −.24 (.20) | .04 (.18) |
| Gender×CD | −.21 (.12) | −.17 (.12) | −.21 (.12) | −.33 (.12)** |
| Gender×CU×CD | .15 (.08)* | .12 (.08) | .11 (.08) | .12 (.08) |
Notes: Data presented are from Step 3 of the hierarchical regression models conducted with each dependent variable. Unstandardized beta (SE). Onset = Whether or not adolescents reported any use or impairment by 9th grade (0=no, 1=yes); Family History = Parent-rated history of substance use across 1st and 2nd degree relatives (yes/no); Dep-Adol = Adolescent-reported DISC depression symptom count from 6th grade; Gender (0=Female, 1=Male); CU-Adol = Adolescent-reported APSD Callous-Unemotional scale administered in 6th grade; CD-Adol = Adolescent-reported DISC Conduct Disorder symptom count from 6th grade. Age, depression, CU and CD were centered across gender. All interactions were computed using centered variables.
p < .05,
p < .01
Figure 1.
Gender × adolescent-reported CU × adolescent-reported CD interaction uniquely predicts onset of alcohol use by 9th grade.
On the other hand, results of Step 1 with parent ratings found that CU uniquely predicted the onset of use-related impairment (b = .17, SE = .07, p < .05) over and above covariates, but not the onset of alcohol use (b = .10, SE = .06, p = .10), marijuana use (b = .09, SE = .08, p = .22) or use of both alcohol and marijuana (b = .12, SE = .08, p = .12). Adolescents rated by their parents as having elevated CU traits in 6th grade were more likely to have experienced impairment due to use by 9th grade than those with low parent-reported CU traits. Parent-reported CU remained a unique predictor of impairment onset (b = .17, SE = .07, p < .05) when 6th grade CD severity was added into the equation in Step 2. The CU × CD interaction was nonsignificant, and no gender interactions uniquely predicted the onset of alcohol use, marijuana use, use of both substances, or use-related impairment in Step 3 (see Table 4).
Table 4.
Parent-Reported Risk Factors for Onset of Adolescent Use and Impairment by 9th Grade
| Predictors | Alcohol | Marijuana | Alcohol and Marijuana | Impairment |
|---|---|---|---|---|
| Age | .22 (.25) | .53 (.31) | .46 (.23) | .31 (.29) |
| Family History | .16 (.21) | .46 (.27) | .46 (.28) | .43 (.24) |
| Dep-Par | .08 (.03)** | .04 (.04) | .06 (.04) | .04 (.03) |
| Gender | −.44 (.21)* | −.43 (.26) | −.34 (.28) | −.57 (.24)* |
| CU-Par | .06 (.09) | −.03 (.12) | .00 (.12) | .20 (.10)* |
| CD-Par | .05 (.08) | .14 (.09) | .19 (.10)* | .06 (.09) |
| CU×CD | −.04 (.04) | −.02 (.04) | −.03 (.05) | −.06 (.04) |
| Gender×CU | .06 (.13) | .17 (.16) | .15 (.17) | −.10 (.15) |
| Gender×CD | .02 (.11) | .02 (.12) | −.04 (.12) | .02 (.11) |
| Gender×CU×CD | .01 (.05) | −.01 (.06) | .00 (.06) | .05 (.06) |
Notes: Data presented are from Step 3 of the hierarchical regression models conducted with each dependent variable. Unstandardized beta (SE). Onset = Whether or not adolescents reported any use or impairment by 9th grade (0=no, 1=yes); Family History = Parent-rated history of substance use across 1st and 2nd degree relatives (yes/no); Dep-Par = Parent-reported DISC depression symptom count from 6th grade; Gender (0=Female, 1=Male); CU-Par = Parent-reported APSD Callous-Unemotional scale administered in 6th grade; CD-Par = Parent-reported DISC Conduct Disorder symptom count from 6th grade. Age, depression, CU and CD were centered across gender. All interactions were computed using centered variables.
p < .05,
p < .01
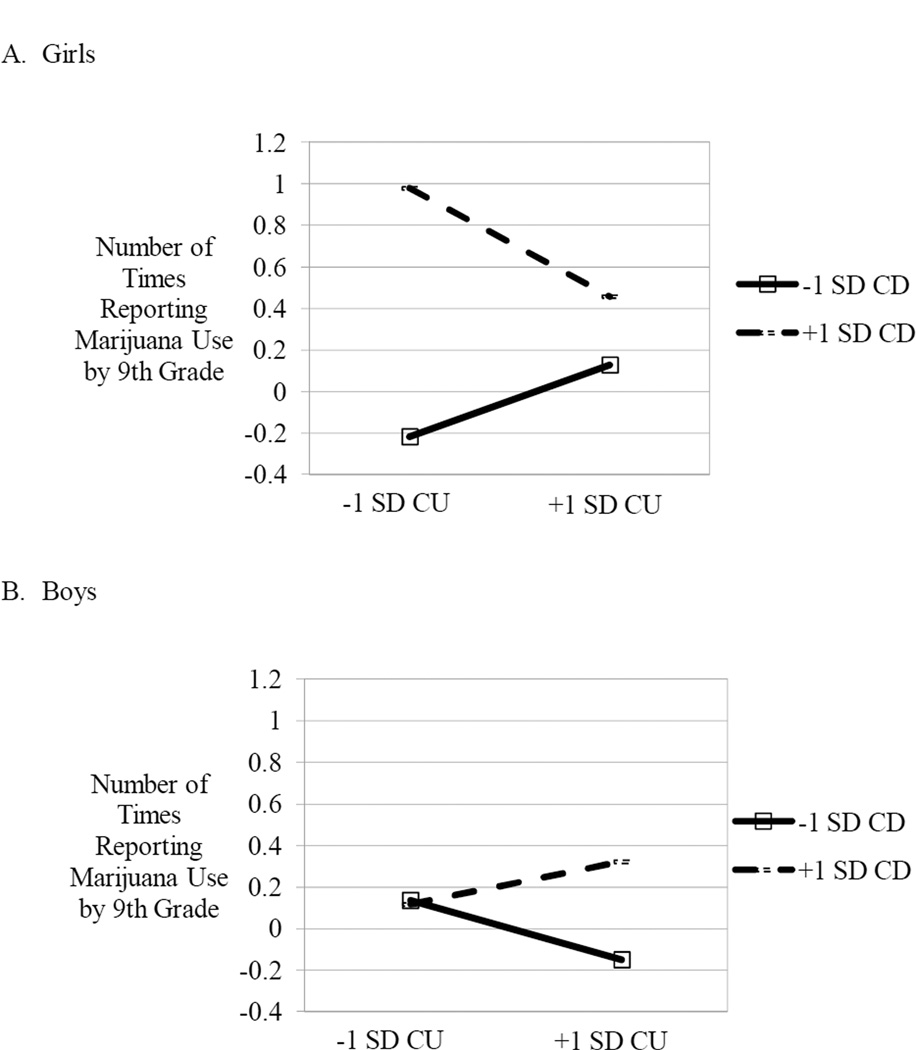
Predicting Recurrence of Substance Use and Impairment
Results of Step 1 with adolescent ratings indicated that, over and above covariates, CU was a unique predictor of recurrent alcohol use (b = .10, SE = .03, p < .01), marijuana use (b = .08, SE = .02, p < .01), use of both alcohol and marijuana (b = .06, SE = .02, p < .01), and use-related impairment (b = .10, SE = .03, p < .01). Adolescents reporting elevated CU traits in 6th grade were more likely than those with lower levels of CU traits to report repeated use of alcohol, marijuana, or both substances and to report recurrent use-related impairment, by 9th grade. However, when 6th grade CD symptoms were entered into the equation in Step 2, adolescent-reported CU traits no longer predicted the recurrence of alcohol use (b = .06, SE = .03, p = .06), marijuana use (b = .00, SE = .02, p = .94), use of both alcohol and marijuana (b = .01, SE = .02, p = . 73), or use-related impairment (b = .03, SE = .03, p = .34). Conversely, CD symptoms increased the likelihood of repeated use of alcohol (b = .08, SE = .02, p < .01), marijuana (b = .08, SE = .01, p < .01), alcohol and marijuana (b = .07, SE = .01, p < .01), as well as impairment (b = .11, SE = .02, p < .01). As shown in Table 5, Step 3 analyses found that gender moderated the effect of the interaction between CU and CD on every measure of substance use and impairment recurrence. Follow-up testing found that CU × CD was a significant predictor of recurrent alcohol use reported by girls (b = -.09, SE = .03, p < .01), but not by boys (b = .01, SE = .01, p = .11). Similar to the pattern displayed in Figure 1A, girls reporting low CU and high CD in 6th grade were most likely to have used alcohol repeatedly by 9th grade. The main effect of CU (b = .07, SE = .03, p < .05), but not CD (b = .02, SE = .02, p = .36), was significant in boys. Follow-up analysis found that CU × CD was a significant predictor of recurrent marijuana use for girls (b = -.04, SE = .02, p < .05) and boys (b = .02, SE = .004, p < .01). As shown in Figure 2, girls with low CU and high CD in 6th grade, as well as boys with high CU and high CD in 6th grade, were those most likely to report repeated use of marijuana by 9th grade. The same pattern held for recurrent use of both alcohol and marijuana (CU × CD for girls: b = -.05, SE = .02, p < .01; CU × CD for boys: b = .02, SE = .003, p < .01) and impairment (CU × CD for girls: b = −.06, SE = .02, p < .05; CU × CD for boys: b = .02, SE = .005, p < .01).
Table 5.
Adolescent-Reported Risk Factors for Recurrent Substance Use and Impairment by 9th Grade
| Predictors | Alcohol | Marijuana | Alcohol and Marijuana | Impairment |
|---|---|---|---|---|
| Age | .05 (.10) | .09 (.07) | −.01 (.06) | .06 (.09) |
| Family History | .11 (.08) | .14 (.06)* | .11 (.05)* | .08 (.07) |
| Dep-Adol | .03 (.01)** | .01 (.01) | .01 (.01) | .01 (.01) |
| Gender | −.48 (.09)** | −.23 (.06)** | −.23 (.05)** | −.36 (.08)** |
| CU-Adol | −.04 (.05) | −.03 (.03) | −.03 (.03) | −.02 (.04) |
| CD-Adol | .15 (.03)** | .12 (.02)** | .11 (.02)** | .19 (.03)** |
| CU×CD | −.09 (.02)** | −.04 (.02)** | −.05 (.01)** | −.06 (.02)** |
| Gender×CU | .10 (.06) | .02 (.04) | .03 (.04) | .05 (.06) |
| Gender×CD | −.12 (.04)** | −.09 (.03)** | −.09 (.02)** | −.15 (.03)** |
| Gender×CU×CD | .10 (.03)** | .07 (.02)** | .07 (.02)** | .08 (.02)** |
Notes: Data presented are from Step 3 of the hierarchical regression models conducted with each dependent variable. Unstandardized beta (SE). Recurrence = Number of visits (up to 9th grade) that adolescents reported any use or impairment; Family History = Parent-rated history of substance use across 1st and 2nd degree relatives (yes/no); Dep-Adol = Adolescent-reported DISC depression symptom count from 6th grade; Gender (0=Female, 1=Male); CU-Adol = Adolescent-reported APSD Callous-Unemotional scale administered in 6th grade; CD-Adol = Adolescent-reported DISC Conduct Disorder symptom count from 6th grade. Age, depression, CU and CD were centered across gender. All interactions were computed using centered variables.
p < .05,
p < .01
Figure 2.
Gender × adolescent-reported CU × adolescent-reported CD uniquely predicts recurrent marijuana use by 9th grade.
Step 1 analyses with parent ratings revealed that CU traits did not predict recurrent alcohol use (b = .03, SE = .03, p = .26), marijuana use (b = .03, SE = .02, p = .14), or use of both alcohol and marijuana (b = .03, SE = .02, p = .11) over and above the covariates, but it did significantly predict use-related impairment recurrence (b = .06, SE = .02, p < .05). As with the prediction of impairment onset, adolescents rated by their parents as having elevated CU traits in 6th grade were more likely to repeatedly report impairment by 9th grade than those with lower levels of CU traits. When CD symptoms were entered into the equation in Step 2, parent-reported CU traits continued to predict impairment recurrence (b = .05, SE = .02, p < .05), while CD did not contribute any additional risk (b = .02, SE = .02, p = .37). However, as part of Step 3, gender did not moderate the prediction of recurrent alcohol use, marijuana use, use of both substances, or use-related impairment (Table 6).
Table 6.
Parent-Reported Risk Factors for Recurrent Adolescent Use and Impairment by 9th Grade
| Predictors | Alcohol | Marijuana | Alcohol and Marijuana | Impairment |
|---|---|---|---|---|
| Age | .21 (.11) | .17 (.07)* | .08 (.07) | .14 (.10) |
| Family History | .13 (.09) | .12 (.06) | .10 (.05)* | .11 (.08) |
| Dep-Par | .04 (.01)** | .01 (.01) | .01 (.01) | .02 (.01)* |
| Gender | −.36 (.09)** | −.12 (.06)* | −.13 (.05)* | −.20 (.08)** |
| CU-Par | .03 (.04) | .01 (.03) | .02 (.02) | .07 (.04) |
| CD-Par | .02 (.04) | .02 (.02) | .01 (.02) | .02 (.03) |
| CU×CD | −.01 (.02) | −.01 (.01) | .00 (.01) | −.01 (.02) |
| Gender×CU | .00 (.06) | .00 (.04) | −.01 (.03) | −.04 (.05) |
| Gender×CD | −.03 (.05) | .02 (.03) | .00 (.03) | −.01 (.04) |
| Gender×CU×CD | .02 (.02) | .01 (.02) | .01 (.01) | .02 (.02) |
Notes: Data presented are from Step 3 of the hierarchical regression models conducted with each dependent variable. Unstandardized beta (SE). Recurrence = Number of visits (up to 9th grade) that adolescents reported any use or impairment; Family History = Parent-rated history of substance use across 1st and 2nd degree relatives (yes/no); Dep-Par = Parent-reported DISC depression symptom count from 6th grade; Gender (0=Female, 1=Male); CU-Par = Parent-reported APSD Callous-Unemotional scale administered in 6th grade; CD-Par = Parent-reported DISC Conduct Disorder symptom count from 6th grade. Age, depression, CU and CD were centered across gender. All interactions were computed using centered variables.
p < .05,
p < .01
Discussion
This study was conducted to clarify the degree to which CU traits uniquely predict the onset and recurrence of substance use and impairment over and above CD symptoms, and whether gender moderates these associations. Adolescents reporting elevated CU traits in 6th grade were more likely than those with lower CU traits to endorse onset and recurrent use of alcohol, marijuana or both substances, as well as use-related impairment, by 9th grade. However these associations were accounted for by CD symptoms. Adolescents whose parents rated them as exhibiting greater CU traits in 6th grade were also more likely to endorse use-related impairment onset and recurrence by 9th grade, regardless of their level of CD symptoms. Notably, our results indicate that adolescent gender should be considered when investigating associations between CU traits and substance use outcomes, as different patterns of results were observed for boys and girls. Though boys reporting high CU traits and high CD symptoms were not more likely to report the onset or recurrence of alcohol use, they were most likely to report recurrent marijuana use, use of both alcohol and marijuana, and impairment due to use. Conversely, girls reporting low CU traits and high CD were most likely to endorse alcohol use onset and recurrence, as well as recurrent marijuana use, use of both substances, and impairment.
To our knowledge, this was the first study to highlight gender as a moderator of the association between adolescent-reported CU traits and substance use. In light of the significant gender interactions with adolescent-reported CU traits and CD symptoms, outcomes will be discussed separately by gender, beginning with our findings with boys. Consistent with our expectations, adolescent boys reporting elevated CU traits and CD symptoms in 6th grade were at greatest risk of recurrent substance use and impairment by 9th grade, relative to those reporting elevated CU traits- or CD-only, or low levels of CU traits and CD symptoms. Mounting evidence from predominantly male samples underscores the risk of persistent and severe delinquency in youth with elevated CU traits and CD symptoms (Frick & Moffitt, 2010), as well as their insensitivity to punishment and their positive expectancies for deviant behavior (Frick & White, 2008). As such, boys with elevated CU traits and CD symptoms may engage in recurrent substance use because they are less impacted by negative consequences and are less likely to cease experimenting with substances, even if they are impaired. At the same time, boys reporting elevated CU traits and CD symptoms in 6th grade were not more likely to report alcohol use by 9th grade. Reporting any alcohol use by this early age is atypical and predictive of poor outcomes (King & Chassin, 2007). Early alcohol use is more common, and potentially less harmful, than early recurrent use of multiple substances or repeatedly endorsing use-related impairment. Thus, CU traits may only predict the most severe manifestations of use by early adolescent boys over and above CD symptoms. Studies are needed to replicate these findings and to examine mechanisms (e.g., responsiveness to punishment, positive expectancies) that may facilitate recurrent and problematic use by adolescent boys with elevated CU traits and CD symptoms.
While we found the expected pattern of results with boys, outcomes were quite different for girls. Specifically, self-reported CU traits did not increase risk for early and problematic substance use in girls with conduct problems. These results corroborated prior research indicating that CU traits and CD symptoms do not interact synergistically in the prediction of female antisocial behavior (Dadds et al., 2005; Frick, Cornell, Barry, et al. 2003). Yet, they were inconsistent with previous studies showing that CU traits increase risk of poor outcomes in some girls (Marsee & Frick, 2007; Pardini, Stepp, Hipwell, Stouthamer-Loeber, & Loeber, 2012). Perhaps CU traits did not increase risk of substance use and impairment among girls in this study because of the limited number of girls who endorsed CU traits in our non-referred sample. Relative to boys, many fewer girls exhibited any CU traits and even fewer exhibited CU traits and CD symptoms. Furthermore, the construct of CU may manifest differently in non-referred girls than those in adjudicated or clinic-referred samples, with behavior patterns from the latter samples mapping on better to how CU appears in boys (Verona et al 2010). CU traits may be a more relevant risk factor in analyses conducted with girls exhibiting more severe behavior problems. Additionally, it may be that puberty influenced associations among CU traits, CD symptoms and substance use among the early adolescent girls in this study. As suggested by Caspi and Moffitt (1991) and Dick and colleagues (2000), a subset of girls in our sample may have matured early, begun exhibiting conduct problems, and used alcohol and marijuana regardless of their level of CU traits. Finally, given evidence suggesting that girls with low CU traits and high CD symptoms have higher rates of anxiety disorders than those with high CU and high CD (Pardini et al., 2012), anxiety could have played a role in exacerbating substance use among girls with conduct problems in this study.
Of note, gender was found to be a moderator in analyses with adolescent ratings of CU traits and CD symptoms, but not with tests including parent ratings of adolescent CU and CD. Instead, we found that adolescents (both girls and boys) whose parents reported they had elevated CU traits in 6th grade were more likely than those with lower CU traits to endorse the onset and recurrence of use-related impairment by 9th grade. These data corroborate the results of the prior study underscoring positive associations between CU traits and substance use among non-referred adolescents (Hillege et al., 2010) and extend them by indicating that CU traits prospectively predict the onset and recurrence of substance use problems in early adolescence. At the same time, parent ratings of CU traits did not predict the onset or recurrence of alcohol and/or marijuana use, outcomes which were predicted by adolescent-rated CU traits. We cannot rule out that respondent effects may have facilitated stronger associations between adolescent-reported CU traits and adolescent-reported substance use outcomes in this study. For this reason, it is recommended that future studies compare the degree to which adolescent- and parent-reported CU traits increase risk of substance use over and above CD symptoms.
Despite the many strengths of this study (e.g., large, diverse sample; longitudinal data), several weaknesses limit the generalizability of our findings. First, our sample is comprised of youth residing in the metropolitan area of Seattle, where use patterns may differ from those of youth in other parts of the country, including suburban or rural locations (Way, Stauber, Nakkula, & London, 1994). Second, the power to detect links between CU and substance use may have been reduced by the relatively low levels of use by our young adolescents. Though adolescents may have underreported their level of use, other research indicates that self-reports of lifetime use are reliable and valid (Shillington & Clapp, 2000). Third, the measure of CU traits used in this study included fewer items than the subscale proposed by Frick and Hare (2001). By eliminating two items that lowered the internal consistency of our CU trait scale, as has been done elsewhere (Poythress et al., 2006), we are more confident in our results but mindful that they may not necessarily generalize to other studies measuring CU traits with Frick and Hare’s original scale. Finally, although one of the strengths of the study is its focus on an important developmental window, the results may not apply to pre- or late-adolescent populations.
Taken together, this study highlights the importance of accounting for adolescent gender and CD symptoms when examining CU traits as a risk factor for substance use. It also provides preliminary evidence in support of boys with elevated CU traits and CD symptoms being at greatest risk for recurrent and problematic substance use in early adolescence. Amid calls for adding CU traits as a modifier of CD diagnostic criteria in DSM-V (Frick & Moffitt, 2010), the degree to which CU traits confer additional risk of delinquency and relevant correlates, such as substance use, among youth with CD needs to be established. Particularly warranted are studies examining environmental (e.g., parenting, peer deviance), cognitive (e.g., positive expectancies), and neurobiological (e.g., impulsivity) mechanisms, as well as gender differences. This work will have implications for future substance use prevention and intervention efforts with at-risk youth.
Acknowledgments
This work was supported by grants from the National Institutes of Health, including R01 AA018701 (awarded to Dr. McCarty) and R01 MH/DA63711 (awarded to Drs. Vander Stoep and McCauley), Seattle Children’s Hospital Steering Committee Grant and American Foundation for Suicide Prevention Grant (awarded to Dr. Vander Stoep), and UW Provost Bridge Funding (awarded to Drs. Vander Stoep and McCauley).
Footnotes
Portions of the analyses were presented at the biennial meeting of the International Society for Research on Child and Adolescent Psychopathology (June, 2011).
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont; 2001. [Google Scholar]
- Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology. 2002;70:1224–1239. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- Bailey SL, Flewelling RL, Rachal JV. The characterization of inconsistencies in self-reports of alcohol and marijuana use in a longitudinal study of adolescents. Journal of Studies on Alcohol. 1992;53:636–647. doi: 10.15288/jsa.1992.53.636. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW. Psychometric evaluation of the Customary Drinking and Drug Use Record: A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Cable N, Sacker A. The role of adolescent social disinhibition expectancies in moderating the relationship between psychological distress and alcohol use and misuse. Addictive Behaviors. 2007;32:282–295. doi: 10.1016/j.addbeh.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE. Individual differences are accentuated during periods of social change. Journal of Personality and Social Psychology. 1991;61:157–168. doi: 10.1037//0022-3514.61.1.157. [DOI] [PubMed] [Google Scholar]
- Chassin L, Ritter J, Trim RS, King KM. Adolescent substance use disorders. In: Mash EJ, Barkley RA, editors. Child Psychopathology. 2nd ed. New York: Guilford Press; 2003. pp. 199–230. [Google Scholar]
- Costello EJ, Angold A. Scales to assess child and adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:726–737. doi: 10.1097/00004583-198811000-00011. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Fraser J, Frost A, Hawes DJ. Disentangling the underlying dimensions of psychopathy and conduct problems in childhood: A community study. Journal of Consulting and Clinical Psychology. 2005;73:400–410. doi: 10.1037/0022-006X.73.3.400. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Hawes DJ, Frost ADJ, Vassallo S, Bunn P, Hunter K, et al. Learning to ‘talk the talk’: The relationship of psychopathic traits to deficits in empathy across childhood. Journal of Child Psychology and Psychiatry. 2009;50:599–606. doi: 10.1111/j.1469-7610.2008.02058.x. [DOI] [PubMed] [Google Scholar]
- Dick DM, Rose RJ, Viken RJ, Kaprio J. Pubertal timing and substance use: Associations between and within families across late adolescence. Developmental Psychology. 2000;36:180–189. [PubMed] [Google Scholar]
- Fontaine NMG, Rijsdijk FV, McCrory EJP, Viding E. Etiology of different developmental trajectories of callous-unemotional traits. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:656–664. doi: 10.1016/j.jaac.2010.03.014. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Bodin SD, Barry CT. Psychopathic traits and conduct problems in community and clinic-referred samples of children: Further development of the Psychopathy Screening Device. Psychological Assessment. 2000;12:382–393. [PubMed] [Google Scholar]
- Frick PJ, Cornell AH, Barry CT, Bodin SD, Dane HE. Callous-unemotional traits and conduct problems in the prediction of conduct problem severity, aggression, and self-report of delinquency. Journal of Abnormal Child Psychology. 2003;31:457–470. doi: 10.1023/a:1023899703866. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Cornell AH, Bodin SD, Dane HE, Barry CT, Loney BR. Callous-unemotional traits and developmental pathways to severe conduct problems. Developmental Psychology. 2003;39:246–260. doi: 10.1037//0012-1649.39.2.246. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Hare RD. Antisocial Process Screening Device (APSD): Technical Manual. Tonawanda, NY: Multi-Health Systems Inc.; 2001. [Google Scholar]
- Frick PJ, Moffitt TE. A proposal to the DSM-V Childhood Disorders and the ADHD and Disruptive Behavior Disorders Work Groups to include a specifier to the diagnosis of conduct disorder based on the presence of callous-unemotional traits. 2010 http://www.dsm5.org/Proposed%20Revision%20Attachments/Proposal%20for%20Callous%20and%20Unemotional%20Specifier%20of%20Conduct%20Disorder.pdf.
- Frick PJ, Stickle TR, Dandreaux DM, Farrell JM, Kimonis ER. Callous-unemotional traits in predicting the severity and stability of conduct problems and delinquency. Journal of Abnormal Child Psychology. 2005;33:471–487. doi: 10.1007/s10648-005-5728-9. [DOI] [PubMed] [Google Scholar]
- Frick PJ, White SF. Research review: The importance of callous-unemotional traits for developmental models of aggressive and antisocial behavior. Journal of Child Psychology and Psychiatry. 2008;49:359–375. doi: 10.1111/j.1469-7610.2007.01862.x. [DOI] [PubMed] [Google Scholar]
- Ginzler JA, Garrett SB, Baer JS, Peterson PL. Measurement of negative consequences of substance use in street youth: An expanded use of the Rutgers Alcohol Problem Index. Addictive Behaviors. 2007;32:1519–1525. doi: 10.1016/j.addbeh.2006.11.004. [DOI] [PubMed] [Google Scholar]
- Gretton HM, Hare RD, Catchpole REH. Psychopathy and offending from adolescence to adulthood. Journal of Consulting and Clinical Psychology. 2004;72:636–645. doi: 10.1037/0022-006X.72.4.636. [DOI] [PubMed] [Google Scholar]
- Harvey PD, Stokes JL, Lord J, Pogge DL. Neurocognitive and personality assessment of adolescent substance abusers. Assessment. 1996;3:241–253. [Google Scholar]
- Hillege S, Das J, de Ruiter C. The Youth Psychopathic Traits Inventory: Psychometric properties and its relation to substance use and interpersonal style in a dutch sample of non-referred adolescents. Journal of Adolescence. 2010;33:83–91. doi: 10.1016/j.adolescence.2009.05.006. [DOI] [PubMed] [Google Scholar]
- Jessor R. Problem-behavior theory, psychosocial development, and adolescent problem drinking. British Journal of Addiction. 1987;82:331–342. doi: 10.1111/j.1360-0443.1987.tb01490.x. [DOI] [PubMed] [Google Scholar]
- Johnson RA, Gerstein DR. Age, period, and cohort effects in marijuana and alcohol incidence: United States females and males, 1961–1990. Substance Use and Misuse. 2000;35:925–948. doi: 10.3109/10826080009148427. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Schulenberg JE, O’Malley PM, Johnston LD, Bachman JG, Li G, et al. The social norms of birth cohorts and adolescent marijuana use in the United States, 1976–2007. Addiction. 2011;106:1790–1800. doi: 10.1111/j.1360-0443.2011.03485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King KM, Chassin L. A prospective study of the effects of age of initiation of alcohol and drug use on young adult substance dependence. Journal of Studies on Alcohol and Drugs. 2007;68(2):256–265. doi: 10.15288/jsad.2007.68.256. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Loney BR, Butler MA, Lima EN, Counts CA, Eckel LA. The relation between salivary cortisol, callous-unemotional traits, and conduct problems in an adolescent non-referred sample. Journal of Child Psychology and Psychiatry. 2006;47:30–36. doi: 10.1111/j.1469-7610.2005.01444.x. [DOI] [PubMed] [Google Scholar]
- Lynam DR, Caspi A, Moffitt TE, Loeber R, Stouthamer-Loeber M. Longitudinal evidence that psychopathy scores in early adolescence predict adult psychopathy. Journal of Abnormal Psychology. 2007;116:155–165. doi: 10.1037/0021-843X.116.1.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam DR, Charnigo R, Moffitt TE, Raine A, Loeber R, Stouthamer-Loeber M. The stability of psychopathy across adolescence. Development and Psychopathology. 2009;21:1133–1153. doi: 10.1017/S0954579409990083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mailloux DL, Forth AE, Kroner DG. Psychopathy and substance use in adolescent male offenders. Psychological Reports. 1997;81:529–530. [PubMed] [Google Scholar]
- Marsee MA, Frick PJ. Exploring the cognitive and emotional correlates to proactive and reactive aggression in a sample of detained girls. Journal of Abnormal Child Psychology. 2007;35:969–981. doi: 10.1007/s10802-007-9147-y. [DOI] [PubMed] [Google Scholar]
- Marsee MA, Silverthorn P, Frick PJ. The association of psychopathic traits with aggression and delinquency in non-referred boys and girls. Behavioral Sciences and the Law. 2005;23:803–817. doi: 10.1002/bsl.662. [DOI] [PubMed] [Google Scholar]
- McMahon RJ, Witkiewitz K, Kotler JS the Conduct Problems Prevention Research Group. Predictive validity of callous-unemotional traits measured in early adolescence with respect to multiple antisocial outcomes. Journal of Abnormal Psychology. 2010;119:752–763. doi: 10.1037/a0020796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller ET, Neal DJ, Roberts LJ, Baer JS, Cressler SO, Metrick J, et al. Test-retest reliability of alcohol measures: Is there a difference between internet-based assessment and traditional methods? Psychology of Addictive Behaviors. 2002;16:56–63. [PubMed] [Google Scholar]
- Murrie DC, Cornell DG. The Millon Adolescent Clinical Inventory and Psychopathy. Journal of Personality Assessment. 2000;75:110–125. doi: 10.1207/S15327752JPA7501_8. [DOI] [PubMed] [Google Scholar]
- Obradovic J, Pardini DA, Long JD, Loeber R. Measuring interpersonal callousness in boys from childhood to adolescence: An examination of longitudinal invariance and temporal stability. Journal of Clinical Child and Adolescent Psychology. 2007;36:276–292. doi: 10.1080/15374410701441633. [DOI] [PubMed] [Google Scholar]
- Pardini DA, Lochman JE, Frick PJ. Callous/unemotional traits and social-cognitive processes in adjudicated youths. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:364–371. doi: 10.1097/00004583-200303000-00018. [DOI] [PubMed] [Google Scholar]
- Pardini D, Stepp S, Hipwell A, Stouthamer-Loeber M, Loeber R. The clinical utility of the proposed DSM-5 callous-unemotional subtype of conduct disorder in young girls. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:62–73. doi: 10.1016/j.jaac.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poythress ND, Douglas KS, Falkenback D, Cruise K, Lee Z, Murrie DC, et al. Internal consistency reliability of the self-report Antisocial Process Screening Device. Assessment. 2006;13:107–113. doi: 10.1177/1073191105284279. [DOI] [PubMed] [Google Scholar]
- Roussy S, Toupin J. Behavioral inhibition deficits in juvenile psychopaths. Aggressive Behavior. 2000;26:413–424. [Google Scholar]
- Schaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone ME, Shaffer D, Dulcan MK, Jensen PS, Fisher P, Bird HR, et al. Criterion validity of the NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3) Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:878–888. doi: 10.1097/00004583-199607000-00013. [DOI] [PubMed] [Google Scholar]
- Shillington AM, Clapp JD. Self-report stability of adolescent substance use: Are there differences for gender, ethnicity and age? Drug and Alcohol Dependence. 2000;60:19–27. doi: 10.1016/s0376-8716(99)00137-4. [DOI] [PubMed] [Google Scholar]
- Skenderian JJ, Siegel JT, Crano WD, Alvaro EE, Lac A. Expectancy change and adolescents’ intentions to use marijuana. Psychology of Addictive Behaviors. 2008;22:563–569. doi: 10.1037/a0013020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug and Alcohol Dependence. 2004;75(3):287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Vander Stoep A, McCauley E, Thompson KA, Herting JR, Kuo ES, Stewart DG, et al. Universal emotional health screening at the middle school transition. Journal of Emotional and Behavioral Disorders. 2005;13:213–223. doi: 10.1177/10634266050130040301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verona E, Sadeh N, Javdani E. The influence of gender and culture on child and adolescent psychopathy. In: Salekin RT, Lynam DR, editors. Handbook of Child and Adolescent Psychopathy. New York, NY: Guilford Press; 2010. pp. 401–419. [Google Scholar]
- Viding E, Frick PJ, Plomin R. Aetiology of the relationship between callous-unemotional traits and conduct problems in childhood. British Journal of Psychiatry. 2007;190S:s33–s38. doi: 10.1192/bjp.190.5.s33. [DOI] [PubMed] [Google Scholar]
- Viding E, Simmonds E, Petrides KV, Frederickson N. The contribution of callous-unemotional traits and conduct problems to bullying in early adolescence. Journal of Child Psychology and Psychiatry. 2009;50:471–481. doi: 10.1111/j.1469-7610.2008.02012.x. [DOI] [PubMed] [Google Scholar]
- Way N, Stauber HY, Nakkula MJ, London P. Depression and substance use in two divergent high school cultures: A quantitative and qualitative analysis. Journal of Youth and Adolescence. 1994;23:331–357. [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: The Family History Screen. Archives of General Psychiatry. 2000;57:675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;51:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]