Abstract
Purpose
To determine whether bifocal soft contact lenses with a distance center design provide myopic defocus to the peripheral retina similar to corneal reshaping contact lenses.
Methods
Myopic subjects underwent five cycloplegic autorefraction readings centrally and at 10, 20, and 30 degrees temporally, nasally, superiorly, inferiorly while wearing a Proclear Multifocal “D” contact lens with a +2.00 D add (CooperVision, Fairport, NY) and after wearing a Corneal Refractive Therapy (Paragon Vision Sciences, Mesa, AZ) contact lens for two weeks
Results
Fourteen subjects completed the study. Nine (64%) were female, and 12 (86%) were Caucasian. The average (± standard deviation) spherical equivalent non-cycloplegic manifest refraction for the right eye was −2.84 ± 1.29 D. The average logMAR best-corrected, binocular high contrast visual acuity was −0.17 ± 0.15 while wearing the bifocal soft contact lens, and −0.09 ± 0.16 following corneal reshaping contact lens wear (ANOVA, p = 0.27). The orthokeratology contact lens yielded a more myopic peripheral optical profile than the soft bifocal contact lens at 20 and 30 degrees eccentricity (except inferior at 20 degrees); the two modalities were similar at 10 degrees eccentricity.
Conclusions
Our data suggest that the two modalities are dissimilar despite the statistical similarities. The corneal reshaping contact lens shows an increase in relative peripheral myopic refraction, a pattern achieved by other studies, but the bifocal lens does not exhibit such a pattern. The low statistical power of the study could be a reason for a lack of providing statistical difference in other positions of gaze, but the graphical representation of the data shows a marked difference in peripheral optical profile between the two modalities. More sophisticated methods of measuring the peripheral optical profile may be necessary to accurately compare the two modalities and to determine the true optical effect of the bifocal soft contact lens on the peripheral retina.
Keywords: myopia, peripheral, refractive error, orthokeratology, soft bifocal, contact lens
Myopia is a very common visual condition that affects more than 100 million people in the United States alone.1 There is no cure to date, and current research primarily focuses on determining the mechanisms that may slow progression.
As gas permeable contact lens (GP) materials and designs improve, clinicians and researchers note complete myopia treatment with corneal reshaping contact lenses2–11 as well as a reduction of myopia progression associated with corneal reshaping contact lens wear.12–14 Recent studies indicate slowed axial elongation while wearing corneal reshaping contact lenses.12–15
The most prominent theory regarding how corneal reshaping contact lenses may slow myopia progression implicates a side effect of the refractive correction. Myopic defocus slows eye growth, and hyperopic blur increases eye growth in animals,16–17 and until recently, it was believed that was due solely to optical blur presented to the fovea. Recent primate studies indicate that the peripheral retina may be more responsible for the regulation of eye growth than previously thought possible.18–20 Specifically, Smith and colleagues showed that peripheral form deprivation and peripheral hyperopic blur with clear central vision led to myopic eye growth, and once the peripheral form deprivation was removed, the eyes emmetropized, even if the fovea was ablated.18, 20 Smith and colleagues also showed that ablation of the fovea and parafovea do not alter induced myopic eye growth or emmetropization in primates.19
Several investigators have extended similar findings to humans. Airline pilots with peripheral hyperopic defocus are more likely to develop myopia21, though this interpretation of their findings has been disputed in a recent publication.22 Furthermore, children with myopic eyes experience relative hyperopia in the periphery that hyperopic and emmetropic eyes do not.23 and in longitudinal analyses, children who became myopic had more relative hyperopic peripheral blur than emmetropic children two years before the onset of myopia.24
Contrary to the aforementioned studies, Mutti and colleagues showed that although relative peripheral hyperopic blur was related to myopia progression, the magnitude of the effect was extremely small, and relative peripheral hyperopic blur was not related to axial elongation.25 Two other studies have failed to find a consistent difference in the peripheral refraction between refractive error groups.26–27 However, myopic defocus is a much stronger signal to slow eye growth than hyperopic blur is to increase eye growth,28 so while peripheral hyperopic blur may not be related to myopia progression, peripheral myopic defocus may still be related to slower axial elongation.
Corneal reshaping contact lenses provide clear central vision while creating myopic defocus on the peripheral retina, as indicated by the association between increased spherical aberration and peripheral myopic defocus29 and peripheral myopia that increases with retinal eccentricity.30–32 This peripheral myopic defocus may act as a signal to slow eye growth.
Bifocal soft contact lenses with a distance center design should provide a similar optical profile to the myopic retina, due to the central corrected refractive error with less minus power in the periphery. Indeed, anecdotal evidence33 and evidence from controlled trials34–35 exists to confirm that distance center bifocal soft contact lenses may indeed slow myopia progression, and the prevailing theory is that the lenses provide myopic defocus to the peripheral retina to slow eye growth.
If both corneal reshaping and bifocal soft contact lenses have a similar effect on the peripheral optical profile, it may stand to reason that both modalities may slow the progression of myopia by a shared trait: peripheral myopic defocus. The purpose of this investigation is to determine whether a distance center bifocal soft contact lens provides myopic defocus to the peripheral retina similar to a corneal reshaping contact lens.
METHODS
The study was approved by the Biomedical Institutional Review Board of The Ohio State University. Parents provided informed, written permission, and children provided assent.
Eligibility criteria included patients aged 8 to 35 years, adequate ocular health for contact lens wear, best-corrected visual acuity of 20/25 in each eye at distance and near, and non-cycloplegic spherical component manifest refraction between −0.75 DS and −5.00 DS, with no more than −0.75 D of cylinder.
Consecutive subjects were examined for eligibility at the baseline examination via non-cycloplegic manifest refraction, corneal topography, and slit lamp examination. Standard refraction with Jackson crossed cylinder and von Graefe balance was conducted with least minus for best visual acuity as the end point.
Binocular logMAR visual acuity was assessed at distance and near. The distance visual acuity chart was calibrated to a luminance of 75 to110 cd/m2. Standing 4 m from the chart, with the results of the manifest refraction before the eyes, subjects read every letter on each line, beginning at the top of the chart. They continued until three or more letters were read incorrectly after reading an entire line. The total number of letters read correctly was recorded and converted to logMAR visual acuity. The same procedure was followed while reading a near chart at 40 cm with ambient room light and a stand lamp directed at the chart.
Subjects were fit with a Proclear Multifocal lens with a distance center in each eye. The initial power of the contact lens was the vertex-adjusted spherical equivalent of the manifest refraction with a +2.00 D add power. The subjects then repeated the logMAR visual acuity testing at distance and near after just a few minutes of settling time.
The contact lenses were removed, and two drops of 1% tropicamide were administered 5 minutes apart. Autorefraction was performed 25 minutes after the last drop with the multifocal lenses on the eye.
The Grand Seiko WR-5100K (Grand Seiko Co., Ltd.; Fukuyama, Japan) autorefractor was used to measure the peripheral optical profile. The patients were instructed to view markings on a wall at 10, 20, and 30 degrees in the temporal, nasal, superior, and inferior quadrants. The “X” markings were large enough for vision-corrected subjects to fixate, and they were located 1.27 to 1.35 m from the subject’s eye. The refractive error in primary gaze was measured while the subject fixated a 20/30 letter on a near point card placed beyond the subject’s far point while viewed through a +4.00 D Badal lens. A minimum of five measurements was taken for each position of gaze. Any result that was greater than 1.00 D (spherical or cylindrical component) from the mode was manually discarded.
Vertical targets at 10 degrees were directly viewed by rotating the eyes. A mirror system was established to view the superior targets at 20° and 30°. The subjects looked superior into a mirror, which reflected targets presented at 20° and 30° in the inferior position. The subject fixated the center of the camera aperture on the autorefractor for the 20° inferior position, and the subject looked down into a mirror to fixate a target that was actually located at 30° superior. Using the mirror system and fixating the center of the camera aperture on the autorefractor enabled subjects to fixate targets not otherwise possible with the Grand Seiko WR-5100K.36
Once the peripheral optical profile measurement was performed on both eyes, the subject discarded the multifocal lenses and CRT contact lenses were fit. Each initial CRT contact lens was based on the subjects’ spherical component from the manifest refraction and the flat keratometry value. A drop of anesthetic was placed in the eye prior to contact lens insertion. Once the fit was acceptable, lenses were dispensed, and patients attended a brief follow-up visit the next morning.
Patients were examined approximately ten days after the initial fit. Binocular logMAR visual acuity was assessed at distance and near, and cycloplegia was achieved in the same manner as day one. The peripheral optical profile was measured in the exact method as was performed during the baseline examination, except no contact lens was on the eye.
Contact Lenses
The multifocal lens was the Proclear Multifocal “D” lens (CooperVision, Fairport, NY) with a distance center design and a +2.00 D add. The lens material is omafilcon A, with 62% water content, and a 14.4 mm diameter. The central spherical zone of this lens is 2.3 mm in diameter, with an aspheric annular zone progressively increasing in plus power out to an 8.5 mm diameter. The vertex-adjusted spherical equivalent was used for the initial power selection.
The Paragon CRT lenses (Paragon Vision Sciences, Mesa, AZ) were made of HDS 100 material. The lenses had a 10.5 mm diameter, with a 6 mm optic zone diameter, a 1 mm wide sigmoid return zone diameter (RZD), an infinite radius landing zone angle (LZA), and a peripheral edge ellipse. The lens fit was observed, and necessary adjustments were made according to the manufacturer’s recommendations.
Statistical Methods
Data were dual entered into a Microsoft Excel database, and a corrected dataset was analyzed using SPSS (IBM Corporation, Somers, NY). Student’s t-tests were performed to compare the refractive error at each peripheral optical profile location between bifocal soft and corneal reshaping modalities. Bonferroni correction for multiple testing was used to determine significant differences at each location (0.05 / 13 = 0.004). A repeated measures one-way analysis of variance (ANOVA) was performed to compare peripheral refraction between the two modalities: bifocal soft contact lenses and corneal reshaping contact lenses.
RESULTS
Of the sixteen subjects recruited for this study, ten subjects (62.5%) were female and fourteen subjects (87.5%) were Caucasian, with an average (± SD) age of 26.6 ±2.8 years. The subjects had slightly less than 3.00 D myopia with very little astigmatism. Two subjects did not complete the study, due to difficulties with insertion and removal of the lenses. Demographic and ocular information for the enrolled subjects and the subjects who completed the study are presented in Table 1. There were no statistically or clinically meaningful differences between those enrolled and those who completed the study. At baseline, the average logMAR best-spectacle-corrected, binocular, high contrast visual acuity for the fourteen subjects who completed the study was −0.14 ± 0.08 (Snellen 20/14). The average logMAR visual acuity was −0.17 ± 0.15 (20/13) while wearing bifocal soft contact lenses, and −0.09 ± 0.16 (20/17) with corneal reshaping contact lens wear (ANOVA, p = 0.27). On average, the subjects’ peripheral refractive error was measured 13.8 ± 2.9 days after commencing corneal reshaping contact lens wear.
Table 1.
Demographic information of subjects enrolled and subjects who completed the study. Numbers are mean ± SD unless otherwise noted. There are no significant differences between the two groups.
| Subjects Enrolled (n = 16) | Subjects Completed (n = 14) | ||||||
|---|---|---|---|---|---|---|---|
| Mean age (years) | 26.6 ± 2.8 | 25.1 ± 2.9 | |||||
| Gender (% female) | 62.5 | 66.7 | |||||
| Ethnicity (%) | |||||||
| Asian or Pacific Islander | 6.3 | 7.1 | |||||
| Black, not of Hispanic origin | 6.3 | 7.1 | |||||
| Caucasian, not of Hispanic origin | 87.5 | 85.7 | |||||
| Baseline BVA OU (logMAR) | −0.14 ± 0.08 | −0.14 ± 0.08 | |||||
| Bifocal soft VA (logMAR) | −0.16 ± 0.14 | −0.17 ± 0.15 | |||||
| CRT VA (logMAR) | −0.10 ± 0.16 | –0.09 ± 0.16 | |||||
| Baseline Refractive Error (D) | |||||||
| M | −2.84 ± 1.29 | −2.88 ± 1.22 | |||||
| J0 | −0.01 ± 0.07 | −0.01 ± 0.07 | |||||
| J45 | +0.02 ±0.12 | +0.02 ±0.13 | |||||
There was not a significant interaction between eye and lens type, eye and degrees of eccentricity, or eye and gaze direction, so data from the right eye only were included. There was a significant interaction between lens type and degree of eccentricity (p < 0.001) and also between the degree of eccentricity and gaze direction (p = 0.009), indicating that bifocal soft and corneal reshaping contact lenses do not provide equivalent optical profiles in the periphery (Table 2).
Table 2.
Statistical values of repeated measures ANOVA for interactions. All values based off Greenhouse-Geisser adjustment.
| Interaction Source | df | Mean Square | F | Significance |
|---|---|---|---|---|
| Eye * Eccentricity | 2.12 | 1.40 | 0.95 | 0.41 |
| Eye * Lens | 2.39 | 0.42 | 0.48 | 0.65 |
| Eye * Gaze | 2.28 | 0.78 | 0.65 | 0.58 |
| Lens * Eccentricity | 1.26 | 122.86 | 22.73 | < 0.001 |
| Eccentricity * Gaze | 3.73 | 6.11 | 3.90 | 0.009 |
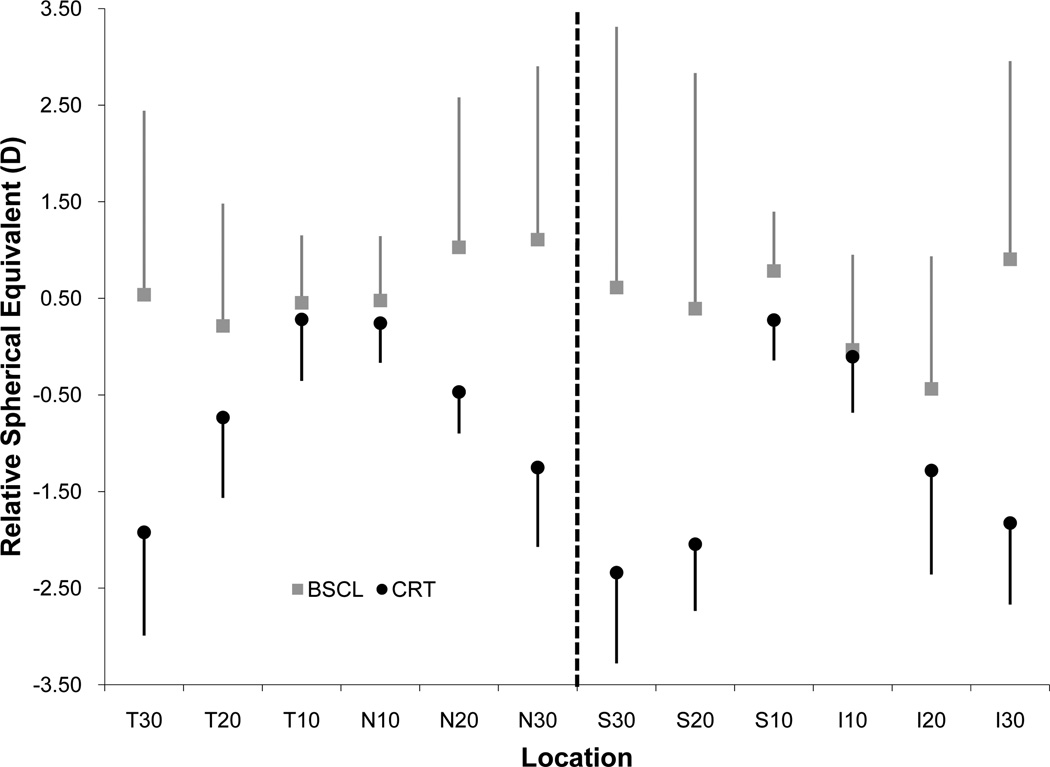
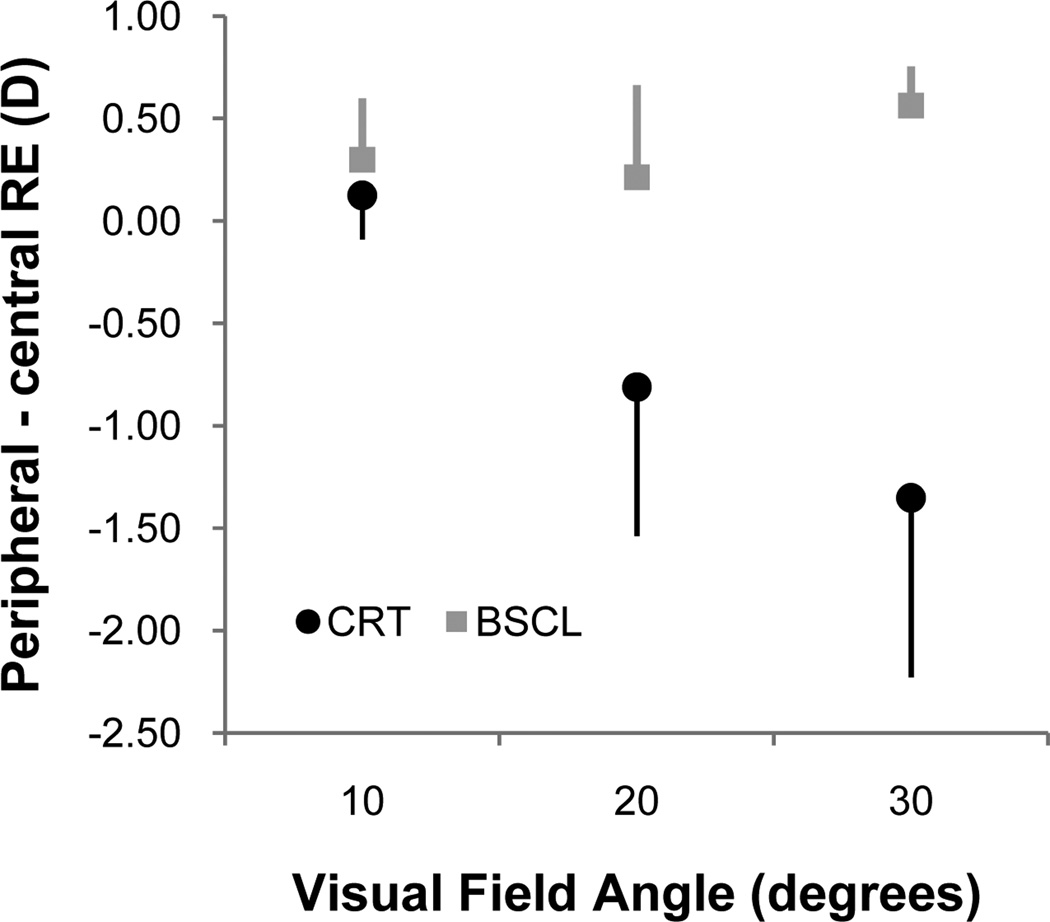
Figure 1 shows the mean ± SD relative spherical equivalent peripheral autorefractions of the right eye at each retinal location. The increase in myopic spherical equivalent refraction with increasing eccentricity is apparent with corneal reshaping contact lens wear, but not bifocal soft contact lens wear. Averaging each eccentricity across the four gazes provides a similar picture. Corneal reshaping lenses provide relative myopia in the periphery, but there is little change with bifocal soft contact lenses (Figure 2).
Figure 1.
Relative spherical equivalent refractive error at each gaze (T = temporal; N = nasal; S = superior; I = inferior) and eccentricity (10°, 20°, and 30°) for corneal reshaping (CRT) and bifocal soft (BSCL) contact lenses.
Figure 2.
Relative peripheral spherical equivalent refractive error at each eccentricity (10°, 20°, and 30°), averaged across each of the four locations (superior, inferior, nasal, and temporal) for corneal reshaping (CRT) and bifocal soft (BSCL) contact lenses.
Statistical comparison of the peripheral refraction (difference = bifocal soft – corneal reshaping) at each location is shown in Table 3. Corneal reshaping values are more myopic than bifocal soft values at all 30° locations, and at all 20° locations except inferior. Corneal reshaping values are less myopic than bifocal soft values in primary gaze. There is not a significant difference between corneal reshaping and bifocal soft contact lens wearers at any of the 10° locations.
Table 3.
Statistical comparison of spherical equivalent peripheral refraction between bifocal soft and corneal reshaping contact lenses for the right eye. A positive difference means corneal reshaping values are more myopic or less hyperopic than bifocal soft values.
| Location | Mean ± SD difference | 95% CI for difference |
|---|---|---|
| Central | −0.51 ± 0.41 | −0.74,−0.27 |
| Temporal | ||
| 10 | −0.13 ± 1.02 | −0.71, +0.46 |
| 20 | +0.65 ± 1.09 | +0.02, +1.30 |
| 30 | +1.84 ± 1.80 | +0.80, +2.88 |
| Nasal | ||
| 10 | +0.11 ± 0.91 | −0.42, +0.64 |
| 20 | +1.15 ± 1.55 | +0.25, +2.04 |
| 30 | +2.11 ± 2.07 | +0.92, +3.30 |
| Superior | ||
| 10 | +0.23 ± 1.13 | −0.42, +0.88 |
| 20 | +1.64 ± 1.84 | +0.57, +2.70 |
| 30 | +2.02 ± 1.99 | +0.87, +3.17 |
| Inferior | ||
| 10 | −0.06 ± 1.09 | +0.56, −0.22 |
| 20 | +0.60 ± 1.66 | −0.35, +1.56 |
| 30 | +2.18 ± 2.25 | +0.89, +3.48 |
DISCUSSION
Both corneal reshaping12–14 and bifocal soft33–35, 37 contact lenses may slow axial elongation of the eye, and if they both work via the same mechanism, it is thought to be due to myopic defocus presented to the peripheral retina. This study compared the effect of corneal reshaping and bifocal soft contact lenses on the peripheral refractive error.
Bifocal soft and corneal reshaping contact lenses do not affect central and peripheral refractive error similarly. Centrally, the soft bifocal contact lenses provided more myopic refractive error than the corneal reshaping contact lenses. The central optic zone of the Proclear Multifocal lens is 2.3 mm in diameter, compared to a central treatment zone with corneal reshaping contact lens wear, depicted by corneal topography, of approximately 4 mm. The entrance pupil of the Grand Seiko autorefractor is 2.0 mm, so it is more likely to include the peripheral ring of “plus” power on a Proclear Multifocal contact lens wearer than a corneal reshaping contact lens wearer. This may explain the more myopic central refraction for bifocal soft contact lens wearers than the corneal reshaping contact lens wearers despite better than 20/20 visual acuity for both vision correction modalities. Refraction through the center of a bifocal soft contact lens has not been reported in the literature, but the spherical equivalent refractive error reported after stable corneal reshaping contact lens wear ranges from −0.17 D to −0.55 D, depending on the time of day it is measured and the method of measurement.11–12, 31, 38–40 The average central spherical equivalent refractive error in this study was −0.42 D, within the range of values reported by other studies.
There were no significant differences between bifocal soft and corneal reshaping contact lenses at 10 degrees eccentricity, but at 20 and 30 degrees eccentricity the corneal reshaping contact lens wearers had significantly more myopic refractive error than the bifocal soft contact lens wearers (except in inferior gaze at 20 degrees). In theory, we expected to see an increasing myopic shift in both the bifocal soft and corneal reshaping contact lenses, but that was not the case. There was almost no myopic shift in refractive error with the bifocal soft contact lens.
According to the Proclear Multifocal fitting guide, the near add power gradually increases 1.2 mm (approximately 21.8°) from the central cornea to 4.3 mm (approximately 55.1°) from the central cornea (assuming the entrance pupil of the eye is 3.0 mm posterior to the anterior cornea). It is likely that the 10° and 20° eccentricities included no to low add power. Although the 30° eccentricity was expected to measure refractive error within the near add portion of the lens, contact lenses typically decenter opposite the direction of gaze, potentially resulting in refractive error measurements that don’t reach the peripheral reading addition power of the lens. The bifocal soft contact lens was assessed for appropriate fit at the initial examination, but movement of the lens in various gazes was not recorded. For example, when refractive error is measured in temporal gaze, the lens may decenter nasally, which increases the likelihood that the autorefractor measures through the central distance portion of the contact lens and results in apparently less myopic refractive error in the periphery. Turning the head instead of the eyes to peripheral targets may reduce the likelihood of this potential source of error.
The peripheral targets were large “X” targets located 1.27 to 1.35 m from the subject’s eye, resulting in an accommodative stimulus of 0.74 to 0.79 D. All subjects’ refractive error was corrected when viewing the targets, so proper fixation was likely, and the same residual accommodation and accommodative stimulus were possible for both corneal reshaping and soft bifocal contact lens wearers, so the peripheral targets were not expected to affect the results of the investigation.
Our sample size of 14 subjects provides 50% power to detect a 1.00 D difference (assuming variability of 1.00 D) between the two lens modalities. If we increased our sample size, we may find statistically significant differences between corneal reshaping and bifocal contact lens wear at 10 and 20 degree gazes. However, given the significant differences observed in the 30 degree peripheral optical profile between corneal reshaping and bifocal soft contact lenses, further recruitment of subjects is not warranted. We are interested in the similarities in the peripheral optical profile of the two modalities, not the differences. If the two modalities provide similar peripheral optical profiles, we may then assume that both treatments slow myopia progression due to the peripheral myopic defocus.
Although soft bifocal contact lenses appear to slow myopia progression in initial studies,33–35, 37 this study did not measure myopic refractive error in the retinal periphery of soft bifocal contact lens wearers. Peripheral myopic refractive error with soft bifocal contact lenses may not have been measured because the +2.00 D add power may be lower than the peripheral plus measured on corneal reshaping contact lens wearers. The annular ridge may induce a much more dramatic optical shift in light rays compared to a +2.00 D add power. The Proclear Multifocal lens is designed with a 2.3 mm wide distance center, which blends into intermediate powers and doesn’t reach the full +2.00 D add power until 5 mm outside of the center. This subtle increase in near add power out to the 5 mm zone may not allow the peripheral optical profile to perform in a way similar to the corneal reshaping contact lens. An analysis of the topography of the corneal reshaping contact lens effect versus an eye wearing the Proclear Multifocal contact lens may give a better assessment of these differences, but from our results it is difficult to determine what may cause the differences found between corneal reshaping and bifocal soft contact lenses. In the future, possibly utilizing a computer based ray-tracing program may help give a better representation of the compared optics reaching the eye when comparing the lens modalities.
CONCLUSIONS
Although many people assume that bifocal soft and corneal reshaping contact lenses both slow myopia progression by providing myopic defocus to the retinal periphery, results from this study cannot confirm that bifocal soft contact lenses provide myopic defocus to the retinal periphery. Perhaps the bifocal soft contact lenses do not provide myopic defocus in the retinal periphery or perhaps an alternate study design, such as turning the head instead of the eyes in order to minimize contact lens decentration,41 is required to measure peripheral myopic defocus with soft contact lenses.
ACKNOWLEDGMENTS
NIH Grant T35 EY007151, Paragon Vision Sciences, CooperVision, Alcon
JJW has received research materials from Paragon Vision Sciences, CooperVision, and Alcon. He also consults with Bausch & Lomb and Johnson & Johnson Vision Care.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
AT has no conflicts to disclose.
REFERENCES
- 1.Vitale S, Ellwein L, Cotch MF, Ferris FL, 3rd, Sperduto R. Prevalence of refractive error in the United States, 1999–2004. Arch Ophthalmol. 2008;126:1111–1119. doi: 10.1001/archopht.126.8.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berntsen DA, Mitchell GL, Barr JT. The effect of overnight contact lens corneal reshaping on refractive error-specific quality of life. Optom Vis Sci. 2006;83:354–359. doi: 10.1097/01.opx.0000221401.33776.54. [DOI] [PubMed] [Google Scholar]
- 3.Lipson MJ. Long-term clinical outcomes for overnight corneal reshaping in children and adults. Eye Contact Lens. 2008;34:94–99. doi: 10.1097/ICL.0b013e31811eba10. [DOI] [PubMed] [Google Scholar]
- 4.Lipson MJ, Sugar A. Corneal reshaping: is it a good alternative to refractive surgery? Curr Opin Ophthalmol. 2006;17:394–398. doi: 10.1097/01.icu.0000233961.19004.cf. [DOI] [PubMed] [Google Scholar]
- 5.Lipson MJ, Sugar A, Musch DC. Overnight corneal reshaping versus soft daily wear: a visual quality of life study (interim results) Eye Contact Lens. 2004;30:214–217. doi: 10.1097/01.icl.0000140236.23820.97. [DOI] [PubMed] [Google Scholar]
- 6.Lipson MJ, Sugar A, Musch DC. Overnight corneal reshaping versus soft disposable contact lenses: vision-related quality-of-life differences from a randomized clinical trial. Optom Vis Sci. 2005;82:886–891. doi: 10.1097/01.opx.0000180818.40127.dc. [DOI] [PubMed] [Google Scholar]
- 7.Lu F, Jiang J, Qu J, Jin W, Mao X, Shen Y. Clinical study of orthokeratology in young myopic adolescents. Int Contact Lens Clin. 1999;26:113–116. doi: 10.1016/s0892-8967(00)00032-8. [DOI] [PubMed] [Google Scholar]
- 8.Rah MJ, Jackson JM, Jones LA, Marsden HJ, Bailey MD, Barr JT. Overnight orthokeratology: preliminary results of the Lenses and Overnight Orthokeratology (LOOK) study. Optom Vis Sci. 2002;79:598–605. doi: 10.1097/00006324-200209000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Ritchey ER, Barr JT, Mitchell GL. The comparison of overnight lens modalities (COLM) study. Eye Contact Lens. 2005;31:70–75. doi: 10.1097/01.icl.0000146323.18919.13. [DOI] [PubMed] [Google Scholar]
- 10.Soni PS, Nguyen TT, Bonanno JA. Overnight orthokeratology: visual and corneal changes. Eye Contact Lens. 2003;29:137–145. doi: 10.1097/01.ICL.0000072831.13880.A0. [DOI] [PubMed] [Google Scholar]
- 11.Walline JJ, Rah MJ, Jones LA. The Children's Overnight Orthokeratology Investigation (COOKI) pilot study. Optom Vis Sci. 2004;81:407–413. doi: 10.1097/01.opx.0000135093.77007.18. [DOI] [PubMed] [Google Scholar]
- 12.Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30:71–80. doi: 10.1080/02713680590907256. [DOI] [PubMed] [Google Scholar]
- 13.Kakita T, Hiraoka T, Oshika T. Influence of overnight orthokeratology on axial elongation in childhood myopia. Invest Ophthalmol Vis Sci. 2011;52:2170–2174. doi: 10.1167/iovs.10-5485. [DOI] [PubMed] [Google Scholar]
- 14.Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93:1181–1185. doi: 10.1136/bjo.2008.151365. [DOI] [PubMed] [Google Scholar]
- 15.Cheung SW, Cho P, Fan D. Asymmetrical increase in axial length in the two eyes of a monocular orthokeratology patient. Optom Vis Sci. 2004;81:653–656. doi: 10.1097/01.opx.0000144742.57847.b1. [DOI] [PubMed] [Google Scholar]
- 16.Troilo D, Wallman J. The regulation of eye growth and refractive state: an experimental study of emmetropization. Vision Res. 1991;31:1237–1250. doi: 10.1016/0042-6989(91)90048-a. [DOI] [PubMed] [Google Scholar]
- 17.Smith EL, 3rd, Hung LF, Harwerth RS. Effects of optically induced blur on the refractive status of young monkeys. Vision Res. 1994;34:293–301. doi: 10.1016/0042-6989(94)90088-4. [DOI] [PubMed] [Google Scholar]
- 18.Smith EL, 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF. Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2005;46:3965–3972. doi: 10.1167/iovs.05-0445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith EL, 3rd, Ramamirtham R, Qiao-Grider Y, Hung LF, Huang J, Kee CS, Coats D, Paysse E. Effects of foveal ablation on emmetropization and form-deprivation myopia. Invest Ophthalmol Vis Sci. 2007;48:3914–3922. doi: 10.1167/iovs.06-1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith EL, 3rd, Hung LF, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009;49:2386–2392. doi: 10.1016/j.visres.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoogerheide J, Rempt F, Hoogenboom WP. Acquired myopia in young pilots. Ophthalmologica. 1971;163:209–215. doi: 10.1159/000306646. [DOI] [PubMed] [Google Scholar]
- 22.Rosen R, Lundstrom L, Unsbo P, Atchison DA. Have we misinterpreted the study of Hoogerheide et al.(1971)? Optom Vis Sci. 2012;89:1235–1237. doi: 10.1097/OPX.0b013e318264f2d1. [DOI] [PubMed] [Google Scholar]
- 23.Mutti DO, Sholtz RI, Friedman NE, Zadnik K. Peripheral refraction and ocular shape in children. Invest Ophthalmol Vis Sci. 2000;41:1022–1030. [PubMed] [Google Scholar]
- 24.Mutti DO, Hayes JR, Mitchell GL, Jones LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48:2510–2519. doi: 10.1167/iovs.06-0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mutti DO, Sinnott LT, Mitchell GL, Jones-Jordan LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker JD, Zadnik K. Relative peripheral refractive error and the risk of onset and progression of myopia in children. CLEERE Study Group. Invest Ophthalmol Vis Sci. 2011;52:199–205. doi: 10.1167/iovs.09-4826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seidemann A, Schaeffel F, Guirao A, López-Gil N, Artal P. Peripheral refractive errors in myopic, emmetropic, and hyperopic young subjects. J Opt Soc Am (A) 2002;19:2363–2373. doi: 10.1364/josaa.19.002363. [DOI] [PubMed] [Google Scholar]
- 27.Calver R, Radhakrishnan H, Osuobeni E, O'Leary D. Peripheral refraction for distance and near vision in emmetropes and myopes. Ophthalmic Physiol Opt. 2007;27:584–593. doi: 10.1111/j.1475-1313.2007.00518.x. [DOI] [PubMed] [Google Scholar]
- 28.Liu Y, Wildsoet C. The effect of two-zone concentric bifocal spectacle lenses on refractive error development and eye growth in young chicks. Invest Ophthalmol Vis Sci. 2011;52:1078–1086. doi: 10.1167/iovs.10-5716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berntsen DA, Barr JT, Mitchell GL. Higher-order aberration changes after corneal refractive therapy (CRT) Invest Ophthalmol Vis Sci. 2004;45 E-Abstract 1543. [Google Scholar]
- 30.Charman WN, Mountford J, Atchison DA, Markwell EL. Peripheral refraction in orthokeratology patients. Optom Vis Sci. 2006;83:641–648. doi: 10.1097/01.opx.0000232840.66716.af. [DOI] [PubMed] [Google Scholar]
- 31.Queirós A, González-Méijome JM, Jorge J, Villa-Collar C, Gutiérrez AR. Peripheral refraction in myopic patients after orthokeratology. Optom Vis Sci. 2010;87:323–329. doi: 10.1097/OPX.0b013e3181d951f7. [DOI] [PubMed] [Google Scholar]
- 32.Kang P, Swarbrick H. Peripheral refraction in myopic children wearing orthokeratology and gas-permeable lenses. Optom Vis Sci. 2011;88:476–482. doi: 10.1097/OPX.0b013e31820f16fb. [DOI] [PubMed] [Google Scholar]
- 33.Aller TA, Wildsoet C. Bifocal soft contact lenses as a possible myopia control treatment: a case report involving identical twins. Clin Exp Optom. 2008;91:394–399. doi: 10.1111/j.1444-0938.2007.00230.x. [DOI] [PubMed] [Google Scholar]
- 34.Aller TA. Controlling myopia progression - why not try something that works for a change?: Symposium #6, abstract #3. In: McBrien NA, Young TL, Pang CP, Hammond C, Baird P, Saw SM, Morgan IG, Mutti DO, Rose KA, Wallman J, Gentle A, Wildsoet CF, Gwiazda J, Schmid KL, Smith E, 3rd, Troilo D, Summers-Rada J, Norton TT, Schaeffel F, Megaw P, Beuerman RW, McFadden S, eds. Myopia: recent advances in molecular studies; prevalence, progression and risk factors; emmetropization; therapies; optical links; peripheral refraction; sclera and ocular growth; signalling cascades; and animal models. Optom Vis Sci. 2009;86:55. [Google Scholar]
- 35.Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118:1152–1161. doi: 10.1016/j.ophtha.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 36.Ehsaei A, Mallen EA, Chisholm CM, Pacey IE. Cross-sectional sample of peripheral refraction in four meridians in myopes and emmetropes. Invest Ophthalmol Vis Sci. 2011;52:7574–7585. doi: 10.1167/iovs.11-7635. [DOI] [PubMed] [Google Scholar]
- 37.Walline JJ, Jones-Jordan LA, Greiner KL, McVey M. The effects of soft bifocal contact lenses on myopia progression in children. Optom Vis Sci. 2011;88 doi: 10.1097/OPX.0000000000001884. E-Abstract 110642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheung SW, Cho P, Chui WS, Woo GC. Refractive error and visual acuity changes in orthokeratology patients. Optom Vis Sci. 2007;84:410–416. doi: 10.1097/OPX.0b013e31804f5acc. [DOI] [PubMed] [Google Scholar]
- 39.Hiraoka T, Okamoto C, Ishii Y, Kakita T, Okamoto F, Takahashi H, Oshika T. Patient satisfaction and clinical outcomes after overnight orthokeratology. Optom Vis Sci. 2009;86:875–882. doi: 10.1097/OPX.0b013e3181ae34d5. [DOI] [PubMed] [Google Scholar]
- 40.Reim TR, Lund M, Wu R. Orthokeratology and adolescent myopia control. Contact Lens Spectrum. 2003;18(3):40–42. [Google Scholar]
- 41.Wolffsohn JS, Hunt OA, Basra AK. Simplified recording of soft contact lens fit. Cont Lens Anterior Eye. 2009;32:37–42. doi: 10.1016/j.clae.2008.12.004. [DOI] [PubMed] [Google Scholar]