Abstract
HYPOTHESIS
We hypothesize that among patients with lung cancers the KRAS/EGFR mutation profile and overall survival of “collegiate smokers” (former smokers who smoked between 101 lifetime cigarettes and 5 pack years) are distinct from those of never smokers and former smokers with ≥ 15 pack years.
METHODS
We collected age, sex, stage, survival, and smoking history for patients evaluated from 2004 to 2009 with advanced stage lung cancers and known KRAS/EGFR status. Mutation profile and overall survival were compared using Fisher’s exact test and log-rank test, respectively.
RESULTS
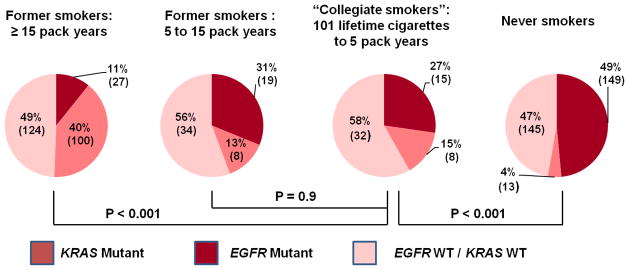
Data were available for 852 patients with advanced stage lung cancers with known KRAS/EGFR status. 6% were “collegiate smokers”, 36% were never smokers, and 30% were former smokers with ≥ 15 pack years. The mutation profile of “collegiate smokers” (15% KRAS mutations, 27% EGFR mutations) was distinct from those of never smokers (p < .001) and former smokers with ≥ 15 pack years (p < .001)and not significantly different from those of former smokers with 5 to 15 pack years (p = 0.9). Median overall survival for “collegiate smokers” was 25 months, compared to 32 months for never smokers (p = 0.4), 33 months for former smokers with 5–15 pack years (p = 0.48),and 21 months for former smokers with ≥ 15 pack years (p = 0.63).
CONCLUSIONS
“Collegiate smokers” with advanced stage lung cancers represent a distinct subgroup of patients with a higher frequency of KRAS mutations and lower frequency of EGFR mutations compared to never smokers. These observations reinforce the recommendation for routine mutation testing for all patients with lung cancers and that no degree of tobacco exposure is safe.
Keywords: Collegiate Smokers, non-small cell lung cancers, epidermal growth factor receptor mutation, KRAS mutation
INTRODUCTION
The discovery of driver lesions in epidermal growth factor receptor (EGFR), KRAS, and anaplastic lymphoma kinase (ALK) has led to the identification of distinct genetic sub-types of lung cancers. This information is revolutionizing the treatment of lung cancer. We have demonstrated that the frequency of KRAS mutations increases and EGFR mutation decreases with greater tobacco exposure, and EGFR mutations are less common in patients who smoked greater than 15 pack years.1, 2 These EGFR mutations predict sensitivity to EGFR tyrosine kinase inhibitors.3–5 By contrast, lung cancers harboring KRAS mutations are found in patients with a variety of tobacco exposures ranging from never smokers to heavy smokers, while patients whose tumors harbor ALK rearrangements are more likely never or light smokers compared to those patients whose tumors do not harbor ALK rearrangements.6, 7
For patients with advanced lung cancers, we have shown that cigarette smoking is associated with worse survival after a diagnosis.8 We have also demonstrated that patients with advanced lung cancers harboring KRAS mutations have a shorter survival compared to those of patients with tumors harboring EGFR mutations and patients whose tumors are wild-type for KRAS and EGFR.9
Whether the tobacco exposure of “collegiate smokers”, individuals who are former smokers with a lifetime exposure between 101 cigarettes and 5 pack years, is sufficient to impact their prognosis is unknown. We hypothesize that the KRAS and EGFR mutation profile and overall survival of “collegiate smokers” will be distinct from never smokers and former smokers with ≥ 15 pack year smoking histories. The ≥ 15 pack year number was chosen as we had previously determined that that EGFR mutation frequency above that amount of cigarette exposure was significantly different than the frequency seen in never smokers. 1
MATERIALS AND METHODS
This cohort includes patients evaluated at Memorial Sloan-Kettering Cancer Center between 2004 and 2009 with known KRAS and EGFR status and advanced stage lung cancers (stage IIIB/IV by the American Joint Committee on Cancer Staging Manual, sixth edition) at the time of initial diagnosis or at the time of recurrent disease after prior surgery or radiation. Patients with squamous and small cell lung cancers did not undergo EGFR/KRAS analysis. Patients with lung cancers evaluated at MSKCC complete a prospective, self-administered smoking questionnaire at the time of their initial visit. The history of smoking, number of pack years smoked, and years since stopping smoking were determined using the smoking questionnaire. We obtained demographic and clinical information regarding gender, race, age, stage, and survival. EGFR exon 19 deletions and EGFR exon 21 L858R amino acid substitutions were identified by previously reported mutation-specific PCR-based methods.10–12 KRAS codon 12 and 13 mutation identification was performed by both mass-spectrometry (Sequenom)-based genotyping and direct sequencing. ALK testing was not available for patients prior to 2009 and was not evaluated in this cohort. Medical record review was performed with a waiver of authorization approved by our Institutional Review Board. Mutation profile was compared across groups using the Fisher’s exact test. Overall survival following diagnosis with advanced stage lung cancer was estimated using Kaplan-Meier method and compared across groups using the log-rank test. Patients alive at the end of the study were censored at the time of the last available follow-up.
Patients were categorized as never smokers if they had smoked 100 or fewer lifetime cigarettes, current smokers if they continue to smoke or quit less than 12 months prior to completion of the smoking questionnaire, and former smokers if they quit smoking at least 12 months prior to completion of the smoking questionnaire. Race was reported by the patient.
RESULTS
Detailed smoking history and clinical data were available for 852 patients with advanced stage lung cancers (492women, 360 men).97% of this patient population had adenocarcinoma, and the remaining 3% included patients with non-small cell lung cancer not otherwise specified and large cell neuroendocrine carcinoma. Demographic characteristics are summarized in Table 1. “Collegiate smokers” had stopped smoking a median of 30 years prior to diagnosis (range 1 to 60 years).
Table 1.
Patient Characteristics
| N | % | |
|---|---|---|
| Men | 360 | 42 |
| Women | 492 | 58 |
| Median Age (range), years | 64 (26–92) | |
| Smoking History | ||
| Never Smoker | 307 | 36 |
| “Collegiate” Smoker | 55 | 6 |
| Former Smoker with 5 to 15 pack years | 61 | 7 |
| Former Smoker with ≥15 pack years | 251 | 30 |
| Current Smoker | 178 | 21 |
| Race | ||
| White | 710 | 83 |
| Asian | 67 | 8 |
| Unknown/Other | 75 | 9 |
Mutation profiles are depicted in Figure 1.The mutation profile of “collegiate smokers” is different from those patients who had never smoked (p <.001) and of former smokers who had smoked ≥ 15 pack years (p < .001) but similar to that of patients who were former smokers with 5–15 pack years (p = 0.9). Among former smokers with smoking histories ≥ 15 pack years, 40% had KRAS mutations, 11% had EGFR mutations, and 49% were wild type for KRAS and EGFR mutations.
Figure 1.
Mutation Profile for Never Smokers, Collegiate Smokers, and Former Smokers with ≥ 15 pack year smoking histories
Median overall survival after diagnosis of advanced stage lung cancer for “collegiate smokers” was 25 months, compared to 32 months for never smokers (p = 0.4), 21 months for former smokers with ≥ 15 pack years (p = 0.63), and 33 months for former smokers with 5–15 pack years (p = 0.48).
DISCUSSION
Many persons with lung cancers state that they “only smoked in college” or for just a few years when they were younger. Since we prospectively collect smoking questionnaires for all patients with advanced stage lung cancers, we were in a position to assess whether the mutational profile and course of lung cancer were different from individuals who never smoked or had greater exposures to cigarette smoking. We defined “collegiate smokers” as former smokers who have smoked between 101 lifetime cigarettes and 5 pack years. Based on this data, “collegiate smokers” with advanced stage lung cancers represent a distinct group of patients with a higher percentage of KRAS mutations and lower percentage of EGFR mutations as compared to never smokers. The median overall survival of “collegiate smokers” was not significantly different from never smokers, former smokers with 5–15 pack years, and former smokers with ≥ 15 pack years but not significantly different in this relatively small cohort.
Heavier cigarette smoking history is associated with decreased survival after a diagnosis of advanced stage lung cancer.8 Likewise, recent work has demonstrated that any amount of smoking exposure greater than 1 pack year can impact the likelihood of EGFR and KRAS mutations among patients with lung cancers.2 Although the majority of gene expression alterations associated with smoking return to the levels associated with never smokers, expression of a subset of genes remains affected, even decades after smoking cessation.13 Building on this work, these data serve as a reminder that the effects of even minimal amounts of cigarette smoking decades earlier influence the biology and perhaps the outcome of lung cancers. Additionally, many clinicians continue to choose EGFR-targeted therapy based on clinical history, including never or “collegiate” smoking history. These data reinforce the necessity of performing routine molecular testing on all patients with lung cancers. Lastly, this data remind us that no amount of cigarette smoking is safe.
References
- 1.Pham D, Kris MG, Riely GJ, et al. Use of cigarette-smoking history to estimate the likelihood of mutations in epidermal growth factor receptor gene exons 19 and 21 in lung adenocarcinomas. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2006;24:1700–1704. doi: 10.1200/JCO.2005.04.3224. [DOI] [PubMed] [Google Scholar]
- 2.Dogan S, Shen R, Ang DC, et al. Molecular Epidemiology of EGFR and KRAS Mutations in 3026 Lung Adenocarcinomas: Higher Susceptibility of Women to Smoking-related KRAS-mutant Cancers. Clinical cancer research : an official journal of the American Association for Cancer Research. 2012 doi: 10.1158/1078-0432.CCR-11-3265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pao W, Miller V, Zakowski M, et al. EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib anderlotinib. Proceedings of the National Academy of Sciences of the United States of America. 2004;101:13306–13311. doi: 10.1073/pnas.0405220101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paez JG, Janne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 5.Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. The New England journal of medicine. 2004;350:2129–2139. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 6.Riely GJ, Kris MG, Rosenbaum D, et al. Frequency and distinctive spectrum of KRAS mutations in never smokers with lung adenocarcinoma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2008;14:5731–5734. doi: 10.1158/1078-0432.CCR-08-0646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaw AT, Yeap BY, Mino-Kenudson M, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2009;27:4247–4253. doi: 10.1200/JCO.2009.22.6993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janjigian YY, McDonnell K, Kris MG, et al. Pack-years of cigarette smoking as a prognostic factor in patients with stage IIIB/IV nonsmall cell lung cancer. Cancer. 2010;116:670–675. doi: 10.1002/cncr.24813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson ML, Sima CS, Chaft J, et al. Association of KRAS and EGFR mutations with survival in patients with advanced lung adenocarcinomas. Cancer. 2012 Jul 18; doi: 10.1002/cncr.27730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan Q, Pao W, Ladanyi M. Rapid polymerase chain reaction-based detection of epidermal growth factor receptor gene mutations in lung adenocarcinomas. The Journal of molecular diagnostics : JMD. 2005;7:396–403. doi: 10.1016/S1525-1578(10)60569-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pao W, Miller VA, Politi KA, et al. Acquired resistance of lung adenocarcinomas to gefitinib or erlotinib is associated with a second mutation in the EGFR kinase domain. PLoS medicine. 2005;2:e73. doi: 10.1371/journal.pmed.0020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li AR, Chitale D, Riely GJ, et al. EGFR mutations in lung adenocarcinomas: clinical testing experience and relationship to EGFR gene copy number and immunohistochemical expression. The Journal of molecular diagnostics : JMD. 2008;10:242–248. doi: 10.2353/jmoldx.2008.070178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bosse Y, Postma DS, Sin DD, et al. Molecular Signature of Smoking in Human Lung Tissues. Cancer research. 2012;72:3753–3763. doi: 10.1158/0008-5472.CAN-12-1160. [DOI] [PubMed] [Google Scholar]