Abstract
Background
Scapular notching is a common worrying finding after reverse total shoulder arthroplasty (RSA). Eccentric glenospheres have recently been developed in an attempt to prevent notching. The purpose of this study was to evaluate the clinical and radiological results of RSA with an eccentric glenosphere and compare the incidence and the severity of scapular notching using a concentric glenosphere.
Methods
A prospective evaluation was performed of 57 consecutive RSA performed over a two-year period. At a minimum of two years postoperatively, 47 RSAs with a mean 30.4 months follow-up were evaluated clinically and radiographically and compared to a historical control group of concentric glenospheres performed by the same surgeon.
Results
The mean Constant score significantly increased (from 32.4 to 71.8) postoperatively (p < 0.0001). Active forward flexion and external rotation also significantly increased (p < 0.0001). Overall, scapular notching was present in 19 shoulders (40.4 %). Grade 1 notching was observed in 13 shoulders (27.7 %), grade 2 in five shoulders (10.6 %), grade 3 in one shoulder (2.1 %), and grade 4 in no shoulders. There was no significant difference in the incidence (p = 0.289) of notching between the eccentric and concentric glenospheres. However, the severity of notching was significantly decreased (p = 0.011) with an eccentric glenosphere. The postoperative Constant score was not significantly different between patients with or without notching (p = 0.651).
Conclusion
A Grammont type RSA with eccentric glenosphere can result in good clinical outcomes. An eccentric glenosphere does not prevent notching, but decreases the severity of scapular notching at early follow-up.
Introduction
Scapular notching is the most common worrying radiographic finding observed after reverse total shoulder arthroplasty (RSA). The incidence ranges from 44 % to 96 % and increases both in severity and frequency at longer-term follow-up [3, 7, 13, 15, 19–22]. In this phenomenon, bony erosion of the inferior scapular neck is caused by mechanical impingement between the scapula and the humeral polyethylene insert during adduction and rotation of the arm [20]. Furthermore, polyethylene wear debris leads to an osteolytic reaction which contributes to progression of scapular notching [17]. Extensive scapular notching affects functional outcome [2] and may lead to glenoid loosening.
Several implant factors have been implicated in the development of scapular notching including the amount of glenosphere offset, inclination of the humeral component, and cranial-caudal positioning [10, 13, 17, 19, 20]. Cranial-caudal positioning of the glenosphere is appealing in particular because it can be altered without affecting the centre of rotation of the implant. In vitro investigation has determined that inferior positioning of the glenosphere was more important that tilt in limiting mechanical impingement between the humerus and scapula [16].
Maximising the concept of inferior positioning, eccentric glenospheres have recently been developed in order to potentially prevent notching. The purpose of this study was to evaluate the clinical and radiological results of RSA with an eccentric glenosphere and compare the incidence and the severity of scapular notching with a concentric glenosphere. The study hypothesis was that an eccentric glenosphere would reduce the incidence and severity of scapular notching compared to a concentric glenosphere.
Materials and methods
Study group
This was a prospective review of all RSAs performed between November 2006 and November 2008 at a single institution. Prior to initiation, the study protocol was approved by the Hospital Ethics Committee. The inclusion criteria were an eccentric glenosphere component and minimum follow-up of 24 months with complete functional outcome and radiographic data. The only exclusion criterion was the use of a concentric glenosphere component.
Operative technique
The senior author performed all operations. The same Grammont-type [9] RSA implant was used in all cases (Aequalis Reversed II; Tornier, Edina, MN). During the study period an eccentric glenosphere was placed in all cases possible. The situation in which this could not be performed was in those cases which required bone grafting for extensive glenoid erosion. A deltopectoral approach was used, 2 cm of the pectoralis major tendon was released, and the subscapularis tendon (if intact) was tenotomised at the level of anatomical neck. The humeral head was cut with 0 to 20 degree retroversion following natural retroversion. The inferior aspect of the glenoid was clearly exposed and the glenoid base plate was placed as inferiorly as possible. The glenoid base plate was placed in approximately 10 degrees of inferior tilt. The number of screws used for fixation, either three screws (four shoulders) or four screws (43 shoulders), was dictated by the available glenoid bone stock and the surgeon’s preference. An eccentric glenosphere was then fixed to the base plate. The eccentric glenosphere provided by the manufacturer (Tornier, Edina, MN) provides 2 mm of inferior offset in order to generate glenoid overhang (Figs. 1, 2 and 3). A 36-mm diameter glenosphere was inserted in 39 shoulders, and a 42-mm diameter glenosphere was inserted in four shoulders. The choice between 36-mm and 42-mm glenosphere not randomised, but based on the surgeon’s preference. The humeral component was then placed in the standard fashion. In all cases an attempt was made to repair the subscapularis tendon via transosseous sutures. A soft tissue biceps tenodesis was also systematically performed when the tendon was still present.
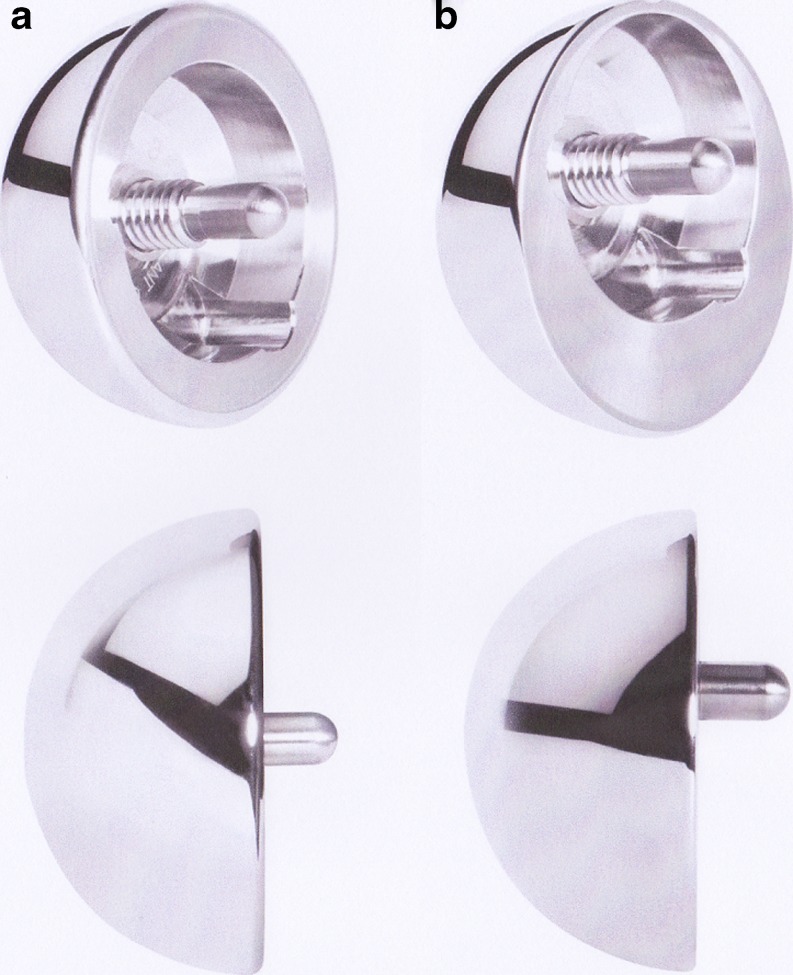
Fig. 1.
a A standard glenosphere is centred at its attachment to a metaglene. b In an eccentric glenosphere the attachment to the metaglene is offset such that the glenosphere position can be altered without changing the position of the metaglene
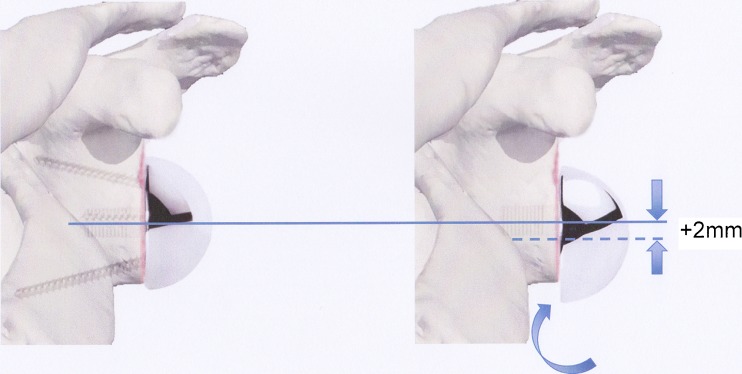
Fig. 2.
In a standard glenosphere (left) the inferior aspect of the glenosphere is frequently flush with the lower border of the scapular neck. With an eccentric design (right) the glenosphere can be shifted inferiorly without changing the position of the metaglene base plate. Note: The position of the metaglene remains the same (solid blue line), but the centre of the glenosphere has been shifted inferiorly 2 mm (dashed blue line). The inferior overhang of the glenosphere provides a space between the glenosphere and the scapular neck (curved blue arrow), which may decrease notching
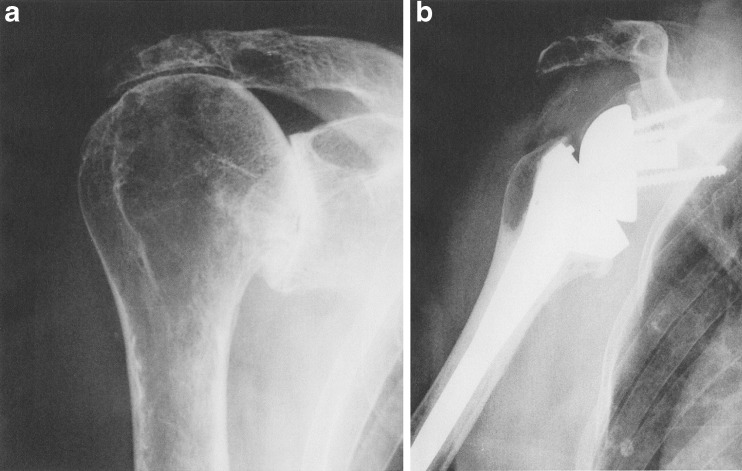
Fig. 3.
Preoperative (a) and postoperative (b) radiographs of an individual with rotator cuff arthropathy managed with a reverse total shoulder arthroplasty using an eccentric glenosphere
Postoperative rehabilitation
Postoperatively, the shoulder was immobilised with a simple sling that held the arm in internal rotation for four weeks. During this period, the sling was removed for hygiene and the patient was allowed to use the hand on the involved side for simple activities of daily living. No lifting was allowed. Passive range of motion was initiated immediately. After four weeks the sling was discontinued and activity was allowed as tolerated.
Clinical and radiographic evaluation
A standardised clinical assessment was performed preoperatively and then postoperatively at six weeks, three months, six months, one year, and annually thereafter. At each time point an independent observer assessed active range of motion (including forward flexion, external rotation with the arm at the side, and internal rotation behind the back) and a Constant score was obtained [5].
Radiographs taken at each time point included anterior-posterior (AP) views of the glenohumeral joint in neutral rotation, internal rotation, and external rotation, a supraspinatus outlet view, and an axillary lateral view. All radiographs were obtained under fluoroscopic control using Lévigne’s protocol [13]. Scapular notching was graded according to the Sirveaux classification [20]: grade 1 for a notch limited to the scapular pillar, grade 2 for a notch reaching the inferior screw of the base plate, grade 3 for a notch extending beyond the inferior screw, and grade 4 for a notch reaching the base-plate’s central peg. For purposes of analysis notching was categorised as “not severe” (grade 1 or 2) and “severe” (grade 3 or 4) [14].
Osteophytes of inferior scapular neck were recorded on the AP view. Glenoid and humeral component loosening (radiolucent lines greater than 1 mm) were also evaluated [18]. Progression of scapular notching was defined as greater than or equal to a 1 grade increase in notching after initial observation of notching.
Statistical analysis
Preoperative and postoperative Constant score and range of motion were compared with the Student’s t-test. In order to identify the clinical relevance of notching, preoperative characteristics of patients with and without notching were evaluated using the Wilcoxon test and Pearson's chi-squared test. The incidence and the severity of scapular notching were compared with a previous published series using Pearson's chi-squared test values estimated by Monte-Carlo simulation. This previous series consisted of 152 cases of RSA with centric glenosphere by the same surgeon between May 1995 and June 2003 [21]. All statistical analysis was performed by a trained statistician using StatView (SAS Institute, Cary, NC, USA). The level of significance was set at p ≤ 0.05.
Results
Sixty-three RSAs were performed during the study period. In six cases a concentric glenosphere with glenoid bone graft was used for treatment of severe glenoid erosion. An eccentric glenosphere was used in the remaining 57 shoulders. Five patients died prior to the minimum 24-months follow-up and five patients had incomplete data, leaving a total of 47 shoulders in 46 patients available for study. The average age at the time of surgery was 74.4 years (50–84 years). There were 32 women (33 shoulders) and 14 men (14 shoulders). The aetiology was rotator cuff tear arthropathy in 21 shoulders (44.7 %), revision arthroplasty in eight shoulders (17 %), irreparable massive rotator cuff tear in six shoulders (12.8 %), primary arthritis with biconcave glenoid or advanced fatty degeneration of rotator cuff in seven shoulders (14.9 %), post traumatic osteoarthritis in three shoulders (6.4 %), and rheumatoid arthritis in two shoulders (4.3 %). Thirty-one shoulder operations involved the dominant extremity. The mean body mass index at the time of surgery was 25.1 (range 17.3–33.3). The mean follow-up period was 30 months (range 24–49 months).
The mean Constant score increased from 32.4 preoperatively to 71.8 points postoperatively (p < 0.0001). Compared to preoperative values, postoperatively there were statistically significant improvements in active forward flexion and external rotation. On the other hand, active internal rotation increased from preoperative to postoperative values but the difference did not reach statistical significance (Table 1).
Table 1.
Functional outcome
| Parameter | Preoperative | Postoperative | P value |
|---|---|---|---|
| Constant score | |||
| Pain | 4.0 | 12.8 | P < 0.0001 |
| Activity | 7.6 | 17.4 | P < 0.0001 |
| Mobility | 16.3 | 32.6 | P < 0.0001 |
| Strength | 4.5 | 8.8 | P < 0.0001 |
| Total | 32.4 | 71.8 | P < 0.0001 |
| Range of motion | |||
| Elevation | 89.4° | 146.6° | P < 0.0001 |
| External rotation | 12.6° | 28.9° | P < 0.0001 |
| Internal rotation | Buttocks | L1 | Not significant |
Scapular notching was present in 19 shoulders (40.4 %). The notching was grade 1 in 13 shoulders (27.7 %), grade 2 in five shoulders (10.6 %), and grade 3 in one shoulder (2.1 %). There were no instances of grade 4 notching (Table 2). All notches were seen on the AP view and 12 notches were also identified on axial view (Fig. 2). Progression of notching over time was identified in five shoulders (10.6 %) and occurred at a mean of 23 months.
Table 2.
Scapular notching with an eccentric compared to a concentric glenosphere
| Grade | Eccentric glenosphere, n = 47 | Concentric glenosphere, n = 152 |
|---|---|---|
| 0 | 28 (59.6 %) | 127 (38 %) |
| 1 | 13 (27.7 %) | 75 (22.3 %) |
| 2 | 5 (10.6 %) | 62 (18.4 %) |
| 3 | 1 (2.1 %) | 47 (13.9 %) |
| 4 | 0 | 26 (7.7 %) |
There was no significant difference in the incidence of scapula notching between the eccentric glenospheres in the current cohort and the concentric glenospheres in the historical control group (p = 0.289). On the other hand, the severity of notching was significantly lower in the eccentric cohort than in the concentric group (p = 0.011).
Osteophytes of inferior scapular neck were identified in five shoulders (10.6 %): four shoulders with notching and one shoulder without notching. No radiolucent lines were observed around the humeral implant or around the central peg or screws of the glenoid component.
There was no difference in preoperative factors or final functional outcome among patients with or without notching (Table 3). At final follow-up, the mean forward flexion was 150.0° in the shoulders with notching, compared to 144.2° in those without notching (p = 0.4041). The mean active external rotation was 28.9° in the shoulders with notching and 28.9° in those without notching (p = 0.4862, respectively).
Table 3.
Scapular notching and patient factors
| Parameter | Notching, n = 19 | No notching, n = 28 | P value |
|---|---|---|---|
| Aetiologies | |||
| Primary osteoarthritis | 4 | 3 | n.s |
| Massive rotator cuff tear | 2 | 4 | n.s |
| Cuff tear arthropathy | 8 | 13 | n.s |
| Post traumatic arthritis | 0 | 3 | n.s |
| Rheumatoid arthritis | 2 | 0 | n.s |
| Revision arthroplasty | 3 | 5 | n.s |
| Age (y) | 74.6 | 74.2 | n.s |
| Male: female | 7:12 | 7:21 | n.s |
| Follow-up period (months) | 31 | 29.1 | n.s |
| BMI | 25.5 | 24.7 | n.s |
| Postoperative Constant score | 72.2 | 71.6 | n.s |
BMI body mass index, n.s not significant
Complications
An axillary nerve palsy occurred in two patients (4.3 %) and a transient brachial plexus palsy occurred in one patient (2.1 %). The first axillary nerve palsy was a transient palsy in a 78-year-old woman with advanced cuff tear arthropathy (superior migration, acetabularisation, and glenohumeral arthritis). Her palsy completely recovered five months after surgery. The other axillary nerve palsy was a permanent palsy that occurred during revision of an unconstrained total shoulder arthroplasty in a 76-year-old woman. The brachial plexus nerve palsy occurred in a 75-year-old woman with a previous hemiarthroplasty and preoperative glenoid erosion. Her function fully returned within eight months following surgery. No other intraoperative or postoperative complications were observed. No patient required revision surgery.
Discussion
The purpose of this study was to evaluate the radiographic and functional outcome of a consecutive series of RSAs performed with an eccentric glenosphere. Several implant modifications have been suggested to limit scapular notching. Frankle et al. proposed lateralisation of the centre of rotation with metallic offset [8]. At short-term follow-up of 33 months, they reported a 0 % incidence of notching. However, this approach creates more torque on the glenoid component and may increase the risk of glenoid loosening, particularly in osteoporotic bone [2]. Increasing the inclination (neck-shaft angle) of the humeral component to a more vertical orientation decreases impingement in biomechanical investigations but may create a conflict superiorly and alter prosthetic instability in early abduction [2, 9, 11]. Altering the position of the glenosphere through an eccentric implant is appealing because it may be accomplished without the negatives of the aforementioned alternatives.
A few biomechanical investigations have evaluated the impact of an eccentric glenosphere [4, 6, 16]. Nyffeler et al. reported that lowering the position of baseplate to the inferior border of the glenoid significantly improved adduction and abduction angles and might reduce the risk of inferior glenoid notching [16]. In this study a 25-degree adduction deficit with an uncovered inferior glenoid was reduced to one degree when the glenosphere was placed in a position overhanging the inferior glenoid. Notably, an inferior glenosphere position was more beneficial than inferior tilt in producing impingement-free range of motion. Similarly, Chou et al. reported that an eccentric glenosphere reduced the adduction deficit by 14.5 degrees with a 36-mm glenosphere and 17.5 degrees with a 44-mm glenosphere [4]. There was no statistically significant difference in total range of motion between the 36-mm and 44-mm eccentric glenospheres, showing that the major advantage between these two variables is eccentricity of the glenosphere. Furthermore, in clinical practice glenosphere size is dictated by patient size, whereas an eccentric glenosphere can be placed regardless of size.
Our study evaluated the clinical impact of these biomechanical findings in a prospective analysis of RSA performed with an eccentric glenosphere. Similar to previous studies [3, 13, 15, 19–22], in our study there were significant improvements in Constant score and range of motion following a RSA. Importantly, at a mean follow-up of 30 months there were no severe complications such as glenoid loosening, dislocation, or infection. Initially, we were concerned that shifting the centre of rotation inferiorly with an eccentric glenoid would increase shear forces on the glenoid. Gutierrez et al. recently reported a computer model study of an eccentric glenosphere in which an inferior eccentric glenosphere (6-mm inferior offset) with inferior tilt provided the most uneven distribution of forces and might be detrimental [11]. The inferior offset in this model was three times greater than the offset clinically applied in our study. Based on our study, it appears that a 2-mm eccentric glenoid is safe at short-term follow-up. Longer follow-up, however, is necessary to verify this conclusion.
The incidence of scapular notching ranges from 44 % to 96 % with an increasing size and incidence in the longer-term follow-up with RSA of conventional medialised design [3, 7, 13, 15, 19–22]. Sirveaux et al. found inferior scapular notch in 50 of 77 patients (65 %) at a mean follow-up of 44.5 months [20]. Lévigne et al. noted the presence of scapular notching in 62 % of 337 shoulders at an average follow-up of 47 months and found that the frequency and extension of notching was correlated with the length of follow-up [13]. Werner et al. found notching in 98 % of 48 cases, but noted that in 79 % the notch did not progress beyond one year of follow-up [22]. In our study, scapular notching was observed in 19 of 47 shoulders (40.4 %). Compared to a historical control group of concentric RSAs implanted using the same surgical technique, the incidence of notching was not changed (p = 0.289). However, perhaps more important than the incidence of notching, is the severity of notching. Previous studies have reported an incidence of severe notching of 18 % to 45.6 % (Table 4) [3, 7, 13, 15, 19–22]. In our study, 94.7 % of the notching observed was only grade 1 or 2 in severity. Severe notching decreased from 37 % with a concentric glenosphere to 5.3 % with an eccentric glenosphere. Such a reduction may be important given the relationship between severe notching and functional outcome observed over a longer follow-up [20].
Table 4.
Comparison of scapular notching reported using Grammont-type reverse total shoulder arthroplasties
| Parameter | Sirveaux et al. [20] | Boileau et al. [3] | Werner et al. [22] | Simovitch et al. [19] | Nolan et al. [15] | Lévigne et al. [13] | Wall et al. [21] | Mizuno et al. (our study) |
|---|---|---|---|---|---|---|---|---|
| N | 80 | 45 | 48 | 77 | 71 | 337 | 152 | 47 |
| Follow-up (months) | 44 | 40 | 48 | 44 | 24 | 47 | 40 | 30 |
| Notching | 64 % | 68 % | 96 % | 44 % | 49 % | 62 % | 51 % | 40 % |
| No notching | 36 % | 32 % | 4 % | 56 % | 51 % | 38 % | 49 % | 60 % |
| Grades 1 & 2 | 74 % | 82 % | 54 % | 59 % | 74 % | 66 % | 63 % | 95 % |
| Grades 3 & 4 | 26 % | 18 % | 46 % | 41 % | 26 % | 34 % | 37 % | 5 % |
Despite the improvement in severity of notching, it is clear that with a conventional medialised RSA design there is a limitation to prevention of notching with an eccentric glenosphere. Ultimately, increasing lateral offset with bone may be the next step to prevent notching. Frankle et al. used a metallic lateralised RSA design and did not report any notching [8]. However, they had several complications caused by glenoid loosening, suggesting that metallic lateralisation has a risk of glenoid loosening because of increased torque on the glenoid. Kempton et al. reported on a combination of a metallic lateralised RSA and a reduced humeral neck shaft angle [12]. They found that six of 37 shoulders (16 %) had grade 1–2 notching and no grade 3–4 notching at a mean follow-up of 16 months. While these results are encouraging, there is still concern for long-term glenoid loosening and failure from the increased torque with these designs.
In order to reduce the torque on the glenoid, Boileau et al. developed the bony increased-offset reverse shoulder arthroplasty (BIO-RSA) [1]. In this modification a humeral head autograft is used to increase lateral offset. This approach to increasing offset maintains a more medialised centre of rotation (with consequent lower shear forces) compared to the approach of increasing through the implant itself. In this series the incidence of notching was eight of 42 shoulders (19 %) at mean follow-up of 28 months. Additionally, the authors noted greater improvements in rotation and cosmesis as a result of the modification. Considering the advantages of a BIO-RSA, a traditional RSA with an eccentric glenosphere may be a viable option for patients in whom a humeral head autograft cannot be harvested due to poor bone quality or revision arthroplasty.
The majority of previous studies have not found any relationship between scapular notching and functional outcome [3, 13, 15, 19, 21, 22]. Only Sirveaux et al. reported that scapular notching can affect the Constant score when they are severe [20]. In our study, no significant difference in postoperative Constant score was observed between patients with or without scapular notching. Additionally, no significant difference was seen in postoperative active range of motion between the patients with or without notching. However, these findings are limited by the relatively short follow-up of this cohort.
This study has several limitations. First, the follow-up term is relatively short. The patients in this cohort will be closely followed in an effort to gain more information regarding the long-term survivorship of this eccentric glenosphere. Second, we did not perform radiographic evaluation with computed tomography scans. However, fluoroscopic control was used to obtain the radiographs so we believe that notching was adequately visualised. Third, we had no control series with concentric glenosphere. The study design used historical controls rather than a randomised comparison and the size of glenosphere was based on surgeon preference. However, because the surgical technique did not change between the historical control group and our study we believe the design adequately represents the improvement with an eccentric design.
Conclusion
At early term follow-up an eccentric glenosphere decreases the severity of scapular notching with a Grammont type RSA without adverse glenoid complications. This design modification may be one of the additional solutions to avoid scapular notching.
Footnotes
Level of evidence: IV, case-control study
Contributor Information
Naoko Mizuno, Email: nao-miz@hcc5.bai.ne.jp.
Gilles Walch, Phone: +33-4-37530024, FAX: +33-4-37530025, Email: walch.gilles@wanadoo.fr.
References
- 1.Boileau P, Moineau G, Roussanne Y, O’Shea K. Bony increased-offset reversed shoulder arthroplasty. Minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res. 2011;469:2558–2567. doi: 10.1007/s11999-011-1775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14(1 Suppl):147S–161S. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: the Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527–540. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Chou J, Malak SF, Anderson IA, Astley T, Poon PC. Biomechanical evaluation of different designs of glenospheres in the SMR reverse total shoulder prosthesis: Range of motion and risk of scapular notching. J Shoulder Elbow Surg. 2009;18:354–359. doi: 10.1016/j.jse.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 5.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 6.Dedy NJ, Stangenberg M, Liem D, Hurschler C, Simmen B, Riner M, Marquardt B, Steinbeck J. Effect of posterior offset humeral components on range of motion in reverse shoulder arthroplasty. Int Orthop. 2011;35:549–554. doi: 10.1007/s00264-010-1079-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farshad M, Gerber C. Reverse total shoulder arthroplasty-from the most to the least common complication. Int Orthop. 2010;34:1075–1082. doi: 10.1007/s00264-010-1125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frankle M, Levy JC, Pupello D, Siegal S, Saleem A, Mighell M, Vasey M. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency: a minimum two-year follow-up study of sixty patients: surgical technique. J Bone Joint Surg Am. 2005;87:1697–1705. doi: 10.2106/JBJS.D.02813. [DOI] [PubMed] [Google Scholar]
- 9.Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–68. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- 10.Gutierrez S, Levy JC, Frankle MA, Cuff D, Keller TS, Pupello DR, Lee WE., 3rd Evaluation of abduction range of motion and avoidance of inferior scapular impingement in a reverse shoulder model. J Shoulder Elbow Surg. 2008;17:608–615. doi: 10.1016/j.jse.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Gutierrez S, Walker M, Willis M, Pupello DR, Frankle MA. Effects of tilt and glenosphere eccentricity on baseplate/bone interface forces in a computational model, validated by a mechanical model, of reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20:732–739. doi: 10.1016/j.jse.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 12.Kempton LB, Balasubramaniam M, Ankerson E, Wiater JM. A radiographic analysis of the effects of prosthesis design on scapular notching following reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2011;20:571–576. doi: 10.1016/j.jse.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 13.Lévigne C, Boileau P, Favard L, Garaud P, Mole D, Sirveaux F, Walch G. Scapular notching in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2008;17:925–935. doi: 10.1016/j.jse.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Lévigne C, Garret J, Boileau P, Alami G, Favard L, Walch G. Scapular notching in reverse shoulder arthroplasty: is it important to avoid it and how? Clin Orthop Relat Res. 2011;469:2512–2520. doi: 10.1007/s11999-010-1695-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nolan BM, Ankerson E, Wiater JM. Reverse total shoulder arthroplasty improves function in cuff tear arthropathy. Clin Orthop Relat Res. 2011;469:2476–2482. doi: 10.1007/s11999-010-1683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nyffeler RW, Werner CM, Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg. 2005;14:524–528. doi: 10.1016/j.jse.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Nyffeler RW, Werner CM, Simmen BR, Gerber C. Analysis of a retrieved delta III total shoulder prosthesis. J Bone Joint Surg Br. 2004;86:1187–1191. doi: 10.1302/0301-620X.86B8.15228. [DOI] [PubMed] [Google Scholar]
- 18.Sanchez-Sotelo J, O’Driscoll SW, Torchia ME, Cofield RH, Rowland CM. Radiographic assessment of cemented humeral components in shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10:526–31. doi: 10.1067/mse.2001.118482. [DOI] [PubMed] [Google Scholar]
- 19.Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007;89:588–600. doi: 10.2106/JBJS.F.00226. [DOI] [PubMed] [Google Scholar]
- 20.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–395. doi: 10.1302/0301-620X.86B3.14024. [DOI] [PubMed] [Google Scholar]
- 21.Wall B, Nove-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 22.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–1486. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]