Abstract
Purpose
The aim of this study is to evaluate the accuracy of VISIONAIRE (Smith & Nephew Inc., Memphis, TN, USA) Patient Matched cutting tibial jigs in comparison with extramedullary (EM) tibial instrumentation by analysing data as detected by intra-operative use of VectorVision knee navigation software from BrainLAB (Redwood City, CA, USA).
Methods
Twelve patients were selected for unilateral total knee replacement (TKR). They underwent a full-length weight-bearing anteroposterior (AP) radiograph and magnetic resonance imaging (MRI). During surgery, once the EM guides were placed and fixed on the tibia, the orientation in the coronal and sagittal planes was checked by the navigator and then compared with the data obtained by measuring the orientation of VISIONAIRE Patient Matched cutting tibial jigs. An unsatisfactory result was considered an error ≥2° in both coronal and sagittal planes for the tibial component as a possible error of 4° could result.
Results
In the coronal plane the mean deviation of the EM tibial guides from the ideal alignment (0°) was 0.7 ± 0.39° and of the VISIONAIRE was 129 ± 1.55° (P = 0.22). In the sagittal plane the mean deviation of the EM tibial guides from 3° of posterior slope was −1.62 ± 1.78° and of the VISIONAIRE was +1.16 ± 4.29° (P < 0.05). Negative values indicate a more posterior slope from the ideal and positive values an anterior slope.
Conclusions
This preliminary study documented only a fair accuracy of the method with a consistent risk of error of more of 3° especially in the sagittal plane. We could speculate that the problem in the sagittal plane was due to the fact that the pre-operative protocol does not include a lateral X-ray projection of the knee and only includes an AP standing X-ray of the straight leg and MRI.
Introduction
Total knee arthroplasty (TKA) has been established as reliable treatment for osteoarthritis of the knee [1]. Axial alignment of the limb with restoration of the mechanical axis is a determinant of the outcome [2]. A number of studies [3–5] have suggested that alignment errors of >3° are associated with more rapid failure and less satisfactory functional results.
Improvements in surgical techniques and understanding of the biomechanics of the complex knee joint, materials and implant design have contributed to the success of surgery. The accuracy of implant placement has reached a plateau with little improvement in the extramedullary (EM) guiding system [6–8].
The use of a computer-based system during total knee replacement (TKR) has become more common in recent years due to the inability of the standard instrumentation to accurately determine the correct location of crucial alignment landmarks (the centre of the femoral head and the centre of the ankle). A number of studies [9–13] have suggested that there is improved alignment when this technology is used.
In recent years the opportunity to create new systems to reduce the costs and surgical time has arisen. The system should also be precise enough to obtain a good alignment, minimising the instrumentation size and surgical time whilst being reliable. The VISIONAIRE Patient Matched Technology (Smith & Nephew Inc., Memphis, TN, USA) is a system designed to reduce the overall instrumentation complexity, to reduce the overall time and eventually the costs of the TKA surgery with the use of custom cutting blocks for every patient.
The hypothesis of this study is that the EM guiding system is more accurate in positioning tibial components than the VISIONAIRE. The aim of this study is to evaluate the accuracy and reliability of VISIONAIRE Patient Matched cutting tibial jigs in comparison with EM tibial instrumentation by analysing data as detected by intra-operative use of VectorVision knee navigation software from BrainLAB (Redwood City, CA, USA).
Materials and methods
Between February 2011 and May 2011, 15 patients with primary gonarthrosis were selected for unilateral TKR. All patients were operated with the cemented posterior stabilised cruciate ligament sacrificing prosthesis (Journey BCS, Smith & Nephew Inc., Memphis, TN, USA) by the same surgeon using the VISIONAIRE Patient Matched cutting jigs. None of the patients had the patella resurfaced.
The first three patients were excluded from this study, as they were considered as a warm up to set up the procedure. Therefore 12 patients entered the study and demographic data are showed in Table 1.
Table 1.
Demographic data
| Characteristic | Value |
|---|---|
| Age (mean, SD, range) | 72 ± 4.7 (66–81) |
| Sex | 3 men and 9 women |
| Side | 6 right and 6 left |
| Preoperative full leg deformity (mean, SD, range) | 8.9 ± 3.39° (4.2–14.2) |
No patient had a bleeding diathesis. Anti-inflammatory drugs were suspended seven days before surgery. Before surgery, an autologous blood transfusion programme was undertaken following a predetermined schedule: all patients pre-donated two units of autologous blood.
All patients fully consented to be included in the study. The study was approved by the local Ethics Committee, and written informed consent was obtained from every subject.
Rationale for pre-operative imaging used for VISIONAIRE Technology alignment
All patients underwent a full-length weight-bearing radiograph and magnetic resonance imaging (MRI) of the knee following the protocol approved by the manufacturer.
The Smith & Nephew VISIONAIRE™ imaging protocol is compatible with MRI machines with a magnet strength of at least a 1.5 T using a standard knee coil as the imaging device, which is readily available in MR facilities and widely used on a routine basis. On average, the scan takes approximately 8–10 min per total scan, where complete knee scans can range anywhere from 30 min to 1 h.
An additional anteroposterior (AP) long, standing X-ray was done. The pre-operative study was sent to the Smith & Nephew laboratory to produce the tibial and femoral resection guides.
On the X-ray, lines are drawn for the mechanical axes of the femur and tibia. The angle between the two lines is measured as the leg deformity angle and listed in the preoperative plan. Lines are drawn for the mechanical and anatomical axes of the femur. The angle between the two lines is measured as the valgus angle and it will later be applied to the 3D MRI model for varus/valgus alignment. Femur landmarks are the distal sulcus, proximal shaft and a virtual intramedullary (IM) rod created from the sulcus to the centre of the proximal shaft in the 3D model. The 3D MRI model with virtual IM rod is superimposed over the X-ray. The mechanical axis is drawn relative to the IM rod using the valgus angle from the X-ray (ex 6°). The distal femoral resection is planned to be perpendicular (90°) to the mechanical axis. Flexion alignment is set from the “virtual IM rod” to be consistent with standard instrumentation. Flexion is defined by the shape and bow of the patient’s femur. Distal resection is set perpendicular to the virtual rod. The standard flexion plan is described as 4° because the literature suggests that the mechanical axis is flexed ~4° on average relative to the IM rod. Epicondyles are chosen from the MRI in both axial and coronal views considering the lateral prominence and medial sulcus. The epicondylar axis (TEA) then is drawn between the two landmarks and applied to the 3D model. Whiteside’s line (AP axis) is drawn through the deepest part of the sulcus and verified by rotating the 3D model through a range of motion. The posterior condylar axis (PCA) is drawn through the most posterior points after flexion is set with the virtual IM rod. The TEA axis is the default primary rotation landmark and is checked against the AP and PCA axes for consistency.
On the X-ray lines are drawn for the mechanical and anatomical axes of the tibia. The angle between the two lines is measured as the tibia deformity angle and is later applied to the 3D model for tibia varus/valgus alignment. Tibial landmarks are the proximal tibial anterior cruciate ligament (ACL) footprint, distal tibia and virtual IM rod created from the ACL footprint to the centre of the distal shaft. The 3D MRI model with virtual IM rod is superimposed over the X-ray. The mechanical axis is placed relative to the IM rod using the bow angle from the X-ray. According to the Journey implant tibia and femur resection was planned to be perpendicular (90°) to the mechanical axis in the coronal plane. The slope alignment is set from the “virtual IM rod” (anatomical axis) to be consistent with standard IM instrumentation and is set to 3°. The slope can be changed based on surgeon preference. The default rotation line is drawn from the ACL footprint to the medial one third of the tubercle. Size and rotation are then adjusted for optimum coverage and posterior fit (estimating osteophyte removal). The size is set large enough to cover cortical bone, while minimising overhang.
Operative technique and prosthesis
All patients were operated upon by the same surgeon in the same hospital. The operations were carried on in a bloodless field using a pneumatic tourniquet at a pressure of 350 mmHg after exsanguination.
Using a medial parapatellar approach, a medial parapatellar arthrotomy was done in all patients but one. Following the surgical technique we did not remove any osteophytes from tibial and femoral surfaces.
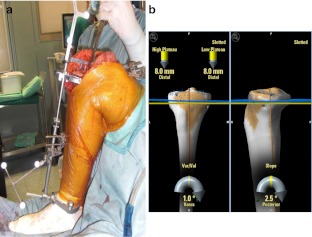
Accuracy of the EM guide was assessed first in all cases to reduce intra-operative bias. Deviation from the 0° mechanical axis and from 3° of posterior slope was recorded (Fig. 1a, b). Then the accuracy of VISIONAIRE was assessed. The patient-specific guide was placed and fixed. The orientation of the cutting slot was assessed with the same technique as previously described (Fig. 2a, b).
Fig. 1.
a, b The orientation of the EM guide was recorded
Fig. 2.
a, b The orientation of the VISIONAIRE guide was recorded
The following data were recorded: coronal plane of the tibia and femur, posterior slope of the tibia and flexion of the femur. An unsatisfactory result was considered an error ≥2° in both planes for each component (as a possible error of 4° could result should an error in the same direction occur in both the tibial and femoral resection). In the case of a great deviation from the planned resection a recut was performed.
The results were analysed using Student’s t test for statistical significance (P < 0.05).
Results
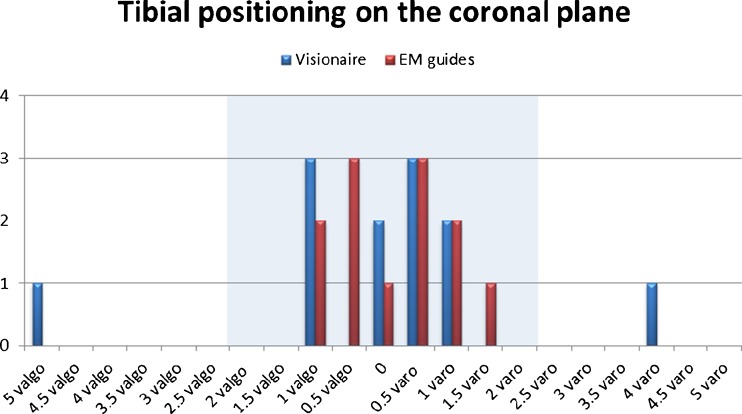
On the coronal plane the mean deviation of the EM tibial guides from ideal alignment was 0.7 ± 0.39° (range 0–1.5) and no patient exceeded 2°. Regarding the positioning of patient matched cutting jigs the mean deviation was 1.29 ± 1.55° (range 0–5) with two cases exceeding 2° (P = 0.22) (Fig. 3).
Fig. 3.
EM guide vs VISIONAIRE in the coronal plane
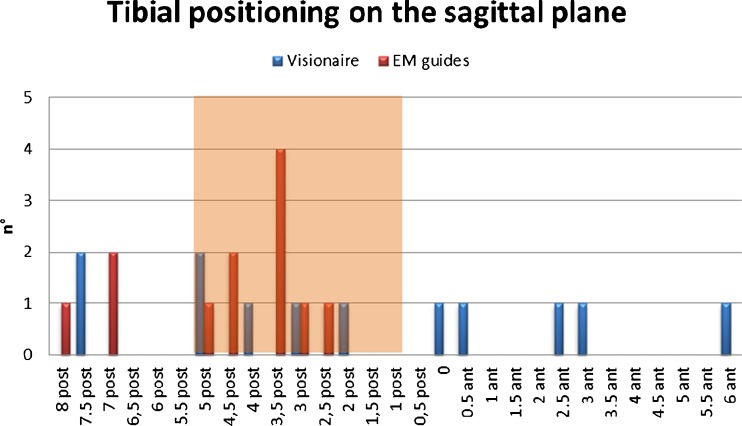
In the sagittal plane the mean deviation of the EM tibial guides from ideal alignment (3° of posterior slope) was −1.62° ± 1.78° (range −5 to +7°) and four patients exceeded 2°. Regarding the positioning of patient matched cutting jigs the mean deviation was +1.16 ± 4.29° (range −4.5 to +9°) with nine cases exceeding 2° (P < 0.05) (Fig. 4). Negative values indicate a more posterior slope from the ideal and positive values an anterior slope.
Fig. 4.
EM guide vs VISIONAIRE in the sagittal plane
Discussion
Ishii et al. [14] found that no significant differences were noted between alignments achieved using the IM tibial guide and those of EM guides with the standard technique, but EM avoids the potential complications of IM guide use, including fat embolisation and hypoxia, intra-operative fracture, loss of polymethyl methacrylate pressurisation, and inability of IM rod passage due to deformity, retained hardware or pathologic bone disease. [15]
This study seems to support our hypothesis. Considering as optimal parameters in the coronal plane a total of maximum 3° varus/valgus, a maximum deviation of 2° on the tibia and 2° on the femur should be permitted. As no previous studies documented the effect of tibial slope on performance of the knee, we considered as optimal parameters 3° of posterior slope on the tibia.
According to the criteria used in this study we found a significant difference in accuracy in the standard technique as compared with error exceeding ≥2° in 15 % of cases in the coronal plane and 58 % in the sagittal plane, both occurring in the VISIONAIRE measurement.
The patient matched cutting jigs technology should be the last end point of surgery. One theoretical advantage of this system is the possible reduction of operating time, because the surgeon could cut without other instrumentation. However the accuracy of the technology should be carefully assessed before becoming a routine practice.
To our knowledge there are still very few published studies regarding the use of custom-fit cutting blocks. In a preliminary laboratory study Hafez et al. [16] analysed the use of this technology on cadaver knee and plastic bones. Despite the limitations expressed in their study, they reported they were able to achieve good alignment and reduce overall surgery time. In a recent small case series study Klatt et al. [17] found the custom-fit technique resulted in malalignment; in fact, component positioning, as measured by the navigation system and referenced to the mechanical axis, ranged from 5° valgus to 7.5° varus. In another recent clinical study Spencer et al. [18] studied the use of custom-fit technology in 21 patients with the use of postoperative computed tomography (CT) scans. They obtained satisfactory clinical results and an acceptable alignment. Their postoperative coronal alignment was close but not ideal to the mechanical axis possibly leading to early wear rates. Noble et al. [19] found that custom-made cutting jigs are mostly reliable, but their study is based on the postoperative X-ray. All previous authors [16–19] agreed that the custom cutting blocks are able to reduce surgery time, sterilisation costs and surgical complications such as bleeding, infections and embolism.
In our early series the surgery time was impossible to calculate due to the extra time for placing trackers on the landmark acquisition for the computer-assisted surgery (CAS); instead, the effect of VISIONAIRE on the overall costs of the procedure could be calculated only after the development of the surgical technique.
A limitation of this study was represented by the sample size, but the data collected documented an only fair accuracy of this method with an higher risk of error in the sagittal plane. We could speculate that the greater inaccuracy in this plane could be attributed to the fact that the pre-operative study does not include a lateral imaging of the leg, but only MRI restricted to the knee.
Conclusions
The standard instrumentation in the hands of experienced surgeons could lead to a better alignment of the prosthesis as compared with MRI-based patient matched cutting jigs.
References
- 1.Lundblad H, Kreicbergs A, Söderlund V, Ulfgren AK, Stiller CO, Jansson KA (2011) The value of preoperative grade of radiographic and histological changes in predicting pain relief after total knee arthroplasty for osteoarthritis. Knee Surg Sports Traumatol Arthrosc. [Epub ahead of print] [DOI] [PubMed]
- 2.Ishida K, Matsumoto T, Tsumura N, Kubo S, Kitagawa A, Chin T, Iguchi T, Kurosaka M, Kuroda R. Mid-term outcomes of computer-assisted total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1107–1112. doi: 10.1007/s00167-010-1361-4. [DOI] [PubMed] [Google Scholar]
- 3.Linden-van der Zwaag HM, Bos J, Heide HJ, Nelissen RG. A computed tomography based study on rotational alignment accuracy of the femoral component in total knee arthroplasty using computer-assisted orthopaedic surgery. Int Orthop. 2011;35(6):845–850. doi: 10.1007/s00264-010-1082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Magnussen RA, Weppe F, Demey G, Servien E, Lustig S. Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res. 2011;469(12):3443–3450. doi: 10.1007/s11999-011-1988-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hernández-Vaquero D, Suarez-Vazquez A, Iglesias-Fernandez S. Can computer assistance improve the clinical and functional scores in total knee arthroplasty? Clin Orthop Relat Res. 2011;469(12):3436–3442. doi: 10.1007/s11999-011-2044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rottman SJ, Dvorkin M, Gold D. Extramedullary versus intramedullary tibial alignment guides for total knee arthroplasty. Orthopedics. 2005;28(12):1445–1448. doi: 10.3928/0147-7447-20051201-16. [DOI] [PubMed] [Google Scholar]
- 7.Jenny JY. Influence of intramedullary versus extramedullary alignment: guides on final total knee arthroplasty component position by Antonio Maestro et al. (pp 552–558) J Arthroplasty. 1999;14(7):898–899. doi: 10.1016/S0883-5403(99)90047-5. [DOI] [PubMed] [Google Scholar]
- 8.Yang SH, Liu TK. Intramedullary versus extramedullary tibial alignment guides in total knee arthroplasty. J Formos Med Assoc. 1998;97(8):564–568. [PubMed] [Google Scholar]
- 9.Tigani D, Masetti G, Sabbioni G, Ben Ayad R, Filanti M, Fosco M (2012) Computer-assisted surgery as indication of choice: total knee arthroplasty in case of retained hardware or extra-articular deformity. Int Orthop. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 10.Cheng T, Zhao S, Peng X, Zhang X (2011) Does computer-assisted surgery improve postoperative leg alignment and implant positioning following total knee arthroplasty? A meta-analysis of randomized controlled trials? Knee Surg Sports Traumatol Arthrosc. [Epub ahead of print] [DOI] [PubMed]
- 11.Blakeney WG, Khan RJ, Wall SJ. Computer-assisted techniques versus conventional guides for component alignment in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2011;93(15):1377–1384. doi: 10.2106/JBJS.I.01321. [DOI] [PubMed] [Google Scholar]
- 12.Brin YS, Nikolaou VS, Joseph L, Zukor DJ, Antoniou J. Imageless computer assisted versus conventional total knee replacement. A Bayesian meta-analysis of 23 comparative studies. Int Orthop. 2011;35(3):331–339. doi: 10.1007/s00264-010-1008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seon JK, Park SJ, Lee KB, Li G, Kozanek M, Song EK. Functional comparison of total knee arthroplasty performed with and without a navigation system. Int Orthop. 2009;33(4):987–990. doi: 10.1007/s00264-008-0594-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ishii Y, Ohmori G, Bechtold JE, Gustilo RB. Extramedullary versus intramedullary alignment guides in total knee arthroplasty. Clin Orthop Relat Res. 1995;318:167–175. [PubMed] [Google Scholar]
- 15.Dennis DA, Channer M, Susman MH, Stringer EA. Intramedullary versus extramedullary tibial alignment systems in total knee arthroplasty. J Arthroplasty. 1993;8(1):43–47. doi: 10.1016/S0883-5403(06)80106-3. [DOI] [PubMed] [Google Scholar]
- 16.Hafez MA, Chelule KL, Seedhom BB, Sherman KP. Computer-assisted total knee arthroplasty using patient-specific templating. Clin Orthop Relat Res. 2006;444:184–192. doi: 10.1097/01.blo.0000201148.06454.ef. [DOI] [PubMed] [Google Scholar]
- 17.Klatt BA, Goyal N, Austin MS, Hozack WJ. Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplasty. 2008;23(1):26–29. doi: 10.1016/j.arth.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Spencer BA, Mont MA, McGrath MS, Boyd B, Mitrick MF. Initial experience with custom-fit total knee replacement: intra-operative events and long-leg coronal alignment. Int Orthop. 2009;33(6):1571–1575. doi: 10.1007/s00264-008-0693-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noble JW, Jr, Moore CA, Liu N. The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty. 2012;27(1):153–155. doi: 10.1016/j.arth.2011.07.006. [DOI] [PubMed] [Google Scholar]