Abstract
Purpose
This paper presents experimental findings to substantiate the use of multilevel bone fragment lengthening for managing extensive long bone defects caused by diverse aetiologies and shows its clinical introduction which could provide a solution for the problem of reducing the total treatment time.
Methods
Both experimental and clinical multilevel lengthening to bridge bone defect gaps was performed with the use of the Ilizarov method only.
Results
The experimental findings and clinical outcomes showed that multilevel defect fragment lengthening could provide sufficient bone formation and reduction of the total osteosynthesis time in one stage as compared to traditional Ilizarov bone transport. The method of multilevel regeneration enabled management of critical-size defects that measured on average 13.5 ± 0.7 cm in 78 patients.
Conclusions
The experimental and clinical results proved the efficiency of the Ilizarov non-free multilevel bone plasty that can be recommended for practical use.
Introduction
The Ilizarov system of reconstructive management of long bone defects is based on the principle of non-free bone plasty [1]. It implies that bone loss is compensated for by distraction regeneration and results in consolidation at the docking site of the transported bone fragment. Moreover, the soft tissue envelope remains preserved and allows for bone growth in length and shape [1–4]. The technique of the Ilizarov bone transport following osteotomy of a defect fragment has been used by orthopaedic surgeons worldwide, and its merits are well known [2–7]. Nevertheless, despite the high rehabilitation effect of the Ilizarov non-free bone plasty, a number of authors emphasize that it requires several stages and takes a long time in cases of extensive bone defects [5–8]. The surgeons of the Russian Ilizarov Scientific Center proposed technologies of distraction osteosynthesis for bone plasty through several distraction areas in an affected segment in order to cover an extensive defect at a single stage by growing bone tissue that structurally remodels during a shorter time of transosseous osteosynthesis [10, 11]. Therefore, this study was aimed at presenting the experimental findings of multilevel defect management performed by the author and its clinical introduction that could provide a solution for reducing the total treatment time.
Materials and methods
Experiment
Sixty-six adult dogs were included in the experiment performed at the author’s institution between 2000 and 2005. Defects were modeled in the distal metadiaphysis (groups I, II), proximal metadiaphysis (groups III, IV), and diaphysis (group V) of the tibia. They measured 20.9 ± 0.3 % of the original tibial length. Each animal in groups I and III underwent bifocal distraction in one post-resection fragment consecutively using the Ilizarov apparatus while in groups II, IV and V distraction was simultaneous at two levels. The proximal fragments were lengthened in the conditions of preserved blood supply but the distal ones had disturbed major blood flow. The experimental models developed were similar to long bone defects that can be encountered in clinical practice due to resection, injury, repeated surgeries or failures. The experimental conditions and devices were adequate to clinical situations and allowed for bone formation monitoring during distraction and fixation.
Clinical application
Seventy-eight consecutive patients aged from seven to 49 years underwent surgeries due to long bones defects that averaged 13.5 ± 0.7 cm (range 6.0–30 cm) and were managed with the techniques of multilevel lengthening using the Ilizarov apparatus. The pathology had formed from six months to 29 years prior to admission to our hospital (mean 5.8 ± 0.7 years). The records of patients who had been treated at the author’s department till the end of 2011 were studied retrospectively. Thirteen patients had femoral defects, 19 had forearm bones defects, and five cases were humeral defects. The largest group was 41 patients with tibial defects. The pathology was caused by injuries in 40 individuals; 19 had segmental bone resection defects due to primary tumour and nine due to hematogenous osteomyelitis; ten cases were of congenital etiology.
Radiography, CT, histological and clinical studies were used to evaluate bone regeneration.
The studies were approved by the institutional ethical committee and were performed in accordance with the ethical standards laid down in the Declaration of Helsinki. All persons included into the study gave their informed consent and the study of human subjects followed the rules of clinical practice in the Russian Federation (RF Ministry of health order # 266). The “Principles of laboratory animal care” were followed, as well as the national regulations on laboratory practice (RF Ministry of health orders # 755, 267).
Results
Experiment
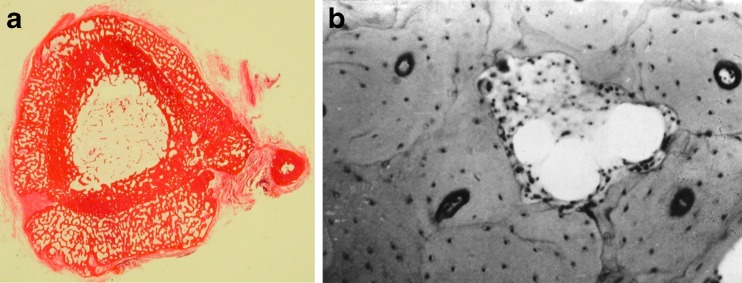
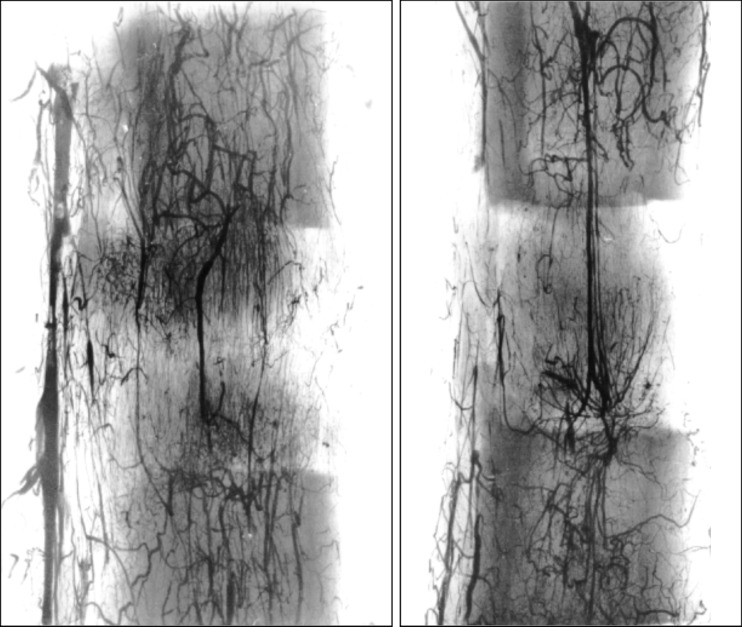
Distraction regeneration by dosed transport of non-free osteotomised autologous grafts in post-resection gaps had zonal structure (Fig. 1). In the animals of groups I, II and V, bone formation was provided by active participation of endosteal and periosteal bone structures in the distraction osteogenesis. Layers of cancellous bone tissue formed on the surface of transported fragment portions, particularly on the distal one. More cancellous bone was formed on the non-free autografts during their consecutive transport. Resorption cavities were formed in the cortices of the fragment portions (Fig. 2). The cortices of the transported fragment portions were thick enough due to compact periosteal layers of newly formed cancellous bone tissue. Lengthening of the proximal fragments in favourable conditions was for restoration of the anatomical and functional integrity of the intraosseous arterial network in the affected tibia (Fig. 3). The two-level but non-invasive break of the fragment for performing bifocal lengthening did not interrupt blood flow along the nutrient artery to the transported portions.
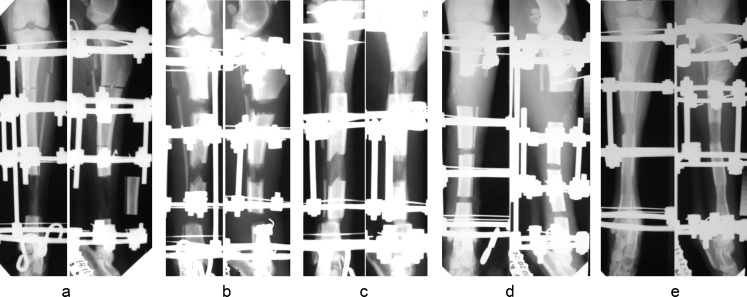
Fig. 1.
Radiographs of experimental animals during osteosynthesis: in the proximal fragment after the surgery (a), during transport of bone fragment portions (b), before apparatus removal (c). In the distal fragment seven days of distraction, 13 days of experiment (d); 75 days of fixation, 105 days of experiment (e)
Fig. 2.
a Histotopogram of proximal fragment portion cross-section (hematoxylin eosin staining). b Histotopogram part showing resorption cavity in the cortex of the transported down portion (microphoto, lens 10, objective 10)
Fig. 3.
Vasogram of the tibia by 19 days of distraction and 26 days of the experiment. a Proximal regeneration portion (AP). b Distal regeneration portion (lateral view)
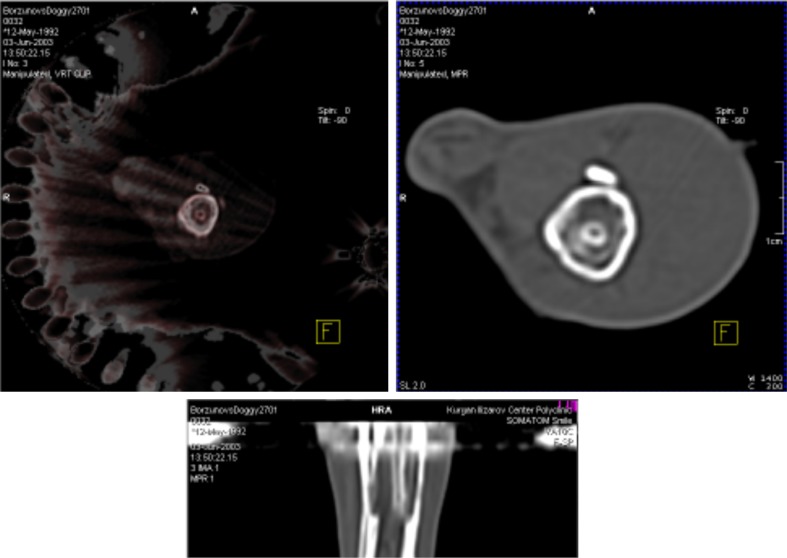
Bone formation by two-level lengthening of the distal tibial fragment in groups III and IV featured participation of mostly periosteal bone structures. The disturbed medullary blood flow in the distal tibial fragment had predetermined the decreased activity of endosteal osteogenesis. The transported fragment portions had porous cortices and numerous resorption cavities filled in with necrotic content. Periosteal cancellous bone layers were not observed along the entire periphery of fragment portions and were less than 1 mm thick. Distraction regeneration was of the hypoplastic type (Fig. 1). Planimetric evaluation of the distraction osteogenesis revealed that the gap in the regenerates exceeded the area of newly formed bone tissue. It took a longer period for regenerated bone to restructure into typical bone tissue after the apparatus had been removed. Hypoplastic regenerates were unstable to functional loading for a long period. Moreover, bifocal distal fragment lengthening was characterized by prolonged disturbance in the major medullary blood flow. In the animals of group III, the major flow along the nutrient artery was observed in the proximal fragment portion only at the end of the fixation period. However, the CT study showed restored major blood flow in the proximal regeneration area with the nutrient artery bone marrow canal formed by day 31 of fixation (Fig. 4). The major blood flow along the intraosseous pool was observed in the animals of group IV only by fixation day 74.
Fig. 4.
CT of the proximal regeneration portion on the 57th fixation day
Regenerated bone tissue mineralization followed the same pattern in all groups, i.e. bone density values in the newly formed bone parts approximated the values of the matched parts in the contralateral segment by the period from six to nine months in the groups I, II and V after removal of the apparatus but in the animals of groups III and IV only after 1.5 years.
Clinical application
Two main techniques of distraction osteogenesis were used for bone defect management in our series of patients, with multilevel one-fragment lengthening in 48 cases and both fragments lengthened in 21 patients. Seven cases were treated by a combination of the above techniques. Two clinical situations required multilevel lengthening in one fragment and lengthening in the adjacent segment. The variants are shown in the diagrams (Fig. 5).
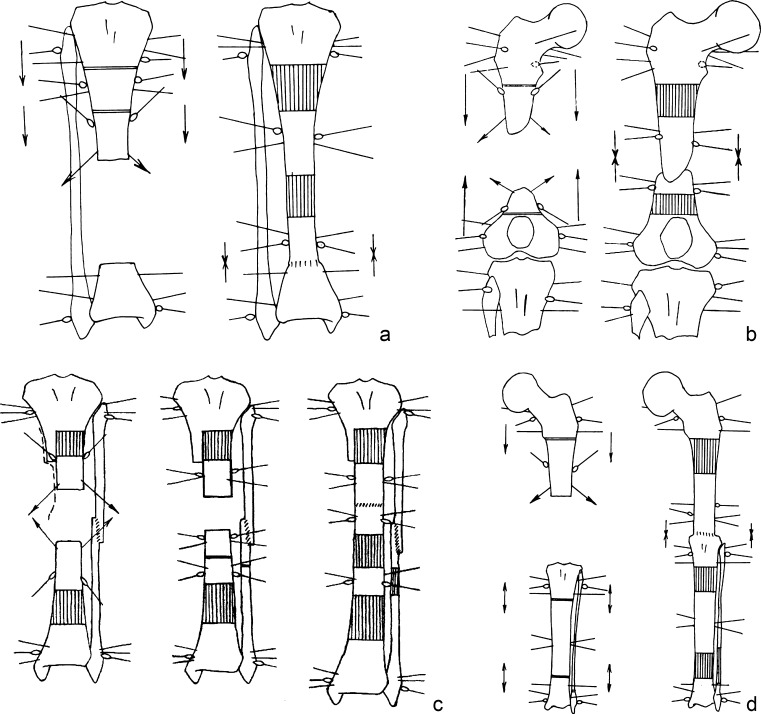
Fig. 5.
Osteosynthesis diagrams simultaneous multilevel lengthening of the proximal tibial fragment (a), lengthening of both femoral fragments (b), lengthening in the conditions of soft tissue scars using sequential multilevel lengthening of both tibial fragments (c), and multilevel lengthening involving adjacent segment (d)
All bone defects bridged during one stage and united at docking sites. For all segments, distraction averaged 110.4 ± 7.7 days and fixation period was 160.9 ± 9.4 days.
We compared the outcome measures that refer to treatment duration of large tibial defects that ranged from 12 to 14 cm by using Ilizarov traditional bone transport (bifocal compression distraction method, combined or consecutive techniques) and by multilevel techniques (consecutive and simultaneous).
Table 1 demonstrates that distraction period can be reduced 2.5 times and fixation from 1.3 to 1.9 times when the multilevel techniques were used.
Table 1.
Comparative measures of tibial defect repair by using Ilizarov techniques
| Parameter | Bifocal combined compression distraction | Bifocal consecutive compression distraction | Multilevel consecutive fragment lengthening | Multilevel simultaneous fragment lengthening |
|---|---|---|---|---|
| Defect (cm) | 12 ± 1.8 | 11.9 ± 0.6 | 12.2 ± 1.5 | 14.1 ± 1.6 |
| Defect to segment limb ratio (%) | 30.4 ± 5.7 | 31.6 ± 1.5 | 36.6 ± 3.6 | 42.3 ± 4.0 |
| Distraction (days) | 127.0 ± 36.1 | 144.7 ± 12.6 | 56.0 ± 4.8 | 52.8 ± 4.7 |
| Fixation (days) | 180.0 ± 25.9 | 199.0 ± 18.0 | 101.5 ± 13.4 | 167.8 ± 18.6 |
| Total osteosynthesis time (days) | 323.0 ± 52.1 | 361.2 ± 25.6 | 284.1 ± 30.5 | 291.4 ± 28.6 |
| Fixation index (days/cm)a | 17.8 ± 3.3 | 26.1 ± 2.9 | 10.3 ± 1.3 | 16.5 ± 1.9 |
| Osteosynthesis index (days/cm)b | 30.7 ± 4.2 | 46.4 ± 3.9 | 28.8 ± 5.0 | 28.7 ± 1.7 |
| Lengthened amount (cm) | 10.8 ± 1.2 | 8.8 ± 0.7 | 11.2 ± 1.6 | 10.1 ± 0.7 |
| Lengthened amount, % | 92.0 ± 4.6 | 74.3 ± 3.5 | 91.2 ± 4.6 | 78.3 ± 8.1 |
a Fixation index: ratio of fixation (days) to lengthened amount (cm)
b Osteosynthesis index: ratio of total osteosynthesis period (days) to lengthened amount (cm)
Discussion
Critical-size bone defects are a challenging problem for orthopaedic surgeons. At present, the two prevailing methods for bone defect repair that provide vascular ties of the graft with the soft tissues are the Ilizarov non-free bone plasty and free vascularized grafts. They are considered to be methods of choice, and the studies that compared the efficiency of these two methods stated that there were no great advantages between them in obtaining anatomic integrity or functional outcomes [12–14].
Long bone defect fragment lengthening could be an ideal type of bone plasty by which a non-free vascularized bone graft is transported gradually and purposefully to the targeted area. But appreciating greatly the Ilizarov non-free bone plasty for bone defect management, most authors emphasize its essential drawback, the so called “Achilles heel”, i.e. a long treatment period that requires great patient’s compliance and constant care by an orthopaedic surgeon [5–8, 15].
Therefore, a large-scale experiment was undertaken to reveal bone formation during extensive defect repair using distraction osteogenesis in several foci. It proved bone formation consistency and reduction of distraction time due to bifocal regeneration. It also showed high activity of endosteal and periosteal distraction osteogenesis by two-level fragment lengthening in the conditions of preserved major blood flow. When two-level transport was performed by disturbed major intraosseous vessels the regeneration areas were hypoplastic. Bone regeneration took a longer time but the process was adaptive. A number of previous experiments had also shown the importance of blood supply for bone regeneration and osteogenic potential of bone plasty but the conditions of experiments were different [16, 17].
As for clinical situations, some surgeons use bone transport over intramedullary nail to avoid wearing an external fixator for a long time during defect repair but the combination cannot accelerate distraction osteogenesis [8, 9, 15]. The analysis of multilevel lengthening in our series testified its efficiency in reducing the total treatment time at one stage. Multilevel techniques for defect management have been already used by several authors, and they advocate them [18–20]. However, all existing methods of large defect repair are technically demanding and yield good results in the hands of experienced surgeons.
Conclusion
The experimental findings have revealed that multilevel techniques of non-free bone plasty are competent in restoring the anatomy and function of the affected limb segments. The clinical outcomes of their use for long bone heterogenic defect reconstruction have confirmed the possibility of reducing the time and the number of treatment stages. The results obtained are good grounds for application of multilevel non-free Ilizarov bone plasty in clinical practice.
Acknowledgement
I highly appreciate V.I. Shevtsov’s advice, the help of N.V. Petrovskaya for assisting during operations on animals, and A.M. Chirkova for histological studies.
Conflict of interest
There are no conflicts of interest.
References
- 1.Ilizarov GA. Transosseous osteosynthesis. Heidelberg: Springer-Verlag; 1992. [Google Scholar]
- 2.Green SA, Jackson JM, Wall DM, Marinow H, Ishkanian J. Management of segmental defects by the Ilizarov intercalary bone transport method. Clin Orthop Relat Res. 1992;280:136–142. [PubMed] [Google Scholar]
- 3.Golyakhovsky V, Frankel VH, Ferrara PL. Operative manual of Ilizarov techniques. St. Louis: Mosby; 1993. [Google Scholar]
- 4.Shevtsov VI, Makushin VD, Kuftyrev LM. Defects of the lower limb bones. Kurgan: Zauralie; 2000. [Google Scholar]
- 5.Paley D, Maar DC. Ilizarov bone transport treatment for tibial defects. J Orthop Trauma. 2000;14(2):76–85. doi: 10.1097/00005131-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 6.El-Alfy B, El-Mowafi H, El-Moghazy N. Distraction osteogenesis in management of composite bone and soft tissue defects. Int Orthop. 2010;34(1):115–118. doi: 10.1007/s00264-008-0574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith WR, Elbatrawy YA, Andreassen GS, et al. Treatment of traumatic forearm bone loss with Ilizarov ring fixation and bone transport. Int Orthop. 2007;31(2):165–170. doi: 10.1007/s00264-006-0172-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liodakis E, Kenawey M, Krettek C, Wiebking U, Hankemeier S. Comparison of 39 post-traumatic tibia bone transports performed with and without the use of an intramedullary rod: the long-term outcomes. Int Orthop. 2011;35(9):1397–1402. doi: 10.1007/s00264-010-1094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keating JF, Simpson AHRW, Robinson CM. The management of fractures with bone loss. J Bone Joint Surg Br. 2005;87-B(2):142–150. doi: 10.1302/0301-620X.87B2.15874. [DOI] [PubMed] [Google Scholar]
- 10.Shevtsov VI, Borzunov DY, Petrovskaya NV. Long bone defect management by polyfocal distraction regeneration. Trauma. 2007;8(4):382–386. [Google Scholar]
- 11.Borzunov DY, Kuftyrev LM. Comparative analysis of treatment results of using various technologies of lengthening fragments in patients with extensive tibial defects. Vestn Travm Ortop im Priorova. 2002;1:29–34. [Google Scholar]
- 12.Yokoyama K, Itoman M, Nakamura K, Tsukamoto T, Saita Y, Aoki S. Free vascularized fibular graft vs. Ilizarov method for post-traumatic tibial bone defect. J Reconstr Microsurg. 2001;17(1):17–25. doi: 10.1055/s-2001-12684. [DOI] [PubMed] [Google Scholar]
- 13.Song HR, Kale A, Park HB, Koo KH, Chae DJ, Oh CW, Chung DW. Comparison of internal bone transport and vascularized fibular grafting for femoral bone defects. J Orthop Trauma. 2003;17(3):203–211. doi: 10.1097/00005131-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 14.El-Gammal TA, Shiha AE, El-Deen, et al. Management of traumatic tibial defects using free vascularized fibula or Ilizarov bone transport: a comparative study. Microsurgery. 2008;28(5):339–346. doi: 10.1002/micr.20501. [DOI] [PubMed] [Google Scholar]
- 15.Kocaoglu M, Eralp L, Rashid HU, Sen C, Bilsel K. Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J Bone Joint Surg Am. 2006;88(10):2137–2145. doi: 10.2106/JBJS.E.01152. [DOI] [PubMed] [Google Scholar]
- 16.Shevtsov VI, Gordievskikh NI, D'iachkov AN, Ruchkina IV. Dynamics of the blood supply in the leg soft tissue in the course of experimental defect filling. Ross Fiziol Zh Im IM Sechenova. 2004;90(9):1156–1160. [PubMed] [Google Scholar]
- 17.DeCoster TA, Simpson AHRW, Wood M, Li G, Kenwright J. Biologic model of bone transport distraction osteogenesis and vascular response. J Orthop Res. 1999;17(2):238–245. doi: 10.1002/jor.1100170213. [DOI] [PubMed] [Google Scholar]
- 18.Rozbruch RS, Weitzman AM, Watson TJ, Freudigman P, Katz HV, Ilizarov S. Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma. 2006;20(3):197–205. doi: 10.1097/00005131-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Sala F, Thabet AM, Castelli F, Miller AN, Capitani D, Lovisetti G, Talamonti T, Singh S. Bone transport for postinfectious segmental tibial bone defects with a combined Ilizarov/taylor spatial frame technique. J Orthop Trauma. 2011;25(3):162–168. doi: 10.1097/BOT.0b013e3181e5e160. [DOI] [PubMed] [Google Scholar]
- 20.Guerreschi F, Azzam W, Camagni M, Lovisetti L, Catagni MA. Tetrafocal bone transport of the tibia with circular external fixation: a case report. J Bone Joint Surg Am. 2010;92(1):190–195. doi: 10.2106/JBJS.H.01109. [DOI] [PubMed] [Google Scholar]