Abstract
Purpose
Hip fractures constitute a serious and common health problem from both individual and public health perspectives. Unified data collection and comparison between countries is recognised as an effective tool for care improvements. However, the variation in patients’ demography, treatment methods and other local cultural aspects in different countries should be considered. The aim of our study was to compare femoral neck fracture patients treated in Kaunas and Lund, concerning functional outcome and quality of life.
Methods
We investigated 99 patients treated by arthroplasty in Kaunas Clinics and 117 patients in Lund University Hospital. Patients were investigated according to the National Swedish Hip Fracture Register model and were followed up for a period of four months after the injury. The patient’s place of residence, mobility, complaints of pain and additional hospital stay were recorded. The EQ-5D questionnaire was used to evaluate quality of life.
Results
Patients in Kaunas were significantly younger, had lower ASA grade and were more mobile before trauma and at four moths follow-up. However, when comparing quality of life at four months follow-up between the institutions, Lund patients reported significantly better self care, felt less pain and discomfort, and had less symptoms of anxiety and depression.
Conclusions
The difference observed in quality of life rating between institutions might be related to local cultures of the countries and should be considered when comparing the data.
Introduction
Hip fractures constitute a serious and common health problem among older adults from both the individual and public health perspectives. They are associated with increased morbidity and mortality compared to the general population [1–3]. Treatment methods and the care of patients with hip fractures vary in different countries; such models are usually developed within the context of local cultures and health-care systems.
Lund University hospital (LUH) was the first institution in Europe to introduce national prospective registration of hip fracture patients in 1988 by developing the Swedish Hip Fracture register, eventually covering the whole of Sweden [4]. The scientific data from the register influenced changes in treatment methods, rehabilitation, and also resulted in the introduction of integrated care protocols for care of femoral neck fracture patients. All these changes have significantly improved patients functional outcome and their quality of life [5, 6].
At present Lithuania does not have well defined schemes for the treatment of femoral neck fracture patients. Lack of prospective studies investigating the outcomes impedes the implementation of effective models in clinical practice. The current situation in the country has encouraged us to start a prospective registration of femoral neck fracture patients and compare our results with Lund University Hospital. A standardised prospective comparison has been efficient [7], and the results might change the treatment policies in our country.
The aim of our study was to compare the functional outcome and quality of life in femoral neck fracture (FNF) patients treated in Kaunas Medical University Hospital and LUH.
Patients and methods
We investigated patients with fresh FNF admitted to Kaunas Clinics, Lithuania, and LUH, Sweden. Patients 55 years and older with non pathological femoral neck fractures and treated with arthroplasty were included. We compared patients fracture type, American Society of Anesthesiologists (ASA) grade, demographic variables, mortality rates in the institutions. Functional outcome and quality of life at four months after the trauma were compared in both institutions.
All patients included in the study were investigated prospectively using the same study protocol in Kaunas and Lund. Patients were assessed according to the National Swedish Hip Fracture Register model and were followed up for a period of four months after the injury. The Swedish National Hip Fracture Register consists of three forms for data collection. The first form (form no. 1) is used to collect information about the patient’s admission to the health-care institution, place of residence before the fracture, mobility, and the time and location of discharge. The second form (form no. 2) consists of information collected during the follow-up visit at four months after the injury. The patient’s place of residence, mobility, pain and any additional hospital stay is recorded. The information was collected either via mail or patients were assessed in the outpatient department. Additional surgery, if performed during the follow-up period, is registered on form no. 3. Euro Qol-5D (EQ-5D) [8], a health related questionnaire for quality of life evaluation, was applied four months after the injury.
The study was approved by the ethical committee of the institution.
Statistics
The primary effect variable, used for power calculation analysis, was EQ VAS scoring. Assuming a difference in the means of 10, an SD of 15 for both groups, and aiming for a power of 0.95 and a risk of 0.05 for a type-1 error, 60 patients were required in the Kaunas Clinics and LUH. The Student’s t-test was used to compare the means. Fisher’s exact test was used to compare differences in the proportions of qualitative variables. The McNemar test used to compare differences in the proportions of categorical variables for repeated measurements of the same patient group. For comparison between two categorical variables, the Z test was applied. Linear regression analysis (backward method) was used to evaluate factors including country, sex, age, mobility, use of walking aids before and after the injury, ASA class and type of implant, in relation to the patients’ quality of life according to the EQ-5D outcomes.
Results
Between March 1, 2008 and September 1, 2010 there were 176 FNF treated in Kaunas Clinic and 262 femoral neck fracture patients treated in Lund. A flow chart of all patients treated in both institutions is shown in Fig. 1.
Fig. 1.
Flow chart of all femoral neck fracture patients treated in both institutions
The data of all patients treated in both institutions with arthroplasty is presented in Table 1. Patients in Kaunas were younger, had lower ASA grade and all were treated with total hip arthroplasty, whereas in Lund 84 % of patients received a Bipolar prosthesis.
Table 1.
The comparison of baseline data of femoral neck fracture patients treated with arthroplasty in Kaunas and Lund
| Hospitals | Age | Gender | ASA grade | Type of fracture | Method of surgery |
|---|---|---|---|---|---|
| Kaunas clinics, n = 147 | 78 (SD 9) | Male 38 (25.9 %) | I – 2 (1.4 %) | Non-displaced 8 (5.4 %) | Bipolar 0, 0.0 % |
| II – 80 (54.4 %) | |||||
| Female 109 (74.1 %) | III – 61(41.5 %) | Displaced 139 (94.6 %) | THA 147, 100.0 % | ||
| IV – 4 (2.7 %) | |||||
| V – 0 | |||||
| LUH, n = 167 | 83 (SD 8) | Male 49 (29.3 %) | I – 6 (3.6 %) | Non-displaced 4 (2.4 %) | Bipolar 141, 84.4 % |
| II – 59 (35.3 %) | |||||
| Female 118 (70.7 %) | III – 96 (57.5 %) | Displaced 163 (97.6 %) | THA 26, 15.6 % | ||
| IV – 6 (3.6 %) | |||||
| V – 0 | |||||
| p value | <0.001 | 0.53 | 0.007 | 0.3 | <0.001 |
Before the end of four months follow-up out of the remaining 147 patients treated with arthroplasty, 15 (10 %) patients died in Kaunas as compared to 29 (17 %) out of 167 patients in Lund (p = 0.07). Patients who were unable to answer the EQ-5D questionnaire due to cognitive impairment, who were lost to follow-up or underwent additional surgery, were also excluded from functional outcome and quality of life analysis (Fig. 1). Thus functional and quality of life outcome at four months was investigated in 99 femoral neck fracture patients treated with arthroplasty in Kaunas and 117 in Lund.
A four-month period after the trauma was not sufficient for patients to regain their pre-fracture mobility in both institutions. Significant differences were observed between the institutions before trauma and at four months follow-up; patients in Kaunas were more mobile (p < 0.001) and were using fewer walking aids (p < 0.001; Table 2).
Table 2.
Comparative data according to hip fracture register forms of patients before fracture and after four months in both institutions (Z-test)
| Variables | Before trauma, n (%) | At 4 months, n (%) | ||||
|---|---|---|---|---|---|---|
| Kaunas clinics, n = 99 | LUH, n = 117 | p | Kaunas clinics, n = 99 | LUH, n = 117 | p | |
| Place of residence | ||||||
| Home | 78 (78.8) | 91 (77.8) | 0.86 | 92 (92.9) | 81 (69.2) | 0.001 |
| Social facilities | 2 (2) | 21 (17.9) | <0.001 | 5 (5.1) | 31 (26.5) | <0.001 |
| Health care institutions | 19 (19.2) | 5 (4.3) | <0.001 | 2 (2) | 5 (4.3) | 0.36 |
| Mobility | ||||||
| Walked alone out of doors | 83 (83.8) | 73 (62.4) | 0.001 | 54 (54.6) | 50 (42.7) | 0.09 |
| Walked out of doors only if accompanied | 10 (10.1) | 3 (2.6) | 0.03 | 19 (19.2) | 1 (0.9) | <0.001 |
| Walked alone indoors but not out of doors | 6 (6.1) | 35 (29.9) | <0.001 | 21(21.2) | 42 (35.9) | 0.02 |
| Walked indoors only if accompanied | 0 | 4 (3.4) | 0.06 | 2 (2) | 14 (12) | 0.005 |
| Unable to walk | 0 | 2 (1.7) | 0.2 | 3 (3) | 10 (8.5) | 0.1 |
| Walking aids usage | ||||||
| Can walk without aids | 63 (63.7) | 68 (58.1) | 0.42 | 20 (20.2) | 28 (23.9) | 0.53 |
| One or two walking stick, crutch or tripod | 33 (33.3) | 12 (10.3) | <0.001 | 58 (58.6) | 20 (17.1) | 0.001 |
| Walking frame | 3 (3) | 34 (29) | <0.001 | 18 (18.2) | 53 (45.3) | <0.001 |
| Wheelchair /bedbound | 0 | 3 (2.6) | 0.1 | 3 (3) | 16 (13.7) | 0.006 |
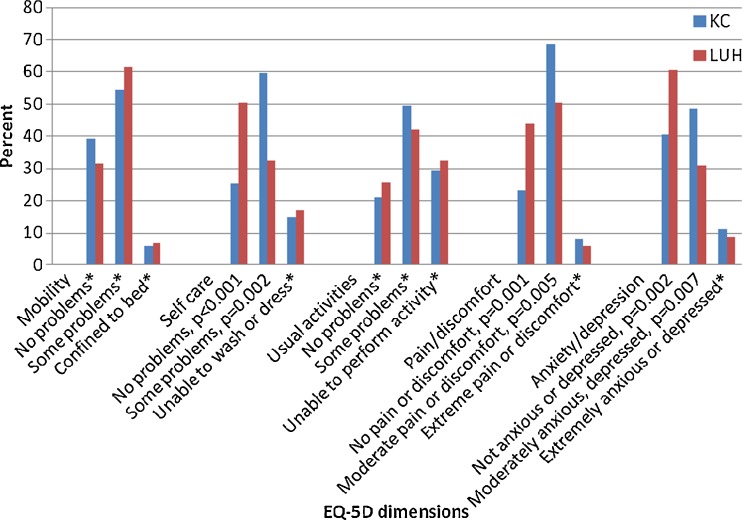
Patients in Lund reported significantly better self care, felt less pain and discomfort, and had less symptoms of anxiety and depression according EQ-5D (Fig. 2).
Fig. 2.
Comparative results of patient self reporting health status, according to the EQ-5D questionnaire between countries. *no significant difference
An additional analysis of patients rating their current health-related quality of life state (EQ VAS) at four months follow-up in Kaunas was 55 (SD 22) as compared to 69 (SD18) in Lund (p < 0.001).
In regression analysis worse mobility from EQ-5D was related to worse mobility before fracture and higher ASA grade. Sweden as country of residence, better mobility before and after the trauma and lower ASA grade significantly affected better patient self care from EQ-5D. Better rates of usual activities from EQ-5D were significantly related to Sweden as country of residence, younger age and better mobility before and after the trauma. Better rating of pain/discomfort dimension from EQ-5D was related to Sweden as country of residence and to usage of less walking aids at follow-up. Better rating of anxiety/depression from EQ-5D was significantly related to country of residence (Sweden) and better mobility at follow-up (Table 3).
Table 3.
Factors affecting quality of life according to EQ-5D (multiple linear regression analysis data)
| EQ dimensions | Variables | Regression coefficient (B) | 95 % Confidence interval | p value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Mobility | Mobility before fracture | 0.2 | 0.1 | 0.3 | <0.001 |
| ASA | 0.2 | 0.05 | 0.3 | 0.008 | |
| Self care | Country of residence | −0.5 | −0.7 | −0.4 | <0.001 |
| Mobility before fracture | 0.2 | 0.1 | 0.3 | 0.001 | |
| ASA | 0.2 | 0.1 | 0.4 | <0.001 | |
| Mobility at follow-up | 0.2 | 0.1 | 0.3 | <0.001 | |
| Usual activities | Country of residence | −0.4 | −0.6 | −0.2 | <0.001 |
| Age | 0.01 | 0.005 | 0.02 | 0.004 | |
| Mobility before fracture | 0.2 | 0.1 | 0.3 | <0.001 | |
| Mobility at follow-up | 0.3 | 0.2 | 0.3 | <0.001 | |
| Pain/discomfort | Country of residence | −0.3 | −0.4 | −0.1 | <0.001 |
| Walking aids at follow-up | 0.1 | 0.04 | 0.2 | 0.001 | |
| Anxiety/depression | Country of residence | −0.4 | −0.5 | −0.2 | <0.001 |
| Mobility at follow-up | 0.2 | 0.1 | 0.3 | <0.001 | |
Discussion
Comparing the whole group of patients admitted during the inclusion period and treated with THA in both institutions we found that the patients in Lithuania were significantly younger than those in Sweden (78 years versus 82 years). This age difference might have been related to general age differences in the population between Lithuania and Sweden. The older age in Lund might have been associated with a longer life expectancy in Sweden (79.4 for men and 83.5 for women in 2009) compared to Lithuania (67.5 for men and 78.7 for women in 2009) [9]. The older age of the patients and the possibly related higher number of leading co-morbidities might explain our finding of higher ASA scores in Lund. Furthermore, that the occurrence of FNF in Sweden in older patients suggests that the older population in Sweden either has more efficient osteoporosis management or better fall prevention for the elderly compared to patients in Lithuania.
When analysing the distribution of implant types we found that all patients in Kaunas were treated with THA compared to only 16 % of patients in Lund, whereas the remaining patients received a bipolar prosthesis. The explanation for this is that use of bipolar prostheses is not a common practice in Lithuania due to the policy of the State Patients Fund. One may suspect that the significant differences in the types of prostheses used might influence comparisons of the functional and quality of life outcomes between the two institutions. However, recent studies showed that there was no significant difference in quality of life in the short-term follow-up when bipolar or THA was implanted in patients with FNFs [10, 11].
The majority of the patients in Kaunas before and after injury were living in their own homes, whereas in Lund a significantly greater number of patients were living in social facilities. These differences related to a higher amount of well-organised service houses with a wider spectrum in Sweden [7], whereas in Lithuania there is a shortage of social care institutions for elderly people. Another influencing factor could be older mean age of the patients in Lund, whereas it is known that older age due to all co-morbidities is a risk factor for institutionalisation.
The patients in Kaunas were more mobile and used walking aids less before trauma and at the four-month follow-up compared to the patients in Lund. One possible explanation for this is that patients in the Kaunas clinics were significantly younger and had a lower ASA grade compared to the patients in LUH. Both of these factors (younger age and lower ASA grade) could explain why the patients in Lithuania had better health conditions pre-fracture and at the four-month follow up after surgery, though patients did not regain their pre-fracture functional status at four months follow-up in both institutions. This is in accord with reports that 50–75 ℅ of hip fracture patients never reaching their former functional capacity level [12–15].
We can expect that more mobile patients who are younger and have lower ASA scores rate their quality of life after treatment as being better. However, when comparing the results of the different EQ-5D dimensions at the four-month follow-up in both institutions we found the opposite case. The patients in Lund reported significantly better levels of self-care, less pain and discomfort and fewer symptoms of anxiety and depression. Mobility and the activities of daily living dimensions of the EQ-5D did not significantly differ between the countries. These findings might have been associated with differences in the self-reporting of quality of life questionnaires between the countries. Molzahn et al. assessed the HRQL of adults over 60 years of age [16]. Testing was simultaneously completed in 22 centres. The authors reported that Lithuanian people rated their quality of life as being the lowest; however, in Sweden the quality of life ratings were among the highest. This is in agreement with our regression analysis results, where country of residence was found to be the most significant factor affecting patients' self care, usual activities, pain/discomfort and anxiety/depression.
We conclude that femoral neck fracture patients in Kaunas were younger and more mobile before and at follow-up compared to the patients in Lund; however, the patients in Lund rated their quality of life higher after treatment. This could be related to the local cultures in the different countries and should be considered when such data are compared.
Acknowledgments
Conflict of interest
No competing interest declared.
References
- 1.Zuckerman JD. Hip fracture. N Engl J Med. 1996;334:1519–1525. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 2.Balen R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HJ. Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res. 2001;390:232–243. doi: 10.1097/00003086-200109000-00027. [DOI] [PubMed] [Google Scholar]
- 3.Leonardsson O, Sernbo I, Carlsson A, Akesson K, Rogmark C. Long-term follow-up of replacement compared with internal fixation for displaced femoral neck fractures: results at 10 years in a randomised study of 450 patients. J Bone Joint Surg Br. 2010;92(3):406–412. doi: 10.1302/0301-620X.92B3.23036. [DOI] [PubMed] [Google Scholar]
- 4.Thorngren K-G (1993) Experience from Sweden. In: Medical audit. Rationale and practicalities. Cambridge University Press, Cambridge, UK, pp 365–375
- 5.Hommel A. Improved safety and quality of care for patients with a hip fracture. Dissertation. Sweden: Lund University; 2007. [Google Scholar]
- 6.Thorngren KG. National registration of hip fractures. Acta Orthop. 2008;79(5):580–582. doi: 10.1080/17453670810016579. [DOI] [PubMed] [Google Scholar]
- 7.Cserháti P, Fekete K, Berglund-Rödén M, Wingstrand H, Thorngren K-G. Hip fractures in Hungary and Sweden—differences in treatment and rehabilitation. Int Orthop. 2002;26(4):222–228. doi: 10.1007/s00264-002-0349-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 9.European Commission. Demographic change in the EU. Available from: http://ec.europa.eu/social/main.jsp?catId=502&langId=en. Accessed 20 March 2012
- 10.Blomfeldt R, Törnkvist H, Eriksson K, Söderqvist A, Ponzer S, Tidermark JA. Randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br. 2007;89(2):160–165. doi: 10.1302/0301-620X.89B2.18576. [DOI] [PubMed] [Google Scholar]
- 11.Hedbeck CJ, Enocson A, Lapidus G, Blomfeldt R, Törnkvist H, Ponzer S, et al. Comparison of bipolar hemiarthroplasty with total Hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Joint Surg Am. 2011;93(5):445–450. doi: 10.2106/JBJS.J.00474. [DOI] [PubMed] [Google Scholar]
- 12.Sernbo I, Johnell O. Consequences of a hip fractures: a prospective study over 1 year. Osteoporos Int. 1993;3:148–153. doi: 10.1007/BF01623276. [DOI] [PubMed] [Google Scholar]
- 13.Stromberg L. Hip fractures in the elderly-social. Economic and psychological aspects of rehabilitation. Dissertation. Stockholm: Karolinska Instituten; 1998. [Google Scholar]
- 14.Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55(9):M498–507. doi: 10.1093/gerona/55.9.M498. [DOI] [PubMed] [Google Scholar]
- 15.Pasco JA, Sanders KM, Hoekstra FM, Henry MJ, Nicholson GC, Kotowicz MA. The human cost of fracture. Osteoporos Int. 2005;16(12):2046–2052. doi: 10.1007/s00198-005-1997-y. [DOI] [PubMed] [Google Scholar]
- 16.Molzahn AE, Kalfoss M, Schick Makaroff K, Skevington SM. Comparing the importance of different aspects of quality of life to older adults across diverse cultures. Age Ageing. 2011;40(2):192–199. doi: 10.1093/ageing/afq156. [DOI] [PubMed] [Google Scholar]