Abstract
On average participants in behavioral weight loss interventions lose 8 kilograms (kg) at 6 months, but there is marked variability in outcomes with some participants losing little or no weight. Individuals with difficulties with internal disinhibition (i.e., eating in response to emotions or thoughts) typically lose less weight in such programs and may require an innovative, specialized approach. This pilot study examined the preliminary acceptability and efficacy of a 24-week acceptance-based behavioral intervention for weight loss amongst overweight and obese adults reporting difficulty with eating in response to emotions and thoughts. Participants were 21 overweight or obese men and women (mean age=52.2±7.6 years; baseline mean body mass index=32.8±3.4). 86% completed the 6-month program and a 3-month follow-up assessment. Ratings of program satisfaction averaged 4.9 on a 5-point scale. Multilevel modeling analyses indicated participants lost an average of 12.0 kg (SE=1.4) after 6 months of treatment and 12.1 kg (SE=1.9) at 3-month follow-up, thus exceeding the weight losses typically seen in behavioral treatment programs. Decreases in internal disinhibition and weight-related experiential avoidance were found at 6-months and 3-month follow-up. Greater decreases in weight-related experiential avoidance were associated with greater weight loss at the end of the program (r=.64, p=.002), suggesting a potential mechanism of action. Although there have been a few preliminary studies using acceptance-based approaches for obesity, this is the first study to specifically target emotional overeaters, a subgroup that might be particularly responsive to this new approach. Our findings provide initial support for the feasibility, efficacy and acceptability of this approach for this subgroup of participants. Further study with longer follow-up, a more diverse sample, and comparison to a standard behavioral program is clearly warranted.
Nearly two thirds of Americans are overweight or obese and the prevalence continues to rise (Ogden et al., 2006). Excessive weight is a risk factor for significant health problems, including coronary heart disease, Type 2 diabetes, degenerative joint disease, and hypertension (Flegal, Graubard, Williamson, & Gail, 2005; NHLBI, 1998). Each year, obesity-related medical conditions are estimated to take the lives of 365,000 Americans and cost our country an estimated $75 billion dollars (Finkelstein, Fiebelkorn, & Wang, 2004).
The treatment of choice for overweight and moderately obese individuals is behavioral weight control. Behavioral treatments focus on changing diet and physical activity behaviors in order to produce weight loss. On average, participants lose about 8 kg at the end of 6 months of treatment, resulting in significant health improvements (Diabetes Prevention Program Research Group, 2002; Look AHEAD Research Group, 2007). However, there is considerable variability in initial weight losses, with some participants losing greater than 10% of initial body weight and others losing little or even gaining weight.
One issue that may contribute to the variability in outcomes is the failure of standard behavioral weight loss programs to adequately address internal antecedents for eating and exercise behaviors (e.g., eating in response to negative emotions). Internal disinhibition has been defined as a tendency to eat in response to thoughts and feelings (Niemeier, Phelan, Fava, & Wing, 2007). Previous studies have shown that individuals who report high levels of internal disinhibition are less successful at losing weight or keeping it off than other participants in these programs (Butryn, Thomas, & Lowe, 2009; Niemeier et al., 2007). It is therefore important to develop more tailored treatment approaches that can better address the needs of these individuals who have problems with overeating in response to emotional or cognitive cues.
Standard behavioral weight loss programs include only two to three sessions addressing overeating in response to emotions and thoughts. Participants are taught to control these thoughts and feelings with techniques such as cognitive restructuring, distraction, and refocusing strategies. A recent analogue study suggested that these control strategies may actually make it more difficult to cope with food cravings and lead to greater consumption of craved foods, whereas acceptance-based strategies were found to lead to better outcomes (e.g., less consumption) in those most susceptible to food cravings (Forman, Hoffman, et al., 2007).
Acceptance-based strategies form the basis of a new generation of therapies (“Third Wave”) that include Acceptance and Commitment Therapy (ACT), Mindfulness-based Cognitive Therapy, and Dialectical Behavior Therapy (DBT). These approaches have shifted the focus from changing internal thoughts and feelings to accepting these thoughts and feelings to thereby promote behavior that is consistent with personal values and life goals. Third generation approaches have been used successfully in a variety of different areas, including depression, generalized anxiety, epilepsy, posttraumatic stress disorder, pain management, and smoking cessation (Brown et al., 2008; Forman, Herbert, Moitra, Yeomans, & Geller, 2007; Lundgren, Dahl, Melin, & Kies, 2006; McCracken, Vowles, & Eccleston, 2005; Orsillo & Batten, 2005; Vowles & McCracken, 2008; Woods, Wetterneck, & Flessner, 2006). Several third generation approaches have been successfully applied to eating and weight-related disorders, including both mindfulness-based eating awareness training (MB-EAT) and DBT for binge eating disorder (Kristeller & Wolever, 2011; Telch, Agras, & Linehan, 2001) and ACT for diabetes management (Gregg, Callaghan, Hayes, & Glenn-Lawson, 2007).
Three studies have applied ACT-based approaches to the management of obesity specifically (Forman, Butryn, Hoffman, & Herbert, 2009; Lillis, Hayes, Bunting, & Masuda, 2009; Tapper et al., 2009). Lillis and colleagues examined the effect of ACT on maintenance of weight loss. They randomly assigned 84 overweight individuals who had lost weight within the past 2 years to a waiting list control group or to attend a 1-day mindfulness and acceptance-based workshop targeting obesity-related stigma and psychological distress. At 3-month follow-up, on average ACT participants had lost an additional 1.6% of their body weight whereas the control group gained .3%. Moreover, 35% of participants in ACT lost 2.3 kg or more, compared to 11% in the control group. Using a similar workshop-based approach, Tapper et al. (2009) randomly assigned 62 women who were attempting to lose weight to attend four 2-hour ACT-based workshops (delivered weekly for 3 weeks with the final workshop at 3 months) or a control condition that continued with their normal diets. At 6-months, workshop participants reported engaging in significantly more physical activity than control participants; weight loss findings revealed a trend for more weight loss in the ACT group with a difference of 1.35 kg. Interestingly, neither of these workshop-based treatment approaches integrated specific weight loss techniques with ACT content; both were designed to complement participants’ own weight loss efforts by teaching ACT strategies.
A recent uncontrolled trial of an integrated ACT-based behavioral weight loss program suggested positive effects of a more intensive ACT approach. Forman et al. (2009) conducted a 12-week weight loss trial with 29 overweight/obese women. Weight losses among completers averaged 6.6% of body weight at post-treatment and 9.6% at 6 month follow-up; however there was a high level of attrition in this study (52% at 6 months), making it difficult to evaluate these effects and raising questions about the acceptability of this approach. Although this pilot suggested that the ACT approach had successfully modified emotional eating and eating-linked emotional acceptance and these changes were related to the weight loss outcomes, this study included a general sample of overweight/obese women, and did not specifically target women who reported problems with emotional overeating. Unpublished preliminary data were reported recently by Forman and colleagues (2010) from a randomized controlled trial comparing their acceptance-based behavioral weight loss to standard behavioral weight loss treatment. At 40 weeks, they report 13.6% weight loss in the acceptance-based group vs. 9.8% in the standard group (Forman et al., 2010).
As noted above, these prior studies of ACT-based strategies have used these for the general population of overweight/obese individuals. However, ACT-based strategies may be particularly helpful for obese individuals who report problems overeating in response to thoughts and emotions for several reasons (Forman et al., 2009). First, ACT teaches people to “accept” (i.e. be mindful of and tolerate) internal states, such as hunger, negative affect, and fatigue after exercise, which are particularly problematic for this subgroup. The extent to which people accept these internal experiences versus the extent to which they try to avoid such experiences (i.e., engage in experiential avoidance), has been shown to predict binge eating (Telch et al., 2001), alcohol abuse (Brown, Evans, Miller, Burgess, & Mueller, 1997), and smoking (Brown, Lejuez, Kahler, & Strong, 2002). Second, ACT recognizes that ongoing adherence to a behavior that increases distress will occur only if an individual has committed to life goals that justify the distress (Forman et al., 2009). ACT focuses on the identification and internalization of values and life goals and lasting commitment to behaviors that are consonant with these life goals. Finally, ACT stresses mindfulness and awareness, and thus may help patients remain aware of their weight loss goals and their eating in the face of emotional and environmental cues that could otherwise lead to “mindless” eating.
The purpose of the present pilot study was to develop an acceptance-based behavioral weight loss intervention and test its preliminary acceptability and efficacy in overweight and obese individuals reporting high levels of internal disinhibition (eating in response to emotional or cognitive cues). This pilot study expands on the ACT-based weight loss studies to date in several important ways. First, acceptance and commitment strategies were fully integrated with behavioral weight loss strategies unlike the workshop-based approaches of Lillis et al. (2009) and Tapper et al. (2009). In addition, treatment was provided weekly for 6-months, a timeframe comparable to the weight loss phases of standard behavioral weight loss approaches (Diabetes Prevention Program Research Group, 2002; Look AHEAD Research Group, 2007). Finally, this study is the first to apply this approach specifically to individuals who endorse difficulty with eating in response to emotional and cognitive cues, a subgroup within the obese population that may be particularly likely to benefit from an enhanced approach to emotional eating. The primary aim of this pilot study was to assess changes in weight and psychological variables over the 6-month treatment program, and 3-month follow-up. Secondary aims were to examine the acceptability of the program and to explore the relationship between changes in psychological variables and weight changes to identify potential mechanisms of action of the treatment.
Method
Participants
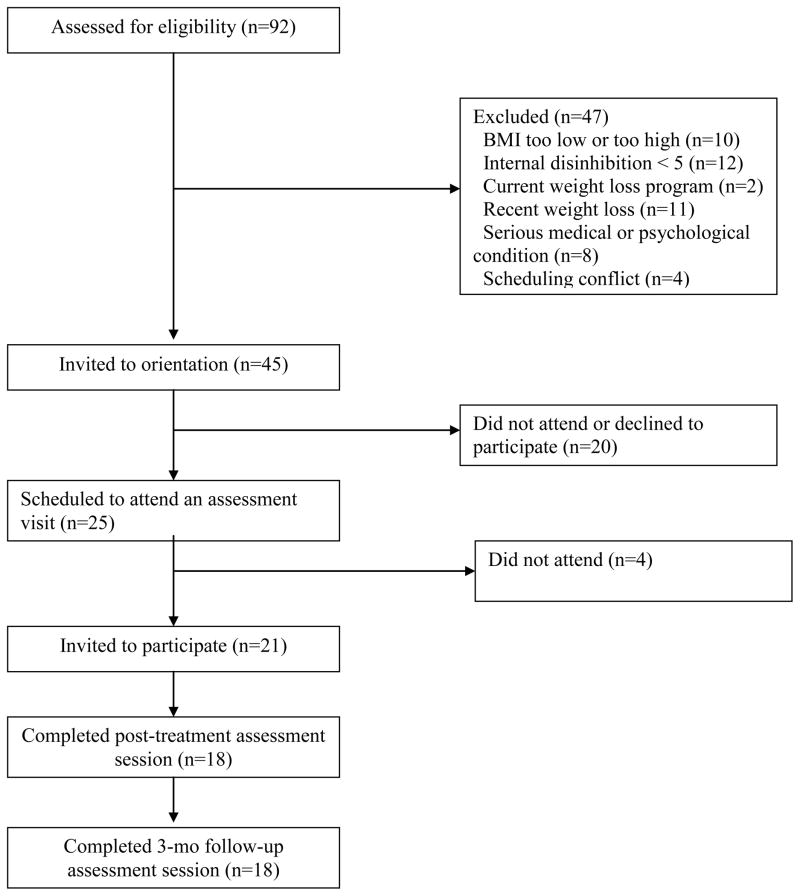
Participants were recruited via newspaper advertisements that sought individuals interested in weight loss who also have trouble controlling their eating when stressed. Potential participants were screened by phone and then in person to determine eligibility. Eligibility criteria included age between 21 and 70 years, body mass index (BMI) between 27 and 40 kg/m2 and a score of 5 or greater on the Internal Disinhibition subscale of the Eating Inventory (scores on this subscale range from 0–8). This cut-off was selected based on analyses of data from two behavioral weight loss trials where participants scoring 5 or greater on internal disinhibition at baseline lost significantly less weight over the course of 18 months than those scoring under 5 (4.8 kg vs. 7.6 kg, p=.015; Wing, 2010). In a prior behavioral weight loss trial the mean score on the internal disinhibition subscale was 4.2 (SD=2.4) (Niemeier et al., 2007). Participants were excluded for the following: current participation in a weight loss program, recent weight loss, pregnancy, serious medical conditions (e.g., heart attack or stroke), serious psychological disorders (e.g., bipolar disorder, schizophrenia, or eating disorder), or a planned move (see Figure 1). Participants who reported medical conditions that may interfere with their ability to safely complete the intervention or engage in regular physical activity were required to obtain written permission from their physician. All participants provided written informed consent to participate and all study procedures were approved by a local Institutional Review Board.
Figure 1.
Participant enrollment and retention.
Design
Given the preliminary nature of this study, a single group design was used. Participants were recruited in 2 cohorts of 10 or 11 participants and received a 24-week group intervention that incorporated both standard behavioral weight control strategies and acceptance-based components. Assessments were held at baseline, at the end of the 6-month treatment, and after a 3-month period with no treatment contact. Participants were compensated twenty dollars at the 6-month assessment and at the 3-month follow-up.
Acceptance-based behavioral intervention (ABBI) treatment components
A manualized treatment that incorporated acceptance-based approaches and standard behavioral techniques was used throughout the intervention. Interventionists were a PhD-level clinical psychologist, a clinical psychology intern, and a masters-level nurse with expertise in behavioral weight loss. All sessions were audiotaped and KPR provided feedback to interventionists regarding adherence to acceptance-based principles. The program included weekly 1-hour meetings for 6 months, with a private weigh-in at each session.
Behavioral components
Participants were taught the core components of behavioral weight loss, including standard diet and exercise prescriptions for weight loss (i.e. 1200–1500 kcal/day; less than 25% of calories from fat; gradual increase in physical activity from 10 to 40 minutes on 5 days per week); self-monitoring; stimulus control; problem solving; assertiveness training; goal setting; and relapse prevention (Look AHEAD Research Group, 2007).
Acceptance-based components
Standard behavioral weight loss interventions promote changing maladaptive thoughts and emotions and spend few sessions covering this material. In contrast, ABBI used acceptance-based strategies to address negative thoughts and emotions throughout the entire treatment, including during the delivery of standard behavioral techniques. While change-focused strategies (e.g., stimulus control) were encouraged for coping with the external environment, the following acceptance-based strategies were taught to help participants cope with internal experiences (e.g., thoughts, emotions): (1) Values work was done to help participants identify how their eating and activity behaviors fit with their core values. The purpose of values work is to ultimately give participants greater life satisfaction by reducing maladaptive, ineffective behaviors (e.g., eating in response to emotions) that are inconsistent with life values and increasing behaviors that are congruent with valued living (e.g., healthful eating and regular physical activity); (2) Acceptance techniques were used to teach participants to notice (i.e. be mindful of) and tolerate sensations associated with unpleasant thoughts and feelings without attempting to change or avoid them by engaging in ineffective coping strategies; (3) Cognitive Defusion skills were promoted to help participants experience their thoughts and feelings from a psychological distance recognizing them as a product of their minds that do not necessarily need to be acted on. The purpose of this work was to enable participants to recognize that while unpleasant thoughts and feelings appear threatening and intolerable, they are merely uncomfortable experiences that can be tolerated if perceived as transient and only a small aspect of their current experience; and (4) Committed Action strategies were used to encourage participants to focus on their unique values during heightened distress and discomfort in an effort to promote behavioral persistence and valued living.
Combining behavioral and acceptance-based approaches
While behavioral skills and goals (e.g., self-monitoring; problem-solving) in the acceptance-based intervention were the same as those taught in standard behavioral interventions, the methods by which participants developed and learned the skills were quite different. In ABBI, each behavioral skill was taught in the context of how it may relate to thoughts and emotions and ultimately valued living. For example, in problem-solving barriers to accurate food monitoring, an essential component of behavioral weight loss, discussion centered around specific thoughts and feelings that may lead participants not to complete their food diary (e.g., feelings of shame that were avoided by not disclosing consumption). In this way, coping with thoughts and emotions were interwoven throughout the entire treatment as opposed to being addressed in particular sessions. Similarly, acceptance-based skills learned in early lessons, such as mindfulness and defusion, were continually built upon and consistently revisited in later lessons.
Assessments
Assessments were conducted at baseline, after the 6-month treatment, and after 3-months of no treatment. Assessments were completed by non-interventionist staff.
Demographics
Participants reported basic demographic information (e.g., age, race/ethnicity).
Weight, height, and BMI
Participants’ weight was measured to the nearest 0.1 kg using a digital scale and height was measured to the nearest millimeter with a stadiometer. Participants were measured wearing light indoor clothing without shoes. BMI was calculated using the formula weight in kilograms/height in meters2.
Disinhibition
The Eating Inventory (EI; Stunkard & Messick, 1985) is a widely used measure of eating behavior that includes three subscales, cognitive restraint, disinhibition, and hunger. Previous research has shown that the disinhibition scale includes two subscales, internal and external disinhibition (Niemeier et al., 2007). The internal disinhibition subscale (e.g., “When I feel blue, I overeat”) was shown to predict weight loss and maintenance, whereas scores on the external subscale (e.g., “I usually eat too much at social occasions, like parties and picnics”) were not related to outcome. As noted above, scores of ≥5 on the Internal subscale of the EI were required for eligibility for the study. This instrument was also used to examine changes in disinhibition over the course of the treatment and was thus administered at baseline, 6-month assessment, and 3-month follow-up. Higher scores indicate higher levels of the measured construct. The EI has demonstrated adequate internal consistency and test-retest reliability (Stunkard & Messick, 1988). Changes in all subscales have been seen in many prior weight loss studies (Karlsson, Persson, Sjostrom, & Sullivan, 2000; Klem, Wing, McGuire, Seagle, & Hill, 1998).
Experiential Avoidance and Inflexibility: Weight-focused
The Acceptance and Action Questionnaire for Weight-Related Difficulties (AAQW; Lillis & Hayes, 2008) is a 22-item questionnaire designed to assess experiential avoidance and psychological inflexibility specifically as it relates to body weight, food and eating. Participants indicate how true various statements are for them (e.g., “I need to get rid of my eating urges to eat better”) on a scale fromNever (1) to Always True (7). Higher scores indicate greater weight-related experiential avoidance.
Distress Tolerance
The Distress Tolerance Scale (DTS; Simons & Gaher, 2005) is a 15-item scale that measures affective distress tolerance. This scale produces an overall score that assesses difficulties with distress tolerance and has been shown to have good internal consistency and test-retest reliability (Simons & Gaher, 2005). Higher scores indicate lower distress tolerance.
Treatment acceptability
At follow-up, participants were asked to rate how helpful the program was at modifying the way they cope with emotions and thoughts and developing awareness of how and why they eat. They were also asked more general questions regarding the program including overall utility, satisfaction, whether they would recommend the program to a friend, and how this program compares to other weight loss programs they have tried. Each item is rated on a 5-point Likert scale; higher scores indicate greater program favorability.
Statistical analyses
The Statistical Analysis Software, Version 9.2 (SAS) was used for all analyses. Descriptive statistics were calculated to examine participant characteristics and treatment acceptability items. The Proc MIXED procedure within SAS 9.2 for Windows was used for all multilevel modeling (MLM) analyses of primary outcome variables to examine changes over time. The MLM models were fit with an autoregressive covariance structure using all available data from each assessment. Planned pairwise comparisons from pre to post-treatment, pre-treatment to 3-month follow-up, and post-treatment to 3-month follow-up were conducted using least square mean difference (LSMD) estimates with Bonferroni-adjusted p-values and adjusted 95% confidence intervals (CI). Simple correlations were conducted to examine the association between weight change and change in targeted process variables.
Results
The 21 participants (19 females; 2 males) who entered the trial were age 52.2 ± 7.6 years, with a BMI of 32.8 ± 3.4 and body weight of 88.8 ± 11.2 kg. Ninety percent reported that they were non-Hispanic White, 4.8% Hispanic, and 4.8% other. Eighteen of 21 participants (86%) completed the 6-month assessment and 3-month follow-up. There were no baseline differences between completers and non-completers on demographic characteristics (gender, education, racial/ethnic background) or outcome variables (BMI, psychological variables). Participants attended an average of 20.5 ± 4.8 of the 24 sessions (86% of sessions).
ABBI was associated with significant weight loss outcomes, measured in kilograms of body weight, with a significant effect across time (F(2, 25.1)=37.7, p<0.0001). The majority of weight loss occurred between baseline and 6 months (LSMD estimate = −12.0kg, SE=1.4, adjusted 95% CI = −15.5 to −8.5). At their 3-month follow-up session, participants maintained their weight losses from baseline (LSMD estimate = −12.1kg, SE=1.9, adjusted 95% CI = −16.9 to −7.4), with no difference in weight change between 6-month assessment and 3-month follow-up (LSMD estimate = −0.1kg, SE=1.4, adjusted 95% CI = −3.7 to 3.4). BMI also significantly decreased over time (F(2, 34.1)=40.0, p<.0001) with a similar pattern of change as weight loss (see Table 1).
Table 1.
The effects across time of ABBI on body weight, BMI and psychological variables with least square mean estimates and differences, standard errors, Bonferroni-adjusted pairwise difference test p-values, and adjusted 95% confidence intervals for the difference estimates
| Variable | Baseline (SE) | Post-treatment difference (SE) and (adj 95% CI) | p-value | 3-month follow-up difference (SE) and (adj 95% CI) | p-value | Post to 3-month difference (SE) and (adj 95% CI) |
|---|---|---|---|---|---|---|
| Weight (kg) | 88.8 (2.3) | −12.0 (1.4) (−15.5, −8.5) | <.0001 | −12.1 (1.9) (−16.9, −7.4) | <.0001 | −0.1* (1.4) (−3.7, 3.4) |
| BMI (kg/m2) | 32.8 (0.8) | −4.4 (0.5) (−5.6, −3.1) | <.0001 | −4.4 (0.7) (−6.1, −2.8) | <.0001 | −0.1 * (0.5) (−1.3, 1.2) |
| Disinhibition (Total) | 12.3 (0.8) | −4.6 (0.6) (−6.2, −3.0) | <.0001 | −4.5 (0.8) (−6.6, −2.4) | <.0001 | 0.1* (0.7) (−1.6, 1.7) |
| Internal Disinhibition | 6.0 (0.5) | −2.6 (0.4) (−3.6, −1.6) | <.0001 | −2.1 (0.5) (−3.4, −0.8) | .0014 | 0.5* (0.4) (−0.6, 1.5) |
| External Disinhibition | 4.3 (0.4) | −1.7 (0.3) (−2.5, −1.0) | <.0001 | −2.2 (0.4) (−3.2, −1.1) | <.0001 | −0.4* (0.3) (−1.2, 0.4) |
| Restraint | 10.4 (0.7) | 6.7 (.7) (4.8, 8.6) | <.0001 | 6.0 (.7) (4.2, 7.9) | <.0001 | −0.7* (0.8) (−2.7, 1.2) |
| Hunger | 7.2 (0.8) | −3.5 (0.5) (−4.7, −2.2) | <.0001 | −3.8 (0.6) (−5.4, −2.2) | <.0001 | −0.3* (0.5) (−1.6, 0.9) |
| Experiential Avoidance and Inflexibility (AAQ-W) | 67.0 (3.1) | −16.8 (2.8) (−23.9, −9.6) | <.0001 | −16.2 (3.7) (−25.6, −6.8) | .0004 | 0.5* (3.0) (−7.0, 8.1) |
| Distress Tolerance Difficulties | 4.2 (0.1) | −0.1 (0.1) (−0.5, 0.1) | .9040 | −0.2 (0.1) (−0.6, 0.1) | .3531 | −0.1* (0.1) (−0.4, 0.2) |
All post-treatment to 3-month follow-up differences were not significant (Bonferroni-adjusted p>.56).
ABBI was also associated with improvements across time on several psychological measures. These variables included both internal disinhibition (F(2, 26.5)=21.3, p<.0001) and external disinhibition (F(2, 37.1)=17.9, p<.0001). As shown in Table 1, participants reported significant decreases in internal disinhibition from baseline to both 6 months (LSMD estimate = −2.6, SE=0.4, adjusted 95% CI = −3.6 to −1.6) and 3-month follow-up (LSMD estimate = −2.1, SE=0.5, adjusted 95% CI = −3.4 to −0.8) with no difference between 6 months and 3-month follow-up (LSMD estimate = 0.5, SE=0.4, adjusted 95% CI = −0.6 to 1.5). Changes in external disinhibition followed a similar pattern. Distress tolerance did not change significantly over time (F(2, 32.7)=1.3, p=.29). Weight-related experiential avoidance and psychological inflexibility decreased significantly over time (F(2, 32.5)=18.0, p<.0001) with changes from baseline to 6-month assessment (LSMD estimate = −16.8, SE=2.8, adjusted 95% CI = −23.9 to −9.6) and maintenance of reductions at 3-month follow-up (LSMD estimate = −16.2, SE=3.7, adjusted 95% CI = −25.6 to −6.8) with no change between 6-month assessment and 3-month follow-up (LSMD estimate = 0.5, SE=3.0, adjusted 95% CI = −7.0 to 8.1).
An examination of the relationship between process variables and weight change revealed a relationship between change in weight- and eating-focused experiential avoidance and psychological inflexibility and change in weight at both post-treatment (r=.64, p=.002) and 3-month follow-up (r = .62, p=.003). There were no significant relationships between change in internal or external disinhibition and distress tolerance and change in weight.
Participants rated the program very highly. Mean ratings of program satisfaction (4.9 ± 0.2), willingness to recommend the program to a friend (5.0 ± 0.0), overall utility (4.9 ± 0.2), and favorability of the program relative to others (4.8 ± 0.4) all approached the maximum level of 5.0. Participants reported that the intervention was effective at modifying the way they cope with emotions (4.4 ± 0.8) and thoughts (4.3 ± 0.6) and increasing their awareness of how and why they eat (4.8 ± 0.5).
Discussion
This study piloted the use of an acceptance-based behavioral weight loss intervention, evaluating its acceptability, feasibility, and initial effectiveness in individuals reporting high levels of internal disinhibition, or tendency to eat in response to emotional or cognitive cues. High levels of internal disinhibition have been associated with difficulty with both initial weight loss and weight loss maintenance and may contribute to the high level of variability in outcome of standard behavioral weight loss programs (Butryn et al., 2009; Niemeier et al., 2007). The treatment developed for this study targeted emotional and cognitive triggers for unhealthy weight control behaviors through the use of acceptance-based skills including cognitive defusion, mindfulness, values internalization and committed action. Although there have been several recent studies applying acceptance-based strategies to the problem of weight loss or weight loss maintenance, this is the first study to incorporate these strategies in a weight loss program designed specifically for emotional overeaters.
This innovative approach yielded impressive weight loss results. Multilevel modeling analyses indicated a mean weight loss of 12.0 kg (SE 1.4) at post-treatment. Standard 6-month behavioral weight loss programs achieve average weight losses of approximately 8-kg at the end of active treatment (Wing, 2004). Given that individuals with high levels of internal disinhibition typically achieve lower than average weight losses in standard programs (Butryn et al., 2009; Wing, 2010), the fact that participants in this acceptance-based intervention not only met but exceeded an 8-kg weight loss is impressive. In addition, weight regain following cessation of treatment is a common problem in standard behavioral weight loss programs (Wing, 2004); participants in this study maintained their weight loss (12.1 kg (SE=1.9)) at the 3-month follow-up with no contact between post-treatment and follow-up. These weight loss results also compared favorably with results from other acceptance-based weight loss interventions. Forman et al. (2009) examined the effectiveness of a 12-week acceptance-based weight loss program and reported 6.2 kg weight loss at posttreatment and 8.5 kg at 6-month follow-up in their completer analysis. Besides being shorter in treatment duration, Forman et al. recruited and treated participants at their worksite and had a significantly more diverse sample than the present study which may account for the difference in weight loss findings. Another important difference between this study and Forman and colleagues’ pilot and ongoing randomized controlled trial is our targeting of individuals high in internal disinhibition at baseline. The Forman et al. pilot study reported significant attrition (52% at 6-months) whereas 86% of participants completed this study. The high level of attrition in the Forman et al. study may suggest that acceptability of an acceptance-based approach is improved by targeting the treatment to those who have difficulties with eating in response to thoughts and feelings. Our completion rate is comparable to weight loss trials of a similar length using standard overweight populations (e.g., Subak et al., 2009; Wadden et al., 2005). The strong weight loss results found in our pilot suggest that using an acceptance-based approach may greatly enhance outcomes for the subgroup of individuals who report high levels of eating in response to internal cues.
This acceptance-based intervention also had significant effects on the psychological outcomes. Internal disinhibition decreased from baseline to 6-months and effects were maintained at 3-month follow-up. Our acceptance-based approach specifically targeted experiential avoidance as related to eating and weight. As anticipated, there was a significant decrease in weight-related experiential avoidance and psychological inflexibility from pre to post-treatment. In addition, these changes were associated with changes in weight in this study. These findings are consistent with previous research. Forman et al. (2009) found significant decreases in disinhibition and increases in food-related experiential acceptance, mindfulness and motivation. In their study, food-related experiential acceptance was associated with weight loss outcome. Because in both of these studies, measurement of change in experiential avoidance and change in weight were concomitant, no causal inferences can be drawn. However, taken together, these findings provide strong support for applying acceptance-based approaches to the treatment of eating in response to emotional and cognitive triggers.
Finally, it is important to note the high level of satisfaction that participants expressed with this novel approach. Participants indicated that the acceptance-based intervention was highly effective at helping them cope with thoughts and feelings related to weight control and increased their awareness of how and why they eat. These results suggest that this novel approach to behavioral weight loss was extremely well received by participants and increased their perceived ability to cope with uncomfortable internal states.
This study has some limitations. There was no standard care control group, limiting our ability to draw conclusions about the effectiveness of this novel approach relative to traditional behavioral weight loss treatments. However, our participants achieved 12 kg (or 13% of original body weight) weight loss on average, suggesting that this approach is extremely promising for improving weight loss outcomes among a population that typically struggles in standard programs. The sample was also primarily Caucasian, and predominantly female which limits generalizability of our findings. In addition, while weight losses were maintained over a 3-month untreated follow-up period, a much longer follow-up period would be needed in order to determine whether weight losses would be maintained long-term.
Despite these limitations, this preliminary effectiveness study provides strong support that a sizable subgroup of individuals who report significant problems with internal disinhibition may benefit substantially from an acceptance-based behavioral weight loss intervention that targets increasing adaptive coping skills. The weight losses achieved compare favorably with outcomes reported in both standard weight loss programs and a prior study using an acceptance-based approach. In addition, study strengths include a high completion rate and a 3-month untreated follow-up period showing maintenance of weight loss.
Our findings preliminarily suggest that targeting this subpopulation that achieves suboptimal weight loss in standard interventions using acceptance-based treatment may enhance overall weight loss outcomes in behavioral programs and provide a substantial benefit to the treatment of obesity. Further research that compares this acceptance-based approach to standard behavioral weight loss intervention in the context of a randomized controlled trial with an extended follow-up period and more diverse sample is warranted.
Highlights.
We tested the efficacy of an acceptance-based behavioral weight loss intervention.
Participants were overweight and reported internal disinhibition.
Average weight loss at 6-months was 12 kg and it was maintained at 3-month follow up.
Acceptance-based approaches to weight loss warrant further study.
Acknowledgments
The authors would like to thank Rheanna Ata, Jacki Hecht, RN, Erica Robichaud, MSW, RD, and Victoria Winn for their invaluable assistance on this project.
This research was supported by grant 5K23-DK73536 from the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Heather M. Niemeier, Email: niemeieh@uww.edu.
Tricia Leahey, Email: tleahey@lifespan.org.
Kathleen Palm Reed, Email: kpalm@clarku.edu.
Richard A. Brown, Email: Richard_Brown@Brown.edu.
Rena R. Wing, Email: rwing@lifespan.org.
References
- Brown RA, Evans DM, Miller IW, Burgess ES, Mueller TI. Cognitive-behavioral treatment for depression in alcoholism. Journal of Consulting and Clinical Psychology. 1997;65(5):715–726. doi: 10.1037//0022-006x.65.5.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;111(1):180–185. [PubMed] [Google Scholar]
- Brown RA, Palm KM, Strong DR, Lejuez CW, Kahler CW, Zvolensky MJ, et al. Distress tolerance treatment for early-lapse smokers: rationale, program description, and preliminary findings. Behavior Modification. 2008;32(3):302–332. doi: 10.1177/0145445507309024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butryn ML, Thomas JG, Lowe MR. Reductions in internal disinhibition during weight loss predict better weight loss maintenance. Obesity. 2009;17(5):1101–1103. doi: 10.1038/oby.2008.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein EA, Fiebelkorn IC, Wang G. State-level estimates of annual medical expenditures attributable to obesity. Obesity Research. 2004;12(1):18–24. doi: 10.1038/oby.2004.4. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. Journal of the American Medical Association. 2005;293(15):1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- Forman EM, Butryn ML, Hoffman KL, Herbert JD. An open trial of an acceptance-based behavioral intervention for weight loss. Cognitive and Behavior Practice. 2009;16:223–235. [Google Scholar]
- Forman EM, Butryn ML, Shaw JA, Glassman LH, Clark VL, Belmont A, et al. Preliminary outcomes from the Mind Your Health project: A randomized controlled trial comparing standard behavioral and acceptance-based behavioral interventions for obesity. Paper presented at the 44th annual convention of the Association for Behavioral and Cognitive Therapies; San Francisco, CA. 2010. [Google Scholar]
- Forman EM, Herbert JD, Moitra E, Yeomans PD, Geller PA. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification. 2007;31(6):772–799. doi: 10.1177/0145445507302202. [DOI] [PubMed] [Google Scholar]
- Forman EM, Hoffman KL, McGrath KB, Herbert JD, Brandsma LL, Lowe MR. A comparison of acceptance- and control-based strategies for coping with food cravings: an analog study. Behaviour Research and Therapy. 2007;45(10):2372–2386. doi: 10.1016/j.brat.2007.04.004. [DOI] [PubMed] [Google Scholar]
- Gregg JA, Callaghan GM, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2007;75(2):336–343. doi: 10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- Karlsson J, Persson LO, Sjostrom L, Sullivan M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. International Journal of Obesity and Related Metabolic Disorders. 2000;24(12):1715–1725. doi: 10.1038/sj.ijo.0801442. [DOI] [PubMed] [Google Scholar]
- Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. Psychological symptoms in individuals successful at long-term maintenance of weight loss. Health Psychology. 1998;17(4):336–345. doi: 10.1037//0278-6133.17.4.336. [DOI] [PubMed] [Google Scholar]
- Kristeller JL, Wolever RQ. Mindfulness-based eating awareness training for treating binge eating disorder: the conceptual foundation. Eating Disordors. 2011;19(1):49–61. doi: 10.1080/10640266.2011.533605. [DOI] [PubMed] [Google Scholar]
- Lillis J, Hayes SC. Measuring avoidance and inflexibility in weight related problems. International Journal of Behavioral Consultation and Therapy. 2008;4:30–40. [Google Scholar]
- Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: a preliminary test of a theoretical model. Annals of Behavioral Medicine. 2009;37(1):58–69. doi: 10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]
- Look AHEAD Research Group. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007;30(6):1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundgren T, Dahl J, Melin L, Kies B. Evaluation of acceptance and commitment therapy for drug refractory epilepsy: a randomized controlled trial in South Africa--a pilot study. Epilepsia. 2006;47(12):2173–2179. doi: 10.1111/j.1528-1167.2006.00892.x. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Vowles KE, Eccleston C. Acceptance-based treatment for persons with complex, long standing chronic pain: a preliminary analysis of treatment outcome in comparison to a waiting phase. Behaviour Research and Therapy. 2005;43(10):1335–1346. doi: 10.1016/j.brat.2004.10.003. [DOI] [PubMed] [Google Scholar]
- NHLBI. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Obesity Research. 1998;6:51S–210S. [PubMed] [Google Scholar]
- Niemeier HM, Phelan S, Fava JL, Wing RR. Internal disinhibition predicts weight regain following weight loss and weight loss maintenance. Obesity. 2007;15(10):2485–2494. doi: 10.1038/oby.2007.295. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of the American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Orsillo SM, Batten SV. Acceptance and commitment therapy in the treatment of posttraumatic stress disorder. Behavior Modification. 2005;29(1):95–129. doi: 10.1177/0145445504270876. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29(2):83–102. [Google Scholar]
- Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Messick S. Eating Inventory Manual. San Antonio, TX: Psychological Corporation; 1988. [Google Scholar]
- Subak LL, Wing R, West DS, Franklin F, Vittinghoff E, Creasman JM, et al. Weight loss to treat urinary incontinence in overweight and obese women. New England Journal of Medicine. 2009;360(5):481–490. doi: 10.1056/NEJMoa0806375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, Moore L. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite. 2009;52(2):396–404. doi: 10.1016/j.appet.2008.11.012. [DOI] [PubMed] [Google Scholar]
- Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69:1061–1065. doi: 10.1037//0022-006x.69.6.1061. [DOI] [PubMed] [Google Scholar]
- Vowles KE, McCracken LM. Acceptance and values-based action in chronic pain: a study of treatment effectiveness and process. Journal of Consulting and Clinical Psychology. 2008;76(3):397–407. doi: 10.1037/0022-006X.76.3.397. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Berkowitz RI, Womble LG, Sarwer DB, Phelan S, Cato RK, et al. Randomized trial of lifestyle modification and pharmacotherapy for obesity. New England Journal of Medicine. 2005;353(20):2111–2120. doi: 10.1056/NEJMoa050156. [DOI] [PubMed] [Google Scholar]
- Wing RR. Behavioral approaches to the treatment of obesity. In: Bray G, Bouchard C, editors. Handbook of Obesity. 2. New York, NY: Macel Dekker, Inc; 2004. [Google Scholar]
- Wing RR. Unpublished raw data. 2010. Internal disinhibition upon entry to a behavioral weight loss program predicts weight loss. [Google Scholar]
- Woods DW, Wetterneck CT, Flessner CA. A controlled evaluation of acceptance and commitment therapy plus habit reversal for trichotillomania. Behaviour Research and Therapy. 2006;44(5):639–656. doi: 10.1016/j.brat.2005.05.006. [DOI] [PubMed] [Google Scholar]