Abstract
It has become increasingly more evident that the meniscus plays an important role in contributing to knee joint longevity. Advances in surgical techniques by orthopaedic surgeons to repair traumatized menisci have led to better long term outcomes, decreasing the incidence of articular cartilage degeneration. Advances have also been made in rehabilitative techniques following meniscal repair. These techniques along with sound rehabilitation principles to include a criteria based progression have contributed to excellent outcomes and earlier return to function and sport. The role of the meniscus, recent advances in surgical repair and the current post-operative rehabilitation techniques employed by sports rehabilitation specialists today are discussed.
Keywords: Knee, Meniscus, Surgery, Rehabilitation
Introduction
The population, in general has become more athletically active and individuals are staying active longer. Meniscal injuries have become very common among professional and amateur athletes and are one of the most common indications for knee surgery [1].
Although the incidence of meniscal pathology is difficult to estimate, the increased exposure to athletic activity increases the risk of injury to these structures. Hede and coworkers [2], reported the mean annual incidence of meniscus tears as 9.0 in males and 4.2 in females per 10,000 inhabitants. Tears were found to be more common in the third, fourth and fifth decades of life.
It has become more and more clearer in recent decades that meniscal excision leads to articular cartilage degeneration [3–5]. Degenerative changes have been found to be directly proportional to the amount of meniscus removed [6]. Even partial meniscectomy results in higher than normal stress on the underlying articular cartilage [6–10]. An vitro study by Seedhom and Hargreaves demonstrated that removal of 16% to 34% of the meniscus resulted in a 350% increase in contact forces [10].
Therefore it has been generally recognized that the amount of meniscal tissue removed should be minimized, repaired or replaced [7–9]. This article will focus on the current treatment strategies employed in the rehabilitation of individuals who have undergone a meniscal repair procedure.
Basic science
Meniscal cartilage plays a crucial role in the function and biomechanics of the knee joint. The meniscus functions in load bearing, load transmission, shock absorption, joint stability, joint lubrication, and joint congruity [11–13].
The knee menisci (medial and lateral) are wedge-shaped semilunar disks made of fibrocartilage interposed between the tibia and the condyles of the femur. The lateral meniscus is O-shaped while the medial meniscus is C-shaped with a larger posterior horn.
The menisci are attached to the tibia by the coronary ligaments and by direct insertion of the anterior and posterior horns into the bone. The menisci also attach to the joint capsule. The medial meniscus attaches to the deep layer of the medial collateral ligament and the lateral meniscus attaches loosely to the lateral joint capsule. The posterior horn of the lateral meniscus is attached to the femur via the meniscofemoral ligament. The capsular attachments of the medial meniscus are more secure than the lateral meniscus [14, 15].
The menisci consist of approximately 75% type I collagen [16]. Collagen types II, III, IV and V are also present. Most of the collagen fibers are oriented circumferentially to resist tensile forces and contain hoop stresses which are generated while weight bearing [17]. Radially oriented “ties” hold circumferential fibers together and provide resistance to shear [18].
Each meniscus is divided anatomically into horizontal thirds: the posterior horn, the mid-body, and the anterior horn. Menisci are divided into vertical thirds when looking at blood supply. The most peripheral 20% to 30% of the medial meniscus and the peripheral 10–25% of the lateral meniscus receive a rich blood supply from the medial and lateral genicular arteries [19].
Vascularization decreases approaching the inner portion of the meniscus and becomes dependent upon diffusion [20]. Because of the poor blood supply, tears that extend to the inner avascular area have a more difficult time with healing. Arnoczky and Warren have reported that in order for meniscus tears to heal, the tear needs to be in contact with the peripheral vascular area [19].
Free nerve endings (nociceptors) and 3 different mechanoreceptors (Ruffini corpuscles, Pacinian corpuscles, and Golgi tendon organs) can be found in the horns and in the outer two-thirds of the body of the menisci [20–23]. The menisci therefore may serve as proprioceptive structures, providing a feedback mechanism for joint position sense [24•, 25]. Karahan, et al. demonstrated that partial meniscectomy patients had a significant loss of knee joint position sense at knee flexion angles of 60 and 75° at a mean 2 year follow-up [24•].
The distal surface of the femur is convex and rests on a relatively flat tibial plateau, whereas the concave proximal surface of the meniscus deepens the articular fossae of the tibia to create more congruity with the femoral condyles [26, 27]. To retain this congruity during knee joint flexion, the whole meniscus moves posteriorly on the tibial plateau to accommodate the femoral rollback on the tibial plateau, and, in particular, the anterior horn shows great displacements to stay in close contact with the declining diameter of the femoral condyles [26, 28•, 29]. In this manner, the meniscus stabilizes the knee joint and contributes to load bearing and shock absorption [22].
The menisci occupy 60% of the contact area between the tibial and femoral cartilage surfaces and transmit 50% of the joint compressive forces in full extension and approximately 85% of the load in 90° of extension [30]. The lateral meniscus picks up 70% of the load transmitted across the lateral compartment while the medial meniscus & articular cartilage share the load across the medial compartment [31].
The medial meniscus has been shown to be a significant restraint to anterior tibial displacement [12]. The lateral meniscus is more mobile than the medial meniscus and may rotate as much as 15–20° [32].
The function of the meniscus is reflected in its anatomy because its cells and extracellular matrix are arranged in such a way that compressive forces, shear stresses, circumferentially directed forces, and tensile hoop stresses can be endured and redirected optimally [31, 33, 34].
Mechanism of injury
The meniscus can fail from either mechanical or biochemical (degenerative) causes [35]. Noncontact forces are the most frequent mechanism of injury to the menisci [12]. These stresses result from a sudden acceleration or deceleration in conjunction with a change of direction (rotation force) that traps the menisci between the tibia and femur, which results in a tear. In jumping sports such as basketball and volleyball, the additional element of a vertical force with angular momentum (varus or valgus) on landing can contribute to a meniscal injury. This scenario can increase the likelihood of a tear when hyperextension or hyperflexion forces accompany significant rotation between the joint surfaces.
Contact injuries involving valgus or varus forces have contributed to meniscal pathology. Ligament injuries to the ACL or MCL or both in which increased tibial displacement occurs can displace the menisci from its peripheral attachments and result in a tear. In chronic ACL insufficiency, the incidence of meniscal pathology can approach 98% [36]. The medial meniscus injury rate has been found to be higher than that for the lateral side (86.9% vs. 28.9%) in this population [37].
Degenerative meniscal lesions are common in older individuals. The menisci become stiffer and less compliant with age [38]. It has been observed that meniscal tissue from patients over 40 years of age has a lesser cellularity and a decreased healing response than tissue from younger patients [39].
The most common types of meniscal tears are vertical longitudinal, oblique, degenerative, radial and horizontal [40]. Meniscal lesions present with varied clinical symptoms such as pain, effusion, locking, and persistent focal joint line tenderness. Displaced tears, such as bucket handle tears, can produce locking and “giving way” episodes. Nondisplaced tears can alter meniscus mobility and produce abnormal traction stresses on the capsule and synovium, which result in pain and swelling [41].
Surgical management (meniscal repair overview)
Surgical options include meniscectomy (partial or total), meniscal repair or meniscus transplantation. Meniscal tear pattern, geometry, site, vascularity, size, stability, tissue viability or quality, as well as associated pathology, are all taken into account when determining whether to resect or repair a meniscal lesion [42]. The physical health, activity level and aspirations of the patient may be taken into consideration during the management decision process. Co-morbidities, such as heart disease, obesity, axial alignment, and degenerative joint disease are considered in the decision process to excise, repair, replace or even avoid surgery. The aspirations of patients are also considered.
Improved surgical techniques along with advanced instrumentation and repair methods have enabled orthopaedic surgeons to repair menisci what were once thought of as unrepairable. The first reported meniscal repair was reported by Annandale in 1885 [43]. Meniscal repair techniques have evolved from the placement of sutures across the torn meniscus through arthrotomy to using arthroscopy. Published meniscal repair results have supported favorable success at extended follow up in over 70–90% of patients [44–48]. Clinical studies have demonstrated that the rates of healing after repairs of the lateral meniscus are better than those after repairs of the medial meniscus [49–51].
The goal of a meniscus repair is to allow the torn edges of the meniscus to heal once they have been fixated with sutures. The most important factor in determining repairability is the location of the tear, as tears in the vascular periphery of the meniscus can produce a healing response. The ideal tear is an acute, vertical, longitudinal tear in the peripheral one-third of the meniscus in a young patient who has a stable knee or will have concomitant reconstruction of the ACL [52]. Radially oriented tears in the posterior horn of the meniscus may be repaired because of the abundant blood supply in this region, Repairs of tears that extend 4–5 mm beyond the peripheral rim of the meniscus traditionally have been not been advocated due to questions regarding healing potential and possibility of retears
In younger patients, meniscal repair can be considered for tears that extend into the central, avascular zone of the meniscus. Rubman and colleagues reported that 159 (80%) of 198 knees in which a tear in the central, avascular zone had been repaired had no symptoms at the time of follow-up [48]. Arnocsky et al. have demonstrated that insertion of a fibrin clot in the avascular zone of a meniscal defect has promoted healing in the canine model [53].
Flap tears and horizontal cleavage tears generally are not repairable. Radial tears in the middle portion of the meniscus have a poor potential for healing [54]. Although both acute and chronic tears can be successfully repaired, clinical studies have reported better healing rates after acute repair [55, 56].
Surgical procedures to repair the meniscus vary. In relatively stable tears the literature has reported the use of rasping and trephination [57–59]. Arthroscopic meniscal repair techniques can be divided into three techniques based upon suture placement. They include an inside-out repair, outside-in repair, and all-inside repair.
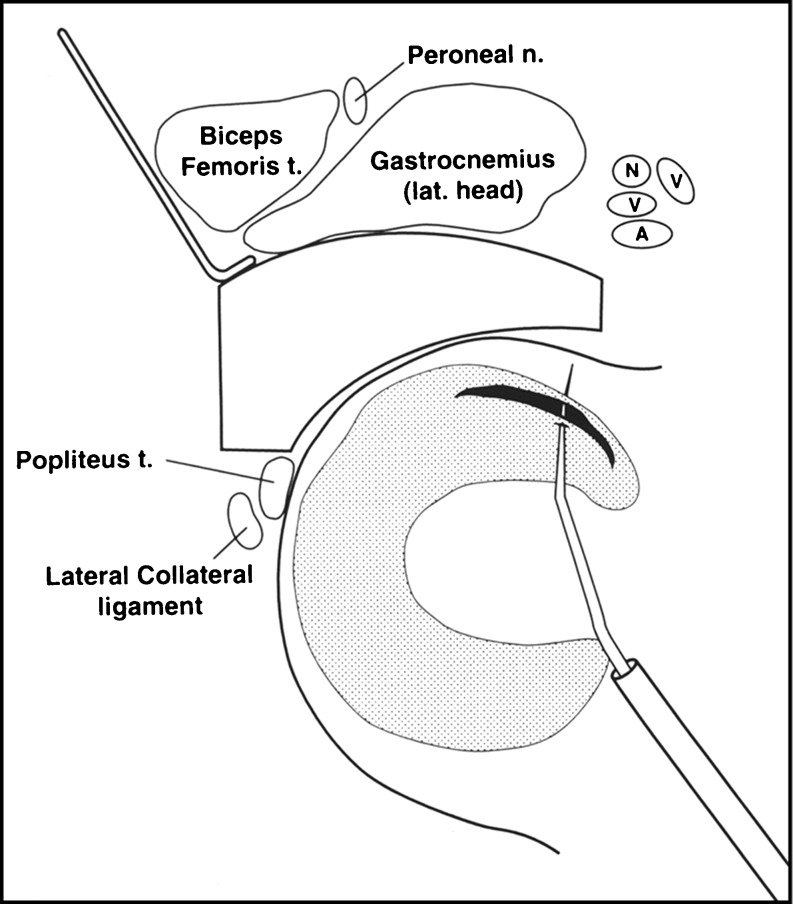
The arthroscopic inside-out surgical technique involves the placement of sutures across the meniscus inside the joint and the sutures are then tied down outside the joint capsule [60]. (Figure 1) This technique has been successful with tears to the middle one-third and to some degree tears of the posterior horns [61, 62].
Fig. 1.
Inside-Out Meniscal Repair: The arthroscopic inside-out surgical technique involves the placement of sutures across the meniscus inside the joint and the sutures are then tied down outside the joint capsule. (Courtesy HSS Sports Medicine Service)
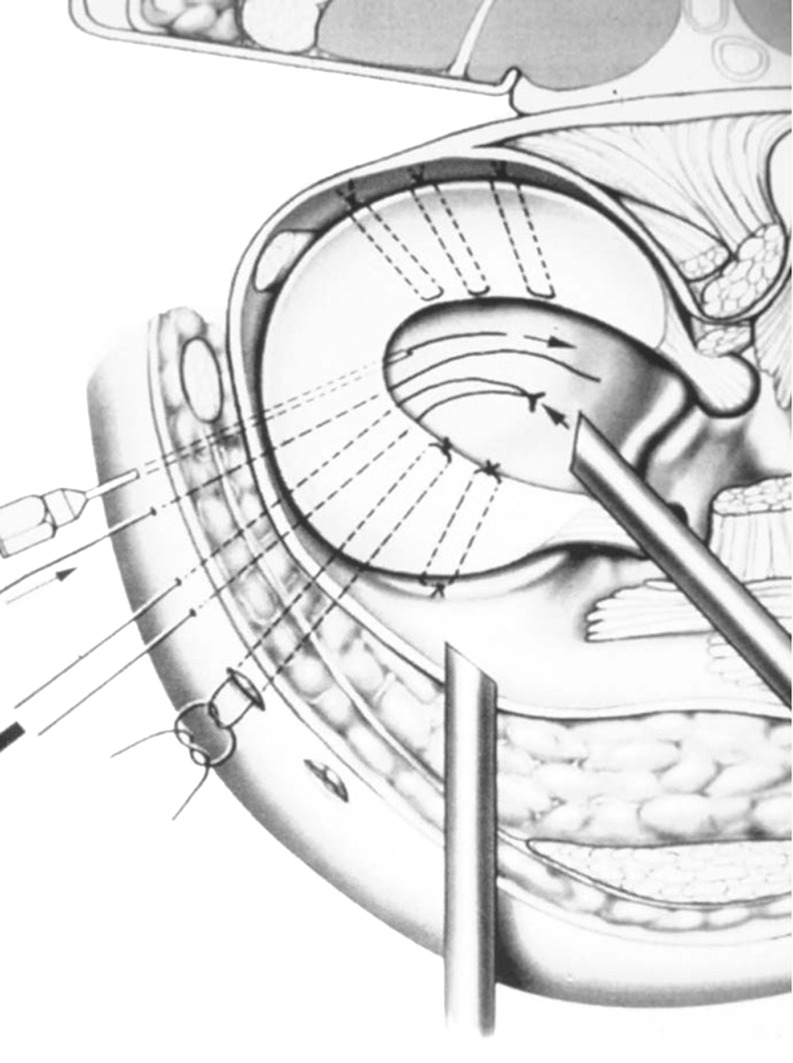
The arthroscopic outside-in surgical technique was developed by Warren as a method to decrease the risk of injury to the peroneal nerve during arthroscopic repair of the lateral meniscus. The procedure involves the placement of a suture with a Mulberry knot to one side of the meniscus tear inside the joint and then sutures are tied on the joint capsule [63, 64] (Fig. 2). This technique has been advocated in repairing tears to the mid-one-third and anterior horn regions [65].
Fig. 2.
Outside-In Meniscal Repair: The arthroscopic outside-in surgical technique involves the placement of a suture to one side of the meniscus tear inside the joint and then sutures are tied on the joint capsule. (Courtesy HSS Sports Medicine Service)
The arthroscopic all inside surgical technique involves the placement of a suture anchors, biodegradable screws, darts and/or “arrows” through an arthroscopic portal to stabilize the tear [66]. Devices include the T-fix (Acufex Microsurgical Inc., Mansfield, MA) and Meniscal Arrow (BIONX, Malvem, PA). Because it does not make use of any incisions, the all-inside technique is favorable in decreasing the risk of iatrogenic neurovascular damage. This technique has favorable results for posterior horn tears [66–68].
Rehabilitation principles for the meniscal repair patient (Table 1)
Table 1.
Rehabilitation principles for the meniscal repair patient
| Individualize Program: Consider Pre-Injury Status |
|---|
| Apply a Working Knowledge of the Basic Sciences to the Rehabilitation Program |
| Base Rehabilitation on Current Clinical Research |
| Team Approach to Rehab: Responsibilities & Communication |
| Adhere to the Rules of Rehabilitation |
| Rule #1: Create a safe environment |
| Rule #2: Do not hurt the patient |
| Rule #3: Be aggressive without breaking rules #1 and #2 |
| Follow a Functional Progression |
| Follow evaluation-based guidelines |
Individualize program : consider Pre-injury status
No two meniscal patients with the same diagnosis present identically. Therefore, the most important principle guiding a rehabilitation program following meniscal repair surgery is individualization [69]. The pre-injury status of the patient needs to be taken under serious consideration as different patients present in different physical condition at the time of their initial evaluation. The patient may be an elite athlete, a recreational athlete, or a nonathlete in weak physical condition.
The rehabilitation specialist should take into consideration the axial alignment of the patient. Habata et al. reported an association between atraumatic tears of the medial meniscus and varus deformity [70]. Medial meniscus repair patients with a varus deformity and lateral meniscus repair patients with a valgus deformity may need a more conservative approach in their rehabilitation as the compressive loads in the respective involved compartment are higher. Surgeons may elect to delay weight bearing and/or place these individuals in an unloader brace.
Apply a working knowledge of the basic sciences to the rehabilitation program
To provide quality care to individuals who have undergone a meniscal repair, a thorough understanding of menisci function and biomechanics is needed. Knowing how and when the menisci are placed under stress during activities of daily living and specific exercises will assist the rehabilitation specialist in safely advancing the patient through the rehabilitative course and optimize functional outcome. An appreciation of the inflammatory process and nature of tissue healing is invaluable in safely preparing the patient to return to the desired level of activity.
Base rehabilitation on current clinical research
Recent rehabilitation guidelines now have a more scientific rationale and basis. The rehabilitation specialist should keep abreast of current advances in surgical procedures, clinical evaluation and treatment techniques to ensure that contemporary interventions are being provided to produce an optimal outcome.
Team approach to rehab: responsibilities & communication
For a successful outcome after meniscal repair, the orthopaedic surgeon, rehabilitation specialist and patient must work responsibly together as a team. Communication among the team members is vital. The surgeon has the responsibility of performing the proper surgical procedure to address the meniscal lesion, as well as directing the postoperative rehabilitation program. Discussing the procedure or providing the rehabilitation specialist with a copy of the operative note will assist the clinician in understanding any post-operative precautions (weight bearing status, range of motion restrictions, etc.) and in developing realistic and measurable goals. The surgical technique, including the number of incisions and location and nature of the meniscal repair, has a direct effect on the progression of the patient’s rehabilitation program. The more soft tissue dissection there is, especially capsular incisions, the more hemarthrosis and muscle inhibition will occur postoperatively [71].
The surgeon should also share any associated pathology findings with the rehabilitation specialist. Patients with degenerative joint disease may take longer for rehabilitate and require a slower therapeutic progression than those patients with pristine articular surfaces. Patients with chondromalacia patellae may not be candidate’s for certain isotonic or isokinetic knee extension exercises. Patients with an ACL-deficient knee will require increased proprioceptive and neuromuscular training in their therapeutic exercise program.
The responsibilities of the clinician assigned to the patient with a meniscal repair include: being current with the most contemporary approaches in rehabilitating this population and communicating with the surgeon as to the patient’s progress and compliance to the therapeutic recommendations of the physician and rehabilitation specialist.
The patient has an important role as well. The patient should adhere to the advice given by the surgeon and rehabilitation specialist. This includes compliance to prescribed home therapeutic exercises and recommended activity modifications in their daily routine. There are 168 h in a week, but a patient may be under the supervision of the rehabilitation clinician only three times per week for 3 h (2%). This leaves the patient responsible for his or her own care for 165 h (98% of the time). Patient compliance, therefore, is imperative for a successful outcome.
Adhere to the rules of rehabilitation
The rules of rehabilitation as described by Gray [72] can be easily applied to patients who have sustained a meniscal injury or who have underwent a surgical procedure to address a meniscal lesion.
Rule #1. Create a safe environment
The rehabilitation specialist should use his or her knowledge of the basic sciences to ensure that a prescribed exercise or activity does not compromise the healing response of the repaired menisci… For example: maintain weight bearing and ROM precautions after a complex meniscal repair procedure.
Rule #2 Do not hurt the patient
Prescribe exercises and activities that are pain free. Gains in ROM, strength, and flexibility can best be achieved in this manner. Modifications can be made by adapting pain free arcs of motion on strengthening equipment and functional activities. It is also important to counsel patients not to hurt themselves. Hence a subset of this rule can be, “Not to have the patient hurt the patient” This can be achieved by having patients maintain close awareness of the knee and modify their activity level to meet their present condition.
Rule #3. Be aggressive without breaking rules #1 and #2
The rehabilitation specialist can be aggressive as long as a safe environment is maintained during the prescribed therapeutic exercises and the patient does not complain of knee pain during the exercise or activity. The goals of athletic individuals are often high with a rapid return to sport activity a top priority. Following these rules can result in a safe, expeditious and optimal outcome.
Follow a functional progression
A functional progression was defined by Kegerreis as an ordered sequence of activities enabling the acquisition or reacquisition of skills required for the safe, effective performance of athletic endeavors [73]. The patient should master a simple activity before advancing to a more demanding activity. Criteria therefore need to be established to ensure a safe progression.
An early goal in rehabilitation after meniscus repair surgery is to have the patient establish quadriceps control. This can be demonstrated by having the patient perform a straight leg raise without pain or an extensor lag. The functional progression can be advanced as ROM and muscle strength display improvement. The next criterion in the progression is to have the patient reestablish a normal non-antalgic gait pattern. Consider that “every step is therapy” and to encourage the patient to ambulate with a heal-toe gait pattern while progressively weight bearing with crutches. Additional strategies used include decreasing stride length, emphasizing quality ambulation over quantity and utilizing water (e.g. underwater treadmill) for ambulation training so as to gradually apply increased load through the knee joint.
Walking in chest-deep water results in a 60–75% reduction in weight bearing, while walking in waist-deep water results in a 40–50% reduction in weight bearing [74, 75]. Normalizing a gait pattern facilitates gains in ROM.
The patient is then asked to exhibit the ability to ascend stairs, followed by the ability to descend stairs. After demonstrating the ability to eccentrically control body weight descending stairs, the patient may initiate a running program. As muscle strength, balance, and flexibility demonstrate improvement, higher-level activities including agility-promoting, plyometric, and sport-specific activities are introduced as therapeutic interventions
Following meniscal repair, a designated protective phase will often hold back the patient from this natural progression. The clinician and patient need to respect the restrictions so designated to optimize outcome.
Follow evaluation-based guidelines
Today’s rehabilitation programs following meniscal repair surgery should follow a plan that is not as structured as the protocols of yesteryear. Each patient will progress at a different pace. Protocols can accelerate a program too quickly for the patient whose progress is delayed and can hold back the patient who is progressing very well. Though certain precautions are established, the rehabilitation specialist should refrain from following a “cookbook” approach to treatment. Instead, the clinician should combine basic scientific knowledge and physical examination skills to guide the patient through the rehabilitative course. Clinical guidelines developed by treating clinicians and the referring surgeons should incorporate flexible time frames in the progression to allow for individualization, for example: “week 4–6 -discontinue crutches when non-antalgic gait is demonstrated” versus “week 6—discontinue crutches for ambulation.” Continual reassessment of the patient is vital to ensure a consistent and safe progression of the program. Too rapid a progression in therapy or normal functional activities of daily living is demonstrated by increased effusion and pain. This is most likely related to muscular fatigue, which leaves the articular surfaces unprotected against compressive forces. Therapeutic exercise programs, therefore, often must be modified based on changes in subjective and objective findings [76].
A comprehensive evaluation sets the baseline from which progress is measured. A comprehensive history reveals the mechanism of injury, how the injury was initially managed, medical diagnosis including workup (radiographs, MRI scans, etc.), surgery date, and postsurgical management.
Observations document patient’s weight bearing status, gait deviations, joint effusion, muscle atrophy, and joint alignment. Attention to the patient’s subjective complaints is of the utmost importance throughout the rehabilitative process. Reports of pain (location and description), lack of mobility, and weakness have a direct effect on the progression of a rehabilitation program. The physical examination should document available active (AROM) and passive range of motion (PROM). Girth measurements should be taken above, at, and below each knee joint for comparison to assess muscle atrophy
Manual muscle testing may reveal a proximal or distal weakness or muscle imbalance. Quadriceps testing is often not appropriate in the immediate postoperative setting. Neurovascular integrity should be evaluated. Assessment of patellar orientation and tracking where appropriate can provide valuable information when quadriceps strengthening exercises are implemented at a later date. Flexibility assessment is important, as tight muscles about one joint can alter forces at another joint. Gait evaluation (when applicable) can be useful in assessing the patient’s biomechanical profile.
The clinical evaluation would not be complete without defining goals and a treatment plan to meet these goals. The information gathered should be reviewed with the patient. Realistic goals should be discussed and established by the patient, surgeon, and rehabilitation specialist. The patient should be brought to understand the magnitude of their surgery and the timetable for recovery. Goals should be specific to the individual needs of the patient. Goals should be functional and measurable as well. The patient should be made aware of his or her role in the rehabilitative process. Patient compliance with activity modifications and home therapeutic exercises is vital for complete rehabilitation and a successful outcome [69].
A treatment plan can only be developed when the clinical findings from a comprehensive examination are considered. The rehabilitation specialist should develop a prioritized problem list. Specific rehabilitation strategies can then be used to address each problem. Examples include utilizing cryotherapy to control or decrease pain and joint effusion, and ROM exercises to address a loss of knee flexion or extension. Throughout the rehabilitative course a criteria-based functional progression of therapeutic exercises should be followed.
Treatment strategies after arthroscopic meniscal repair
The post-operative management of a meniscal repair takes on a more conservative approach as compared to partial meniscectomy to allow for successful healing of the repair. Rehabilitation guidelines differ among surgeons and remain controversial [77–84]. Discrepancies exist in the amount of weight bearing and knee flexion allowed in the early post-operative time frame as well as the time frame for return to sports activity. Barber reported no differences in healing rates between patients who followed a more conservative and protective program and patients who participated in a more accelerated program (weight bearing, ROM exercises, and early return to sports activity) [77]. Kocabey [81] reported excellent results utilizing rehabilitation guidelines that were individualized depending on type/size of meniscal repair. For Anterior Posterior (AP) longitudinal tears ≤3 cm weight bearing was unrestricted without a brace and ROM progressively allowed to 125° of flexion at 3–6 weeks. For AP longitudinal tears >3 cm weight bearing was unrestricted with a locked brace and 0–125° ROM limit lifted weeks 6–8. Return to sport for AP tears allowed at 3 months. Complex and Radial meniscus tear protocols restricted weight bearing and ROM with brace initially, but were FWB with AROM 0–125° by 6–8 weeks. Patient’s returned to sport by 4–5 months post-operatively. Bryant et al. allowed for FWB with crutches and brace locked in extension for 3 weeks post surgery but then after allowed for WBAT and unlimited ROM with comparable results [82]. O’Shea and Shellbourne also reported high rates of meniscal healing with rehabilitation programs that allowed for unrestricted ROM, weight bearing beginning post-op day 3 meniscal repairs [83]. Noyes and Barber-Westin reported very good results in 76% of patients, 87% of which were asymptomatic at 33 months [84]. Weight bearing was limited for initial 4–6 weeks depending on type of repair, and ROM progressively advanced to 135° of flexion over 6 week period.
Programs should be individualized to the type of surgical procedure performed, the type of meniscal tear repaired and the basic science information that is currently available. Therefore, information from the surgeon regarding the classification of the tear, the anatomic site of the repair (vascular vs. nonvascular) and location within the meniscus (anterior or posterior) should directly affects the postoperative regimen.
During weight bearing, compressive forces are loaded across the menisci. These tensile forces create hoop stresses which expand the menisci in extension [85]. Morgan et al. demonstrated that extension appears to reduce the meniscus to the capsule, whereas flexion causes tears in the posterior horn to displace from the capsule [49]. Becker et al. have reported that weight bearing flexion from full extension to 90° increases the pressure on the posterior horn by, roughly, a factor of 4 [86]. The compressive loads applied while weight bearing in full extension following a vertical, longitudinal repair or bucket-handle repair can reduce the meniscus and stabilize the tear [65, 85]. In complete transactions of circumferential fiber bundles of the meniscus, such as radial tears that comprise the whole cross-section or posterior root tears, weight bearing should be delayed because the hoop stresses would distracts the tear margins and compromise healing [87].
The menisci translate dorsally with knee flexion. This motion depends not only on the flexion angle but also on the weight bearing condition [88]. Walker and Erkman demonstrated that progressive knee flexion subjects the menisci to greater stress [89]. Thompson et al. demonstrated that the meniscus translates posteriorly with flexion; however, meniscal movement was at a minimum at less than 60° of flexion [90]. Thus, consideration is given to limiting flexion to 60° during the early period of healing.
Tibial rotation causes large excursions of the meniscus within the first 30° of flexion [91]. Terminal flexion is accompanied by a large dorsal translation of the condyles and causes increased compressive stress of the meniscus [86, 92]. Therefore, deep squats and tibial rotation are avoided in the early phases of rehabilitation following meniscal repair.
There is evidence in a canine model that the maximum tensile strength of meniscus repairs reaches 80% by 12 weeks, which suggests that the suture/scar combination provides enough stability for clinical function [93]. However, many surgeons defer their patients from returning to pivoting sports until 4 or more months post-operatively.
Meniscal repair guidelines post—operative phase I (week 0–6)
The rehabilitation guidelines following meniscal repair at our institution are divided into three phases and are outlined in Table 2. The first phase is designed to protect the repair and allow for maximal healing. Rehabilitation is initiated immediately post-operatively. The patient is placed in a double-upright knee brace that is locked in full extension. This brace is used exclusively for ambulation and sleeping for the first 4–6 post-operative weeks. A progressive program of weight bearing as tolerated is initiated for bucket-handle and vertical, longitudinal tears. Weight bearing will be limited to toe-touch for radial or more complex repairs for 4–6 weeks as compressive loading may cause distraction of these repairs. Weight bearing with the knee in progressive flexion is avoided till 4–6 weeks as the meniscus is subjected to greater stress in this position [89].
Table 2.
Meniscus repair rehabilitation guidelines
| Meniscal Repair Guidelines Post – Operative Phase I (Week 0-6) |
|---|
| Goals: |
| • Emphasis on full passive extension |
| • Control post-operative pain/swelling |
| • Range of Motion →90° flexion |
| • Regain quadriceps control |
| • Independence in home therapeutic exercise program |
| Precautions: |
| • Avoid active knee flexion |
| • Avoid ambulation without brace locked @ 0° prior to 4 weeks |
| • Avoid prolonged standing/walking |
| Treatment Strategies: |
| • Towel extensions, prone hangs, etc. |
| • Quadriceps re-education (Quad Sets with EMS or EMG) |
| • Progressive Weight Bearing PWB→WBAT with brace locked at 0°with crutches |
| o Toe-Touch Weight Bearing for complex or radial tears |
| • Patella mobilization |
| • ctive-Assisted flexion/extension 90→0° Exercise |
| • SLR’s (all planes) |
| • Hip progressive resisted exercises |
| • Proprioception Board (bilateral weight bearing) |
| • Aquatic therapy – Pool ambulation or Underwater Treadmill (Week 4-6) |
| • Short Crank ergometry (if ROM > 85°) |
| • Leg Press (bilateral/60→0° arc) (if ROM > 85°) |
| • OKC quadriceps isometrics (submaximal/bilateral @ 60°) (if ROM > 85°) |
| • Upper extremity cardiovascular exercises as tolerated |
| • Hamstring and calf stretching |
| • Cryotherapy |
| • Emphasize patient compliance to home therapeutic exercise program and weight bearing and Range of motion precautions/progression |
| Criteria for Advancement: |
| • Ability to SLR without Quadriceps lag |
| • ROM 0 → 90° |
| • Demonstrate ability to unilateral (involved extremity) weight bear without pain |
| Meniscal Repair Guidelines Post – Operative Phase 2 (Week 6-14) |
| Goals: |
| • Restore Full ROM |
| • Restore normal gait (non-antalgic) |
| • Demonstrate ability to ascend and descend 8”stairs with good leg control without pain |
| • Improve ADL endurance |
| • Improve lower extremity flexibility |
| • Independence in home therapeutic exercise program |
| Precautions: |
| • Avoid descending stairs reciprocally until adequate quadriceps control & lower extremity alignment |
| • Avoid pain with therapeutic exercise & functional activities |
| • Avoid running and sport activity |
| Treatment Strategies: |
| • Progressive Weight Bearing/WBAT with crutches/cane (brace opened 0→60°), if good quadriceps control (good quad set/ability to SLR without lag or pain) |
| • Aquatic therapy – Pool ambulation or Underwater Treadmill |
| • D/C crutches/cane when gait is non-antalgic |
| • Brace changed to MD preference (Unloader brace, Patella sleeve, etc.) |
| • Active-assistive range of motion exercises |
| • Patella mobilization |
| • SLR’s (all planes) with weights |
| • Proximal progressive resisted exercises |
| • Neuromuscular training (Bilateral→Unilateral Support) |
| o Balance Apparatus, Foam surface, Perturbations |
| • Short Crank ergometry °→Standard ergometry (if knee ROM > 115°) |
| • Leg Press (bilateral/eccentric/unilateral progression) |
| • Squat program (PRE) 0°→60° |
| • OKC quadriceps isotonics (pain-free arc of motion) |
| • Initiate Forward Step Up & Step Down programs |
| • Stairmaster |
| • Retrograde treadmill ambulation |
| • Quadriceps stretching |
| • Eliptical Machine |
| • Forward Step Down Test (NeuroCom) |
| • Upper extremity cardiovascular exercises as tolerated |
| • Cryotherapy |
| • Emphasize patient compliance to home therapeutic exercise program |
| Criteria for Advancement: |
| • ROM to WNL |
| • Ability to descend 8”stairs with good leg control without pain |
| Meniscal Repair Guidelines Post – Operative Phase 3 (Week 14-22) |
| Goals: |
| • Demonstrate ability to run pain free |
| • Maximize strength and flexibility as to meet demands of activities of daily living |
| • Hop Test > 85% limb symmetry |
| • Isokinetic test > 85% limb symmetry |
| • Lack of apprehension with sport specific movements |
| • Flexibility to accepted levels of sport performance |
| • Independence with gym program for maintenance and progression of therapeutic exercise program at discharge |
| Precautions: |
| • Avoid pain with therapeutic exercise & functional activities |
| • Avoid sport activity till adequate strength development and MD clearance |
| Treatment Strategies: |
| • Progress Squat program < 90° flexion |
| • Lunges |
| • Retrograde treadmill running |
| • Start forward running (treadmill) program at 4 months post-op if 8” step down satisfactory |
| • Continue LE strengthening & flexibility programs |
| • Agility program/sport specific (sport cord) |
| • Start plyometric program when sufficient strength base demonstrated |
| • Isotonic knee flexion/extension (pain & crepitus free arc) |
| • Isokinetic training (fast → moderate → slow velocities) |
| • Functional testing (Hop Test) |
| • Isokinetic Testing |
| • Home therapeutic exercise program: Evaluation based |
| Criteria for Advancement: |
| • Symptom-free running and sport-specific agility |
| • Hop Test > 85% limb symmetry |
| • Isokinetic Test > 85% limb symmetry |
| • Lack of apprehension with sport specific movements |
| • Flexibility to accepted levels of sport performance |
| • Independence with gym program for maintenance and progression of therapeutic exercise program at discharge |
© Hospital For Special Surgery Sports Rehabilitation & Performance Center
The patient is instructed in ROM exercises to attain full extension and the recommended degree of flexion AAROM exercises are performed with flexion restricted to 90° during the initial (4–6 week) protection phase. Repairs to the posterior horn are limited to 70° for the first 4 weeks, and then progressed as tolerated. Active or resisted knee flexion is avoided during this phase due to the attachment of the semimembranosus muscle on the medial meniscus and the popliteus muscle on the lateral meniscus [94].
At 4–6 weeks post-operatively, the hinged brace is opened to 60° to allow for ROM during gait. Gait training using a pool or underwater treadmill is utilized to unload the involved extremity. Crutches are discharged when a non-antalgic gait is demonstrated. It is imperative that the prescribed weight bearing status and ROM allowance be enforced during in the early phase of rehabilitation. These precautions need to be reinforced continually to the patient to provide the optimal environment for meniscal healing.
Quadriceps re-education is addressed post-op day one with the patient instructed to perform quadriceps setting exercises with a rolled towel under their surgical knee. Electrical stimulation and/or biofeedback can be used should the patient demonstrate quadriceps inhibition (Fig. 3).
Fig. 3.

Quadriceps setting utilizing Kneehab Electrical Stimulation Device (NeuroTech Biomedical Research, Galway, Ireland)
Straight leg raising in multiple planes are encouraged for the development of proximal strength. Weights (progressive resistive exercise) are added to these exercises when tolerated along with exercise machines to further advance proximal strengthening.
Research suggests that a certain level of deafferentation occurs after lower extremity joint injury [95]. As the central nervous system receives decreased sensory information, there is decreased ability to adequately stabilize the lower extremity [95, 96]. Efforts to regain proprioception loss begin as soon as the patient demonstrates the ability to bear 50% of their weight. A rocker board with bilateral support is utilized starting in a sagital plane and is then progressed to a more challenging coronal plane. A computerized balance platform can be utilized for patient feedback (Fig. 4).
Fig. 4.

Dynamic stabilization training using Biodex Balance System (Biodex Medical Systems, Shirley, NY).
As flexion ROM improves to greater than 85°, select OKC and CKC exercises are introduced to the therapeutic exercise program. Bilateral leg press and mini-squats are performed inside a 60°−0° arc of motion. Quadriceps isometrics are performed submaximally at 60° of flexion. Stationary bicycling is added to the rehabilitation program by utilizing a short crank (90 mm) ergometer.
Hamstring and calf stretching exercises are added into both formal and home therapeutic exercise programs. Cryotherapy and electrical stimulation (TENS) may be utilized for pain control. Home therapeutic exercise programs are continually updated [97].
Meniscal repair guidelines post—operative phase 2 (week 6–14)
The second post-operative phase following meniscal repair is dedicated to restoring normal ROM to the involved knee and improving muscle strength to the level needed to perform activities of daily living.
The demonstration of a normal gait pattern is an early goal of this phase. AAROM exercises are progressed as tolerated with the goal of attaining full ROM by the end of this phase. As ROM improves to 110° → 115° cycling is advanced to a standard 170 mm ergometer. Quadriceps stretching is added as range of motion increases to greater than 120°. Leg press exercise will progress to eccentric and eventually unilateral training utilizing greater range of motion (<90°). A squat program with progressive resistance is initiated utilizing a physioball for support and comfort inside a 60°→ 0° arc of motion. A forward step up program is begun on successive step heights (4”, 6”, 8”). Stairmaster and elliptical machine are incorporated as symptoms allow. Retrograde treadmill ambulation on progressive percentage inclines is utilized to facilitate quadriceps strengthening. When full ROM and improved quadriceps control is demonstrated OKC knee isotonic extension exercises are implemented inside a pain-free/crepitus-free arc of motion. Bilateral knee extensions are initiated prior to unilateral exercise.
A forward step down program is initiated on successive height increments (4”, 6”, 8”). The functional strength goal at the end of this phase is for the patient to demonstrate pain-free descent from an 8” step with adequate lower extremity control without deviations (Fig. 5). At 14 weeks post-operatively a Forward Step Down Test [98] is performed to assist in objectively measuring functional lower extremity muscle strength. The test entails having the patient step down from an 8” step onto a forceplate as slowly and controlled as possible with each leg. Lower extremity control is observed for deviations. Mean impact and limb comparison are calculated and compared to the established norms of 10% body weight and 85% symmetry, respectively.
Fig. 5.

Forward step-down from an 8” step, demonstrating quadriceps control in the post-surgical extremity
Neuromuscular training is advanced to include unilateral balance activities, such as contralateral elastic band exercises and balance systems training. As these activities are mastered, the rehabilitation specialist can incorporate less stable surfaces (foam rollers, rocker boards, etc.) as well as perturbation training to these activities to further enhance neuromuscular development.
Attainment of ROM and muscle strength is crucial to allow for a safe advancement through the rehabilitation program. Reciprocally descending stairs, for example, should be avoided until a sufficient lower extremity strength base is demonstrated. Pain while performing ROM and strengthening exercises is the best indicator in knowing when to modify treatment choices. Patellofemoral symptoms should be continually monitored.
The patient’s home therapeutic exercise program is continually updated based evaluative findings and functional level.
Meniscal Repair Guidelines Post—Operative Phase 3 (Week 14–22)
The focus of the final phase of rehabilitation following meniscal repair is directed at optimizing functional capabilities and preparing the patient/athlete for a safe return to sport activities.
At 4 months post-operatively, given symmetrical ROM and demonstrated quadriceps control, a running program on a treadmill is initiated. Retrograde running is preceded by forward running. An initial emphasis on speed over shorter distances vs. slower distance running is recommended.
Lower extremity strengthening and flexibility programs are continued. Advanced strengthening activities including isokinetic and plyometric training are introduced. Plyometric training should follow a functional sequence with the components of speed, intensity, load, volume and frequency being monitored and progressed accordingly. Activities begin with simple drills and advance to more complex exercises (e.g. double leg jumping vs. box drills). Agility exercises are introduced with the demands of the individual’s sport taken into consideration, e.g. deceleration, cutting, sprinting. The rehabilitation specialist should be certain to observe any apprehension during the agility activity progression.
To quantify strength and power both isokinetic and functional testing are performed. The goals of isokinetic testing include a less than 15% deficit for quadriceps and hamstring average peak torque and total work at test velocities of 180° and 300°/s. Functional testing links specific components of function and the actual task and provides direct evidence to prove functional status. Single-leg hop test [99] and cross-over hop test [100] are performed with the goal of achieving an 85% limb symmetry score.
The results of these tests along with any other pertinent clinical findings including the lack of apprehension with sport specific movements are presented to the referring orthopaedic surgeon for the final determination of sports participation [88].
Conclusion
Advances in basic science over the last three decades have contributed tremendously to our knowledge of the menisci’s function and repairability. Advances in arthroscopic techniques have enhanced the surgeons ability to salvage what were once considered irrapairable lesions.
The rehabilitation specialist should consider each patient as an individual and progress the patient along a criteria based progression in order to achieve a safe and satisfactory outcome.
The patient needs to be educated to the importance of their role in the rehabilitative process Compliance to home therapeutic exercises needs to be emphasized. The patient must also be encouraged to modify their functional activities to their present strength level throughout the rehabilitative course.
Clinical research has laid a foundation for which the rehabilitation following meniscal repair is based. Further research in the form of laboratory science and clinical outcomes are needed to substantiate treatment strategies employed during the rehabilitation of these patients.
Acknowledgments
Disclosure
No potential conflicts of interest relevant to this article were reported.
Contributor Information
John T. Cavanaugh, Phone: +1-212-6061005, FAX: +1-212-7742089, Email: cavanaughj@hss.edu
Sarah E. Killian, Phone: +1-212-6061005, FAX: +1-212-7742089, Email: killians@hss.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Howell GED. Clinical presentation of the knee. In: Bulstrode CJK, Buckwalter J, Carr A, Marsh L, Fairbank J, Wilson-MacDonald J, Bouden G, editors. Oxford textbook of orthopedics and trauma. New York: Oxford University Press; 2002. pp. 1108–1113. [Google Scholar]
- 2.Hede A, Jensen DB, Blyme P, et al. Epidemiology of meniscal lesions in the knee: 1.215 open operations in Copenhagen 1982-84. Acta Orthop Scand 5:435437, 1990 [DOI] [PubMed]
- 3.Allen PR, Denham RA, Swan AV. Late degenerative changes after meniscectomy. Factors affecting the knee after operation. J Bone Joint Surg Br. 1984;66(5):666–671. doi: 10.1302/0301-620X.66B5.6548755. [DOI] [PubMed] [Google Scholar]
- 4.Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30B(4):664–670. [PubMed] [Google Scholar]
- 5.Jorgensen U, Sonne-Holm S, Lauridsen F, Rosenklint A. Long-term Follow-up of Meniscectomy in Athletes. A Prospective Longitudinal Study. J Bone Joint Surg Br. 1987;69B(1):80––83. doi: 10.1302/0301-620X.69B1.3818740. [DOI] [PubMed] [Google Scholar]
- 6.Cox JS, Nye CE, Schaefer WW, et al. The degenerative effects of partial and total resection of the medial meniscus in dogs’ knees. Clin Orthop. 1975;109:178–183. doi: 10.1097/00003086-197506000-00026. [DOI] [PubMed] [Google Scholar]
- 7.Macnicol MF, Thomas NP. The knee after meniscectomy. J Bone Joint Surg Br. 2000;82:157–159. doi: 10.1302/0301-620X.82B2 .10847. [DOI] [PubMed] [Google Scholar]
- 8.Rockborn P, Messner K. Long-term results of meniscus repair and meniscectomy: a 13-year functional and radiographic follow-up study [comments] Knee Surg Sports Traumatol Arthrosc. 2000;8:2–10. doi: 10.1007/s001670050002. [DOI] [PubMed] [Google Scholar]
- 9.Packer JD, Rodeo SA. Meniscal allograft transplantation. Clin Sports Med. 2009;28(2):259–283. doi: 10.1016/j.csm.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 10.Seedhom BB, Gardreanes DJ. Transmission of load in the knee joint with special reference to the role of the menisci, part II. Experimental results, discussions, and conclusions. Eng Med Biol. 1979;B:220-8.
- 11.Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clinical Orthopedics. 1980;149:283–290. [PubMed] [Google Scholar]
- 12.Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. Journal of Bone and Joint Surgery Am. 1982;64A(6):883–888. [PubMed] [Google Scholar]
- 13.Wirth CJ, Peters G. Meniscus injuries of the knee joint: pathophysiology and treatment principles, in Baillière’s Clinical Orthopedics: Baillière Tindall. London,1997, pp123-44.
- 14.Warren RF, Arnoczky SP, Wickiewicz TL. Anatomy of the Knee. In: Nicholas JA, Hershman EB, editors. The lower extremity and spine in sports medicine. St. Louis: CV Mosby; 1986. pp. 657–694. [Google Scholar]
- 15.Rath E, Richmond JC. The menisci: basic science and advances in treatment. Br J Sports Med. 2000;34:252–257. doi: 10.1136/bjsm.34.4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghosh P, Taylor TK. The knee joint meniscus. A fibrocartilage of some distinction. Clin Orthop Relat Res 1987;(224):52–63. [PubMed]
- 17.Fithian DC, Kelly MA. Material properties and structure-function relationships in the menisci. Clin Orthop. 1990;252:19–31. [PubMed] [Google Scholar]
- 18.Cole BJ, Carter TR, Rodeo SA. Allograft meniscal transplantation: backround, technique and results. J Bone Joint Surg. 2002;84(7):1236–1250. [Google Scholar]
- 19.Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10(2):90–95. doi: 10.1177/036354658201000205. [DOI] [PubMed] [Google Scholar]
- 20.Day B, Mackenzie WG, Shim SS, Leung G. The vascular and nerve supply of the human meniscus. Arthroscopy. 1985;1(1):58–62. doi: 10.1016/S0749-8063(85)80080-3. [DOI] [PubMed] [Google Scholar]
- 21.O’Connor BL, McConnaughey JS. The structure and innervation of cat knee menisci, and their relation to a “sensory hyposthesis” of meniscal function. Am J Anat. 1978;153:431–442. doi: 10.1002/aja.1001530306. [DOI] [PubMed] [Google Scholar]
- 22.Assimakpoulos AP, Katonis PG, Agapitos MV, Exarchou El. The innervation of the human meniscus. Clin Orthop. 1992;75:232–236. [PubMed] [Google Scholar]
- 23.Gronblad M, Korkala O, Liesi P, Karaharju E. Innervation of synovial membrane and meniscus. Acta Orthop Scand. 1985;56:484–486. doi: 10.3109/17453678508993040. [DOI] [PubMed] [Google Scholar]
- 24.Karahan M, Kocaoglu B, et al. Effect of partial medial meniscectomy on the proprioceptive function of the knee. Arch Orthop Trauma Surg. 2010;130(3):427–431. doi: 10.1007/s00402-009-1018-2. [DOI] [PubMed] [Google Scholar]
- 25.Jerosch J, Prymka M. Proprioceptive deficits of the knee joint after rupture of the medial meniscus] Unfallchirurg. 1997;100(6):444–448. doi: 10.1007/s001130050140. [DOI] [PubMed] [Google Scholar]
- 26.Fu FH, Thompson WO. Motion of the meniscus during knee flexion. In: Mow VC, Arnoczky SP, Jackson DW, editors. Knee meniscus: basic and clinical foundations. New York: Raven; 1992. pp. 75–89. [Google Scholar]
- 27.Mow VC, Ratcliffe A, Chern KY, et al. Structure and function relationships of the menisci of the knee. In: Mow VC, Arnoczky SP, Jackson DW, et al., editors. Knee meniscus: basic and clinical foundations. New York: Raven; 1992. pp. 37–57. [Google Scholar]
- 28.Bedi A, Kelly NH, Baad M, et al. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92(6):1398–1408. doi: 10.2106/JBJS.I.00539. [DOI] [PubMed] [Google Scholar]
- 29.Vedi V, Williams A, Tennant SJ, et al. Meniscal movement: an in-vivo study using dynamic MRI. J Bone Joint Surg Br. 1999;81:37–41. doi: 10.1302/0301-620X.81B1.8928. [DOI] [PubMed] [Google Scholar]
- 30.Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints–Part I: Tibial surface of the knee. J Biomech Eng. 1983;105(3):216–225. doi: 10.1115/1.3138409. [DOI] [PubMed] [Google Scholar]
- 31.Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clinical Orthopedics and Related Research. 1975;109:184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 32.Muller W. The Knee. New York: Springer; 1982. [Google Scholar]
- 33.DeHaven KE. The role of the meniscus. In: Ewing JW, editor. Articular cartilage and knee joint function: basic science and arthroscopy. New York: Raven Press, Ltd.; 1990. pp. 103–115. [Google Scholar]
- 34.Fithian DC, Kelly MA, Mow VC. Material properties and structure-function relationships in the menisci. Clin Orthop Relat Res. 1990;252:19–31. [PubMed] [Google Scholar]
- 35.Radin EL. Factors influencing the progression of osteoarthrosis. In: Ewing JW, editor. Articular cartilage and knee joint function. New York: Raven; 1990. pp. 301–309. [Google Scholar]
- 36.Arnoczky SP, Adams ME, DeHaven KE, et al. Meniscus. P. 427. In Woo SL-Y, BuckwalterJA (eds): Injury and Repair of the Musculoskeletal Soft Tissues. American Academy of Orthopaedic Surgeons, Park Ridge, IL., 1988.
- 37.Warren RF, Marshall J. Injuries of the anterior cruciate ligament and medial collateral ligament of the knee. Clin Orthop. 1978;136:191. [PubMed] [Google Scholar]
- 38.Hough AL, Webber RJ. Pathology of the meniscs. Clin Orthop. 1990;252:32–40. [PubMed] [Google Scholar]
- 39.Mesiha M, Zurakowski D, Soriano J, et al. Pathologic characteristics of the torn human meniscus. Am J Sports Med. 2007;35:103–112. doi: 10.1177/0363546506293700. [DOI] [PubMed] [Google Scholar]
- 40.Swenson YM, Harner CD. Knee ligament and meniscal injuries. Orthop Clin North Am. 1995;26(3):529–546. [PubMed] [Google Scholar]
- 41.DeHaven KE. Injuries to the menisci of the knee. p.905.In Nicholas JA, Hershmann EB (eds): The Lower Extremity and Spine in Sports Medicine. CV Mosby, St.Louis 1986
- 42.Sgaglione NA, Steadman JR, Shaffer B, et al. Current concepts in meniscus surgery: resection to replacement. Arthroscopy. 2003;19(suppl 1):161–188. doi: 10.1016/j.arthro.2003.10.032. [DOI] [PubMed] [Google Scholar]
- 43.Annandale T. An operation for displaced semilunar cartilage. Br Med J. 1885;1:779. doi: 10.1136/bmj.1.1268.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Belzer J, Cannon W. Meniscal tears: treatment in the stable and unstable knee. Journal of the American Academy of Orthopedic Surgeons. 1993;1(1):41–47. doi: 10.5435/00124635-199309000-00006. [DOI] [PubMed] [Google Scholar]
- 45.Gillquist J, Messner K. Long-term results of meniscal repair. Sports Medicine Arthroscopy. 1993;1:159–163. doi: 10.1097/00132585-199300120-00009. [DOI] [Google Scholar]
- 46.Cannon WD, Vittori JM. The incidence of healing in an arthroscopic meniscal repairs in ACL-reconstructed knees versus stable knees. Am J Sports Med. 1992;20(2):176–181. doi: 10.1177/036354659202000214. [DOI] [PubMed] [Google Scholar]
- 47.Sommerlath K, Gilquist J. Knee function after meniscus repair and total meniscectomy: A 7-year follow-up study. Arthroscopy. 1987;3(3):166–169. doi: 10.1016/S0749-8063(87)80059-2. [DOI] [PubMed] [Google Scholar]
- 48.Rubman MH, Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscal tears that extend into the avascular zone. A review of 198 single and complex tears. Am J Sports Med. 1998;26:87–95. doi: 10.1177/03635465980260013301. [DOI] [PubMed] [Google Scholar]
- 49.Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med. 1991;19:632–637. doi: 10.1177/036354659101900614. [DOI] [PubMed] [Google Scholar]
- 50.Nicholas SJ, Rodeo SA, Ghelman B, et al. Arthroscopic meniscal repair using the outside-in technique. Read at the American Orthopaedic Society for Sports Medicine Specialty Day Meeting, Anaheim, California, 1991.
- 51.Trommel MF, Simonian PT, Potter HG, Wickiewicz TL. Different healing rates with the outside-in technique for meniscal repair. Am J Sports Med. 1998;26:446–452. doi: 10.1177/03635465980260031901. [DOI] [PubMed] [Google Scholar]
- 52.Rodeo SA. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect. 2000;49:195–206. [PubMed] [Google Scholar]
- 53.Arnoczky SP, Warren RF, Spivak JM. Meniscal repair using an exogenous fibrin clot. An experimental study in dogs. J Bone Joint Surg Am. 1988;70(8):1209–1217. [PubMed] [Google Scholar]
- 54.Cannon WD. Meniscal healing. In Arthroscopic Meniscal Repair, pp. 7-12. Edited by W. D. Cannon. Rosemont, Illinois, AmericanAcademy of Orthopaedic Surgeons, 1999.
- 55.Henning CE, Lynch MA, Yearout KM, et al. Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop. 1990;252:64–72. [PubMed] [Google Scholar]
- 56.Tenuta JJ, Arciero RA. Arthroscopic evaluation of meniscal repairs: factors that effect healing. Am J Sports Med. 1994;22:797–802. doi: 10.1177/036354659402200611. [DOI] [PubMed] [Google Scholar]
- 57.Zhang Z, Arnold JA, Williams T, et al. Repair by trephination and suturing of longitudinal injuries in the avascular area of the meniscus in goats. Am J Sports Med. 1995;23(1):35–41. doi: 10.1177/036354659502300106. [DOI] [PubMed] [Google Scholar]
- 58.Okuda K, Ochi M, Shu N, Uchio Y. Meniscal rasping for repair of meniscal tear in the avascular zone. Arthroscopy. 1999;15(3):281–286. doi: 10.1016/S0749-8063(99)70035-6. [DOI] [PubMed] [Google Scholar]
- 59.Uchio Y, Ochi M, Adachi N, et al. Results of rasping of meniscal tears with and without anterior cruciate ligament injury as evaluated by second-look arthroscopy. Arthroscopy. 2003;19(5):463–469. doi: 10.1053/jars.2003.50109. [DOI] [PubMed] [Google Scholar]
- 60.Henning CE. Arthroscopic repair of meniscal tears. Orthopedics. 1983;6:1130–1132. doi: 10.3928/0147-7447-19830901-08. [DOI] [PubMed] [Google Scholar]
- 61.Scott GA, Jolly BC, Henning CE. Combined posterior incision and arthroscopic intra-articular repair of the meniscus. An examination of factors affecting healing. J Bone and Joint Surgery American. 1986;68(6):847–861. [PubMed] [Google Scholar]
- 62.Sgaglione NA, Steadman JR, Shaffer B, et al. Current concepts in meniscus surgery: resection to replacement. Arthroscopy. 2003;19(suppl 1):161–188. doi: 10.1016/j.arthro.2003.10.032. [DOI] [PubMed] [Google Scholar]
- 63.Warren RF. Arthroscopic meniscus repair. Arthroscopy. 1985;1:170–172. doi: 10.1016/S0749-8063(85)80005-0. [DOI] [PubMed] [Google Scholar]
- 64.Morgan CD, Casscells SW. Arthroscopic meniscus repair: a safe approach to the posterior horns. Arthroscopy. 1986;2(1):3–12. doi: 10.1016/S0749-8063(86)80003-2. [DOI] [PubMed] [Google Scholar]
- 65.Rodeo SA. Arthroscopic meniscal repair with use of the outside-in technique. Journal Bone & Joint Surgery American. 2000;82(1):127–141. [Google Scholar]
- 66.Morgan CD. The “all-inside” meniscus repair. Arthroscopy. 1991;7(1):120–125. doi: 10.1016/0749-8063(91)90093-D. [DOI] [PubMed] [Google Scholar]
- 67.Cannon WD, Jr, Morgan CD. Meniscal repair. Part II: Arthroscopic repair techniques. J Bone Joint Surg Br. 1994;76A:294–311. [Google Scholar]
- 68.Albrecht-Olsen P, Kristensen G, Burgaard P, et al. The arrow versus horizontal suture in arthroscopic meniscus repair. A prospective randomized study with arthroscopic evaluation. Knee Surg Sports Traumatol Arthrosc. 1999;7(5):268–273. doi: 10.1007/s001670050162. [DOI] [PubMed] [Google Scholar]
- 69.Cavanaugh JT. Rehabilitation following meniscal surgery. In: Engle RP, editor. Knee Ligament Rehabilitation. New York: Churchill Livingston; 1991. pp. 59–69. [Google Scholar]
- 70.Habata T, Ishimura M, Ohgushi H, et al. Axial alignment of the lower limb in patients with isolated meniscal tear. J Orthop Sci. 1998;3:85–89. doi: 10.1007/s007760050026. [DOI] [PubMed] [Google Scholar]
- 71.Zarins B, Boyce J, Harris BA. Knee rehabilation following arthroscopic meniscectomy. Clin Orthop Rel Res. 1985;198:36. [PubMed] [Google Scholar]
- 72.Gray G. Successful strategies for closed chain testing and rehabilitation. Chain Research Seminar; May 1989.
- 73.Kegerreis S. The construction and implementation of a functional progression as a functional progression as a component of athletic rehabilitation. J Orthop Sports Phys Ther 1983; 14. [DOI] [PubMed]
- 74.Bates A, Hanson N. The principles and properties of water. In: Aquatic exercise therapy. Philadelphia: WB Saunders, 1996:1–320.
- 75.Harrison RA, Hilman M, Bulstrode S. Loading of the lower limb when walking partially immersed: implications for clinical practice. Physiotherapy. 1992;78:164. doi: 10.1016/S0031-9406(10)61377-6. [DOI] [Google Scholar]
- 76.Cavanaugh JT. Rehabilitation for non operative and operative management of knee injuries. In: Callaghan J, Simonian P, Wickiewicz T, editors. The adult knee. Lipponcott: Wilkens Publishers; 2003. pp. 380–430. [Google Scholar]
- 77.Barber FA. Accelerated rehabilitation for meniscus repairs. Arthroscopy. 1994;10:206–210. doi: 10.1016/S0749-8063(05)80095-7. [DOI] [PubMed] [Google Scholar]
- 78.Cooper DE, Arnoczky SP, Warren RF. Meniscal repair. Clin Sports Med. 1991;10(3):529–548. [PubMed] [Google Scholar]
- 79.DeHaven KE, Lohrer WA, Lovelock JE. Long term results of open meniscal repair. Am J Sports Med. 1995;23:524–530. doi: 10.1177/036354659502300502. [DOI] [PubMed] [Google Scholar]
- 80.Rispoli DM, Miller MD. Options in meniscal repair. Clin Sports Med. 1999;18:77–91. doi: 10.1016/S0278-5919(05)70131-9. [DOI] [PubMed] [Google Scholar]
- 81.Kocabey Y, Nyland J, Isabell WM, Caborn DN. Patient outcomes following T-Fix meniscal repair and a modifiable, progressive rehabilitation program, a retrospective study. Arch Orthop Trauma Surg. 2004;124:592–596. doi: 10.1007/s00402-004-0649-6. [DOI] [PubMed] [Google Scholar]
- 82.Bryant D, Dill J, Litchfield R, et al. Effectiveness of bioabsorbable arrows compared with inside –out suturing for vertical, repairable meniscal lesions. American Orthopedic Society for Sports Medicine. 2007;35(7):889–896. doi: 10.1177/0363546506298582. [DOI] [PubMed] [Google Scholar]
- 83.O’Shea JJ, Shelbourne KD. Repair of locked bucket-handle meniscal tears in knees with chronic anterior cruciate ligament deficiency. AJSM. 2003;31(2):216–220. doi: 10.1177/03635465030310021001. [DOI] [PubMed] [Google Scholar]
- 84.Noyes FR, Barber-Westin SD. Arthroscopic Repair of meniscus Tears Extending Into the Avascular Zone With or Without Anterior Cruciate Ligament Reconstruction in Patients 40 years of age and Older. Arthroscopy. The Journal of Arthrocopic and Related Surgery. 2000;16(8):822–829. doi: 10.1053/jars.2000.19434. [DOI] [PubMed] [Google Scholar]
- 85.Richards DP, Barber FA, Herbert MA. Compressive loads in longitudinal lateral meniscus tears: a biomechanical study in porcine knees. Arthroscopy. 2005;21:1452–1456. doi: 10.1016/j.arthro.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 86.Becker R, Wirz D, Wolf C, et al. Measurement of meniscofemoral contact pressure after repair of bucket-handle tears with biodegradable implants. Arch Orthop Trauma Surg. 2005;125:254–260. doi: 10.1007/s00402-004-0739-5. [DOI] [PubMed] [Google Scholar]
- 87.Gao J, Wei X, Messner K. Healing of the anterior attachment of the rabbit meniscus to bone. Clin Orthop Relat Res. 1998;348:246–258. doi: 10.1097/00003086-199803000-00036. [DOI] [PubMed] [Google Scholar]
- 88.Johal P, Williams A, Wragg P, et al. Tibiofemoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using “interventional” MRI. J Biomech. 2005;38:269–276. doi: 10.1016/j.jbiomech.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 89.Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clinical Orthopedics and Related Research. 1975;109:184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 90.Thompson WO, Thaete FL, Fu FH, Dye SF. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med. 1991;19(3):210–215. doi: 10.1177/036354659101900302. [DOI] [PubMed] [Google Scholar]
- 91.Tienen TG, Buma P, Scholten JGF, et al. Displacement of the medial meniscus within the passive motion characteristics of the human knee joint: An RSA study in human cadaver knees. Knee Surg Sports Traumatol Arthrosc. 2005;13:287–292. doi: 10.1007/s00167-004-0511-y. [DOI] [PubMed] [Google Scholar]
- 92.Johal P, Williams A, Wragg P, et al. Tibiofemoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using “interventional” MRI. J Biomech. 2005;38:269–276. doi: 10.1016/j.jbiomech.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 93.Kawai Y, Fukubayashi T, Nishino J. Meniscal suture an experimental study in the dog. Clin Orthop. 1989;243:286–293. [PubMed] [Google Scholar]
- 94.Fritz JM, Irrgang JJ, Harner CD. Rehabilitation following allograft meniscal transplantation: a review of the literature and case study. Journal of Orthopedic Sports Physical Therapy. 1996;24(2):98–106. doi: 10.2519/jospt.1996.24.2.98. [DOI] [PubMed] [Google Scholar]
- 95.Freeman MA, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:669–677. [PubMed] [Google Scholar]
- 96.Johansson H, Sjolander P, Soojka P. Activity in receptor afferents from the anterior cruciate ligament evokes reflex effects on fusimotor neurones. Neurosci Res. 1990;8:54–59. doi: 10.1016/0168-0102(90)90057-L. [DOI] [PubMed] [Google Scholar]
- 97.Cavanaugh JT, Gately CT. Meniscal Repair and Transplantation. In Postsurgical Rehabilitation Guidelines for the Orthopedic Clinician Cioppa-Mosca J, Cahill JB, Cavanaugh JT, et al (eds) Elsevier Publishers pp. 453-468, 2006
- 98.Cavanaugh JT, Stump TJ. Forward step down test. J Orthop Sports Phys Ther. 2000;30(1):A-46. [Google Scholar]
- 99.Daniel DM, Malcolm L, Stone ML, et al. Quantification of knee stability and function. Contemp Orthop. 1982;5:83–91. [Google Scholar]
- 100.Barber SD, Noyes FR, Mangine RE, et al. Quantitative assessment of functional limitations in normal and anterior cruciate ligament deficient knees. Clin Orthop. 1990;255:204–214. [PubMed] [Google Scholar]