Abstract
Diabetes mellitus is a prevalent chronic health condition associated with significant morbidity and mortality. Those with diabetes must acquire self-efficacy in the tasks necessary for them to successfully manage their disease. In this study, a controlled pre- and post-design was used to determine the effect of an adult support and education group visit program embedded in an urban academic family medicine practice on weight and the achievement of treatment goals for hemoglobin A1C, low-density lipoprotein (LDL) blood concentration, and blood pressure (BP) several months after it was implemented. Participants in the program were matched to a comparison group based on age, gender, race/ethnicity, and zip code group, a surrogate marker for socioeconomic status. The distribution of demographic characteristics and co-morbidities was similar between the groups. Significant increases occurred in the proportion of participants achieving both an A1C concentration <7% (CMH=4.6613, p = 0.0309) while controlling for baseline AIC concentration, and a BP<140/90 mm Hg (CMH=5.61, p = 0.018) controlling for baseline BP compared to the comparison group. The hemoglobin A1C concentration declined in 76.9% of the participants in the group visit program compared to 54.3% in the comparison group (CMH=8.9911, p = 0.0027). The increase in the proportion of group visit participants achieving the target LDL concentrations did not achieve statistical significance. The proportion of participants who lost weight was similar to that in the comparison group. Early experience with the program was encouraging and suggested it may improve patients’ management of their diabetes mellitus in an urban, predominantly African American population.
Keywords: Diabetes mellitus, Group visit program, Family practice, Outcomes
Introduction
The estimated prevalence of diagnosed diabetes in the United States rose from 4.2% in 2002 to 8.3% in 2010.1 Diabetes causes substantial chronic disability and decreased quality of life, and is the leading cause of kidney failure, nontraumatic lower-limb amputations, and new cases of blindness among adults in the USA. In addition, diabetes is a major cause of heart disease and stroke and is the seventh leading cause of death in the USA.1 It is estimated that diabetes mellitus was responsible for $174 billion in excess medical expenditures and $58 billion in lost productivity costs in 2011.1
Many of the complications of diabetes can be prevented with optimal diabetes management. The role of self-management in achieving optimal diabetes management and control to prevent complications is fundamental because individuals with diabetes make multiple decisions on a daily basis that impact control of their diabetes including decisions about diet, physical activity, and taking medications.2 Self-management support is demonstrated to enable people with diabetes to assume responsibility for managing their condition.2,3 It has been proposed that this support include individualized diabetic assessment, collaboration between diabetic patients and providers in goal setting, learning of concrete behaviors and skills necessary to successfully manage the disease, and ongoing support for the desired behavior change.3 Cochrane reviews of randomized controlled trials and qualitative reviews that evaluated interventions to improve the management of diabetes mellitus in primary care, outpatient, and community settings support the important role of self-management education.4–6
In July 2009, a large, urban, academic family medicine practice affiliated with Thomas Jefferson University launched a group visit program for its adult diabetic patients to engage and support them in the management of their disease. The 4-week program is led by an interdisciplinary team that includes a diabetes health educator, a nurse, a pharmacist, and resident and attending physicians. The group meets weekly for 3 h. New patients begin the program with a brief visit with a resident physician. Medications are adjusted, lab tests are ordered, immunizations are given, and referrals are arranged as needed during this initial visit. Each of the four sessions includes time for discussion of a self-management related topic, development of individual action plans for managing the disease, and an opportunity to visit with a family medicine physician. The diabetes health educator or other team member leads the discussion of the diabetes-related topic, such as nutrition, blood glucose monitoring, and prevention of diabetic complications. Patients are recruited for the program within the practice via postings and physician referrals. The purpose of this study was to evaluate the effect of this diabetes support and education group visit program on the achievement of hemoglobin A1C concentration, low-density lipoprotein concentration and blood pressure (BP) targets, and on weight changes several months after the program began.
Methods
A controlled pre- and post-study design was used to compare differences in the measured outcomes between the diabetic patients in the group visit program and those in a matched comparison group. The group visit and the comparison patients were drawn from the family medicine practice. They were at least 18 years of age, had a diagnosis of type 2 diabetes mellitus, and had at least one visit to the practice between July 2008 and June 2009. Members of the intervention group were patients who had participated in the group visit program at least once during the period from July through September 2009. They were identified from attendance records. Other adult diabetic patients in the family practice were eligible for inclusion in the comparison group.
Members of the intervention and comparison groups were matched on gender, one of five age categories (18–19, 20–34, 35–44, 45–64, and ≥65 years), one of three race/ethnicity categories (African American, Caucasian, or others) and one of three residential zip code groups. Zip code was used as a surrogate measure of socioeconomic status because of the observed relationship between zip code group and percent of households living below 200% of the federal poverty level. Each patient in the group visit program was matched on these variables with up to four comparison patients, who were selected randomly from the group of diabetic patients who did not participate in the program.
The other baseline variables collected on participants in the intervention and comparison groups were height; smoking history; diagnoses of hypertension, hyperlipidemia, and depression; albumin:creatinine ratio; type of treatment for diabetes mellitus; and prescriptions for an angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB), a statin and aspirin. The variables recorded for both groups before and after the group visit program had met for several months were weight, body mass index, number of office visits, hemoglobin A1C concentration, LDL concentration, and BP. The baseline variables of each group, and the changes from baseline, with adjustment for baseline values during the follow-up period of 7 months, were compared with the Cochran Mantel Haenszel (CMH) statistic. The number of office visits during the follow-up period was also compared. The level of significance for group comparisons was set at an alpha value of less than 0.05. SAS Enterprise Guide 4.1 was used for data analysis. The study was approved by the Thomas Jefferson University Institutional Review Board.
Results
The 64 group visit program participants in 27 strata were identified. Data were available for 52 of these participants and 236 comparison group patients in 26 strata. The distribution of the baseline demographics, comorbidities, and other measured characteristics of patients in the group visit program and the comparison group are shown in Tables 1 and 2. The majority of patients in both groups were female, at least 45 years of age, African American and obese. The prevalences of hypertension, hyperlipidemia, depression, coronary artery disease, microalbuminuria, and proteinuria were similar between the study groups. Most patients’ diabetes mellitus was treated with oral antidiabetic medications, sometimes in combination with insulin. A statin, low-dose aspirin, and either an ACE inhibitor or an ARB were prescribed for a similar proportion of patients in both groups. Participants in the group visit program tended to have more office visits from July 2009 through the follow-up period (CMH statistic 14.9603, p = 0.0001).
Table 1.
Characteristics of group visit and comparison patients
| Group visit program (N = 52) | Comparison group (N = 236) | p Values | |
|---|---|---|---|
| Age group, years (%) | 0.3778 | ||
| 20 to 34 | 3.9 | 1.7 | |
| 35 to 44 | 9.6 | 10.6 | |
| 45 to 64 | 59.6 | 69.1 | |
| 65 and older | 26.9 | 18.6 | |
| Race/ethnicity (%) | 0.2811 | ||
| African American | |||
| Caucasian | 80.8 | 87.3 | |
| Other | 10.2 | 7.2 | |
| Gender, female (%) | 6.8 | 5.5 | 0.5953 |
| Comorbidities (%) | 69.2 | 72.9 | |
| Coronary artery disease | 0.6684 | ||
| Depression | 15.4 | 13.1 | 0.2634 |
| Hyperlipidemia | 23.1 | 16.5 | 0.5310 |
| Hypertension | 80.8 | 84.3 | 0.5757 |
| Microalbuminemia | 94.2 | 92 | 0.2655 |
| Proteinuria | 24 | 17.5 | 0.2655 |
| Current smoker (%) | 8 | 10.8 | 0.4522 |
| 13.5 | 17.8 |
Table 2.
Characteristics of group visit and comparison patients
| Group visit program (N = 52) | Comparison group (N = 236) | p Values | |
|---|---|---|---|
| Body mass index (%) | 0.1594 | ||
| Underweight | 0 | 0.4 | |
| Normal weight | 4.1 | 8.5 | |
| Overweight | 16.3 | 21.3 | |
| Obese | 44.9 | 46.4 | |
| Morbidly obese | 34.7 | 23.4 | |
| Diabetes mellitus treatment (%) | 0.7936 | ||
| Insulin only | 15.4 | 6.8 | |
| Oral medication | 59.6 | 67 | |
| Insulin and oral medication | 19.2 | 18.2 | |
| Not documented | 5.8 | 8.1 | |
| Baseline A1C>7% (%) | 63.5 | 54.2 | 0.226 |
| Baseline LDL≥130 mg /dl (%) | 25.5 | 23.4 | 0.7515 |
| Baseline LDL≥100 mg /dl (%) | 58.8 | 52.3 | 0.4009 |
| Baseline BP≥140/90 mm Hg (%) | 38.5 | 35.2 | 0.6545 |
| Baseline BP≥130/80 mm Hg (%) | 65.4 | 66.1 | 0.9214 |
The attendance of individual participants in the group visit program during the study was variable. Participants attended a range of 1–14 sessions. The average number of sessions attended ± s.d. was 2.7 ± 2.8; the median number 1. Of the participants, 46% attended at least three sessions.
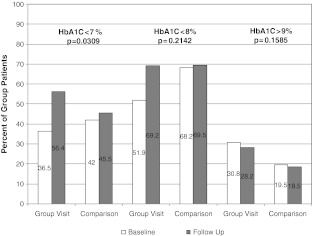
The changes from baseline in the proportion of diabetic patients achieving hemoglobin A1C values, low-density lipoprotein (LDL) blood concentrations, and BP endpoints in the group visit program and the comparison group are compared in Figures 1 and 2. So that A1Cs that were normal (<7%) at the time of the initial measurement would not bias the results, the A1C outcomes were adjusted for baseline A1C concentration. The proportion of patients in the group visit program with a hemoglobin A1C concentration less than 7% in the follow-up period compared to the baseline period was statistically significant (CMH=4.6613, p = 0.0309) Adjustment for the number of office visits during the follow-up period did not show any effect (CMH 0.6507, p = 0.4199). The hemoglobin A1C concentration declined in 76.9% of the patients in the group visit program compared to 54.3% in the comparison group (CMH=8.9911, p = 0.0027). The change in the proportion of patients with a hemoglobin A1C less than 8% or greater than 9% in the intervention group was not significantly different from that observed in the comparison group.
FIGURE 1.
Observed changes between baseline and follow-up periods in percentage of patients achieving hemoglobin A1C (HbA1C) targets in the group visit program and comparison group.
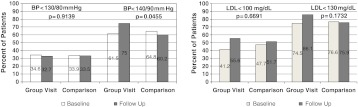
FIGURE 2.
Observed changes between baseline and follow-up periods in percentage of patients achieving BP and low-density lipoprotein (LDL) concentration targets in the group visit program and comparison group.
There was greater improvement in the proportion of diabetics whose BP was less than 140/90 mm Hg in the intervention group than in the comparison group (CMH=3.9999, p = 0.0455). The improvement persisted after adjustment for the baseline BP (CMH=5.602. p = 0.0179) and for the number of office visits during the follow-up period (CMH=3.8936, p = 0.0485). However, the change in the proportion of diabetics with a BP less than 130/80 mm Hg was similar whether or not adjustments were made for the baseline BP or the number of office visits.
The improvement in the percentage of group visit program participants who had a low-density lipoprotein blood concentration less than 130 and 100 mg /dl during the follow-up period was not significantly different from that observed in the comparison group (unadjusted CMH=1.8551 and p = 0.1732 for LDL<130 mg /dl, and CMH=0.1827 and p = 0.6691 for LDL<100 mg /dl, respectively). This remained true when the change from the baseline period was adjusted for the baseline value (CMH=1.9813 and p = 0.1593 for LDL<130 mg /dl, and CMH=1.0843 and p = 0.2977 for LDL<100 mg /dl), and for the number of office visits during the follow-up period (CMH=0.2.2771 and p = 0.1313 for LDL<130 mg /dl, and CMH=0.1609 and p = 0.6883 for LDL<100 mg /dl).
The changes in weight from the baseline to the follow-up period were similar among those in the group visit program and the comparison group. The median weight loss was −3.5 pounds (IQR −11 to +5 pounds) in the intervention group and −1 pound (IQR −7 to +3.8 pounds) in the comparison group. The weight changes ranged from a loss of 89 pounds to a gain of 28 pounds among those participating in the group visit program and from a loss of 44 pounds to a gain of 25 pounds among those in the comparison group. Fifty-four percent in the group visit program and 44% of those in the comparison group lost weight (CMH=1.5723, p = 0.2099).
Discussion
Participation in the Jefferson Family Medicine group visit program was associated with improvement in the proportions of diabetics with a BP less than 140/90 mmHg, a significant decline in A1C, and a hemoglobin A1C concentration less than 7% in a predominantly urban African American population. Although the evaluation did not demonstrate that participation in the program was associated with improvement in the percentage of diabetics who achieved the target low-density lipoprotein concentrations, the change from baseline in this endpoint was in the desired direction. In fact, the change from baseline in all endpoints except weight was in the desired direction to a greater degree for those who attended the group visit program.
Group visits can improve the quality of chronic disease management compared to the usual office visit.6 They provide more time for self-management education and skill building and may reduce perceived barriers to behavior change.6 Group visits can improve patient satisfaction by increasing patients’ trust in providers and promoting patients’ engagement in their care.6,7 Studies have demonstrated group visit programs can reduce emergency department visits, visits to specialists and hospital admissions and the associated costs of care.6,8 However, the heterogeneity of studies makes it difficult to consistently demonstrate their effectiveness at improving intermediate outcomes of care.5,6,9,10
A Cochrane review found that there were few studies of group-based training for self-management strategies in predominantly African American populations with type 2 diabetes mellitus.5 The authors concluded further studies were required to confirm the efficacy of group-based training programs in African Americans and other ethnic minorities. Such studies in African American adults are important because older African Americans have a higher incidence of diabetes and a higher rate of hospitalization than whites.11 The rate of hospitalization for the long-term complications of diabetes was higher among older African Americans than whites age 65 years and older—806 admissions per 100,000 population among African Americans compared to 264,000 per 100,000 among the white population.11 This study provides evidence of the effectiveness of group-based training for African Americans with diabetes.
This study had some limitations. It was not possible to randomly assign study patients to the group visit and comparison groups. A quasi-experimental matched controlled pre- and post-study design was used to reduce the risk of bias. Those in the group visit program and the comparison group were matched on gender, age, race, and zip code group in an effort to control for the possible influence these variables may have on the measured outcomes. Nonetheless, there may have been unmeasured characteristics of patients who volunteered to participate in the program that differed from those in the comparison group. It was not possible to measure change from baseline because of the lack of baseline or follow-up data on some group visit program participants and comparison patients. An effort was not made to define and select near matches when exact matches were not available.
It has been observed that improvement in diabetes-related outcomes may be related to the dose of the intervention participants receive.12 In this study, a larger impact of the group visit program may have been observed had a greater proportion of patients participating in the group visit program attended more sessions. Only 46% of those who participated in the program attended at least three of the four sessions.
The evaluation of the group visit program took place during the first year of its implementation. As a result, the number of initial participants in the program was modest. In addition, the program was assessed early in its inception, before the program, its process, and educational materials were well-established.
Conclusion
Early experience with the group visit program was encouraging and suggested it may improve patients’ management of their diabetes mellitus in an urban, predominantly African American population.
Acknowledgments
We thank the members of the Jefferson Family Medical Associates Southeastern Pennsylvania (SEPA) Chronic Care Collaborative Committee (Janis Bonat, Nancy Brisbon, Victor Diaz, Kathleen Hilbert) for their advice and assistance; members of the team for their leadership and participation; the medical residents for leading group sessions; and the patients who engage in the program and contribute suggestions for the program’s improvement.
Contributor Information
Jeffrey A. Reitz, Email: jreitz@christianacare.org
Mona Sarfaty, Email: mona.sarfaty@jefferson.edu.
Brooke Salzman, Email: brooke.salzman@jefferson.edu.
References
- 1.National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 2.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Affairs. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 3.Fisher EB, Brownson CA, O’Toole ML, Shetty G, Anwuri VV, Glasgow RE. Ecological approaches to self-management: the case of diabetes. Am J Public Health. 2005;95(9):1523–1535. doi: 10.2105/AJPH.2005.066084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Renders CM, Valk GD, Griffin SJ, Wagner E, van Eijk JT, Assendelft WJJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev. 2001;(1):CD001481. [DOI] [PMC free article] [PubMed]
- 5.Deaken TA, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;(2):CD003417. [DOI] [PubMed]
- 6.Jaber R, Braksmajer A, Trilling JS. Group visits: a qualitative review of current research. J Am Board Fam Med. 2006;19:276–290. doi: 10.3122/jabfm.19.3.276. [DOI] [PubMed] [Google Scholar]
- 7.Davis AM, Sawyer DR, Vinci LM. The potential of group visits in diabetes care. Clin Diabetes. 2008;26(2):58–62. doi: 10.2337/diaclin.26.2.58. [DOI] [Google Scholar]
- 8.Clancy DE, Dismuke CE, Magruder KM, Simpson KN, Bradford D. Do diabetes group visits lead to lower medical charges. Am J Manage Care. 2008;14:39–44. [PubMed] [Google Scholar]
- 9.American Diabetes Association Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(Suppl 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riley SM, Marshall ES. Group visits in diabetes care: a systematic review. Diabetes Educ. 2010;36:936–944. doi: 10.1177/0145721710385013. [DOI] [PubMed] [Google Scholar]
- 11.Fitzner K, Dietz DA, Moy E. How innovative treatment models and data use are improving diabetes care among older African American adults. Pop Health Manage. 2011;14:143–155. doi: 10.1089/pop.2010.0012. [DOI] [PubMed] [Google Scholar]
- 12.Brown SA, Blozis SA, Kouzekanani K, Garcia AA, Winchell M, Hanis CL. Dosage effects of diabetes self-management education for Mexican Americans. Diabetes Care. 2005;28:527–532. doi: 10.2337/diacare.28.3.527. [DOI] [PMC free article] [PubMed] [Google Scholar]