Abstract
Pelvic fixation is most frequently indicated in the pediatric population for the treatment of neuromuscular scoliosis with significant pelvic obliquity. Neuromuscular scoliosis surgery is associated with a high risk of complications, and this is further increased by extension of fusion to the sacrum. Numerous techniques have been described for pelvic fixation associated with a long spine fusion each with its own set of specific benefits and risks. This article reviews the contemporary surgical techniques of pelvic fixation used to extend a spine fusion to the sacrum and pelvis focusing on the management of neuromuscular scoliosis, including their biomechanical rationale, results, and complications.
Keywords: Pediatrics, Pelvic fixation, Scoliosis surgery, Neuromuscular scoliosis, Pelvic obliquity, Lumbosacral fusion, Sacropelvic unit, Galveston technique, Iliac screws, Iliosacral screws, Maximum width (MW) construct, Jackson intrasacral rod fixation, S-rods, Dunn McCarthy technique, Sacral alar screws, S2 Iliac screws, Transiliac fixation, Sacral bar
Introduction
Neuromuscular scoliosis surgical treatment is the most common indication in the pediatric population for extension of a long spine fusion to the pelvis to address the commonly associated pelvic obliquity [1]. Pelvic fixation is occasionally needed at the pediatric age for the treatment of high-grade spondylolisthesis, congenital lumbosacral scoliosis, and as part of a growing rod construct for managing early-onset scoliosis [2–7]. A progressive pelvic obliquity with an unbalanced spine deformity adversely affects sitting balance, pressure, and quality of life [8–12].
Pelvic obliquity is defined in the Scoliosis Research Society revised glossary of terms as an angulation of the pelvis from the horizontal in the frontal plane. According to Dubousset, it is best defined as “any fixed malalignment existing between the spinal and pelvic structures either in the frontal, sagittal or horizontal planes” [13]. Pelvic obliquity can originate from leg length inequality, contractures about the hip, spinal deformity, or as a combination of these causes [14]. A frequently associated transverse plane pelvic asymmetry further complicates the three-dimensional understanding and surgical treatment of this deformity [15•].
Neuromuscular scoliosis carries a higher morbidity compared to idiopathic and congenital scoliosis [16–22, 23•, 24]. Extending the fusion to the sacrum in these frail patients further increases the technical difficulty of the procedure, operative time, blood loss, and risk of infection [25]. The surgeon should be familiar with various techniques of pelvic fixation for pediatric deformity correction including their advantages and potential complications.
Pelvic obliquity measurement
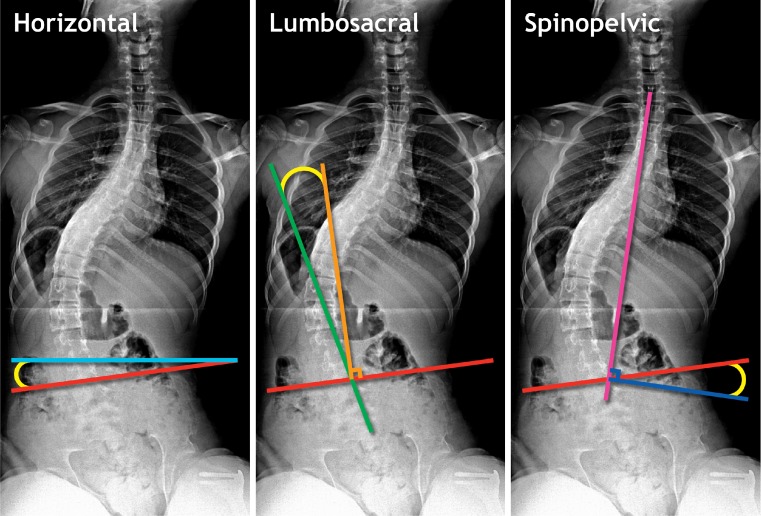
Anteroposterior radiographs of the spine including the pelvis should be used preferably in the sitting position for nonambulatory patients [26]. Three methods of radiographic measurement of pelvic obliquity are commonly used (Fig. 1). Osebold et al. described horizontal pelvic obliquity as the angle subtended by a line drawn between the most proximal points on the iliac crest and a line drawn parallel to the lower end of the roentgenogram [27]. Allen and Ferguson used a lumbosacral measurement represented by the angle subtended by a line drawn through the spinous process of L4 and L5 and a perpendicular though the iliac crest line [28]. Other authors estimate pelvic obliquity by measuring the angle between a line drawn perpendicular from the middle of T1 to S1 and the iliac crest line [29]. Because of the uncertainty of a horizontal standard line, the lumbosacral measurement and the spinopelvic angle should be theoretically less influenced by patient positioning than the horizontal pelvic obliquity measurement. However, a radiographic study has demonstrated that among these three measurements, the one with the least interobserver and intraobserver variability was the horizontal pelvic obliquity [26].
Fig. 1.
Methods of radiographic measurement of pelvic obliquity used on anteroposterior radiographs of the spine including the pelvis: horizontal pelvic obliquity as described by Osebold et al. (angle subtended by a line drawn between the most proximal points on the iliac crest (red) and a line (light blue) drawn parallel to the lower end of the roentgenogram); lumbosacral measurement from Allen and Ferguson (angle subtended by a line drawn through the spinous process of L4 and L5 (green) and a perpendicular (orange) though the iliac crest line); spinopelvic angle as described by Maloney et al. (angle between a line drawn perpendicular (dark blue) from the middle of T1 to S1 (magenta) and the iliac crest line)
Indication for pelvic fixation
The most frequent reason to fuse the spine to the pelvis in the pediatric population is scoliosis and associated fixed significant pelvic obliquity in a nonambulatory neuromuscular patient [1]. The main goal of surgical treatment is to provide a solid and aligned spinopelvic unit in both planes to provide firm sitting balance [30]. This outcome is usually achieved with a long fusion from the upper thoracic spine to the sacrum/pelvis [1] although the need to extend the fusion to the pelvis in certain cases can be debated. While fusion down to the pelvis is generally recommended, a pelvic obliquity of <15° can be left uninstrumented [31–35, 36•].
Traditionally, extending spinal fusion to the pelvis was not recommended in ambulatory neuromuscular patient with scoliotic deformity and associated pelvic obliquity [37, 38] because of the suspected risk of losing walking capacity postoperatively. This widespread myth is not supported by recent literature. While a decrease of functional status is expected during the first six months after surgery [39], no alteration of ambulatory function at midterm is expected for patients with spastic cerebral palsy after long spine fusion including the pelvis [40]. The confounding factor of the natural history of ambulatory deterioration in progressive neuromuscular conditions such as Duchenne Muscular Dystrophy and Spinal Muscular Atrophy is often incorrectly associated with loss of ambulation of scoliosis treatment. On the contrary, spine fusion extending to the pelvis in patients with myelomeningocele is associated with permanent loss of ambulation capacity in 27 to 75 % of patients, especially in exercise walkers [41–43]. Ambulation in patients with high-level myelomeningocele likely relies on a mobile lumbosacral junction to thrust the lower limbs forward [43], and therefore, fusion to the pelvis can decrease ambulatory ability in these patients. It is imperative that such patients understand this possible ambulation change in the context of the natural history of ambulatory status; many patients with a high-level lesion also lose their walking ability during their teenage years, an occurrence likely attributable to increasing body weight with growth or obesity [44].
Operative techniques
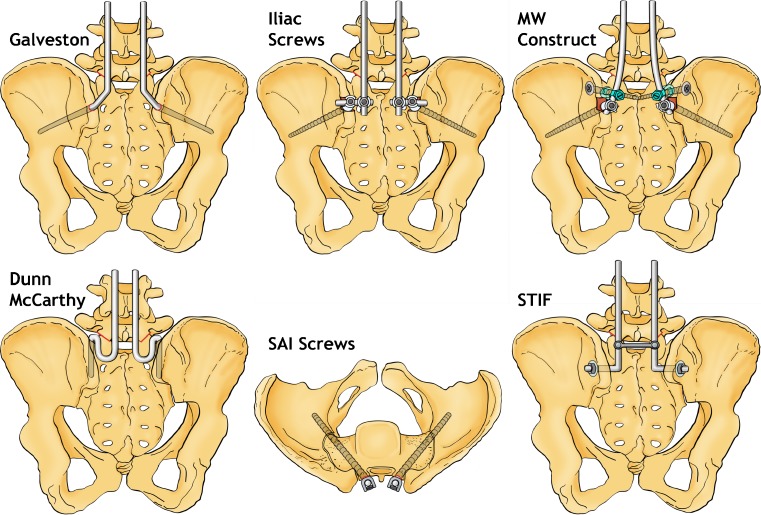
Three zones of fixation to the sacral pelvic unit have been described anatomically: zone 1 is comprised of the S1 vertebral body and the most cephalad regions of the sacral ala; zone 2 consists of the sacrum below zone 1; zone 3 includes the ilium bilaterally [45]. Biomechanical findings support the relevance of this classification in two ways. There is an increase of biomechanical strength of fixation from zone 1 to zone 3, and each mode of fixation in each zone has been associated with unique modes of failure [46–51]. Biomechanically, sacral screws alone represent the weakest form of sacropelvic anchorage in long spine fusion to the sacrum with an associated high rate of failure of fixation [52]. The techniques used for treating pediatric neuromuscular scoliosis with significant pelvic obliquity are most commonly zone 3 fixation types (Fig. 2).
Fig. 2.
Sacropelvic fixation techniques used for the treatment of pediatric neuromuscular scoliosis: Galveston instrumentation with intrailiac smooth L-rods; Iliac screws anchored to the spinal rod with a lateral connector; Maximum width (MW) spinopelvic construct, combining iliac and iliosacral screws; S-rods according to Dunn and McCarthy; Sacral alar iliac (SAI) screws (top view); Spinopelvic transiliac fixation (STIF) implant system
Galveston technique
The use of bilateral intrailiac L-rod fixation for a long spine fusion to the pelvis is one of the most well documented fixation techniques in the literature for neuromuscular pediatric patients [28]. Its use is becoming less common with the development and availability of modern spine instrumentation. Traditionally, it was associated with the Luque construct of sublaminar segmental wire fixation at the lumbar and thoracic spine [53].
Depending on the thickness of the iliac crest and the patient size, 6.35 mm (1/4 inch) or 4.75 mm (3/16 inch) diameter rods are used combined with 16-gauge sublaminar wires for spinal anchorage [19]. An intracortical pathway is made through the distal ilium. Staying as distal as possible in the ilium will help to obtain the longest and largest bonny tunnel [1]. The rod is bent into 3 segments: one intra-osseous portion that will be inserted in the ilium, one that runs over the posterior surface of the sacrum, and a third that passes across the length of the spinal segment to be instrumented. The rod penetrates the ilium to the posterior sacral surface at a level of the lower margin of the posterosuperior iliac spine (PSIS). It should travel within 1.5 cm of the sciatic notch and be inserted to a depth of al least 6 cm, ideally 9 to 10 cm, depending on the anatomy of the patient [54].
Advantages of this technique of pelvic fixation are its low profile and superior resistance to flexion forces. Its corrective power regarding pelvic obliquity correction in neuromuscular patients ranges from 40 % to 77 % in retrospectives series at final follow-up [19, 55–59]. But as the rod is smooth and crosses the unfused sacroiliac joint, its mechanical mode of failure is proximal displacement between the iliac tables, leading to the “windshield wiper” effect over time [46]. This radiological finding is not always associated with a defect of fusion. The lumbosacral pseudarthrosis rate is about 5 % [19]. Another drawback of the Galveston fixation is that it requires complicated three-dimensional bending of the rods for proper placement within the ilium. A preoperative hyperkyphotic spine (thoracic, thoracolumbar, or lumbar) is a contra-indication for using the Galveston technique as this is associated with increased incidence of posterior rod pull-out and subsequent distal loss of sagittal plane correction in spastic cerebral palsy patients. An anterior lumbar release and non-instrumented anterior fusion in this subset of patients further increases the risk for posterior pullout of the rods from the pelvis [60].
Evolutions of the original Galveston pelvic fixation technique include distal rigid cross-locking of the rods with transverse connector, the “unit” rod, and augmentation of fixation with S1 pedicle screws [52, 61, 62]. Adding an inferior long transverse connector in horizontal distraction (device for transverse traction, DTT) to push against the rods will prevent them from backing out of iliac wings [19, 52, 55, 63]. Because of the risk of translation (compromising correction of pelvic obliquity) or rotation of two unlinked L-rods with respect to one another, Moseley and Koreska designed the “unit” rod [61]. It is made of a single continuous stainless steel 6.35 mm (1/4 inch) with a proximal U-bend. Unit rods are additionally pre-shaped in three dimensions with kyphosis, lordosis, and pelvic portions to simplify their insertion. The correction of pelvic obliquity associated with this implant ranges from 57.8 % to 86 % at longest follow-up in retrospective series with pseudarthrosis affecting 0 to 5.9 % of patients [29, 40, 61, 64–66].
Finally, some authors modify the original Galveston technique with the addition of a DTT and S1 pedicle screws with the aim to increase the strength of the sacral pelvic anchorage. Achieving anterior cortical sacral purchase with medially converging sacral pedicle screw in a triangular fashion creates a three-point fixation system with increased pelvic obliquity control. This concept is supported by biomechanical in vitro data demonstrating that it significantly increased resistance to failure and stiffness at the lumbosacral junction [48]. Marchesi et al. reported the clinical efficiency of this modification in a consecutive series of 25 patients with Duchenne’s neuromuscular scoliosis with 74 % of pelvic obliquity correction at follow-up and no pseudarthrosis [62].
Iliac screws
Together with the recent trend to treat neuromuscular scoliosis patients with pedicle screws instrumentation through a posterior-only approach, the use of screws instead of smooth rods to anchor the ilium is increasingly documented in the literature [32, 33, 67, 68]. It offers the theoretical advantage of diminishing implant pullout or cutout associated with a smooth rods inserted in the iliac wings.
Locally, the iliac apophysis and crest must be removed with a rongeur to allow maximal recession of the screw heads to decrease the profile of the implant in order to minimize the risk of skin sores due to screw head prominence. Screws 6 to 8 mm in diameter (50 to 70 mm long) are inserted in each iliac wing with an entry point 2 cm superior to the PSIS. The screws are aiming toward the region above the greater sciatic notch. Human cadaveric studies have demonstrated that the longer intrailiac path from the PSIS is the one aiming towards the anterior inferior iliac spine (AIIS). This direction corresponds to a constantly straight substantial column of bone that is amenable to safe instrumentation, with 8 mm screws providing at least three times stronger anchorage for spinal instrumentation compared to standard Galveston technique with 6.25 mm smooth rods [69, 70]. They are connected to the longitudinal rod on each side with a lateral connector. Most authors report this technique for the treatment of neuromuscular scoliosis in pediatric patients without additional sacral fixation. Proximal spinal anchorage is done with sublaminar wires [67, 71] or with pedicle screws from the L5 level [32, 33, 72].
Pelvic obliquity correction associated with such techniques range from 59 to 83.3 % with no pseudarthrosis reported [32, 67, 68, 71, 72]. Complications directly involving iliac screws are mainly rod disengagement from the lateral connector and radiolucencies around the screws [67, 71]. Interestingly, the addition of a second iliac screw on each side was associated with significantly fewer implant-related complications in a comparative retrospective review. This additional pair of screws is inserted with an entry point 2 cm further superiorly to the first ones and is attached to the rod with a lateral connector as well [71]. The use of iliac screws combined with sacral screws as a low profile alternative to iliosacral screws in neuromuscular patients with body weight less than 35 kg has been recently reported in a prospective study [73]. This construct was associated with 81.7 % pelvic obliquity correction at follow-up and with no lumbopelvic pseudarthrosis. The authors of this study reported the use of a horizontal 4.5 mm titanium rod to connect the two sacral screws and the two iliac screws. This pelvic segmental anchorage was then linked to each spinal rod on each side with a 90° long-offset connector (“T-construct”). In addition to its low profile, it also offers the theoretical advantage of a three-dimensional four-point fixation in three different bones at the sacropelvic level, compared with iliac screws alone.
Iliosacral screws
Iliosacral screws were first introduced as one of the three main techniques of the Cotrel-Dubousset (CD) sacral instrumentation, the two others being alar staples and sacral screws [74]. Sacral staples have been used in the past for long spine fusion to the pelvis with posterior distraction systems such as Harrington instrumentation; they are not considered to provide sufficient stability except in distraction and result in high rates of lumbosacral pseudarthrosis [75, 76]. Sacral screws in the pediatric patient population are most often used for short lumbopelvic fusion such as in the treatment of spondylolisthesis. This screw configuration alone at the pelvic level provides relatively good control in the sagittal plane; however, the power of correction in the frontal plane is less satisfactory because of the medial position of the screws as compared to zone 3 fixation techniques resulting in a shorter lever arm in the frontal plane and potentially less corrective power of pelvic obliquity. Iliosacral screws offer the theoretical advantage of increasing the corrective lever arm and bony purchase by adding to the fixation area of the S1 pedicle using the two cortices of the posterior ilium [77].
Traditionally, cannulated 7 mm screws are used. After L5 inferior facetectomies, guide pins are inserted bilaterally with an entry point slightly proximal and superior to the posterior superior iliac spine, 1 cm below the iliac crest. They are directed to enter the sacrum at the base of the ascending articular process of S1 and aimed at the opposite anterolateral cortex of S1 with a medial orientation of 45° for increased pull-out strength into the S1 pedicle [78]. They are passing posterior and proximal to the sacroiliac joint. The iliosacral screw on each side is finally connected to the spinal rod with a regular lumbar hook or, ideally, with a specific connector designed with two canals, one for the screw and one for the rod [74, 77].
This instrumentation technique has shown its efficiency in retrospective and prospective studies with pelvic obliquity correction ranging from 39.1 to 84 % and low rates of lumbosacral pseudarthrosis (0 to 0.65 %) [77, 79, 80]. Complications directly involving this type of construct are mainly early unilateral screw pull-out and rod disengagement. Screw dislodgement can be treated percutaneously by changing for a longer screw [77, 80, 81]. To diminish the difficulty of three-dimensional distal rod contouring associated with this type of fixation in case of pelvic obliquity, Zahi et al. proposed first linking the iliosacral screws to a short rod on each side instead of directly extending the spinal rods down to the iliosacral screws. Compression and distraction maneuvers are then applied between these short rods and the long spinal rods. The two short pelvic rods are subsequently connected to the long rods on each side using parallel connectors. This technique has been shown to be as efficient in terms of pelvic obliquity correction and lumbopelvic fusion rates as the conventional iliosacral screws technique in the comparative prospective study [80].
Maximum width (MW) spinopelvic construct
In 1999, Arlet et al. introduced the idea of combining the two threaded implants with the highest biomechanical fixation strength to the pelvis [48], iliosacral and iliac screws, in a maximum width (MW) construct to further increase the stabilization at the lumbosacral junction in the treatment of neuromuscular pelvic obliquity [82].
The scoliotic curve at the spinal level can be instrumented with hooks, screws, or sublaminar wires. Then, iliosacral screws are inserted on each side (using guiding Kirschner wire and 7 mm diameter screws). On the side of the higher hemipelvis, a downgoing laminar hook is inserted above the iliosacral screw, and an upgoing laminar hook is inserted below the iliosacral screw of the lower hemipelvis. A 6 or 7 mm regular iliac screw is inserted bilaterally in the iliac wing with an entry point 1 to 2 cm below the iliosacral screw. Its direction is 2 cm above the sciatic notch and perpendicular to the future rod. It is inserted until its side opening is aligned with the laminar hook sitting on the iliosacral screw. The rods are attached to the side opening of both the hook and the screw. Pelvic obliquity correction is finally accomplished with compression and distraction at the lumbosacral level. The original description of the technique proposed to add a crosslink in distraction in the low lumbar area, but this addition is probably not mandatory if pedicle screws are used at the lumbar levels [82, 83]. The final appearance of the construct is an “M” on the posteroanterior radiograph and a “W” on axial reconstruction.
Unfortunately, this interesting sacropelvic fixation is poorly documented in the current literature. Carroll et al. reported a 61 % reduction of pelvic obliquity in a series of 6 neuromuscular patients at 3 months of follow-up [83]. While it has been suggested that the average rate of correction of pelvic obliquity is 80 % using the construct, this is not currently supported by a peer-review publication. No complications specific to this technique have been reported yet [84]. Since this particular technique combines iliac and iliosacral screws, it could be associated, theoretically, with increased hardware prominence in low weight patients.
Sacral alar iliac technique
Sacral alar iliac (SAI) or S2 iliac screws have been recently proposed by Sponseller as an alternative method for lumbopelvic fixation in pediatric patients [85]. These screws are inserted with a starting point 1 mm caudal and 1 mm distal to the S1 dorsal foramen. This starting point makes them in-line with S1 promontory screws and lumbar pedicle screws, thus eliminating the need for cross-connectors [86, 87]. A computed tomographic analysis in skeletally mature adolescents demonstrated that their entry point is also 15 mm deeper than the PSIS starting point, thus potentially minimizing implant prominence when compared to Galveston or iliac screws fixation techniques [86]. Their trajectory is approximatively 40° of lateral angulation in the transverse plane and 40° of caudal angulation in the sagittal plane. This more oblique angle, when compared to other iliac fixation techniques, further prevents the screw from backing out dorsally. Another theoretical advantage of this type of fixation is increased bone purchase through the sacrum when compared with iliac screws. The length of these screws typically ranges from 70 and 100 mm with a diameter from 7.5 to 10 mm [87, 88].
The correction of pelvic obliquity with this technique, when combined with S1 pedicle screws for neuromuscular scoliosis, was 70 % in a consecutive series of 26 patients [88]. The reported complications in this study directly associated with this type of fixation were postoperative lucencies around two screws, one patient with bilateral SI joint pain requiring revision to longer SAI screws with full pain relief, and one patient with an asymptomatic break at the neck of an SAI screw two years after surgery. The course of S2 iliac screws violates the sacroiliac joint in 60 % of cases [87], and the long-term clinical significance of such articular violation is unknown. Additional long-term clinical studies with a higher number of patients are probably mandatory to support the advantages further and to assess the complications associated with sacral alar iliac fixation.
S-rods (Dunn McCarthy)
S-rods fixation of the sacropelvis was described by Dunn and McCarthy in 1989 [89]. This technique was developed primarily for, but not limited to, pediatric patients with myelodysplasia [89–91]. Prebent S shaped rods are placed over the sacral ala after releasing the iliolumbar ligaments between the transverse processes of L5 and the ilium. Distraction can be applied between the alar rod and an infralaminar hook or a pedicle screw at L4 (or above) in order to seat firmly the S portion anteriorly and posteriorly around the ala. Because of the anterior support on the sacral ala, this construct is considered to provide an effective lever arm against flexion forces. Therefore it is considered to be most useful in nonambulatory patients with neuromuscular conditions, especially when associated with thoracolumbar or lumbar kyphosis. Its insufficient resistance against distraction, rotation, and lateral bending at the lumbopelvic junction probably makes this type of fixation less suitable in ambulatory patients [45]. Another drawback of this instrumentation in patients with an intact spinal cord is the risk of L5 nerve root irritation with a 14 % incidence of unilateral neuropathic lower extremity pain [92]. In addition to its strong moment arm against flexion, the other theoretical advantages of the S rods fixation are its low profile and the fact that it does not span an unfused sacroiliac joint. Finally, it does not require fixation into the ilia, which are frequently small and impaired by former pelvic procedures in children with myelomeningocele [89]. A retrospective review of 67 neuromuscular patients, mainly with myelomeningocele (65.7 %), demonstrated an average correction of pelvic obliquity of 53 % with no significant loss of correction at a mean follow-up of 6 years. Lumbopelvic pseudarthrosis was not encountered in this study [90].
A complication specific to this construct is the migration of the S rod into the sacrum on the high side of pelvic obliquity [89, 90]. Warner and Fackler proposed a modification of the original Dunn McCarthy technique for the fixation of the lumbopelvic junction after kyphectomy for lumbar kyphosis in myelodysplasic pediatric patients, where the rods are inserted on both sides through the first sacral foramina. The L-rods are bent during the surgery, and since the sacral foramina is aligned with the position of the rod at the spinal level, no lateral bending is needed. This modified Dunn McCarthy technique was associated with a substantial decrease of deformity recurrence, pseudarthrosis, and instrumentation problems when compared to a historical cohort of patients treated with Harrington compression rod instrumentation for the same indication [91].
Intrasacral rod fixation
Intrasacral rod fixation was first introduced by Jackson. It combines S1 transpedicular endplate fixation at S1 with two sacral screws and two rods inserted beyond the sacral screws into the lateral sacral mass. A computed tomographic anatomic study has demonstrated the feasibility and theoretical safety of inserting 7 mm diameter rods in the lateral sacral masses. Moreover, an indirect “sacroiliac buttress” is provided by the ilia along with the sacroiliac interosseous ligament, the existence of which could theoretically help resist the bending moments during flexion across the lumbosacral junction [93]. A human cadaveric study confirmed increased rotational and flexion stiffness of this type of fixation when compared with the Galveston technique and isolated anterior constructs [94].
In Jackson’s original technique, the S1 transpedicular screws were inserted under strict anteroposterior and lateral fluoroscopic control. Such imaging is technically demanding in cases of severe pelvic obliquity. Mazda et al. developed an original template to insert these screws in a so-called “cylinder of safety” [95]. Two Kirschner wires are first inserted through this template with an entry point 5 mm above and 5 mm lateral to the first sacral foramina under lateral fluoroscopic control. Then, two cannulated screws (7 mm) are introduced. These screws are designed with an oblique canal angle (usually 10°) to facilitate connection to the rods [96]. Sacral instrumentation is finalized with the positioning of the rods guided by anteroposterior fluoroscopy. They are inserted beyond the sacral screws into the lateral sacral mass distal to S3. The two intrasacral rods are attached with a transverse connector proximally to the sacral screws and linked to the proximal spinal construct with closed lateral connectors. Correction of pelvic obliquity is completed with distraction or compression maneuvers and in situ bending [97].
Intrasacral rod fixation using the modified Jackson technique has been associated with a significant pelvic obliquity reduction in 96.6 % of 55 pediatric neuromuscular patients in a prospective study at a mean follow-up of 10.3 years [97]. No complication directly involving this type of construct, such as breakage, pull-out, or loosening of the intrasacral rods, has been reported. No lesion of presacral neurovascular structure occurred in this last study, a finding that is probably linked to the fact that the tip of the sacral screws penetrates the L5-S1 disc with this technique rather than the anterior cortex of S1. Another theoretical advantage of this construct is that it does not span an unfused joint. Nevertheless, in all patients, a radiolucent line with a peripheral rim of sclerosis developed around the intrasacral rod within six months of surgery, mimicking the “windshield wiper” effect of the Galveston fixation. Regardless, this radiological finding was never associated with pain and did not evolve subsequently during follow-up [97].
Sacral bars and spinopelvic transiliac fixation (STIF) technique
Historically, transiliac fixation with the Harrington sacral bar represents the first generation of pelvic instrumentation [98]. It was supplanted by the Galveston technique and other forms of sacropelvic instrumentation because of its frequent complications, which include lateral bar migration and disengagement of the hook connecting the spinal rod to the sacral bar [75]. Nevertheless, this technique continues to represent an interesting alternative to more modern pelvic instrumentation in selected pediatric deformity cases. Sacral dysraphism can prevent instrumentation of the sacrum, and dysplastic ilia or planned or previous pelvic osteotomies can limit access for iliac fixation. History of prior posterior iliac crest bone graft procedure in revision cases can also weaken iliac fixation.
Widmann et al. proposed a modification of the original sacral bar technique to eliminate the frequent complications [99]. The modification includes the use of a low lumbar crosslink between the spinal rods and the use of two long malleable crosslinks bent at 90° connecting the sacral bar to the spinal rod on each side. It achieved a correction of pelvic obliquity of 62.9 % with 20 % of loss of pelvic fixation in the ilium in the retrospective review of the same authors. Another evolution of the sacral bar fixation is the spinopelvic transiliac fixation (STIF) technique introduced by King [100]. This spinal implant system consists of L-shaped paravertebral rods with threaded distal ends with specifically designed washers and locking nuts. The threads of the rods are inserted through the posterior ilium at the level of S2. The rods are then rigidly linked just proximal to the right angle bend. The locking nuts are tightened over the washer and the ilium resulting in compression of the sacroiliac joints on each side. The pelvis is then cantilevered across the scoliotic spine and anchored by a combination of wires, hooks, or screws. The STIF construct demonstrated greater biomechanical stability in cadaveric specimens under axial compression and flexion over Galveston fixation [100]. It was clinically effective with a correction of 67 % of pelvic obliquity at long-term follow-up, with a pseudarthrosis rate of 7.4 % [101]. A supposed advantage of this fixation is that it could induce sacroiliac joints fusion by cinching the joints together and by laying bone graft from the spine to the iliac crest while also eliminating sacroiliac joint pain. Complications directly involving the modified sacral bar and STIF technique include inferior prominent hardware over the sacrum sometimes necessitating revision [99, 101].
Comparative clinical studies
The number of clinical studies comparing pelvic fixation techniques for the treatment of pediatric spine deformity is limited. Most of them are retrospective reviews and control groups are often heterogenous; the traditional Galveston technique represents the most frequently used control group [52, 73, 83, 88, 102–104]. A retrospective study of 16 patients reported increased intraoperative and immediate postoperative failure of fixation of sacral screws (44%) and iliosacral screws (28%) compared to Galveston fixation (0 %). The same study showed that 77% of patients with medical complications, including neurogenic pain, were in the sacral screws arm of the study [52]. Bulman et al. retrospectively compared the Galveston technique performed with the “unit” rod to two unlinked L-rods in patients with cerebral palsy and showed that the use of the “unit” rod was associated with a better correction of pelvic obliquity (79.3 % vs. 43.4 %, respectively)[102]. The superior correction of pelvic obliquity associated with this single continuous implant was also confirmed by another multicenter retrospective review comparing the “unit” rod to custom-bent rods anchored to the pelvis with iliac screws or rods, S-rods, or sacral screws (74 vs 22 %, respectively). However, the unit rod was associated with higher transfusion requirements (1278 vs 729 mL), increased infection rates (15 vs 5 %), more clinically apparent implant prominence (12 vs 2 instances), and longer intensive care unit (4 vs 3 days) and hospital stays (14 vs 13 days) in this last study [104]. When compared to traditional Galveston fixation, iliac screws were found to deliver better pelvic obliquity correction (80 % vs. 67 %, respectively) and to be associated with less pelvic anchor motion and surrounding radiolucencies at latest follow-up in a retrospective series of neuromuscular patients [103]. Similarly, a retrospective case control review with a small sample size reported a nearly 30 % better correction of pelvic obliquity with the MW construct (combining iliosacral and iliac screws) when compared to Galveston fixation [83]. Zahi et al. compared the radiological results and complications of the T-construct (combining iliac and sacral screws) to iliosacral screws in a prospective series of neuromuscular patients. Their preliminary results suggested a similar correction of pelvic obliquity in both groups but increased complications in the iliosacral screws group [73]. Finally, in a retrospective review, Sponseller et al. reported a significantly better correction of pelvic obliquity with SAI screws when compared to pelvic fixation with sacral or iliac screws (70 % vs. 50 %, respectively) and similar complication rates between the two groups [88].
Authors’ preferred treatment
The authors generally recommend extension of spine fusion to the pelvis for the surgical treatment of non-ambulatory neuromuscular scoliosis despite the magnitude of pelvic obliquity; in ambulatory neuromuscular scoliosis patients with minimal fixed pelvic obliquity (<15°), we avoid extension to the pelvis. We tend to favor the use of iliac screws for pelvic anchorage with the addition of S1 screws when feasible. Occasionally, we use sacral alar iliac screws; however, in our experience, this type of fixation can be technically difficult in patients with lumbar hyperlordosis, a situation frequently encountered in spastic cerebral palsy patients. In patients with severe pelvic obliquity, we consider using the MW technique as we find that this modular construct allows for progressive compression and distraction that enables powerful pelvic obliquity correction. We recently reviewed our results using the MW construct in 25 patients and found an 84 % pelvic obliquity correction at a minimum of two-years follow-up (unpublished data). Our use of transiliac techniques is restricted to select patients presenting with local anomalies making insertion of screws impossible or hazardous, and we reserve Dunn McCarthy S-rods for myelomeningocele patients with a combination of kyphosis and pelvic anomalies precluding the use of screws.
Conclusions
Though many different techniques have been described to extend a long spine fusion to the sacropelvis, it is always essential to remember the general rules of scoliosis surgery in neuromuscular patients. The main goal is to achieve a balanced spine sitting over a level pelvis with a solid spinal and lumbopelvic arthrodesis [30]. An extensive presurgical medical workup, including correction of possible nutritional deficiencies, is of primary importance to decrease the risk of perioperative complications [38, 105]. Given the significant risk of lumbopelvic pseudarthrosis, a strong experience with the specific technique of pelvic fixation chosen is essential. It is also strongly advised to be familiar with more than one technique of pelvic fixation in order to be able to be safe in managing a salvage procedure after intraoperative failure or during revision or to choose the most appropriate construct for selected patients with disturbed sacropelvic anatomy.
Acknowledgement
The authors thank Guylaine Bedard from Shriners Hospital for the illustrations and Dr. Juan Sebastian Rendon for editorial assistance.
Disclosure
No conflicts of interest relevant to this article were reported.
Contributor Information
Romain Dayer, Email: romain.dayer@hcuge.ch.
Jean Albert Ouellet, Email: jean.ouellet@muhc.mcgill.ca.
Neil Saran, Phone: +1-514-2826963, FAX: +1-514-8428664, Email: neil.saran@muhc.mcgill.ca.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Lenke LG, Kuklo TR. Sacropelvic fixation techniques in the treatment of pediatric spinal deformity. Semin Spine Surg. 2004;16(2):114–118. doi: 10.1053/j.semss.2004.07.006. [DOI] [Google Scholar]
- 2.Hosalkar HS, Luedtke LM, Drummond DS. New technique in congenital scoliosis involving fixation to the pelvis after hemivertebra excision. Spine. 2004;29(22):2581–7. doi: 10.1097/01.brs.0000145414.43650.62. [DOI] [PubMed] [Google Scholar]
- 3.Hresko MT, Hirschfeld R, Buerk AA, Zurakowski D. The effect of reduction and instrumentation of spondylolisthesis on spinopelvic sagittal alignment. J Pediatr Orthop. 2009;29(2):157–62. doi: 10.1097/BPO.0b013e3181977de8. [DOI] [PubMed] [Google Scholar]
- 4.Nakamura H, Matsuda H, Konishi S, Yamano Y. Single-stage excision of hemivertebrae via the posterior approach alone for congenital spine deformity: follow-up period longer than ten years. Spine. 2002;27(1):110–5. doi: 10.1097/00007632-200201010-00026. [DOI] [PubMed] [Google Scholar]
- 5.Shufflebarger HL, Geck MJ. High-grade isthmic dysplastic spondylolisthesis: monosegmental surgical treatment. Spine. 2005;30(6 Suppl):S42–8. doi: 10.1097/01.brs.0000155583.55856.f9. [DOI] [PubMed] [Google Scholar]
- 6.Smith JT. Bilateral rib-to-pelvis technique for managing early-onset scoliosis. Clin Orthop Relat Res. 2011;469(5):1349–55. doi: 10.1007/s11999-010-1700-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sponseller PD, Yang JS, Thompson GH, et al. Pelvic fixation of growing rods: comparison of constructs. Spine. 2009;34(16):1706–10. doi: 10.1097/BRS.0b013e3181ab240e. [DOI] [PubMed] [Google Scholar]
- 8.Drummond D, Breed AL, Narechania R. Relationship of spine deformity and pelvic obliquity on sitting pressure distributions and decubitus ulceration. J Pediatr Orthop. 1985;5(4):396–402. doi: 10.1097/01241398-198507000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Larsson EL, Aaro S, Normelli H, Oberg B. Weight distribution in the sitting position in patients with paralytic scoliosis: pre- and postoperative evaluation. Eur Spine J. 2002;11(2):94–9. doi: 10.1007/s00586-001-0373-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murans G, Gutierrez-Farewik EM, Saraste H. Kinematic and kinetic analysis of static sitting of patients with neuropathic spine deformity. Gait Posture. 2011;34(4):533–8. doi: 10.1016/j.gaitpost.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 11.Patel J, Walker JL, Talwalkar VR, et al. Correlation of spine deformity, lung function, and seat pressure in spina bifida. Clin Orthop Relat Res. 2011;469(5):1302–7. doi: 10.1007/s11999-010-1687-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith RM, Emans JB. Sitting balance in spinal deformity. Spine. 1992;17(9):1103–9. doi: 10.1097/00007632-199209000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Dubousset J. Pelvic obliquity: a review. Orthopedics. 1991;14(4):479–81. doi: 10.3928/0147-7447-19910401-13. [DOI] [PubMed] [Google Scholar]
- 14.Winter RB, Pinto WC. Pelvic obliquity. Its causes and its treatment. Spine. 1986;11(3):225–34. doi: 10.1097/00007632-198604000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Ko PS, Jameson PG, 2nd, Chang TL, Sponseller PD. Transverse-plane pelvic asymmetry in patients with cerebral palsy and scoliosis. J Pediatr Orthop. 2011;31(3):277–83. doi: 10.1097/BPO.0b013e31820fc65b. [DOI] [PubMed] [Google Scholar]
- 16.Brenn BR, Theroux MC, Dabney KW, Miller F. Clotting parameters and thromboelastography in children with neuromuscular and idiopathic scoliosis undergoing posterior spinal fusion. Spine. 2004;29(15):E310–4. doi: 10.1097/01.BRS.0000132513.88038.64. [DOI] [PubMed] [Google Scholar]
- 17.Lipton GE, Miller F, Dabney KW, et al. Factors predicting postoperative complications following spinal fusions in children with cerebral palsy. J Spinal Disord. 1999;12(3):197–205. [PubMed] [Google Scholar]
- 18.Lonstein JE, Akbarnia A. Operative treatment of spinal deformities in patients with cerebral palsy or mental retardation. An analysis of one hundred and seven cases. J Bone Joint Surg Am. 1983;65(1):43–55. [PubMed] [Google Scholar]
- 19.Lonstein JE, Koop SE, Novachek TF, Perra JH. Results and complications following spinal fusion for neuromuscular scoliosis in cerebral palsy and static encephalopathy using luque galveston instrumentation: experience in 93 patients. Spine. 2012, In press. [DOI] [PubMed]
- 20.Master DL, Connie PK, Jochen SH, et al. Wound infections after surgery for neuromuscular scoliosis: risk factors and treatment outcomes. Spine. 2011;36(3):E179–85. doi: 10.1097/BRS.0b013e3181db7afe. [DOI] [PubMed] [Google Scholar]
- 21.Modi HN, Suh SW, Yang JH, et al. Surgical complications in neuromuscular scoliosis operated with posterior- only approach using pedicle screw fixation. Scoliosis. 2009;4:11. doi: 10.1186/1748-7161-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mohamad F, Parent S, Pawelek J, et al. Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop. 2007;27(4):392–7. doi: 10.1097/01.bpb.0000271321.10869.98. [DOI] [PubMed] [Google Scholar]
- 23.Reames DL, Smith JS, Fu KM, et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine. 2011;36(18):1484–91. doi: 10.1097/BRS.0b013e3181f3a326. [DOI] [PubMed] [Google Scholar]
- 24.Sponseller PD, Shah SA, Abel MF, et al. Infection rate after spine surgery in cerebral palsy is high and impairs results: multicenter analysis of risk factors and treatment. Clin Orthop Relat Res. 2010;468(3):711–6. doi: 10.1007/s11999-009-0933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCall RE, Hayes B. Long-term outcome in neuromuscular scoliosis fused only to lumbar 5. Spine. 2005;30(18):2056–60. doi: 10.1097/01.brs.0000178817.34368.16. [DOI] [PubMed] [Google Scholar]
- 26.Gupta MC, Wijesekera S, Sossan A, et al. Reliability of radiographic parameters in neuromuscular scoliosis. Spine. 2007;32(6):691–5. doi: 10.1097/01.brs.0000257524.23074.ed. [DOI] [PubMed] [Google Scholar]
- 27.Osebold WR, Mayfield JK, Winter RB, Moe JH. Surgical treatment of paralytic scoliosis associated with myelomeningocele. J Bone Joint Surg Am. 1982;64(6):841–56. [PubMed] [Google Scholar]
- 28.Allen BL, Jr, Ferguson RL. The Galveston technique of pelvic fixation with L-rod instrumentation of the spine. Spine. 1984;9(4):388–94. doi: 10.1097/00007632-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Maloney WJ, Rinsky LA, Gamble JG. Simultaneous correction of pelvic obliquity, frontal plane, and sagittal plane deformities in neuromuscular scoliosis using a unit rod with segmental sublaminar wires: a preliminary report. J Pediatr Orthop. 1990;10(6):742–9. doi: 10.1097/01241398-199011000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Lubicky JP, McCarthy RE. Sacral pelvic fixation in neuromuscular deformities. Semin Spine Surg. 2004;16(2):126–133. doi: 10.1053/j.semss.2004.07.003. [DOI] [Google Scholar]
- 31.Broom MJ, Banta JV, Renshaw TS. Spinal fusion augmented by luque-rod segmental instrumentation for neuromuscular scoliosis. J Bone Joint Surg Am. 1989;71(1):32–44. [PubMed] [Google Scholar]
- 32.Mehta SS, Modi HN, Srinivasalu S. Pedicle screw-only constructs with lumbar or pelvic fixation for spinal stabilization in patients with Duchenne muscular dystrophy. J Spinal Disord Tech. 2009;22(6):428–33. doi: 10.1097/BSD.0b013e3181872d74. [DOI] [PubMed] [Google Scholar]
- 33.Modi HN, Suh SW, Hong JY, et al. Treatment and complications in flaccid neuromuscular scoliosis (Duchenne muscular dystrophy and spinal muscular atrophy) with posterior-only pedicle screw instrumentation. Eur Spine J. 2010;19(3):384–93. doi: 10.1007/s00586-009-1198-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Modi HN, Hong JY, Mehta SS, et al. Surgical correction and fusion using posterior-only pedicle screw construct for neuropathic scoliosis in patients with cerebral palsy: a three-year follow-up study. Spine. 2009;34(11):1167–75. doi: 10.1097/BRS.0b013e31819c38b7. [DOI] [PubMed] [Google Scholar]
- 35.Whitaker C, Burton DC, Asher M. Treatment of selected neuromuscular patients with posterior instrumentation and arthrodesis ending with lumbar pedicle screw anchorage. Spine. 2000;25(18):2312–8. doi: 10.1097/00007632-200009150-00008. [DOI] [PubMed] [Google Scholar]
- 36.Modi HN, Woo Suh S, Song HR, et al. Evaluation of pelvic fixation in neuromuscular scoliosis: a retrospective study in 55 patients. Int Orthop. 2010;34(1):89–96. doi: 10.1007/s00264-008-0703-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Banta JV, Drummond DS, Ferguson RL. The treatment of neuromuscular scoliosis. AAOS Instruct Course Lectures. 1999;48:551–61. [PubMed] [Google Scholar]
- 38.McCarthy RE. Management of neuromuscular scoliosis. Orthop Clin North Am. 1999;30(3):435–49. doi: 10.1016/S0030-5898(05)70096-1. [DOI] [PubMed] [Google Scholar]
- 39.Askin GN, Hallett R, Hare N, Webb JK. The outcome of scoliosis surgery in the severely physically handicapped child. An objective and subjective assessment. Spine. 1997;22(1):44–50. doi: 10.1097/00007632-199701010-00008. [DOI] [PubMed] [Google Scholar]
- 40.Tsirikos AI, Lipton G, Chang WN, et al. Surgical correction of scoliosis in pediatric patients with cerebral palsy using the unit rod instrumentation. Spine. 2008;33(10):1133–40. doi: 10.1097/BRS.0b013e31816f63cf. [DOI] [PubMed] [Google Scholar]
- 41.Mazur J, Menelaus MB, Dickens DR, Doig WG. Efficacy of surgical management for scoliosis in myelomeningocele: correction of deformity and alteration of functional status. J Pediatr Orthop. 1986;6(5):568–75. doi: 10.1097/01241398-198609000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Müller EB, Nordwall A, Wendt L. Influence of surgical treatment of scoliosis in children with spina bifida on ambulation and motoric skills. Acta Paediatr. 1992;81(2):173–6. doi: 10.1111/j.1651-2227.1992.tb12197.x. [DOI] [PubMed] [Google Scholar]
- 43.Schoenmakers MA, Gulmans VA, Gooskens RH, et al. Spinal fusion in children with spina bifida: influence on ambulation level and functional abilities. Eur Spine J. 2005;14(4):415–22. doi: 10.1007/s00586-004-0768-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Findley TW, Agre JC, Habek RV, et al. Ambulation in the adolescent with myelomeningocele. I: Early childhood predictors. Arch Phys Med Rehabil. 1987;68:518–522. [PubMed] [Google Scholar]
- 45.O’Brien MF, Kuklo TR, Lenke LG. Sacropelvic instrumentation: anatomic and biomechanical zones of fixation. Semin Spine Surg. 2004;16(2):76–90. doi: 10.1053/j.semss.2004.07.007. [DOI] [Google Scholar]
- 46.Kornblatt MD, Casey MP, Jacobs RR. Internal fixation in lumbosacral spine fusion. A biomechanical and clinical study. Clin Orthop Relat Res. 1986;203:141–50. [PubMed] [Google Scholar]
- 47.Leong JC, Lu WW, Zheng Y, et al. Comparison of the strengths of lumbosacral fixation achieved with techniques using one and two triangulated sacral screws. Spine. 1998;23(21):2289–94. doi: 10.1097/00007632-199811010-00008. [DOI] [PubMed] [Google Scholar]
- 48.McCord DH, Cunningham BW, Shono Y, et al. Biomechanical analysis of lumbosacral fixation. Spine. 1992;17(8 Suppl):S235–43. doi: 10.1097/00007632-199208001-00004. [DOI] [PubMed] [Google Scholar]
- 49.Schwab FJ, Nazarian DG, Mahmud F, Michelsen CB. Effects of spinal instrumentation on fusion of the lumbosacral spine. Spine. 1995;20(18):2023–8. doi: 10.1097/00007632-199509150-00014. [DOI] [PubMed] [Google Scholar]
- 50.Shirado O, Zdeblick TA, McAfee PC, Warden KE. Biomechanical evaluation of methods of posterior stabilization of the spine and posterior lumbar interbody arthrodesis for lumbosacral isthmic spondylolisthesis. A calf-spine model. J Bone Joint Surg Am. 1991;73(4):518–26. [PubMed] [Google Scholar]
- 51.Stovall DO, Jr, Goodrich JA, Lundy D, et al. Sacral fixation technique in lumbosacral fusion. Spine. 1997;22(1):32–7. doi: 10.1097/00007632-199701010-00006. [DOI] [PubMed] [Google Scholar]
- 52.Camp JF, Caudle R, Ashmun RD, Roach J. Immediate complications of Cotrel-Dubousset instrumentation to the sacro-pelvis. A clinical and biomechanical study. Spine. 1990;15(9):932–41. doi: 10.1097/00007632-199009000-00018. [DOI] [PubMed] [Google Scholar]
- 53.Luque ER. Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res. 1982;163:192–8. [PubMed] [Google Scholar]
- 54.Allen BL, Jr, Ferguson RL. A 1988 perspective on the Galveston technique of pelvic fixation. Orthop Clin North Am. 1988;19(2):409–18. [PubMed] [Google Scholar]
- 55.Benson ER, Thomson JD, Smith BG, Banta JV. Results and morbidity in a consecutive series of patients undergoing spinal fusion for neuromuscular scoliosis. Spine. 1998;23(21):2308–17. doi: 10.1097/00007632-199811010-00012. [DOI] [PubMed] [Google Scholar]
- 56.Boachie-Adjei O, Lonstein JE, Winter RB, et al. Management of neuromuscular spinal deformities with Luque segmental instrumentation. J Bone Joint Surg Am. 1989;71(4):548–62. [PubMed] [Google Scholar]
- 57.Ferguson RL, Allen BL., Jr Staged correction of neuromuscular scoliosis. J Pediatr Orthop. 1983;3(5):555–62. doi: 10.1097/01241398-198311000-00001. [DOI] [PubMed] [Google Scholar]
- 58.Gau YL, Lonstein JE, Winter RB, et al. Luque-Galveston procedure for correction and stabilization of neuromuscular scoliosis and pelvic obliquity: a review of 68 patients. J Spinal Disord. 1991;4(4):399–410. doi: 10.1097/00002517-199112000-00001. [DOI] [PubMed] [Google Scholar]
- 59.Lascombes P, Fabre B, Fresler F, et al. Surgical treatment of spinal deformity due to cerebral motor disorders using a Luque type appliance. Chir Pediatr. 1989;30(6):271–6. [PubMed] [Google Scholar]
- 60.Sink EL, Newton PO, Mubarak SJ, Wenger DR. Maintenance of sagittal plane alignment after surgical correction of spinal deformity in patients with cerebral palsy. Spine. 2003;28(13):1396–403. doi: 10.1097/01.BRS.0000067088.99346.73. [DOI] [PubMed] [Google Scholar]
- 61.Bell DF, Moseley CF, Koreska J. Unit rod segmental spinal instrumentation in the management of patients with progressive neuromuscular spinal deformity. Spine. 1989;14(12):1301–7. doi: 10.1097/00007632-198912000-00006. [DOI] [PubMed] [Google Scholar]
- 62.Marchesi D, Arlet V, Stricker U, Aebi M. Modification of the original Luque technique in the treatment of Duchenne’s neuromuscular scoliosis. J Pediatr Orthop. 1997;17(6):743–9. doi: 10.1097/00004694-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 63.Brook PD, Kennedy JD, Stern LM, et al. Spinal fusion in Duchenne’s muscular dystrophy. J Pediatr Orthop. 1996;16(3):324–31. doi: 10.1097/01241398-199605000-00006. [DOI] [PubMed] [Google Scholar]
- 64.Dias RC, Miller F, Dabney K, et al. Surgical correction of spinal deformity using a unit rod in children with cerebral palsy. J Pediatr Orthop. 1996;16(6):734–40. doi: 10.1097/01241398-199611000-00007. [DOI] [PubMed] [Google Scholar]
- 65.Nectoux E, Giacomelli MC, Karger C, et al. Complications of the Luque-Galveston scoliosis correction technique in paediatric cerebral palsy. Orthop Traumatol Surg Res. 2010;96(4):354–61. doi: 10.1016/j.otsr.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 66.Rinsky LA. Surgery of spinal deformity in cerebral palsy. Twelve years in the evolution of scoliosis management. Clin Orthop Relat Res. 1990;253:100–9. [PubMed] [Google Scholar]
- 67.Gitelman A, Joseph Jr SA, Carrion W, Stephen M. Results and morbidity in a consecutive series of patients undergoing spinal fusion with iliac screws for neuromuscular scoliosis. Orthopedics. 2008;31(12). [DOI] [PubMed]
- 68.Tsirikos AI, Mains E. Surgical Correction of spinal deformity in patients with cerebral palsy using pedicle screw instrumentation. J Spinal Disord Tech. 2012. [DOI] [PubMed]
- 69.Berry JL, Stahurski T, Asher MA. Morphometry of the supra sciatic notch intrailiac implant anchor passage. Spine. 2001;26(7):E143–8. doi: 10.1097/00007632-200104010-00002. [DOI] [PubMed] [Google Scholar]
- 70.Schwend RM, Sluyters R, Najdzionek J. The pylon concept of pelvic anchorage for spinal instrumentation in the human cadaver. Spine. 2003;28(6):542–7. doi: 10.1097/01.BRS.0000049925.58996.66. [DOI] [PubMed] [Google Scholar]
- 71.Phillips JH, Gutheil JP, Knapp DR., Jr Iliac screw fixation in neuromuscular scoliosis. Spine. 2007;32(14):1566–70. doi: 10.1097/BRS.0b013e318067dcff. [DOI] [PubMed] [Google Scholar]
- 72.Hahn F, Hauser D, Espinosa N, et al. Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J. 2008;17(2):255–61. doi: 10.1007/s00586-007-0558-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zahi R, Thévenin-Lemoine C, Rogier A, et al. The “T-construct” for spinopelvic fixation in neuromuscular spinal deformities. Preliminary results of a prospective series of 15 patients. Childs Nerv Syst. 2011;27(11):1931–5. doi: 10.1007/s00381-011-1411-3. [DOI] [PubMed] [Google Scholar]
- 74.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop Relat Res. 1988;227:10–23. [PubMed] [Google Scholar]
- 75.Bonnett C, Brown JC, Perry J, et al. Evolution of treatment of paralytic scoliosis at Rancho Los Amigos Hospital. J Bone Joint Surg Am. 1975;57(2):206–15. [PubMed] [Google Scholar]
- 76.McMaster MJ. Anterior and posterior instrumentation and fusion of thoracolumbar scoliosis due to myelomeningocele. J Bone Joint Surg Br. 1987;69(1):20–5. doi: 10.1302/0301-620X.69B1.3818727. [DOI] [PubMed] [Google Scholar]
- 77.Miladi LT, Ghanem IB, Draoui MM, et al. Iliosacral screw fixation for pelvic obliquity in neuromuscular scoliosis. A long-term follow-up study. Spine. 1997;22(15):1722–9. doi: 10.1097/00007632-199708010-00007. [DOI] [PubMed] [Google Scholar]
- 78.Zindrick MR, Wiltse LL, Widell EH, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203:99–112. [PubMed] [Google Scholar]
- 79.Teli MG, Cinnella P, Vincitorio F, et al. Spinal fusion with Cotrel-Dubousset instrumentation for neuropathic scoliosis in patients with cerebral palsy. Spine. 2006;31(14):E441–7. doi: 10.1097/01.brs.0000221986.07992.fb. [DOI] [PubMed] [Google Scholar]
- 80.Zahi R, Vialle R, Abelin K, et al. Spinopelvic fixation with iliosacral screws in neuromuscular spinal deformities: results in a prospective cohort of 62 patients. Childs Nerv Syst. 2010;26(1):81–6. doi: 10.1007/s00381-009-0966-8. [DOI] [PubMed] [Google Scholar]
- 81.Neustadt JB, Shufflebarger HL, Cammisa FP. Spinal fusions to the pelvis augmented by Cotrel-Dubousset instrumentation for neuromuscular scoliosis. J Pediatr Orthop. 1992;12(4):465–9. doi: 10.1097/01241398-199207000-00009. [DOI] [PubMed] [Google Scholar]
- 82.Arlet V, Marchesi D, Papin P, Aebi M. The ‘MW’ sacropelvic construct: an enhanced fixation of the lumbosacral junction in neuromuscular pelvic obliquity. Eur Spine J. 1999;8(3):229–31. doi: 10.1007/s005860050163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Carroll EA, Shilt JS, Jacks L. MW construct in fusion for neuromuscular scoliosis. Eur Spine J. 2007;16(3):373–7. doi: 10.1007/s00586-006-0077-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Arlet V. Comments on the article: MW construct in fusion for neuromuscular scoliosis (Eben A. Carroll, Jeffrey Scott Shilt, Laura Jacks) Eur Spine J. 2007;16(3):379–80. doi: 10.1007/s00586-006-0140-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sponseller PD. The S2 portal to the Ilium. Roundtables in Spine Surgery. 2007;2(2):83–87. [Google Scholar]
- 86.Chang TL, Sponseller PD, Kebaish KM, Fishman EK. Low profile pelvic fixation: anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine. 2009;34(5):436–40. doi: 10.1097/BRS.0b013e318194128c. [DOI] [PubMed] [Google Scholar]
- 87.O’Brien JR, Yu WD, Bhatnagar R, et al. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine. 2009;34(12):E439–42. doi: 10.1097/BRS.0b013e3181a4e3e4. [DOI] [PubMed] [Google Scholar]
- 88.Sponseller PD, Zimmerman RM, Ko PS, et al. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine. 2010;35(20):1887–92. doi: 10.1097/BRS.0b013e3181e03881. [DOI] [PubMed] [Google Scholar]
- 89.McCarthy RE, Dunn H, McCullough FL. Luque fixation to the sacral ala using the Dunn-McCarthy modification. Spine. 1989;14(3):281–3. doi: 10.1097/00007632-198903000-00007. [DOI] [PubMed] [Google Scholar]
- 90.McCarthy RE, Bruffett WL, McCullough FL. S rod fixation to the sacrum in patients with neuromuscular spinal deformities. Clin Orthop Relat Res. 1999;364:26–31. doi: 10.1097/00003086-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 91.Warner WC, Jr, Fackler CD. Comparison of two instrumentation techniques in treatment of lumbar kyphosis in myelodysplasia. J Pediatr Orthop. 1993;13(6):704–8. doi: 10.1097/01241398-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 92.Walick KS, King JT, Johnston CE, Rathjen KE. Neuropathic lower extremity pain following Dunn-McCarthy instrumentation. Spine. 2008;33(23):E877–80. doi: 10.1097/BRS.0b013e3181877b99. [DOI] [PubMed] [Google Scholar]
- 93.Jackson RP, McManus AC. The iliac buttress. A computed tomographic study of sacral anatomy. Spine. 1993;18(10):1318–28. doi: 10.1097/00007632-199308000-00011. [DOI] [PubMed] [Google Scholar]
- 94.Glazer PA, Colliou O, Lotz JC, Bradford DS. Biomechanical analysis of lumbosacral fixation. Spine. 1996;21(10):1211–22. doi: 10.1097/00007632-199605150-00015. [DOI] [PubMed] [Google Scholar]
- 95.Mazda K, Khairouni A, Penneçot GF, Bloch J. The ideal position of sacral transpedicular endplate screws in Jackson’s intrasacral fixation. An anatomic study of 50 sacral specimens. Spine. 1998;23(19):2123–6. doi: 10.1097/00007632-199810010-00017. [DOI] [PubMed] [Google Scholar]
- 96.Mazda K, Penneçot GF, Decrette E, Bensahel H. The intrasacral fixation in pediatric practice: problems and prospectives [abstract]. Proceeding of the Pediatric Orthopaedic Society of North America. J Ped Orthop. 1995;15:847. [Google Scholar]
- 97.Ilharreborde B, Hoffmann E, Tavakoli S. Intrasacral rod fixation for pediatric long spinal fusion: results of a prospective study with a minimum 5-year follow-up. J Pediatr Orthop. 2009;29(6):594–601. doi: 10.1097/BPO.0b013e3181b2b403. [DOI] [PubMed] [Google Scholar]
- 98.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44-A:591–610. [PubMed] [Google Scholar]
- 99.Widmann RF, Hresko MT, Hall JE. Lumbosacral fusion in children and adolescents using the modified sacral bar technique. Clin Orthop Relat Res. 1999;364:85–91. doi: 10.1097/00003086-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 100.King AG, Thomas KA, Zembo MM, et al. Analysis of the STIF technique for spino-pelvic fixation. Orthop Trans. 1996;20:128–9. doi: 10.1097/00004694-200009000-00023. [DOI] [PubMed] [Google Scholar]
- 101.King AG, Thomas KA, Eiserloh HL, 3rd, et al. Analysis of the STIF technique for spino-pelvic fixation: clinical results in 19 patients with neuromuscular scoliosis. J Pediatr Orthop. 2000;20(5):667–76. doi: 10.1097/01241398-200009000-00023. [DOI] [PubMed] [Google Scholar]
- 102.Bulman WA, Dormans JP, Ecker ML, Drummond DS. Posterior spinal fusion for scoliosis in patients with cerebral palsy: a comparison of Luque rod and Unit Rod instrumentation. J Pediatr Orthop. 1996;16(3):314–23. doi: 10.1097/01241398-199605000-00005. [DOI] [PubMed] [Google Scholar]
- 103.Peelle MW, Lenke LG, Bridwell KH, Sides B. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine. 2006;31(20):2392–8. doi: 10.1097/01.brs.0000238973.13294.16. [DOI] [PubMed] [Google Scholar]
- 104.Sponseller PD, Shah SA, Abel MF, et al. Scoliosis surgery in cerebral palsy: differences between unit rod and custom rods. Spine. 2009;34(8):840–4. doi: 10.1097/BRS.0b013e31819487b7. [DOI] [PubMed] [Google Scholar]
- 105.Jevsevar DS, Karlin LI. The relationship between preoperative nutritional status and complications after an operation for scoliosis in patients who have cerebral palsy. J Bone Joint Surg Am. 1993;75(6):880–4. doi: 10.2106/00004623-199306000-00008. [DOI] [PubMed] [Google Scholar]