Abstract
Total ankle arthroplasty has been gaining significant popularity for the treatment of ankle arthritis. Subsequent rates of revision surgery secondary to symptomatic bony impingement have been reported in 6–45 % of cases. Arthroscopic debridement of bony impingement following total ankle has been recently reported as an effective therapy. An arthroscopic technique has been recently published by one of the senior authors. In this paper, we expand this technique and retrospectively review our experience with arthroscopic debridement of twenty ankles in twenty patients with symptomatic bony impingement following total ankle arthroplasty.
Keywords: Ankle arthroplasty, Arthroscopic, Impingement, Heterotopic Ossification, Foot, Ankle
Introduction
Degenerative arthritis of the ankle is a disabling problem that affects greater than 50,000 new patients in the US each year [1]. The treatment of ankle arthritis remains a challenging and controversial problem. Historically, ankle arthrodesis has been the mainstay of treatment. Recently, ankle replacement has become increasingly popular. Surgically, the advantages of ankle arthroplasty over arthrodesis have been reported to include retained ankle plantar and dorsiflexion, improved gait, greater patient function, and decreased stress on adjacent joints with slower progression of hind foot degenerative changes [1–3]. While early generations of ankle replacements were quickly abandoned due to high rates of failure as a result of instability and loosening, recent designs incorporate major improvements; these advancements include: mobile bearing polyethylene components, cementless fixation, and minimal bone resection. These designs have been reported to have much more success for treating severe ankle arthritis. The probability of survival ranges from 70 % to 98 % at 3 to 6 years and from 80 % to 95 % at 8 to 12 years [4•, 5•, 6]. Due to these recent advances, more patients are receiving total ankle arthroplasty (TAA) than ever before.
While outcomes following the new generation of TAA have been promising, pain relief following TAA may be incomplete. In their series, Pyevich et al. reported that only 55 % of patients reported complete resolution of pain at an average follow-up of 4.8 years [7]. Furthermore, revision rates following TAA have been reported from 7 % to 28 % [6, 8–11]. The most common reasons for persistent pain and revision surgery include the presence of heterotopic bone, aseptic loosening, implant failure, malalignment, and component subsidence. Impingement remains a common source of persistent pain and dysfunction following TAA. Causes of impingement include heterotopic bone formation, oversizing of the talar component, inadequate resection of the bone during implantation and/or malposition of the prosthesis, resulting in impingement of the implant on the malleolus. Heterotopic bone formation has been reported to occur in 25 % of patients after TAA [12•], however, most patients do not have symptoms severe enough to require surgical debridement. Rates of subsequent surgery for impingement from heterotopic bone or the prosthesis have been reported in 6–45 % of the cases [4•, 5•, 11, 13, 14].
The current standard of care for debridement of bony impingement following TAA is through an open arthrotomy. Shirzad et al. recently described a technique for arthroscopic debridement of impingement following TAA [15]. Arthroscopic debridement has multiple potential advantages over open arthrotomy. For one, it is an outpatient procedure. There is also a shorter recovery period for patients, which ultimately leads to a faster return to function [16]. Given these advantages, arthroscopic debridement has a theoretically improved risk-benefit profile as a treatment method for impingement when compared with open arthrotomy. In this article, we represent the surgical technique for arthroscopic debridement for impingement in patients with total ankle replacements and review our experience with the technique.
Surgical technique
Indications for arthroscopic intervention of the medial or lateral gutter impingement include a minimum of 90 days, preferably 6 months, status post total ankle replacement, pain localized to either or both malleolar regions with weight bearing, isolated pain with palpation of the medial and/or lateral gutters, and radiographic evidence (standing X-ray or CT scan) of prosthesis-malleolar or prosthesis-hypertrophic boney contact (Fig. 1).
Fig. 1.
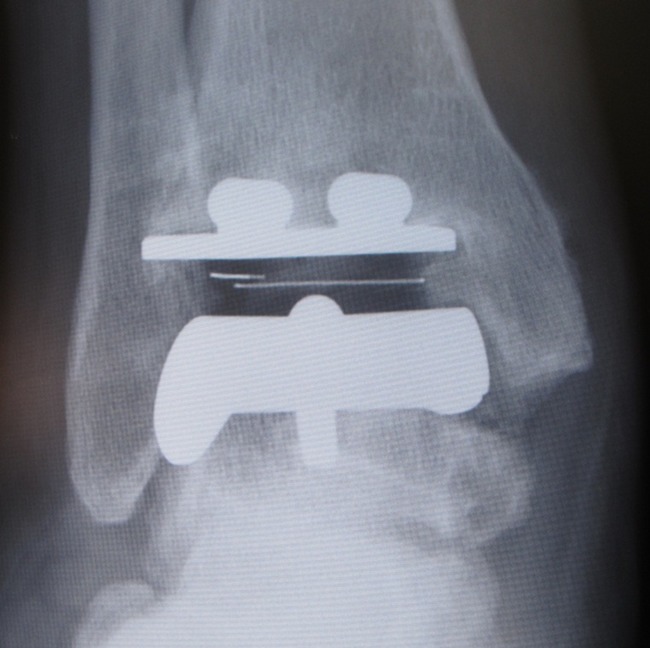
Impingement of the medial gutter post-total ankle replacement showing prosthesis medial malleolar contact
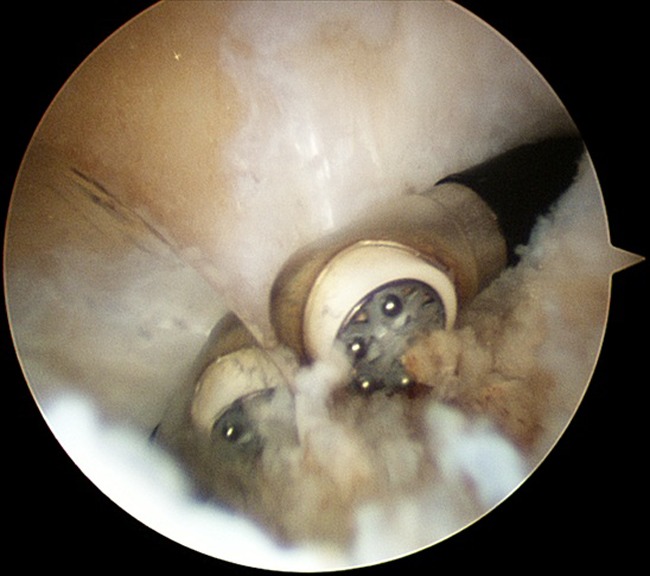
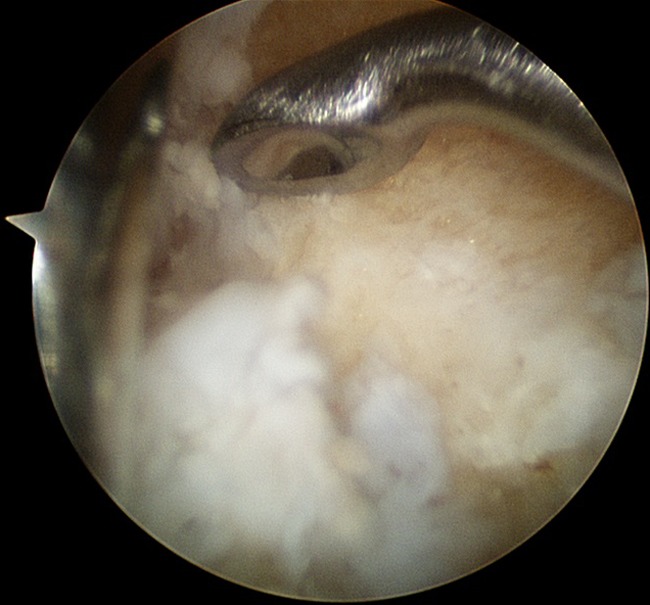
A regional block (popliteal or ankle) and prophylactic antibiotics are given prior to the start of the procedure. The leg is exsanguinated and a thigh-high tourniquet is inflated to 300 mmHg. A tourniquet is used in all cases. No joint distraction devices are necessary. Standard anteromedial and anterolateral ankle arthroscopy portals are created [17]. For lateral gutter debridement, a 2.7 or 1.9-mm, 30° arthroscope is inserted through the anteromedial portal, and a 3.5-mm aggressive shaver is inserted through the anterolateral portal. Shavers and burrs matching the outside diameter of the barrel housing, as well as those with partial unhooding of the cutting edge, are typically more effective at removal of bony impingement than the fully protected instruments. Scar tissue is then carefully resected from the anterior aspect of the joint using the shaver (Fig. 2). This tissue can be quite dense and may require a variety of small joint arthroscopic scissors and biters in order to visualize the joint effectively. The ankle prostheses are highly reflective and can lead to some confusion when trying to orienting the arthroscope (Fig. 3). Quite often, the use of a small right-angled curette is needed to lift up and separate the scar tissue near the lateral gutter to allow for resection of this tissue with the shaver (Fig. 4). Turning the shaver on forward and using it as a burr can often eliminate the soft tissue covering of bone faster than an oscillating shaver.
Fig. 2.
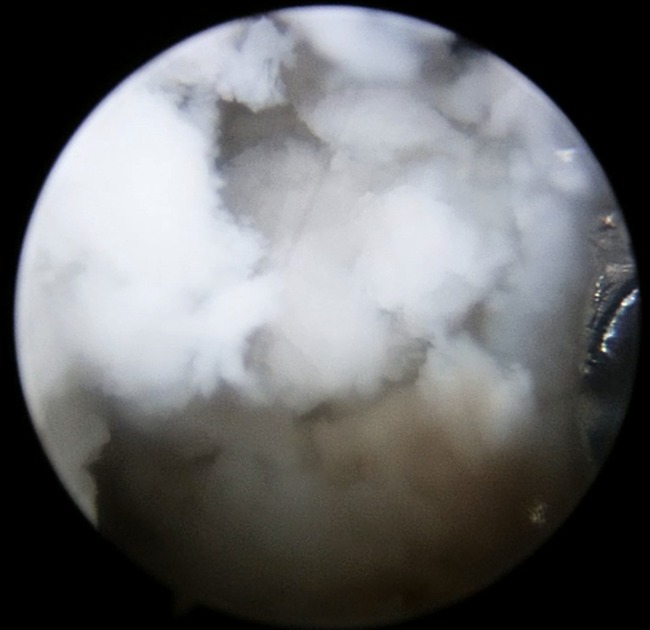
Dense scar tissue visualized in the anterior ankle joint
Fig. 3.
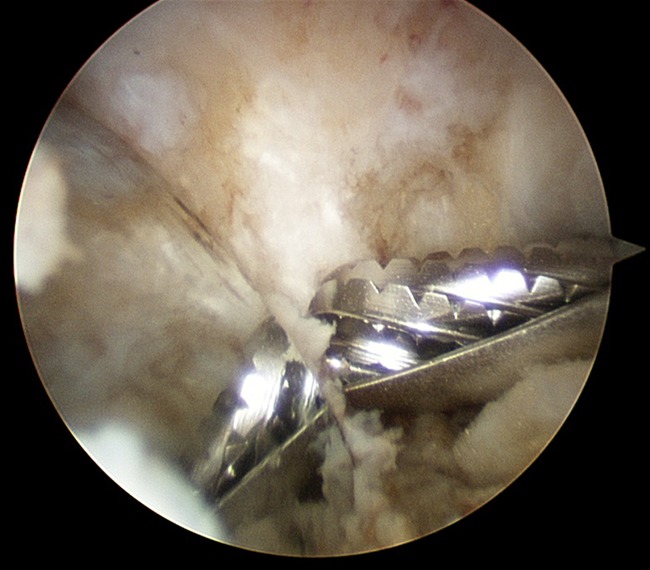
Reflective surface of the talar component
Fig. 4.
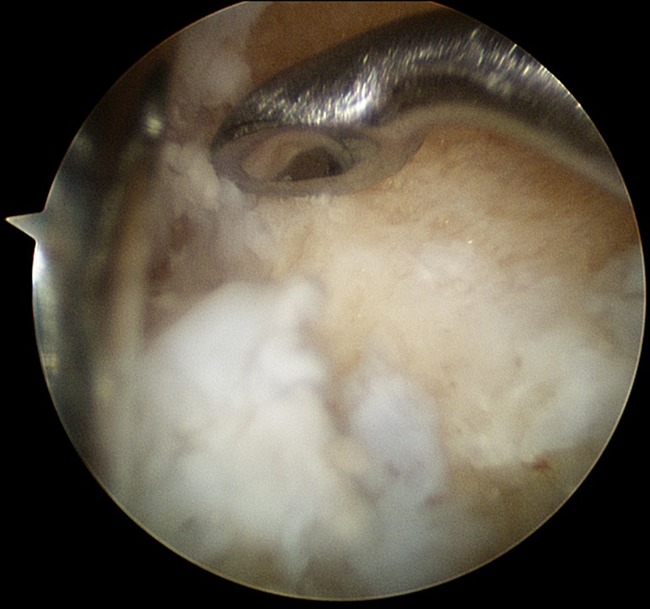
A small right-angled curette is used to elevate and loosen the dense scar tissue in the gutter
Once the anterior aspect of the lateral gutter is visualized, the soft tissue in the gutter is excised until the lateral malleolus and lateral aspect of the talus and/or prosthesis is seen. The Arthrocare (Austin, Texas) Opus wand, which is a bipolar radiofrequency wand that coblates tissue, is used to facilitate the removal of the soft tissue (Fig. 5) and allow visualization of the malleoli. Arthroscopic burrs (3.5 mm) are then used, carefully, to debride the bony impingement on the affected side. Care should be taken to ensure that the backside of the shaver or burr with the hood is immediately adjacent to the talus when beginning the debridement, otherwise, too much bone can be inadvertently resected, which increases the risk of fracture. This is especially true if the prosthesis is wedged between both malleoli making it difficult to get any initial separation within the joint.
Fig. 5.
Coblation with the Opus wand is effective at removal of the tissue in the gutters
After creating space within the lateral gutter, the arthroscope can be taken over the top of the talar component to look down the gutter (Fig. 6). From this anterior to posterior view, the talar shelf bone or the malleolar bone can be visualized as a cause of impingement and then removed. Care is taken to keep the casing end of the shaver, or burr, in contact with the prosthesis, not only to avoid inadvertently resecting too much malleolar bone and destabilizing the component, but also to prevent damage to the metal and polyethylene of the TAA implant itself. Scuffs and scratches on the metal prosthesis must be avoided as they can potentially lead to abrasive or third body wear of the polyethylene. The lateral gutter is debrided with the shaver, burr, and curettes until a clear path is seen between the prosthesis and lateral malleolus. Once the majority of bone has been removed from the malleolus, the remaining shelf of posterior bone can be penetrated with a drill bit which is less likely to injure the soft tissue posteriorly than a burr (Fig. 7). To ensure adequate decompression, visualization of the peroneal tendons is essential after debridement on the lateral side. Similarly, visualization of the posterior tibial tendon is seen on the medial side (Fig. 8).
Fig. 6.

View over the top of the talar component allows for visualization of the gutter and removal of boney debris with the grasper
Fig. 7.
The medial gutter has been debrided and the remaining posterior shelf on the medial malleolus has been drilled allowing visualization of the posterior tibial tendon through the holes
Fig. 8.
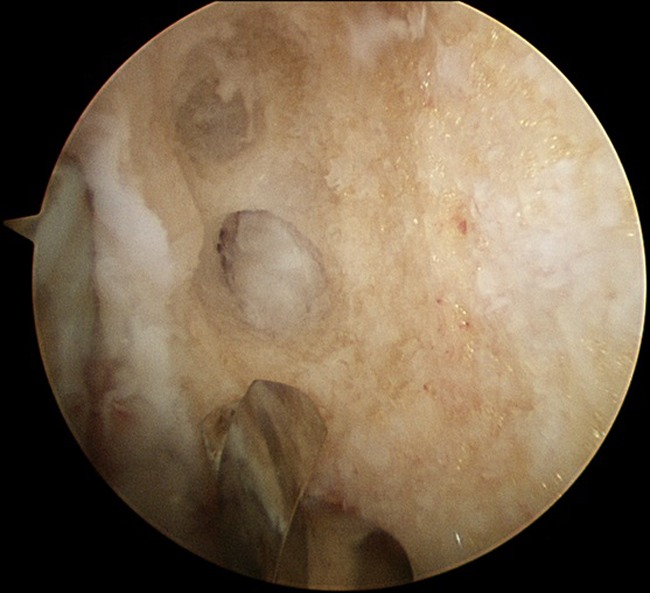
The posterior tibial tendon is carefully visualized, demonstrating adequate debridement
Intraoperative fluoroscopy is used to verify adequate debridement of all areas of bony impingement and can be used to evaluate the amount of bone resected (Fig. 9). The incision sites are closed using an absorbable suture on the capsular tissue and a nylon suture on the skin. The skin incision is 0.25 in. in length, allowing one stitch through the capsule. A sterile compressive dressing is applied, and the patient is placed into a standard postoperative walking boot. Patients are permitted to bear weight as tolerated; however, they are cautioned against too much activity, which may lead to chronic drainage from the portal sites, subsequently increasing infection risk.
Fig. 9.
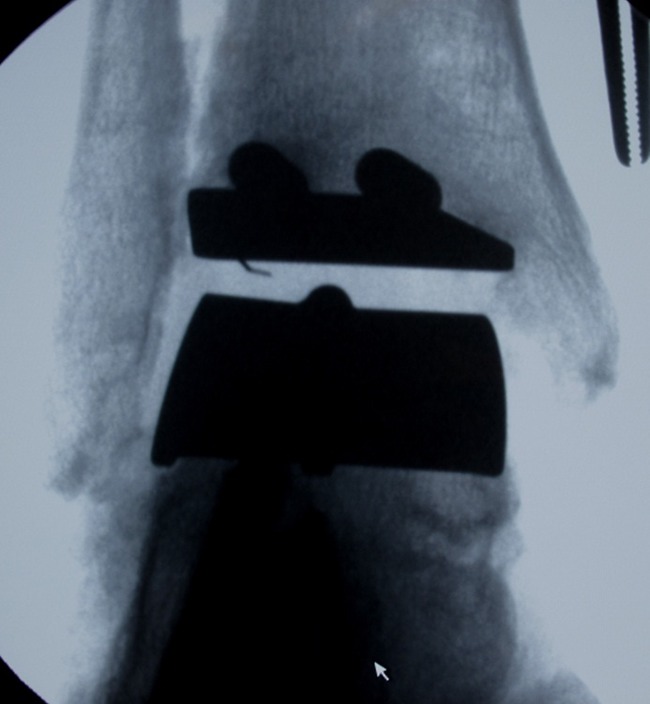
Intraoperative fluoroscopic view demonstrating decompression of the medial gutter
Our experience
A total of twenty ankles in twenty patients were identified that have been treated using the arthroscopic technique described above. All twenty of the patients were treated by the two senior authors. Of the twenty patients who underwent arthroscopic debridement, eighteen patients had sufficient follow-up to determine the success of the procedure. Sixteen of these twenty patients (80 %) reported an initial resolution of their pain following the procedure. Of these sixteen patients, six developed recurrent symptoms and ultimately required further intervention, three of whom went on to have an open arthrotomy. Two of these patients had a distal fibular resection and one had a distal medial malleolar resection. Of the four patients with poor outcomes, four are considering repeat surgical intervention (one patient has gone on to develop subsidence of her talar component and is being considered for revision arthrodesis, two patients are considering repeat arthroscopy, and one is considering an open arthrotomy). No wound complications were reported, and no post-operative infections were reported. All procedures were performed on an outpatient basis, and none of the patients were admitted to the hospital following the procedure.
Discussion
Total ankle arthroplasty has recently been gaining popularity for the treatment of ankle arthritis due to improved success rates with the latest generations of prosthetic implants. Despite these recent improvements, pain resolution is not absolute. Revision surgery secondary to persistent pain due to bony impingement has been reported in 6–45 % of cases [4•, 5•, 11, 13, 14]. An arthroscopic technique that has recently been published challenges the standard of treatment, open ankle arthrotomy [15]. Arthroscopic debridement of impingement due to soft tissue has been shown to be an effective method of relieving pain secondary to impingement in the native ankle, while having the benefit of being able to be performed as an outpatient procedure with minimal recovery time and limited post-operative morbidity when compared with open arthrotomy. Scranton et al. demonstrated that despite being planned as an outpatient procedure, 27 % of patients who underwent open arthrotomy for anterior ankle impingement required 2–3 days post-operative hospitalization for pain control. None of their patients who underwent arthroscopic debridement required hospitalization for pain control. Additionally, patients who underwent arthroscopic debridement had a faster average functional recovery of 5 weeks versus 8 weeks in the arthrotomy group [16].
While these results have been established in the literature in native ankles, to our knowledge, no comparative data looking at the post-operative result of open arthrotomy versus arthroscopic debridement following TAA has been published. Both techniques have been described following TAA in the literature [4•, 5•, 11, 13, 14]. Our experience demonstrates that arthroscopic debridement of bony and soft tissue impingement following TAA echoes the results seen in the native ankle. The procedure was performed on an outpatient basis; patients demonstrated minimal post-operative recovery time and had minimal post-operative morbidity. The obvious concern specific to arthroscopy following TAA is iatrogenic damage to the TAA prosthesis. With careful placement of the portal incisions and care with placement of the arthroscopic devices, iatrogenic damage can be avoided. However, further investigation into the true incidence of implant damage is needed as this was not specifically monitored in our current patient population.
Conclusion
Impingement following total ankle arthroplasty remains a significant source of post-operative pain and cause for subsequent reoperation. Treatment of symptomatic impingement has been described by debridement through an open arthrotomy as well as via arthroscopic debridement. Our experience with the arthroscopic technique described demonstrates that arthroscopic debridement is both a medically and cost-effective treatment option.
Acknowledgments
Disclosure
No conflicts of interest relevant to this article were reported.
Contributor Information
Andrew B. Richardson, Phone: +1-919-6848111, FAX: +1-919-6817672, Email: andrew.richardson@dm.duke.edu
James K. DeOrio, Phone: +1-919-6602358, FAX: +1-919-6608568, Email: james.deorio@duke.edu
Selene G. Parekh, Phone: +1-919-4719622, FAX: +1-919-4771929, Email: selene.parekh@gmail.com
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Saltzman CL, Mann RA, Ahrens JE, et al. Prospective controlled trial of star total ankle replacement versus ankle fusion: initial results. Foot Ankle Int. 2009;30(7):579–596. doi: 10.3113/FAI.2009.0579. [DOI] [PubMed] [Google Scholar]
- 2.Saltzman CL, Kadoko RG, Suh JS. Treatment of isolated ankle osteoarthritis with arthrodesis or the total ankle replacement: a comparison of early outcomes. Clinics in Orthopedic Surgery. 2010;2(1):1–7. doi: 10.4055/cios.2010.2.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.SooHoo NF, Zingmond DS, Ko CY. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J Bone Joint Surg Am. 2007;89(10):2143–2149. doi: 10.2106/JBJS.F.01611. [DOI] [PubMed] [Google Scholar]
- 4.Mann JA, Mann RA, Horton E. STAR (TM) Ankle: Long-Term Results. Foot Ankle Int. 2011;32(5):473–484. doi: 10.3113/FAI.2011.0473. [DOI] [PubMed] [Google Scholar]
- 5.Easley ME, Adams SB, Hembree WC, et al. Results of total ankle arthroplasty. J Bone Joint Surg Am. 2011;93A(15):1455–1468. doi: 10.2106/JBJS.J.00126. [DOI] [PubMed] [Google Scholar]
- 6.Haddad SL, Coetzee JC, Estok R, et al. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis - A systematic review of the literature. J Bone Joint Surg Am. 2007;89A(9):1899–1905. doi: 10.2106/JBJS.F.01149. [DOI] [PubMed] [Google Scholar]
- 7.Pyevich MT, Saltzman CL, Callaghan JJ, et al. Total ankle arthroplasty: a unique design - Two to twelve-year follow-up. J Bone Joint Surg Am. 1998;80A(10):1410–1420. [PubMed] [Google Scholar]
- 8.Spirt AA, Assal M, Hansen ST. Complications and failure after total ankle arthroplasty. J Bone Joint Surg Am. 2004;86A(6):1172–1178. doi: 10.2106/00004623-200406000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Kopp FJ, Patel MM, Deland JT, et al. Total ankle arthroplasty with the agility prosthesis: Clinical and radiographic evaluation. Foot Ankle Int. 2006;27(2):97–103. doi: 10.1177/107110070602700205. [DOI] [PubMed] [Google Scholar]
- 10.Knecht SI, Estin M, Callaghan JJ, et al. The agility total ankle arthroplasty - Seven to sixteen-year follow-up. J Bone Joint Surg Am. 2004;86A(6):1161–1171. [PubMed] [Google Scholar]
- 11.Rippstein PF, Huber M, Coetzee C, et al. Total ankle replacement with use of a new three-component implant. J Bone Joint Surg Am. 2011;93A(15):1426–1435. doi: 10.2106/JBJS.J.00913. [DOI] [PubMed] [Google Scholar]
- 12.Lee KB, Cho YJ, Park JK, et al. Heterotopic ossification after primary total ankle arthroplasty. J Bone Joint Surg Am. 2011;93A(8):751–758. doi: 10.2106/JBJS.J.00178. [DOI] [PubMed] [Google Scholar]
- 13.Hintermann B, Valderrabano V, Dereymaeker G, et al. The HINTEGRA ankle: Rationale and short-term results of 122 consecutive ankles. Clin Orthop. 2004;424:57–68. doi: 10.1097/01.blo.0000132462.72843.e8. [DOI] [PubMed] [Google Scholar]
- 14.Kurup HV, Taylor GR. Medial impingement after ankle replacement. Int Orthop. 2008;32(2):243–246. doi: 10.1007/s00264-006-0300-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shirzad K, Viens NA, DeOrio JK. Arthroscopic treatment of impingement after total ankle arthroplasty: technique tip. Foot Ankle Int. 2011;32(7):727–729. doi: 10.3113/FAI.2011.0727. [DOI] [PubMed] [Google Scholar]
- 16.Scranton PE, Mcdermott JE. Anterior tibiotalar spurs - a comparison of open versus arthroscopic debridement. Foot Ankle. 1992;13(3):125–129. doi: 10.1177/107110079201300303. [DOI] [PubMed] [Google Scholar]
- 17.Ferkel RD, Scranton PE. Arthroscopy of the Ankle and Foot. J Bone and Joint Surg Am. 1993;75A(8):1233–1242. doi: 10.2106/00004623-199308000-00016. [DOI] [PubMed] [Google Scholar]


