Abstract
Background
During in-hospital cardiac arrests, it is uncertain how long resuscitation should continue prior to termination of efforts. We hypothesized that the duration of resuscitation varies across hospitals, and that patients at hospitals with longer attempts have higher survival rates.
Methods
Between 2000 and 2008, we identified 64,339 patients with cardiac arrests at 435 hospitals within a large national registry. For each hospital, we calculated the median duration of resuscitation before termination of efforts among its non-survivors as a measure of the hospital’s overall tendency for longer attempts. We then determined the association between a hospital’s tendency for longer attempts and risk-adjusted survival using multilevel regression models.
Findings
The overall proportion of patients achieving immediate survival with return of spontaneous circulation (ROSC) was 48·5% while 15·4% survived to discharge. For patients achieving ROSC, the median resuscitation time was 12 minutes (IQR: 6–21) while it was 20 minutes (IQR: 14–30) for those not achieving ROSC (i.e., non-survivors). Compared with patients at hospitals with the shortest attempts (median duration, 16 minutes), patients at hospitals with the longest attempts (median duration, 25 minutes) had a higher likelihood of ROSC (adjusted risk-ratio 1·12, [95% CI: 1·06–1·18]; p <0·001) and survival to discharge (adjusted risk-ratio 1·12, [95% CI: 1·02–1·23]; p=0·021). These findings were more prominent in cardiac arrests due to asystole and pulseless electrical activity (p for interaction<0.01 for both ROSC and survival to discharge).
Interpretation
The duration of resuscitation attempts varies across hospitals. Patients at hospitals with longer attempts have a higher likelihood of ROSC and survival to discharge, particularly when the arrest is due to asystole and pulseless electrical activity.
Funding
The American Heart Association, the Robert Wood Johnson Foundation Clinical Scholars Program, the National Institutes of Health.
Of every 1000 patients hospitalized in Western countries, it is estimated that between 1 and 5 will suffer a cardiac arrest with fewer than 20% surviving to discharge.1,2 One of the most challenging decisions facing clinicians who care for these patients is determining when to terminate resuscitation efforts. Clinicians are frequently reluctant to continue efforts when return of spontaneous circulation (ROSC) has not occurred early on during cardiac arrest, given the overall poor prognosis for such patients.3 However, there is unfortunately a lack of empirical evidence to guide clinicians regarding an appropriate length of attempts at resuscitation prior to termination of efforts. In the absence of such data, guidelines have been unable to directly address this issue,4,5 and clinicians have come to rely largely upon case series and expert opinion to guide their practice.3,6–9 Although this has likely led to considerable differences in the duration of resuscitation attempts among non-survivors, little is known about the extent of such variation in routine practice and its potential relationship with survival.
Accordingly, we assessed patterns of duration in resuscitation attempts and risk-adjusted survival at a large number of hospitals in the United States. Rather than examining hospital-level variation in resuscitation duration among all hospitalized patients with cardiac arrest, however, we specifically focused on non-survivors in order to approximate each hospital’s overall tendency for practicing longer attempts prior to termination of efforts. We then hypothesized that the duration of resuscitation among non-survivors would vary substantially across hospitals, and that patients at hospitals with longer attempts would have a higher likelihood of ROSC and survival to discharge.
METHODS
Data source
Formerly known as the National Registry of Cardiopulmonary Resuscitation (NRCPR), the Get With the Guidelines–Resuscitation (GWTG–R) is a large, multicenter observational registry of in-hospital cardiac arrests. The database has been described in detail in previous studies.10,11 Briefly, trained research personnel at participating hospitals prospectively collect information on consecutive patients with in-hospital cardiac arrests, defined by the absence of a central palpable pulse, apnea, and unresponsiveness. Cases are identified by centralized collection of cardiac arrest flow sheets, reviews of hospital paging-system logs, routine checks for use of code carts (carts stocked with emergency equipment), and hospital billing charges for resuscitation medications. The registry uses standard Utstein definitions, which are precisely defined variables for uniform reporting of cardiac arrests developed by international experts.12
Study population
Between January 1, 2000 and August 26, 2008, we identified 93,535 patients aged 18 years or older at 537 acute care hospitals with an “index” in-hospital cardiac arrest (i.e., the first arrest for a patient during a hospitalization) due to pulseless ventricular tachycardia (VT), ventricular fibrillation (VF), pulseless electrical activity (PEA), and asystole.
Because of the distinct circumstances of cardiac arrests in certain settings, we excluded a total of 18,604 patients who were in emergency departments, operating rooms, post-operative areas, procedure areas (e.g., cardiac catheterization, electrophysiology, and angiography suites), rehabilitation areas, or whose location was unknown or missing at the time of their cardiac arrest.
We also excluded 1,330 patients with implantable cardioverter-defibrillators. We further restricted our sample to hospitals with 10 or more arrests during the study period and that reported at least 6 months of data, excluding 6,099 patients from 96 hospitals that did not meet these criteria. Finally, we excluded 3,163 patients with cardiac arrests that lasted less than two minutes to avoid “partial” resuscitations, or incomplete data on resuscitation duration. Our final study population consisted of 64,339 patients at 435 hospitals (see Appendix Figure 1).
Study definitions and endpoints
Our 2 primary study endpoints focused on survival: (1) immediate survival with ROSC during the cardiac arrest; and (2) survival to hospital discharge. ROSC was specifically defined as the restoration of a pulse for at least 20 minutes during the cardiac arrest. In addition, we performed analyses to evaluate concerns about whether longer resuscitation attempts resulted in worse neurological status despite improvements in survival (see details below). Neurological status was available for 8,724 (84·6%) patients who survived to discharge and was categorized into 5 groups based on previously developed cerebral performance categories (CPCs), measured at the time of hospital discharge: no major disability, moderate disability, severe disability, coma or vegetative state, and brain death.13 Consistent with prior work, a favourable neurological status was defined as a CPC score of 1 or 2.14,15
Covariate of interest
The key independent variable for these analyses was the median duration of resuscitation attempts at a hospital among its non-survivors—patients who never achieved ROSC prior to the termination of efforts. Duration (in minutes) was coded as integers, and specifically defined as the time from onset of cardiac arrest to when efforts were terminated and the patient declared dead. Onset of cardiac arrest was defined as when the absence of a palpable central pulse, apnea, or unresponsiveness was first recognized. Efforts were considered terminated at the time when cardiopulmonary resuscitation was stopped in patients without ROSC. We focused on non-survivors (rather than all patients) when calculating the median duration of resuscitation attempts for a hospital, given that a hospital’s overall propensity for longer resuscitation efforts would be best reflected by its length of attempts in patients who ultimately did not survive. For instance, a hospital that routinely performed resuscitation for a median of 30 minutes among its non-survivors would be considered to practice more prolonged attempts than a hospital whose non-survivors were resuscitated for a median of 15 minutes.
Statistical analyses
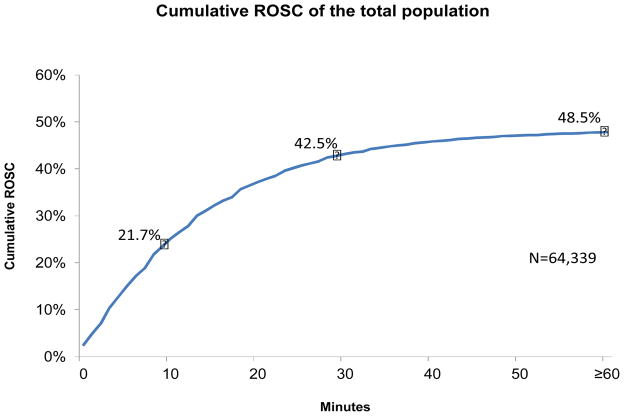
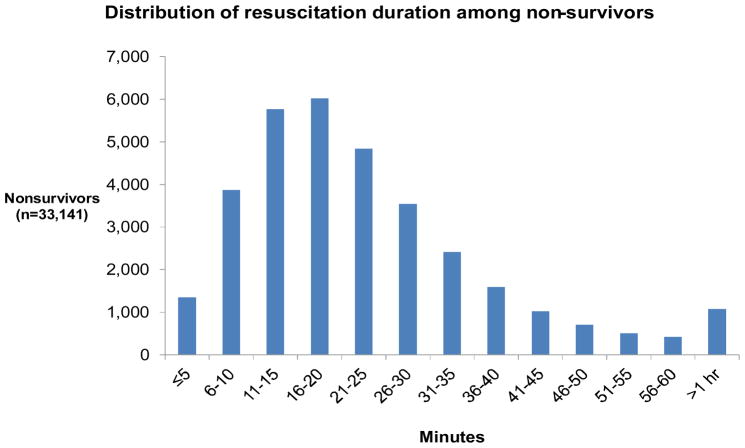
We stratified patients by survival status and resuscitation duration (≤10, 11–19, 20–29, and ≥30 minutes). We employed Kruskal-Wallis and Chi-square tests, as appropriate, to compare baseline patient differences in demographics and clinical characteristics across strata of resuscitation duration. We then graphed the cumulative rates of ROSC in the entire study cohort, as well as the distribution of resuscitation duration in non-survivors.
We used multilevel Poisson regression models with hospital-specific, random intercepts to determine the association between patients achieving ROSC and their hospital’s median duration of resuscitation attempts.16 Because odds ratios generated from logistic regression may overestimate risk when the frequency of outcome is high,17,18 we used Poisson regression to directly estimate risk-ratios for ROSC. We classified hospitals into quartiles based on their median duration of resuscitation among non-survivors, prior to their inclusion in these models.
Based on previous work,19 the regression models adjusted for additional patient-level covariates that may be linked to outcomes: “shockable” initial pulseless rhythms (pulseless VT and VF); age; race; illness category (medical non-cardiac, medical cardiac, surgical cardiac, surgical non-cardiac and trauma, obstetric, and other); pre-existing conditions (none, myocardial infarction during hospitalization, hypotension/hypoperfusion, hepatic insufficiency, baseline depression in central nervous system function, acute stroke, infection or septicemia, metastatic or haematologic malignancy, renal failure, major trauma); interventions in place at the time of cardiac arrest (invasive airway, chest tube, assisted or mechanical ventilation, vasopressors, antiarrhythmics, vasodilators); monitoring with an arterial line; a witnessed arrest; event location (intensive care unit [ICU], general floor/telemetry); and the time from admission to event. The models also accounted for: off-hours cardiac arrest (weekend or nights [11pm–7am]); initiation and time to first chest compressions; and study period (years 2002–2002, 2003–2005, and 2006–2008).
Finally, we adjusted for hospital characteristics that were available in 411 (94·5%) of the 435 hospitals after merging the data with information available from the 2009 American Hospital Association Annual Survey,20 with missing information accounted for using an indicator variable as a separate covariate. The hospital characteristics included were: geographic region, rural location, availability of cardiothoracic surgery, and the presence of an emergency department.
Similar regression models were constructed to evaluate survival to discharge, and survival rates after stratifying patients based on their presenting rhythm (asystole and PEA versus pulseless VT and VF).
Finally, we evaluated the concern of whether higher survival rates at hospitals with longer attempts may be associated with a worse neurologic status among survivors at those hospitals due to potentially prolonged efforts. For these analyses, we constructed similar regression models that examined the likelihood of survival with a favourable neurological status (i.e., defined as a CPC score of 1 or 2) across the quartiles of hospitals.
During all analyses, p-values of <0·05 were considered significant and all test were 2-sided. Stata version 11 (StataCorp, LP, College Station, TX) was used for all analyses.
Role of the funding source
Oversight for the entire process of data collection, analysis, and reporting is provided by the American Heart Association (AHA), its National Center staff, the NRCPR/GWTG–R Scientific Advisory Board (SAB), and the AHA Executive Database Steering Committee (EDSC).21 Research proposals to the GWTG–R are sequentially reviewed by a Data Manager, the Research Task Force, a Scientific Advisory Board Sponsor, and final approval is granted by the AHA EDSC. The original draft of the manuscript was reviewed by the EDSC, and appropriate revisions were incorporated prior to submitting for publication. The institutional review board of the University of Michigan Medical School approved this study and waived the requirement for written informed consent. Drs. Goldberger and Nallamothu had full access to the study data, vouch for the accuracy and completeness of the analysis, and had final responsibility to submit for publication.
RESULTS
Study Population
We identified 64,339 patients with an in-hospital cardiac arrest at 435 hospitals. The initial cardiac arrest rhythm was VT or VF in 12,924 (20·1%), and PEA or asystole in 51,415 (79·9%) patients. Overall, the median resuscitation duration in the study population including both survivors and non-survivors was 17 minutes (interquartile range [IQR]: 10–26). A total of 31,198 (48·5%) patients achieved ROSC, while 33,141 (51·5%) patients died after termination of resuscitation efforts. For patients achieving ROSC, the median resuscitation time was 12 minutes (IQR: 6–21) while it was 20 minutes (IQR: 14–30) for non-survivors who died after termination of efforts.
Among those who achieved ROSC, mean hospital length of stay (truncated at death or hospital discharge) was 8·3 days (standard deviation [SD]: 15·0). By comparison, 9,912 (15·4%) patients ultimately survived to discharge with mean hospital length of stay from ROSC to discharge of 16·6 days (SD: 18·0). Among 8,724 patients who survived to discharge and who also had CPC assessments, 7,034 (80·6%) had a favourable neurological status (CPC ≤ 2). The rate of a favourable neurological status among survivors to discharge did not significantly differ based on resuscitation duration (4,738 of 5,838 [81·2%] for those with resuscitation durations of <15 minutes versus 1,724 of 2,156 [80·0%] for ≥15 minutes to ≤30 minutes, and 572 of 730 [78·4%] for those with resuscitation durations >30 minutes; p for comparison, 0·131). However, mean and median CPC assessments were modestly higher among patients with longer resuscitation durations. A complete breakdown of CPC assessments by resuscitation duration for the entire cohort overall, and stratified by rhythm type, is shown in Appendix Table 1.
Baseline characteristics of patients who achieved ROSC and non-survivors are described in Tables 1 and 2, respectively, stratified by resuscitation duration. A number of statistically significant differences were demonstrated due to the large size of the study population; however, sizeable differences between baseline characteristics and shorter attempted resuscitation duration were less frequent. Among patients who achieved ROSC, those differences included a higher percentage of patients with resuscitation durations ≤10 minutes among those with pre-existing conditions like septicaemia or major trauma; critical care interventions in place at time of arrest; arrests in the ICU; and witnessed arrests (Table 1). By comparison, among non-survivors—other than those with myocardial infarction during admission—a larger percentage of patients with pre-existing conditions were resuscitated ≤10 minutes compared with ≥30 minutes (Table 2).
TABLE 1.
Baseline characteristics of patients achieving ROSC stratified by duration of resuscitation*
| Overall (n=31,198) | ≤10 minutes (n=13,964) | 11–19 minutes (n=7,881) | 20–29 minutes (n=4,933) | ≥30 minutes (n=4,420) | P | |
|---|---|---|---|---|---|---|
| Age (years) | 0·0001 | |||||
| Median | 69 | 68 | 69 | 70 | 68 | |
| Interquartile Range | 57–78 | 56–78 | 57–78 | 57–79 | 56–78 | |
| Male Sex, % (n) | 55·8 (17,405) | 55·5 (7,753) | 56·3 (4,439) | 55·8 (2,750) | 55·7 (2,463) | 0·723 |
| Race, % (n) | <0·0001 | |||||
| Black | 19·0 (5,921) | 18·7 (2,615) | 21·2 (1,672) | 17·1 (842) | 17·9 (792) | |
| Non-black | 81·0 (25,277) | 81·3 (11,349) | 78·8 (6,209) | 82·9 (4,091) | 82·1 (3,628) | |
| Pre-existing conditions, % (n) | ||||||
| Renal insufficiency | 37·1 (11,576) | 36·3 (5,064) | 39·1 (3,083) | 37·3 (1,840) | 36·0 (1,589) | <0·0001 |
| Hepatic insufficiency | 8·8 (2,748) | 8·9 (1,244) | 8·9 (699) | 8·4 (412) | 8·9 (393) | 0·676 |
| Malignancy | 11·9 (3,725) | 11·3 (1,582) | 13·0 (1,027) | 12·2 (600) | 11·7 (516) | 0·002 |
| Decrease in CNS function | 13·9 (4,347) | 14·8 (2,064) | 14·2 (1,120) | 13·1 (644) | 11·7 (519) | <0·0001 |
| Septicemia | 17·7 (5,534) | 18·2 (2,547) | 18·5 (1,459) | 17·1 (845) | 15·5 (683) | <0·0001 |
| Major trauma | 3·5 (1,082) | 4·1 (577) | 3·1 (247) | 2·7 (132) | 2·9 (126) | <0·0001 |
| Acute stroke | 4·5 (1,398) | 4·7 (650) | 4·4 (350) | 4·5 (221) | 4·0 (177) | 0·339 |
| None | 3·1 (956) | 2·8 (392) | 2·9 (225) | 3·2 (158) | 4·1 (181) | <0·0001 |
| Hypotension/hypoperfusion | 28·8 (8,973) | 29·8 (4,166) | 27·6 (2,176) | 27·9 (1,378) | 28·4 (1,253) | 0·002 |
| MI during admission | 19·6 (6,127) | 20·8 (2,903) | 18·0 (1,416) | 19·0 (938) | 19·7 (870) | <0·0001 |
| Critical care interventions in place at time of arrest, % (n) | ||||||
| Assisted/mechanical ventilation | 30·4 (9,474) | 36·3 (5,071) | 26·2 (2,067) | 24·8 (1,221) | 25·2 (1,115) | <0·0001 |
| Invasive airway | 30·0 (9,360) | 35·8 (4,996) | 25·8 (2,030) | 24·7 (1,217) | 25·3 (1,117) | <0·0001 |
| Vasopressors | 28·1 (8,772) | 31·5 (4,396) | 25·5 (2,008) | 25·0 (1,235) | 25·6 (1,133) | <0·0001 |
| Antiarrhythmics | 7·5 (2,327) | 8·5 (1,182) | 6·6 (523) | 6·5 (318) | 6·9 (304) | <0·0001 |
| Vasodilators | 1·6 (495) | 1·9 (265) | 1·2 (91) | 1·4 (69) | 1·6 (70) | <0·0001 |
| Arterial line | 11·2 (3,480) | 13·4 (1,875) | 9·3 (730) | 8·9 (440) | 9·8 (435) | <0·0001 |
| Chest tube | 4·3 (1,348) | 4·9 (685) | 3·5 (272) | 4·2 (205) | 4·2 (186) | <0·0001 |
| 1·6 (495) | 1·9 (265) | 1·2 (91) | 1·4 (69) | 1·6 (70) | <0·0001 | |
| Location, % (n) | <0·0001 | |||||
| ICU | 59·4 (18,528) | 66·8 (9,323) | 52·8 (4,160) | 52·8 (2,602) | 55·3 (2,443) | |
| General floor/telemetry | 40·6 (12,670) | 33·2 (4,641) | 47·2 (3,721) | 47·3 (2,331) | 44·7 (1,977) | |
| Rhythm during arrest, % (n) | <0·0001 | |||||
| VT/VF | 25·8 (8,040) | 28·0 (3,912) | 22·8 (1,799) | 25·0 (1,236) | 24·7(1,093) | <0·0001 |
| PEA/asystole | 74·2 (23,158) | 72·0 (10,052) | 77·2 (6,082) | 75·0 (3,697) | 75·3 (3,327) | |
| Illness category, % (n) | <0·0001 | |||||
| Medical/cardiac | 33·8 (10,537) | 33·8 (4,713) | 33·1 (2,611) | 34·3 (1,694) | 34·4 (1,519) | |
| Medical/noncardiac | 43·1 (13,442) | 41·6 (5,808) | 46·3 (3,646) | 44·1 (2,174) | 41·0 (1,814) | |
| Surgical/cardiac | 9·3 (2,907) | 10·2 (1,419) | 7·3 (574) | 8·9 (439) | 10·8 (475) | |
| Surgical/noncardiac and trauma | 13·7 (4,263) | 14·4 (2,007) | 13·2 (1,038) | 12·6 (619) | 13·6 (599) | |
| Obstetric | 0·09 (29) | 0·08 (11) | 0·09 (7) | 0·08 (4) | 0·16 (7) | |
| Other | 0·06 (20) | 0·04 (6) | 0·06 (5) | 0·06 (3) | 0·14 (6) | |
| Witnessed arrest, % (n) | <0·0001 | |||||
| Witnessed | 81·3 (25,367) | 85·3 (11,907) | 78·2 (6,162) | 76·8 (3,790) | 79·4 (3,508) | |
| Not witnessed | 18·7 (5,831) | 14·7 (2,057) | 21·8 (1,719) | 23·2 (1,143) | 20·6 (912) | |
| Arrests on nights/weekends, % (n) | 41·4 (12,929) | 39·5 (5,518) | 43·5 (3,430) | 42·0 (2,071) | 43·2 (1,910) | <0·0001 |
The group resuscitated for 11–19 minutes excludes those resuscitated ≤10 minutes and ≥20 minutes; the group resuscitated for 20–29 minutes excludes those resuscitated ≤20 minutes and ≥30 minutes; the group resuscitated for ≥30 minutes excludes those resuscitated <30 minutes
CHF = congestive heart failure; CNS = central nervous system; ICU = intensive care unit; MI = myocardial infarction; PEA = pulseless electrical activity; VF = ventricular fibrillation; VT = ventricular tachycardia
TABLE 2.
Baseline characteristics of non-survivors stratified by duration of resuscitation*
| Overall (n=33,141) | ≤10 minutes (n=5,221) | 11–19 minutes (n=10,083) | 20–29 minutes (n=9,061) | ≥30 minutes (n=8,776) | P | |
|---|---|---|---|---|---|---|
| Age (years) | 0·0001 | |||||
| Median | 70 | 72 | 72 | 70 | 67 | |
| Interquartile Range | 57–80 | 59–82 | 59–81 | 57–79 | 55–77 | |
| Male Sex, % (n) | 59·6 (19,736) | 59·4 (3,103) | 59·7 (6,023) | 60·5 (5,483) | 58·4 (5,127) | 0·040 |
| Race, % (n) | <0·0001 | |||||
| Black | 21·7 (7,188) | 20·3 (1,058) | 22·0 (2,213) | 23·1 (2,092) | 20·8 (1,825) | |
| Non-black | 78·3 (25,953) | 79·7 (4,163) | 78·1 (7,870) | 76·9 (6,969) | 79·2 (6,951) | |
| Pre-existing conditions, % (n) | ||||||
| Renal insufficiency | 34·6 (11,458) | 36·1 (1,884) | 35·1 (3,545) | 34·1 (3,088) | 33·5 (2,941) | 0·007 |
| Hepatic insufficiency | 8·2 (2,724) | 10·7 (557) | 8·5 (859) | 7·7 (698) | 7·0 (610) | <0·0001 |
| Malignancy | 15·1 (4,995) | 17·7 (923) | 16·4 (1,656) | 14·4 (1,301) | 12·7 (1,115) | <0·0001 |
| Decrease in CNS function | 14·7 (4,855) | 17·9 (934) | 16·1 (1,619) | 13·9 (1,255) | 11·9 (1,047) | <0·0001 |
| Septicemia | 17·4 (5,752) | 22·0 (1,150) | 19·0 (1,915) | 15·6 (1,413) | 14·5 (1,274) | <0·0001 |
| Major trauma | 3·5 (1,173) | 5·0 (263) | 3·5 (354) | 3·1 (280) | 3·2 (276) | <0·0001 |
| Acute stroke | 4·5 (1,503) | 5·0 (262) | 4·7 (471) | 4·6 (412) | 4·1 (358) | 0·059 |
| None | 3·9 (1,302) | 3·1 (162) | 3·8 (378) | 4·2 (383) | 4·3 (379) | 0·001 |
| Hypotension/hypoperfusion | 29·4 (9,734) | 36·0 (1,881) | 28·8 (2,908) | 26·7 (2,419) | 28·8 (2,526) | <0·0001 |
| MI during admission | 16·0 (5,300) | 13·1 (685) | 14·1 (1,419) | 16·7 (1,516) | 19·2 (1,680) | <0·0001 |
| Critical care interventions in place at time of arrest, % (n) | ||||||
| Assisted/mechanical ventilation | 30·6 (10,140) | 44·1 (2,304) | 30·3 (3,052) | 24·9 (2,258) | 28·8 (2,526) | <0·0001 |
| Invasive airway | 30·1 (9,967) | 43·5 (2,271) | 30·1 (3,030) | 24·6 (2,232) | 27·7 (2,434) | <0·0001 |
| Vasopressors | 29·7 (9,856) | 41·4 (2,163) | 29·3 (2,956) | 24·9 (2,258) | 28·3 (2,479) | <0·0001 |
| Antiarrhythmics | 4·4 (1,468) | 5·5 (288) | 3·8 (385) | 4·0 (361) | 5·0 (434) | <0·0001 |
| Vasodilators | 1·1 (379) | 0·8 (40) | 0·9 (93) | 1·3 (113) | 1·5 (133) | <0·0001 |
| Arterial line | 8·6 (2,853) | 11·2 (587) | 8·0 (808) | 7·0 (633) | 9·4 (825) | <0·0001 |
| Chest tube | 2·8 (941) | 3·1 (164) | 2·2 (220) | 2·4 (215) | 3·9 (342) | <0·0001 |
| Location, % (n) | <0·0001 | |||||
| ICU | 54·0 (17,886) | 64·0 (3,339) | 51·4 (5,181) | 48·2 (4,371) | 56·9 (4,995) | |
| General floor/telemetry | 46·0 (15,255) | 36·1 (1,882) | 48·6 (4,902) | 51·8 (4,690) | 43·1 (3,781) | |
| Rhythm during arrest, % (n) | <0·0001 | |||||
| VT/VF | 14·7 (4,884) | 12·3 (641) | 13·2 (1,326) | 15·5 (1,408) | 17·2 (1,509) | <0·0001 |
| PEA/asystole | 85·3 (28,257) | 87·7 (4,580) | 86·8 (8,757) | 84·5 (7,653) | 82·8 (7,267) | |
| Illness category, % (n) | <0·0001 | |||||
| Medical/cardiac | 30·3 (10,040) | 27·2 (1,419) | 28·1 (2,836) | 31·1 (2,821) | 33·8 (2,964) | |
| Medical/noncardiac | 50·4 (16,701) | 54·4 (2,841) | 54·0 (5,445) | 50·5 (4,572) | 43·8 (3,843) | |
| Surgical/cardiac | 5·1 (1,692) | 3·7 (193) | 3·6 (359) | 4·4 (401) | 8·4 (739) | |
| Surgical/noncardiac and trauma | 14·1 (4,667) | 14·7 (766) | 14·2 (1,435) | 13·9 (1,255) | 13·8 (1,211) | |
| Obstetric | 0·08 (26) | 0·02 (1) | 0·05 (5) | 0·07 (6) | 0·16 (14) | |
| Other | 0·05 (15) | 0·02 (1) | 0·03 (3) | 0·07 (6) | 0·06 (5) | |
| Witnessed arrest, % (n) | <0·0001 | |||||
| Witnessed | 74·1 (24,551) | 77·1 (4,023) | 71·0 (7,158) | 71·4 (6,471) | 78·6 (6,899) | |
| Not witnessed | 25·9 (8,590) | 23·0 (1,198) | 29·0 (2,925) | 28·6 (2,590) | 21·4 (1,877) | |
| Arrests on nights/weekends, % (n) | 46·7 (15,504) | 46·1 (2,408) | 47·1 (4,749) | 47·0 (4,253) | 46·7 (4,094) | <0·0001 |
The group resuscitated for 11–19 minutes excludes those resuscitated ≤10 minutes and ≥20 minutes; the group resuscitated for 20–29 minutes excludes those resuscitated ≤20 minutes and ≥30 minutes; the group resuscitated for ≥30 minutes excludes those resuscitated <30 minutes
CHF = congestive heart failure; CNS = central nervous system; ICU = intensive care unit; MI = myocardial infarction; PEA = pulseless electrical activity; VF = ventricular fibrillation; VT = ventricular tachycardia
Figure 1 displays the cumulative rates of ROSC for the overall study cohort over time. Of the 48·5% who achieved ROSC, 87·6% had restoration of a pulse by 30 minutes (representing 42·5% of the study sample). These trends were consistent across different groups based on the rhythm at presentation (Appendix Figure 2). As shown in Figure 2, among non-survivors, efforts were terminated within 10 minutes in 15·8% and within 30 minutes in 76·6%.
Figure 1.
Shown is the cumulative percentage of patients achieving ROSC. Overall, 48·5% of the total population achieved ROSC. By 30 minutes, 42·5% achieved ROSC.
Figure 2.
Shown is the distribution of resuscitation duration among non-survivors; efforts were terminated within 10 minutes in 15·8% and within 30 minutes in 76·6%.
Resuscitation Duration and Survival
The median resuscitation duration among non-survivors of hospitals in the shortest quartile was 16 minutes, rising to 19, 22, and 25 minutes in subsequent quartiles of hospitals with longer median resuscitation durations. Overall, patients with cardiac arrests at hospitals with longer median resuscitation durations had higher overall survival. For example, patients at hospitals with the longest median duration (25 minutes) had a 12% higher likelihood of achieving ROSC (adjusted risk-ratio 1·12, [95% CI: 1·06–1·18]; p<0·001) compared with patients at hospitals with the shortest median duration (16 minutes) (Table 3a). This effect was most prominent among patients with cardiac arrests due to PEA or asystole (p for interaction effect, 0·002), although in patients with VT or VF the same trend approached statistical significance across hospital quartiles. Stratified results in each of these groups are presented in Table 3b.
TABLE 3a.
Adjusted risk ratios and rates by hospital quartile: ROSC and survival to discharge among all patients
| ROSC* | Survival to discharge** | |||||
|---|---|---|---|---|---|---|
| Total 64,339 patients at 435 hospitals |
Adjusted risk- ratio (95% CI) | Adjusted rate | P | Adjusted risk- ratio (95% CI) | Adjusted rate | P |
|
Quartile 1 13,994 patients at 113 hospitals Median: 16 minutes |
Ref | 45·3% | Ref | Ref | 14·5% | Ref |
|
Quartile 2 18,783 patients at 121 hospitals Median: 19 minutes |
1·04 (0·99–1·09) | 47·0% | 0·116 | 1·05 (0·96–1·14) | 15·2% | 0·304 |
|
Quartile 3 19,106 patients at 107 hospitals Median: 22 minutes |
1·08 (1·03–1·13) | 48·8% | 0·002 | 1·05 (0·96–1·14) | 15·2% | 0·280 |
|
Quartile 4 12,456 patients at 94 hospitals Median: 25 minutes |
1·12 (1·06–1·18) | 50·7% | <0·0001 | 1·12 (1·02–1·23) | 16·2% | 0·021 |
ROSC = return of spontaneous circulation
P for trend <0·0001
P for trend 0·031
TABLE 3b.
Adjusted risk-ratios and rates for ROSC by hospital quartile: PEA/asystole and VT/VF*
| PEA/asystole*¶ | VT/VF** | |||||
|---|---|---|---|---|---|---|
| Total 64,339 patients at 435 hospitals |
Adjusted risk-ratio (95% CI) | Adjusted rate | P | Adjusted risk-ratio (95% CI) | Adjusted rate | P |
|
Quartile 1 13,994 patients at 113 hospitals Median: 16 minutes |
Ref | 41·6% | Ref | Ref | 60·6% | Ref |
|
Quartile 2 18,783 patients at 121 hospitals Median: 19 minutes |
1·04 (0·99–1·09) | 43·1% | 0·158 | 1·03 (0·98–1·08) | 62·4% | 0·224 |
|
Quartile 3 19,106 patients at 107 hospitals Median: 22 minutes |
1·10 (1·04–1·16) | 45·6% | 0·001 | 1·02 (0·98–1·07) | 61·8% | 0·400 |
|
Quartile 4 12,456 patients at 94 hospitals Median: 25 minutes |
1·15 (1·08–1·22) | 47·7% | <0·0001 | 1·06 (1·01–1·11) | 64·1% | 0·027 |
PEA = pulseless electrical activity; VT = ventricular tachycardia; VF = ventricular fibrillation
P for interaction 0.002
P for trend <0·0001
P for trend 0·065
Similar results were seen when we examined survival to discharge of the overall population. Patients at hospitals in the quartile with the longest attempts had a 12% higher rate of survival to discharge compared with those at hospitals in the quartile with the shortest attempts (adjusted risk-ratio 1·12, [95% CI: 1·02–1·23]; p=0·0.021) (Table 3a). Furthermore, when we analyzed survival to discharge by presenting rhythm, the findings were significant for cardiac arrests due to PEA and asystole, but not for VT or VF (p for interaction effect <0·001) (Table 3c).
TABLE 3c.
Adjusted risk-ratios and rates for survival to discharge by hospital quartile: PEA/asystole and VT/VF*
| PEA/asystole*¶ | VT/VF** | |||||
|---|---|---|---|---|---|---|
| Total 64,339 patients at 435 hospitals |
Adjusted risk- ratio (95% CI) | Adjusted rate | P | Adjusted risk- ratio (95% CI) | Adjusted rate | P |
|
Quartile 1 13,994 patients at 113 hospitals Median: 16 minutes |
Ref | 10·2% | Ref | Ref | 32·1% | Ref |
|
Quartile 2 18,783 patients at 121 hospitals Median: 19 minutes |
1·06 (0·94–1·18) | 10·7% | 0·351 | 1·03 (0·96–1·11) | 33·2% | 0·399 |
|
Quartile 3 19,106 patients at 107 hospitals Median: 22 minutes |
1·09 (0·97–1·23) | 11·1% | 0·132 | 0·98 (0·90–1·06) | 31·4% | 0·570 |
|
Quartile 4 12,456 patients at 94 hospitals Median: 25 minutes |
1·20 (1·05–1·36) | 12·2% | 0·006 | 1·02 (0·93–1·12) | 32·8% | 0·662 |
PEA = pulseless electrical activity; VT = ventricular tachycardia; VF = ventricular fibrillation
P for interaction 0·002
P for trend 0·005
P for trend 0·886
Finally, we investigated whether the improved survival noted at hospitals with longer median durations of resuscitation attempts occurred at the expense of poorer neurological functioning among survivors at these hospitals at the time of discharge. Overall, we found that the proportion of patients surviving to discharge with a favourable neurological status (CPC ≤ 2) was not statistically different across hospital quartiles (82·0% for patients at hospitals in the quartile with the longest attempts versus 81·6% for those in the quartile with the shortest attempts; p=0·858).
DISCUSSION
Despite numerous advances in resuscitation care, overall survival after in-hospital cardiac arrest remains poor.22,23 Practitioners have been concerned about the tendency to prolong resuscitation efforts,4 although few empirical data are available to guide clinical practice. Our analysis found substantial variation across hospitals in the duration of resuscitation attempts. Importantly, we also discovered that patients at hospitals which averaged longer resuscitation attempts had a higher likelihood of achieving ROSC and survival to discharge, after accounting for differences in patients across hospitals. In fact, hospitals in the quartile with the longest resuscitation duration had, on average, more than 50% longer attempts than hospitals in the shortest quartile (25 minutes versus 16 minutes). While this may appear to be a modest suggestion on the surface, this amount of additional time has substantial implications in critically ill patients when one considers it as the time needed for re-evaluating clinical responses and providing additional treatments.
Investigators have published relatively few studies that examine the impact of resuscitation duration on clinical outcomes, and most of these studies have important limitations. One report by Ballew et al. found that in a series of 313 patients, the percentage of patients who survived to discharge was 45% when resuscitation duration lasted <5 minutes, and <5% when the resuscitation extended beyond 20 minutes.6 Another series found only a 2% survival if the resuscitation was continued beyond 10 minutes,9 while others have determined that resuscitation duration was an independent predictor of mortality both during and after the arrest.7 More recently, an analysis from a single-hospital registry in Taiwan suggested that the rate of achieving ROSC was >90% among patients resuscitated for less than 10 minutes but approximately 50% for those resuscitated for 30 minutes or more.24
Based upon this literature, experts have generally advocated for reassessing efforts when responses to treatment have not become apparent early on during resuscitation, and these recommendations may have broad influence in contemporary practice.3 While these findings indicate that longer resuscitation durations are clearly associated with worse survival, this interpretation in isolation may be misleading when trying to make inferences about the length of resuscitation attempts affect survival. First, these studies include survivors and non-survivors in their assessments of resuscitation duration. Including survivors in the determination of resuscitation duration shifts the distribution of resuscitation duration in the entire study population toward shorter time periods overall, and makes it less optimal as an explanatory variable, as ROSC typically occurs early on among most survivors. Second, it does not consider cumulative survival rates over time or examine the potential impact of extending resuscitation attempts. For example, in the paper by Ballew et al. discussed above, more than 50% of survivors were resuscitated for longer than 5 minutes and 10% were resuscitated for longer than 20 minutes. In the analysis from Taiwan, more than 30% of patients achieving ROSC did so only after 30 minutes of resuscitation. Finally, the earlier studies above typically represented a single hospital, and resuscitation duration may be influenced by local practices.
Our analysis addresses limitations of earlier studies and extends this body of work. It specifically takes advantage of potential differences in the local practice of resuscitation across hospitals. Our findings suggest that how long resuscitation efforts are continued prior to their termination varies substantially across hospitals. By looking at the distribution of resuscitation duration among survivors and non-survivors of cardiac arrest separately, we also confirmed that most survivors achieve ROSC early on during resuscitation but noted that a non-trivial number of survivors also require longer than 30 minutes prior to ROSC. This last observation is important because we also found that fewer than 25% of those who died during the cardiac arrest were resuscitated for at least 30 minutes, suggesting that attempts in most patients are rarely extended for this long.
Our most notable finding, however, was that longer attempts at resuscitation may be linked to higher rates of ROSC and survival to discharge. We found that patients at hospitals where longer attempts occurred had higher survival rates when compared with hospitals where attempts were shorter, independent of measured patient characteristics. This may be because hospitals that more reliably implement guidelines for resuscitation care systematically perform resuscitation attempts for longer, and this is the reason behind improved survival. However, the finding also suggests an opportunity for improving care in this high-risk population by standardizing the time required for continuing resuscitation attempts prior to decisions regarding termination of efforts.
So how may our results impact clinical practice? In one of the earliest studies of in-hospital cardiac arrest, Dr. Edward Stemmler noted that in 103 patients at his institution, the “duration of a single resuscitative attempt varied from a few minutes to almost 3 hours” with most attempts terminated when ROSC could not be established after a 15- to 30-minute trial.8 In the nearly 50 years that have intervened since this study, we unfortunately have not come much closer to determining when resuscitation should be terminated, after long enough efforts. In this context, our findings, utilizing patient and hospital level data from the largest representative sample of patients with in-hospital cardiac arrest in the United States, provide empiric evidence that there continues to be a wide variation in clinical practice and suggest standardized approaches to ensure resuscitation attempts occur for at least a minimum period of time could improve survival. Of course, we are unable to provide a specific cutoff from these data, and furthermore, are hesitant to do so. This aspect of care will always require clinical judgment as increasing the length of resuscitative measures must be always balanced against the potential downside of futile care. Yet, on the whole, it could be argued that extending resuscitation attempts by 10 or 15 minutes more will have marginal effects on resource utilization once efforts have already begun, but may improve outcomes. This will require further study.
A particularly noteworthy finding is that patients with PEA or asystole may derive the most benefit from longer attempts. Some literature has supported stopping resuscitative efforts if asystole has been present for more than 10 minutes without an identifiable and reversible cause,3 and that hospitalized patients who sustain an unwitnessed PEA or asystole arrest for more than 10 minutes are unlikely to survive.25 In our sample of in-hospital cardiac arrests, the likelihood of achieving ROSC and survival to discharge was significantly worse when the initial rhythm is PEA and asystole, compared with VT or VF. However, these patients also appear to be the most likely to benefit from longer resuscitation attempts, with an increase in ROSC from approximately 42% to 48% between hospitals in the shortest to longest quartiles. Those with VT or VF had a less pronounced effect. These findings may reflect the fact that survival among patients with VT or VF is frequently driven mostly by their immediate response to defibrillation, rather than other factors.
Our study should be interpreted with the following limitations in mind. While GWTG–R offers a unique opportunity to study resuscitation duration, it is a voluntary registry. Although our final study population consisted of 435 hospitals with broad regional representation from across the United States, these findings may not be representative of all hospitals, since participating hospitals tend to be larger. Second, the observational nature of this study means that we cannot directly demonstrate a causal relationship between longer resuscitation attempts and higher survival rates. It may be that factors related to better resuscitation care, such as more reliable implementation of guidelines, are associated with longer resuscitation attempts and improved survival. In this regard, unmeasurable variables that affect the duration of resuscitation—namely, the quality of chest compressions and code team performance—also may affect decision-making in regard to resuscitation care and outcomes, but are not collected in this registry adding to the potential for residual confounding.26,27 This also means that rates of survival to discharge may stem from hospital-specific administrative practices, such as discharge planning, following resuscitation. Third, as with any observational registry there remains the possibility that errors may occur during data collection or that there may be variation in how arrests are documented across hospitals. However, prior studies that have examined the overall accuracy of the GWTG–R through a random, re-auditing process suggest mean error rates are low overall at approximately 2·4%.10 Finally, we were unable to account for long-term outcomes in survivors of resuscitation, including functional status, after hospital discharge. The extent to which these critically ill patients benefit from survival months to years after their cardiac arrest should be the ultimate measure of the utility of resuscitation measures.
In summary, we found significant variation across hospitals in the duration of resuscitation attempts. Patients at hospitals with longer resuscitation durations had higher rates of ROSC and survival to discharge, particularly with PEA and asystole. Although the optimal resuscitation duration for any individual patient will continue to remain a bedside decision that relies on careful clinical judgment, hospitals may need to consider whether efforts to systematically increase their duration of resuscitation attempts prior to termination efforts may improve survival in these high-risk patients.
Supplementary Material
Acknowledgments
The American Heart Association provides operational funding for the GWTG–Resuscitation, and the final manuscript draft was approved by the American Heart Association’s Scientific Committee.
Funding:
Dr. Goldberger is a 2010–2012 Robert Wood Johnson Foundation Clinical Scholar. Dr. Chan is supported by a Career Development Grant Award (K23HL102224) from the National Heart, Lung, and Blood Institute.
Footnotes
Contributions:
ZDG, PSC, RAB, SLK, and BKN conceived and designed the study. BKN and PSC provided the overall supervision of the study. ZDG, PSC, and BKN drafted the report. All authors contributed to the statistical analysis and critical revision of the report, and have approved the final revision.
Conflicts of interest:
None of the authors have any conflicts of interest to disclose.
References
- 1.Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39:2401–6. doi: 10.1097/CCM.0b013e3182257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33:237–45. doi: 10.1007/s00134-006-0326-z. [DOI] [PubMed] [Google Scholar]
- 3.Eisenberg MS, Mengert TJ. Cardiac resuscitation. N Engl J Med. 2001;344:1304–13. doi: 10.1056/NEJM200104263441707. [DOI] [PubMed] [Google Scholar]
- 4.2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 5.Nolan JP, Soar J, Zideman DA, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation. 2010;81:1219–76. doi: 10.1016/j.resuscitation.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 6.Ballew KA, Philbrick JT, Caven DE, Schorling JB. Predictors of survival following in-hospital cardiopulmonary resuscitation. A moving target. Arch Intern Med. 1994;154:2426–32. [PubMed] [Google Scholar]
- 7.Bedell SE, Delbanco TL, Cook EF, Epstein FH. Survival after cardiopulmonary resuscitation in the hospital. N Engl J Med. 1983;309:569–76. doi: 10.1056/NEJM198309083091001. [DOI] [PubMed] [Google Scholar]
- 8.Stemmler EJ. Cardiac resuscitation. A 1-year study of patients resuscitated within a university hospital. Ann Intern Med. 1965;63:613–8. doi: 10.7326/0003-4819-63-4-613. [DOI] [PubMed] [Google Scholar]
- 9.Schultz SC, Cullinane DC, Pasquale MD, Magnant C, Evans SR. Predicting inhospital mortality during cardiopulmonary resuscitation. Resuscitation. 1996;33:13–7. doi: 10.1016/s0300-9572(96)00986-0. [DOI] [PubMed] [Google Scholar]
- 10.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 11.Chan PS, Krumholz HM, Spertus JA, et al. Automated external defibrillators and survival after in-hospital cardiac arrest. JAMA. 2010;304:2129–36. doi: 10.1001/jama.2010.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–97. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 13.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 14.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 15.Morrison LJ, Visentin LM, Kiss A, et al. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2006;355:478–87. doi: 10.1056/NEJMoa052620. [DOI] [PubMed] [Google Scholar]
- 16.Snijders TA, Rosker RJ. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. 2. Sage Publications Ltd; London: 2012. [Google Scholar]
- 17.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–3. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 18.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 19.Larkin GL, Copes WS, Nathanson BH, Kaye W. Pre-resuscitation factors associated with mortality in 49,130 cases of in-hospital cardiac arrest: a report from the National Registry for Cardiopulmonary Resuscitation. Resuscitation. 2010;81:302–11. doi: 10.1016/j.resuscitation.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 20.American Hospital Association. American Hospital Association Annual Survey Database for Fiscal Year 2009. Chicago American Hospital Association; 2009. http://www.ahadata.com/ahadata/html/AHASurvey.html. [Google Scholar]
- 21.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299:785–92. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 22.Tresch D, Heudebert G, Kutty K, Ohlert J, VanBeek K, Masi A. Cardiopulmonary resuscitation in elderly patients hospitalized in the 1990s: a favorable outcome. J Am Geriatr Soc. 1994;42:137–41. doi: 10.1111/j.1532-5415.1994.tb04940.x. [DOI] [PubMed] [Google Scholar]
- 23.Warner SC, Sharma TK. Outcome of cardiopulmonary resuscitation and predictors of resuscitation status in an urban community teaching hospital. Resuscitation. 1994;27:13–21. doi: 10.1016/0300-9572(94)90016-7. [DOI] [PubMed] [Google Scholar]
- 24.Shih CL, Lu TC, Jerng JS, et al. A web-based Utstein style registry system of in-hospital cardiopulmonary resuscitation in Taiwan. Resuscitation. 2007;72:394–403. doi: 10.1016/j.resuscitation.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 25.van Walraven C, Forster AJ, Stiell IG. Derivation of a clinical decision rule for the discontinuation of in-hospital cardiac arrest resuscitations. Arch Intern Med. 1999;159:129–34. doi: 10.1001/archinte.159.2.129. [DOI] [PubMed] [Google Scholar]
- 26.Jain R, Kuhn L, Repaskey W, et al. Physician implicit review to identify preventable errors during in-hospital cardiac arrest. Arch Intern Med. 2011;171:89–90. doi: 10.1001/archinternmed.2010.475. [DOI] [PubMed] [Google Scholar]
- 27.Jones PG, Miles JL. Overcoming barriers to in-hospital cardiac arrest documentation. Resuscitation. 2008;76:369–75. doi: 10.1016/j.resuscitation.2007.08.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.