Abstract
Objective
The description of the operation technique and retrospective review of 15 consecutive patients who were treated by posterior sacral dome resection and single-stage reduction with pedicle screw fixation for high-grade, high-dysplastic spondylolisthesis.
Materials and methods
All the patients had high-grade, high-dysplatic spondylolisthesis L5 and were treated by posterior sacral dome resection and posterior single-stage reduction from L4–S1. The average age at the time of surgery was 17.3 (11–28) years. The average follow-up time is 5.5 (2–11.6) years. Clinical and radiologica data were retrospectively reviewed.
Results
Spondylolisthesis was reduced from average 99% preoperative to 29% at the last follow-up. L5 incidence improved from 74° to 56°, the lumbosacral angle improved from 15° kyphosis to 6° lordosis, lumbar lordosis decreased from 69° to 53° from preoperative to the last follow-up. While pelvic incidence of 77° remained unchanged, sacral slope decreased from 51° to 46° and pelvic tilt increased from 25° to 30°. Clinical outcome was subjectively rated to be much better than before surgery by 14 out of 15 patients. Four out of 15 patients had temporary sensory impairment of the L5 nerve root which resolved completely within 12 weeks. There were no permanent neurological complications or no pseudarthrosis.
Conclusion
The sacral dome resection is a shortening osteotomy of the lumbosacral spine which allows a single-stage reduction of L5 without lengthening of lumbosacral region in high-grade spondylolisthesis, which helps to avoid neurological complications. This is a safe surgical technique resulting in a good multidimensional deformity correction and restoration of spino-pelvic alignment towards normal values with a satisfactory clinical outcome.
Keywords: High-grade spondylolisthesis, Sacral dome resection, Posterior reduction, Spino-pelvic alignment
Introduction
The treatment of high-grade spondylolisthesis remains controversial in terms of in situ fusion versus reduction. While satisfactory clinical outcome has been reported after in situ fusion [6, 14], this procedure is associated with higher rates of pseudarthrosis and slip progression [2]. Without reduction the lumbosacral alignment does not improve and the sagittal spinal imbalance, as well as the cosmetic deformity of the trunk remains. The aim of operation in such patients is to restore the spino-pelvic alignment and sagittal profile of the spine with a minimal neurological risk.
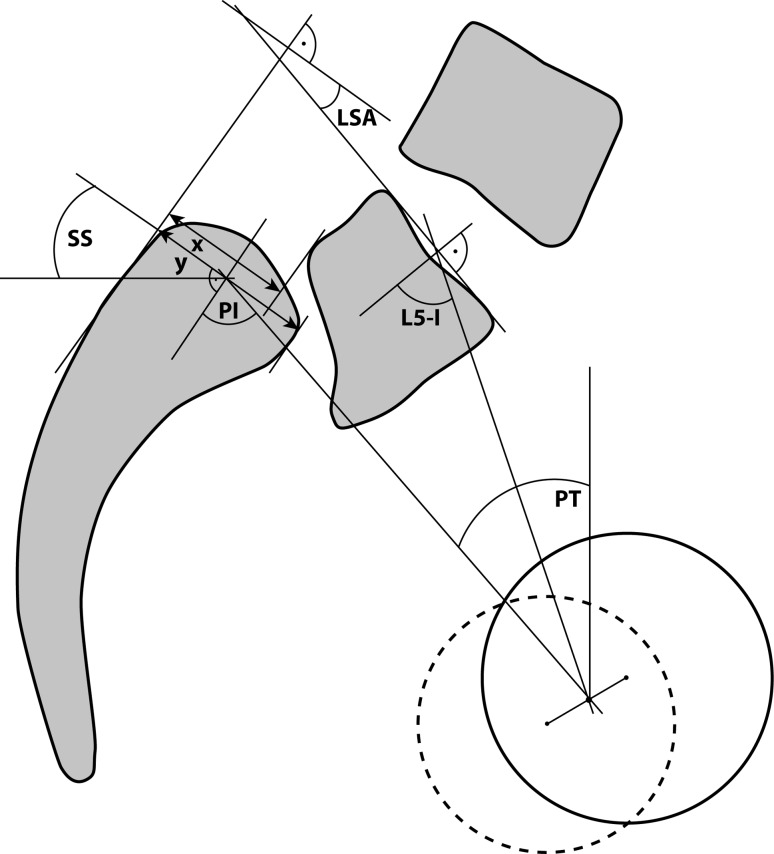
Reduction of the slipped L5 over S1 in high-grade spondylolisthesis places the L5 nerve root under tension which can lead to neurological complications [17, 19, and 20]. The reduction however restores the segmental lordosis, improves lumbosacral alignment and therefore the overall sagittal profile of the spine [12, 13]. Restoration of lumbosacral alignment is relevant for clinical and radiographic outcome and is determined by the lumbosacral angle (LSA), L5 incidence (L5I), percentage of slippage and lumbar lordosis [11, 12]. Spino-pelvic alignment is characterized by descriptors of pelvic orientation such as the pelvic tilt (PT) and the sacral slope (SS) which describe the spatial orientation of the pelvis in the sagittal plane. Pelvic incidence (PI) is the sum of sacral slope and pelvic tilt (PI = SS + PT) [5, 15]. Pelvic morphology and spino-pelvic alignment are abnormal in high-grade spondylolisthesis [8, 10]. While PI remains constant as a morphologic descriptor, surgical reduction of L5 over S1 can improve lumbosacral and spino-pelvic alignment as reflected by changes in PT and SS.
Patients and methods
15 consecutive patients who underwent surgery for high-grade spondylolisthesis L5 were retrospectively reviewed. The average age was 17.3 years which ranged from 11 to 28 years. Eight patients were females. Seven patients had spondyloptosis as defined by a slip of over 100%. The average amount of L5 slippage was 94% (53–150%). All the patients had radiological parameters of developmental high grade dysplasia in lumbosacral junction including trapezoid shaped L5 vertebra body, dome shaped sacrum [16]. Two patients had pars elongation and others had spondylolysis in isthmic region of L5. The indications for surgery were progressive spondylolisthesis to more than 50% in growing age, persistent back pain with L5 radicular symptoms and symptoms of cauda equina irritation in patients with high-grade spondylolisthesis.
Clinical outcome was subjectively graded by the patients at the last follow-up as much better, better, unchanged or worse compared to the preoperative state. Radiographic outcome was assessed by measuring spino-pelvic parameters which reportedly characterize spino-pelvic alignment and correspond to the outcome [11]. Follow-up examinations were performed after 3 months, 1 and 2 years and a final follow-up visit upon data collection. The average follow-up period was 5.5 (2.0–11.6) years.
Surgical technique
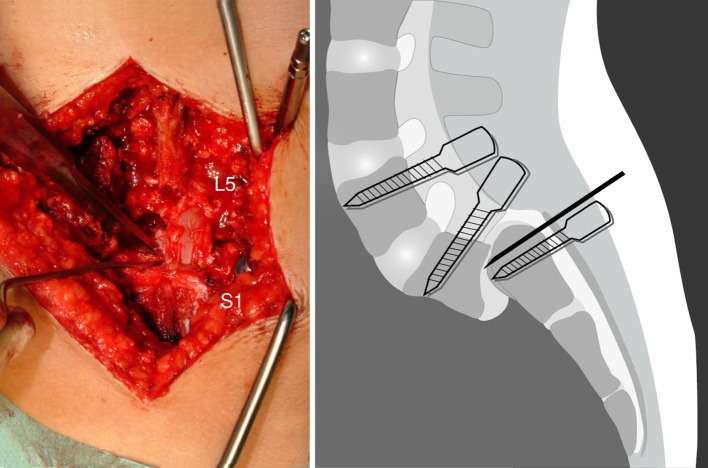
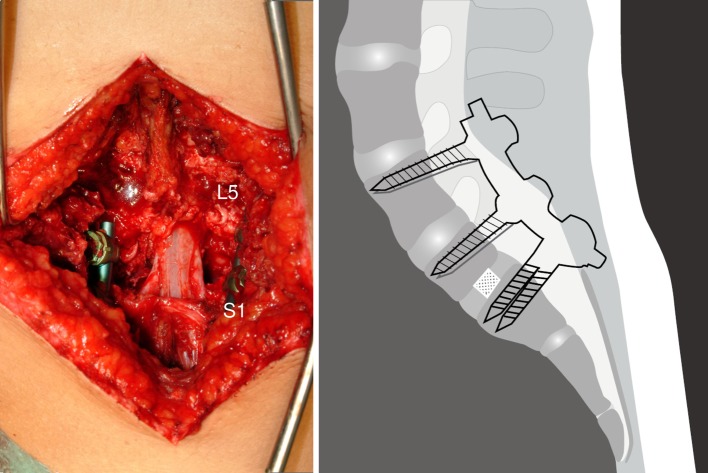
Intraoperative neuromonitoring using SEP and MEP is done routinely. L4–S2 is exposed from the midline. Pedicle screws are inserted in L4, L5 and S1. S1 pedicle screws are placed in a more caudal position to leave room for the sacral dome osteotomy and resection. All S1 pedicle screws are placed to the anterior cortex for bicortical purchase. Divergent screws in sacral wings at the level of S2 are used in addition to standard S1 pedicle screws when the surgeon feels that the screw hold in S1 is not strong enough. A complete removal of lamina L5, flavectomy L4/5 and L5/S1 are performed. L5 roots are thoroughly decompressed in the isthmus region by removing bony callus and granulation tissues of the spondylolysis. The L5 roots are exposed laterally until exiting from the foramen. If necessary the cranial part of the ala of sacrum is excised to release the L5 roots from tension completely. The annulus fibrosus in high-grade spondylolisthesis always has a bulging part in the foramen below the existing L5 roots. Special care is taken to remove this bulging part far laterally under the L5 roots. The L5/S1 disc is exposed bilaterally between the S1 and L5 roots and excised. The osteotomy of the sacral dome is performed from both sides in an antero-medial direction using ordinary straight osteotomes, after which the upper part of the sacrum together with attached disc fragments are removed piece by piece (Fig. 1). In some cases, the anterior lip of the lower plate of the L5 vertebra body needs to be osteotomised and excised through the disc space to remodel the trapezoid shape of L5 body. A lateral fluoroscopy or a lateral radiograph is helpful to make sure that the extent of the osteotomy is adequate. During this procedure, the segment L5/S1 gradually becomes mobile. The rods are contoured in lordosis and firmly fixed to the S1 screws first. The L4 and L5 screws are sequentially reduced to the fixed rods, reducing the slipped L5 on to the osteotomised surface of S1. Distraction or lengthening during this reduction procedure is avoided. L5 roots are continuously visualized to make sure that they are not stretched. When adequate amount of sacral dome is resected, the reduction is possible without lengthening of L4–S1 and without tension on the L5 roots. The amount of slip reduction is determined by the development of tension in the L5 roots. It is not necessary to aim for full reduction. Correction of the lumbosacral kyphosis and a good L5 nerve root decompression are more important than a full slip reduction. No forceful reduction is undertaken when the development of tension in L5 roots does not allow a full reduction. The sacral dome resection is a shortening osteotomy of the lumbosacral junction and any maneuver causing lengthening of the lumbosacral junction is avoided during the whole procedure. The space between the end plates of L5 and S1 is either supported by titanium mesh cages or iliac crest bone, depending on the amount of space available after the reduction. Titanium mesh cages are used if the space was high enough. If the space is very narrow, only bone grafts were inserted (Figs. 2, 3). Posterolateral intertransverse fusion L4–S1 is done using iliac crest bone. Ambulation of the patients began on the second postoperative day. No braces were worn.
Fig. 1.
Sacral dome osteotomy from posterior using ordinary straight osteotomes
Fig. 2.
Intraoperative photograph and drawing after the reduction
Fig. 3.
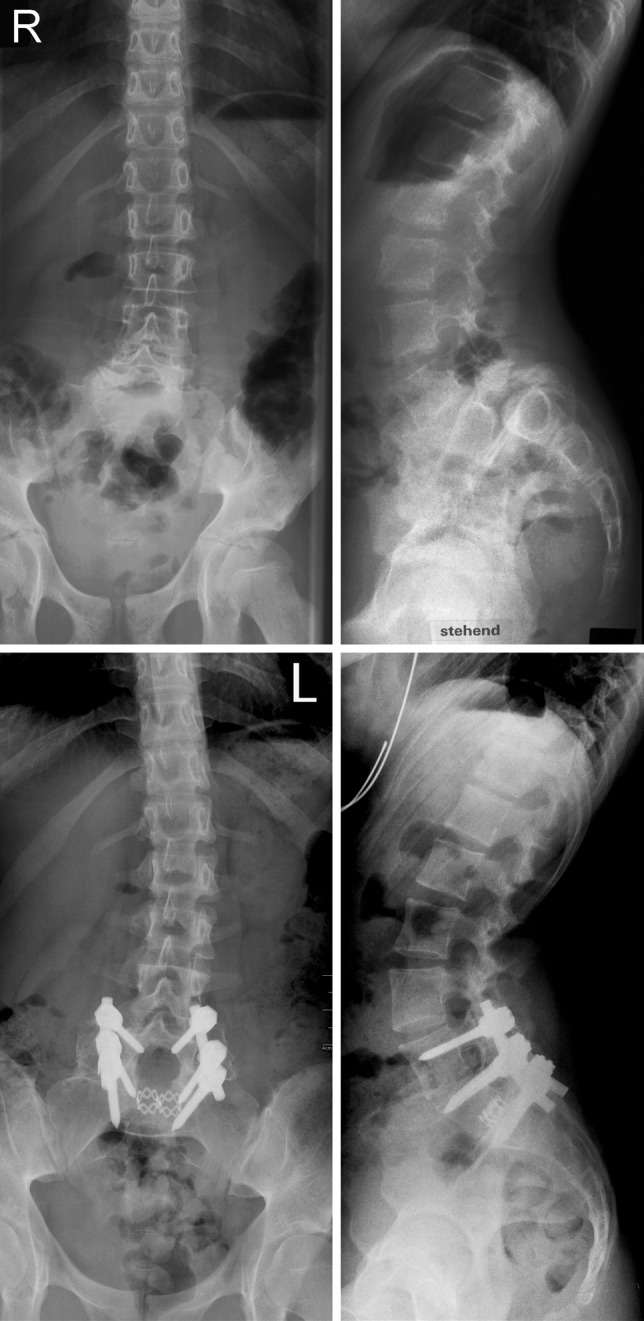
Radiographs preoperative and 5 years postoperative
Radiographic parameters (Fig. 4)
Fig. 4.
L5 Slip is x/y in percent, L5 incidence (L5-I), lumbosacral angle (LSA), pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS)
The severity of spondylolisthesis is measured as percentage of forward slip of L5 over S1. Lumbar lordosis (LL) is the Cobb angle from the superior endplates of L1–L5. L5 incidence (L5-I) is the angle between a perpendicular line to the L5 superior endplate and a line joining the center of the bicoxo-femoral axis and the center of the superior endplate of L5. The LSA or slip angle is the angle between the lines on the superior endplates of L5 and S1. Pelvic incidence is the angle between a line connecting the centre of the upper endplate of S1 to the bicoxo-femoral axis and a line perpendicular to the end plate of S1. Pelvic tilt is the angle between a vertical line and a line connecting the centre of the upper endplate of S1 to the bicoxo-femoral axis, and SS is the angle between a horizontal line and the endplate of S1.
Statistics
Due to the small number of patients, non-parametric statistics were employed using SPSS 16 for Mac. The Friedman test for related samples was used to analyze significant changes of radiographic parameters over the follow-up period. P values below 0.05 were considered to be significant.
Results
Clinical outcome
Since it is a retrospective study, we were not able to do the comparative analysis on subjective clinical outcome. The patients were asked at the last follow-up to grade the subjective result retrospectively as much better, better, unchanged or worse, compared to preoperative state. Fourteen out of 15 patients graded their subjective global outcome as much better, while one patient graded unchanged. The preoperative L5 radicular pain in 14 patients and the preoperative symptoms of caudal equine irritation in 2 patients resolved completely.
Radiographic outcome
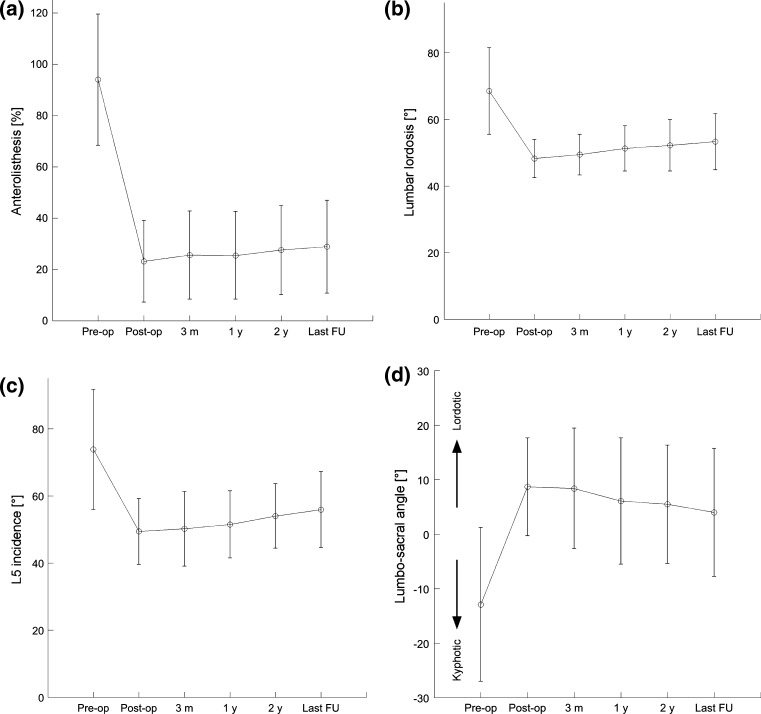
Fusion was observed in the radiographs in all patients after 1 year. The reduction of the L5 slip improved from preoperative 94.0 ± 25.6 to 23.2 ± 15.9% postoperatively, without any significant change at the last follow-up 25.3 ± 16.7% (p = 0.263) (Fig. 5a). Lumbar lordosis (LL) changed from preoperative 68.5 ± 13.0° to 48.2 ± 5.7° postoperatively and remained constant at the last follow-up 53.3 ± 8.4° (Fig. 5b). L5 incidence (L5-I) improved from 73.8 ± 17.9° to 49.4 ± 9.8° and did not change significantly at the last follow-up 55.9 ± 11.3° (p = 0.241) (Fig. 5c). The LSA changed from preoperative −14.9 ± 14.1°, indicating a kyphotic deformity, to postoperative 6.1 ± 5.0°, demonstrating a restoration of lumbosacral lordosis, and remained unchanged to the last follow-up 5.5 ± 7.3° (p = 0.051) (Fig. 5d).
Fig. 5.
The changes in lumbosacral parameters. a Slip percent b Lumbar lordosis c L5 incidence d Lumbosacral angle
The preoperative PI was 76.6 ± 5.3°, PT was 25.0 ± 8.4° and SS was 50.8 ± 8.4° in average. According to the classification of high-grade spondylolisthesis by Hresko et al. [9], all 15 patients exhibited a balanced pelvic version which was determined by using the formula they provided in the publication. Pelvic incidence did not change from pre-operative 76.6 ± 5.3° to last follow-up 75.8 ± 6.7°. Sacral slope decreased slightly, but significantly from pre-operative 50.8 ± 8.4° to postoperative 46.2 ± 8.5° (p = 0.036) and remained constant to the last follow-up 47.5 ± 12.9°. In accordance with the interdependence of SS and PT as defined by PI = PT + SS, PT increased significantly from 25.0 ± 8.4° to 29.6 ± 8.5° (p = 0.036) and remained unchanged to the last follow up 28.3 ± 12.6°.
Complications
Intraoperative neuromonitoring was uneventful without any significant changes in anterior tibial and extensor hallucis longus muscles in all patients. Postoperative L5 sensory impairment developed in 4 out of 15 patients. All of these sensory symptoms appeared on the first postoperative day and resolved after 12 weeks. There were no permanent neurological injury, pseudarthrosis and no implant failures.
Discussion
This is a retrospective review of 15 adolescents and young adults with high-grade high dysplastic spondylolisthesis treated by sacral dome resection and single stage reduction from posterior approach. The surgical technique is described and the radiological and clinical results are reported.
The best way to treat a high-grade high dysplastic spondylolisthesis is to correct the multidirectional deformity of lumbosacral junction with minimal neurological risks. Even though there are conflicting reports about the in situ fusion for high-grade isthmic spondylolisthesis [14, 18], the instrumented fusion with reduction has a clear advantage like facilitation of full nerve decompression, promotion of bony union, restoration of body posture and mechanics, as well as improvement of appearance. The reduction procedure is known to be associated with neurological complications [17, 19, 20, 22]. There are various descriptions of reduction from posterior alone or anterior posterior combined procedures [1–3]. The aim of the surgery is to decompress the spinal canal and nerve roots, as well as to improve the lumbosacral deformity. The reduction of a severely slipped L5 is usually associated with elongation of the lumbosacral junction. Bohlman and Cook [1] first described the removal of the upper corner of the S1 vertebral body to decompress the nerve roots in a surgical procedure where the reduction was not undertaken. Gaines and Nichols [7] described an extensive anteroposterior procedure for L5 vertebrectomy and reduction from L4 on to S1 in the treatment of spondyloptosis, which was a procedure of shortening of the lumbosacral junction. We believe that avoidance of elongation in the lumbosacral junction is one of the key components to reduce neurological complications. In our present technique, the sacral dome is excised from posterior approach to produce shortening in this region. In addition to this, the sacral dome resection results in complete mobilization of the L5/S1 segment, facilitates complete L5 nerve root release laterally. We did not have any permanent neurological complications and all the preoperative neurological symptoms regressed. We made sure that the L5 roots were free and as tensionless as possible after the reduction. The secondary development of L5 sensory symptoms on the first postoperative day was observed in 4 patients despite uneventful neuromonitoring. This was probably due to the reaction of L5 roots to manipulation and tension and these symptoms were temporary.
Shufflebarger et al [21] described a technique of posterior reduction using temporary distraction from upper lumbar spine to sacrum to assist in reduction and then fusing monosegmentally L5/S1. Progression of slip angle and sacral bending were seen in their series. We believe that instrumented fusion from L4 to S1 has advantages over monosegmental L5/S1 fusion. Firstly, screw purchase in severely dysplastic L5 pedicles may be weak and unreliable and secondly, the L4/5 facet joints are usually abnormal in severely dysplastic high-grade spondylolisthesis. We recommend an instrumented fusion from L4 to S1 to avoid loss of correction and sacral bending, as well as development of spondylolisthesis of L4. Sacral dome excision and reduction produce ample bony surfaces between the bodies of L5 and S1 for anterior column fusion. In L5/S1 segment, the interbody fusion is important as the transverse processes of L5 in these patients are frequentyl too small for a reliable posterolateral fusion alone. Posterolateral fusion is done between the transverse processes of L4–S1. Some authors tried to achieve anterior column fusion in L5/S1 by means of additional anterior fusion [4]. With our present technique, we were able to achieve good anterior column fusion without an additional anterior procedure. As retrograde ejaculation is a known complication of the anterior approach to L5–S1, this is a significant advantage of the present technique.
We agree with Labelle et al [11] that the key to a successful clinical outcome is to reduce L5 over S1. A significant improvement of sagittal lumbosacral alignment is achieved in our series. The L5 incidence changed from 74° to 56°, there was restoration of lumbosacral lordorsis from 15° kyphosis to 6° lordosis, which in turn improved the preoperative lumbar hyperlordosis. Restoration of lumbosacral alignment not only resulted in a reduction of lumbar lordosis but also in a less anteversion of the pelvis as indicated by the increased PT.
Only one report has focused on the global lumbosacral or spino-pelvic alignment after surgical reduction of high-grade spondylolisthesis to our knowledge [12]. Labelle et al correlated radiologic measurements with clinical outcome after surgery. They retrospectively reviewed 73 patients recruited from 10 Institutions. Sixty-two patients were treated by a one-stage posterior surgical procedure and in 55 patients, instrumentation was carried out from L4 to S1. Thirty two patients exhibited a balanced pelvis with high SS/low PT according to Hresko et al. [9], which showed a slight improvement in terms of reduction of SS and an increase in PT. This is in accordance with our findings. In our series, none of the patients exhibited an unbalanced pelvis. Small but significant changes in SS and PT were observed in patients with balanced pelvis. While results of surgical reduction in patients with a balanced pelvis may seem less dramatic than with an unbalanced pelvis, they nevertheless indicate a favorable improvement towards more normal values and reduction of the excessive lumbar lordosis after the operation.
The posterior alone approach with shortening sacral dome resection, single-stage reduction and pedicle-screw fixation from L4 to S1 allowed the restoration of spino-pelvic alignment towards more physiological values, with minimal risks for neurological injury. Fusion was observed in all cases after 1 year and radiographic parameters remained unchanged throughout the follow-up period. There was neither loss of correction nor bending of the sacrum. All but one patient retrospectively reported their outcome to be “much better” than before the surgery.
We conclude that sacral dome resection from posterior approach in high-grade spondylolisthesis is a shortening osteotomy of the lumbosacral junction. It is very useful for single-stage posterior reduction of L5–S1 with the use of pedicle screws avoiding lengthening of lumbosacral junction and avoiding additional anterior surgery. This procedure followed by the instrumented fusion of L4–S1 produces a good multidimensional deformity correction with a minimal risk of neurological injury and a satisfactory clinical outcome. This is a safe surgical procedure to restore spino-pelvic alignment and the sagittal profile of the spine in the treatment of high-grade high dysplastic spondylolisthesis.
Conflict of interest
None.
References
- 1.Bohlman HH, Cook SS. One-stage decompression and posterolateral and interbody fusion for lumbosacral spondyloptosis through a posterior approach. Report of two cases. J Bone Joint Surg Am. 1982;64(3):415–418. [PubMed] [Google Scholar]
- 2.Bradford DS, Gotfried Y. Staged salvage reconstruction of grade-iv and v spondylolisthesis. J Bone Joint Surg Am. 1987;69(2):191–202. [PubMed] [Google Scholar]
- 3.Bradford DS, Boachie-Adjei O. Treatment of severe spondylolisthesis by anterior and posterior reduction and stabilization. A long-term follow-up study. J Bone Joint Surg Am. 1990;72(7):1060–1066. [PubMed] [Google Scholar]
- 4.DeWald RL, Faut MM, Taddonio RF, Neuwirth MG. Severe lumbosacral spondylolisthesis in adolescents and children. Reduction and staged circumferential fusion. J Bone Joint Surg Am. 1981;63(4):619–626. [PubMed] [Google Scholar]
- 5.Duval-Beaupere G, Schmidt C, Cosson P. A barycentremetric study of the sagittal shape of spine and pelvis: The conditions required for an economic standing position. Ann Biomed Eng. 1992;20(4):451–462. doi: 10.1007/BF02368136. [DOI] [PubMed] [Google Scholar]
- 6.Frennered AK, Danielson BI, Nachemson AL, Nordwall AB. Midterm follow-up of young patients fused in situ for spondylolisthesis. Spine (Phila Pa 1976) 1991;16(4):409–416. doi: 10.1097/00007632-199104000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Gaines RW, Nichols WK. Treatment of spondyloptosis by two stage l5 vertebrectomy and reduction of l4 onto s1. Spine (Phila Pa 1976) 1985;10(7):680–686. doi: 10.1097/00007632-198509000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Hanson DS, Bridwell KH, Rhee JM, Lenke LG. Correlation of pelvic incidence with low- and high-grade isthmic spondylolisthesis. Spine (Phila Pa 1976) 2002;27(18):2026–2029. doi: 10.1097/00007632-200209150-00011. [DOI] [PubMed] [Google Scholar]
- 9.Hresko MT, Labelle H, Roussouly P, Berthonnaud E. Classification of high-grade spondylolistheses based on pelvic version and spine balance: Possible rationale for reduction. Spine (Phila Pa 1976) 2007;32(20):2208–2213. doi: 10.1097/BRS.0b013e31814b2cee. [DOI] [PubMed] [Google Scholar]
- 10.Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Chopin D, Hresko T, Dimnet J. Spondylolisthesis, pelvic incidence, and spinopelvic balance: A correlation study. Spine (Phila Pa 1976) 2004;29(18):2049–2054. doi: 10.1097/01.brs.0000138279.53439.cc. [DOI] [PubMed] [Google Scholar]
- 11.Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O’Brien M. The importance of spino-pelvic balance in l5–s1 developmental spondylolisthesis: A review of pertinent radiologic measurements. Spine (Phila Pa 1976) 2005;30(6 Suppl):S27–S34. doi: 10.1097/01.brs.0000155560.92580.90. [DOI] [PubMed] [Google Scholar]
- 12.Labelle H, Roussouly P, Chopin D, Berthonnaud E, Hresko T, O’Brien M. Spino-pelvic alignment after surgical correction for developmental spondylolisthesis. Eur Spine J. 2008;17(9):1170–1176. doi: 10.1007/s00586-008-0713-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lamartina C, Zavatsky JM, Petruzzi M, Specchia N. Novel concepts in the evaluation and treatment of high-dysplastic spondylolisthesis. Eur Spine J. 2009;18(Suppl 1):133–142. doi: 10.1007/s00586-009-0984-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lamberg T, Remes V, Helenius I, Schlenzka D, Seitsalo S, Poussa M. Uninstrumented in situ fusion for high-grade childhood and adolescent isthmic spondylolisthesis: Long-term outcome. J Bone Joint Surg Am. 2007;89(3):512–518. doi: 10.2106/JBJS.E.00545. [DOI] [PubMed] [Google Scholar]
- 15.Legaye J, Duval-Beaupere G, Hecquet J, Marty C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marchetti PG, Bartolozzi P (1997) Classification of spondylolisthesis as a guideline for treatment. In: Bridwell KH, DeWald RL (eds) The textbook of spinal surgery. 2nd edn. Lippincott-Raven Philadelphia, pp 1211–1254
- 17.Muschik M, Zippel H, Perka C. Surgical management of severe spondylolisthesis in children and adolescents. Anterior fusion in situ versus anterior spondylodesis with posterior transpedicular instrumentation and reduction. Spine (Phila Pa 1976) 1997;22(17):2036–2042. doi: 10.1097/00007632-199709010-00020. [DOI] [PubMed] [Google Scholar]
- 18.Newton PO, Johnston CE., 2nd Analysis and treatment of poor outcomes following in situ arthrodesis in adolescent spondylolisthesis. J Pediatr Orthop. 1997;17(6):754–761. doi: 10.1097/00004694-199711000-00010. [DOI] [PubMed] [Google Scholar]
- 19.O’Brien JP, Mehdian H, Jaffray D. Reduction of severe lumbosacral spondylolisthesis. A report of 22 cases with a ten-year follow-up period. Clin Orthop Relat Res. 1994;300:64–69. [PubMed] [Google Scholar]
- 20.Petraco DM, Spivak JM, Cappadona JG, Kummer FJ, Neuwirth MG. An anatomic evaluation of l5 nerve stretch in spondylolisthesis reduction. Spine (Phila Pa 1976) 1996;21(10):1133–1138. doi: 10.1097/00007632-199605150-00002. [DOI] [PubMed] [Google Scholar]
- 21.Shufflebarger HL, Geck MJ. High-grade isthmic dysplastic spondylolisthesis: Monosegmental surgical treatment. Spine (Phila Pa 1976) 2005;30(6 Suppl):S42–S48. doi: 10.1097/01.brs.0000155583.55856.f9. [DOI] [PubMed] [Google Scholar]
- 22.Smith MD, Bohlman HH. Spondylolisthesis treated by a single-stage operation combining decompression with in situ posterolateral and anterior fusion. An analysis of eleven patients who had long-term follow-up. J Bone Joint Surg Am. 1990;72(3):415–421. [PubMed] [Google Scholar]