Abstract
Background
The purpose of the study was to report radiological outcomes after total disc replacement (TDR) in the cervical spine through a 24 months follow-up (FU) prospective study with a special focus on sagittal alignment and kinematics at instrumented and adjacent levels.
Materials and methods
Thirty-two patients, who sustained one-level TDR with a ball-and-socket arthroplasty (Discocerv™ implant, Scient’x/Alphatec Spine, USA) were consecutively included in the study. Clinical (visual analogical scale and neck disability index) and radiological parameters were measured preoperatively and postoperatively at 3/6 months, 1-year and 2-year FU. Sagittal alignment, ranges of motion (ROM) and center of rotations (CORs) were analyzed using specific motion analysis software (Spineview™, Paris, France). Patients CORs were compared with those of a control group of 39 normal and asymptomatic subjects.
Results
Both local and C3–C7 lordosis significantly increased postoperatively (+8° and +13° at 2 years, respectively). At instrumented level ROM in flexion–extension (FE) was measured to 10.2° preoperatively versus 7.5° at 1 year and 6.1° at 2 years. There were no differences in ROM at adjacent levels between pre and postoperative assessments. When compared with control group and preoperative measurements, we noted postoperative cranial shift of the COR at instrumented level for patients group. In contrast, there was no difference in CORs location at adjacent levels.
Conclusion
Through this prospective study, we observed that cervical lordosis consistently increased after TDR. In addition, although ball-and-socket arthroplasty did not fully restore native segmental kinematics with significant reduction of motion in FE and consistent cranial shift of the COR, no significant changes in terms of ROM and CORs were observed at adjacent levels.
Keywords: Biomechanics, Kinematics, Cervical spine, Cervical disc prosthesis, Artificial disc, Mobility
Introduction
Anterior cervical discectomy and fusion (ACDF) is traditionally the gold standard to manage cervical degenerative disc disease with radicular pain refractory to conservative treatment. However, ACDF can potentially result in iatrogenic effects such as pseudarthrosis and early adjacent degenerative level by increase of stresses at adjacent levels [1–4]. Experimental studies demonstrated that fusion could generate increase in mechanical forces with hypermobility and increase in intradiscal pressure on adjacent discs above and below the intervertebral segment fused, and thus may explain the mechanism of early adjacent disc degeneration [5–9].
By preserving some amount of motion and reproducing more closely physiologic kinematics of cervical spine, total disc replacement (TDR) may avoid report of stresses on adjacent discs and thus potentially reduce the incidence of adjacent segment disease [10]. Several studies evaluated preservation of motion at instrumented level comparing pre versus postoperative segmental range of motion (ROM) in flexion–extension (FE) [11–17] and confirmed that ROM was generally maintained after TDR ranging from 5° to 10°.
Restoring physiological cervical spine kinematics involves restoring not only the amount of motion, but also the nature of the motion, however, most clinical studies focused on the amount of motion after cervical arthroplasty [11–17]. The quality of motion can be clinically evaluated by measuring the mean center of rotation (COR) on dynamic X-rays. Only few studies investigated changes in COR after cervical TDR [12, 18, 19]. In fact, the quality of motion restored in vivo and its consequences on adjacent kinematics after cervical arthroplasty is largely unknown. To our knowledge, no previous study investigated changes in COR at adjacent levels after ball-and-socket arthroplasty in the cervical spine.
Otherwise, the capacity of TDR to restore sagittal alignment is still under investigation [12, 14].
Thus, to contribute to a better understanding of the in vivo biomechanical behavior of TDR in the cervical spine, our objective in the current study was to report clinical and radiological outcomes after cervical disc arthroplasty using ball-and-socket design. Radiological assessment included sagittal alignment and kinematics analysis (ROM and COR) in the sagittal plane at the treated and also adjacent levels using a computer-assisted method.
Materials and methods
Study design
From January 2006 to June 2008, 32 patients who underwent single-level cervical TDR (Discocerv™, Scient’x/Alphatec Spine Inc., Carlsbad, CA, USA) were prospectively and consecutively included in the study. All patients had a minimal follow-up (FU) of 24 months (mean 37.6 ± 10.2). Indication for surgery was cervical radiculopathy secondary to soft disc herniation with no (n = 27/32) or minimal osteophytes (n = 5/32), with or without neurological deficit and pain resistant to medical treatment for more than 3 months.
Patients with pluri-segmental disease, severe facet and/or disk arthrosis, previous cervical spine surgery, traumatic or tumoral disease, severe metabolic bone disease, instability and/or osteoporosis were excluded from the study.
Patients’ demographic data are summarized in Table 1.
Table 1.
Patients characteristics (n = 32) and surgery data
| Mean | SD | Min | Max | |
|---|---|---|---|---|
| Age (years) | 42.3 | 8.9 | 27 | 65 |
| Body mass index (kg/m²) | 24.7 | 5.5 | 18.1 | 35.6 |
| Gender | 14 men, 18 women | – | – | – |
| Follow-up (months) | 37.6 | 10.2 | 24 | 58 |
| Surgery duration (min) | 65.6 | 20.6 | 35 | 118 |
| Blood loss (ml) | 67.5 | 77.5 | 0 | 250 |
| Hospital stay (days) | 5.1 | 1.6 | 2 | 9 |
| Reoperation (s) | – | – | – | – |
Surgical technique and postoperative course
After standard anterior approach to the cervical spine under general anesthesia, intervertebral disc was removed while preserving the vertebral endplate cortical bone. Moderate intervertebral distraction using Cloward distractor allowed for disc herniation removal and neuro-foraminal decompression. The posterior longitudinal ligament was only partially removed on the symptomatic side. The implant was then placed with the aim of an optimal sizing and position in both frontal and anteroposterior planes. In the sagittal plane, the aim was to obtain maximal contact between vertebral and prosthetic endplates. If the prosthesis was not strictly in a median place, it was placed again. The height of the implant was determined analyzing the intervertebral height of normal adjacent discs on preoperative radiographs and adapted per-operatively according to the distraction effect observed during implant positioning. The position of the implant could be checked using frontal anteroposterior and lateral fluoroscopic controls during surgical procedure.
Patients were prescribed non-steroidal anti-inflammatory medication for 2 weeks after surgery, but no cervical collar.
Implant
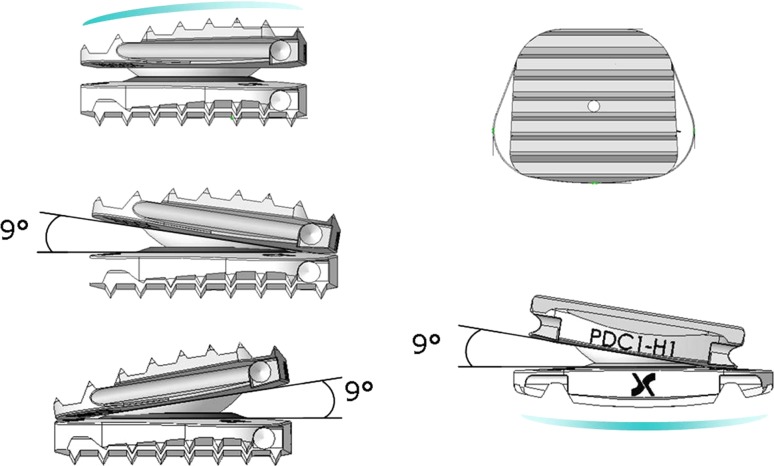
The implant consists of a constrained device with ball-and-socket joint and cranial geometric center (Fig. 1). It uses a combination of pure titanium and titanium alloy for endplates and ceramic-on-ceramic bearing surfaces. Titanium endplates are designed with an anatomical profile characterized by convexity in the sagittal plane for the upper plate and convexity in the frontal plane for the lower plate. Two footprints are available, one 13 × 17 mm and the other 15 × 20 mm; the height ranges from 5 to 8 mm. Finally, in the superior endplate lordotic correction is around 5°.
Fig. 1.
The Discocerv™ device consists of a ball-and socket joint with cranial geometric centre allowing for 18° of ROM in flexion–extension and lateral bending and with no theoretical limitation in axial rotation. The convex part of the articulating joint is located on the superior endplate of the prosthesis
Clinical evaluation
Clinical and radiographical evaluation was performed preoperatively and postoperatively between 3 and 6 months (early FU), at 1 year (M12) and 2 years (M24).
Clinical evaluation included surgery data (operative time and blood loss), complication rates, cervical and radicular visual analogical scale (VAS) and neck disability index (NDI). A patient satisfaction index (PSI) was also obtained postoperatively (Table 2). As recommended by the FDA, we considered the success as an improvement of NDI at 2 years FU equal or superior to 15%. Absolute improvement of clinical scores (NDI and VAS) was defined as follows: M24score–Preopscore.
Table 2.
Patient satisfaction index
| Patient responses | PSI score |
|---|---|
| Surgery met my expectations | 1 |
| Surgery improved my condition enough so that I would go through it again for the same outcome | 2 |
| Surgery helped me but I would not go through it again for the same outcome | 3 |
| I am the same or worse compared to before surgery | 4 |
Radiographical assessment
All radiographical parameters were calculated using quantitative motion analysis specific software (Spineview™ Software, Arts et Metiers ParisTech, Paris, France) which has already been validated [20].
Sagittal alignment
Sagittal alignment was evaluated on lateral X-rays in neutral position by measuring the following parameters (Fig. 2):
C1–C7 lordosis between the line joining the superior edge of the anterior and posterior arches of C1 and the inferior endplate of C7
C3–C7 lordosis between the superior endplate of C3 and the inferior endplate of C7
Discal lordosis between the inferior endplate of the upper vertebra and the superior endplate of the lower vertebra
Local lordosis between the superior endplate of the upper vertebra and the inferior endplate of the lower vertebra
Anterior disc height expressed in percentage and defined as the ratio between the height of the anterior disc space and that of the anterior wall of the upper vertebra
Posterior disc height expressed in percentage and defined as the ratio between the height of the posterior disc space and that of the posterior wall of the upper vertebra.
Fig. 2.
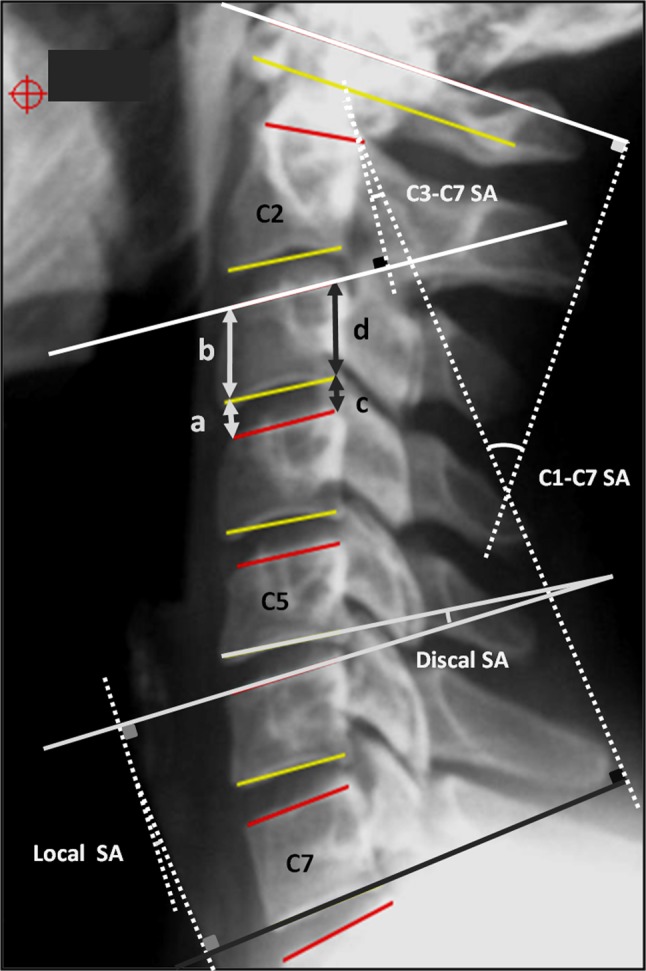
Evaluation of sagittal alignment included measurements of discal, local, C3–C7 and C1–C7 sagittal angles (SA). Anterior and posterior disc height were also calculated on neutral lateral view using a ratio between discal and upper vertebral body heights (a/b and c/d, respectively). SA sagittal angle
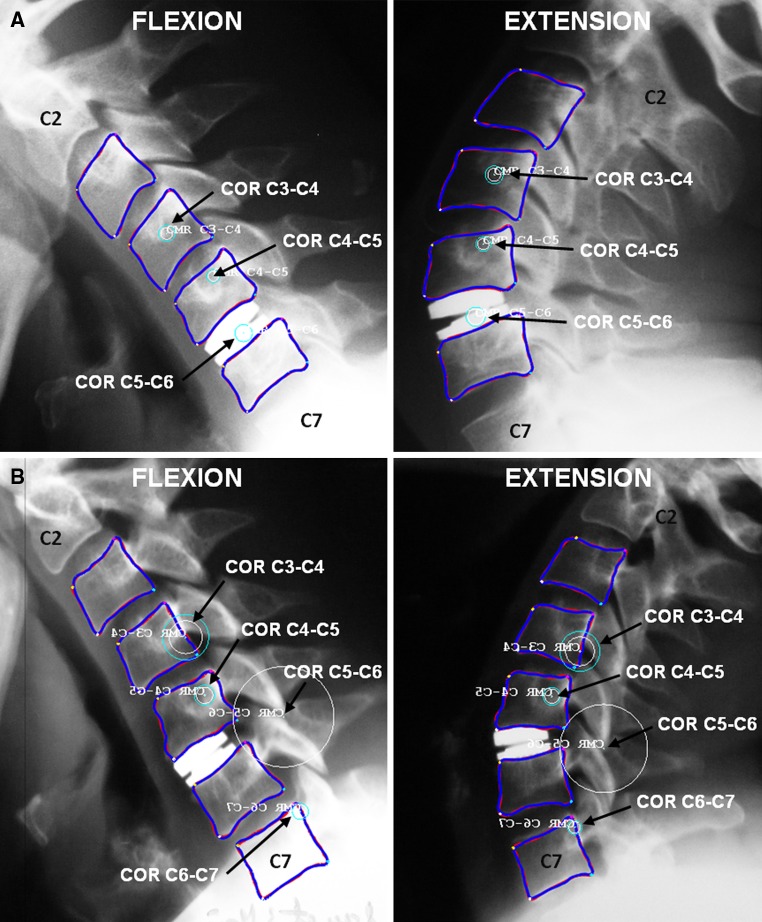
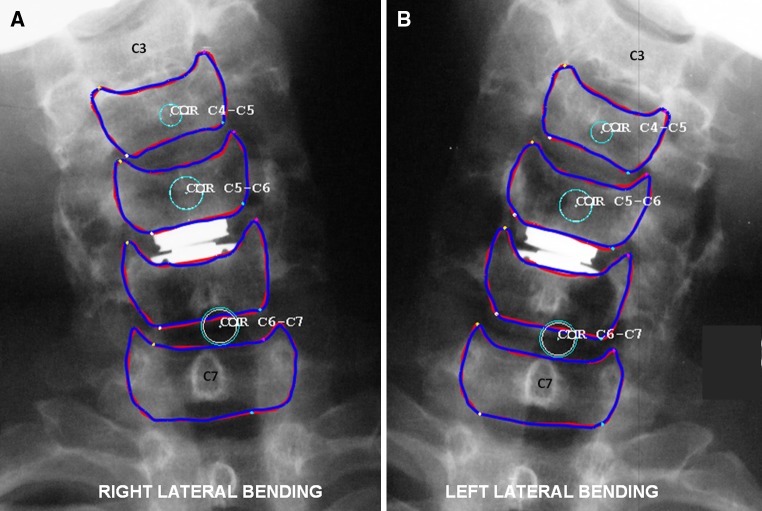
Sagittal kinematics
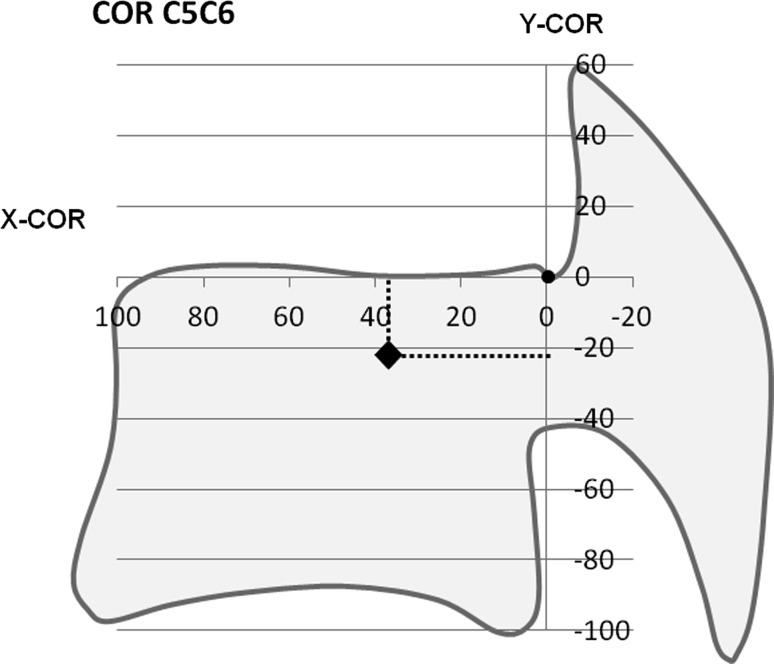
Kinematics analysis included ROM in FE and position of the mean center of rotation (COR) at instrumented and adjacent levels. Measurements were realized on digitized dynamic lateral X-rays in flexion and extension postures. Mean CORs were calculated only when mobility in FE was equal or superior to 3°. The location of COR was calculated using (X, Y) coordinates system (Fig. 3). The postero-superior corner of the lower vertebra was considered as the origin of the (X, Y) 2D landmark, the X axis was directed forward along the superior endplate of the lower vertebral body and the Y axis was directed upward perpendicular to the X axis. COR-X is positive in the anterior direction and COR-Y is positive in the cranial direction. The coordinates (X, Y) of the COR were normalized as percentages based on the length and height of the lower vertebra. Coordinates of patients CORs were then compared pre and postoperatively with those of a control group composed of 39 normal and asymptomatic subjects with a mean age of 35 years old (from 21 to 40). Characteristics of the control group have already been reported in a previous work published by our institution [18].
Fig. 3.
The location of COR was calculated using (X, Y) coordinates system with the postero-superior corner of the lower vertebra considered as the origin of the (X, Y) 2D landmark. The X axis was directed forward along the superior endplate of the lower vertebral body and the Y axis was directed upward perpendicular to the X axis. The coordinates (X, Y) of the COR were normalized as percentages based on the length and height of the lower vertebra. In this example, we illustrated the C6 vertebral body; the X and Y coordinates of COR were measured to +36 and −22, respectively
The impact of patient age, preoperative mobility and preoperative instrumented disc height on sagittal kinematics was also analyzed.
Statistical analysis
The statistical analysis was performed using specific software (XLSTAT™ Software, Addinsoft SARL, Paris, France). For each clinical and radiographical parameter, comparative statistical analysis between pre and postoperative values was carried out using paired-samples Wilcoxon’s test. A simple linear regression analysis was conducted to assess the impact of patient age, preoperative mobility and preoperative instrumented disc height on postoperative ROM. When concerning CORs, independent samples Mann–Whitney test was used to compare patients versus control group. All P values were considered statistically significant for a P < 0.05.
Results
There were 18 women and 14 men included in the study with a mean age of 42.3 ± 8.9 years old. The levels involved were C4–C5, C5–C6 and C6–C7 in 1, 24 and 7 cases, i.e. 3, 75 and 22% of cases, respectively. Only patients with one-level TDR were included in the study.
The mean operative time, blood loss and hospital stay duration are presented in Table 1. Concerning postoperative complications, we noted transient dysphagia in two cases and superficial wound infection in one case, but without necessitating reoperation. No mechanical complication such as implant failure, migration or vertebral body fracture was observed, however we noted six cases of heterotopic ossifications at 2 years FU (n = 6/32, 18.8% of cases).
Clinical outcomes
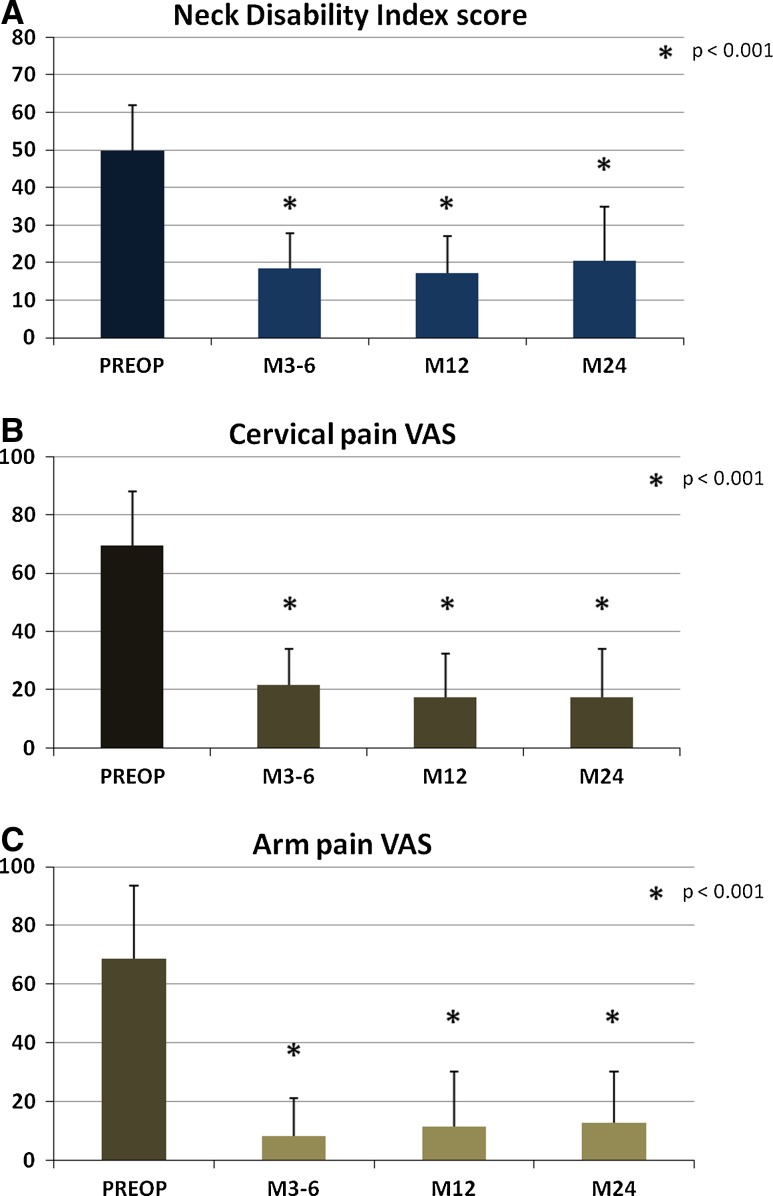
NDI was 49.7 ± 12.2 [18–78] preoperatively versus 18.5 ± 9.4 [2–38] at early postoperative FU, P < 0.001, versus 17.2 ± 9.8 [4–36] at M12, P < 0.001, and versus 20.7 ± 14.1 [0–52] at M24, P < 0.001, Fig. 4a. The absolute improvement at 2 years averaged 29 and success criteria (defined as improvement of NDI equal or superior to 15% at 2 years) was observed for 85.7% of patients (n = 24/28).
Fig. 4.
Mean NDI (a), cervical (b) and arm pain (c) VAS scores at preoperative, M3–6, M12 and M24 assessments. Statistical differences between pre and postoperative scores are mentioned on each graph
Cervical and radicular VAS significantly reduced from 69.6 ± 18.5 [25–95] and 69.3 ± 24.7 [10–100] preoperatively to 21.6 ± 12.3 [0–63] and 8 ± 12.7 [0–50] at early FU, to 17.4 ± 15.1 [0–60] and 11 ± 18.5 [0–70] at M12 and to 17.3 ± 16.6 [0–60] and 12.8 ± 17.5 [0–67] at M24, respectively, Fig. 4b, c. All the differences were statistically significant with P < 0.001.
Patients satisfaction index at 2 years was 1 in 80% (n = 24/30), 2 in 20% (n = 6/30) and 3 in 3.3% (n = 1/30) of cases.
Sagittal alignment
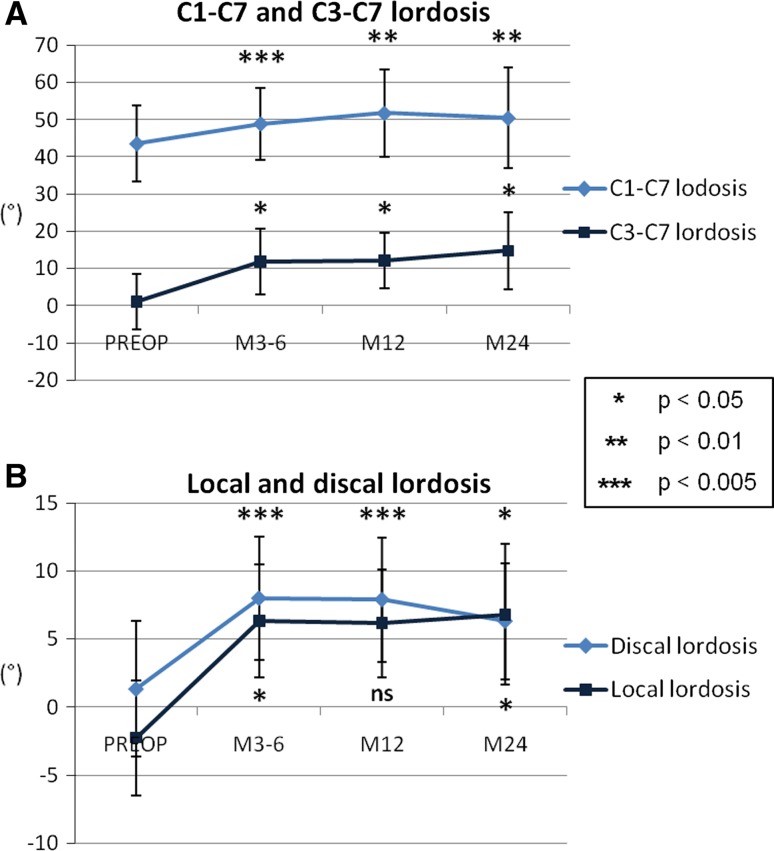
Sagittal angles
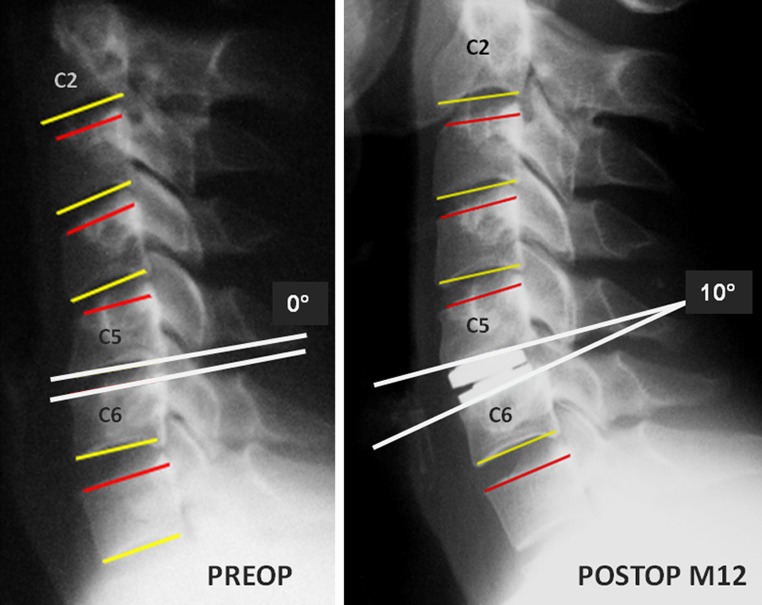
The mean C1–C7 and C3–C7 global lordosis significantly increased from 43.5° ± 10° [24–62] and 1° ± 7.5° [−13.5 to 9] preoperatively to 49° ± 9.5° [31–67] and 12° ± 9° [−2.5 to 23.5] postoperatively at early FU, to 52° ± 11.5° [19–72] and 12° ± 7.5° [−0.5 to 18.5] at M12 and to 50.5° ± 13.5° [29–75] and 14° ± 10° [−3 to 34.5] at M24; respectively. Statistical significances are presented in Fig. 5a. The mean discal and local lordosis also significantly increased from 1.5° ± 5° [−7 to 15.5] and −2° ± 4° [−7 to 3] preoperatively to 8° ± 4.5° [1–17] and 6.5° ± 4° [0–11] postoperatively at early FU, to 8° ± 4.5° [1–17] and 6° ± 4° [1–13] at M12 and to 6.5° ± 4.5° [−4 to 13] and 7° ± 5° [1–15] at M24, respectively. Statistical significances are presented in Fig. 5b. One illustrative case is presented in Fig. 6.
Fig. 5.
Global (a) and segmental (b) lordosis at preoperative, M3–6, M12 and M24 assessments. Statistical differences between pre and postoperative scores are mentioned on each graph
Fig. 6.
Illustrative case demonstrating restoration of both segmental and global lordosis after TDR at C5–C6
Disc height
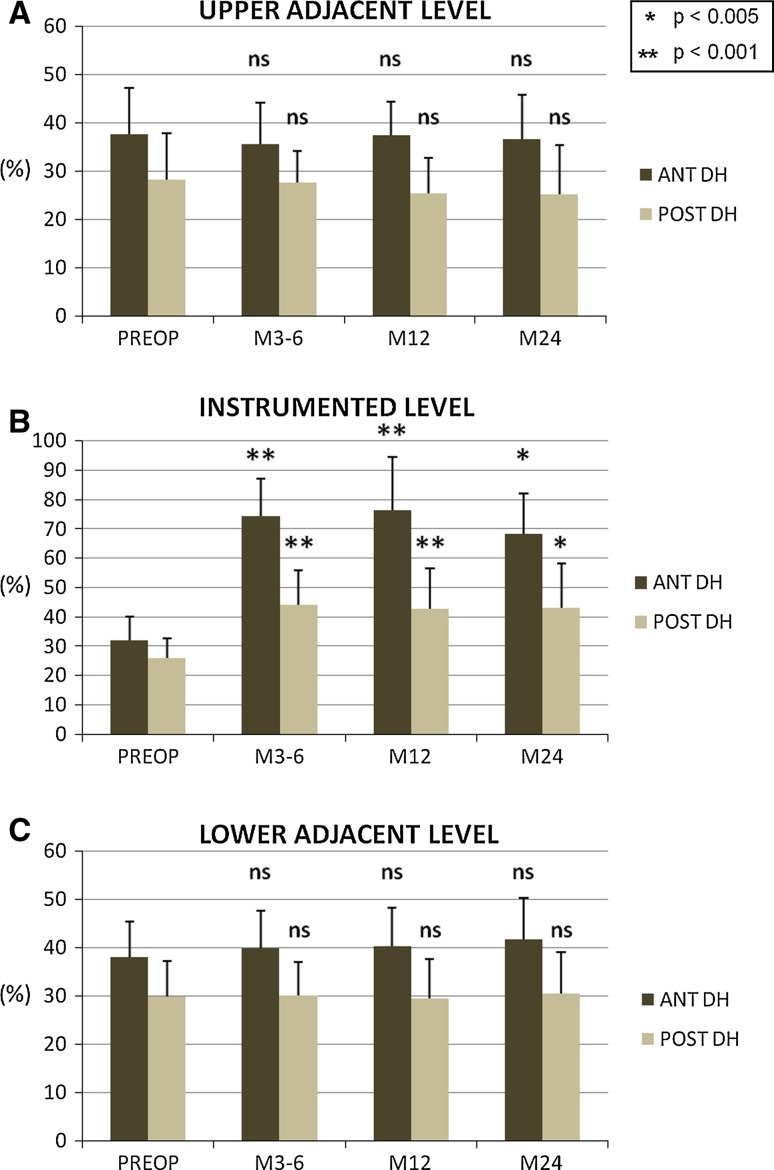
When concerning changes in disc height at operated level, as compared to preoperative values, both anterior and posterior disc height significantly increased at M3–6, M12 and M24 FU, Fig. 7b. Anterior disc height was 32 ± 8% [19–54] preoperatively versus 74 ± 13% [50–94] at M3–6, 76 ± 18% [47–112] at M12 and 68 ± 14% [33–95] at M24. Posterior disc height was 26 ± 7% [14–37] preoperatively versus 44 ± 12% [30–74] at M3–6, 43 ± 14% [30–82] at M12 and 43 ± 15% [23–80] at M24. No significant difference was observed between pre and postoperative (M3–6/M12/M24) disc height (anterior and posterior) at upper and lower adjacent levels, Fig. 7a, c.
Fig. 7.
Anterior and posterior disc heights (DH) at preoperative, M3–6, M12 and M24 assessments for instrumented (b), upper (a) and lower (c) adjacent segments. Statistical differences between pre and postoperative scores are mentioned on each graph
Kinematics
Range of motion
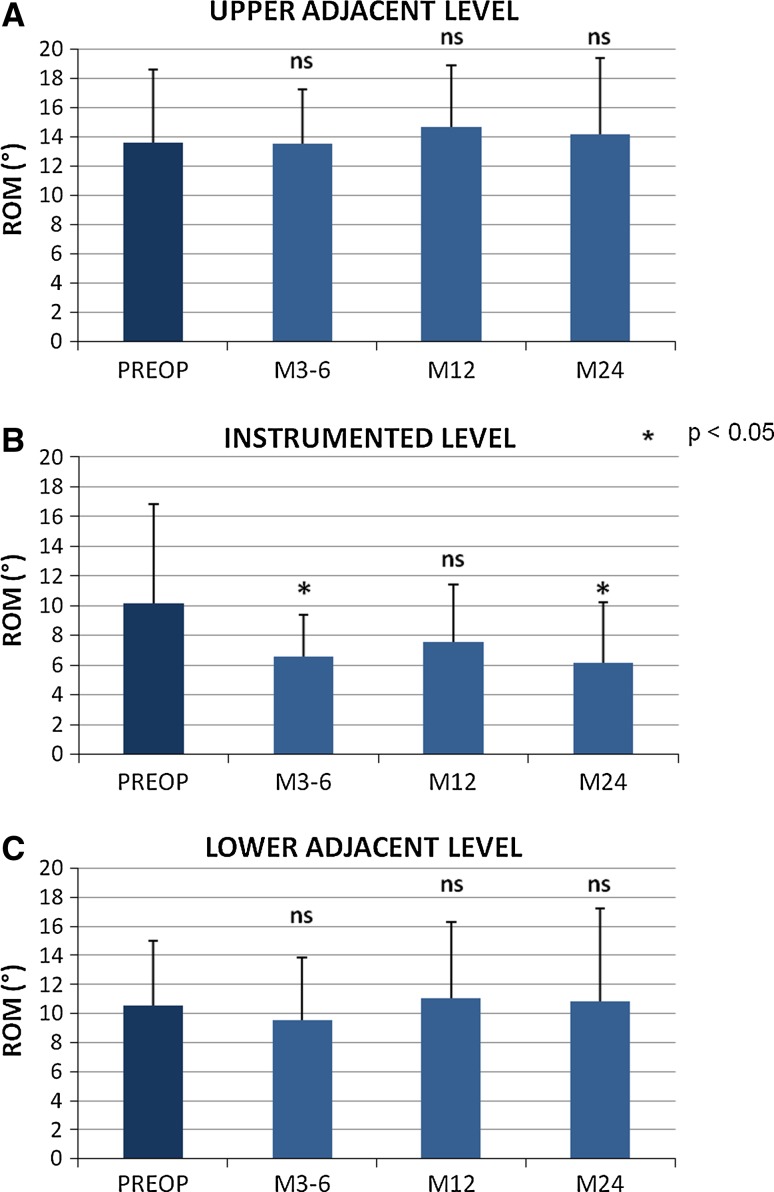
At instrumented level, ROM in FE was measured preoperatively to 10.2° ± 6.5° [0–24]. Postoperatively, we observed reduction of sagittal ROM which was measured to 6.6° ± 3° [1–13] at M3–M6, 7.5° ± 4° [0–15] at M12 and 6.1° ± 4° [0–14] at M24. Statistical significances are reported in Fig. 8b. At M24, we found that 81.25% of the instrumented levels presented with ROM > 3°. Statistical analysis found no correlation between patient age (P = 0.77), preoperative mobility (P = 0.79), preoperative instrumented disc height (P = 0.95) and postoperative ROM in FE. Otherwise, there was no correlation between cervical VAS and postoperative ROM at M12 (P = 0.69) nor at M24 (P = 0.7).
Fig. 8.
ROM in flexion–extension at preoperative, M3–6, M12 and M24 assessments for instrumented (b), upper (a) and lower (c) adjacent segments. Statistical differences between pre and postoperative scores are mentioned on each graph
No significant difference was observed between pre and postoperative (M3–6/M12/M24) sagittal ROM at upper and lower adjacent levels, Fig. 8a, c.
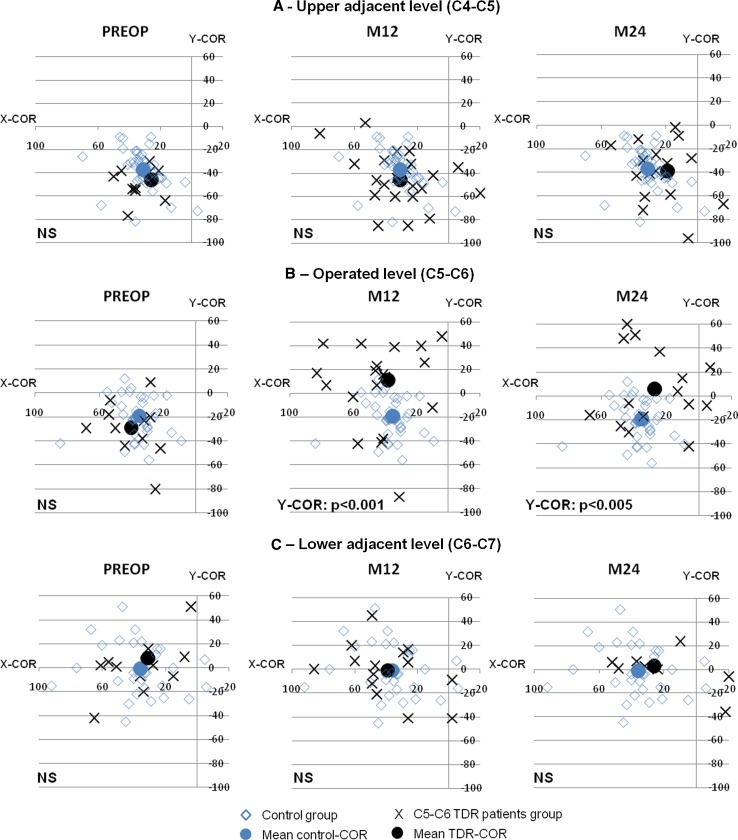
Mean centre of rotation
When compared with preoperative values, we observed consistent cranial shift of the mean COR for operated patients. At instrumented level, the mean X-COR was preoperatively calculated to 36.9 ± 20.2% [−15 to 68] versus 38.8 ± 30.8% [−62 to 83] at M12, P > 0.05, and 20.1 ± 35.6% [−92 to 67] at M24, P = 0.03; the mean Y-COR was preoperatively calculated to −25.3 ± 24.1% [−80 to 12] versus 15.8 ± 39.1% [−87 to 86] at M12, P = 0.003, and 7.6 ± 45% [−74 to 115] at M24, P < 0.05.
When concerning upper adjacent level, mean X-COR was preoperatively calculated to 25.8 ± 22.7% [−58 to 50] versus 33.7 ± 21.8% [−20 to 82] at M12, P > 0.05, and 19.5 ± 20.3% [−38 to 54] at M24, P > 0.05; mean Y-COR was preoperatively calculated to −36.4 ± 23.3% [−77 to 6] versus −42.3 ± 21.9% [−85 to 3] at M12, P > 0.05, and −36.3 ± 23.9% [−96 to 5] at M24, P > 0.05.
When concerning lower adjacent level, mean X-COR was preoperatively calculated to 27.9 ± 27.4% [−27 to 65] versus 39.3 ± 24.1% [−2 to 86] at M12, P > 0.05, and 26.1 ± 38.1% [−37 to 93] at M24, P > 0.05; mean Y-COR was preoperatively calculated to 14.2 ± 38.9% [−42 to 101] versus −1.1 ± 23.3% [−41 to 45] at M12, P > 0.05, and 2.8 ± 53.1% [−122 to 87] at M24, P > 0.05.
CORs of the control group and those of patients instrumented with TDR at C5–C6 (n = 24/32) are illustrated in Fig. 9 for instrumented and adjacent levels. Two illustrative cases are presented in Fig. 10a, b.
Fig. 9.
Location of COR at preoperative, M12 and M24 assessments for patients with C5–C6 TDR (n = 24/32). Patients COR were compared with COR obtained from a control group of normal and asymptomatic subjects for operated level (C5–C6), upper adjacent level (C4–C5) and lower adjacent level (C6–C7). The dispersion of CORs around the mean position is greater for instrumented levels than for control levels
Fig. 10.
Illustrative case (a) demonstrating that postoperative COR at operated level (C5–C6) was confounded with the geometric center of the prosthesis. In contrast to the second illustrative case (b), postoperative COR at operated level (C5–C6) was located in the facets joint area suggesting a kinematic conflict during flexion–extension
Discussion
The aim of the study was to report outcomes after TDR in the cervical spine with a special interest for sagittal alignment and kinematics at instrumented and adjacent levels. Concerning clinical outcomes, we noted that our results were concordant with those of most randomized studies carried out in the US [13, 17, 21–23].
Sagittal alignment
Even if correlations between changes in spine curvature and clinical outcomes are still under investigations, kyphotic changes after TDR should be avoided to limit axial neck pain and avoid report of stresses at adjacent levels. In our study, compared with preoperative data, segmental lordosis increased postoperatively on average by approximately 6°/7° when C3–C7 lordosis increased on average by approximately 10°/11°. Thus, the Discocerv™ device, which is specifically designed to maintain segmental lordosis with lordotic shape of the upper plate, demonstrated its capacity to restore both segmental and global lordosis. Increase in lordosis after TDR has already been reported in the literature. For instance, Anakwenze et al. [24] reported increase in operated level (+3°) and C2–C6 (+3.1°) lordosis after ProDiscC™ implantation (ball-and-socket design). In fact, postoperative segmental lordosis may be predominantly affected by TDR design, whereas restoration of global cervical spine curvature may depend mostly on cervical pain relief.
Some studies reported that sagittal alignment in the cervical spine could be altered after TDR implantation [25–28]. This adverse effect was particularly noted after implantation of Bryan™ disc [26, 28]. As example, Kim et al. [28] found that only 36% of patients with a preoperative lordotic sagittal orientation of the functional spine unit were able to maintain segmental lordosis following surgery (which consisted of implantation of Bryan™ device at one level). The loss of lordosis was considered to be mostly related to the endplates preparation and to the TDR design. These findings are in contrast with ours and suggest that specific TDR design may be useful in maintaining physiologic sagittal alignment and that too much passive design should be avoided.
One must care that the restoration of lordosis is still controversy in the cervical spine considering that that there is no valid rules for sagittal balance in the cervical spine and that straight spine can sometimes be the neutral position in asymptomatic volunteers.
Kinematics
When compared with preoperative ROM in FE (around 10°), we found that Discocerv™ device restored only partially cervical spine kinematics in the sagittal plane (postoperative ROM around 6°/7°). When compared with ROM of control group (around 15° for FE at C5–C6), reduction of mobility appears more obvious. In fact, most in vivo studies reported that ROM in FE after cervical TDR ranged only from 4° to 10° [11–17, 19, 21, 22, 28], whereas in vivo ROM from normal and asymptomatic population ranged from 15° to 20° [29–34]. As examples, Powell et al. [19] found 8.4° ROM in FE at 2 years in a series of 48 patients operated with Bryan™ cervical arthroplasty; Murrey et al. [22] reported 9.4° of sagittal ROM for patients instrumented with Pro-DiscC™ (n = 103) at 2 years; and Kim et al. [28] found only 4.9° of ROM in FE in a series of 55 Bryan™ artificial discs implanted in 47 patients.
Thus, current TDR designs fail to restore complete quantitative kinematics in the cervical spine. In fact, most current TDR consist of ball-and-socket design characterized by a 3 df joint (3D rotations but no translation) with a fixed COR during motion (considering bearing surfaces remain congruent). In contrast, the native intervertebral disc permits 6 df mobility (3D rotations and 3D translations). As a consequence, complete restoration of natural kinematics is unlikely with ball-and-socket implants and this is in accordance with our results and those reported in the literature.
Restoration of physiological intervertebral motion requires not only maintaining ROM, but also reproducing as much as possible the quality of motion. In our study, analysis of mean CORs allowed for qualitative evaluation of cervical spine kinematics. Compared with preoperative data as well as data from control group, instrumented segments with Discocerv™ device demonstrated to have significant cranial shift of the mean COR (illustrated case in Fig. 10a). This result could be expected seeing that the geometric centre of the prosthesis is placed cranially with the convex surface on the superior plate and the concave surface on the inferior plate. These findings confirm that the location of COR in vivo is highly correlated with the TDR design and particularly with the position of the prosthesis rotation center. Rousseau et al. [18], comparing different cervical TDR designs, confirmed that neither the cranial nor caudal types of ball-and-socket designs was able to fully restore the normal mobility in terms of ROM and COR in a series of 51 patients. In addition, this author also reported cranial shift of COR after TDR using ball-and-socket design with cranial geometric center (Prestige™ LP) like the prosthesis analyzed in our study. Our findings are concordant with literature data and confirm that TDR design strongly influences the nature of intervertebral motion observed in vivo. Otherwise, we observed that the mean COR of instrumented segments typically differs from the theoretical geometrical center of the implant suggesting that the rotation was not exactly conducted around the geometric centre of the prosthesis and that bearing surfaces of the prosthesis did not stay in true contact during all the ROM. These findings may probably result from kinematic conflicts in the facet joints and/or uncovertebral areas and/or from abnormal stresses of soft tissues (illustrated case in Fig. 10b).
Rationale of TDR with cranial geometric center (like Discocerv™ or Prestige™ implants) is that, in contrast to FE motion, the COR in lateral bending and axial rotation is located above the intervertebral space, as illustrated in Fig. 11 [34]. Restoring a more physiological COR in the frontal plane may allow for restoration of a more physiological kinematic in axial rotation and lateral bending and theoretically limiting uncovertebral and facet kinematic conflicts during these motions [35, 36]. In fact, TDR with caudal centre of rotation is more suitable during FE motion, whereas TDR with cranial centre of rotation is preferred during lateral bending and axial rotations. As a consequence, restoration of native intervertebral kinematics in the cervical spine is probably unlikely using TDR with fixed centre of rotation.
Fig. 11.
Mean COR during lateral bending is located above the intervertebral disc, however, because of coupled motion, lateral bending is not strictly executed in the frontal plane making measurement of COR not really relevant on 2D X-rays
Adjacent segments
Although cervical TDR restored only partly ROM in FE, we did not observe any changes in ROM at both upper and lower adjacent levels. These results suggest that maintaining some mobility at instrumented level is sufficient to avoid hypermobility and report of stresses at adjacent levels. These findings are concordant with most of those reported in the literature about adjacent segments kinematics [14, 16, 21]. Powell et al. [19] were the only authors who reported increased sagittal FE motion at adjacent segments in a patients group operated with cervical arthroplasty.
In addition, we did not find significant changes in CORs position at adjacent segments between pre and postoperative measurements neither between patients and control groups, suggesting that not only extent of motion was preserved at adjacent levels, but also the quality of motion, at least during FE.
Maintaining ROM and physiologic COR at adjacent levels may limit and/or delay adjacent segment degeneration. This is supporting by the results from the three prospective and randomized trials carried out in the US and involving cervical disc prosthesis according to which the arthroplasty groups had an overall lower rate of adjacent segment surgery at 2 years compared with ACDF [13, 17, 21, 22].
Finally, as compared to preoperative values, we did not observe significant reduction of disc height at 2 years FU suggesting that no severe discal degeneration has been induced at adjacent levels. However, we presume that 2-year FU is too short to allow for establishment of any conclusions on potential protection of adjacent levels after cervical TDR and further long-term studies are needed to confirm the capacity of TDR to reduce adjacent level disease.
Limitation
One limitation of in vivo studies is that radiographical analysis of kinematics mainly focused on sagittal mobility with limited investigation for motions in frontal and axial planes. In fact, due to the coupled motions during lateral bending and axial rotation, intervertebral motion in frontal plane is not strictly a 2D motion. Consequently, analysis of kinematics on bending plain radiographs is neither reliable nor reproducible. Three-dimensional imaging system could be helpful for a better in vivo investigation of cervical spine 3D kinematics [37].
Conclusion
Through this 2-year FU prospective study focused on cervical spine sagittal alignment and kinematics, we could observe that cervical lordosis consistently increased after TDR. This was true for both segmental and global lordosis. Otherwise, we noted that ball-and-socket arthroplasty did not fully restore native segmental kinematics with significant reduction of motion in FE and consistent cranial shift of the COR. Finally, the in vivo biomechanical behavior of the prosthesis was not so far from a good fusion with lordosis maintained at the operated level.
Despite these significant alterations to native kinematics at index level, no changes in ROM neither CORs were observed at adjacent levels.
Conflict of interest
None.
References
- 1.Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine. 1999;24:670–675. doi: 10.1097/00007632-199904010-00011. [DOI] [PubMed] [Google Scholar]
- 2.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004;4:624–628. doi: 10.1016/j.spinee.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 4.Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17:79–85. doi: 10.1097/00024720-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine. 2002;27:2431–2434. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 6.Wigfield CC, Skrzypiec D, Jackowski A, Adams MA. Internal stress distribution in cervical intervertebral discs. The influence of an artificial cervical joint and simulated anterior interbody fusion. J Spinal Disord Tech. 2003;16:441–449. doi: 10.1097/00024720-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, McAfee PC. Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine. 2005;30:1165–1172. doi: 10.1097/01.brs.0000162441.23824.95. [DOI] [PubMed] [Google Scholar]
- 8.Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, Lim J. Changes in adjacent-level disc pressure and facet joint force after cervical arthroplasty compared with cervical discectomy and fusion. J Neurosurg Spine. 2007;7:33–39. doi: 10.3171/SPI-07/07/033. [DOI] [PubMed] [Google Scholar]
- 9.Barrey C, Campana S, Persohn S, Perrin G, Skalli W (2011) Cervical disc prosthesis versus arthrodesis using one-level, hybrid and two-level constructs: an in vitro investigation. Eur Spine J (Epub ahead of print) [DOI] [PMC free article] [PubMed]
- 10.Galbusera F, Bellini CM, Brayda-Bruno M, Fornari M. Biomechanical studies on cervical total disc arthroplasty: a literature review. Clin Biomech. 2008;23:1095–1104. doi: 10.1016/j.clinbiomech.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Porchet F, Metcalf N. Clinical outcomes with the prestige II cervical disc: preliminary results from a prospective randomised clinical trial. Neurosurg Focus. 2004;17:E6. doi: 10.3171/foc.2004.17.3.6. [DOI] [PubMed] [Google Scholar]
- 12.Pickett GE, Rouleau JP, Duggal N. Kinematic analysis of the cervical spine following implantation of an artificial cervical disc. Spine. 2005;30:1949–1954. doi: 10.1097/01.brs.0000176320.82079.ce. [DOI] [PubMed] [Google Scholar]
- 13.Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. 2007;6:09–198. doi: 10.3171/spi.2007.6.3.198. [DOI] [PubMed] [Google Scholar]
- 14.Rabin D, Pickett GE, Bisnaire L, Duggal N (2007) The kinematics of anterior cervical discectomy and fusion versus artificial cervical disc: a pilot study. Neurosurg 61:ONS100–ONS105 [DOI] [PubMed]
- 15.Ramadan AS, Mitulescu A, Schmitt Total disc replacement with the Discocerv™ (Cervidisc Evolution) cervical prosthesis: early results of a second generation. Eur J Orthop Surg Traumatol. 2007;17:513–520. doi: 10.1007/s00590-007-0242-0. [DOI] [Google Scholar]
- 16.Sasso RC, Best NM. Cervical kinematics after fusion and Bryan disc arthroplasty. J Spinal Disord Tech. 2008;21:19–22. doi: 10.1097/BSD.0b013e3180500778. [DOI] [PubMed] [Google Scholar]
- 17.Heller JG, Sasso RC, Papadopoulos SM, Anderson PA, Fessler RG, Hacker RJ, et al. Comparison of Bryan cervical disc arthroplasty with anterior cervical decompression and fusion. Clinical and radiographic results of a randomized, controlled, clinical trial. Spine. 2009;34:101–107. doi: 10.1097/BRS.0b013e31818ee263. [DOI] [PubMed] [Google Scholar]
- 18.Rousseau MA, Cottin P, Levante S, Nogier A, Lazennec JY, Skalli W. In vivo kinematics of two types of ball-and-socket cervical disc replacements in the sagittal plane. Cranial versus caudal geometric center. Spine. 2008;33:E6–E9. doi: 10.1097/BRS.0b013e31815e5dce. [DOI] [PubMed] [Google Scholar]
- 19.Powell JW, Sasso RC, Metcalf NH, Anderson PA, Hipp JA. Quality of spinal motion with cervical disk arthroplasty. Computer-aided radiographic analysis. J Spinal Disord Tech. 2010;23:89–95. doi: 10.1097/BSD.0b013e3181991413. [DOI] [PubMed] [Google Scholar]
- 20.Champain S, Benchikh K, Nogier A, Mazel C, DeGuise J, Skalli W. Validation of new clinical quantitative software applicable in spine orthopaedic studies. Eur Spine J. 2006;15:982–991. doi: 10.1007/s00586-005-0927-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sasso RC, Smucker JD, Hacker RJ, Heller JG. Clinical outcomes of BRYAN cervical disc arthroplasty: a prospective randomized controlled multicenter trial with 24 month follow-up. J Spinal Disord Tech. 2007;20:481–491. doi: 10.1097/BSD.0b013e3180310534. [DOI] [PubMed] [Google Scholar]
- 22.Murrey D, Janssen M, Delamarter R, Goldstein J, Zigler J, Tay B, et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 2009;9:275–286. doi: 10.1016/j.spinee.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 23.Beaurain J, Bernard P, Dufour T, Fuentes JM, Hovorka I, Huppert J, Steib JP, Vital JM, et al. Intermediate clinical and radiological results of cervical TDR (Mobi-C®) with up to 2 years follow-up. Eur Spine J. 2009;18:841–850. doi: 10.1007/s00586-009-1017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anakwenze OA, Auerbach JD, Milby AH, Lonner BS, Balderston RA. Sagittal cervical alignment after cervical disc arthroplasty and anterior cervical discectomy and fusion: results of a prospective, randomized, controlled trial. Spine. 2009;34:2001–2007. doi: 10.1097/BRS.0b013e3181b03fe6. [DOI] [PubMed] [Google Scholar]
- 25.Johnson JP, Lauryssen C, Cambron HO, Pashman R, Regan JJ, Anand N, Bray R. Sagittal alignment and the Bryan cervical artificial disc. Neurosurg Focus. 2004;17:E4. doi: 10.3171/foc.2004.17.6.14. [DOI] [PubMed] [Google Scholar]
- 26.Fong SY, DuPlessis SJ, Casha S, Hurlbert RJ. Design limitations of Bryan disc arthroplasty. Spine J. 2006;6:233–241. doi: 10.1016/j.spinee.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 27.Pickett GE, Sekhon LH, Sears WR, Duggal N. Complications with cervical arthroplasty. J Neurosurg Spine. 2006;4:98–105. doi: 10.3171/spi.2006.4.2.98. [DOI] [PubMed] [Google Scholar]
- 28.Kim SK, Shin JH, Arbatin JJ, Park MS, Chung YK, McAfee PC. Effetcs of a cervical disc prosthesis on maintaining sagittal alignment of the functional spinal unit and overall sagittal balance of the cervical spine. Eur Spine J. 2008;17:20–29. doi: 10.1007/s00586-007-0459-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White AA, Panjabi MM. Clinical biomechanics of the spine, edn 2. Philadelphia: Lippincott; 1990. [Google Scholar]
- 30.Amevo B, Worth D, Bogduk N. Instantaneous axes of rotation of the typical cervical motion segments: a study in normal volunteers. Clin Biomech. 1991;6:111–117. doi: 10.1016/0268-0033(91)90008-E. [DOI] [PubMed] [Google Scholar]
- 31.Dvorak J, Panjabi M, Novotny J, Antinnes J. In vivo flexion/extension of the normal cervical spine. J Orthop Res. 1991;9:828–834. doi: 10.1002/jor.1100090608. [DOI] [PubMed] [Google Scholar]
- 32.Holmes A, Wang C, Han ZH, Dang GT. The range and nature of flexion-extension motion in the cervical spine. Spine. 1994;19:2505–2510. doi: 10.1097/00007632-199411001-00003. [DOI] [PubMed] [Google Scholar]
- 33.Watier B. Etude expérimentale du rachis cervical: comportement mécanique in vitro et cinématique in vivo (thesis in French) Paris: Ecole Nationale Supérieure d’Arts et Métiers; 1997. [Google Scholar]
- 34.Bogduk N, Mercer S. Biomechanics of the cervical spine. I: normal kinematics. Clin Biomech. 2000;15:633–648. doi: 10.1016/S0268-0033(00)00034-6. [DOI] [PubMed] [Google Scholar]
- 35.Barrey C, Mosnier T, Jund J, Perrin G, Skalli W. In vitro evaluation of a ball-and-socket cervical disc prosthesis with cranial geometric center. J Neurosurg Spine. 2009;11:538–546. doi: 10.3171/2009.6.SPINE0949. [DOI] [PubMed] [Google Scholar]
- 36.Snyder JT, Tzermiadianos MN, Ghanayem AJ, Voronov LI, Rinella A, Dooris A, et al. Effect of uncovertebral joint excision on the motion response of the cervical spine after total disc replacement. Spine. 2007;32:2965–2969. doi: 10.1097/BRS.0b013e31815cd482. [DOI] [PubMed] [Google Scholar]
- 37.Rousseau MA, Laporte S, Chavary-Bernier E, Lazennec JY, Skalli W. Reproducibility of measuring the shape and three-dimensional position of cervical vertebrae in upright position using the EOS stereoradiography system. Spine. 2007;32:2569–2572. doi: 10.1097/BRS.0b013e318158cba2. [DOI] [PubMed] [Google Scholar]