Abstract
Study design
Analysis of the Nationwide Inpatient Sample (NIS) from 1998 to 2008.
Objective
To analyze the most recent available and nationally representative data for risk factors contributing to in-hospital mortality after primary lumbar spine fusion.
Summary of background data
The total number of lumbar spine fusion surgeries has increased dramatically over the past decades. While the field of spine fusion surgery remains highly dynamic with changes in perioperative care constantly affecting patient care, recent data affecting rates and risk for perioperative mortality remain very limited.
Methods
We obtained the NIS from the Hospital cost and utilization project. The impact of patient and health care system related demographics, including various comorbidities as well as postoperative complications on the outcome of in-hospital mortality after spine fusion were studied. Furthermore, we analyzed the timing of in-hospital mortality.
Results
An estimated total of 1,288,496 primary posterior lumbar spine fusion procedures were performed in the US between 1998 and 2008. The average mortality rate for lumbar spine fusion surgery was 0.2 %. Independent risk factors for in-hospital mortality included advanced age, male gender, large hospital size, and emergency admission. Comorbidities associated with the highest in-hospital mortality after lumbar spine fusion surgery were coagulopathy, metastatic cancer, congestive heart failure and renal disease. Most lethal complications were cerebrovascular events, sepsis and pulmonary embolism. Furthermore, we demonstrated that the timing of death occurred relatively early in the in-hospital period with over half of fatalities occurring by postoperative day 9.
Conclusion
This study provides nationally representative information on risk factors for and timing of perioperative mortality after primary lumbar spine fusion surgery. These data can be used to assess risk for this event and to develop targeted intervention to decrease such risk.
Keywords: Perioperative mortality, Lumbar spine fusion, Risk factor, Complication, Comorbidity
Introduction
Although lumbar spine fusion surgery is one of the most commonly performed spine surgical procedures, it is associated with the risk of perioperative complications as well as death [1]. However, a paucity of most recent data exists on nationally representative rates regarding perioperative mortality, risk factors and the timing of this adverse outcome.
Most published studies, however, are limited by the fact that they are not nationally representative [2, 4], represent selected patient populations only [4], are based on fairly dated information [4, 5], and are not specifically focused on primary lumbar spine fusion surgical outcomes [3, 5]. Further, few data are focused on the immediate perioperative period, which is the time frame that is most amenable to be influenced by treating physicians.
Although lumbar spine fusion is considered a relatively safe procedure, investigations on the most recent mortality rate and contributing risk factors are required for multiple reasons. First, the aging population will increase the utilization of lumbar spine fusion surgeries [6]. This trend is likely to increase the absolute number of deaths associated with this surgery, even if overall mortality rates remain unchanged. Second, a dramatic increase of the utilization of more complex spine procedures has been shown, which ultimately was associated with an increased mortality [7]. Third, as advanced age has been shown to be associated with an increase in mortality rate, rises in the utilization among this patient population will most likely increase the incidence of death after this procedure, as advanced age has repeatedly been linked to higher rates of mortality [4, 8, 9].
Therefore, we analyzed data collected for the largest nationally representative in-hospital data base in the US, the Nationwide Inpatient Sample (NIS), to (1) determine the overall mortality rate and determine characteristics of patients that did and did not die after primary lumbar spine surgery, (2) to determine perioperative risk factors for a fatal outcome, and (3) to determine the timing of in-hospital death. We hypothesize (1) that patient demographics, surgical indications, certain comorbidities as well as complications are associated with an increased in-hospital mortality rate and (2) that fatalities occurred relatively early post operatively.
Materials and methods
Database
The Nationwide Inpatient Sample (NIS) is a database of the healthcare cost and utilization project. It is sponsored by the agency for healthcare research and quality and represents the largest inpatient discharge database within the United States. Detailed information is available online [10, 11]. The current study was exempt from review by the institutional review board due to sufficient de-identification of the data (documentation available on request).
Selection of study sample and statistical method
All primary posterior lumbar spine fusion procedures between 1998 and 2008 were included in this study. The surgeries were identified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for primary posterior lumbar spine fusion (81.08) [12].
Rates of major complications were tabulated by identifying entries that listed ICD-9-CM diagnosis codes consistent with postoperative cerebral infarction, sepsis, shock/cardiorespiratory arrest, acute myocardial infarction, cardiac complications (except myocardial infarction), pneumonia, and pulmonary embolism. In-hospital mortality rates were determined for each year.
Approximately, 30 % of entries in the race category were not available and were imputed as “white”. This approach was based on the fact that facilities with high rates of missing data for race served populations with higher than average white/black patient ratios [13]. To assess the impact of this approach on results we also analyzed data by creating a separate category for missing values. No differences when using either approach were found.
All statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC). To facilitate analysis of data collected in a complex survey design and to obtain consistent estimates of mean and variance parameters taking into account the complex survey data setting, SAS procedures SURVEYMEANS, SURVEYFREQ, and SURVEYLOGISTIC were utilized for descriptive analyses and logistic regression modeling efforts.
Weighted means and percentages were shown for continuous and categorical variables, respectively. Two multivariate logistic regression models were built to determine the impact of comorbidities and complications, respectively, on the outcome of perioperative mortality after lumbar spine fusion surgery while controlling for demographic variables. Comorbidities included in the full logistic model are alcohol abuse, congestive heart failure, chronic lung disease, coagulopathy, diabetes mellitus, liver disease, electrolyte/fluid disorders, cancer, metastatic cancer, neurologic disease, peripheral vascular disease, renal failure and cardiac valvular disease. Complications included in the full logistic model are postoperative cerebral infarction, sepsis, shock/cardiorespiratory arrest, acute myocardial infarction, cardiac complications (except myocardial infarction), pneumonia, and pulmonary embolism. Both logistic models were adjusted by the same demographic variables and hospital characteristics including spine diagnosis, age, gender, race, hospital location, size, teaching status and admission type. Note that in the in the full model regression considering postoperative complications, the Deyo Index was considered as a measure of overall comorbidity burden.
To fit a parsimonious model with strong predictive covariates only, we took the following steps. First, clinical judgment and significance at P value of 15 % level in univariate analyses were used to select variables for the process of multivariable modeling. Second, further variable selection was achieved through a nonparametric bootstrapping process [14]. In the bootstrap procedure, the original set of data of size N became a parent population from which samples of size N were randomly drawn with replacement. One hundred bootstrap samples were created, and a stepwise procedure was applied to each sample utilizing forward selection method (with selection entry level = 0.20). From this analysis, we calculated the percentage of samples for which each variable was included in the model from the 100 samples. Percent inclusion was used to determine the prognostic importance of a variable because it was expected that a prognostically important variable would be included in the model for a majority of the bootstrap samples. A model was formulated that contained the variables with percent inclusion greater than 80 % (cutoff decided a priori). For variables, which were not included, if the frequency of pair wise combinations included in the model was greater than 90 %, then include the one with the largest frequency in the final model. In addition, the c-statistic was the same as the area under the receiver-operating characteristic curve and was used to measure how well the model discriminates between observed data at different levels of the outcome [15]. Third, the model finalized at the second step was processed one more time utilizing the SURVEYLOGISTIC procedure instead of the LOGISTIC procedure to be able to obtain appropriate estimates of the variance for the weighted survey data. This step was necessary because the SURVEYLOGISTIC does not allow for forward selection procedure. This kind of switch in methods is shown by Hosmer et al. [16] to be appropriate.
Results
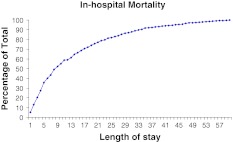
Between 1998 and 2008 an estimate of 1,288,496 posterior primary lumbar spine fusions were performed in the US. Of those, 0.2 % (n = 1,938) patients died during their in-hospital stay. In-hospital deaths occurred relatively early, with more than one-half of all fatalities occurring by day 9 (Fig. 1).
Fig. 1.
This figure depicts the in-hospital mortality over the length of stay
The average age and comorbidity burden was significantly higher in patients who died during the hospitalization as compared to patients who did not (P < 0.0001 and P < 0.0002, respectively) (Table 1).
Table 1.
Patient demographics
| Group | Alive | Died | P value |
|---|---|---|---|
| Demographics (N = 1,288,496) | |||
| N | 264,335 | 393 | |
| Weighted, N | 1,283,996 | 1,938 | |
| (%) | 99.8 | 0.2 | |
| Average age (years) | 54.3 | 66.9 | <0.0001 |
| Average comorbidity index | 0.4 | 0.6 | 0.0002 |
| Age groups (%) | |||
| 0–44 | 27.8 | 6.5 | <0.0001 |
| 45–64 | 43.4 | 28.7 | |
| 65–74 | 18.4 | 30.2 | |
| >75 | 10.4 | 34.6 | |
| Gender (%) | |||
| Male | 44.5 | 53.1 | 0.0006 |
| Female | 55.5 | 46.9 | |
| Race (%) | |||
| White | 89.0 | 88.5 | 0.50 |
| Black | 4.5 | 5.9 | |
| Hispanic | 4.0 | 3.2 | |
| Other | 2.5 | 2.4 | |
| Admission type (%) | |||
| Emergent | 3.4 | 15.9 | <0.0001 |
| Elective | 90.1 | 70.9 | |
| Urgent + other | 6.5 | 13.2 | |
| Hospital size (%) | |||
| Small | 12.0 | 6.2 | 0.0002 |
| Medium | 22.2 | 19.5 | |
| Large | 65.8 | 74.3 | |
| Hospital location (%) | |||
| Rural | 4.9 | 3.4 | 0.20 |
| Urban | 95.1 | 96.6 | |
| Hospital teaching status (%) | |||
| Non-teaching | 46.1 | 37.1 | 0.0003 |
| Teaching | 53.9 | 62.9 | |
When different age groups were compared, the majority of patients who remained alive was under 65 years of age. In comparison, the majority among fatalities was over 65 years old.
Patients of male gender were more frequently among mortalities compared to females (P = 0.0006). Patients of different racial groups were not affected differently in respect to mortality rates (P = 0.5018). However, emergent and urgent operations were more frequently affected by a fatal outcome compared to elective primary lumbar spine fusion surgery recipients (P < 0.0001). Mortalities were also over proportionately represented among patients receiving surgery in large versus small (P = 0.0002) and in teaching institutions (P = 0.0003). No difference in the incidence of fatalities was found between urban versus rural hospitals (P = 0.1964) (Table 1).
Most patient comorbidities were more prevalent among fatalities compared to non-fatalities except for diabetes mellitus (P = 0.3348) (Table 2).
Table 2.
List of comorbidities of patients undergoing spinal surgery
| Comorbidities | Alive (%) | Died (%) | P value |
|---|---|---|---|
| Alcohol abuse | 0.9 | 2.6 | 0.0011 |
| Congestive heart failure | 1.6 | 17.4 | <0.0001 |
| Chronic lung disease | 12.4 | 17.3 | 0.0028 |
| Coagulopathy | 1.1 | 17.1 | <0.0001 |
| Diabetes mellitus | 11.4 | 9.8 | 0.3348 |
| Liver disease | 0.7 | 4.2 | <0.0001 |
| Fluid and electrolyte disturbances | 6.1 | 32.0 | <0.0001 |
| Cancer | 1.5 | 7.4 | <0.0001 |
| Metastatic cancer | 0.3 | 3.7 | <0.0001 |
| Neurologic disorders | 2.6 | 10.5 | <0.0001 |
| Peripheral vascular disease | 1.5 | 3.5 | 0.0021 |
| Renal disease | 0.8 | 8.1 | <0.0001 |
| Cardiac valvular disease | 2.7 | 7.8 | <0.0001 |
All studied complications were more frequent among in-hospital mortalities compared to survivors (P < 0.0001 for all comparisons) (Table 3).
Table 3.
List of complications of patients undergoing spinal surgery
| Complications | Alive (%) | Died (%) | P value |
|---|---|---|---|
| Cerebrovascular infarction | 0.1 | 9.8 | <0.0001 |
| Pulmonary complication | 1.2 | 43.7 | <0.0001 |
| Sepsis | 0.3 | 22.1 | <0.0001 |
| Myocardial infarction | 0.3 | 16.8 | <0.0001 |
| Cardiac complications | 3.0 | 36.2 | <0.0001 |
| Pneumonia | 1.2 | 20.6 | <0.0001 |
| Pulmonary embolism | 0.2 | 8.5 | <0.0001 |
Multivariate regression analysis of preoperative risk factors (patient demographics, admission type, comorbidities and surgical indication) are displayed in Table 4. The highest odds for perioperative mortality were observed among patient’s ≥75 years of age and those with the comorbidities of congestive heart failure, coagulopathy and liver disease. The diagnoses of scoliosis, trauma and oncologic diseases showed the greatest impact on perioperative mortality. Postoperatively, all evaluated complications proved to be independent risk factors for a fatal event, with the most significant being shock, sepsis and cerebrovascular infarction (Table 5).
Table 4.
Multivariate analysis of risk factors and comorbidities for primary posterior lumbar spine fusion surgery
| Multivariate regression: risk factors for in-hospital mortality | |||||
|---|---|---|---|---|---|
| Category | Variable | Odds ratio | 95 % Confidence intervals | P value | |
| Age (reference: 45–46 years) | 0–44 years | 0.30 | 0.19 | 0.48 | <0.0001 |
| 65–74 | 2.50 | 1.87 | 3.33 | <0.0001 | |
| ≥75 | 4.35 | 3.25 | 5.82 | <0.0001 | |
| Gender (reference: female) admission type (reference: elective) | Male | 1.67 | 1.34 | 2.09 | <0.0001 |
| Emergent | 2.11 | 1.45 | 3.08 | 0.0001 | |
| Other | 1.76 | 1.28 | 2.43 | 0.0006 | |
| Comorbidities (reference: absence of disease) | Congestive heart failure | 4.49 | 3.25 | 6.21 | <0.0001 |
| Liver disease | 3.77 | 1.99 | 7.14 | <0.0001 | |
| Neurologic disease | |||||
| Diabetes mellitus | 0.58 | 0.40 | 0.83 | 0.0028 | |
| Coagulopathy | 6.89 | 4.98 | 9.52 | <0.0001 | |
| Neurologic disease | 2.99 | 2.08 | 4.30 | <0.0001 | |
| Renal failure | 2.61 | 1.64 | 4.17 | <0.0001 | |
| Electrolyte and fluid abnormalities | 2.79 | 2.13 | 3.66 | <0.0001 | |
| Electrolyte and fluid abnormalities | 2.79 | 2.12 | 3.66 | <0.0001 | |
| Diagnosis (reference: degenerative disc disease) | Spinal stenosis | 1.07 | 0.765 | 1.50 | 0.6841 |
| Scoliosis | 4.07 | 2.29 | 7.24 | <0.0001 | |
| Spondylolisthesis | 1.54 | 0.97 | 2.43 | 0.0671 | |
| Trauma | 4.77 | 2.96 | 7.68 | <0.0001 | |
| Oncologic | 6.38 | 3.50 | 11.64 | <0.0001 | |
| Multiple Diagnosis | 0.68 | 0.50 | 0.91 | 0.0096 | |
| Other | 1.65 | 1.05 | 2.59 | 0.0308 | |
Table 5.
Multivariate analysis of complications following primary posterior lumbar spine fusion surgery
| Multivariate regression: risk factors for in-hospital mortality | |||||
|---|---|---|---|---|---|
| Category | Variable | Odds ratio | 95 % Confidence intervals | P value | |
| Complications (reference: absence of complication) | Cerebrovascular infarction | 19.14 | 9.92 | 36.91 | <0.0001 |
| Sepsis | 19.81 | 12.76 | 30.76 | <0.0001 | |
| Myocardial infarction | 7.54 | 4.45 | 12.76 | <0.0001 | |
| Cardiac complications | 3.46 | 2.43 | 4.94 | <0.0001 | |
| Pneumonia | 3.04 | 1.91 | 4.83 | <0.0001 | |
| Pulmonary embolism | 10.10 | 5.39 | 18.92 | <0.0001 | |
| Shock | 150.96 | 92.37 | 246.71 | <0.0001 | |
Discussion
Utilizing nationally representative data we determined an in-hospital mortality rate of 0.2 % associated with primary posterior lumbar spine fusion. The majority of perioperative fatalities occurred within the first week-and-a-half of admission. Risk factors for increased risk of in-hospital death included advanced age, male gender, non-elective admissions and a number of comorbidities. Postoperative complications were associated with the highest odds of in-hospital mortality.
The mortality rates identified in our study are in concordance with previously published data [2–4]. While relatively low, the true mortality rate associated with this procedures remains unknown as data post discharge from the hospital are limited. However, it has been shown that the 30-day post-discharge mortality is particularly increased in the elderly [2]. Irrespectively, the increasing number of spine fusion surgeries in an aging population with more comorbid burden means that the absolute number of mortalities is likely to increase. It should be mentioned, that posterior lumbar fusions are associated with lower mortality risk than for example anterior or thoracic approaches and that these data cannot be extrapolated to other spine surgical procedures [17].
Advanced age and increasing comorbidity burden were associated with increased rates and adjusted risk of death during the patients’ hospitalization. Similar results have been published within an analysis of the NIS between 1993 and 2002 [18]. Especially patients over 65 years of age seem to have an increased risk when compared to patients under 65 years. While often linked to an increased comorbid burden among the elderly, age remained an independent risk factor even when controlling for various comorbidities in our analysis. This suggests, that age specific factors, like the physiologic decline in end organ reserve may play a role.
We found an over-proportional frequency of mortalities in large and teaching versus small and non-teaching hospitals. While speculative, this may be attributable to the fact that complex surgeries are more likely to be performed at a large, tertiary teaching facilities, thus explaining higher complication and mortality rates [3]. However, it must be mentioned that according to Farjoodi et al. [19] surgical volume of the hospital for lumbar spine surgery is inversely correlated to the complication and mortality rate. The effect of facility size however has not been studied in this context and requires further evaluation.
In our analysis, the majority of studied comorbidities were associated with a significantly increased risk of perioperative mortality especially metastatic cancer, coagulopathy, congestive heart failure and renal disease. In this context, increased comorbidity burden has been correlated to inpatient complications in the past among lumbar spine fusion patients [20]. This finding is likely associated with the decreased capacity of affected organs to compensate for perioperative insults.
Not surprisingly, postoperative complications were associated with greatest increase for the risk of mortality, especially cerebrovascular infarction, sepsis, myocardial infarction and pulmonary embolism. This finding is consistent with those in other orthopedic surgical settings and may be attributed to the independent addition of the morbidities of these adverse events to the already existing risk for mortality [21].
We further identified a number of surgical indications to be associated with an increase in the odds for perioperative mortality. Not surprisingly, scoliosis, trauma, oncologic and multiple indications were independent risk factors for increased mortality when compared to degenerative disc disease. However, it is important to mention that not each tumor, trauma or scoliosis case require the same surgical intervention. Even within each listed indication the surgical treatment might encompasses a different perioperative mortality risk. Scoliosis surgery and procedures for oncologic disorders generally require more complex interventions. In some trauma cases, the management beyond the surgical intervention itself can be challenging and therefore may lead to an increased risk of mortality.
The majority of deaths occurred relatively early during the patients hospitalization. Although data on timing of death after posterior lumbar spine fusion are not available, Parvizi et al. [22] have shown that almost 90 % of all life-threatening complications among joint surgical patients occur within the first 4 days postoperatively. This finding may therefore explain early mortalities seen in our analysis.
Analysis of the NIS database is associated with some limitations. The presented data has to be put in the right context prior to interpretation. Detailed surgical and perioperative clinical information is not available in the database. For example, no information of blood loss, length of surgery, and patient related factors like body mass index is available. As every other inpatient database, the NIS database does not capture complications or deaths outside of the in-hospital period. Therefore, the presented mortality rates almost certainly represent an underestimation of true mortality rates of posterior spine fusion procedures. Additionally, possible coding bias has to be considered. In the ICD-9-CM coding system there are a number of alternative code options for each disease. However, in this analysis we attempted to reduce such bias by utilizing recognized definitions of diseases used with administrative databases.
In conclusion, we determined a nationally representative in-hospital mortality rate after primary posterior spine fusion of 0.2 %. Furthermore, we established the timing for postoperative deaths to occur early after the procedure. We identified various patient characteristics, comorbidities, surgical indications and complications as risk factors for increased perioperative mortality. Our study provides important information, which allows for the characterization of factors associated with in-hospital mortality after primary posterior lumbar spine fusion surgery, thus allowing clinicians to gage such risk and consider the allocation of resources to prevent adverse outcomes accordingly.
IRB
As the data used in this study are sufficiently de-identified this project was exempt from review by the institutional review board.
Acknowledgments
This study was performed with funds from the Hospital for the Department of Anesthesiology at the Hospital for Special Surgery (Stavros G. Memtsoudis) and Center for Education and Research in Therapeutics (CERTs) (AHRQ RFA-HS-05-14) (Ya-lin Chiu) and Clinical Translational Science Center (CTSC) (NIH UL1-RR024996) (Yan Ma).
Conflict of interest
None.
Contributor Information
Matthias Pumberger, Email: matthiaspumberger@gmail.com.
Stavros G. Memtsoudis, Phone: +1-212-6061206, FAX: +1-212-5174481, Email: MemtsoudisS@hss.edu
References
- 1.Garrett WE, Jr, Swiontkowski MF, Weinstein JN, et al. American board of orthopaedic surgery practice of the orthopaedic surgeon: part-II, certification examination case mix. J Bone Joint Surg Am. 2006;88:660–667. doi: 10.2106/JBJS.E.01208. [DOI] [PubMed] [Google Scholar]
- 2.Oldridge NB, Yuan Z, Stoll JE, et al. Lumbar spine surgery and mortality among medicare beneficiaries, 1986. Am J Public Health. 1994;84:1292–1298. doi: 10.2105/AJPH.84.8.1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma Y, Passias P, Gaber-Baylis LK, et al. Comparative in-hospital morbidity and mortality after revision versus primary thoracic and lumbar spine fusion. Spine J. 2010;10:881–889. doi: 10.1016/j.spinee.2010.07.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Juratli SM, Mirza SK, Fulton-Kehoe D, et al. Mortality after lumbar fusion surgery. Spine. 2009;34:740–747. doi: 10.1097/BRS.0b013e31819b2176. [DOI] [PubMed] [Google Scholar]
- 5.Li G, Patil CG, Lad SP, et al. Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine. 2008;33:1250–1255. doi: 10.1097/BRS.0b013e3181714a44. [DOI] [PubMed] [Google Scholar]
- 6.Cowan JA, Jr, Dimick JB, Wainess R, et al. Changes in the utilization of spinal fusion in the United States. Neurosurgery. 2006;59:15–20. doi: 10.1227/01.NEU.0000219836.54861.CD. [DOI] [PubMed] [Google Scholar]
- 7.Kalanithi PS, Patil CG, Boakye M. National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine. 2009;34:1963–1969. doi: 10.1097/BRS.0b013e3181ae2243. [DOI] [PubMed] [Google Scholar]
- 8.Walid MS, Robinson JS 3rd, Abbara M, Tolaymat A, Robinson JS Jr (2011) De novo spine surgery as a predictor of additional spine surgery at the same or distant spine regions. Ger Med Sci 9:Doc10 [DOI] [PMC free article] [PubMed]
- 9.Deyo RA, Cherkin DC, Loeser JD, et al. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74:536–543. [PubMed] [Google Scholar]
- 10.HCUP Databases. Healthcare cost and utilization project (HCUP) (2008) Agency for healthcare research and quality, Rockville. http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 15 Mar 2010
- 11.Introduction to the HCUP national inpatient sample (NIS) 2006 (2008) Agency for healthcare research and quality, healthcare cost and utilization project (HCUP). Rockville. http://www.hcup-us.ahrq.gov/db/nation/nis/2006NIS_INTRODUCTION.pdf. Accessed 15 Mar 2010
- 12.HCUP comorbidity software healthcare cost and utilization project (HCUP) (2009) Agency for healthcare research and quality, Rockville. http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed 15 Oct 2010
- 13.Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. 1. New York: Springer; 2001. pp. 215–265. [Google Scholar]
- 14.Sauerbrei W, Schimacher M. A bootstrap resampling procedure for model building: application to the cox regression model. Stat Med. 1992;11(20):93–109. doi: 10.1002/sim.4780111607. [DOI] [PubMed] [Google Scholar]
- 15.Gonen M. Analyzing receiver operating characteristic curves with SAS. 1. Cary: SAS Institute Inc; 2007. [Google Scholar]
- 16.Hosmer DW, Lemeshow S. Applied logistic regression. 2. New York: Wiley; 2000. [Google Scholar]
- 17.Memtsoudis SG, Vougioukas VI, Ma Y, et al (2010) Perioperative morbidity and mortality after anterior, posterior, and anterior/posterior spine fusion surgery. Spine (Epub ahead of print) [DOI] [PMC free article] [PubMed]
- 18.Li G, Patil CG, Lad SP, et al. Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine. 2008;33:1250–1255. doi: 10.1097/BRS.0b013e3181714a44. [DOI] [PubMed] [Google Scholar]
- 19.Farjoodi P, Skolasky RL, Riley LH 3rd (2011) The effects of hospital and surgeon volume on postoperative complications after lumbar spine surgery. Spine. (epub ahead of print) [DOI] [PubMed]
- 20.Raffo CS, Lauerman WC. Predicting morbidity and mortality of lumbar spine arthrodesis in patients in their ninth decade. Spine. 2006;31:99–103. doi: 10.1097/01.brs.0000192678.25586.e5. [DOI] [PubMed] [Google Scholar]
- 21.Memtsoudis SG, Della Valle AG, Besculides MC, et al. Risk factors for perioperative mortality after lower extremity arthroplasty: a population-based study of 6,901,324 patient discharges. J Arthroplasty. 2010;25:19–26. doi: 10.1016/j.arth.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 22.Parvizi J, Mui A, Purtill JJ, et al. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89:27–32. doi: 10.2106/JBJS.E.01443. [DOI] [PubMed] [Google Scholar]