Abstract
Purpose
The last few decades have witnessed a paradigm shift in the assessment of outcome in spine surgery, with patient-centred questionnaires superseding traditional surgeon-based assessments. The assessment of complications after surgery and their impact on the patient has not enjoyed this same enlightened approach. This study sought to quantify the incidence and bothersomeness of patient-rated complications 1 year after surgery.
Methods
Patients with lumbar degenerative disorders, operated with the goal of pain relief between October 2006 and September 2010, completed a questionnaire 1 year postoperatively enquiring about complications arising as a consequence of their operation. They rated the bothersomeness of any such complications on a 5-point scale. Global outcome of surgery and satisfaction at the 12-month follow-up were also rated on 5-point Likert scales. The multidimensional Core Outcome Measures Index (COMI) was completed preoperatively and at the 12-month follow-up.
Results
Of 2,282 patients completing the questionnaire (92 % completion rate), 687 (30.1 %) reported complications, most commonly sensory disturbances (36 % of those with complications) or ongoing/new pain (26 %), followed by motor problems (8 %), pain plus neurological disturbances (11 %), and problems with wound healing (6 %). The corresponding “bothersomeness” ratings for these were: 1 % not at all, 23 % slightly, 27 % moderately, 31 % very, and 18 % extremely bothersome. The greater the bothersomeness, the worse the global outcome (Rho = 0.51, p < 0.0001), patient satisfaction (Rho = 0.44, p < 0.0001) and change in COMI score (Rho = 0.52, p < 0.0001).
Conclusion
Most complications reported by the patient are perceived to be at least moderately bothersome and hence are not inconsequential. Complications and their severity should be assessed from both the patient’s and the surgeon’s perspectives—not least to better understand the reasons for poor outcome and dissatisfaction with treatment.
Keywords: Self-assessment, Complications, Bothersomeness, Global treatment outcome, Satisfaction
Introduction
Over the last few decades there has been a paradigm shift in the assessment of outcome in spine surgery, with patient-centred questionnaires superseding traditional clinician-based assessments and “hard” measures such as the accuracy of screw placement, fusion status, physical impairment (e.g. strength and range of motion), etc. [5]. This change came about as a result of the realisation that “objective” measures are often of little relevance to the issue of whether the patient is able to function well and in a relatively pain-free manner in his/her everyday activities, and to enjoy a good quality of life [6]. Ultimately, it is compromises in these domains that drive the patient into the healthcare system in the first place and, accordingly, improvements in these areas constitute the outcomes of greatest importance to the patient. When extended to domains such as work capacity and healthcare utilisation, they also become the outcomes that are of greatest importance to society. The incidence of complications is commonly used as an indicator of the quality of healthcare and is another important outcome measure in spine surgery [24]. However, the assessment of complications after surgery and their impact on the patient’s life has thus far not adopted the same progressive patient-oriented approach that other outcomes have enjoyed. Most studies in the literature still only report complications as documented by members of medical staff involved at the various stages in the treatment of the patient [17]. The input of the patient is rarely considered, despite the fact that he/she is probably in the best position to report on the post-operative course in relation to the occurrence of any complications. In a recent study, the incidence of patient-rated complications at 12 months after surgery was reported to be much greater than that typically reported by surgeons at the same point in time [9]. However, the severity of these complications was not assessed, and it was unclear whether the patients had reported effects that impacted notably on their life or were instead just “trivial/inconsequential” events whose mention was merely provoked by the act of enquiry itself. The present study therefore sought to examine the perceived severity of patient-rated post-operative complications reported 1 year after spine surgery. The hypothesis was that the previously reported high frequency of patient-rated complications after lumbar spine surgery was due to the patients’ reporting of trivial or inconsequential events.
Methods
The study was carried out using the framework of the Spine Society of Europe (SSE) Spine Tango Spine Surgery Registry together with our own local spine surgery outcomes database. It involved the prospectively collected data from the consecutive patients of 21 surgeons (11 of whom had each performed at least 45 of the included cases). Participants were all operated in our Spine Centre orthopaedic and neurosurgery departments over a 4-year period between 1st October 2006 and 30th September 2010. The inclusion criteria were: undergoing spine surgery with the main pathology being lumbar degenerative disorder and with at least one of the treatment goals being pain relief as documented in the Spine Society of Europe (SSE) Spine Tango registry; good understanding of written German or English, or after 2007 Italian, French, Spanish, or Portuguese. Exclusions included emergency cases who could not be administered a patient pre-operative questionnaire.
The consent information given to patients during the final 20–30 min pre-operative consultation was standardised and provided in written as well as oral format. Patients were informed about their spinal disorder and its treatment options. With the help of radiographic imaging and a model of the spine, the surgical procedure was explained. Potential treatment-related intraoperative and post-operative complications (and any with a specifically higher risk for that particular patient) were discussed, as were factors such as the length of the expected hospital stay, the period of expected disability/absence from work and the planned rehabilitation programme. All patients with neurological deficits were informed about the likelihood and likely timescale of recovery. The diagnosis, planned surgical treatment and possible complications were documented for the patient in a pre-printed brochure containing tick-boxes and sections to be supplemented with handwritten notes in relation to the patient’s own clinical situation. The patients were given the opportunity to ask questions during the consultation.
Pathology, history, surgeon credentials, surgical procedures, and surgical and general complications prior to discharge were all documented by the surgeon on the Spine Tango surgery form.
Patients were requested to complete the Core Measures Outcome Index (COMI) questionnaire [14, 16] both preoperatively and 12 months after surgery. The questionnaires were sent to the patients to complete at home, to guarantee information free of external (care-provider) influence. The COMI is a multidimensional index (whose score ranges from 0 to 10) consisting of validated questions covering the domains of pain (leg/buttock and back pain intensity, each measured separately on a 0–10 graphic rating scale), function, symptom-specific well-being, general quality of life, and social and work disability. It was originally developed based on the recommendations for a short series of core outcome questions by an expert group in the field of low back pain outcome measurement [6] and was subsequently validated as an outcome instrument by different research groups [2, 7, 8, 12–14, 25]. In addition to the COMI questions answered both before and 12 months after surgery, at the 12-month follow-up there were 3 questions inquiring about overall satisfaction with treatment of the back problem in the hospital [5 categories from “very satisfied” (score of 1) to “very dissatisfied” (score of 5)], the global outcome of surgery [5 categories from “helped a lot” (score of 1) to “made things worse” (score of 5)], and the occurrence and nature of any complications that had arisen. The latter was addressed using the question “did any complications arise as a consequence of your operation 12 months ago (e.g. problems with wound healing, paralysis, sensory disturbances, etc.)? If so, give details.” The patients were free to describe, in their own words, any problems that they perceived as being an unwanted and unexpected consequence of the surgery. Since the patients’ descriptions of complications did not necessarily correspond with those typically reported in the scientific literature, and were not always worded using conventional medical terms, several categories were established, to which the different complications could then be assigned. The methodology for developing these categories has been described previously [9]. If the patient indicated a complication, they were required to rate its bothersomeness on a 5-point scale [not at all bothersome (score of 1), slightly bothersome (2), moderately bothersome (3), very bothersome (4), extremely bothersome (5)], using an adaptation of the pain bothersomeness question [6].
Statistical analysis
Depending on the nature of the data (continuous or categorical, respectively), descriptive values are presented as either means and standard deviations (SDs) or distributions (% values). Univariate analyses (Spearman rank correlations or Chi-square tests as appropriate) were used to explore the associations between variables. Differences between groups (e.g. those with complications and those with no complications) were examined using the independent Student t test (continuous data) and Chi-square contingency analysis (categorical variables).
Significance was accepted at the p < 0.05 level.
Results
Compliance with documentation
Over the period of study, the average compliance rate for the surgeons’ completion of the Surgical Forms in relation to the registry data collected within our Spine Centre was approximately 85 % (i.e. 85 % of all spine surgeries that were carried out had an accompanying Spine Tango Surgery Form). 2,282 patients completed the 12-month patient questionnaire (which represented a 92 % compliance rate). Their mean age was 61 (SD 15) years and there were 1,222 (49 %) men and 1,251 (51 %) women.
Patient-rated complications
Out of 2,282 patients, 687 (30 %) patients reported complications. The incidence of patient-rated complications varied for the different surgeons from 22 to 42 % (including only those spine surgeons who had operated on at least 45 of the patients in the study). There was no statistically significant difference in the proportion of complications reported by men and women (men 31 %; women 29 %; p = 0.38), or by younger and older patient groups (<60 years, 31 %; ≥60 years, 29 %; p = 0.61). Similarly, the type of health insurance cover of the patient did not influence the % complications that they reported (private/semi-private 29 %, basic obligatory 31 %, p = 0.62). There was a difference, however, in relation to the “previous surgery” categories (first ever spine surgery 26 %; first-time surgery at the given level 32 %; previous spine surgery at the given level 36 %; p < 0.0001).
The patients’ free-text descriptions of their complications were categorised as shown in Table 1. These most commonly comprised sensory disturbances (36 % of all complications reported) or new/ongoing pain (26 %) (with a combination of both pain and neurological disturbances in a further 11 % patients), followed by motor disturbances (8 %; and motor plus sensory disturbances, 3 %). Problems with wound healing were reported at a rate of 6 %, and local infections, systemic infections and internal medicine problems at approx 1–2 % each. Other incidental, unique, or infrequent complaints made up a further 7 %.
Table 1.
Distribution of complications reported by the patients at 12-month post-surgery (N = 687/2,282 reported a complication)
| Complications | No. of patients | Patients (%) |
|---|---|---|
| Sensory disturbances | 247 | 36.0 |
| Pain (new and/or ongoing) | 180 | 26.2 |
| Pain and neurological disturbance | 72 | 10.5 |
| Motor disturbances | 57 | 8.3 |
| Motor and sensory disturbances | 17 | 2.5 |
| Wound healing problems | 43 | 6.2 |
| Infection—wound/local | 11 | 1.6 |
| Infection—systemic/unspecified | 7 | 1.0 |
| Internal medicine problems | 6 | 0.9 |
| Othera | 47 | 6.8 |
| Total | 687 | 100 |
a“Other” complications included general neurological problems, dizziness, fatigue, CSF leakage, genito-urinary problems, psychological problems, stiffness/difficulty moving, and complications that did not fit any of the aforementioned/above categories
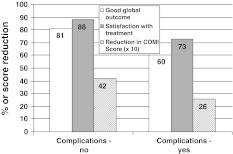
Patient-rated complications showed a significant association with global outcome and satisfaction (Fig. 1): a “good” global outcome (operation helped or helped a lot) was found in 81 % of the patients who reported no complications but in only 60 % of those with complications (p < 0.0001); the corresponding figures for “satisfaction with treatment received” were 88 % (for no patient-rated complications) and 73 % (complications) (p < 0.0001). There was also a significant difference between the groups for the reduction in the multidimensional COMI score (i.e. improvement) from pre-surgery to 12 months postoperatively: a reduction of 4.2 (SD 2.9) points was seen in the group with no complications compared with just 2.6 (SD 2.9) points in the group reporting complications (p < 0.0001).
Fig. 1.
Outcome in patients with and without self-reported complications
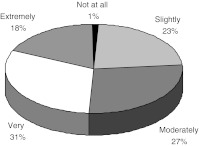
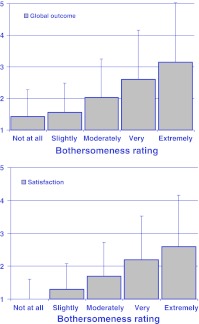
The distribution of the “bothersomeness” ratings for the complications was: 1 % not at all, 23 % slightly, 27 % moderately, 31 % very, and 18 % extremely bothersome (Fig. 2). Bothersomeness ratings were significantly associated with global outcome ratings (Rho = 0.51, p < 0.0001) and satisfaction ratings (Rho = 0.44, p < 0.0001) (Fig. 3), and also with the reduction in COMI score from pre-operative to 12 months post-operative (Rho = 0.52, p < 0.0001).
Fig. 2.
Distribution of bothersomeness ratings for the patients’ self-reported complications
Fig. 3.
Mean global outcome scores [1 (best) to 5 (worst)] (top) and satisfaction ratings [1 (best) to 5 (worst)] (bottom) in relation to complication bothersomeness category
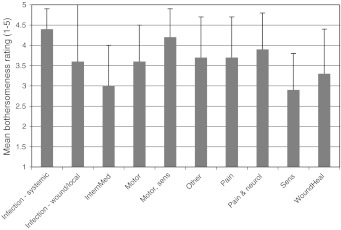
Figure 4 shows the mean bothersomeness scores (on a 1–5 scale; the higher the number, the more bothersome the complication) for each of the main complication types. Infection, combined motor and sensory disturbances, and combined pain and neurological disturbances each had significantly (p < 0.05) greater mean bothersomeness ratings than wound healing, internal medicine, and sensory disturbances.
Fig. 4.
Association between type of self-reported complication and mean bothersomeness ratings in patients reporting a complication
Surgeon-rated complications
The rate of surgical and general complications recorded prior to discharge for the group under study was 9.1 and 8.4 %, respectively. The average surgeon-assessed complication rate in patients for whom forms had been completed 12 months postoperatively was 7.4 %. However, it was not possible to make a valid comparison with the individual patient-ratings on a one-to-one basis due to the considerably lower number of surgeon forms available at 12 months (approximately 10 %); this was the result of (1) the lack of routine follow-up beyond 6–12 weeks carried out by some surgeons, especially in the case of patients who had simple decompression with no problems at the first post-operative check-up and (2) the much later (compared with the surgery forms) introduction into the surgeon’s daily routine of the Tango surgeon follow-up forms.
Discussion
The complication rates reported in the literature in connection with clinical trials or observational studies of surgical interventions/devices typically relate to complications that do not directly concern the patient or compromise the subjective result of treatment [3, 4, 10, 22, 23]. In the present study, we assessed complications from a patient-orientated approach, providing patients with a free-text field in the questionnaire to describe any new and/or untoward problems that had arisen (in their opinion) as a result of surgery. The overall complication rate (approximately 30 %) was similar to that reported in a previous study in which the same questionnaire item was used to assess patient-rated complications [9]. However, in the latter study, the severity of the reported complications was not investigated. This was addressed in the present study by introducing into the patient’s follow-up questionnaire a specific item to assess the impact of any self-reported complications, in terms of their perceived bothersomeness for the patient. Contrary to previous assumptions that the high patient-rated complication rate (approximately 30 %) might stem from the reporting of trivial or inconsequential matters, just over half of those reporting a complication stated that it was very or extremely bothersome.
Also confirming previous findings [9], there was a significant association between the presence of a patient-rated complication and the global treatment outcome, satisfaction with treatment, and reduction in Core Outcome Measures Index score from pre-surgery to 12 months’ follow-up. Moreover, the present study revealed that an extremely bothersome complication was associated with a significantly worse global outcome score than was a complication considered not at all bothersome (Fig. 3). There was an approximately stepwise worsening in the mean global outcome rating with increasing degree of bothersomeness. The same pattern was seen for satisfaction. Hence, overall, we can conclude that the reported complications are neither infrequent nor inconsequential, as far as the patient is concerned.
In keeping with the previous study [9], there was no influence of age, gender, or insurance status on the incidence of patients’ self-rated complications at 12 months’ follow-up; however, those patients who had previous surgery at the given vertebral level reported a higher rate than those undergoing first-time surgery. This concurs with the literature on surgeon-reported surgical complications, where significantly higher complications are reported for repeat surgery [22], and serves to at least partially substantiate/validate the patient-reported data.
The different types of complications were associated with different levels of bothersomeness for the patient: typically, problems with wound healing, internal medicine, and sensory disturbances were less troublesome than infections, combined motor and sensory disturbances, and combined pain and neurological disturbances. Overall, pain was one of the most prevalent complications (occurring in over one-third of patients) and it was also perceived as being relatively bothersome. Some may not consider pain to be an adverse event or complication, per se. One could argue, however, that in surgery that is specifically carried out with the intention of relieving this symptom, then—according to the definition of a complication as an undesirable, unintended, and direct result of the operation that affects the patient and that would not have occurred had the operation gone as well as could reasonably be hoped [19]—it should perhaps be considered so. The only issue might be whether the patient is referring to ongoing/new pain that began immediately after the last operation, or pain that has developed insidiously over the preceding 12 months (which may simply be due to a continuation of degenerative processes). This issue cannot be resolved within the confines of the present study but should certainly be the subject of further investigation. Nonetheless, our findings (currently unpublished) of similar complication rates and bothersome ratings at the early (3-month) follow-up would tend to challenge this explanation. It might also be questioned whether at follow-up the patients—overlooking the specification “arising as a consequence of your operation—reported symptoms e.g. sensory disturbances that had actually been present before surgery, that they had hoped would improve after surgery, even though the surgeon had informed them to the contrary. Previous studies have shown large discrepancies between the surgeon’s and patient’s respective understanding of the patient’s pre-operative status and expectations of surgery, even directly after the informed consent process has taken place [11]. If further studies should reveal that this is indeed an issue, then the questionnaire might be modified to include the words “new, not present before the operation” when enquiring about complications (e.g.,“did any complications (new problems, not present before the operation) arise as a consequence of your operation 12 months ago e.g. problems with wound healing, paralysis, sensory disturbances, etc.)?” Doing so would, however, automatically preclude “ongoing or more severe symptoms in the same region” counting as a complication, even if the intention had been to address these with the surgical intervention; whether this is indeed the correct approach would require further evaluation. Either way, based on the answers given by the patients, it is clear that their concept of a ‘‘complication’’ differs from the “typical” one of a surgeon. Since pain was not listed in the examples given in the complications item (i.e. the patients were not prompted to focus on this), yet it was frequently reported as a complication, we feel that it should be acknowledged as such—or at least open to discussion, when formalising our definitions concerning the “unwanted effects of surgery”.
One criticism that could be levelled at the interpretation of the current findings is that some of the patients may have had surgery targeting the most likely source of pain, but in the context of multiple other possible pain-sources. The surgeon of course believes that he/she knows the source of the pain; otherwise, surgery would not be offered. However, degenerative disease is most commonly multisegmental, with some segments contributing more to the symptoms than others. Indicating surgery is a balancing act between causing harm (through surgery) and providing benefit (by treating the pathology). The optimal balance might not always be achieved in every case, and this might underlie some of the reported “complications”.
“Complications” may also be reported, erroneously, as a result of something unusual that happens coincidentally during the post-operative period (completely unrelated to the surgery), for which the patient naturally tries to identify a cause. If the patient reflects on the situation, looking for an answer, he/she may look for something notable that happened recently. The likelihood that the recent surgery would be held responsible for this event is then fairly high. For example, a patient may have a herniated disc and pain. Surgery is done, and the pain is gone. But a couple of months after surgery, the patient has “nodus haemorrhoidalis” and thinks: “Wait. I had never had haemorrhoids in my life! Now, after surgery, I have. This is surely due to the surgery!” In other words, any negative event in a patient’s life that occurs after surgery might be referred to as an adverse event as perceived by the patient, even if it is just a coincidence. However, we had only few such “unconvincing-sounding” complications, and doubt that this explains a high proportion of incidents.
It was beyond the scope of the present study to examine and report on the consequences and subsequent treatment of the patients declaring a complication. Not all patients necessarily still had the complication at the 12-month follow-up; they were only asked if anything had occurred since the operation 12 months ago and how bothersome it had been. Nonetheless, some of the patients did still have persistent bothersome symptoms at 12 months and there are a number of reasons why these were perhaps not resolved. Firstly, in the eyes of the surgeon the problem may not have been something he/she could actually do anything about. Secondly, at the first post-operative follow-up (around 8 weeks), the surgeon may not have perceived how disabling things were for the patient and unintentionally regarded the issue as irrelevant and not warranting treatment. And finally, the surgeon may have adopted a “wait and see” approach, believing that the situation would improve with time. The detailed investigation of these self-reported complications and their sequelae, as well as their possible discrepancy with the surgeon’s perspective, are subjects worthy of further study.
Overall, the findings of the present study highlight the importance of systematically and routinely evaluating both treatment outcomes and complications of surgery from the patient’s perspective. Doing so would allow us to acquire the information necessary to adequately inform the patient prior to surgery not only about the likely benefits of treatment but also the potential (albeit “non life-threatening”) complications/side-effects and their likely impact on the patient’s quality of life. Assessing such attributes from a patient-orientated perspective provides the basis for counselling patients preoperatively using simple statistics and the type of language that they themselves use and understand. This should allow patients to more meaningfully take part in the decision-making process and promote the establishment of realistic expectations of surgery. It is well known that aligning expectations with reality can have a significant impact on outcome and patient satisfaction [15, 20].
Certain limitations of the present study require mention. The “bothersomeness” question was not validated against any external criterion or “gold standard” in relation to the complications encountered by the patient after spine surgery. However, bothersomeness is widely recognised as a useful tool for classifying the impact of symptoms in many medical fields [1, 6, 18, 21] and it appeared to deliver an appropriate tool for our needs. We specifically wanted to use a question that was couched in “patient-friendly” terms, that was not based solely on the absolute intensity of the symptoms, and that did not focus on the consequences simply in terms of the need for further treatment or the effect on function. We expected that the scores for bothersomeness would correlate with those used to assess treatment outcome and satisfaction, which indeed proved to be the case. In this sense, its strong relationship with the other outcome measures was itself partially testament to its validity. A completed Spine Tango surgery form was required to identify patients fitting the inclusion criteria for the study. This meant that those patients for whom no form had been completed by the surgeon, yet who would have been eligible for inclusion, represented a source of missing data (estimated as approximately 15 %). However, from the analyses carried out to date on these (details not shown), we have no reason to believe that these cases were anything other than “missing at random”. Emergency cases and a small minority of patients who did not receive the patient questionnaire due to administrative errors were not assessed preoperatively, although all were nonetheless invited to complete the 12-month questionnaire and deliver information about post-operative complications, and the questionnaire return rate at this time-point was highly respectable.
In conclusion, the rather high rate of complications from the patients’ perspective, and the impact they appear to have on the patient’s life (i.e. their degree of “bothersomeness”), suggest the need for a new approach to the assessment of complications in spine surgery. Consideration of the patient’s view, to complement/supplement that of the surgeon, would provide a basis for better educating the patient preoperatively and would also assist in understanding the poor results and dissatisfaction observed in some patients after surgery.
Acknowledgements
We are grateful to Gordana Balaban, Julian Amacker, Kirsten Clift, Sara Preziosa, and Selina Nauer for their help with the data collection.
Conflict of interest
None.
References
- 1.Cramer JA, Silberstein SD, Winner P. Development and validation of the Headache Needs Assessment (HANA) survey. Headache. 2001;41:402–409. doi: 10.1046/j.1526-4610.2001.111006402.x. [DOI] [PubMed] [Google Scholar]
- 2.Damasceno LH, Rocha PA, Barbosa ES, Barros CA, Canto FT, Defino HL, Mannion AF (2011) Cross-cultural adaptation and assessment of the reliability and validity of the Core Outcome Measures Index (COMI) for the Brazilian-Portuguese language. Eur Spine J. doi:10.1007/s00586-011-2100-3 [DOI] [PMC free article] [PubMed]
- 3.Desai A, Ball PA, Bekelis K, Lurie J, Mirza SK, Tosteson TD, Weinstein JN. SPORT: does incidental durotomy affect long-term outcomes in cases of spinal stenosis? Neurosurgery. 2011;69:38–44. doi: 10.1227/NEU.0b013e3182134171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desai A, Ball PA, Bekelis K, Lurie JD, Mirza SK, Tosteson TD, Weinstein JN. Outcomes after incidental durotomy during first-time lumbar discectomy. J Neurosurg Spine. 2011;14:647–653. doi: 10.3171/2011.1.SPINE10426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deyo RA. Measuring the functional status of patients with low back pain. Arch Phys Med Rehabil. 1988;69:1044–1053. [PubMed] [Google Scholar]
- 6.Deyo RA, Battie M, Beurskens AJHM, Bombardier C, Croft P, Koes B, Malmivaara A, Roland M, Korff M, Waddell G. Outcome measures for low back pain research. A proposal for standardized use. Spine. 1998;23:2003–2013. doi: 10.1097/00007632-199809150-00018. [DOI] [PubMed] [Google Scholar]
- 7.Ferrer M, Pellise F, Escudero O, Alvarez L, Pont A, Alonso J, Deyo R. Validation of a minimum outcome core set in the evaluation of patients with back pain. Spine. 2006;31:1372–1379. doi: 10.1097/01.brs.0000218477.53318.bc. [DOI] [PubMed] [Google Scholar]
- 8.Genevay S, Cedraschi C, Marty M, Rozenberg S, Goumoens P, Faundez A, Balague F, Porchet F, Mannion AF. Reliability and validity of the cross-culturally adapted French version of the Core Outcome Measures Index (COMI) in patients with low back pain. Eur Spine J. 2011;21:130–137. doi: 10.1007/s00586-011-1992-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grob D, Mannion AF. The patient’s perspective on complications after spine surgery. Eur Spine J. 2009;18:380–385. doi: 10.1007/s00586-009-1005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones AA, Stambough JL, Balderston RA, Rothman RH, Booth RE., Jr Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine. 1989;14:443–446. doi: 10.1097/00007632-198904000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Lattig F, Fekete TF, O’Riordan D, Mannion AF. Expectations of spinal surgery from the surgeon’s and patient’s perspectives. St Gallen: Swiss Society of Orthopaedics; 2010. [Google Scholar]
- 12.Mannion AF, Boneschi M, Teli M, Luca A, Zaina F, Negrini S, Schulz PJ (2011) Reliability and validity of the cross-culturally adapted Italian version of the Core Outcome Measures Index. Eur Spine J. doi:10.1007/s00586-011-1741-6 [DOI] [PMC free article] [PubMed]
- 13.Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Dvorak J, Jacobshagen N, Semmer NK, Boos N. Predictors of multidimensional outcome after spinal surgery. Eur Spine J. 2007;16:777–786. doi: 10.1007/s00586-006-0255-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Semmer NK, Jacobshagen N, Dvorak J, Boos N. Outcome assessment in low back pain: how low can you go? Eur Spine J. 2005;14:1014–1026. doi: 10.1007/s00586-005-0911-9. [DOI] [PubMed] [Google Scholar]
- 15.Mannion AF, Junge A, Elfering A, Dvorak J, Porchet F, Grob D. Great expectations: really the novel predictor of outcome after spinal surgery? Spine. 2009;34:1590–1599. doi: 10.1097/BRS.0b013e31819fcd52. [DOI] [PubMed] [Google Scholar]
- 16.Mannion AF, Porchet F, Kleinstück F, Lattig F, Jeszenszky D, Bartanusz V, Dvorak J, Grob D. The quality of spine surgery from the patient’s perspective: part 1. The Core Outcome Measures Index (COMI) in clinical practice. Eur Spine J. 2009;18:367–373. doi: 10.1007/s00586-009-0942-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mirza SK, Deyo RA, Heagerty PJ, Turner JA, Lee LA, Goodkin R. Towards standardized measurement of adverse events in spine surgery: conceptual model and pilot evaluation. BMC Musculoskelet Disord. 2006;7:53. doi: 10.1186/1471-2474-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20:1899–1909. doi: 10.1097/00007632-199509000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Sokol DK, Wilson J. What is a surgical complication? World J Surg. 2008;32:942–944. doi: 10.1007/s00268-008-9471-6. [DOI] [PubMed] [Google Scholar]
- 20.Stambough JL. Matching patient and physician expectations in spine surgery leads to improved outcomes. Spine J. 2001;1:234. doi: 10.1016/S1529-9430(01)00088-2. [DOI] [PubMed] [Google Scholar]
- 21.Steen N, Hutchinson A, McColl E, Eccles MP, Hewison J, Meadows KA, Blades SM, Fowler P. Development of a symptom based outcome measure for asthma. BMJ. 1994;309:1065–1068. doi: 10.1136/bmj.309.6961.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stromqvist F, Jonsson B, Stromqvist B (2011) Dural lesions in decompression for lumbar spinal stenosis: incidence, risk factors and effect on outcome. Eur Spine J. doi:10.1007/s00586-011-2101-2 [DOI] [PMC free article] [PubMed]
- 23.Stromqvist F, Jonsson B, Stromqvist B. Dural lesions in lumbar disc herniation surgery: incidence, risk factors, and outcome. Eur Spine J. 2010;19:439–442. doi: 10.1007/s00586-009-1236-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Veen EJ, Steenbruggen J, Roukema JA. Classifying surgical complications: a critical appraisal. Arch Surg. 2005;140:1078–1083. doi: 10.1001/archsurg.140.11.1078. [DOI] [PubMed] [Google Scholar]
- 25.White P, Lewith G, Prescott P. The core outcomes for neck pain: validation of a new outcome measure. Spine. 2004;29:1923–1930. doi: 10.1097/01.brs.0000137066.50291.da. [DOI] [PubMed] [Google Scholar]