Abstract
Approximately 800,000 times a year, an emergency physician admits a patient with symptomatic heart failure (HF). Yet, only a minority of emergency department (ED) patients with HF are severely ill as a result of pulmonary edema, myocardial ischemia or cardiogenic shock. The majority of patients are not in need of an acute intervention beyond decongestion, and few patients during hospitalization have invasive diagnostic testing or therapeutic procedures that require intense monitoring. While hospitalization is clearly an inflection point, marking a threshold that independently predicts a worse outcome, the exact impact of hospitalization on post-discharge events has not been well elucidated. Thus, large subsets of HF patients are hospitalized without a clear need for time-sensitive therapies or procedures. We estimate up to 50% of ED patients with HF could be safely discharged after a brief period of observation, thus avoiding unnecessary admissions, and minimizing readmissions.
Observation unit (OU) management may be beneficial for low- and intermediate-risk HF patients as continued treatment and more precise risk-stratification may ensue, avoiding inpatient admission. Whether OU management is comparable or superior to the current approach must be compared in a randomized clinical trial. Critical endpoints include time to symptom resolution and discharge, post-discharge event rates, and a cost-effective analysis of each management strategy. It is our strong assertion that now is the time for such a trial and that the results will be critically important if we are to effectively impact hospitalizations for HF in the near future.
Background
Approximately 800,000 times a year, an emergency physician admits a patient with symptomatic heart failure (HF). Yet, only a minority of emergency department (ED) patients with HF are severely ill as a result of pulmonary edema, myocardial ischemia or cardiogenic shock.(1–3) While additional patients, such as those with advanced HF who decompensate, genuinely require admission, a sizable proportion of ED HF patients present a disposition challenge: “Can this ED patient with HF be safely discharged to home?” When managing a severely ill patient with HF in the ED, the answer is easy: no. However, many of the ED patients with HF are not acutely ill, have congestion due to worsening chronic HF, and only require symptomatic treatment.(4,5) In fact, patients are most often admitted due to the uncertainty regarding post-discharge events, which may be inversely related to their appearance upon initial presentation. We believe that a large number of these admissions could be avoided, yet patients could still receive timely and effective care.
ED presentations for HF have mirrored those of acute coronary syndromes (ACS) but the success of the acute care algorithms has not been the same. Both disease processes have gone through an evolution of therapies based on a better understanding of pathophysiology and aimed at improving outcomes. Patients with ACS are now treated with aggressive medical therapy in the ED, including early definitive interventions, and at hospital discharge patients are treated with appropriate secondary prevention measures aimed at minimizing ACS recurrence and readmissions. Recently there have been similar advancements in the outpatient management of HF. Patients with systolic dysfunction now benefit from angiotensin converting enzyme inhibitors or aldosterone receptor antagonists, beta blockers, resynchronization therapy and implantable defibrillators.(6) Outcomes have improved largely due to these improvements in outpatient therapy, but acute care pathways have not consistently optimized use of evidence-based, guideline driven care. Two critical unmet needs remain. Those patients with HF and preserved systolic function have no therapy of proven benefit. Further, specific ED-based therapeutic interventions lack a solid evidence base. Regardless of ejection fraction, HF patients have a high rate of early post-discharge events, with mortality and/or re-hospitalization affecting approximately 33% of patients within 60–90 days.(7) However, it is not clear that hospitalization per se is the answer to decreasing these post-discharge event rates while it is reasonably clear that optimizing process of care strategies is associated with better short and long-term outcomes. As we continue to test new therapies to improve symptoms and outcomes in HF, and as we struggle to reduce the enormous costs associated with hospitalizations for HF, it is desirable to evaluate alternatives to hospitalization.
Although hospitalization is clearly an inflection point, marking a threshold that independently predicts a worse outcome, the exact impact of hospitalization on post-discharge events has not been well elucidated.(8,9) This is especially the case as many HF hospitalizations are driven by gaps in process of care rather than worsening pathophysiology. Further research is required to determine whether hospitalization is merely a marker of high risk, whether treatment or lack of treatment somehow affects post-discharge outcomes, or whether certain hospitalizations have no impact on outcomes at all. Several registry findings suggest that for some patients, hospitalization may not significantly impact the high event rate. First, the majority of patients are not in need of an acute intervention beyond decongestion. While most are still admitted to the hospital, in part due to complex medical comorbidities, the treatment received is solely intravenous diuretics.(4,10–12) Second, few patients during hospitalization have invasive diagnostic testing or therapeutic procedures that require intense monitoring.(13) Third, patients who require intravenous inotropic agents, mechanical circulatory support, or hemodynamic monitoring account for a minority of admissions.(14,15) Thus, a large subset of HF patients are hospitalized without a clear need for time-sensitive therapies or procedures.
ED Disposition for Acute Heart Failure
Currently about 10–20% of ED presentations for HF are discharged directly home.(10) Selecting the proper patient for ED-based management is important, as simply triaging a higher number of patients to discharge from the ED is not the answer. Patients discharged directly from the ED have higher post-discharge event rates than the 20–30% encountered after discharge from an inpatient setting.(16,17) Improving initial risk-stratification to safely increase ED discharges, or transition low-risk patients to alternative treatment pathways, thus avoiding hospitalization, is crucial to conserve healthcare resources, if this can be accomplished with similar clinical outcomes as conventional strategies. Importantly, many of the patients who return to the ED soon after discharge are also admitted to the hospital, but approximately 40% are due to non-cardiac reasons.(18,19) The majority of these non-cardiac readmissions also present for initial evaluation to the ED. Regardless of etiology, reducing preventable 30-day readmissions for patients discharged after HF hospitalization is a national quality improvement initiative, with financial consequences for hospitals that have high rates of readmission.
We postulate that a two-level targeted ED evaluation is imperative to determine an ED patient’s risk profile and discharge eligibility. The first level of risk-stratification explores 3 broad areas during the initial ED evaluation to identify patients with high-risk features(11): (Table 1): 1) important precipitants, such as ischemia, uncontrolled arrhythmias and infection; 2) presenting hemodynamics, such as hypoxia, low blood pressure, and cardiogenic shock; 3) other confounding/contributing conditions, such as renal dysfunction, hyponatremia, chronic obstructive lung disease and diabetes. Simple diagnostic testing and physical examination can identify the vast majority of these potential high-risk features. Thus, status at the time of initial presentation will determine a large component of the risk profile associated with early ED disposition decision making.
Table 1.
Initial Approach to ED patients with HF identifying important acute precipitants, hemodynamics, and other contributing conditions
| Prognostic Factor | Assessment | ED Intervention |
|---|---|---|
| Acute Precipitants | ||
| Ischemia | ECG and troponin | Antiplatelet, reperfusion, nitroglycerin |
| Infection | Chest radiograph, physical exam, urinalysis | Antibiotics, occasionally intravenous fluids |
| Arrhythmia | ECG | Rate and rhythm control via pharmacotherapy or electrical cardioversion |
| Hemodynamics | ||
| Hypotension | Vital signs | Intravenous fluids, vasopressors, inotropes |
| Hypoxia | Pulse oximetry | Oxygen, NIV, intubation |
| Organ perfusion | Mental status, capillary refill | Intravenous fluids, vasopressors, inotropes |
| Contributing Conditions | ||
| Renal dysfunction | BUN, creatinine | Vasodilators, diuresis, intravenous fluids |
| Hyponatremia | Serum sodium level | Fluid restriction |
| COPD | Pulse oximetry | Bronchodilators, steroids, oxygen |
| Diabetes | Blood glucose | Insulin, oral hypoglycemic agents |
BUN: blood urea nitrogen; COPD: chronic obstructive pulmonary disease; ECG: electrocardiography; NIV= non-invasive ventilation;
Concurrent with the diagnostic work-up, ED treatment is also begun. This is largely in the form of intravenous diuretics and topical or sublingual nitroglycerin. Evaluation after initial treatment is an important second level of ED risk-stratification. Patients generally take 1 of 3 pathways after ED therapy and depending upon their response, the remaining balance of risk can be determined. The first group is comprised of low-risk patients who respond to initial therapy, returning quickly to their baseline and not exhibiting any high-risk features. They may be eligible for ED discharge, in lieu of or after a brief period of observation.(20) The second group constitutes the high-risk patients, representing about 20% of all ED patients, who develop a worsening clinical profile after therapy. This profile includes: continued symptoms, worsening renal function, hypotension, or an elevated troponin. These patients would be poor candidates for ED discharge and should be promptly triaged to an inpatient unit for early interventions and further care.(21) The third group consists of patients with intermediate risk, who have a partial response to therapy, in which symptoms improve partially with none of the high-risk features developing. However, because of their incomplete response they require continued treatment and observation.
This ED-based two-level risk-stratification provides a foundation for disposition decision making. Those deemed high-risk, either at initial evaluation or after initial therapy, should be admitted to the hospital for a more comprehensive evaluation, treatment and risk-assessment. However, in those without high-risk features, we propose an alternative to conventional hospitalization.
Alternatives to Hospitalization in those Patients not Eligible for ED Discharge
The patient who is hospitalized for HF (HHF) receives ongoing acute therapy with a goal of optimizing volume status, leading to symptom improvement, thus facilitating discharge. These HF patients are in need of an “inpatient equivalent”, where acute therapy can be delivered, inexpensive testing can be conducted, an effective care transition planned and inpatient hospitalization can be avoided. The importance of this is highlighted by the fact that the NHLBI has identified effective alternatives to hospital admission in ED patients with HF a high priority.(22) We believe there is a sizable subset of ED patients with HF who would benefit from a period of observation and treatment, thus avoiding an inpatient admission.
Investing in a new ED approach to patients with HF is instrumental if we aim to reduce hospital admissions and readmissions. As over 80% of HF admissions and readmissions originate in the ED, the emergency physician serves an important role as the gate keeper for the inpatient with HF. They are ideally positioned to facilitate a paradigm shift away from hospital admission, and toward observation unit (OU) management. We estimate up to 50% of HF patients could be safely discharged from the ED after a brief period of observation, thus avoiding unnecessary admissions, and minimizing readmissions.(23,24) This would be a significant change to our current approach of nearly universal hospitalization in ED patients with HF who currently cannot be discharged directly from the ED. Conservatively, changing the disposition decision from admission to an OU stay in merely 5% of the 400,000 “non-high-risk” patients would result in savings of 80,000 hospital days and over $80M annually in the United States (20,000 patients at an average cost savings of $4000).(25,26)
Importantly, the OU is an ideal place to address many of the issues which hamper ED discharge and have been associated with early readmission in patients with HF (Table 2). OU management is compelling for HF management for several other reasons. First, a high proportion of patients experience improvement in dyspnea during their ED stay as a result of standard therapy.(27) Many have complete resolution within 24 hours of initial therapy, which is the typical time period of observation. Second, the monitoring of blood pressure, heart rate, urine output, and body weight can be readily provided in the OU. Third, the simple diagnostic testing that occurs during an inpatient admission, such as electrolyte testing, echocardiography, BNP/NT-proBNP and serial troponin measurements can easily be performed in the OU. Fourth, HF education and arranging outpatient follow-up are key components of OU management. These two key tasks are associated with decreased readmission, are incorporated in recently updated ACC/AHA performance measures, and are key components of OU management.(28–30) Nonetheless, OU management for HF continues to be vastly underutilized.
Table 2.
Common Observation Unit interventions which may facilitate safe and early discharge and avoid inpatient admission
| Issue to be Addressed | Method |
|---|---|
| 1) Observe response to therapy | 1) Vital signs, dyspnea testing, urine output |
| 2) Identify high-risk features | 2) Serial troponin and ECG, electrolytes, renal function |
| 3) Routine Diagnostic Testing | 3) Echocardiography |
| 4) HF education | 4) Educational pamphlets, videos, and personalized teaching by nurse practitioner |
5) Guideline directed medical therapy for HF
|
5) Prescriptions filled prior to discharge, documented plan for dose titration and provision of close monitoring |
| 6) Arrange early follow-up | 6) HF team member meets with patient at time of discharge and arranges follow-up in < 7 days |
| 7) Optimize medication regimen | 7) HF team member ensures proper regimen individualizing to the patient’s EF and comorbidities |
ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; ECG: electrocardiography; EF: ejection fraction; HF: heart failure
The purpose of an OU is to simultaneously treat and risk-stratify patients while determining the need for hospitalization. The typical entry point for OU admission is the ED, where initial evaluation and treatment occur. Consensus guidelines have been developed to identify appropriate ED patients with HF for OU management.(31) (Table 3) While those patients found to be high-risk would be ineligible for OU management, over 50% of ED patients qualify for OU management. After OU evaluation, the 75% of patients who have responded to therapy, have no identifiable high-risk features, and have a satisfactory follow-up care plan are discharged home. Their rates of readmission are similar to or better than those who are managed in an inpatient setting.(32) Patients with an inadequate response to initial therapy or with high-risk features identified during their OU stay are admitted to the hospital for further management. The OU has been used to safely discharge and conserve resources in ED patients with HF.(32)
Table 3.
Recommendations for appropriate candidates for an OU Stay
| High-risk Features to Avoid in ED Patients Considered for OU Management | ||
|---|---|---|
| Recommended | Suggested | |
| Blood pressure | SBP > 100 mmHg | SBP > 120 mmHG |
| Respiratory rate | < 32 breaths/min | NR |
| Renal function | BUN < 40 mg/dl | NR |
| Creatinine < 3.0 mg/dl | NR | |
| ACS | No ischemic changes or elevated troponin | NR |
| Natriuretic peptides | NR | BNP<1000; NT- proBNP<5000 |
ACS= acute coronary syndrome; BNP= b-type natriuretic peptide; BUN= blood urea nitrogen; NR= no recommendations; NT-BNP: N-terminal BNP; SBP= systolic blood pressure
The interventions in the OU are not complex or costly, and in fact, conserve significant resources compared to admission. If the OU is safe, efficient and minimizes healthcare expenditures, why have they not been universally implemented? The need for skillful coordination of the transition of care and the absence of a robust database to demonstrate non-inferiority, if not superiority, to conventional care remain significant hurdles. Previously, there were few financial incentives for selecting an OU stay over inpatient hospitalization for HF. However, that has changed as the Center for Medicare Services provides reimbursement for OU-based HF care while instituting penalties for excessive hospital readmissions.
There are several necessary steps to maximize OU utilization and optimize patient management: 1) on the local level, increased collaboration among emergency physicians, cardiologists, hospitalists and primary care physicians to ensure continuity of care from ED admission through hospital discharge and outpatient follow-up; 2) on the national level, dissemination of successful protocols, including patient selection and therapeutic pathways; 3) from a research perspective, patient selection, comparative outcome, and cost-effectiveness studies further identifying optimal OU patients and protocols that maximize healthcare resource utilization.
Future Directions
Evidence-based therapies have resulted in improvements in the outpatient management of HF.(33) Despite an increasingly complex population of patients, the overall length of hospital stay has decreased. However, post-discharge event rates remain disturbingly high, and it is not clear that hospitalization mitigates these event rates. While we continue to explore clinical trials evaluating therapies aimed at reducing subsequent events, simultaneous efforts using novel management strategies are needed. Emergency physicians are key stake holders in this process, as the ED is the point of triage and disposition for the majority of HF patients who are considered for hospital admission. A focused initial ED evaluation using readily-available baseline data is the first step in identifying HF patients who may be eligible for ED discharge. The response to therapy initiated in the ED constitutes the second level of risk assessment. OU management may be beneficial for low- and intermediate-risk HF patients as continued treatment and more precise risk-stratification may ensue, avoiding inpatient admission and readmission, and dispositioning patients to an appropriate level of care in the hospital. Alternatives to hospitalization, such as the one we propose, are crucial to our overall goal of allocating resources to those high-risk patients in need of intense evaluation and therapy, while simultaneously facilitating outpatient management of lower-risk patients.
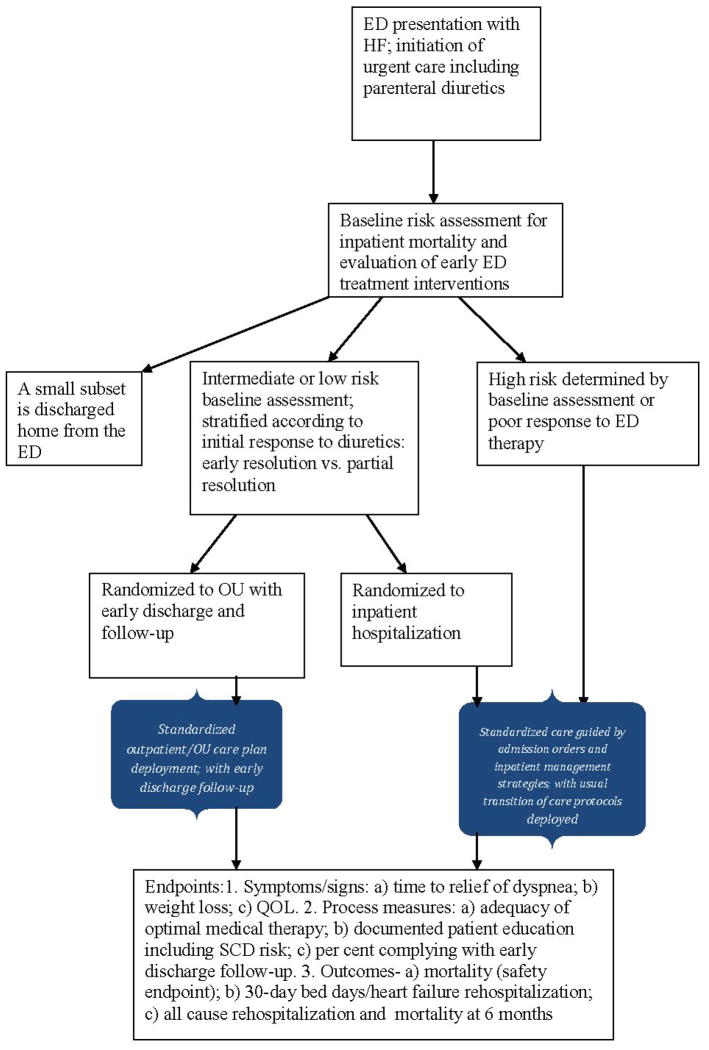
Whether our proposed risk assessment and disposition strategy is comparable or superior to the current approach must be compared in a randomized clinical trial. We now propose such a trial and have summarized the research algorithm in Figure 1. Patients who are initially evaluated in the ED and found to be at high-risk for inpatient morbidity and mortality are admitted to an inpatient setting for immediate intense evaluation and therapy. Those patients who are initially triaged as intermediate or low-risk and have some response to initial therapy are randomized to either OU or inpatient management. Critical endpoints include time to symptom resolution and discharge, post-discharge event rates, and a cost-effective analysis of each management strategy. With a sample size of 700 patients (power = 0.91, alpha = 0.05) the study would be able to detect a 35% reduction in the odds that the number of bed days exceeds any chosen cutoff. It is our strong assertion that now is the time for such a trial and that the results will be critically important if we are to effectively impact hospitalizations for HF in the near future.
Figure 1. ED Patient Enrollment in a Randomized OU Trial of AHF Management.
The figure demonstrates patient flow from initial ED presentation and baseline assessment through randomization and outpatient follow-up. The proposed endpoints are also provided.
Acknowledgments
This work was supported in part by National Heart, Lung and Blood Institute grant K23HL085387.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sean P. Collins, Vanderbilt University, Nashville, TN.
Peter S. Pang, Northwestern University, Chicago, Il.
Gregg C. Fonarow, University of California at Los Angeles, Los Angeles, CA.
Clyde W. Yancy, Northwestern University, Chicago, Il.
Robert O. Bonow, Northwestern University, Chicago, Il.
Mihai Gheorghiade, Northwestern University, Chicago, Il.
References
- 1.Nieminen MS, Brutsaert D, Dickstein K, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27:2725–36. doi: 10.1093/eurheartj/ehl193. [DOI] [PubMed] [Google Scholar]
- 2.Fonarow GC, Abraham WT, Albert NM, et al. Day of admission and clinical outcomes for patients hospitalized for heart failure: findings from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF) Circ Heart Fail. 2008;1:50–7. doi: 10.1161/CIRCHEARTFAILURE.107.748376. [DOI] [PubMed] [Google Scholar]
- 3.Fonarow GC, Stough WG, Abraham WT, et al. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll of Cardiol. 2007;50:768–77. doi: 10.1016/j.jacc.2007.04.064. [DOI] [PubMed] [Google Scholar]
- 4.Collins SP, Peacock WF, Lindsell CJ, et al. S3 detection as a diagnostic and prognostic aid in emergency department patients with acute dyspnea. Ann Emerg Med. 2009;53:748–57. doi: 10.1016/j.annemergmed.2008.12.029. [DOI] [PubMed] [Google Scholar]
- 5.Collins SP, Pang PS, Lindsell CJ, et al. International variations in the clinical, diagnostic, and treatment characteristics of emergency department patients with acute heart failure syndromes. Eur J Heart Fail. 2010;12:1253–60. doi: 10.1093/eurjhf/hfq133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:e391–479. doi: 10.1161/CIRCULATIONAHA.109.192065. [DOI] [PubMed] [Google Scholar]
- 7.Gheorghiade M, Abraham WT, Albert NM, et al. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296:2217–26. doi: 10.1001/jama.296.18.2217. [DOI] [PubMed] [Google Scholar]
- 8.Gheorghiade M, De Luca L, Fonarow GC, Filippatos G, Metra M, Francis GS. Pathophysiologic targets in the early phase of acute heart failure syndromes. Am J Cardiol. 2005;96:11G–17G. doi: 10.1016/j.amjcard.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J. 2007;154:260–6. doi: 10.1016/j.ahj.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 10.Weintraub NL, Collins SP, Pang PS, et al. Acute heart failure syndromes: emergency department presentation, treatment, and disposition: current approaches and future aims: a scientific statement from the American Heart Association. Circulation. 2010;122:1975–96. doi: 10.1161/CIR.0b013e3181f9a223. [DOI] [PubMed] [Google Scholar]
- 11.Gheorghiade M, Braunwald E. A proposed model for initial assessment and management of acute heart failure syndromes. JAMA. 2011;305:1702–3. doi: 10.1001/jama.2011.515. [DOI] [PubMed] [Google Scholar]
- 12.Fonarow GC, Abraham WT, Albert NM, et al. Factors identified as precipitating hospital admissions for heart failure and clinical outcomes: findings from OPTIMIZE-HF. Archives of internal medicine. 2008;168:847–54. doi: 10.1001/archinte.168.8.847. [DOI] [PubMed] [Google Scholar]
- 13.Gheorghiade M, Pang PS, Ambrosy AP, et al. A comprehensive, longitudinal description of the in-hospital and post-discharge clinical, laboratory, and neurohormonal course of patients with heart failure who die or are re-hospitalized within 90 days: analysis from the EVEREST trial. Heart Fail Rev. 2012;17:485–509. doi: 10.1007/s10741-011-9280-0. [DOI] [PubMed] [Google Scholar]
- 14.Adams KF, Jr, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE) AmHeart J. 2005;149:209. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 15.Abraham WT, Adams KF, Fonarow GC, et al. In-hospital mortality in patients with acute decompensated heart failure requiring intravenous vasoactive medications: an analysis from the Acute Decompensated Heart Failure National Registry (ADHERE) Journal of the American College of Cardiology. 2005;46:57–64. doi: 10.1016/j.jacc.2005.03.051. [DOI] [PubMed] [Google Scholar]
- 16.Rame JE, Sheffield MA, Dries DL, et al. Outcomes after emergency department discharge with a primary diagnosis of heart failure. Am Heart J. 2001;142:714–9. doi: 10.1067/mhj.2001.118473. [DOI] [PubMed] [Google Scholar]
- 17.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New Eng J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 18.Dunlay SM, Redfield MM, Weston SA, et al. Hospitalizations after heart failure diagnosis a community perspective. J Am Coll Cardiol. 2009;54:1695–702. doi: 10.1016/j.jacc.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Connor CM, Miller AB, Blair JE, et al. Causes of death and rehospitalization in patients hospitalized with worsening heart failure and reduced left ventricular ejection fraction: results from Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) program. American heart journal. 2010;159:841–849. e1. doi: 10.1016/j.ahj.2010.02.023. [DOI] [PubMed] [Google Scholar]
- 20.Peacock WF, Fonarow GC, Ander DS, et al. Society of Chest Pain Centers recommendations for the evaluation and management of the observation stay acute heart failure patient-parts 1–6. Acute Card Care. 2009;11:3–42. doi: 10.1080/02652040802688690. [DOI] [PubMed] [Google Scholar]
- 21.Collins SP, Lindsell CJ, Storrow AB, et al. Early changes in clinical characteristics after emergency department therapy for acute heart failure syndromes: identifying patients who do not respond to standard therapy. Heart Fail Rev. 2012;17:387–94. doi: 10.1007/s10741-011-9294-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peacock WF, Braunwald E, Abraham W, et al. National Heart, Lung, and Blood Institute working group on emergency department management of acute heart failure: research challenges and opportunities. J Am Coll Cardiol. 2010;56:343–51. doi: 10.1016/j.jacc.2010.03.051. [DOI] [PubMed] [Google Scholar]
- 23.Graff L, Orledge J, Radford MJ, Wang Y, Petrillo M, Maag R. Correlation of the Agency for Health Care Policy and Research congestive heart failure admission guideline with mortality: peer review organization voluntary hospital association initiative to decrease events (PROVIDE) for congestive heart failure. Ann Emerg Med. 1999;34:429–37. doi: 10.1016/s0196-0644(99)80043-2. [DOI] [PubMed] [Google Scholar]
- 24.Collins SP, Lindsell CJ, Naftilan AJ, et al. Low-risk acute heart failure patients: external validation of the Society of Chest Pain Center’s recommendations. Crit Path Cardiol. 2009;8:99–103. doi: 10.1097/HPC.0b013e3181b5a534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Association AH. Heart Disease and Stroke Statistics- 2004 Update. Dallas: 2003. [Google Scholar]
- 26.Association AH. Heart Disease and Stroke Statistics- 2005 Update. Dallas: 2004. [Google Scholar]
- 27.Mebazaa A, Pang PS, Tavares M, et al. The impact of early standard therapy on dyspnoea in patients with acute heart failure: the URGENT-dyspnoea study. Eur Heart J. 2010;31:832–41. doi: 10.1093/eurheartj/ehp458. [DOI] [PubMed] [Google Scholar]
- 28.Metra M, Gheorghiade M, Bonow RO, Dei Cas L. Postdischarge assessment after a heart failure hospitalization: the next step forward. Circulation. 2010;122:1782–5. doi: 10.1161/CIRCULATIONAHA.110.982207. [DOI] [PubMed] [Google Scholar]
- 29.Bonow RO, Ganiats TG, Beam CT, et al. ACCF/AHA/AMA-PCPI 2011 Performance Measures for Adults With Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. J Am Coll Cardiol. 2012;59:1812–32. doi: 10.1016/j.jacc.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 30.Gheorghiade M, Peterson ED. Improving postdischarge outcomes in patients hospitalized for acute heart failure syndromes. JAMA. 2011;305:2456–7. doi: 10.1001/jama.2011.836. [DOI] [PubMed] [Google Scholar]
- 31.Peacock WF, Fonarow GC, Ander DS, et al. Society of Chest Pain Centers Recommendations for the evaluation and management of the observation stay acute heart failure patient: a report from the Society of Chest Pain Centers Acute Heart Failure Committee. Crit Path Cardiol. 2008;7:83–6. doi: 10.1097/01.hpc.0000317706.54479.a4. [DOI] [PubMed] [Google Scholar]
- 32.Storrow AB, Collins SP, Lyons MS, Wagoner LE, Gibler WB, Lindsell CJ. Emergency department observation of heart failure: preliminary analysis of safety and cost. Congest Heart Fail. 2005;11:68–72. doi: 10.1111/j.1527-5299.2005.03844.x. [DOI] [PubMed] [Google Scholar]
- 33.Fonarow GC, Albert NM, Curtis AB, et al. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF) Circulation. 2010;122:585–96. doi: 10.1161/CIRCULATIONAHA.109.934471. [DOI] [PubMed] [Google Scholar]