Abstract
Background and Objective
To evaluate corneal wound healing after femtosecond laser-assisted keratoplasty (FLAK) using in vivo confocal microscopy (IVCM).
Study Design
Prospective, interventional, consecutive case series of 17 eyes after mushroom-shaped FLAK. IVCM was performed preoperatively and at 1, 3, 6, and 12 months to assess wound healing.
Results
Mean keratocyte activation grade increased from preoperative levels to 1 month postoperatively in both the central (0.41 ± 0.62 to 1.73 ± 1.03) and peripheral (0.47 ± 0.52 to 1.57 ± 1.09) cornea, then gradually decreased through 12 months. Dendritic cells increased from preoperative to 1 month postoperative in both the central (0.71± 0.83 to 1.33 ± 0.98) and peripheral (0.79 ± 0.70 to 1.42 ± 0.90) cornea, then gradually decreased until 6 months. Stromal reinnervation was 1 month postoperatively in 8 patients (50%). By 12 months, subepithelial nerves were observed centrally in 5 patients (45.5%).
Conclusions
IVCM after FLAK shows an initial increase in keratocyte activation and dendritic cells that decrease over time. Corneal reinnervation is seen as early as 1 month postoperatively.
Introduction
Penetrating keratoplasty (PK) is currently one of the most common and successful transplant procedures performed in the United States.1 Its success is due in part to refinements in instrumentation that have taken place since the first successful corneal transplant was performed over 100 years ago. A recent development in the evolution of PK is the use of laser technology for performing corneal trephination, beginning with the excimer laser in the 1990s.2,3 More recently, the femtosecond laser, with its precise, programmable incisions and minimal collateral tissue damage, has shown great promise for this application.4–8 Recent studies suggest that femtosecond laser-assisted keratoplasty (FLAK) may result in improved corneal healing, earlier suture removal,7 faster visual recovery, less astigmatism,8 and increased wound strength as compared to conventional PK.9,10
Although clinical outcomes of FLAK have been reported in the literature, postoperative corneal changes at the cellular level have not been previously characterized after FLAK. In vivo confocal microscopy (IVCM) permits noninvasive, high-resolution, high-magnification imaging of the microstructures of the cornea, and is an ideal imaging modality for longitudinal assessment of postoperative corneal wound healing. IVCM findings after conventional PK have been previously described, including activated keratocytes,11–13 dendritic cells (in the setting of graft rejection),14 graft reinnervation,15–18 needle-like opacities,13 and small hyperreflective particles sometimes referred to as microdots.13 Activated keratocytes are found in the corneal stroma and are thought to represent cells transitioning to a repair phenotype that is most commonly observed postoperatively.19 Dendritic (Langerhans) cells are antigen-presenting cells that are typically observed in the basal epithelium and Bowman membrane; while they are present to some extent in normal corneas, their numbers are increased in inflammatory and postoperative states.14,20,21 Needle-like opacities and microdots are thought to represent cellular debris or other disorganized extracellular material and have been described in postoperative and inflammatory corneal conditions.13,22–24 Previous studies have described IVCM findings after femtosecond laser-assisted corneal procedures other than FLAK, including LASIK flap creation, isolated stromal ablation, lamellar keratoplasty, and arcuate keratotomy.25–34 We believe that better characterization of postoperative corneal changes at the cellular level will provide useful insight into the corneal wound healing process after FLAK. This study was undertaken as an interim assessment to quantitate and analyze longitudinal IVCM findings in patients in the first year after FLAK in this ongoing study.
Patients/Materials and Methods
Patients
This prospective, interventional, consecutive case series was performed at the University of Michigan, W.K. Kellogg Eye Center, was approved by the Institutional Review Board of the University of Michigan Medical School, and is registered at clinicaltrials.gov. Seventeen patients were enrolled from November 2007 to October 2009. Informed consent was obtained from all study participants and data were collected in a HIPAA-compliant manner. Of the patients enrolled, 10 were caucasian, 4 african american, 2 asian and 1 hispanic. Inclusion criteria included age ≥ 18 years, corneal opacification or ectasia, best-corrected visual acuity ≤ 20/40 in the affected eye, and the ability to participate in follow-up visits. Exclusion criteria were corneal opacification sufficiently dense to prevent visualization of the iris, corneal thickness ≥ 1200 μm at the 9 mm peripheral zone, severe corneal thinning, prior penetrating keratoplasty or incisional surgery, poor visual potential in the nonoperative eye, a history of glaucoma or steroid-induced rise in intraocular pressure, or active intraocular inflammation or infection. All patients enrolled in the study underwent FLAK using a mushroom-shaped incision. Patients were evaluated with IVCM preoperatively and at 1, 3, 6, and 12 months postoperatively.
Donor corneas were obtained from the Michigan Eye Bank. Mean donor age was 45 ± 19 years (range, 15–69 years), mean endothelial cell density was 2891 ± 447 cells/mm2 (range, 2415–4310 cells/mm2) and death-to-preservation time ranged from 2 to 15 hours. The corneal tissue was prepared with the femtosecond laser on the day of surgery, which was within 7 days of preservation.
FLAK Surgical Technique
The donor and recipient corneas were cut using a 60 kHz femtosecond laser (IntraLase, Abbott Medical Optics, Irvine, CA) in the W.K. Kellogg Eye Center refractive surgery suite. The donor tissue was cut after mounting on an artificial anterior chamber (Katena Products, Inc, Denville, NJ) and use of a standard applanation lens with preprogrammed laser energy, depth and pattern. Laser trephination (side cut) and lamellar (ring cut) energy were 3.0 μJ, spot and line separations were both 5 μm, as recommended for keratoplasty with femtosecond laser.
All donor corneal buttons and recipient eyes were cut with a mushroom pattern. Laser treatments were conducted from posterior to anterior, in order to avoid blockage of subsequent laser shots by the accumulating gas bubbles. The posterior side cuts were initiated at a depth of 1200 μm from the anterior corneal surface in donor corneas, and 200 microns posterior to the thickest portion of the cornea at 7–9 mm from the center of the cornea as assessed by anterior segment optical coherence tomography (Visante OCT, Carl Zeiss Meditec, Dublin, CA) in recipients. The lamellar cuts were planar incisions parallel to the anterior corneal surface at approximately 50% depth in the recipient cornea. The depth of the lamellar cut in the donor and recipient were matched from the anterior surface. The anterior side cuts were trephination cuts from the lamellar surface towards the anterior corneal surface. The anterior diameter was 9.0–9.4 mm while the posterior diameter was 7.0–7.5 mm. The laser cut interfaces of the donor cornea were swept with a Barraquer spatula to break any remaining stromal bridges. The corneal button was stored in Optisol tissue preservation medium (Bausch and Lomb, Inc., Rochester, NY) until transplantation on the same day, within 1 hour after tissue preparation.
The recipient corneas were cut with similar technique, pattern and settings except for undersizing of the diameter by 0.2 mm and retaining a 40–100 μm tissue bridge of uncut stroma in the anterior side cut in order to maintain globe integrity during transportation to the operating room. Alignment marks were not used in the donor or recipient corneas in this study.
The patients received topical anesthesia with proparacaine 0.5% eye drops prior to the laser incisions and a retrobulbar block or general anesthesia after transportation to the operating room located adjacent to the refractive surgery suite. After surgical preparation and draping, the anterior chamber was entered using either a Barraquer spatula or miniature Wescott scissors. The precut donor tissue was then sutured using standard technique with a combination of 10-0 nylon interrupted and 11-0 nylon running sutures. Postoperatively, patients were placed on topical moxifloxocin 0.5% four times per day for 1 week and prednisolone acetate 1% four times a day, tapered beginning at 3 months postoperatively.
In Vivo Confocal Microscopy
IVCM was performed using a laser scanning confocal microscope, the Heidelberg Retina Tomograph II Rostock Cornea Module (Heidelberg Engineering, Heidelberg, Germany). An optically clear gel was placed on the front surface of the microscope lens and on the ocular surface as a coupling agent. The microscope provides a 400×400 μm en face view of corneal microstructures layer by layer. Contact examination was performed to obtain up to three full-thickness video sequence scans of the central and temporal peripheral cornea at each visit. Due to limitations of the instrumentation, the same precise area of cornea was not scanned at each visit; rather, several representative scans of the cornea in the central and peripheral regions were obtained.
Corneal scans were randomized prior to review. Poor quality images were excluded from the analysis. Still images from the video sequences were evaluated for degree of keratocyte activation, number of dendritic cells, and the presence of corneal nerves, needle-like opacities, and microdots. Grading was based on the maximal findings identified within each corneal scan or set of scans if more than one was obtained at a particular visit. Interpretation was based on standard images (Figs 1–3) and the following definitions:
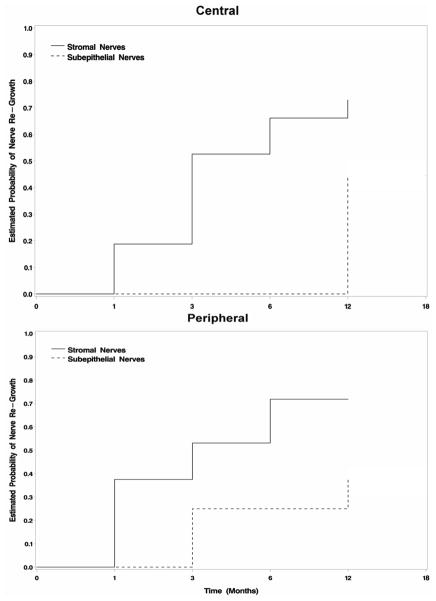
Figure 1.
Keratocyte activation. In vivo confocal microscopy standard images used for grading keratocyte activation. Grade 0: 0–25% of keratocytes with visible cell processes; grade 1: 25–50% activation; grade 2: 50–75% activation, grade 3: 75–100% activation.
Figure 3.
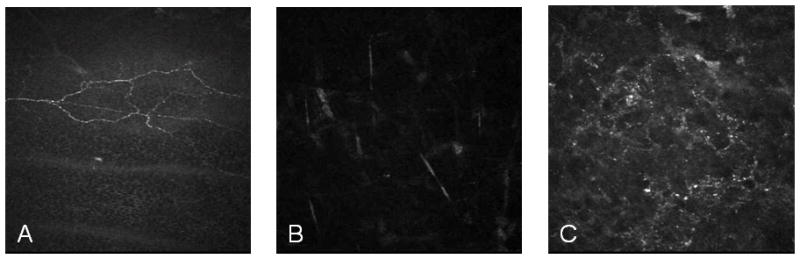
In vivo confocal microscopy standards used for determining the presence of (A) subepithelial corneal nerves, (B) needle-like opacities, and (C) microdots.
Activated keratocytes: keratocytes with visible cytoplasmic processes. Scans were evaluated beginning at a depth of 100 μm to minimize interference from subepithelial and/or anterior stromal hyperreflectivity. Grade 0: 0 to 25% of keratocytes exhibit activation; grade 1: 25 to 50%; grade 2: 50 to 75%; grade 3: 75 to 100% (Fig 1).
Dendritic cells: identified by characteristic morphology and location in the basal epithelium. Grade 0: no dendritic cells; grade 1: 1 to 5 dendritic cells; grade 2: 6 to 20 dendritic cells; grade 3: >20 dendritic cells (Fig 2). Grading was based on the maximum number of cells counted in a 400×400 μm frame within a given scan.
Corneal nerves: characterized by the typical appearance of subepithelial or stromal nerve fiber bundles (Fig 3A). Nerves were noted as being either present or absent in the subepithelial and stromal locations.
Needle-like opacities: thin, linear, randomly oriented structures visible within the stroma (Fig 3B) noted to be present or absent.
Microdots: small, hyperreflective dots also found within the stroma (Fig 3C) noted to be present or absent.
Figure 2.
Dendritic (Langerhans) cells. In vivo confocal microscopy standard images used for grading dendritic cells. Grade 0 (not shown): no dendritic cells in the basal epithelium; grade 1: 1–5 cells; grade 2: 6–20 cells; grade 3: >20 cells.
All scans were evaluated by a single reviewer (KHK) who was masked as to timing of scans. Twenty-five percent of the scans were also evaluated by a second reviewer (RMS) to determine the level of interobserver reliability in all IVCM parameters evaluated, which was good to excellent (κ=0.62 to 0.86).
Statistical Analysis
Statistical analysis was performed using SAS 9.2 software (SAS Institute, Cary, North Carolina). Student’s t test was used to compare pre- and postoperative keratocyte activation and dendritic cell grading. The significance of keratocyte activation and dendritic cell association was calculated using Fisher’s exact test. Kaplan-Meier analysis was performed for survival analysis of regeneration of stromal and subepithelial nerves in the central and peripheral cornea.
Results
Demographics
Seventeen eyes (11 right/6 left) of 17 patients (6 male/11 female) with mean follow-up of 9.1 ± 4.3 months (range, 1–12 months) were included in this analysis. Mean age was 37.2 ± 15.1 years (range, 21 to 69 years). 16 patients had keratoconus and 1 had Fuchs dystrophy. IVCM was performed on 17 patients preoperatively, and postoperatively on 17 patients at 1 month, 16 patients at 3 months, 11 patients at 6 months, and 11 patients at 12 months. There were no surgical complications. One patient developed an allograft rejection 2 months after surgery. No donor cornea parameters correlated with IVCM findings of wound healing. Cumulative data from evaluation of pre- and postoperative IVCM scans are shown in Table 1.
Table 1.
In vivo confocal microscopy (IVCM) findings after femtosecond laser-assisted keratoplasty (FLAK)
| Preoperative | 1 month | 3 months | 6 months | 12 months | |||
|---|---|---|---|---|---|---|---|
| Keratocyte activation Mean (SD) | Central | 0.41 (0.62) | 1.73 (1.03) | 1.53 (0.83) | 1.09 (0.54) | 0.91 (0.54) | |
| Peripheral | 0.47 (0.52) | 1.57 (1.09) | 1.15 (0.69) | 1.00 (0.63) | 1.00 (0.67) | ||
| Dendritic cells Mean (SD) | Central | 0.71 (0.83) | 1.33 (0.98) | 0.86 (1.10) | 0.36 (0.81) | 0.55 (0.69) | |
| Peripheral | 0.79 (0.70) | 1.42 (0.90) | 1.18 (0.87) | 0.45 (0.69) | 0.60 (1.07) | ||
| Corneal nerves N (%) | Central | Subepi | 14 (93.3%) | 1 (6.7%) | 0 (0%) | 0 (0%) | 5 (45.5%) |
| Stromal | 16 (94.1%) | 3 (20%) | 6 (40%) | 4 (36.4%) | 4 (40%) | ||
| Peripheral | Subepi | 14 (93.3%) | 0 (0%) | 3 (27.3%) | 1 (9.1%) | 3 (30%) | |
| Stromal | 16 (94.1%) | 6 (42.9%) | 6 (40%) | 5 (45.5%) | 4 (40%) | ||
| Needle-like opacities N (%) | Central | 15 (88.2%) | 14 (87.5%) | 16 (100%) | 9 (81.8%) | 10 (90.9%) | |
| Peripheral | 16 (100%) | 12 (85.7%) | 13 (86.7%) | 11 (100%) | 10 (100%) | ||
| Microdots N (%) | Central | 9 (52.9%) | 11 (68.8%) | 8 (53.3%) | 8 (72.7%) | 10 (90.9%) | |
| Peripheral | 10 (66.7%) | 11 (78.6%) | 9 (60%) | 8 (72.7%) | 7 (70%) | ||
Abbreviations: SD = standard deviation; N = number; subepi = subepithelial
Keratocyte activation
Low grade keratocyte activation was present preoperatively on both the central and peripheral corneal scans. The mean keratocyte activation grade increased significantly from preoperative levels to 1 month postoperatively on both central (0.41 ± 0.62 to 1.73 ± 1.03, p<0.001) and peripheral (0.47 ± 0.52 to 1.57 ± 1.09, p=0.002) scans, then gradually decreased through 12 months on both central (0.91 ± 0.54) and peripheral (1.00 ± 0.67) scans, but did not return to preoperative values (p=0.03 and 0.05, respectively).
Dendritic cells
Mean dendritic cell grade also increased from preoperative levels to 1 month postoperatively on both central (0.71 ± 0.83 to 1.33 ± 0.98, p=0.08) and peripheral (0.79 ± 0.70 to 1.42 ± 0.90, p=0.06) evaluation, then decreased from 1 to 6 months. There was a slight increase in presence of dendritic cells from 6 to 12 months on both central (0.36 ± 0.81 to 0.55 ± 0.69) and peripheral (0.45 ± 0.69 to 0.60 ± 1.07) scans. Mean dendritic cell grade was slightly greater in the periphery than in the central cornea at all time points. There was a significant association between the degree of keratocyte activation and dendritic cells in the central cornea at 6 (p=0.05) and 12 months (p=0.01).
The only patient who had grade 3 dendritic cells in the central cornea at 1 and 3 months postoperatively was also the only patient who developed endothelial allograft rejection in this cohort. The patient maintained a clear cornea and quiet anterior chamber until 4 months after FLAK at which time she developed clinical signs of rejection. Since then, she has had a prolonged course with difficult to treat rejection. She continued to exhibit grade 3 dendritic cells at her 12 month confocal evaluation.
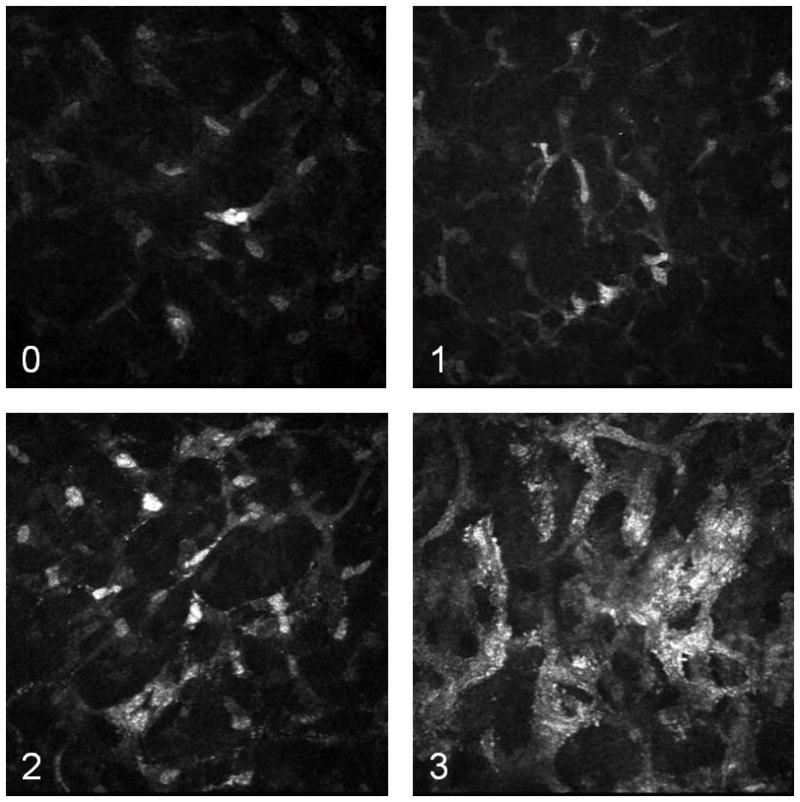
Reinnervation
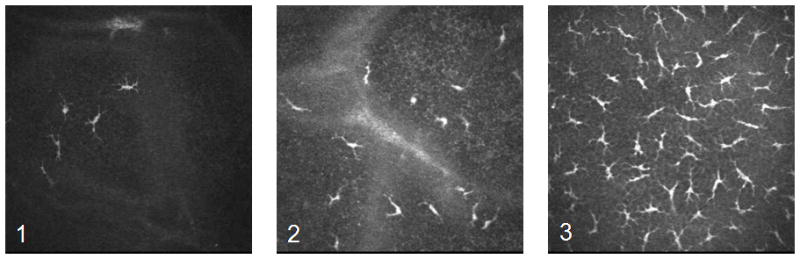
Preoperatively, the subepithelial nerve plexus and stromal nerves were identified in all eyes. Postoperatively, stromal reinnervation was seen prior to regeneration of subepithelial nerves in both the central (p=0.01) and peripheral (p=0.002) cornea (Figure 4). Stromal nerves were seen in 20% (3/15) of central scans and 42.9% (6/14) of peripheral scans at 1 month postoperatively, and remained present on subsequent evaluations through 12 months of follow up. Subepithelial nerves were present in the peripheral cornea in 3 patients at 3 months, and 7 (63.6%) patients at 12 months, including 5 (45.5%) patients with central subepithelial nerves. The postoperative subepithelial and stromal nerves were morphologically quite distinct from the preoperative nerve appearance with increased nerve tortuosity, branching, and beading, as well as more variable nerve diameter (Figure 5).
Figure 4.
Corneal Reinnervation. Kaplan-Meier survival curves of central (top) and peripheral (bottom) corneal reinnervation showing stromal nerve regeneration preceding presence of subepithelial nerves. Of note, stromal nerves were observed as early as 1 month after surgery.
Figure 5.
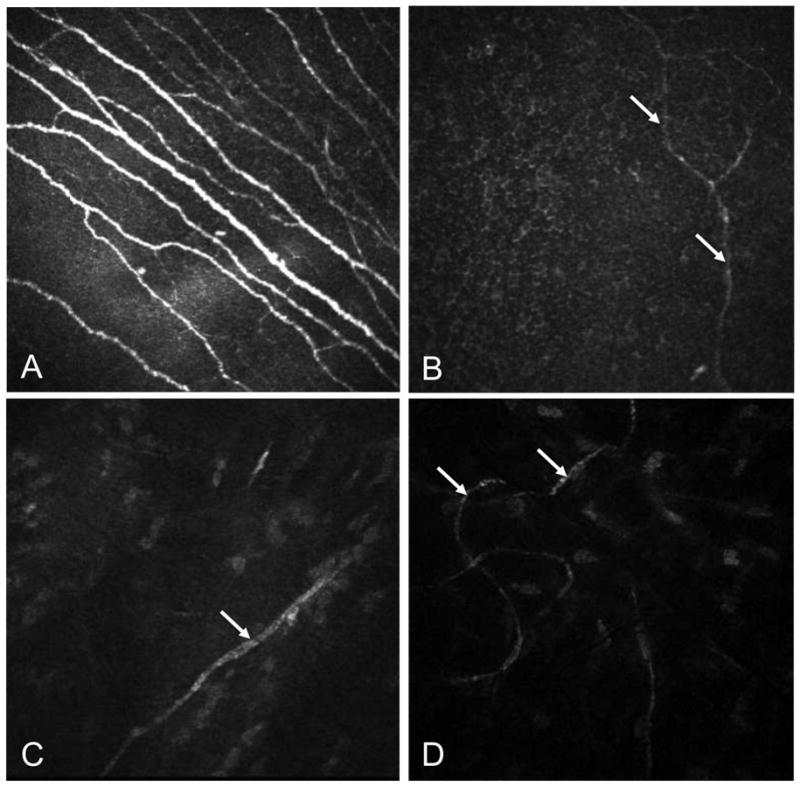
Corneal Nerve Morphology. In vivo confocal microscopy shows irregular morphology of the nerves regenerating after femtosecond laser-assisted keratoplasty. Subepithelial nerves A. preoperatively and B. 1 year postoperatively show marked reduction of nerve density, thinner diameter, and increased tortuosity. Stromal nerves C. preoperatively and D. 1 year postoperatively also show thinner diameter and increased tortuosity.
Needle-like opacities and microdots
Needle-like opacities were present in almost all IVCM examinations in this cohort (range, 81.8% to 100%). The presence of corneal microdots in the central cornea increased from preoperative (50%) to postoperative (90.9%) time points.
Discussion
In this study, we used IVCM to longitudinally evaluate corneal inflammation and wound healing at the cellular level in the first year after FLAK. We examined corneas for degree of keratocyte activation, number of dendritic cells, presence of subepithelial and stromal nerves, needle-like opacities, and microdots in both the central and peripheral cornea.
Keratocyte activation after corneal procedures using the femtosecond laser has been previously described. Keratocyte activation represents cells transitioning to a repair phenotype commonly observed postoperatively.20,21 Our findings confirm that keratocyte activation increases significantly following surgery in both the central (p<0.001) and peripheral (p=0.002) cornea. The level of activation then decreases over time, but it is unknown whether activated keratocytes can completely return to their original state, or whether they remain permanently biochemically altered.19 In addition, the preoperative scans of eyes with keratoconus in our cohort all showed some degree of keratocyte activation, a finding that is consistent with previous IVCM findings in keratoconus.35
Epithelial dendritic cells are believed to participate in cell-mediated immunity in inflammatory conditions.21 We observed an expected increase in dendritic cells immediately after surgery, followed by a substantial decrease until 6 months, and subsequently a slight increase from 6 to 12 months postoperatively. We hypothesize that the decrease in dendritic cells after the initial surgery-induced rise corresponds to decreased inflammation as corneal wound healing progresses, and that the increase in dendritic cells after 6 months is associated with a sub-clinical increase in corneal inflammation as topical corticosteroid eye drops are tapered. There was a significant association between the degree of keratocyte activation and dendritic cells in individual eyes at both 6 (p=0.05) and 12 (p=0.01) months, suggesting a common pathway of corneal inflammation leading to both of these IVCM findings.
Increased levels of epithelial dendritic cells have been observed in the setting of corneal transplant rejection.14 In our study, the only eye that exhibited high grade dendritic cells at both 1 and 3 months postoperatively developed early allograft rejection. Although not readily available in all cornea practices, there may be a role for postoperative IVCM dendritic cell evaluation as a useful adjunct for evaluating subclinical corneal inflammation and identifying patients at risk for rejection who might benefit from more aggressive corticosteroid treatment.
Corneal nerves are disrupted by surgical incisions, and the large circumferential incision in PK causes complete central corneal denervation. Previous IVCM studies have shown great variability in the rate of reinnervation after conventional PK.15–18 In a 3-year study of 46 grafts, Richter et al. observed stromal and subepithelial nerves in the peripheral cornea at 2 and 3 months after surgery, and in the central graft at 7 and 24 months after surgery, respectively.15 Other IVCM studies of corneal reinnervation after conventional PK are limited to central corneal evaluation and/or cross-sectional rather than longitudinal evaluation. In our patient cohort, we observed earlier reinnervation after FLAK than has been previously reported for PK. Stromal nerves were identified in several patients as early as 1 month postoperatively. One eye was identified as having central subepithelial nerves at 1 month postoperatively, but none were noted to have subepithelial nerves at the 3 or 6 month evaluation. In light of this discrepancy, it is possible that the 1 month scan was misinterpreted, and actually demonstrated a morphologically similar structure (e.g. long processes from a mature dendritic cell). Excluding this anomaly, subepithelial reinnervation was seen in 3 patients peripherally at 3 months, and in 5 patients centrally by 1 year postoperatively, still earlier than has been previously reported. The altered nerve morphology that we observed in our cohort (Figure 5) has been previously noted after PK, even many years postoperatively. 15–18
The rate of postoperative nerve fiber regeneration has been shown to depend on both the depth and circumference of the corneal incision.36 We suspect that this rate is also affected by other characteristics of corneal incisions, and that the accelerated nerve regeneration we observed is an indicator of improved corneal healing after FLAK. This observation could be related to shaped trephination allowing for better wound apposition, or less collateral damage by the femtosecond laser as compared to potential crush injury from the mechanical trephine. Further research is needed to specifically investigate whether differently shaped trephination or modified femtosecond laser settings affect the rate of corneal reinnervation after FLAK.
Needle-like opacities have been described in a variety of settings, including noninfectious keratitis, corneal edema, and after conventional PK. 13,23,24 It has been proposed that they may represent disorganized extracellular matrix, collagen lamellae, or transitional keratocytes. In our study, needle like opacities were seen in almost all evaluations, both before and after surgery, making their clinical significance difficult to ascertain.
Corneal microdots were first described in the setting of long-term contact lens wear,22 although similar hyperreflective particles have also been described after LASIK, DSAEK, and PK.12,13,24 Histologic and ultrastructural correlation of these particles indicate that they are a combination of intracellular and extracellular debris, and degenerating cellular material.37 Microdots were present in half of our patients preoperatively, and increased to 90% by 1 year postoperatively. The clinical significance of corneal microdots remains unclear.
Although this study is limited by relatively small sample size, it is unique in its presentation of a longitudinal, prospective evaluation of IVCM findings before and after corneal transplantation, specifically using a femtosecond laser for shaped trephination. While IVCM image interpretation can be somewhat subjective, our grading scheme was well defined, gradings were performed on images that were randomized with respect to time sequence, and repeat testing of 25% of the scans demonstrated good interobserver reliability (κ=0.62 to 0.86). IVCM is a powerful tool for improving understanding of corneal wound healing in the postoperative period. We hope that grading schemes for IVCM findings, such as the ones used in this study, can be validated and broadly adopted for future comparison of independently conducted studies.
In summary, IVCM after FLAK provides important information about postoperative corneal inflammation and wound healing. Corneal inflammation increases dramatically after surgery, followed by a gradual decrease towards preoperative levels, as seen by the IVCM measures of keratocyte activation and dendritic cells. Our findings suggest improved corneal wound healing after FLAK as compared to conventional PK, as evidenced by earlier regrowth of corneal nerves in both the peripheral and central cornea. Further study is needed to better characterize IVCM findings after FLAK in order to facilitate further comparison with conventional PK and to improve understanding of corneal wound healing after this novel procedure.
Acknowledgments
Financial Support: This study was supported by NIH/NEI EY017885 (RMS), Michigan Institute for Clinical and Health Research New Pilot Clinical Trial Training Grant (UL1RR024986), Midwest Eye Banks, and a departmental grant from Research to Prevent Blindness, Inc. New York, NY. The funding agencies had no role in design or conduct of this research. No authors have proprietary interest in the materials described in the manuscript.
Footnotes
Meeting Presentation: Presented in part at the World Cornea Congress April 2010, Boston, MA, USA
References
- 1.Thompson RW, Jr, Price MO, Bowers PJ, et al. Long-term graft survival after penetrating keratoplasty. Ophthalmology. 2003;110:1396–402. doi: 10.1016/S0161-6420(03)00463-9. [DOI] [PubMed] [Google Scholar]
- 2.Naumann GOH, Seitz B, Lang GK, et al. 193 excimer laser trephination in perforating keratoplasty. Report of 70 patients. Klin Monatsbl Augenheilkd. 1993;203:252–61. doi: 10.1055/s-2008-1045677. [DOI] [PubMed] [Google Scholar]
- 3.Seitz B, Langenbucher A, Kus MM, et al. Non-mechanical corneal trephination with the excimer laser improves outcome after penetrating keratoplasty. Ophthalmology. 1999;106:1156–64. doi: 10.1016/S0161-6420(99)90265-8. [DOI] [PubMed] [Google Scholar]
- 4.Jonas JB, Vossmerbaeumer U. Femtosecond laser penetrating keratoplasty with conical incisions and positional spikes. J Refract Surg. 2004;20:397. doi: 10.3928/1081-597X-20040701-15. [DOI] [PubMed] [Google Scholar]
- 5.Ignacio TS, Nguyen TB, Chuck RS, et al. Top hat wound configuration for penetrating keratoplasty using the femtosecond laser: a laboratory model. Cornea. 2006;25:336–40. doi: 10.1097/01.ico.0000179739.31196.e8. [DOI] [PubMed] [Google Scholar]
- 6.Steinert RF, Ignacio TS, Sarayba MA. “Top hat”-shaped penetrating keratoplasty using the femtosecond laser. Am J Ophthalmol. 2007;143:689–91. doi: 10.1016/j.ajo.2006.11.043. [DOI] [PubMed] [Google Scholar]
- 7.Bahar I, Kaiserman I, Lange AP, et al. Femtosecond laser versus manual dissection for top hat penetrating keratoplasty. Br J Ophthalmol. 2009;93:73–8. doi: 10.1136/bjo.2008.148346. [DOI] [PubMed] [Google Scholar]
- 8.Farid M, Steinert RF, Gaster RN, et al. Comparison of penetrating keratoplasty performed with a femtosecond laser zig-zag incision versus conventional blade trephination. Ophthalmology. 2009;116:1638–43. doi: 10.1016/j.ophtha.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Bahar I, Kaiserman I, McAllum P, et al. Femtosecond laser-assisted penetrating keratoplasty: stability evaluation of different wound configurations. Cornea. 2008;27:209–11. doi: 10.1097/ICO.0b013e31815b7d50. [DOI] [PubMed] [Google Scholar]
- 10.Malta JB, Soong HK, Shtein R, et al. Femtosecond laser-assisted keratoplasty: laboratory studies in eye bank eyes. Curr Eye Res. 2009;34:18–25. doi: 10.1080/02713680802535255. [DOI] [PubMed] [Google Scholar]
- 11.Bourne WM. Cellular changes in transplanted human corneas. Cornea. 2001;20:560–9. doi: 10.1097/00003226-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Hollingsworth JG, Efron N, Tullo AB. A longitudinal case series investigating cellular changes to the transplanted cornea using confocal microscopy. Cont Lens Anterior Eye. 2006;29:135–41. doi: 10.1016/j.clae.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 13.Szaflik JP, Kaminska A, Udziela M, et al. In vivo confocal microscopy of corneal grafts shortly after penetrating keratoplasty. Eur J Ophthalmol. 2007;17:891–6. doi: 10.1177/112067210701700604. [DOI] [PubMed] [Google Scholar]
- 14.Niederer RL, Sherwin T, McGhee CN. In vivo confocal microscopy of subepithelial infiltrates in human corneal transplant rejection. Cornea. 2007;26:501–4. doi: 10.1097/ICO.0b013e3180318107. [DOI] [PubMed] [Google Scholar]
- 15.Richter A, Slowik C, Somodi S, et al. Corneal reinnervation following penetrating keratoplasty-correlation of esthesiometry and confocal microscopy. Ger J Ophthalmol. 1996;5:513–7. [PubMed] [Google Scholar]
- 16.Darwish T, Brahma A, Efron N, et al. Subbasal nerve regeneration after penetrating keratoplasty. Cornea. 2007;26:935–40. doi: 10.1097/ICO.0b013e3180de493f. [DOI] [PubMed] [Google Scholar]
- 17.Niederer RL, Perumal D, Sherwin T, et al. Corneal innervation and cellular changes after corneal transplantation: an in vivo confocal microscopy study. Invest Ophthalmol Vis Sci. 2007;48:621–626. doi: 10.1167/iovs.06-0538. [DOI] [PubMed] [Google Scholar]
- 18.Patel SV, Erie JC, McLaren JW, et al. Keratocyte density and recovery of subbasal nerves after penetrating keratoplasty and in late endothelial failure. Arch Ophthalmol. 2007;125:1693–8. doi: 10.1001/archopht.125.12.1693. [DOI] [PubMed] [Google Scholar]
- 19.Fini EM. Keratocyte and fibroblast phenotypes in repairing cornea. Prog Retin Eye Res. 1999;18:529–51. doi: 10.1016/s1350-9462(98)00033-0. [DOI] [PubMed] [Google Scholar]
- 20.Zhivov A, Stave J, Vollmar B, et al. In vivo confocal microscopic evaluation of Langerhans cell density and distribution in the normal human corneal epithelium. Graefes Arch Clin Exp Ophthalmol. 2005;243:1056–61. doi: 10.1007/s00417-004-1075-8. [DOI] [PubMed] [Google Scholar]
- 21.Mastropasqua L, Nubile M, Lanzini M, et al. Epithelial dendritic cell distribution in normal and inflamed human cornea: in vivo confocal microscopy study. Am J Ophthalmol. 2006;142:736–44. doi: 10.1016/j.ajo.2006.06.057. [DOI] [PubMed] [Google Scholar]
- 22.Böhnke M, Masters BR. Long-term contact lens wear induces a corneal degeneration with microdot deposits in the corneal stroma. Ophthalmology. 1997;104:1887–96. doi: 10.1016/s0161-6420(97)30011-6. [DOI] [PubMed] [Google Scholar]
- 23.Kobayashi A, Maeda A, Sugiyama K. In vivo confocal microscopy in the acute phase of corneal inflammation. Ophthalmic Surg Lasers Imaging. 2003;34:433–6. [PubMed] [Google Scholar]
- 24.Kobayashi A, Mawatari Y, Yokogawa H, et al. In vivo laser confocal microscopy after Descemet stripping with automated endothelial keratoplasty. Am J Ophthalmol. 2008;145:977–985. doi: 10.1016/j.ajo.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 25.Sonigo B, Iordanidou V, Chong-Sit D, et al. In vivo corneal confocal microscopy comparison of IntraLase femtosecond laser and mechanical microkeratome for laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2006;47:2803–11. doi: 10.1167/iovs.05-1207. [DOI] [PubMed] [Google Scholar]
- 26.Javaloy J, Vidal MT, Abdelrahman AM, et al. Confocal microscopy comparison of IntraLase femtosecond laser and Moria M2 microkeratome in LASIK. J Refract Surg. 2007;23:178–87. doi: 10.3928/1081-597X-20070201-10. [DOI] [PubMed] [Google Scholar]
- 27.Patel SV, Maguire LJ, McLaren JW, et al. Femtosecond laser versus mechanical microkeratome for LASIK: a randomized controlled study. Ophthalmology. 2007;114:1482– 90. doi: 10.1016/j.ophtha.2006.10.057. [DOI] [PubMed] [Google Scholar]
- 28.Ramírez M, Hernández-Quintela E, Naranjo-Tackman R. A comparative confocal microscopy analysis after LASIK with the IntraLase femtosecond laser vs Hansatome microkeratome. J Refract Surg. 2007;23:305–7. doi: 10.3928/1081-597X-20070301-15. [DOI] [PubMed] [Google Scholar]
- 29.Meltendorf C, Burbach GJ, Bühren J, et al. Corneal femtosecond laser keratotomy results in isolated stromal injury and favorable wound-healing response. Invest Ophthalmol Vis Sci. 2007;48:2068–75. doi: 10.1167/iovs.06-1150. [DOI] [PubMed] [Google Scholar]
- 30.McCulley JP, Petroll WM. Quantitative assessment of corneal wound healing following IntraLASIK using in vivo confocal microscopy. Trans Am Ophthalmol Soc. 2008;106:84–90. [PMC free article] [PubMed] [Google Scholar]
- 31.Mosca L, Fasciani R, Tamburelli C, et al. Femtosecond laser-assisted lamellar keratoplasty: early results. Cornea. 2008;27:668–72. doi: 10.1097/ICO.0b013e31816736b1. [DOI] [PubMed] [Google Scholar]
- 32.Petroll WM, Bowman RW, Cavanagh HD, et al. Assessment of keratocyte activation following LASIK with flap creation using the IntraLase FS60 laser. J Refract Surg. 2008;24:847–9. doi: 10.3928/1081597x-20081001-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang ZY, Chu RY, Zhou XT, et al. Morphologic and histopathologic changes in the rabbit cornea produced by femtosecond laser-assisted multilayer intrastromal ablation. Invest Ophthalmol Vis Sci. 2009;50:2147–53. doi: 10.1167/iovs.08-2400. [DOI] [PubMed] [Google Scholar]
- 34.Nubile M, Carpineto P, Lanzini M, et al. Femtosecond laser arcuate keratotomy for the correction of high astigmatism after keratoplasty. Ophthalmology. 2009;116:1083–92. doi: 10.1016/j.ophtha.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 35.Hollingsworth JG, Bonshek RE, Efron N. Correlation of the appearance of the keratoconic cornea in vivo by confocal microscopy and in vitro by light microscopy. Cornea. 2005;24:397–405. doi: 10.1097/01.ico.0000151548.46231.27. [DOI] [PubMed] [Google Scholar]
- 36.Chang-Ling T, Vannas A, Holden BA, O’Leary DJ. Incision depth affects the recovery of corneal sensitivity and neural regeneration in the cat. Invest Ophthalmol Vis Sci. 1990;31:1533–41. [PubMed] [Google Scholar]
- 37.Dawson DG, Holley GP, Geroski DH, et al. Ex vivo confocal microscopy of human LASIK corneas with histologic and ultrastructural correlation. Ophthalmology. 2005;112:634–44. doi: 10.1016/j.ophtha.2004.10.040. [DOI] [PubMed] [Google Scholar]