Abstract
Objective
To determine whether racial and ethnic minorities were less likely to meet the Medicare Part D eligibility criteria for medication therapy management (MTM) services compared with whites among the adult non-Medicare population, because some non-Medicare health plans have followed the Medicare example.
Design
Cross-sectional observational study.
Setting
United States, 2007–08.
Patients
16,691 white, 5,923 black, and 9,242 Hispanic adults (>17 years) among the non-Medicare population.
Intervention
Analysis of the Medical Expenditure Panel Survey. MTM eligibility criteria used by Part D plans in 2008 and 2010–11 were examined. Main and sensitivity analyses were conducted to represent the entire range of the eligibility thresholds used by Part D plans. Analyses also were conducted among individuals with heart disease, diabetes, and hypertension.
Main outcome measures
Proportions and odds of patients meeting Part D MTM eligibility criteria.
Results
According to the main analysis examining 2008 eligibility criteria, whites had a higher proportion of eligible individuals than did blacks (3.73% vs. 2.57%) and Hispanics (1.53%, P < 0.05 for both comparisons). According to survey-weighted logistic regression adjusting for patient characteristics, blacks and Hispanics had odds ratios for MTM eligibility of 0.60 (95% CI 0.46–0.79) and 0.54 (0.40–0.72), respectively, compared with whites. Sensitivity analyses, analyses examining 2010–11 eligibility criteria, and analyses among individuals with heart disease, diabetes, and hypertension produced similar findings.
Conclusion
Racial and ethnic minorities have lower odds for meeting Part D MTM eligibility criteria than whites among the adult non-Medicare population. MTM eligibility criteria need to be modified to address these disparities.
Keywords: Medication therapy management services, eligibility criteria, health disparities
The Medicare Prescription Drug, Improvement, and Modernization Act (MMA) implemented in 2006 provided an outpatient prescription drug (Part D) benefit program for Medicare beneficiaries.1,2 According to MMA, the Centers for Medicare & Medicaid Services (CMS) also requires prescription drug plans to offer medication therapy management (MTM) services as part of the Part D benefit. The purpose of providing MTM services to Medicare beneficiaries is to “ensure that covered Part D drugs prescribed to targeted beneficiaries are appropriately used to optimize therapeutic outcomes through improved medication use.”1 Part D plans were required to target only enrollees who “have multiple chronic conditions,” “are taking multiple Part D drugs,” and “are likely to incur annual costs for covered Part D drugs that exceed … (an) initial cost threshold of $4,000.”1,2 The eligibility criteria for MTM services are flexible, and Part D plans can determine their own MTM eligibility criteria within the legislative framework. According to a CMS report, MTM eligibility thresholds used by Part D plans had the following patterns in 2008: the thresholds based on the number of Part D drugs ranged from 2 to 15 (median = 5), the thresholds based on number of chronic conditions ranged from 2 to 5 (median = 3), and the threshold based on Part D drug costs was constant at $4,000.2 In the Call Letter for 2010–11 in which CMS specified requirements for Part D plans to bid for contracts, CMS lowered the allowable minimum MTM eligibility thresholds to no more than eight Part D drugs, three chronic conditions, and $3,000 in drug costs.2,3
MTM services are particularly beneficial for individuals with chronic conditions in whose management pharmaco-therapy plays an important role.4 Minorities in particular need MTM services because some chronic conditions targeted by MTM programs are more prevalent among minorities.2,3,5–8 However, a recently published study based on data analyses of historical data before Part D implementation reported that racial and ethnic minorities would be less likely than whites to be eligible for MTM services. Specifically, that study reported that the adjusted odds for blacks meeting Part D MTM eligibility criteria were 40% to 64% lower than for whites (P < 0.05) and adjusted odds for Hispanics meeting Part D MTM eligibility criteria were 54% to 87% lower than for whites (P < 0.05).2
These findings are not surprising. Two of the three eligibility criteria for MTM services are based on the use and costs of prescription drugs. Racial and ethnic minorities historically tend to use fewer prescription drugs and health services and incur lower costs on prescription drugs and health services than do whites among the Medicare population.9–11 Therefore, utilization-based eligibility criteria would disproportionately exclude minorities from MTM services. Although the third eligibility criterion is based on the number of chronic conditions, a measure of health status, it is arguably based on the use of health services as well because medical conditions can be diagnosed only when seeking health care.
The disparity implications of MTM services are not limited to Medicare beneficiaries. Medicare is the largest regulator and purchaser of health care in the United States, so Medicare policies are oftentimes imitated by other health insurance programs.12 Therefore, prescription drug insurance programs other than those for Medicare Part D have implemented MTM services for their beneficiaries.13–15 While racial and ethnic minorities have been reported to use fewer prescription drugs and incur lower drug costs than do whites among the non-Medicare population,16–20 some plans for the adult non-Medicare population have included in their MTM eligibility criteria components similar to part D MTM eligibility criteria, such as number of chronic conditions and number of prescription drugs.13–15
Objective
The overall objective of this study was to examine whether racial and ethnic disparities exist in meeting Part D MTM eligibility criteria among the adult non-Medicare population. We conducted this study to test the disparity implications of Medicare Part D MTM eligibility criteria among the adult non-Medicare population. Specifically, we examined disparity patterns according to the Part D eligibility criteria for 2008 and for 2010–11. We also examined these disparity implications among individuals with hypertension, heart disease, and diabetes. This study defined disparities as racial and ethnic differences in meeting Part D MTM eligibility criteria after statistically adjusting for patient characteristics that might contribute to those differences.21 Most studies on racial and ethnic disparities take this approach.21 Hypertension, heart disease, and diabetes are among the most frequently targeted chronic conditions by MTM services for Medicare and non-Medicare plans.2,3,13–15,22 They are also priority conditions that federal initiatives have identified for disparity elimination.23
Methods
This study analyzed the adult (>17 years) non-Medicare population from the Medical Expenditure Panel Survey (MEPS; 2007–08).24 Medicare beneficiaries were excluded from the analysis. MEPS is a federal survey cosponsored by the Agency for Healthcare Research and Quality and the National Center for Health Statistics.24 This survey collects information from a sample of nationally representative, noninstitutionalized civilians to produce national estimates on health care use and health care expenditures in the United States.24 MEPS oversampled blacks and Hispanics to facilitate reliable estimates on these populations.24
The MEPS data files relevant to this study are publicly available. These files contain person-level information on demographic characteristics, insurance, employment, income, and uses and expenditures for health care services and prescription medications, as well as information on each medical condition reported by each survey respondent and event-level information on all prescribed medications, including but not limited to medication names and National Drug Codes.24
Determination of MTM eligibility and disparity
When determining the disparity implications of the Part D MTM eligibility criteria, because of the wide variation in eligibility thresholds, it is reasonable to examine the ranges of the thresholds represented by the upper limit, median, mode, and lower limit. For example, in 2008, the lower limit, median, mode, and upper limit of the Part D eligibility thresholds for the criterion based on the number of prescription drugs were 2, 5, 5, and 15, respectively; the lower limit, median, mode, and upper limit of the Part D eligibility thresholds for the criterion based on the number of chronic conditions were 2, 3, 2, and 5, respectively; and the cost thresholds were $4,000.2 Because an individual must meet all three criteria to be eligible for MTM services and there were three unique values representing the range of the thresholds for the criterion based on the number of prescription drugs, three unique values representing the range of the thresholds for the criterion based on the number of chronic conditions, and one value for the threshold based on drug cost, we then had to determine the disparity implications of 3 × 3 × 1 = 9 different combinations of these thresholds. We analyzed the combinations represented by the modes (five Part D drugs, two chronic conditions, and $4,000 in drug costs) in the main analysis of this study. All other combinations were analyzed in eight sensitivity analyses. Because Part D plans used the cost threshold of $4,000 in 2007 and in 2008, there was no need to convert 2008 cost threshold to 2007 dollars when using 2007 data.
When analyzing Part D eligibility thresholds for 2010 and 2011, we used methods similar to the testing of the Part D eligibility criteria for 2008. For 2010–11, the lower limit, median, mode, and upper limits of the Part D eligibility thresholds for the criterion based on the number of Part D drugs were 2, 5, 8, and 8, respectively.3,23 For the criterion based on the number of chronic conditions, the lower limit, median, mode, and upper limits of the Part D eligibility thresholds were 2, 3, 3, and 3, respectively.3,23 Therefore, we had to analyze only 3 × 2 × 1 = 6 combinations of thresholds for 2010–11 criteria. We analyzed the combination of the thresholds represented by eight Part D drugs, three chronic conditions, and $3,000 in Part D drug costs in the main analysis. All other combinations were included in the sensitivity analyses.
To determine MTM eligibility according to the criteria based on number of drugs and drug costs, the necessary information was directly available in MEPS.24 Determining eligibility based on the number of chronic conditions was based on a raw count of chronic conditions among a list of 25 chronic conditions.25 Daniel and Malone compiled this list of chronic conditions applicable to Medicare beneficiaries.25 Because the list includes all major chronic conditions targeted in MTM programs for the non-Medicare population, we used the same list here to determine MTM eligibility among the non-Medicare population. Furthermore, to identify chronic conditions in MEPS, we used existing Clinical Classification categories.24 Heart diseases in this study included all cardiovascular diseases, such as pulmonary heart disease, congestive heart failure, and conduction disorders.24
Data analyses
To examine racial and ethnic disparities in meeting Part D MTM eligibility criteria, we used chi-square tests to compare proportions of MTM-eligible individuals across racial and ethnic groups. Logistic regression was used to compare the odds of meeting Part D MTM eligibility criteria across racial and ethnic groups. Because the dependent variables may be affected by individual sociodemographic and health-related characteristics, we controlled for the effects of these characteristics in the regression models. Because Part D MTM eligibility criteria are based primarily on the use of drugs and health services, we used selected aspects of Andersen’s Behavioral Model in Health Services Utilization in determining the inclusion of the following patient characteristics in the regression models: predisposing factors, enabling factors, and need factors.26 Predisposing factors included age, gender, and marital status. Enabling factors included highest degree received, income, insurance status, metropolitan statistical area, and geographic regions.26 Among patient characteristics included in the model, insurance, income, and education (highest degree achieved) variables may be correlated. Therefore, to ensure the reliability of the estimates, we analyzed various models. In addition to using a saturated model including all insurance, income, and education variables, this study analyzed models with six different combinations of these variables, including one model for each group of these variables (e.g., health insurance variables) and one model for each combination of two groups of these variables (e.g., health insurance and education variables).
For results interpretation, we looked to odds ratios (ORs), estimated as the natural antilogarithm of coefficients for dummy variables for blacks and Hispanics, for indications of racial and ethnic disparities. An OR less than 1 indicates that blacks or Hispanics had a lower likelihood of being eligible for MTM than did whites. All data analyses in this study took into account the complex survey design of MEPS, including primary sampling units, strata, and personal weights. We conducted data analyses using the survey data analysis procedures in SAS version 9.2 (SAS Institute, Cary, NC). The statistical significance level was set a priori at 0.05. Institutional Review Board (IRB) exemption was obtained from the University of Tennessee IRB office.
Results
The final study sample included 16,691 whites (weighted to 242,241,014), 5,923 blacks (weighted to 43,484,164), and 9,242 Hispanics (weighted to 55,604,436), representing 52.4%, 18.59%, and 29.01% of the sample, respectively. The sociodemographic characteristics of the population varied across racial and ethnic groups (Table 1). Higher percentages of the population existed in the older age groups among whites than among blacks and Hispanics (P < 0.0001 for both comparisons). Whites had a higher proportion of males than did blacks (P = 0.0001) and a lower proportion of males than Hispanics (P = 0.0012). A higher proportion of whites was married than were blacks and Hispanics (P < 0.0001 for both comparisons). A higher proportion of whites had private insurance than did blacks and Hispanics, while lower proportions of whites than blacks and Hispanics had public insurance only or had no insurance (P < 0.0001 for the differences between whites and blacks and the differences between whites and Hispanics). A higher proportion of whites were in the higher income categories than were blacks and Hispanics (P < 0.0001 for both comparisons). Among whites, a higher proportion of the population achieved higher degrees than did blacks and Hispanics (P < 0.0001 for both comparisons). The geographic distributions also varied across racial and ethnic groups. The two regions where the highest proportions of whites resided were the South and Midwest. The two regions where the highest proportions of blacks resided were the South (where as many as 56.33% of blacks resided) and Midwest. The two regions where the highest proportions of Hispanics resided were the South and West (where almost 80% of Hispanics resided). A lower proportion of whites resided in metropolitan statistical areas than did blacks and Hispanics (P < 0.0001 for both comparisons). Regarding health status, whites had higher proportions in better health categories than did blacks and Hispanics (P < 0.0001 for both comparisons).
Table 1.
Sociodemographic characteristics across racial and ethnic groups within the study population
| Characteristic | Non-Hispanic whites No. (%) |
Non-Hispanic blacks No. (%) |
Hispanics No. (%) |
|---|---|---|---|
| Age (years) | |||
| 18–30 | 4,202 (26.70) | 1,911 (33.22) | 3,261 (36.89) |
|
| |||
| 31–40 | 3,383 (19.67) | 1,254 (21.49) | 2,407 (25.86) |
|
| |||
| 41–50 | 3,973 (23.16) | 1,330 (21.98) | 1,985 (20.86) |
|
| |||
| >50 | 5,133 (30.47) | 1,428 (23.30) | 1,589 (16.39) |
|
| |||
| Gender | |||
| Female | 8,678 (50.37) | 3,460 (53.90) | 4,892 (47.68) |
|
| |||
| Male | 8,013 (49.63) | 2,463 (46.10) | 4,350 (52.32) |
|
| |||
| Marital status | |||
| Not married | 6,543 (41.36) | 3,842 (64.85) | 4,107 (48.11) |
|
| |||
| Married | 10,148 (58.64) | 2,081 (35.15) | 5,134 (51.89) |
|
| |||
| Insurance | |||
| Any private | 13,106 (81.12) | 3,446 (63.31) | 3,881 (47.76) |
|
| |||
| Public only | 1,113 (5.12) | 1,127 (15.13) | 1,491 (12.65) |
|
| |||
| No insurance | 2,472 (13.76) | 1,350 (21.56) | 3,870 (39.58) |
|
| |||
| Poverty | |||
| Poor | 1,605 (7.30) | 1,424 (19.28) | 2,072 (18.01) |
|
| |||
| Near poor | 533 (2.40) | 351 (4.72) | 780 (6.69) |
|
| |||
| Low income | 1,745 (9.28) | 1,120 (15.47) | 2,166 (20.13) |
|
| |||
| Middle income | 5,162 (30.51) | 1,831 (33.77) | 2,826 (33.33) |
|
| |||
| High income | 7,646 (50.51) | 1,197 (26.77) | 1,398 (21.84) |
|
| |||
| Highest degree | |||
| Lower than high school | 2,502 (13.30) | 1,562 (22.76) | 4,660 (43.51) |
|
| |||
| GED or high school | 7,624 (45.37) | 2,999 (51.45) | 3,307 (39.22) |
|
| |||
| Bachelor | 3,279 (21.03) | 598 (12.16) | 607 (8.99) |
|
| |||
| Master and higher | 1,644 (10.60) | 259 (5.47) | 184 (2.90) |
|
| |||
| Other | 1,581 (9.69) | 456 (8.16) | 410 (5.37) |
|
| |||
| Region | |||
| Northeast | 2,710 (19.51) | 964 (16.24) | 1,163 (13.99) |
|
| |||
| Midwest | 4,807 (26.62) | 911 (18.07) | 808 (8.15) |
|
| |||
| South | 5,750 (33.65) | 3,560 (56.33) | 3,107 (35.99) |
|
| |||
| West | 3,424 (20.22) | 488 (9.37) | 4,164 (41.87) |
|
| |||
| Metropolitan setting (no) | 3,252 (19.00) | 719 (9.69) | 830 (6.37) |
|
| |||
| Statistical area (yes) | 13,439 (81.00) | 5,204 (90.31) | 8,412 (93.63) |
|
| |||
| Self-perceived health status | |||
| Excellent | 4,834 (30.17) | 1,475 (26.94) | 2,106 (25.51) |
|
| |||
| Very good | 5,853 (35.77) | 1,827 (32.14) | 2,754 (30.90) |
|
| |||
| Good | 4,326 (25.02) | 1,840 (29.57) | 3,074 (31.59 ) |
|
| |||
| Fair | 1,267 (7.01) | 607 (9.05) | 1,102 (10.03) |
|
| |||
| Poor | 390 (2.02) | 155 (2.31) | 197 (1.97) |
Abbreviation used: GED, general educational development.
P < 0.05 for the differences between non-Hispanic whites (whites) and non-Hispanic blacks (blacks) for all variables. P < 0.05 for the difference between whites and Hispanics for all variables.
We compared the proportions of individuals meeting the 2008 eligibility criteria across racial and ethnic groups. According to the main analysis and all eight sensitivity analyses, whites had a higher proportion of eligible individuals than did blacks and Hispanics (Table 2). For example, according to the main analysis, the proportions eligible were 3.73%, 2.57%, and 1.53%, respectively, for whites, blacks, and Hispanics. The proportions of eligible individuals were significantly higher for whites than for blacks and Hispanics (P < 0.05 for the comparison between whites and blacks and the comparison between whites and Hispanics). Almost all sensitivity analyses for the 2008 eligibility criteria produced similar patterns.
Table 2.
Individuals eligible for medication therapy management services across racial and ethnic groups according to the 2008 eligibility criteria
| Analysis | No. of drugs | No. of conditions | Groups | Eligible No. (%) |
|---|---|---|---|---|
| Main analysis a,b | ≥5 | ≥2 | Whites | 677 (3.73) |
| Blacks | 159 (2.57) | |||
| Hispanics | 149 (1.53) | |||
| Sensitivity analysis 1a,b | ≥5 | ≥3 | Whites | 600 (3.27) |
| Blacks | 142 (2.31) | |||
| Hispanics | 130 (1.32) | |||
| Sensitivity analysis 2a,b | ≥5 | ≥5 | Whites | 370 (1.93) |
| Blacks | 78 (1.20) | |||
| Hispanics | 78 (0.69) | |||
| Sensitivity analysis 3a,b | ≥2 | ≥3 | Whites | 633 (3.46) |
| Blacks | 153 (2.43) | |||
| Hispanics | 134 (1.37) | |||
| Sensitivity analysis 4a,b | ≥2 | ≥2 | Whites | 734 (4.09) |
| Blacks | 178 (2.82) | |||
| Hispanics | 162 (1.71) | |||
| Sensitivity analysis 5a,b | ≥2 | ≥5 | Whites | 374 (1.94) |
| Blacks | 80 (1.22) | |||
| Hispanics | 79 (0.71) | |||
| Sensitivity analysis 6b | ≥15 | ≥3 | Whites | 184 (0.91) |
| Blacks | 43 (0.76) | |||
| Hispanics | 30 (0.29) | |||
| Sensitivity analysis 7b | ≥15 | ≥2 | Whites | 188 (0.94) |
| Blacks | 45 (0.80) | |||
| Hispanics | 32 (0.30) | |||
| Sensitivity analysis 8b | ≥15 | ≥5 | Whites | 155 (0.75) |
| Blacks | 32 (0.54) | |||
| Hispanics | 25 (0.22) |
P < 0.05 for the differences between non-Hispanic whites (whites) and non-Hispanic blacks (blacks).
P < 0.05 for the difference between whites and Hispanics.
We also compared the proportions of individuals meeting each individual 2008 eligibility criterion across racial and ethnic groups (Table 3). Whites in general had higher proportions meeting each individual eligibility criterion than did blacks and Hispanics (P < 0.05 for all criteria except P > 0.05 for the comparison between whites and blacks for the criterion based on the number of drugs ≥15).
Table 3.
Individuals eligible for medication therapy management services across racial and ethnic groups according to each eligibility criterion in 2008a
| Criterion | Non-Hispanic whites No. (%) |
Non-Hispanic blacks No. (%) |
Hispanics No. (%) |
|---|---|---|---|
| No. of conditions ≥2a,b | |||
| No | 10,713 (65.37) | 4,281 (73.71) | 7,359 (79.70) |
|
| |||
| Yes | 5,978 (34.63) | 1,642 (26.29) | 1,883 (20.30) |
|
| |||
| No. of conditions ≥3a,b | |||
| No | 13,074 (79.39) | 4,937 (84.53) | 8,224 (89.20) |
|
| |||
| Yes | 3,617 (20.61) | 986 (15.47) | 1,018 (10.80) |
|
| |||
| No. of conditions ≥5a,b | |||
| No | 15,376 (92.79) | 5,611 (95.28) | 8,936 (96.97) |
|
| |||
| Yes | 1,315 (7.21) | 312 (4.72) | 306 (3.03) |
|
| |||
| No. of drugs ≥2a,b | |||
| No | 8,106 (49.37) | 3,452 (58.97) | 6,468 (58.97) |
|
| |||
| Yes | 8,585 (50.63) | 2,471 (41.03) | 2,774 (30.13) |
|
| |||
| No. of drugs ≥5a,b | |||
| No | 13,088 (79.18) | 4,963 (84.56) | 8,285 (89.81) |
|
| |||
| Yes | 3,603 (20.82) | 960 (15.44) | 957 (10.19) |
|
| |||
| No. of drugs ≥15b | |||
| No | 16,412 (98.58) | 5,851 (98.75) | 9,190 (99.54) |
|
| |||
| Yes | 279 (1.42) | 72 (1.25) | 52 (0.46) |
|
| |||
| Drug costs >$4,000a,b | |||
| No | 15,880 (95.45) | 5,717 (96.74) | 9,057 (98.05) |
|
| |||
| Yes | 811 (4.55) | 206 (3.26) | 185 (1.95) |
P < 0.05 for the differences between non-Hispanic whites and non-Hispanic blacks.
P < 0.05 for the differences between non-Hispanic whites and Hispanics.
We used survey-weighted logistic regression to adjust for the effects of sociodemographic characteristics and health status when comparing the odds of meeting 2008 Part D MTM eligibility criteria across racial and ethnic groups in the main analysis. According to the saturated model, blacks and Hispanics had ORs of 0.60 (95% CI 0.46–0.79) and 0.54 (0.40–0.72), respectively. This finding suggests that the odds for blacks and Hispanics to be eligible for MTM services were 40% and 46% lower, respectively, than for whites. Including different combinations of insurance, income, and education variables in the main analysis for 2008 Part D MTM eligibility criteria produced ORs of 0.57–0.62 for blacks and 0.45–0.53 for Hispanics, respectively. These ORs were always statistically significant (P < 0.05).
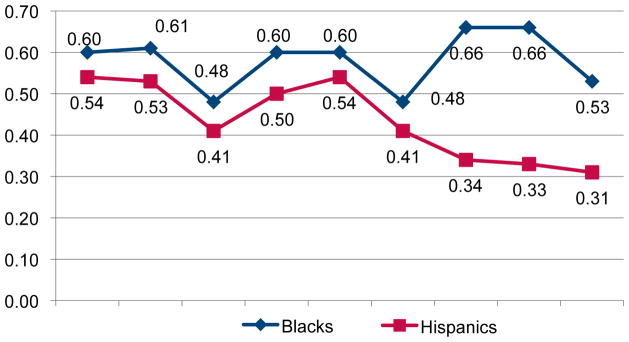
We also conducted multivariate survey-weighted logistic regression for all sensitivity analyses for 2008 eligibility criteria (Figure 1). In all regression analyses for 2008 eligibility criteria, the ORs for blacks to whites were 0.48–0.66 and the ORs for Hispanics to whites were 0.31–0.54 (P < 0.05 for all ORs except ORs for blacks to whites in sensitivity analyses 6 and 7). Including different combinations of insurance, income, and education variables in all regression models for 2008 eligibility criteria produced similar patterns.
Figure 1.
Odds ratios for meeting eligibility criteria for medication therapy management services based on multivariate survey–weighted logistic regression in the main and sensitivity analyses for 2008 eligibility criteria
Abbreviation used: Sensi., sensitivity analysis.
The analyses for 2010 eligibility criteria produced similar results. The ORs for blacks to whites were 0.47–0.54, and the ORs for Hispanics to whites were 0.48–0.52 (P < 0.05 for all ORs). Including different combinations of insurance, income, and education variables produced similar patterns.
The results among individuals with heart disease, diabetes, and hypertension were similar to those in the overall study sample. The patterns of differences in sociodemographic characteristics and health status across racial and ethnic groups were similar to the patterns among the overall study sample. The proportions of eligible individuals for each eligibility criterion among whites were always higher than those among blacks and Hispanics (P < 0.05). We conducted multivariate survey-weighted logistic regression analyses for the main analysis and all sensitivity analyses for 2008 eligibility criteria. In those regression analyses, the ORs for blacks to whites were 0.28–0.47 and the ORs for Hispanics to whites were 0.34–0.59 (P < 0.05 for all ORs). Including different combinations of insurance, income, and education variables produced similar patterns. The analyses for 2010 eligibility criteria among individuals with heart disease, hypertension, and diabetes produced similar results.
Discussion
Based on the analysis of a nationally representative sample of the adult non-Medicare population, we found racial and ethnic disparities in meeting the Part D MTM eligibility criteria among the non-Medicare population. This result held both for 2008 and 2010–11 eligibility criteria. These disparity patterns were true for the overall study sample and for the subpopulation with heart disease, diabetes, and hypertension. Because the population with heart disease, diabetes and hypertension comprises individuals who really need MTM services,2,3,23 disparities in meeting eligibility criteria among this population are even more concerning than are disparities among the general population. These results are consistent with a previous study that reported similar patterns of racial and ethnic disparities among the Medicare population.2
The causes of racial and ethnic disparities in the use of health services and prescription drugs are complicated. They may include differences across racial and ethnic groups in socioeconomic characteristics, literacy levels, knowledge about disease management, trust in the health care system, cultural traditions, and provider and system-level problems.10 Regardless, utilization-based eligibility criteria can lead to greater disparities.
Studies are rare on racial and ethnic disparities stemming from utilization-based eligibility criteria, probably because utilization-based eligibility criteria as causes for disparities are somewhat hidden. One such study reported that blacks with cancer were more likely than whites to be excluded from hospice services despite the fact that blacks were more likely than whites to want hospice services.27 The reason for this pattern was that eligibility criteria for hospice care required that patients give up curative treatment (utilization-based), but blacks had a stronger preference than whites for continuing their cancer treatment.27
This study found that blacks and Hispanics differed from whites in population characteristics. For example, higher proportions of whites belong to older age groups than do blacks and Hispanics. These differences may have contributed to differences in meeting Part D MTM eligibility criteria. However, after we controlled for all relevant patient characteristics existing in MEPS, the residual racial and ethnic disparities were still statistically significant. Thus, health plans need to be cautious when following the Medicare example. Future studies are warranted to develop alternative MTM eligibility criteria so that potential MTM disparities can be eliminated.
One aspect of the study methods worth noting is the appropriateness of using the list of chronic conditions developed by Daniel and Malone for the Medicare population when determining MTM eligibility based on chronic conditions.25 The disease profiles of the adult non-Medicare population are different from those of Medicare beneficiaries. However, the list by Daniel and Malone includes all major chronic conditions that MTM programs typically cover, such as heart disease, hypertension, and diabetes among the adult non-Medicare population.14,15,23,25 Therefore, using the list by Daniel and Malone among the non-Medicare population should be considered appropriate for this study.25
This study analyzed the disparity implications of Part D MTM eligibility criteria among the adult non-Medicare population. One may wonder whether it would be more appropriate to examine the disparity implications of Part D MTM eligibility criteria among a more comparable population such as the nearly elderly who are not covered by Medicare. People may have this concern because Medicare and non-Medicare populations are likely to have different characteristics, and applying the Part D eligibility criteria among the non-Medicare population may not be legitimate. However, MTM programs for the adult non-Medicare population have included components similar to the Part D eligibility criteria.14,15 Therefore, we offer the current study to provide information to policy makers on the disparity implications of applying Part D eligibility criteria to the non-Medicare population.14,15
Despite the potential significant racial and ethnic disparities in meeting Part D MTM eligibility criteria among the adult non-Medicare population, this study did not examine whether these disparities have worsened racial and ethnic disparities in health status. In addition, health plans currently focus primarily on lowering the use and costs of prescription drugs, and typical MTM programs during the early period of MTM implementation were not designed to improve health outcomes.28 However, with the development and maturation of MTM programs, disparities in meeting MTM eligibility criteria may lead to widened gaps in health status between racial and ethnic groups. Therefore, future research should examine whether racial and ethnic disparities in meeting MTM eligibility criteria have aggravated racial and ethnic disparities in health status.
Limitations
A few limitations apply to this study. First, it examined a would-be situation among non-Medicare beneficiaries rather than the real-world situation of MTM takeup across racial and ethnic groups. For example, all prescription drugs, not just covered drugs, were included in the eligibility determination. However, it is difficult to imagine that the real-world situation is much different because of the repeatedly documented lower utilization and costs of health services and prescription medications among minorities compared with whites.16–20 One related limitation is that the MTM eligibility criteria used for the non-Medicare population are not exactly the same as the Part D MTM eligibility criteria. One additional limitation of this study arises from the imperfect information on chronic conditions in MEPS. The information on medical conditions in MEPS was based on patient report before being coded to ICD-9-CM codes by professional coders.24 Nonetheless, the information in MEPS has been considered reliable.18–20,24 A further limitation of this study is that it categorized the study sample into three racial and ethnic groups. This categorization may not accurately capture differences in biology, culture, and values.9
Conclusion
This study found that racial and ethnic minorities have lower odds for meeting Part D MTM eligibility criteria than do whites among the non-Medicare population. This pattern also held among a subgroup of the population that needs MTM services even more on average than does the general population. Future research should explore the health implications of these disparities and determine alternative MTM eligibility criteria that do not lead to racial and ethnic disparities in meeting the eligibility criteria.
Table 4.
Racial and ethnic disparities in meeting the eligibility criteria for medication therapy management services according to the 2008 eligibility criteria in the main analysisa
| Variable | Estimate | χ2 | P | OR (95% CI) |
|---|---|---|---|---|
| Intercept | −9.31 | 596.36 | <0.0001 | — |
| Non-Hispanic whites | — | — | — | — |
| Non-Hispanic blacks | −0.51 | 12.90 | <0.01 | 0.60 (0.46–0.79) |
| Hispanics | −0.62 | 17.46 | <0.0001 | 0.54 (0.40–0.72) |
| Age | 0.07 | 249.12 | <0.0001 | 1.07 (1.06–1.08) |
| Female gender | — | — | — | — |
| Male gender | −0.39 | 17.67 | <0.0001 | 0.68 (0.56–0.81) |
| Not married | — | — | — | — |
| Married | −0.17 | 2.70 | 0.10 | 0.85 (0.70–1.03) |
| Any private insurance | 1.15 | 43.88 | <0.0001 | 3.17 (2.25–4.46) |
| Public insurance only | 1.88 | 93.70 | <0.0001 | 6.58 (4.49–9.63) |
| No insurance | — | — | — | — |
| Poor | — | — | — | — |
| Near poor | −0.09 | 0.10 | 0.75 | 0.92 (0.54–1.56) |
| Low income | 0.21 | 1.96 | 0.16 | 1.24 (0.92–1.67) |
| Middle income | 0.11 | 0.49 | 0.48 | 1.11 (0.83–1.50) |
| High income | 0.25 | 1.97 | 0.16 | 1.28 (0.91–1.80) |
| Lower than high school education | — | — | — | — |
| GED or high school education | 0.29 | 5.30 | 0.02 | 1.33 (1.04–1.70) |
| Bachelor degree | 0.25 | 2.34 | 0.13 | 1.28 (0.93–1.77) |
| Master degree or higher | 0.60 | 11.38 | <0.01 | 1.83 (1.29–2.59) |
| Other education | 0.38 | 4.35 | 0.04 | 1.47 (1.02–2.10) |
| Northeast | — | — | — | — |
| Midwest | 0.18 | 1.53 | 0.22 | 1.20 (0.90–1.60) |
| South | 0.29 | 4.32 | 0.04 | 1.34 (1.02–1.77) |
| West | −0.04 | 0.05 | 0.82 | 0.97 (0.71–1.30) |
| Nonmetropolitan statistical area | — | — | — | — |
| Metropolitan statistical area | 0.18 | 2.40 | 0.12 | 1.20 (0.95–1.52) |
| Self-perceived excellent health status | — | — | — | — |
| Self-perceived very good health status | 0.50 | 6.55 | 0.01 | 1.66 (1.13–2.43) |
| Self-perceived good health status | 1.66 | 95.58 | <0.0001 | 5.28 (3.78–7.38) |
| Self-perceived fair health status | 2.61 | 221.25 | <0.0001 | 13.60 (9.64–19.18) |
| Self-perceived poor health status | 3.64 | 299.85 | <0.0001 | 37.93 (25.14–57.24) |
Abbreviation used: GED, general educational development; OR, odds ratio.
Model Wald χ2 = 1,105.66, P < 0.0001.
At a Glance.
Synopsis
The researchers analyzed the Medical Expenditure Panel Survey (MEPS) and examined medication therapy management (MTM) eligibility criteria used by Part D plans in 2008 and 2010–11 to determine whether blacks and Hispanics were less likely to meet the Medicare Part D eligibility criteria for MTM services than whites among the adult non-Medicare population. In the main analysis examining 2008 eligibility criteria, whites had a higher proportion of eligible individuals than blacks and Hispanics. According to survey-weighted logistic regression adjusting for patient characteristics, blacks and Hispanics had lower odds ratios for MTM eligibility compared with whites. Sensitivity analyses, analyses examining 2010–11 eligibility criteria, and analyses among individuals with heart disease, diabetes, and hypertension produced similar findings.
Analysis
This study can provide information to policy makers on the disparity implications of applying Part D eligibility criteria among the non-Medicare population. It found that blacks and Hispanics have lower odds for meeting Part D MTM eligibility criteria than do whites among the adult non-Medicare population. The disparity patterns were true for the overall study sample and for individuals with heart disease, diabetes, and hypertension—a subpopulation most in need of MTM services. Future studies should be undertaken to develop alternative MTM eligibility criteria so that potential MTM disparities can be eliminated. Furthermore, future research should examine whether racial and ethnic disparities in meeting MTM eligibility criteria have aggravated racial and ethnic disparities in health status.
Acknowledgments
Funding: Pharmaceutical Research and Manufacturers of America (PhRMA) Foundation Research Starter Grant in Health Outcomes and grant no. R01AG040146 from the National Institute On Aging.
To Okoia Uket; Songmei Meng, MS; and Kiraat D. Munshi, MS, for research assistance and to David L. Armbruster, PhD, for editorial assistance.
Footnotes
Disclosure: The authors declare no conflicts of interest or financial interests in any product or service mentioned in this article, including grants, employment, gifts, stock holdings, or honoraria.
Previous presentation: American Public Health Association Annual Meeting, Washington, DC, October 29 to November 2, 2011.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the PhRMA Foundation, the National Institute On Aging, or the National Institutes of Health.
References
- 1.Centers for Medicare & Medicaid Services, Department of Health & Human Services. Medicare Program; Medicare prescription drug benefit: final rule. Fed Regist. 2005;70:4193–585. [PubMed] [Google Scholar]
- 2.Wang J, Mullins CD, Brown LM, et al. Disparity implications of Medicare eligibility criteria for medication therapy management services. Health Serv Res. 2010;45:1061–82. doi: 10.1111/j.1475-6773.2010.01118.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Department of Health & Human Services. [August 15, 2011];Medicare Part D medication therapy management (MTM) programs. 2011 Accessed at www.cms.gov/PrescriptionDrugCovContra/Downloads/MTMFact-Sheet2011063011Final.pdf.
- 4.Bluml BM. Definition of medication therapy management: development of professionwide consensus. J Am Pharm Assoc. 2005;45:566–72. doi: 10.1331/1544345055001274. [DOI] [PubMed] [Google Scholar]
- 5.Byrd L, Fletcher A, Menifield C. Disparities in health care: minority elders at risk. ABNF J. 2007;18:51–5. [PubMed] [Google Scholar]
- 6.Gornick ME. The association of race/socioeconomic status and use of Medicare services: a little-known failure in access to care. Ann N Y Acad Sci. 1999;896:497–500. doi: 10.1111/j.1749-6632.1999.tb08180.x. [DOI] [PubMed] [Google Scholar]
- 7.Gornick ME. Disparities in Medicare services: potential causes, plausible explanations, and recommendations. Health Care Financ Rev. 2000;21:23–43. [PMC free article] [PubMed] [Google Scholar]
- 8.Gornick ME, Eggers PW, Reilly TW, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335:791–9. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- 9.Briesacher B, Limcangco R, Gaskin D. Racial and ethnic disparities in prescription coverage and medication use. Health Care Financ Rev. 2003;25:63–76. [PMC free article] [PubMed] [Google Scholar]
- 10.Schore J, Brown R, Lavin B. Racial disparities in prescription drug use among dually eligible beneficiaries. Health Care Financ Rev. 2003;25:77–90. [PMC free article] [PubMed] [Google Scholar]
- 11.Gaskin DJ, Briesacher BA, Limcangco R, et al. Exploring racial and ethnic disparities in prescription drug spending and use among Medicare beneficiaries. Am J Geriatr Pharmacother. 2006;4:96–111. doi: 10.1016/j.amjopharm.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Eichner J, Vladeck BC. Medicare as a catalyst for reducing health disparities. Health Aff (Millwood) 2005;24:365–75. doi: 10.1377/hlthaff.24.2.365. [DOI] [PubMed] [Google Scholar]
- 13.Schommer JC, Planas LG, Johnson KA, Doucette WR. Pharmacist-provided medication therapy management (part 2): payer perspective in 2007. J Am Pharm Assoc. 2008;48:478–86. doi: 10.1331/JAPhA.2008.08023. [DOI] [PubMed] [Google Scholar]
- 14.Medication Management Systems, Inc. [October 25, 2011];Introduction to Medication Management Systems, Inc.: comprehensive medication therapy management solutions. Accessed at www.meds-management.com/pdf/MMSServices_032010.pdf.
- 15.Pharmacy Society of Wisconsin. [October 25, 2011];About WPQC. Accessed at www.pswi.org/displaycommon.cfm?an=1&subarticlenbr=38.
- 16.Han E, Liu GG. Racial disparities in prescription drug use for mental illness among population in US. J Ment Health Policy Econ. 2005;8:131–43. [PubMed] [Google Scholar]
- 17.Khandker RK, Simoni-Wastila LJ. Differences in prescription drug utilization and expenditures between Blacks and Whites in the Georgia Medicaid population. Inquiry. 1998;35:78–87. [PubMed] [Google Scholar]
- 18.Wang J, Zuckerman IH, Miller NA, et al. Utilizing new prescription drugs: disparities among non-Hispanic whites, non-Hispanic blacks, and Hispanic whites. Health Serv Res. 2007;42:1499–519. doi: 10.1111/j.1475-6773.2006.00682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang J, White-Means SI, Hufstader MA, Walker GD. The economic implications of the racial and ethnic disparities in the use of selective serotonin reuptake inhibitors. Curr Med Res Opin. 2007;23:853–63. doi: 10.1185/030079907x182220. [DOI] [PubMed] [Google Scholar]
- 20.Wang J, Noel JM, Zuckerman IH, et al. Disparities in access to essential new prescription drugs between non-Hispanic whites, non-Hispanic blacks, and Hispanic whites. Med Care Res Rev. 2006;63:742–63. doi: 10.1177/1077558706293638. [DOI] [PubMed] [Google Scholar]
- 21.Hebert PL, Sisk JE, Howell EA. When does a difference become a disparity? Conceptualizing racial and ethnic disparities in health. Health Aff (Millwood) 2008;27:374–82. doi: 10.1377/hlthaff.27.2.374. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Medicare & Medicaid Services, Department of Health & Human Services. [August 16, 2011];Medicare Part D medication therapy management (MTM) programs: 2010 fact sheet. Accessed at www.cms.hhs.gov/Prescription-DrugCovContra/Downloads/MTMFactSheet.pdf.
- 23.Agency for Healthcare Research and Quality. [December 18, 2011];2010 national healthcare disparities report. Accessed at www.ahrq.gov/qual/nhdr10/nhdr10.pdf.
- 24.Agency for Healthcare Research and Quality. [August 15, 2011];Medical Expenditure Panel Survey. Accessed at www.meps.ahrq.gov/mep-sweb. [PubMed]
- 25.Daniel GW, Malone DC. Characteristics of older adults who meet the annual prescription drug expenditure threshold for Medicare medication therapy management programs. J Manag Care Pharm. 2007;13:142–54. doi: 10.18553/jmcp.2007.13.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andersen RM, Davidson PL. Improving access to care in America: individual and contextual factors. In: Andersen RM, Rice TH, Kominski GF, editors. Changing the US health care system: key issues in health services, policy and management. 3. San Francisco, CA: Jossey-Bass; 2007. pp. 3–32. [Google Scholar]
- 27.Fishman J, O’Dwyer P, Lu HL, et al. Race, treatment preferences, and hospice enrollment: eligibility criteria may exclude patients with the greatest needs for care. Cancer. 2009;115:689–97. doi: 10.1002/cncr.24046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guirguis AB, Zingone MM. Medication therapy management and cost-related medication nonadherence. JAMA. 2008;300:1130. doi: 10.1001/jama.300.10.1130-a. [DOI] [PubMed] [Google Scholar]