Abstract
Background
Quadriceps strength deficits are ubiquitous after anterior cruciate ligament (ACL) injury. Deficits prior to surgery can influence knee function post-operatively. Inhibition contributes to quadriceps strength deficits after an ACL injury. Body mass index, meniscal injury, and sex influence functional outcomes after ACL reconstruction. The purpose of this study is to examine the relationship of pre-operative quadriceps strength and post-operative knee function and to investigate how other pre-operative factors may influence this relationship.
Methods
After an ACL injury, subjects received pre-operative rehabilitation and performed quadriceps strength testing. Subjects underwent reconstruction and post-operative rehabilitation. Six months after ACL reconstruction, subjects completed the International Knee Documentation Committee 2000 subjective form (IKDC2000). Linear regression models were developed using IKDC2000 scores at 6 months after ACL reconstruction as the dependent variable.
Results
Fifty-five subjects had complete pre-operative data and IKDC2000 scores at 6 months after ACL reconstruction. Pre-operative involved quadriceps strength was a significant predictor for IKDC2000 scores 6 months after ACL reconstruction. Sex, meniscal injury, pre-operative BMI, and pre-operative involved quadriceps activation ratio were not significant predictors in the regression model.
Conclusions
Pre-operative quadriceps strength can predict IKDC2000 scores 6 months after ACL reconstruction. Deficits in pre-operative quadriceps strength influence self-reported function 6 months after surgery. Factors that are known to influence quadriceps strength and self-reported outcomes do not influence the relationship between pre-operative quadriceps strength and post-operative IKDC2000 scores.
Keywords: quadriceps strength, self-reported function, anterior cruciate ligament, regression
INTRODUCTION
The incidence of injury to the anterior cruciate ligament (ACL) is the highest among internal knee injuries and is greater in sports that require multidirectional activities.1, 2 The sequela seen after ACL injury involve quadriceps strength deficits, neuromuscular dysfunction and biomechanical mal-adaptations and are associated with the development of knee osteoarthritis.3–5 Early ACL reconstruction is the current recommendation by orthopaedic surgeons for young, active individuals who plan to perform multidirectional activities as part of their sport or occupation,6–9 with approximately 125,000 surgeries performed annually in the United States.1, 10 Athletes are frequently counseled to undergo ACL reconstruction with the expectation of normal knee function and a successful return to their previous levels of activity.9, 11, 12 Despite successful restoration of mechanical stability after ACL reconstruction,13, 14 many individuals may continue to exhibit knee instability, pain, quadriceps strength deficits, or reduced range of motion that may account for the inability to achieve satisfactory patient outcomes.3–5, 15–19
Knee function assessed by self-report scores provides a measure of symptoms, function, and sports activity20 and is associated with patient satisfaction.21 Self-reported knee outcome scales provide important information regarding patients’ perception of knee function. The IKDC 2000 subjective knee form (IKDC2000) is a knee-specific self-reported outcome measure for assessing symptoms, function, and sports activity.20, 22 It is frequently used to assess knee function in patients after ACL reconstruction and contains items most relevant to individuals with ACL reconstruction.23 It is able to differentiate between patients with greater knee symptoms from those with lesser symptoms, and those with lower knee function from those with higher knee function.24 Since not all individuals regain satisfactory knee function after ACL reconstruction,25, 26 it is important to examine predictive factors that could influence good knee function and provide an earlier opportunity to target those individuals who may need additional interventions or to change interventions to maximize patient outcomes.
Quadriceps strength deficits are prevalent after ACL injury.15, 17, 27–30 Quadriceps weakness is present after ACL reconstruction, regardless of graft type.31, 32 Quadriceps strength is significantly related to patient satisfaction and knee function during gait.33, 34 Quadriceps strength prior to ACL surgery can influence knee function post-operatively.15, 18, 35, 36 Because of the large impact that quadriceps strength has on knee function, the identification and treatment of quadriceps weakness prior to and after ACL reconstruction is paramount in maximizing patient outcomes.
Body mass index (BMI), meniscal injury, sex, and quadriceps activation deficits may affect the relationship between quadriceps strength and knee function. Body mass index, meniscal injury, and sex influence functional outcomes after ACL reconstruction.24, 35, 37–40 Quadriceps activation deficits contribute to quadriceps strength deficits after an ACL injury.27, 41, 42 The purpose of this study is to examine the relationship of preoperative quadriceps strength and post-operative self-reported knee function and to investigate how other pre-operative factors may influence this relationship.
METHODS
Subjects
One hundred two subjects who sustained a unilateral ACL rupture (Mean: 7.2 weeks; range: 1.1 to 39.9 weeks) were recruited for a prospective longitudinal observational clinical study between June 2005 to April 2010 from a single physical therapy clinic. All subjects were regular participants in level I or II activities (≥ 50 hours/year) prior to ACL rupture.3, 43 Subjects did not have concomitant ligamentous injury, bilateral lower limb involvement, symptomatic meniscal injury, fracture, or full-thickness articular cartilage damage. The ACL rupture was confirmed by magnetic resonance imaging and ≥ 3 mm side-to-side difference3 in anterior tibial translation using a KT-1000 arthrometer (MedMetrics, San Diego, CA). The study was approved by the University of Delaware Institutional Human Subjects Review Board and each subject gave informed consent. All subjects completed a battery of functional tests after pre-operative rehabilitation and completed the IKDC2000 six months after ACL reconstruction.
Of the 102 athletes recruited for this study, 14 chose to pursue non-operative care for their ACL injury. Three subjects were lost to follow-up. One subject did not have ACL reconstruction because the tear was found to be incomplete at the time of arthroscopy. One subject was transferred to another study. Eighty-three subjects therefore comprised the study population (Table 1).
Table 1.
Subject characteristics (n=83)
| Male:Female | 55:28 |
| Activity level (I:II) | 58:25 |
| Meniscal injury? Y:N | 30:53 |
| Age (years, SD) | 26.8 (11.2) |
| BMI (mean, SD) | 25.7 (4.8) |
| Injury to post-training(weeks, SD) | 12.6 (8.3) |
| Weeks of training (weeks, SD) | 5.2 (3.4) |
| Number of treatments (mean, SD) | 8.9 (2.5) |
Testing and Rehabilitation
Prior to surgery, subjects were enrolled in a pre-operative rehabilitation program.28, 44 Pre-operative rehabilitation consisted of progressive exercise training program in order to restore muscle strength and appropriate neuromuscular responses. The exercise program emphasized aggressive strength training and specialized perturbation training. Muscle strength training involved the use of high intensity, low repetition non-weight bearing and weight bearing quadriceps strengthening exercises, augmented with neuromuscular electrical stimulation if subjects demonstrated a quadriceps strength index of less than 80 %.34, 45 Perturbation training was administered according to the protocol outlined by Fitzgerald et al.44
The surgeon performed either a semitendinosus-gracilis autograft or soft tissue allograft ACL reconstruction. After surgery, standardized ACL rehabilitation guidelines were followed for all patients.46 Subjects were systematically progressed through the rehabilitation process based on the clinical milestones in the guidelines. Post-operative rehabilitation guidelines emphasized impairment resolution, aggressive quadriceps strengthening (augmented with NMES if needed), and neuromuscular training. Patients’ progress was monitored using effusion grading and soreness rules.46–48
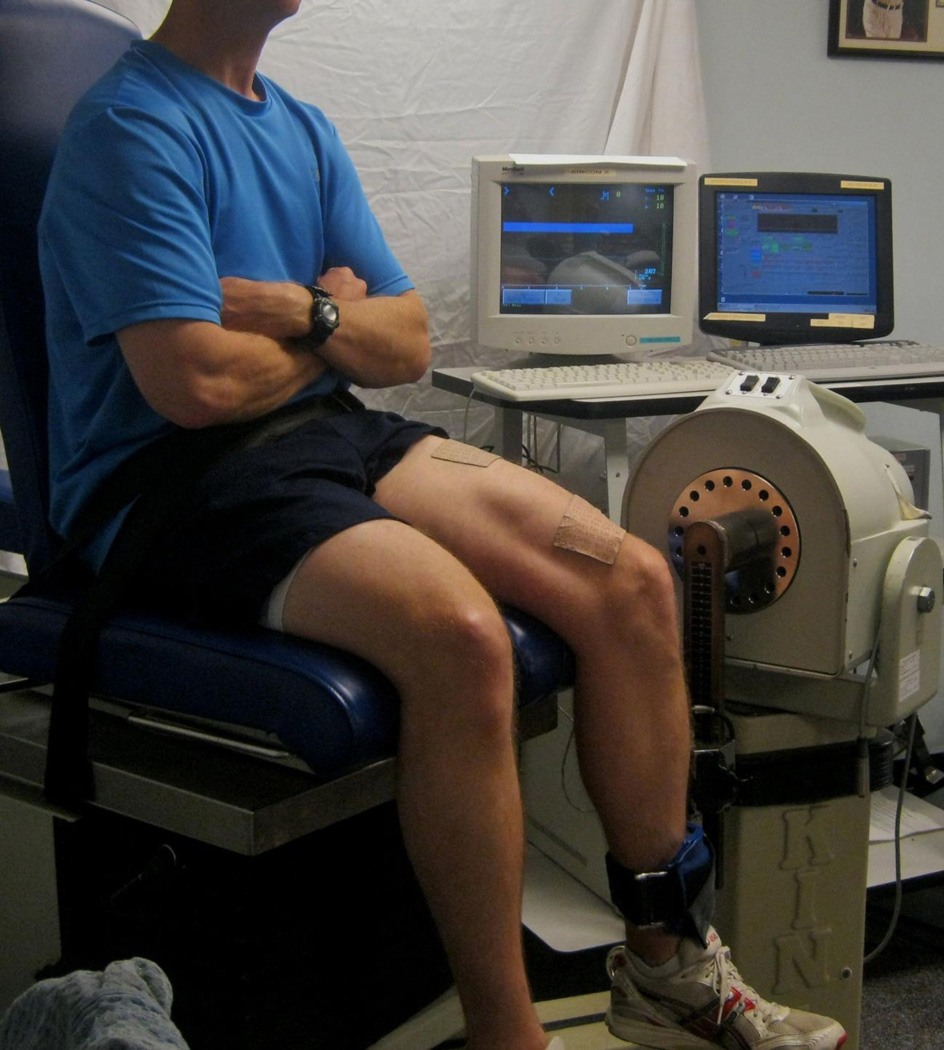
Quadriceps strength testing
Quadriceps strength testing was performed after subjects completed their pre-operative rehabilitation program. Testing consisted of maximal isometric voluntary contraction (MVIC) of the quadriceps with burst superimposition technique (Figure 1).34 This method has high reliability with intraclass coefficients (ICC2,1) of 0.97–0.98.27 The hips and knees are placed in 90 degrees of flexion on an isometric dynamometer (Kin-Com, Chattanooga Corp., Chattanooga, TN). Self-adhesive electrodes (76mm × 127mm) are placed over the muscle bellies of the vastus lateralis and vastus medialis to deliver the electrical stimulation. Patients were encouraged to produce a MVIC by familiarizing them to the testing procedure, and were provided with standardized verbal encouragement from the therapist, and visual feedback from the dynamometer’s real-time visual display. The patient performed a short MVIC to determine the target force during testing. A bar target on the real-time visual display was placed 15–20 percent above the MVIC to provide visual feedback encouragement.
Figure 1.
Maximal volitional isometric contraction of the quadriceps with burst superimposition testing.
Patients performed a 3–5 second MVIC with a burst superimposition stimulation in which a 10-pulse, 100-Hz 600-microsecond train at 135 volts was delivered to the muscles to determine patients’ ability to fully activate the quadriceps muscles. If the subject was unable to achieve 95% muscle activation during the burst superimposition technique, the test was repeated until the patient achieved 95% muscle activation or the subject became fatigued (up to 2 more MVICs). Each MVIC was separated by 2 minutes to allow the muscles to rest and avoid fatigue. Quadriceps force was normalized to body mass index (N/BMI). Involved quadriceps strength index was calculated as a percentage of the ratio of the involved quadriceps force compared to the uninvolved quadriceps force. Quadriceps strength index was calculated for MVIC with and without the burst superimposed stimulation. Volitional muscle activation level was calculated as a percentage of the quotient of the volitional muscle force just prior to the onset of the electrical stimulation by the maximal force produced by the electrical stimulation. Normal muscle activation was operationally defined as 95%.27, 49, 50
International Knee Committee Documentation 2000 subjective knee form (IKDC2000)
The IKDC2000 is a joint-specific outcome measure for assessing symptoms, function, and sports activity pertinent to a variety of knee conditions.20, 22 The form contains 18 questions, in which the total scores are expressed as a percentage. The IKDC2000 contains items regarding symptoms and disabilities important to patients with an ACL tear.51 The IKDC2000 is a valid, reliable, and responsive self-reported outcome measure.20, 52, 53
Data management and statistical analysis
Comparisons were made between preoperative and postoperative quadriceps MVIC values and IKDC2000 scores using paired t-tests. In order to determine if pre-operative involved quadriceps strength could predict IKDC2000 scores at 6 months after ACL reconstruction, hierarchical linear regression models were developed using IKDC2000 scores at 6 months after ACL reconstruction as the dependent variable. In the first step, pre-operative involved quadriceps MVIC was entered, and the second step included sex, meniscal injury, pre-operative BMI, and pre-operative involved quadriceps activation ratio. R2 and R2 change statistics and P values at each step of the model were reported to demonstrate the importance of the variables at each step. Alternate hierarchical linear regression models were developed to determine the influence that order of entry into the regression models might have on the relationship between pre-operative quadriceps strength and IKDC2000 scores after reconstruction, in which sex, meniscal injury, pre-operative BMI, and pre-operative involved quadriceps activation ratio were entered first, followed by pre-operative involved quadriceps MVIC in the second step.
A priori alpha level of 0.05 was set for all analyses. All analyses were conducted in PASW v.18 (SPSS Inc., Chicago, IL).
RESULTS
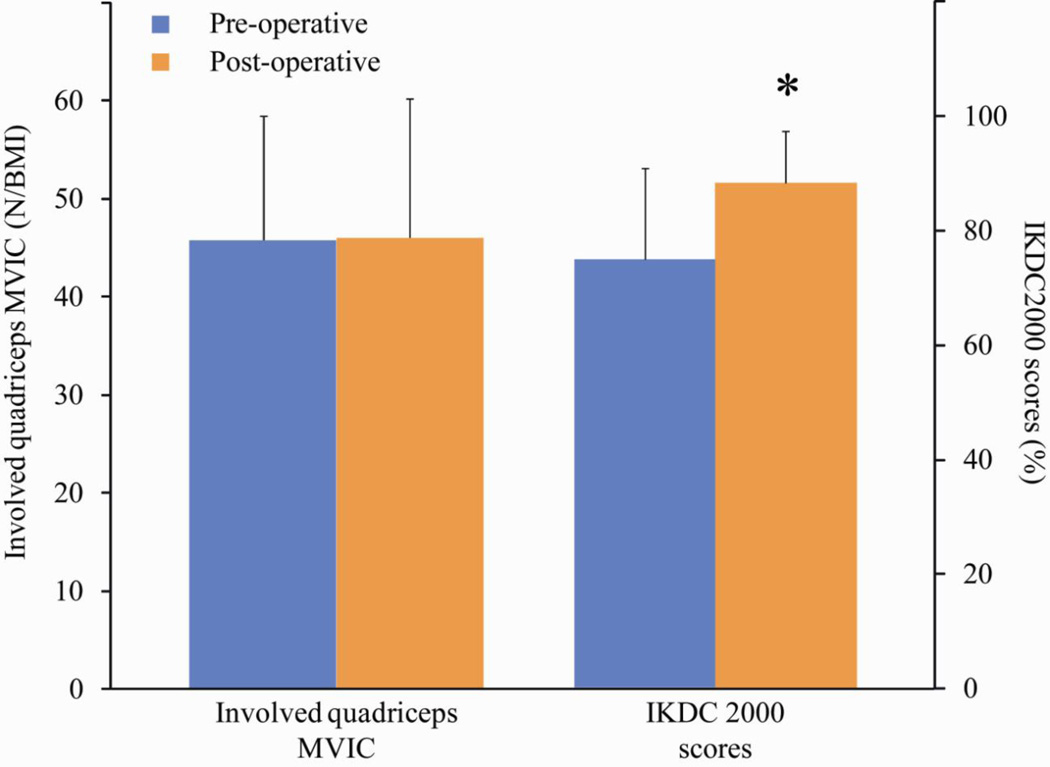
Subject characteristics of 83 subjects are shown in Table 1. Of the 83 subjects, 55 subjects had complete pre-operative data and IKDC2000 scores at 6 months after ACL reconstruction. No significant differences were found between patients who were included and who were excluded on any baseline variable. No significant differences were found between pre-operative and 6 month post-operative values for involved quadriceps MVIC (p=0.80), however, IKDC2000 scores after surgery were significantly higher than IKDC2000 scores before surgery (p<.001) (Figure 2). Hierarchical linear regression models are displayed in Table 2. Preoperative involved quadriceps strength was a significant predictor for IKDC2000 scores 6 months after ACL reconstruction (model 1). This explained 10.7% of the variance in the regression. Sex, meniscal injury, pre-operative BMI, and pre-operative involved quadriceps activation ratio were not significant predictors in either regression model. Alternate hierarchical linear regression models are displayed in Table 3.
Figure 2.
Involved quadriceps MVIC and IKDC2000 scores before (pre-operative) and after (post-operative) ACL reconstruction. (* p<.001)
Table 2.
Pre-operative quadriceps strength as predictor of IKDC2000 scores at 6 months after ACL reconstruction: Hierarchical linear regression modeling
| IKDC2000 scores at 6 months after ACL reconstruction | ||||
|---|---|---|---|---|
| Model | R2 | Adjusted R2 | R2 Change | P value |
| 1 | 0.11 | 0.09 | 0.11 | 0.02 |
| 2 | 0.18 | 0.10 | 0.07 | 0.07 |
| Standardized β for Pre-operative involved quadriceps strength = 0.33 | ||||
Model 1: Pre-operative involved quadriceps MVIC
Model 2: Pre-operative involved quadriceps MVIC, Sex, Meniscal injury, Pre-operative BMI, Pre-operative involved quadriceps activation ratio
Table 3.
Pre-operative quadriceps strength as predictor of IKDC2000 scores at 6 months after ACL reconstruction: Alternate order of entry
| IKDC2000 scores at 6 months after ACL reconstruction | ||||
|---|---|---|---|---|
| Model | R2 | Adjusted R2 | R2 Change | P value |
| 1 | 0.13 | 0.06 | 0.13 | 0.13 |
| 2 | 0.18 | 0.10 | 0.05 | 0.07 |
| Standardized β for Pre-operative involved quadriceps strength = 0.30 | ||||
Model 1: Pre-operative involved quadriceps MVIC, Sex, Meniscal injury, Pre-operative BMI, Pre-operative involved quadriceps activation ratio
Model 2: Pre-operative involved quadriceps MVIC
DISCUSSION
Our hypothesis was supported as pre-operative involved quadriceps strength predicted IKDC2000 scores 6 months after ACL reconstruction. Sex, meniscal injury, pre-operative BMI, and pre-operative quadriceps activation ratio did not influence the relationship between preoperative involved quadriceps strength and IKDC2000 scores at 6 months after surgery.
The results of this study demonstrate that pre-operative quadriceps strength predicts IKDC2000 scores 6 months after ACL reconstruction providing continued evidence that preoperative quadriceps strength can influence knee function post-operatively. Patients with profound pre-operative strength deficits have lower knee function after surgery.15, 17, 35 Eitzen et al35 found that pre-operative quadriceps strength significantly predicted the Cincinnati Knee Scores two years after ACL reconstruction. de Jong and colleagues15 demonstrated that quadriceps strength deficits greater than 20% resulted in lower hop symmetry indexes 6 and 9 months after surgery, but resolved by 12 months.
Sex, meniscal injury, pre-operative BMI, and pre-operative quadriceps activation ratio did not influence our prediction models. These variables were chosen as they influence quadriceps strength or knee function in ACL injury literature. Sex did not influence the relationship between quadriceps strength and IKDC2000 scores. Although, men have stronger quadriceps than women, even when normalized to body weight,54 sex has no effect on the relationship between quadriceps strength and knee function. Meniscal injuries predict lower knee function after ACL reconstruction.35 In this study, meniscal injuries had no influence on the quadriceps strength and IKDC2000 score relationship. Subjects who had meniscal injuries were asymptomatic and exhibited no pain with hopping, which may explain the lack of influence. Therefore, meniscal injuries likely did not impede the rehabilitation process prior to surgery. BMI is a significant predictor of knee function after surgery.39, 40 Kowalchuk and associates40 found that obese patients (BMI greater 30 kg/m2) had 0.4 times the odds of having success after reconstruction than subjects with normal BMI. In our study, only seven subjects had pre-operative BMI greater than 30 kg/m2, which may account for the lack of significance in explaining IKDC2000 scores. Pre-operative quadriceps activation ratio did not influence the relationship between pre-operative quadriceps strength and post-operative IKDC2000 scores. This was not surprising, as only a small percentage (21.8%) of subjects demonstrated preoperative quadriceps activation ratios < 95% and 9.1% demonstrated activation ratios < 90%. Subjects who had a quadriceps index less than 80% prior to training received augmented neuromuscular electrical stimulation. Neuromuscular stimulation, when administered at a high intensity setting, improves quadriceps strength, quadriceps activation ratio and function in patients post ACL reconstruction.32, 55–57 The aggressive nature of our training explains the high number of individuals with little to no activation deficits and excluding activation deficits as an influential factor.
The order of entry into the regression models impacted the relationship between preoperative quadriceps strength and IKDC2000 scores 6 months after ACL reconstruction. When quadriceps strength was entered first into the model, it explained a small, but statistically significant, proportion of the variance than when entered last. When the other variables were entered first into the model, quadriceps strength explained a small and nonsignificant proportion of the variance. The addition of pre-operative involved quadriceps strength in the second step was able to explain an additional 5% of the variance beyond what was explained in the other factors, however, this was not statistically significant. Although, pre-operative involved quadriceps strength is an independent predictor of IKDC2000 scores 6 months after surgery, it only accounts for a small amount of the explained variance, and other unknown factors may influence this relationship.
Quadriceps strength in the ACL-deficient knee prior to ACL reconstruction is a primary contributor to outcomes after reconstructive surgery.15, 17, 35, 58 These results showed that it explained 10.7% of the variance in IKDC2000 scores at 6 months after ACL reconstruction. Eitzen et al35 found the pre-operative quadriceps strength explained 15.6% of the variance in Cincinnati Knee scores two years after reconstruction and those with profound quadriceps strength deficits before surgery were more likely to have large strength deficits after surgery. Clearly, quadriceps weakness continues to be a major concern after ACL injury and reconstruction and can persist for months to years after ACL reconstruction.32, 59 The subjects in this sample received perturbation training and aggressive quadriceps strengthening in an attempt to resolve neuromuscular and quadriceps strength deficits prior to surgery. Pre-operative quadriceps strengthening with weight bearing and non-weight bearing resistance exercises, augmented with perturbation training, significantly improves quadriceps strength before and after ACL reconstruction.28, 29 In addition, assessment of quadriceps strength after a bout of preoperative rehabilitation results in better decision making regarding ACL reconstruction surgery.60 Maximizing quadriceps strength with aggressive rehabilitation prior to ACL reconstruction should be a primary goal for clinicians to optimize knee function after surgery.
Limitations
There are limitations to this study. The results can only be generalized to individuals who sustain an isolated ACL injury or asymptomatic concomitant injuries and should not be generalized to individuals with symptomatic or complex concomitant injuries. These patients were all Level I and II active individuals and the results of this study should not be generalized to individuals involved in less demanding activities. All subjects were reconstructed with either semitendinosus-gracilis autograft or soft-tissue allograft. These prediction models were used to determine IKDC2000 scores 6 months after ACL reconstruction and can only be generalized to short-term outcomes. Other models will need to be devised to determine long-term outcomes after ACL reconstruction. We were only able to include 5 independent variables into our regression models due to the number of subjects in this study. More subjects would allow for additional models to be computed.
CONCLUSIONS
The results of this research study indicate pre-operative quadriceps strength can predict IKDC2000 scores 6 months after ACL reconstruction, confirming the importance of good quadriceps strength prior to ACL reconstruction in predicting better knee function after surgery. Factors that are known to influence quadriceps strength and self-reported outcomes do not influence the relationship between pre-operative quadriceps strength and post-operative IKDC2000 scores.
ACKNOWLEDGMENTS
We thank the University of Delaware Physical Therapy clinic and Martha Callahan with their assistance in patient management and data collection of this study. This research was supported in full/part by a grant from National Institutes of Health (2R01HD037985) and the Promotion of Doctoral Studies – Level I Scholarship from the Foundation for Physical Therapy.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interests statemants
One of the authors has declared a potential conflict of interest. Michael J. Axe is a consultant to Smith & Nephew.
Contributor Information
David Logerstedt, Dept. of Physical Therapy, University of Delaware, 301 McKinly Lab, Newark, DE 19716 USA, Telephone: +1-302-831-8667, Fax: +1-302-831-4234, davlog@udel.edu.
Andrew Lynch, University of Pittsburgh Department of Orthopaedic Surgery, Pittsburgh, PA 15213 USA.
Michael J. Axe, Medical Arts Pavilion I, 4745 Ogletown-Stanton Road, Suite 225, Newark, DE 19713 USA.
Lynn Snyder-Mackler, Dept. of Physical Therapy, University of Delaware, 301 McKinly Lab, Newark, DE 19716 USA.
REFERENCES
- 1.Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, Demaio M, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. The American journal of sports medicine. 2006;34:1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 2.Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: A 10-year study. The Knee. 2006;13:184–188. doi: 10.1016/j.knee.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. The American journal of sports medicine. 1994;22:632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 4.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis and rheumatism. 2004;50:3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 5.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Annals of the rheumatic diseases. 2004;63:269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arroll RG, Sutich E, Foliaki S, Gendall P, Milne C, Moginie G, Phillips J, Pitto R, Thomson R, Tregonning R, Watt J, Blakelock R, Matheson J, Matson N, McNair P, Murphy I, Pfitzinger P, Quin P, Ratima K, Reid D, Tietjens B. In: The Diagnosis and Management of Soft Tissue Knee Injuries: Internal Derangements. Group NZG, editor. 2003. pp. 1–99. [Google Scholar]
- 7.Delay BS, Smolinski RJ, Wind WM, Bowman DS. Current practices and opinions in ACL reconstruction and rehabilitation: results of a survey of the American Orthopaedic Society for Sports Medicine. The American journal of knee surgery. 2001;14:85–91. [PubMed] [Google Scholar]
- 8.Dye SF, Wojtys EM, Fu FH, Fithian DC, Gillquist I. Factors contributing to function of the knee joint after injury or reconstruction of the anterior cruciate ligament. Instructional course lectures. 1999;48:185–198. [PubMed] [Google Scholar]
- 9.Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19:762–770. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 10.Hughes G, Watkins J. A risk-factor model for anterior cruciate ligament injury. Sports medicine (Auckland, NZ. 2006;36:411–428. doi: 10.2165/00007256-200636050-00004. [DOI] [PubMed] [Google Scholar]
- 11.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part I. The American journal of sports medicine. 2005;33:1579–1602. doi: 10.1177/0363546505279913. [DOI] [PubMed] [Google Scholar]
- 12.Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. British journal of sports medicine. 2005;39:127–131. doi: 10.1136/bjsm.2004.010900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. The American journal of sports medicine. 2004;32:1986–1995. doi: 10.1177/0363546504271211. [DOI] [PubMed] [Google Scholar]
- 14.Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M. Double-bundle ACL reconstruction can improve rotational stability. Clinical orthopaedics and related research. 2007;454:100–107. doi: 10.1097/BLO.0b013e31802ba45c. [DOI] [PubMed] [Google Scholar]
- 15.de Jong SN, van Caspel DR, van Haeff MJ, Saris DB. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23:21–28. 28 e1–23 e1. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 16.Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. The Journal of orthopaedic and sports physical therapy. 2010;40:141–154. doi: 10.2519/jospt.2010.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keays SL, Bullock-Saxton J, Keays AC, Newcombe P. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. The Knee. 2001;8:229–234. doi: 10.1016/s0968-0160(01)00099-0. [DOI] [PubMed] [Google Scholar]
- 18.Keays SL, Bullock-Saxton JE, Newcombe P, Keays AC. The relationship between knee strength and functional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21:231–237. doi: 10.1016/S0736-0266(02)00160-2. [DOI] [PubMed] [Google Scholar]
- 19.Myklebust G, Holm I, Maehlum S, Engebretsen L, Bahr R. Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow-up study. The American journal of sports medicine. 2003;31:981–989. doi: 10.1177/03635465030310063901. [DOI] [PubMed] [Google Scholar]
- 20.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, et al. Development and validation of the international knee documentation committee subjective knee form. The American journal of sports medicine. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 21.Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. The Journal of bone and joint surgery. 2002;84-A:1560–1572. doi: 10.2106/00004623-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Wright RW. Knee injury outcomes measures. J Am Acad Orthop Surg. 2009;17:31–39. doi: 10.5435/00124635-200901000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Hambly K, Griva K. IKDC or KOOS: which one captures symptoms and disabilities most important to patients who have undergone initial anterior cruciate ligament reconstruction? The American journal of sports medicine. 2010;38:1395–1404. doi: 10.1177/0363546509359678. [DOI] [PubMed] [Google Scholar]
- 24.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. The American journal of sports medicine. 2006;34:128–135. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 25.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the Preinjury Level of Competitive Sport After Anterior Cruciate Ligament Reconstruction Surgery: Two-thirds of Patients Have Not Returned by 12 Months After Surgery. The American journal of sports medicine. 2010 doi: 10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- 26.Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: a meta-analysis of functional scores. Clinical orthopaedics and related research. 2007;458:180–187. doi: 10.1097/BLO.0b013e31803dcd6b. [DOI] [PubMed] [Google Scholar]
- 27.Chmielewski TL, Stackhouse S, Axe MJ, Snyder-Mackler L. A prospective analysis of incidence and severity of quadriceps inhibition in a consecutive sample of 100 patients with complete acute anterior cruciate ligament rupture. J Orthop Res. 2004;22:925–930. doi: 10.1016/j.orthres.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 28.Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A Progressive 5-Week Exercise Therapy Program Leads to Significant Improvement in Knee Function Early After Anterior Cruciate Ligament Injury. The Journal of orthopaedic and sports physical therapy. 2010 doi: 10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hartigan E, Axe MJ, Snyder-Mackler L. Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. J Orthop Res. 2009;27:724–729. doi: 10.1002/jor.20754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moksnes H, Risberg MA. Performance-based functional evaluation of non-operative and operative treatment after anterior cruciate ligament injury. Scandinavian journal of medicine & science in sports. 2008 doi: 10.1111/j.1600-0838.2008.00816.x. [DOI] [PubMed] [Google Scholar]
- 31.Krishnan C, Williams GN. Factors explaining chronic knee extensor strength deficits after ACL reconstruction. J Orthop Res. 2011;29:633–640. doi: 10.1002/jor.21316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clinics in sports medicine. 2008;27:405–424. doi: 10.1016/j.csm.2008.02.001. vii-ix. [DOI] [PubMed] [Google Scholar]
- 33.Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A. Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. The Journal of orthopaedic and sports physical therapy. 1999;29:400–412. doi: 10.2519/jospt.1999.29.7.400. [DOI] [PubMed] [Google Scholar]
- 34.Snyder-Mackler L, Delitto A, Bailey SL, Stralka SW. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. The Journal of bone and joint surgery. 1995;77:1166–1173. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. British journal of sports medicine. 2009;43:371–376. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 36.Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clinical biomechanics (Bristol, Avon) 2002;17:56–63. doi: 10.1016/s0268-0033(01)00097-3. [DOI] [PubMed] [Google Scholar]
- 37.Ageberg E, Forssblad M, Herbertsson P, Roos EM. Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction: data from the Swedish knee ligament register. The American journal of sports medicine. 2010;38:1334–1342. doi: 10.1177/0363546510361218. [DOI] [PubMed] [Google Scholar]
- 38.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. The American journal of sports medicine. 2010;38:2040–2050. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heijne A, Ang BO, Werner S. Predictive factors for 12-month outcome after anterior cruciate ligament reconstruction. Scandinavian journal of medicine & science in sports. 2009;19:842–849. doi: 10.1111/j.1600-0838.2008.00852.x. [DOI] [PubMed] [Google Scholar]
- 40.Kowalchuk DA, Harner CD, Fu FH, Irrgang JJ. Prediction of patient-reported outcome after single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25:457–463. doi: 10.1016/j.arthro.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. Journal of athletic training. 2010;45:87–97. doi: 10.4085/1062-6050-45.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williams GN, Snyder-Mackler L, Barrance PJ, Axe MJ, Buchanan TS. Muscle and tendon morphology after reconstruction of the anterior cruciate ligament with autologous semitendinosus-gracilis graft. The Journal of bone and joint surgery. 2004;86-A:1936–1946. doi: 10.2106/00004623-200409000-00012. [DOI] [PubMed] [Google Scholar]
- 43.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 44.Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physical active individuals. Physical therapy. 2000;80:128–140. [PubMed] [Google Scholar]
- 45.Delitto A, Rose SJ, McKowen JM, Lehman RC, Thomas JA, Shively RA. Electrical stimulation versus voluntary exercise in strengthening thigh musculature after anterior cruciate ligament surgery. Physical therapy. 1988;68:660–663. doi: 10.1093/ptj/68.5.660. [DOI] [PubMed] [Google Scholar]
- 46.Manal T, Snyder-Mackler L. Practice guidelines for anterior cruciate ligament rehabilitation: a criterion-based rehabilitation progression. Oper Tech Orthop. 1996;6:190–196. [Google Scholar]
- 47.Fees M, Decker T, Snyder-Mackler L, Axe MJ. Upper extremity weight-training modifications for the injured athlete. A clinical perspective. The American journal of sports medicine. 1998;26:732–742. doi: 10.1177/03635465980260052301. [DOI] [PubMed] [Google Scholar]
- 48.Sturgill LP, Snyder-Mackler L, Manal TJ, Axe MJ. Interrater reliability of a clinical scale to assess knee joint effusion. The Journal of orthopaedic and sports physical therapy. 2009;39:845–849. doi: 10.2519/jospt.2009.3143. [DOI] [PubMed] [Google Scholar]
- 49.Stackhouse SK, Dean JC, Lee SC, Binder-MacLeod SA. Measurement of central activation failure of the quadriceps femoris in healthy adults. Muscle & nerve. 2000;23:1706–1712. doi: 10.1002/1097-4598(200011)23:11<1706::aid-mus6>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 50.Park J, Hopkins JT. Quadriceps activation normative values and the affect of subcutaneous tissue thickness. J Electromyogr Kinesiol. 21:136–140. doi: 10.1016/j.jelekin.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 51.Tanner SM, Dainty KN, Marx RG, Kirkley A. Knee-specific quality-of-life instruments: which ones measure symptoms and disabilities most important to patients? The American journal of sports medicine. 2007;35:1450–1458. doi: 10.1177/0363546507301883. [DOI] [PubMed] [Google Scholar]
- 52.Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R, et al. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Joint Bone Spine. 2007;74:594–599. doi: 10.1016/j.jbspin.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 53.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. The American journal of sports medicine. 2006;34:1567–1573. doi: 10.1177/0363546506288855. [DOI] [PubMed] [Google Scholar]
- 54.Huston LJ, Greenfield ML, Wojtys EM. Anterior cruciate ligament injuries in the female athlete. Potential risk factors. Clinical orthopaedics and related research. 2000:50–63. doi: 10.1097/00003086-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 55.Lewek M, Stevens J, Snyder-Mackler L. The use of electrical stimulation to increase quadriceps femoris muscle force in an elderly patient following a total knee arthroplasty. Physical therapy. 2001;81:1565–1571. doi: 10.1093/ptj/81.9.1565. [DOI] [PubMed] [Google Scholar]
- 56.Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ. Knee stability and movement coordination impairments: knee ligament sprain. The Journal of orthopaedic and sports physical therapy. 2010;40:A1–A37. doi: 10.2519/jospt.2010.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Snyder-Mackler L, Delitto A, Stralka SW, Bailey SL. Use of electrical stimulation to enhance recovery of quadriceps femoris muscle force production in patients following anterior cruciate ligament reconstruction. Physical therapy. 1994;74:901–907. doi: 10.1093/ptj/74.10.901. [DOI] [PubMed] [Google Scholar]
- 58.Shelbourne KD, Klotz C. What I have learned about the ACL: utilizing a progressive rehabilitation scheme to achieve total knee symmetry after anterior cruciate ligament reconstruction. J Orthop Sci. 2006;11:318–325. doi: 10.1007/s00776-006-1007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kobayashi A, Higuchi H, Terauchi M, Kobayashi F, Kimura M, Takagishi K. Muscle performance after anterior cruciate ligament reconstruction. International orthopaedics. 2004;28:48–51. doi: 10.1007/s00264-003-0502-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eitzen I, Moksnes H, Snyder-Mackler L, Engebretsen L, Risberg MA. Functional tests should be accentuated more in the decision for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18:1517–1525. doi: 10.1007/s00167-010-1113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]