Abstract
OBJECTIVE
Knee Osteoarthritis (OA) and pain are assumed to be barriers for meeting physical activity guidelines, but this has not been formally evaluated. The purpose of this study was to determine the proportion of people with and without knee OA and knee pain who met recommended physical activity levels through walking.
METHODS
Cross-sectional analysis of community dwelling adults who have or who are at high risk of knee OA from The Multicenter Osteoarthritis Study. Participants wore a StepWatch activity monitor to record steps/day over 7 days. The proportion that met the recommended physical activity levels was determined as those accumulating ≥150 minutes/week at ≥100 steps/minute in bouts lasting ≥10 minutes. These proportions were also determined for those with and without knee OA, as classified by radiograph, and by severity of knee pain.
RESULTS
Of the 1788 study participants (age 67 sd 8 yrs, BMI 31 sd 6 kg/m2, 60% female), lower overall percentages of participants with radiographic knee OA and knee pain met recommended physical activity levels. However, these differences were not statistically significant between those with and without knee OA; 7.3% and 10.1% of men (p=0.34), and 6.3% and 7.8% of women (p=0.51), respectively, met recommended physical activity levels. Similarly, for those with moderate/severe pain versus no pain, 12.9% and 10.9% of men (p=0.74) and 6.7% and 11.0% (p=0.40) of women met recommended physical activity levels.
CONCLUSIONS
Disease and pain have little impact on achieving recommended physical activity levels among people with or at high risk of knee OA.
INTRODUCTION
Knee osteoarthritis (OA) is a painful disease present in more than one in ten adults over the age of 60 in the United States, representing the most common form of arthritis.(1) For older adults, knee OA has emerged as an important public health problem. Knee OA is the leading cause of disability in older adults, is linked to an increased risk of all-cause death, and increases in prevalence with aging.(2-4) At present, there are no curative or disease modifying agents for OA. Rather, the goals of treatment are to reduce pain and functional limitation through pharmacologic and non-pharmacologic means.
The health benefits of physical activity are highly relevant for those with knee OA. Walking results in a reduction in knee pain and improvement in functional ability among people with knee OA.(5-7) As a result, national service organizations promote active lifestyles for people with arthritis, including walking. For instance, the Centers for Disease Control and Prevention and the Arthritis Foundation recommend programs such as ‘Walk with Ease’, which was designed to increase physical activity in people with arthritis.(8) At present, walking is the most common type of leisure time physical activity practiced by adults, including those with arthritis,(9-11) and among adults who report meeting national guidelines for physical activity.(12)
In addition to the specific arthritis-related benefits, there are overall health benefits to physical activity. To that end, the Department of Health and Human Services (DHHS) 2008 Physical Activity Guidelines for Americans(13) outlines the minimal recommended intensity and durations needed to achieve such health benefits. In particular, DHHS recommends physical activity that is of at least a moderate intensity (~ 3.0 METs) to achieve health benefits. This is comparable to walking at ≥100 steps/min or roughly ≥2.5 miles/hour.(14-19) This is generally achievable by most people as healthy adults between the ages of 60 and 79 typically walk between 2.5 to 3.0 miles/hour.(20) Furthermore, the DHHS recommends that physical activity should be performed in bouts lasting at least 10 minutes in duration at this intensity. Finally, to fully meet Physical Activity Guidelines recommended by DHHS, at least 150 minutes of physical activity is needed over the course of the week at these intensities and bout durations.
While it has recently been demonstrated that that few people with knee OA actually meet the full 2008 Physical Activity Guidelines for Americans,(21) it is unclear whether the pathology of OA itself and/or knee pain are the reason why so few meet these guidelines. People with knee OA often slow their gait in part to prevent knee pain.(22, 23) Thus, a failure to meet the 2008 Physical Activity Guidelines among those with knee OA could be because of 1) an inability to walk at a recommended intensity; 2) being capable of meeting the intensity requirement, but not being able to sustain walking for the recommended duration; 3) reasons unrelated to knee OA; or 4) a combination of the three. Understanding which of these parameters, i.e., intensity and/or duration, is problematic would help tailor public health efforts to promote physical activity among people with or at high risk of knee OA.
Therefore, we examined the association of radiographic knee OA and knee pain with meeting the 2008 Physical Activity Guidelines for Americans among a group of adults with and without knee OA and knee pain. We also determined the proportions that satisfied the minimal recommended intensity and bout durations specified by the 2008 Physical Activity Guidelines through walking.
METHODS
The Multicenter Osteoarthritis (MOST) Study
This cross-sectional study sample consisted of participants from the MOST study, a large multicenter longitudinal cohort study of community-dwelling participants who have or are at high risk of knee OA.(24) The MOST study sample at baseline included adults aged 50 to 79 years who were recruited from Birmingham, Alabama and Iowa City, Iowa. Inclusion criteria, based on risk for knee OA, included the presence of known risk factors, including being ≥ 50 years of age, reporting a previous knee injury or operation, and having a body weight in excess of the median weight for each age- and sex-specific group based on data from the Framingham OA Study.(25) Study participants were excluded if they required assistance of another person to walk. The MOST study protocol was approved by the institutional review boards at the University of Iowa in Iowa City, University of California in San Francisco, University of Alabama in Birmingham, and Boston University Medical Center. All MOST study participants provided informed consent.
This particular study focused on a subset of the MOST study cohort, restricting our sample to the 1788 individuals who provided objective walking activity data (see below for method of measurement) collected at the 60-month follow-up exam between May of 2009 and January of 2011. This was the first study visit in MOST where objective walking activity data were collected.
StepWatch Activity Monitor
Physical activity was assessed by measuring daily accumulated step counts using a StepWatch activity monitor (Orthocare Innovations, Oklahoma City, OK). This is a small (70 × 50 × 20 mm; 38 g), waterproof, self-contained device that attaches to the ankle and records the number of strides taken every minute while providing no feedback to the user. The number of strides were doubled to provide a count that included steps from both lower limbs. The StepWatch has high concurrent validity in comparison with several reference standard measures of step frequency in older adults, high convergent validity in comparison with SF-36 scores among participants with OA, and high test-retest reliability in adults.(26, 27)
Each study participant was fitted with the StepWatch and provided written and verbal instructions for attaching the monitor each morning and removing it at bedtime for 7 consecutive days (plus part of the day that the participant received the device and the day it was returned). To determine whether participants wore the monitor long enough to be counted as a full day, we adopted a published method for processing accelerometry data(28) and defined 10 hours of monitoring as indicative of a valid day of monitoring. The 10 hour requirement represents more than 66% of waking hours and has been utilized as a minimal standard in studies of physical activity in the general adult population(29) and people with knee OA.(28) Time worn was counted from the first step recorded in the morning to the last step recorded in the evening. To exclude times participants may have taken the StepWatch off during the day, we omitted times where the monitor registered no steps for 180 consecutive minutes during the day.(28, 30) Finally, we restricted our sample to those participants who had a minimum of 3 days of valid data since previous studies have found this to be the minimum number of days needed for a reliable estimate of habitual physical activity.(26, 31)
Study Outcomes
We classified each participant according to their achievement (yes/no) of the 2008 Physical Activity Guidelines for Americans from DHHS.(13) We classified participants who walked at least a single minute at ≥ 100 steps/minute (steps/min) as being capable of meeting the minimal recommended intensity.(14-19) To ascertain the ability to meet the recommended duration of a single bout of continuous activity, we classified participants who walked at least a single bout of ≥10 minutes at this minimal recommended intensity as meeting the minimal recommended duration. To account for short pauses in walking which can occur, for example, while stopping to cross a street, we allowed for interruptions of walking < 100 step/min for 1 or 2 minutes. Lastly, participants accumulating at least 150 minutes of physical activity meeting these minimal intensity and bout durations were classified as achieving the 2008 Physical Activity Guidelines for Americans. For participants with fewer than 7 days of StepWatch data (n = 457), we standardized available data to 7 day (one week) estimates.
To confirm study participants could walk at a minimal recommended intensity, we used data obtained from a 20-meter walk performed at a usual walking pace at the clinic visit. Participants who walked at a self-selected cadence of ≥ 100 steps/minute during the 20-meter walk were classified as being capable of meeting the minimal recommended intensity.
Radiographic Knee OA and Knee Pain
All participants underwent bilateral weight-bearing posteroanterior (PA) and lateral fixed-flexion radiographic evaluations of the knee, as described elsewhere(24). Two experienced readers blinded to clinical data graded joint space narrowing (JSN) and osteophytes using the OARSI atlas(32) in both tibiofemoral (TF) and patellofemoral (PF) joints (both graded 0-3). The TF joint was also graded according to Kellgren and Lawrence (KL) criteria (0-4). Any disagreements between readers were adjudicated by 3 readers to reach consensus. We defined radiographic OA (ROA) of either knee to be present based on radiographic findings in the TF or PF joints. For the TF joint, ROA was defined as a KL grade ≥ 2. For the PF joint, ROA was defined as an osteophyte score ≥ 2, or a JSN score ≥ 2 with any osteophyte, sclerosis, or cyst score of ≥ 1 on the lateral film.(33, 34) The inter-rater reliability measured by weighted kappa for the KL grade was 0.80.
Knee pain was measured as the mean pain in the past 30 days on a Visual Analogue Scale (VAS) ranging from 0 to 100. Subjects with a VAS range of 0-9 were classified as having no pain,10-39/100 as mild pain, and ≥40/100 as moderate/severe pain.(35) Those with two painful knees were categorized according to the more painful knee.
Potential Confounders
The following factors were considered as potential confounders (based on their association with function and physical activity in previous studies(36-38)) and ascertained by interview, questionnaire, and/or direct measurement as appropriate, at the 60-month clinic visit: age, sex, race (Non-White vs. White), education (<some college vs. ≥college), body mass index (BMI) computed from standardized weight and height assessments classified into World Health Organization categories(39, 40), self-reported comorbidities based on the modified Charlson comorbidity index(41) (≥1 vs. none), depressive symptoms measured with the Center for Epidemiologic Studies Depression Scale (CES-D)(42) (≥ 16 vs. < 16), and widespread pain (present vs. absent), defined by the American College of Rheumatology as pain above and below the waist, pain on the right and left sides of the body, and axial pain based upon a standard homunculus.(43)
Statistical Analysis
Given the recognized differences in physical activity patterns by sex, estimates for men and women were computed separately.(29) We calculated means and standard deviations for continuous variables (e.g., the number of steps/day) and proportions for categorical variables (e.g., proportions meeting minimal recommended intensity, bout duration, and the full 2008 Physical Activity Guidelines). We then stratified the sample by knee ROA (absent/present) and knee pain (none, mild, moderate/severe) categories, respectively, and adjusted proportions for each group using generalized linear models with an interaction term for sex to calculate separate estimates for men and women. For the ROA analyses, the proportions were adjusted by the potential confounders listed above as well as study site (Alabama or Iowa) and we did not adjust for knee pain given its role as a likely intermediate in the causal pathway. For the knee pain analysis, the proportions were adjusted for the potential confounders as well as for study site and ROA. All analyses were calculated using SAS for Windows version 9.2 (SAS Institute, Cary, NC).
RESULTS
Of the 2330 MOST participants attending the 60-month follow-up visit, 16% (377) did not agree to wear the StepWatch, and 2% (58) had monitor malfunctions. Of the remaining 1895 participants who wore the StepWatch, 94% (1788/1895) wore it for at least 3 valid days and represent the study sample. In general, participants included in this analysis were more likely to have better health status (e.g., lower BMI, depressive symptoms, less muscular weakness, and fewer comorbidities) compared with those not included in the analysis (data not shown). The mean (sd) age and BMI of the study sample were 67.2 (7.7) years and 30.7 (6.0) kg/m2, respectively. A majority of the participants were women (60%), white (90%), and did not report needing an assistive device while walking (96%). Table 1 presents additional participant characteristics for men, women, and the entire study sample.
Table 1.
Descriptive characteristics of study participants stratified by sex.
| Men | Women | Combined | |
|---|---|---|---|
| n | 718 | 1070 | 1788 |
| Age [Mean (sd) range] | 66.8 (7.9) 55-84 |
67.4 (7.6) 55-84 |
67.2 (7.7) 55-84 |
| BMI [kg/m] [Mean (sd) range] | 30.8 (5.5) 19.6-56.2 |
30.7 (6.3) 18.2-62.4 |
30.7 (6.0) 18.2-62.4 |
| Education [% ≥ College] | 52 | 43 | 47 |
| Race [% White] | 91 | 90 | 90 |
| Knee pain (VAS: 0-100) [Mean (sd)] | 15.3 (18.2) | 21.2 (22.1) | 18.8 (20.9) |
| None (VAS: 0-9) [%] | 47 | 37 | 41 |
| Mild (VAS: 10-39) [%] | 42 | 42 | 42 |
| Moderate/Severe (VAS: ≥ 40) [%] | 11 | 21 | 17 |
| ROA [%] | 53 | 55 | 54 |
| No assistive device use while walking [%] | 97 | 96 | 96 |
| No Comorbidity [%] | 59 | 59 | 59 |
| Study Site [% Alabama] | 39 | 37 | 38 |
| Depressive Symptoms [% CES-D ≥16] | 7 | 11 | 9 |
Abbreviations: BMI = Body Mass Index; VAS= Visual Analogue Scale; ROA= Radiographic Knee Osteoarthritis; CES-D= Center for Epidemiologic Studies Depression Scale
Minimal recommended intensity was met by 91.2% (95% CI 89.2, 93.3) of men and 91.5% (95% CI 89.8, 93.2) of women (i.e., they were able to walk for at least one minute at ≥100 steps/min) by the StepWatch assessment. Using the 20 meter walk in the clinic, minimal recommended intensity was met by 89.8% (95% CI 87.6, 92.0) of men and 94.3% (95% CI 92.9, 95.7) of women (i.e., they were capable of walking at a self-selected cadence of ≥100 step/min during the observed 20-meter walk). Minimal recommended bout duration was met by 33.4% (95% CI 30.0, 36.9) of men and 32.0% (95% CI 29.2, 34.8) of women (i.e., they had at least one bout of walking for ≥10 continuous minutes (allowing for interruptions) at ≥100 steps/min). Six percent (95% CI 4.3, 7.7) of men and 5.0% (95% CI 3.7, 6.3) of women met the 2008 Physical Activity Guidelines with unadjusted analyses. After adjustment for potential confounders, 9.4% (95% CI 6.4, 12.3) of men and 8.2% (95% CI 4.8, 11.6) of women met the 2008 Physical Activity Guidelines (see Table 2). Furthermore, there were no statistically significant differences between men and women in the adjusted prevalences of meeting the minimal recommended intensity, minimal recommended bout duration, or the 2008 Physical Activity Guidelines.
Table 2.
Crude and adjusted* proportions of men and women meeting recommended intensity, bout duration, and the 2008 Physical Activity Guidelines for Americans.
| Men (% [95% CI]) N = 718 |
Women (% [95% CI]) N = 1070 |
|
|---|---|---|
| Minimum recommended intensity | ||
| Unadjusted | 91.2 [89.2, 93.3] | 91.5 [89.8, 93.2] |
| Adjusted* | 83.1 [78.7, 87.4] | 84.7 [80.7, 88.7] |
| Minimum recommended duration | ||
| Unadjusted | 33.4 [30.0, 36.9] | 32.0 [29.2, 34.8] |
| Adjusted* | 39.7 [33.5, 46.0] | 39.7 [35.0, 44.3] |
| 2008 Physical Activity Guidelines for Americans |
||
| Unadjusted | 6.0 [4.3, 7.7] | 5.0 [3.7, 6.3] |
| Adjusted* | 9.4 [6.4, 12.3] | 8.2 [4.8, 11.6] |
Adjusted for age, sex, race, education, Body Mass Index, comorbidity, depressive symptoms, widespread pain, radiographic knee OA, knee pain, and study site with reference values listed on table 1.
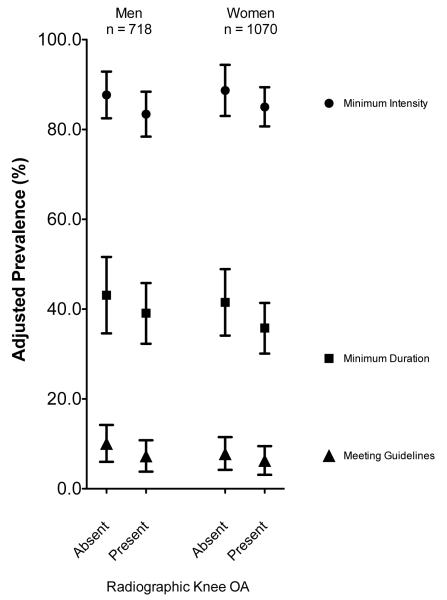
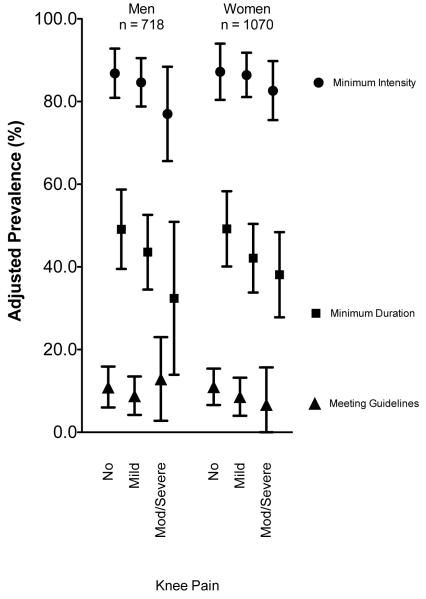
When stratified by ROA and knee pain status, fewer participants with ROA and knee pain met the minimal recommended intensity, the minimal recommended bout duration, or the 2008 Physical Activity Guidelines than their counterparts. However, these differences were small and not statistically significant after adjusting for potential confounders (p>0.05 for all comparisons; see Figures 1 and 2). Specifically, for those with and without ROA, 7.3% and 10.1% of men (p=0.34), and 6.3% and 7.8% of women (p=0.51), respectively, met the 2008 Physical Activity Guidelines. Similarly, for those with no, mild, and moderate/severe knee pain, guidelines were met by 10.9, 8.8, and 12.9% of men and 11.0, 8.6, and 6.7% of women, respectively, which were not statistically significantly different from one another (p >0.05 for all pair-wise comparisons).
Figure 1.
Adjusted* percentages of study participants meeting minimal recommended intensity and bout durations, and the 2008 Physical Activity Guidelines for Americans by ROA presence.
*Adjusted for age, sex, race, education, Body Mass Index, comorbidity, depressive symptoms, widespread pain, and study site.
Using generalized linear models, the differences in proportions meeting the minimal recommended intensity among those with and without ROA were not statistically significant (p=0.23 and 0.29 for men and women, respectively). For the minimal recommended duration, the differences were not statistically significant (p=0.46 and 0.23 for men and women, respectively). Finally, the differences for meeting the 2008 Physical Activity Guidelines were not statistically significant (p=0.34 and 0.51 for men and women, respectively
Figure 2.
Adjusted* percentages of study participants meeting minimal recommended intensity and bout durations, and the 2008 Physical Activity Guidelines for Americans by knee pain presence.
*Adjusted for age, sex, race, education, Body Mass Index, comorbidity, depressive symptoms, widespread pain, radiographic knee OA, and study site.
Using generalized linear models, the differences in proportions meeting the minimal recommended intensity among those with mild and moderate to severe pain were not statistically significant compared with no pain (p=0.59 and 0.14 for men and 0.86 and 0.35 for women). For the minimal recommended duration, the differences were not statistically significant (0.41 and 0.12 for men and 0.25 and 0.13 for women). Finally, the differences for meeting the 2008 Physical Activity Guidelines were not statistically significant (p=0.56 and 0.74 for men, and 0.45 and 0.40 for women).
DISCUSSION
People with or at high risk of knee OA are inactive regardless of the presence of ROA or knee pain. Almost all people with or at high risk of knee OA were able to walk at the minimum intensity of physical activity (as evident both from a clinical walking test and also from free-living objectively monitored behavior) as recommended in the 2008 Physical Activity Guidelines. However, only a third met the minimum bout duration recommendation, and only 9.4% of men and 8.2% of women accumulated enough bouts of sufficient duration and intensity to fully meet the 2008 Physical Activity Guidelines through walking after adjustment for potential confounders.
Neither the disease of OA itself nor knee pain appeared to have substantial impact on the participants’ free-living walking behaviors. In particular, similar proportions of those with and without ROA, and also those with varying degrees of knee pain, met the minimal recommended intensity and bout durations as well as the full 2008 Physical Activity Guidelines after accounting for potential confounders. Any observed differences were minimal (i.e., not meaningfully relevant) and not statistically significant. In other words, participants were similarly inactive regardless of existing ROA or reported pain. For instance among women, the full guidelines were met by 11% with no pain and 6.7% with moderate to severe pain. The low absolute risk difference of 4.3% is arguable small if pain were to have a meaningful impact on one’s ability to meet guidelines. These findings suggest that factors other than disease and/or pain may be responsible for shaping individual walking behaviors. For instance, obesity is relatively common in this sample, and may account for inactivity. On the other hand, similarly low levels of objectively-monitored physical activity are reported for the United States general population. Only 9.5% of men and 7.5% of women between the ages of 20 and 69 years from the National Health and Nutrition Examination Survey (NHANES) met the full 2008 Physical Activity Guidelines for Americans when measured by an accelerometer using similar methodology.(44) Likewise, prevalence estimates are low compared with another large observational study of people with radiographic knee OA, the Osteoarthritis Initiative, which reported only 12.9% of men and 7.7% of women meeting the 2008 Physical Activity Guidelines for Americans.(21)
We find it noteworthy that similarly low levels of physical activity are present in OA cohorts and a sample of the general U.S. population (NHANES), particularly since participants from NHANES were younger on average. This suggests that non-disease factors, such as lifestyle preferences, scheduling, environmental and policy influences likely play important roles in shaping the overall deficiency of sustained bouts of moderate-to-vigorous intensity walking not only among people with or at high risk of knee OA, but also for the overall general population. These findings reflect a broader national public health problem that is not confined to individuals afflicted with OA. Adults in the United States, regardless of health condition, do not appear to accrue enough bouts of moderate-to-vigorous intensity physical activity and consequently are not meeting guidelines. Therefore, while addressing disease and pain may no doubt be beneficial, it may not be the ultimate barrier to the larger overall problem of inactivity in people with knee OA that appears to be more reflective of general inactivity in the population at-large.
We found that most people with or at high risk of knee OA were able to achieve the minimal recommended intensity during walking, but only one out of three walk long enough to accumulate at least 10 minutes in a single bout. Similar prevalences of sustained bouts of physical activity have previously been reported. In the Osteoarthritis Initiative, 60% of men and 43% of women with knee OA recorded at least one bout of physical activity lasting at least 10 minutes,(21) and less than 47% of adults from NHANES accrued at least a single bout lasting at least 10 minutes.(44) Our study findings add that the vast majority of study participants’ usual walking cadence (ascertained during a short distance clinical walking test) is compatible with being able to achieve at least moderate intensity physical activity.(14-19) Therefore, while almost all study participants had sufficient capacity to walk at a minimal recommended intensity, only a third of participants walked at this intensity for at least 10 continuous minutes in free-living conditions.
Limitations of our study should be acknowledged. First, 23% of the MOST study cohort who attended the 60-month visit chose not to wear the accelerometer or provided insufficient data for these analyses. Those included in our study were more likely to have no comorbidities and have fewer depressive symptoms compared with those not included in the analysis. However, the distribution of these characteristics within our sample (n=1788) reflects the overall MOST cohort at the 60 month visit (n=2330). Importantly, the proportions with ROA and different levels of knee pain in our sample were also similar to the overall MOST cohort at the 60 month visit. Furthermore, given that higher levels of physical activity are associated with no comorbidity and fewer depressive symptoms, the true walking levels and patterns among people with or at high risk of knee OA may be even lower than reported. Second, we used step counts as a surrogate marker of overall physical activity and specifically walking activity. Other types of physical activity that involving stepping, such as climbing stairs, could have contributed towards meeting guidelines, though the same intensity and duration criteria needed to be met. Also, pedal strokes while cycling, are recorded as steps by the StepWatch.(45) It is possible that participants engaged in physical activity that did not generate any steps (such as cycling or swimming) or produced relatively few steps (such as gardening and other chores). It is unlikely MOST study participants performed these non-stepping activities with any regularity based upon data collected about other physical activities. Study participants completed the Physical Activities Scale of the Elderly at the MOST baseline visit five years earlier and only 9% of men and 7% of women reported engaging in strenuous non-ambulatory activities such as swimming ‘often’. Given that the prevalence of participating in physical activities other than walking decreases with age and walking for physical activity increases with age,(46) it is unlikely that study participants spent substantially more time in these types of activities at the 60-month visit. Third, participants may have changed daily walking habits with the knowledge that their habitual walking was being recorded. Previous research suggests that this “testing effect” is greatest when participants wear an unsealed monitor, i.e., when participants are aware of how many steps are being recorded.(47) We believe any increases in daily walking due to a testing effect were minimized since the StepWatch did not display recorded data to study participants. Moreover, the bias would again be away from the null if it were present, meaning that true walking would be lower than reported. Fourth, the definition of 100 steps/min as a measure of a minimal recommended intensity is not intended to be a precise measure of moderate intensity, but rather a general physical activity promotion benchmark.(14) Finally, we did not use a separate cadence cut-point for vigorous activity for meeting the 2008 Physical Activity Guidelines since so few participants walked at a vigorous intensity. Conservatively estimating that a vigorous intensity corresponds to 130 steps/min,(16) less than 1% of study participants walked at this intensity for at least one minute, and none walked at this intensity for a single bout of ≥10 continuous minutes.
There are several implications given our study findings. First, the primary barrier to physical activity and meeting guidelines may not be pain and structural disease in people with or at risk of knee OA. Rather, barriers common to the general population, such as a lack of time, activity preferences, reliance on cars for transportation, and urban design are likely more important for physical activity and meeting guidelines.(48, 49) Clinically, a sole focus on reducing knee pain through various intervention modalities may not result in substantial improvements in physical activity to recommended levels unless factors contributing to inactivity more generally are also addressed. More research is needed to identify non-disease factors that can bring about behavioral changes in participation in daily physical activity.
Second, these findings support a strategy that encourages people with or at high risk of knee OA to first increase the duration of walking bouts, and then to accumulate additional frequent bouts throughout the week to meet the 2008 Physical Activity Guidelines. In particular, as only a third accumulated at least a single bout of ≥10 minutes of walking at the recommended intensity, people with or at risk of knee OA should be encouraged to persist for longer durations than they are currently walking. Emphasis on meeting a moderate intensity of walking does not appear to be necessary since most people meet this intensity naturally walking at their usual pace (both in the clinic and also in free-living conditions). This is noteworthy since evidence suggests that gauging physical activity intensity is challenging.(50) Providing a concrete example of ‘moderate intensity’ as likely being compatible with their existing walking particularly when performed in at least 10-minute bouts and repeated throughout the week may serve to encourage people with or at high risk of knee OA that the 2008 Physical Activity Guidelines are more attainable than perhaps was initially believed. While attaining the full guidelines is likely challenging when starting a walking program for people with knee pain, health benefits occur in a dose-response fashion. The 2008 Physical Activity Guidelines for Americans state that “some physical activity is better than none” and additional health benefits occur with more physical activity.(13) For people with symptomatic knee OA, previous randomized controlled trials have demonstrated that walking for 30 to 40 minutes a day three times a week, i.e., less than what is recommended, still results in a decrease in knee pain and improved physical function.(6, 7) These findings bolster the importance of encouraging frequent walking for longer durations even if not able to meet the full 2008 Physical Activity Guidelines for Americans.
Conclusions
These data demonstrate that the proportion of people with or at high risk of knee OA meeting the minimal recommended intensity and bout durations as well as the 2008 Physical Activity Guidelines did not differ significantly based upon the presence of knee OA or pain severity. Our findings imply that most people with or at high risk of knee OA are capable of walking at a cadence associated with intensity recommendations needed to meet the 2008 Physical Activity Guidelines, but only a third persist at this behavior in free-living conditions long enough to accrue a single 10-minute bout. These findings suggest that factors beyond knee OA-related impairments contribute to not meeting the 2008 Physical Activity Guidelines. Since intensity of walking does not seem to be an impediment, our findings support encouraging people with or a high risk of knee OA to walk more frequently and for longer durations to reap the multiple benefits of a physically active lifestyle.
Acknowledgements
Study contributors. We would like to acknowledge Michael LaValley, PhD his consultative role in the analysis of study data. We also acknowledge Michael Cannamela, BS for programming of the StepWatch data which was used for analysis.
Funding/Support: Supported by NIH AG18820, AG 18832, AG 18947, AG 19069, AR007598, NIH AR47885, NIAMS K23AR055127, ACR/REF Rheumatology Investigator, Award, Arthritis Foundation Arthritis Investigator Award, Boston Claude D. Pepper Older Americans Independence Center (P30-AG031679), and the Foundation for Physical Therapy.
Role of the Sponsor: None of the funders of this manuscript had any role in the design and conduct of this study; collection, management, analysis, and interpretation of the data; or preparation of the manuscript.
REFERENCES
- 1.Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26(3):355–69. doi: 10.1016/j.cger.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006;54(1):226–9. doi: 10.1002/art.21562. [DOI] [PubMed] [Google Scholar]
- 3.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84(3):351–8. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nuesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Juni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ. 2011;342:d1165. doi: 10.1136/bmj.d1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 6.Ettinger WH, Jr., Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST) Jama. 1997;277(1):25–31. [PubMed] [Google Scholar]
- 7.Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004;50(5):1501–10. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 8.Intervention Programs. 2011 [cited; Available from: http://www.cdc.gov/arthritis/interventions.htm.
- 9.Yusuf HR, Croft JB, Giles WH, Anda RF, Casper ML, Caspersen CJ, et al. Leisure-time physical activity among older adults. United States, 1990. Arch Intern Med. 1996;156(12):1321–6. [PubMed] [Google Scholar]
- 10.Rafferty A, Reeves M, McGee H, Pivarnik J. Compliance with physical activity recommendations by walking for exercise - Michigan, 1996 and 1998. MMWR Morb Mortal Wkly Rep. 2000;49:560–5. [PubMed] [Google Scholar]
- 11.Hootman JM, Macera CA, Ham SA, Helmick CG, Sniezek JE. Physical activity levels among the general US adult population and in adults with and without arthritis. Arthritis Rheum. 2003;49(1):129–35. doi: 10.1002/art.10911. [DOI] [PubMed] [Google Scholar]
- 12.Simpson ME, Serdula M, Galuska DA, Gillespie C, Donehoo R, Macera C, et al. Walking trends among U.S. adults: the Behavioral Risk Factor Surveillance System, 1987-2000. Am J Prev Med. 2003;25(2):95–100. doi: 10.1016/s0749-3797(03)00112-0. [DOI] [PubMed] [Google Scholar]
- 13.2008 physical activity guidelines for Americans. [cited 2/1/2010]; Available from: http://www.health.gov/PAGuidelines.
- 14.Marshall SJ, Levy SS, Tudor-Locke CE, Kolkhorst FW, Wooten KM, Ji M, et al. Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 minutes. Am J Prev Med. 2009;36(5):410–5. doi: 10.1016/j.amepre.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Tudor-Locke C, Brashear MM, Johnson WD, Katzmarzyk PT. Accelerometer profiles of physical activity and inactivity in normal weight, overweight, and obese U.S. men and women. Int J Behav Nutr Phys Act. 2010;7:60. doi: 10.1186/1479-5868-7-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tudor-Locke C, Fau-Sisson SB, Sisson Sb, Fau-Collova T, Collova T, Fau-Lee SM, Lee Sm, Fau-Swan PD, Swan PD. Pedometer-determined step count guidelines for classifying walking intensity in a young ostensibly healthy population. Can J Appl Physiol. 2005;6(30):666–76. doi: 10.1139/h05-147. [DOI] [PubMed] [Google Scholar]
- 17.Tudor-Locke C, Jones R, Myers AM, Paterson DH, Ecclestone NA. Contribution of structured exercise class participation and informal walking for exercise to daily physical activity in community-dwelling older adults. Res Q Exerc Sport. 2002;73(3):350–6. doi: 10.1080/02701367.2002.10609031. [DOI] [PubMed] [Google Scholar]
- 18.Welk GJ, Differding JA, Thompson RW, Blair SN, Dziura J, Hart P. The utility of the Digi-walker step counter to assess daily physical activity patterns. Med Sci Sports Exerc. 2000;32(9 Suppl):S481–8. doi: 10.1097/00005768-200009001-00007. [DOI] [PubMed] [Google Scholar]
- 19.Wilde BE, Sidman CL, Corbin CB. A 10,000-step count as a physical activity target for sedentary women. Res Q Exerc Sport. 2001;72(4):411–4. doi: 10.1080/02701367.2001.10608977. [DOI] [PubMed] [Google Scholar]
- 20.Bohannon RW, Williams Andrews A. Normal walking speed: a descriptive meta-analysis. Physiotherapy. 2011;97(3):182–9. doi: 10.1016/j.physio.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 21.Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, et al. Objective physical activity measurement in the osteoarthritis initiative: Are guidelines being met? Arthritis Rheum. 2011;63(11):3372–82. doi: 10.1002/art.30562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mundermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52(9):2835–44. doi: 10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- 23.Mundermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: reduced walking speed. Arthritis Rheum. 2004;50(4):1172–8. doi: 10.1002/art.20132. [DOI] [PubMed] [Google Scholar]
- 24.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56(9):2986–92. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 25.Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988;109(1):18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- 26.Mudge S, Taylor D, Chang O, Wong R. Test-retest reliability of the StepWatch Activity Monitor outputs in healthy adults. J Phys Act Health. 7(5):671–6. doi: 10.1123/jpah.7.5.671. [DOI] [PubMed] [Google Scholar]
- 27.Resnick B, Nahm ES, Orwig D, Zimmerman SS, Magaziner J. Measurement of activity in older adults: reliability and validity of the Step Activity Monitor. J Nurs Meas. 2001;9(3):275–90. [PubMed] [Google Scholar]
- 28.Song J, Semanik P, Sharma L, Chang RW, Hochberg MC, Mysiw WJ, et al. Assessing physical activity in persons with knee osteoarthritis using accelerometers: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2010;62(12):1724–32. doi: 10.1002/acr.20305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 30.King WC, Li J, Leishear K, Mitchell JE, Belle SH. Determining activity monitor wear time: an influential decision rule. J Phys Act Health. 8(4):566–80. doi: 10.1123/jpah.8.4.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 Suppl):S531–43. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 32.Altman RD, Hochberg M, Murphy WA, Jr., Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995;3(Suppl A):3–70. [PubMed] [Google Scholar]
- 33.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Felson DT, McAlindon TE, Anderson JJ, Naimark A, Weissman BW, Aliabadi P, et al. Defining radiographic osteoarthritis for the whole knee. Osteoarthritis Cartilage. 1997;5(4):241–50. doi: 10.1016/s1063-4584(97)80020-9. [DOI] [PubMed] [Google Scholar]
- 35.White DK, Zhang Y, Felson DT, Niu J, Keysor JJ, Nevitt MC, et al. The independent effect of pain in one versus two knees on the presence of low physical function in a multicenter knee osteoarthritis study. Arthritis Care Res (Hoboken) 2010;62(7):938–43. doi: 10.1002/acr.20166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guccione AA, Felson DT, Anderson JJ. Defining arthritis and measuring functional status in elders: methodological issues in the study of disease and physical disability. Am J Public Health. 1990;80(8):945–9. doi: 10.2105/ajph.80.8.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jordan J, Luta G, Renner J, Dragomir A, Hochberg M, Fryer J. Knee pain and knee osteoarthritis severity in self-reported task specific disability: the Johnston County Osteoarthritis Project. J Rheumatol. 1997;24(7):1344–9. [PubMed] [Google Scholar]
- 38.Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48(12):3359–70. doi: 10.1002/art.11420. [DOI] [PubMed] [Google Scholar]
- 39.WHO . Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. WHO Technical Report Series 894. World Health Organization; Geneva: 2000. [PubMed] [Google Scholar]
- 40.National Institutes of Health Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 41.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 42.Radloff L. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 43.Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. Report of the Multicenter Criteria Committee The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Arthritis Rheum. 1990;33(2):160–72. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 44.Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: adults compliance with the Physical Activity Guidelines for Americans. Am J Prev Med. 2011;40(4):454–61. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 45.Karabulut M, Crouter SE, Bassett DR., Jr Comparison of two waist-mounted and two ankle-mounted electronic pedometers. Eur J Appl Physiol. 2005;95(4):335–43. doi: 10.1007/s00421-005-0018-3. [DOI] [PubMed] [Google Scholar]
- 46.Siegel PZ, Brackbill RM, Heath GW. The epidemiology of walking for exercise: implications for promoting activity among sedentary groups. Am J Public Health. 1995;85(5):706–10. doi: 10.2105/ajph.85.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clemes SA, Parker RA. Increasing our understanding of reactivity to pedometers in adults. Med Sci Sports Exerc. 2009;41(3):674–80. doi: 10.1249/MSS.0b013e31818cae32. [DOI] [PubMed] [Google Scholar]
- 48.Strazdins L, Broom DH, Banwell C, McDonald T, Skeat H. Time limits? Reflecting and responding to time barriers for healthy, active living in Australia. Health Promot Int. 2011;26(1):46–54. doi: 10.1093/heapro/daq060. [DOI] [PubMed] [Google Scholar]
- 49.Serour M, Alqhenaei H, Al-Saqabi S, Mustafa AR, Ben-Nakhi A. Cultural factors and patients’ adherence to lifestyle measures. Br J Gen Pract. 2007;57(537):291–5. [PMC free article] [PubMed] [Google Scholar]
- 50.Rice KR, Heesch KC, Dinger MK, Fields DA. Effects of 2 brief interventions on women’s understanding of moderate-intensity physical activity. J Phys Act Health. 2008;5(1):58–73. doi: 10.1123/jpah.5.1.58. [DOI] [PubMed] [Google Scholar]