Abstract
OBJECTIVES
While lower Model for End-Stage Liver Disease (MELD) scores due to lower levels of serum creatinine in women might account for some gender disparity in liver transplant (LT) rates, even within MELD scores, women are transplanted at lower rates than men. It is unclear what causes this disparity, but transplant candidate-donor liver size mismatch may be a factor.
METHODS
We analyzed Organ Procurement and Transplantation Network data for patients with end-stage liver disease on the waiting list. Pooled conditional logistic regression analysis was used to assess the association between gender and LT and determine the degree to which this association was explained by lower MELD scores or liver size.
RESULTS
A total of 28,866 patients and 424,001 person-months were included in the analysis. Median estimated liver volume (eLV) and liver weight (eLW) were significantly lower in women than in men on the LT waiting list (P<0.0001). Controlling for region and blood type, women were 25% less likely to receive LT in a given month compared to men (P<0.0001). When MELD was included in the model, the odds ratio (OR) for gender increased to 0.84 suggesting that 9 percentage points of the 25% gender disparity was due to MELD score. When eLV was added to the model, there was an additional 3% increase in OR of gender suggesting that transplant candidate-donor liver size mismatch is an underlying factor for lower LT rates in women compared to men (OR=0.87, P<0.0001).
CONCLUSIONS
Lower LT rates among women on the waiting list can be explained in part by lower MELD scores, eLV and eLW than those of men. However; at least half of the gender disparity still remains unexplained.
Keywords: Liver transplantation, end-stage liver disease, gender disparity, MELD, liver volume, liver weight
INTRODUCTION
Due to organ shortage, donor livers should be allocated to patients with the greatest need. Before implementation of the Model for End-Stage Liver Disease (MELD) 1 in February 2002, liver allocation was based on total waiting time on the liver transplant (LT) list, Child-Turcotte-Pugh score and hospital status 2, 3. In 2002, with the implementation of MELD score that consists of three objective laboratory parameters, fairness in liver allocation improved and mortality rates on the LT waiting list decreased 4. However, recent studies have revealed significantly lower LT and higher mortality rates in women on the United Network for Organ Sharing (UNOS) LT waiting list compared to men 5–7.
Our recent study that investigated gender disparity on the LT waiting list confirmed the results of these earlier studies 6. We estimated that LT rates were 25% lower in women and identified serum creatinine as a potential cause for these lower rates 6. Our results suggested that lower LT rates in women were in part due to the use of serum creatinine in calculating MELD scores and that this led to higher mortality rates 6. However, we also found that gender disparity persisted even within MELD scores 6. Several other reports have also noted lower transplant rates in women even after accounting for MELD scores 7, 8.
The explanation for the disparity in LT rates between men and women remains unclear 6. The hypothesis that liver donor size mismatch contributes to lower LT rates in women compared to men was previously postulated 6, 7, 9, 10. Lai et al. 10 included transplant candidates’ height as a surrogate marker for liver size in the multivariate model and found that women still had lower LT rates after controlling for height 10. To reassess the hypothesis that the liver donor size mismatch contributes to lower LT rates in women compared to men, we compared men and women on the US LT waiting list with respect to rates of receiving a liver transplant, adjusting for estimated liver size of the transplant candidate in addition to potential confounders.
METHODS
Study Population
We analyzed Organ Procurement and Transplantation Network data [Standard Transplant Analysis and Research (STAR) files] as of August 2009. We excluded patients who were younger than 18 years, diagnosed with a liver disease other than ESLD, listed on the waiting list before MELD implementation (February 27, 2002), as an exceptional case (e.g. those with hepatocellular carcinoma who received a priority MELD score) or status 1 and those who received living-donor LT, who were removed from the LT waiting list due to reasons other than death, transplantation, improved or deteriorated condition (e.g. listing in error, refusal of transplant, multiple listings) and those who had missing or biologically implausible height (< 122 cm or > 213 cm) and weight measurements (< 34 kg or > 227 kg) as defined by Das et al. 11. After these exclusions, there were 38,143 patients who fulfilled our study criteria. To avoid potential overestimation of liver volume and weight, we also excluded those who had more than slight ascites (in UNOS dataset, ascites was categorized as 1) absent, 2) slight ascites, and 3) moderate ascites) and missing data on the degree of ascites at listing (9277 patients). After exclusion of patients who had more than slight ascites, a final study cohort comprised of a total of 28,866 patients.
Variables
The variables included in the analysis were patient code, waiting list registration code, registration date, last follow-up date, gender, age at registration, ethnicity/race, diagnosis, reason for removal from the waiting list, registration and updated MELD score, exception status, UNOS region, ABO blood type, weight and height at listing and degree of ascites at listing.
Estimated liver volume (eLV) was calculated using the formulas developed by Urata et al. 12, Vauthey et al.13 and Heinemann et al. 14. Estimated liver weight (eLW) was calculated using the formula developed by Yoshizumi et al. 15, Chouker et al. 16 and Deland et al. 17. Body surface area (BSA) was calculated using formulas developed by DuBois et al. 18 and Mosteller et al. 19 to be used in calculation of eLV and eLW, respectively. Liver volume and weight estimates were included in regression models as categorical variables with 8 categories in order to avoid making a linearity assumption.
Statistical Analysis
For statistical analysis, we used SAS software, Version 9.2, (Cary, NC, USA) 20 and Minitab statistical software (Minitab, Inc., State College, PA) 21. To assess association between gender and LT and to determine the degree to which the association was explained by lower MELD scores or liver volume or liver weight, we used discrete survival analysis (pooled logistic regression) 22, 23 for which we reformatted UNOS dataset into one record per person-month of experience on the LT waiting list 6. Each person-month record in the dataset contained information on the most recent measures of laboratory, clinical variables and current MELD score. In addition, each record indicated whether the individual received a transplant during that month. We excluded person-months that patients were temporarily inactive on the LT waiting list. The person-month dataset was analyzed using logistic regression with transplant as the outcome. This pooled logistic regression was shown to result in approximately the same estimates and standard errors as Cox regression 24 with the advantages that it is easier to model the hazard, explore non-linearities and include time-varying predictor variables 23. In this analysis, we used conditional logistic regression, conditioning on exact MELD score and region to tightly control for these variables without making modeling assumptions. In contrast to previous analyses 6, 10, we chose not to use a competing risk approach because our goal was not to estimate the probability that a person will receive a transplant (which can be affected by mortality rates). Rather, it was to determine the effect of patient characteristics on monthly transplantation rates.
To assess the degree to which various degrees of measurement error in our estimate of liver volume could have had an impact on our adjusted estimates of the female/male transplant rate disparity, we re-estimated the gender disparity after correcting for varying hypothetical degrees of measurement error. To do this, we used the methods of Rosner et al. 25 as implemented in a SAS Macro developed by Spiegelman et al. 26. To use this software for specified degrees of measurement error, we simulated large hypothetical external validation sets embodying varying degrees of measurement error.
We used Wilcoxon Rank-Sum and Chi-square tests to assess differences of quantitative and categorical variables, respectively between women and men.
RESULTS
Clinical Characteristics of Patients with ESLD on the LT Waiting List
A total of 28,866 patients and 424,001 person-months were included in the analysis. Table 1 shows the main characteristics of our study population (Table 1). The median weight, height and BSA were significantly lower in women compared to men (Table 1). The median eLV and median eLW were significantly lower in women than in men on the LT waiting list (Table 2). The median LV estimated based on formula developed by Urata et al. 12 and LW estimated based on formula developed by Yoshizumi et al. 15 and Chouker et al. 16 for the study population were 1390 ml, 1539 g and 2078 g, respectively. For each category below the median value of eLV and eLW, the proportion of women was higher than that of men.
Table 1.
Characteristics of 28,866 Patients with ESLD on the LT Waiting List Registered between February 27, 2002 and August 25, 2009
| Patient Characteristics | Women (n=10741) | Men (n=18125) | |||
|---|---|---|---|---|---|
|
| |||||
| Median | Quartile Range | Median | Quartile Range | P Value | |
| Age at Listing (y) | 54 | 11 | 53 | 10 | <0.0001 |
| BSA at Registration based on Formula Developed by Dubois et al. 18 (m2) | 1.78 | 0.28 | 2.06 | 0.28 | <0.0001 |
| BSA at Registration Based on Formula Developed by Mosteller et al. 19 (m2) | 1.81 | 0.31 | 2.08 | 0.31 | <0.0001 |
| Body Mass Index (kg/m2) at Listing | 27.88 | 8.70 | 28.33 | 6.98 | <0.0001 |
| Height at Listing (cm) | 162.56 | 10.16 | 177.80 | 10.88 | <0.0001 |
| Weight at Listing (kg) | 73.00 | 23.78 | 88.45 | 24.04 | <0.0001 |
| MELD Score at Listing | 14 | 8 | 15 | 8 | <0.0001 |
|
| |||||
| Number | % | Number | % | P Value | |
|
| |||||
| Race/Ethnicity | <0.0001 | ||||
| White | 7497 | 70 | 13387 | 74 | |
| Black | 942 | 9 | 1275 | 7 | |
| Hispanic | 1851 | 17 | 2779 | 15 | |
| Asian | 315 | 3 | 498 | 3 | |
| Others | 136 | 1 | 186 | 1 | |
| Etiology of Cirrhosis | <0.0001 | ||||
| Autoimmune Hepatitis | 926 | 9 | 320 | 2 | |
| Cryptogenic | 1475 | 14 | 1689 | 9 | |
| Alcohol | 1388 | 13 | 4282 | 24 | |
| Hepatitis B | 181 | 2 | 667 | 4 | |
| Hepatitis C | 4147 | 39 | 9621 | 53 | |
| Nonalcoholic Fatty Liver Disease | 946 | 9 | 819 | 5 | |
| Primary Biliary Cirrhosis | 1354 | 13 | 209 | 1 | |
| Primary Sclerosing Cholangitis | 16 | 0 | 32 | 0 | |
| Others | 308 | 3 | 486 | 3 | |
| ABO Blood Type | 0.014 | ||||
| A | 3860 | 36 | 6796 | 38 | |
| AB | 399 | 4 | 736 | 4 | |
| B | 1327 | 12 | 2180 | 12 | |
| O | 5155 | 48 | 8413 | 46 | |
| UNOS Region | <0.0001 | ||||
| 1 | 342 | 3 | 767 | 4 | |
| 2 | 1043 | 10 | 2064 | 11 | |
| 3 | 1287 | 12 | 2229 | 12 | |
| 4 | 1543 | 14 | 2030 | 11 | |
| 5 | 2039 | 19 | 3345 | 18 | |
| 6 | 330 | 3 | 607 | 3 | |
| 7 | 952 | 9 | 1512 | 8 | |
| 8 | 693 | 6 | 1111 | 6 | |
| 9 | 854 | 8 | 1458 | 8 | |
| 10 | 871 | 8 | 1365 | 8 | |
| 11 | 787 | 7 | 1637 | 9 | |
Table 2.
Estimated Liver Volume (eLV) and Estimated Liver Weight (eLW) of Patients with ESLD on the LT Waiting List
| eLV or eLW | Women (n=10741) | Men (n=18125) | |||
|---|---|---|---|---|---|
|
| |||||
| Median | Quartile Range | Median | Quartile Range | P Value | |
| eLV based on Formula Developed by Urata et al.12 (ml) | 1259.36 | 195.44 | 1455.46 | 197.44 | <0.0001 |
| eLW based on Formula Developed by Yoshimuzi et al. 15 (g) | 1398.91 | 241.45 | 1609.29 | 237.98 | <0.0001 |
| eLW based on Formula Developed by Chouker et al. 16 (g) | 1868.74 | 411.50 | 2199.45 | 476.35 | <0.0001 |
| eLV based on Formula Developed by Vauthey et al. 13 (cm3) | 1501.97 | 396.35 | 1847.32 | 390.66 | <0.0001 |
| eLV based on Formula Developed by Heinemann et al. 14 (ml) | 1563.78 | 296.90 | 1861.66 | 299.94 | <0.0001 |
| eLW based on Formula Developed by Deland et al. 17 (kg) | 1.60 | 0.28 | 1.88 | 0.29 | <0.0001 |
Liver Transplant Rates
There were a total of 12,444 transplants with 424,001 person-months of follow-up. The overall LT rate on the waiting list was 0.35 per person-year. Women had lower LT rates compared to men (0.29 vs. 0.39 per person-year, P<0.0001).
Liver Transplant Rates by eLV and eLW among Women and Men with ESLD on the LT Waiting List
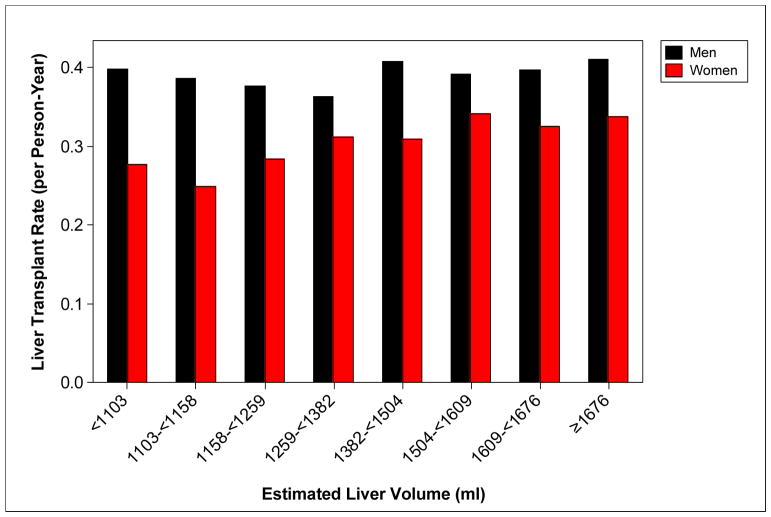
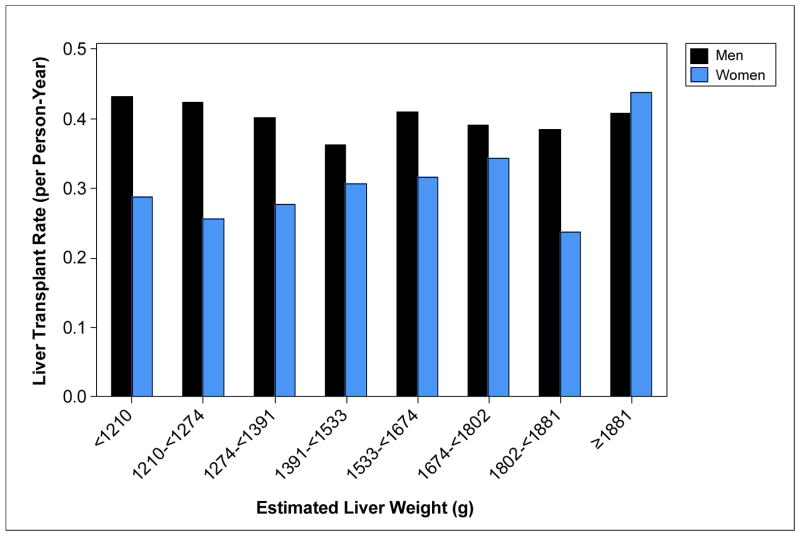
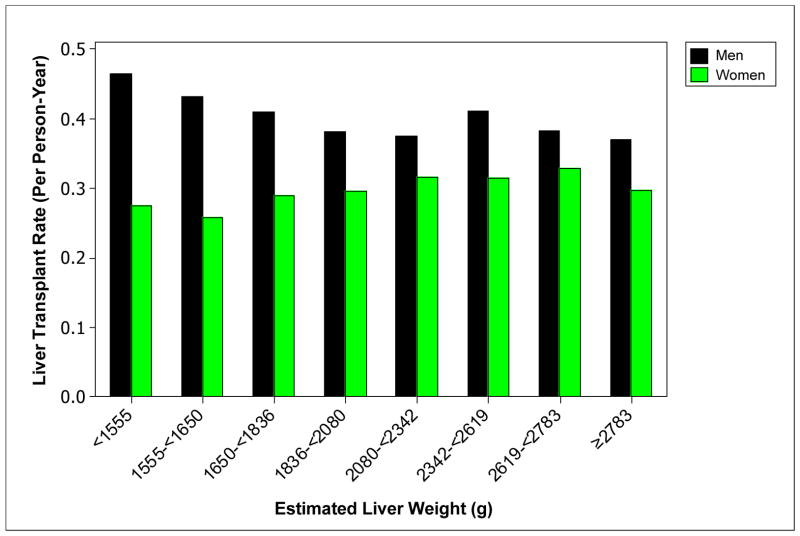
Figure 1, 2, and 3 shows LT rates by LV estimated based on formula developed by Urata et al. 12 and LW estimated based on formulas developed by Yoshizumi et al. 15 and Chouker et al. 16, respectively among women and men with ESLD on the LT waiting list. In each stratum defined by liver size or volume, men had substantially higher transplant rates than women. The figures suggest that the gender disparity is greatest among those with the lowest liver size or volume.
Figure 1.
LT Rates by Liver Volume Estimated Based on Formula Developed by Urata et al. 12 among Women and Men with ESLD on the LT Waiting List
Figure 2.
LT Rates by Liver Weight Estimated Based on Formula Developed by Yoshizumi et al.15 among Women and Men with ESLD on the LT Waiting List
Figure 3.
LT Rates by Liver Weight Estimated Based on Formula Developed by Chouker et al.16 among Women and Men with ESLD on the LT Waiting List
Multivariate Analysis
Table 3 shows the results of fitting multivariable pooled conditional logistic models and the contribution of MELD score, eLV and eLW to gender disparity (Table 3). Controlling for region and ABO blood type only, women had 25% lower monthly transplant rate compared to men [Odds Ratio (OR)=0.75, confidence interval (CI): 0.722 to 0.779, P<0.0001]. When MELD was included in the model, the OR for gender increased to 0.84 suggesting that 9 percentage points of 25% gender disparity was due to MELD score (OR=0.84, CI: 0.803 to 0.876, P<0.0001). When eLV based on formula developed by Urata et al. 12 was added to the model, as a categorical variable with 8 classes, there was an additional 3% increase in the OR of gender (OR=0.87, CI: 0.827 to 0.917, P<0.0001) suggesting that transplant candidate-donor liver size mismatch can be one of the factors for lower transplantation rates in women compared to men (13 percentage points of 25% gender disparity remained unknown). We obtained similar results when we included eLW’s based on formula developed by Yoshizumi et al. 15 (OR=0.86, CI: 0.821 to 0.906, P<0.0001), Chouker et al. 16 (OR=0.86, CI: 0.815 to 0.897, P<0.0001), DeLand et al.17(OR=0.87, CI:0.829 to 0.919, P<0.0001) and eLV’s based on formula developed by Heinemann et al. 14 (OR=0.87, CI: 0.828 to 0.917, P<0.0001) and Vauthey et al. 13 (OR=0.86, CI: 0.821 to 0.906, P<0.0001) in place of eLV estimated based on formula developed by Urata et al. 12 in the multivariable model controlled for region, blood type and MELD score.
Table 3.
Factors by which the LT Rates are Lower in Women than Men, Controlling for other Variables Using Pooled Logistic Regression
| Variables Controlled For | Female/Male Transplant Odds Ratio on the Liver Transplant Waiting List | P Value |
|---|---|---|
| Gender + UNOS Region + Blood Type | 0.75 | <0.0001 |
| Gender + UNOS Region + Blood Type + MELD | 0.84 | <0.0001 |
| Gender + UNOS Region + Blood Type + MELD + eLV1 | 0.87 | <0.0001 |
| Gender + UNOS Region + Blood Type + MELD + eLW2 | 0.86 | <0.0001 |
| Gender + UNOS Region + Blood Type + MELD + eLW3 | 0.86 | <0.0001 |
| Gender + UNOS Region + Blood Type + MELD + eLV4 | 0.87 | <0.0001 |
| Gender + UNOS Region + Blood Type + MELD + eLV5 | 0.86 | <0.0001 |
| Gender + UNOS Region + Blood Type + MELD + eLW6 | 0.87 | <0.0001 |
eLV based on Formula Developed by Urata et al. 12 (ml)
eLW based on Formula Developed by Yoshimuzi et al.15 (g)
eLW based on Formula Developed by Chouker et al. 16 (g)
eLV based on Formula Developed by Heinemann et al. 14 (ml)
eLV based on Formula Developed by Vauthey et al. 13 (ml)
eLW based on Formula Developed by DeLand et al. 17 (kg)
In exploratory work requested by the reviewers of this paper, we examined the effect of controlling for the individual components of MELD (bilirubin, INR, and creatinine) on the transplant disparity. When bilirubin was added to a model which included region and blood type, the gender disparity became greater (OR=0.66, P<0.0001). However, when creatinine or INR were added to the model individually, in each case the disparity diminished (OR=0.83 in each case, P<0.0001).
Sensitivity Analysis to Assess the Possible Impact of Measurement Error
We assessed the degree to which these estimates might be affected by varying degrees of measurement error in our estimates of liver volume. To perform this analysis, we started by refitting the model, treating liver volume as continuous. From that model, adjusting for MELD, region, blood type and estimated liver volume, we found a 15% gender disparity. If the correlation between the eLV and the true liver volume was 80%, the estimate of the gender disparity corrected for measurement error was found to be 13%. If the correlation between eLV and true liver volume was poor (60%), the corrected estimate of disparity was 9%.
DISCUSSION
The hypothesis that liver size mismatch between liver transplant candidate and donor could explain the lower transplantation rates in women on the LT waiting list compared to men was previously postulated by other authors 6, 7, 9, 10. Our results suggest that this is true to some extent. However, the contribution of liver size to the gender disparity appears relatively small and does not explain a large portion of disparity. In this study, our goal was not to estimate the probability that a person will receive a transplant; but rather, it was to determine the effect of patient characteristics on monthly transplantation rates. After taking into account region and blood type, we observed that monthly rate of a transplant was 25% lower for women than men with ESLD on the LT waiting list. Lower MELD scores explain part of this disparity, as after controlling for MELD score, the disparity was reduced to 16%. Finally, after adjusting for the eLV and eLW of the transplant candidate, LT rates in women were still 13% lower than in men. Our results are also consistent with those of Lai et al. 10 who, using a different analysis, found that women had a 12% lower LT rate after controlling for MELD and height.
Although our analysis showed that lower LT rates in women were in part due to liver size in addition to MELD score, explanation for half of the 25% gender disparity still remains unclear. One can speculate that age or etiology of cirrhosis may play a role in this gender disparity, but once a transplant candidate is registered on the LT waiting list with a designated MELD score, demographic or clinical characteristics such as age, etiology of cirrhosis, race do not play any role in liver allocation. We would like to emphasize that these clinical characteristics (e.g. age, race, diagnosis) may play a role on the mortality on the LT waiting list, but they should have no effect on the LT allocation as in the US, the allocation of livers from deceased donors are dependent only on MELD score, ABO blood type and UNOS region. Therefore, in multivariable analysis, we did not control for variables other than MELD score, ABO blood type, UNOS region and liver size.
As the information on the actual size of the transplant candidate livers was not available in the database, we estimated liver size by several formulas previously published. The estimations using these formulas resulted in similar liver sizes and outcomes (Table 2 and 3). As these formulas required transplant candidate body weight or BSA to estimate liver volume and weight, we excluded transplant candidates who had more than slight ascites or missing data on ascites to prevent overestimation of liver volume and liver weight. This may have resulted in selection bias. However; when we repeated our multivariate analysis without excluding those with more than slight ascites or missing data on ascites, we obtained similar results.
Our study had limitations as it was a retrospective analysis. As UNOS database did not have information on actual liver size, we estimated liver weight and volume based on previously published formulas. Using these formulas, we may have underestimated or overestimated the size of the liver. However, our sensitivity analysis provides some assurance that the observed disparity is not simply due to liver size estimation error.
Each of these formulas for liver size and weight has strengths and limitations. The formula developed by Urata et al. 12 was derived from a relatively small number of Japanese subjects in whom the majority was pediatric population. The actual liver volume was measured by computed tomography (CT) 12. The greatest strength of this formula was that among all six estimating formulas, it had the highest R2 (the multivariable model for liver volume explained 96% of change in actual liver volume) 12. The formula developed by Yoshizumi et al. 15 had the largest sample size and was derived from US population of cadaveric liver donors with a large range of age. The formula developed by Chouker et al.16 was derived from autopsies and was the only one that took into account age and gender for subjects between ages of 16 and 50 years of age old and only age for those between 51 and 70 in addition to weight, respectively. In addition, in the study of Chouker et al.16, there was no information regarding whether they excluded the cases with heart failure or shock; livers obtained from autopsies may weight heavier than actual liver weight due to hepatic congestion if there is any involvement of congestive heart failure or shock prior to death. In fact, the highest median liver weight in our study was obtained by using formula derived by Chouker et al. 16 (Table 2 and Figure 3). Heinemann et al. 14 derived an estimating formula from large number of autopsies of Caucasian subjects. However, the R2 of their formula was small 14. Vauthey et al. 13 developed a formula by measuring liver volume using CT in North American and European subjects and excluded Asians and African-Americans. In the study conducted by Deland et al.17, there was no information regarding whether the weight of the gallbladder and hepatic attachments were excluded when the liver weight was measured and R2 of the formula was not reported. As mentioned, all these estimating formulas differ in populations, measurement techniques, and inclusion and exclusion criteria12–17. In order to minimize potential bias that can occur due to these variations among these formulas, we estimated liver weight and volume by not only one formula, but using six independent estimating formulas. We repeated our multivariable analysis by using these different formulas to reduce bias in our results. Each of these formulas resulted in similar outcomes.
As the information on the transplant candidates’ weight and height were not available at the last follow-up on the LT waiting list in the dataset, we estimated liver size based on the weight, height and degree of ascites available at registration on the LT waiting list. Although LT candidates’ weight and ascites are dynamic variables and may change during the stay on the waiting list, these changes should have a minor effect on estimation of liver size as we excluded those who had more than slight ascites and with missing data on ascites.
To our knowledge, this is the first study that showed that LT candidate liver size contributes to disparity on lower LT rates among women on the LT waiting list. We showed that women had significantly lower median eLV and eLW than in men on the LT waiting list and were significantly less likely to receive LT than men. Lower transplantation rates among women on the LT waiting list can be explained in part by lower MELD scores and lower eLV and eLW compared to men. As suggested by Myers et al. 8, this portion of the transplant disparity attributed to MELD might be diminished if MELD was based on eGFR rather than serum creatinine. Finally, even after accounting for MELD and estimated liver size, approximately half of the 25% gender disparity remains unexplained.
Acknowledgments
FUNDING
“The project described was supported by Grant Number 5 K23 DK089008-02 from the National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (to Ayse L. Mindikoglu, M.D., M.P.H.) and its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the NIH”
“This work was supported in part by Health Resources and Services Administration contract 234-2005-370011C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government”.
ABBREVIATIONS
- MELD
Model for End-Stage Liver Disease
- LT
Liver Transplant
- OR
Odds Ratio
- UNOS
United Network for Organ Sharing
- STAR
Standard Transplant Analysis and Research
- ESLD
End-Stage Liver Disease
- eLV
Estimated Liver Volume
- eLW
Estimated Liver Weight
- BSA
Body Surface Area
Footnotes
MEETING MATERIAL
Mindikoglu AL, Magder LS. Impact of Estimated Liver Volume on Gender Disparity in Liver Transplantation Rates among Patients with End-Stage Liver Disease on the Liver Transplant Waiting List. Hepatology 2011; 54 (Suppl 1): 167A (Abstract # 622). Abstract was selected as a Presidential Poster of Distinction and presented at The Liver Meeting 2011 of the American Association for the Study of Liver Diseases (AASLD), San Francisco, California.
References
- 1. [Accessed on February 15, 2009];Allocation of livers. Available at http://www.unos.org/PoliciesandBylaws2/policies/pdfs/policy_8.pdf.
- 2.Coombes JM, Trotter JF. Development of the allocation system for deceased donor liver transplantation. Clin Med Res. 2005;3:87–92. doi: 10.3121/cmr.3.2.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman RB, Jr, Wiesner RH, Harper A, McDiarmid SV, Lake J, Edwards E, Merion R, Wolfe R, Turcotte J, Teperman L. The new liver allocation system: moving toward evidence-based transplantation policy. Liver Transpl. 2002;8:851–8. doi: 10.1053/jlts.2002.35927. [DOI] [PubMed] [Google Scholar]
- 4.Austin MT, Poulose BK, Ray WA, Arbogast PG, Feurer ID, Pinson CW. Model for end-stage liver disease: did the new liver allocation policy affect waiting list mortality? Arch Surg. 2007;142:1079–85. doi: 10.1001/archsurg.142.11.1079. [DOI] [PubMed] [Google Scholar]
- 5.Kanwal F, Dulai GS, Gralnek IM, Han SB, Spiegel BM. The impact of gender on access to liver transplantation in the MELD era. Gastroenterology. 2005;128:A701. [Google Scholar]
- 6.Mindikoglu AL, Regev A, Seliger SL, Magder LS. Gender disparity in liver transplant waiting-list mortality: the importance of kidney function. Liver Transpl. 2010;16:1147–57. doi: 10.1002/lt.22121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moylan CA, Brady CW, Johnson JL, Smith AD, Tuttle-Newhall JE, Muir AJ. Disparities in liver transplantation before and after introduction of the MELD score. JAMA. 2008;300:2371–8. doi: 10.1001/jama.2008.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myers RP, Shaheen AA, Aspinall AI, Quinn RR, Burak KW. Gender, renal function, and outcomes on the liver transplant waiting list: assessment of revised MELD including estimated glomerular filtration rate. J Hepatol. 2011;54:462–70. doi: 10.1016/j.jhep.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 9.Axelrod DA, Pomfret EA. Race and sex disparities in liver transplantation: progress toward achieving equal access? JAMA. 2008;300:2425–6. doi: 10.1001/jama.2008.732. [DOI] [PubMed] [Google Scholar]
- 10.Lai JC, Terrault NA, Vittinghoff E, Biggins SW. Height contributes to the gender difference in wait-list mortality under the MELD-based liver allocation system. Am J Transplant. 2010;10:2658–64. doi: 10.1111/j.1600-6143.2010.03326.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Das SR, Kinsinger LS, Yancy WS, Jr, Wang A, Ciesco E, Burdick M, Yevich SJ. Obesity prevalence among veterans at Veterans Affairs medical facilities. Am J Prev Med. 2005;28:291–4. doi: 10.1016/j.amepre.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Urata K, Kawasaki S, Matsunami H, Hashikura Y, Ikegami T, Ishizone S, Momose Y, Komiyama A, Makuuchi M. Calculation of child and adult standard liver volume for liver transplantation. Hepatology. 1995;21:1317–21. [PubMed] [Google Scholar]
- 13.Vauthey JN, Abdalla EK, Doherty DA, Gertsch P, Fenstermacher MJ, Loyer EM, Lerut J, Materne R, Wang X, Encarnacion A, Herron D, Mathey C, Ferrari G, Charnsangavej C, Do KA, Denys A. Body surface area and body weight predict total liver volume in Western adults. Liver Transpl. 2002;8:233–40. doi: 10.1053/jlts.2002.31654. [DOI] [PubMed] [Google Scholar]
- 14.Heinemann A, Wischhusen F, Puschel K, Rogiers X. Standard liver volume in the Caucasian population. Liver Transpl Surg. 1999;5:366–8. doi: 10.1002/lt.500050516. [DOI] [PubMed] [Google Scholar]
- 15.Yoshizumi T, Gondolesi GE, Bodian CA, Jeon H, Schwartz ME, Fishbein TM, Miller CM, Emre S. A simple new formula to assess liver weight. Transplant Proc. 2003;35:1415–20. doi: 10.1016/s0041-1345(03)00482-2. [DOI] [PubMed] [Google Scholar]
- 16.Chouker A, Martignoni A, Dugas M, Eisenmenger W, Schauer R, Kaufmann I, Schelling G, Lohe F, Jauch KW, Peter K, Thiel M. Estimation of liver size for liver transplantation: the impact of age and gender. Liver Transpl. 2004;10:678–85. doi: 10.1002/lt.20113. [DOI] [PubMed] [Google Scholar]
- 17.DeLand FH, North WA. Relationship between liver size and body size. Radiology. 1968;91:1195–8. doi: 10.1148/91.6.1195. [DOI] [PubMed] [Google Scholar]
- 18.DuBois D, DuBois EF. A formula to estimate the approximate surface area if height and weight be known. Arch Int Med. 1916;17:863–71. [Google Scholar]
- 19.Mosteller RD. Simplified calculation of body-surface area. N Engl J Med. 1987;317:1098. doi: 10.1056/NEJM198710223171717. [DOI] [PubMed] [Google Scholar]
- 20.SAS software. Http://www.Sas.Com/. The data analysis for this paper was generated using SAS software, Version 9.2 of the SAS System for Windows. Copyright © 2002–2008 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
- 21.Minitab 15 Statistical Software (2007). [Computer software]. State College, PA: Minitab, Inc. (www.minitab.com)
- 22.Allison PD. Discrete-time methods for the analysis of event-histories. In: Leinhardt S, editor. Sociological Methodology. San Francisco: Jossey-Bass; 1982. pp. 61–98. [Google Scholar]
- 23.D’Agostino RB, Lee ML, Belanger AJ, Cupples LA, Anderson K, Kannel WB. Relation of pooled logistic regression to time dependent Cox regression analysis: the Framingham Heart Study. Stat Med. 1990;9:1501–15. doi: 10.1002/sim.4780091214. [DOI] [PubMed] [Google Scholar]
- 24.Cox DR. Regression models and life-table. [Accessed on October 13, 2012];J Royal Stati Soci B. 1972 34:187–220. Available at http://www.stat.rutgers.edu/home/rebecka/Stat687/cox.pdf. [Google Scholar]
- 25.Rosner B, Spiegelman D, Willett WC. Correction of logistic regression relative risk estimates and confidence intervals for measurement error: the case of multiple covariates measured with error. Am J Epidemiol. 1990;132:734–45. doi: 10.1093/oxfordjournals.aje.a115715. [DOI] [PubMed] [Google Scholar]
- 26. [Accessed on May 23, 2012];%Blinplus Macro. Available at http://www.hsph.harvard.edu/faculty/donna-spiegelman/software/blinplus-macro/