Abstract
This manuscript describes the functional status trajectory of older (age 65 or older) and younger (age 18–64) adults after Lung Transplantation (LT). After the implementation of the Lung Allocation Score (LAS) in 2005, older adults became the fastest growing subgroup of recipients. Yet the impact of LT on physical function, a main determinant of quality of life in older adults, is unknown. We conducted a retrospective cohort study using United Network for Organ Sharing data on 4805 adults who received a LT during 2005–2009. We divided them into older (≥65, n=774) and younger (18–64, n=4031) cohorts. Functional status was measured by Karnofsky Performance Score (KPS). Mixed models estimated the impact of age group on the rate of functional decline starting at one-year post-transplantation. We controlled for KPS at transplantation, gender, race, diagnosis, LAS and LT type. Age group was not associated with different rates of decline in KPS over time. On average, recipients who were older, received a single LT, or had a low KPS at transplantation had worse functional status post-transplantation when compared to their counterparts, but rarely reached disability at 48-months. Overall, LT had a positive and durable effect on physical function for both older and younger recipients.
Keywords: Age, elderly patients, lung transplantation, United Network for Organ Sharing, activities of daily living
INTRODUCTION
The discipline of adult lung transplantation (LT) in the United States (U.S.) has evolved rapidly since the institution of the Lung Allocation Score (LAS) system in 2005, especially for the subgroup of older recipients (65 or older). The number of older recipients in the year 2011 was 480 (27% of all adult LT), compared to 81 (6.9%) in 2004(1). The LAS algorithm uses the predicted wait-list urgency (one-year survival if not transplanted) and the predicted survival at one-year post-transplantation to produce a score (0–100) that reflects the net transplantation benefit. By design, the LAS system gives preference to older patients, those with diseases that deteriorate quickly resulting in high wait-list mortality and patients with high likelihood of survival post-transplantation. In the post LAS era compared to the pre LAS era, Idiopathic Pulmonary Fibrosis (IPF) traded places with Chronic Obstructive Pulmonary Disease (COPD) as the leading diagnosis for adult LT, candidates of older age and higher co-morbidity index were accepted for transplantation, the overall wait-time for active candidates shortened, and the survival while on wait-list improved. The one-year post-transplantation survival also improved, except for recipients older than 70 who had 2–3 times the likelihood of dying compared to those younger than 70 (1–5).
Most older adults value “quality over quantity” of years remaining to live(6, 7). Quality of life in old age reflects good physical and functional health, independence (control over one’s own life), positive attitude towards life and its events (psychological state), social activities and networking, and financial stability(8). The literature to date on older LT recipients has focused on survival, leaving a substantial gap in the knowledge of the aforementioned geriatric outcomes that contribute to quality of life (9).
In this investigation, we were particularly interested in understanding how older recipients fared following transplantation with regard to physical function and independence. On the one hand, older recipients represent a relatively robust group because in order to receive an organ, they must have high estimated one-year post-transplantation survival despite their age disadvantage. On the other hand, older adults are generally at increased risk of functional decline due to the effects of normal aging and the accumulation of disease. Both IPF and COPD are often accompanied by conditions such as coronary artery disease, diabetes, sleep apnea, osteoporosis, malnutrition, depression, anxiety, frailty, falls, medication interaction and adverse drug events(10, 11). These co-morbidities could impact the physical function and psychological well-being of older recipients before and after LT.
The primary aim of this study is to analyze the long-term (1–5 years post-transplantation) trajectory of physical function among LT recipients in the post LAS era, specifically comparing the trajectories of older (65 and older) to younger (age 18–64) recipients. A secondary aim is to compare the functional trajectories of the subgroups of recipients aged 65–69 to those 70 or older, and recipients of single vs. bilateral LT. Lastly, we describe survival and relevant complications of older and younger recipients.
METHODS
The design was a retrospective cohort study using the clinical registry prospectively collected by the United Network for Organ Sharing (UNOS) on adults who received a LT in the U.S. from May 1st 2005 to December 31st 2009. We specifically employed data obtained at transplantation and during follow-up visits.
We selected 4805 adults (18 or older) who received their first LT (no simultaneous solid organ transplantation) during the study period, survived at least 11-months post-transplantation, and had functional status data at transplantation and once or more after 11-months post-transplantation. We wanted to focus on long-term (1–5 years post-transplantation) trajectories to minimize bias from perioperative complications. Lung transplantation recipients, similar to older adults recovering from other major surgeries (12–18), typically have a period of disability immediately post-surgery followed by functional recovery and rehabilitation. The course of this period is variable, but our analyses assume (based on our clinical experience) that the majority of older recipients reach their “peak” post-transplantation function within a year of the surgery such that functional trajectories thereafter reflect long-term well-being rather than factors influenced by perioperative complications. We began our analysis at 11-months because most recipients in the registry who survived the first year after transplantation had a follow-up visit within 1 month from their one-year transplantation anniversary. The sample was divided by age into older (age ≥65, n=774) and younger (age 18–64, n=4031) cohorts. Encrypted patient and center codes were used to allow examination of patient level data and institutional volume. IRB approval was obtained and the research was conducted in accordance with the Declarations of Helsinki.
The UNOS clinical dataset contained nearly 450 perioperative and 90 follow-up variables. Several variables were considered relevant to our analysis but discarded due to high percentage (>30) of missing data: oxygen requirement, pCO2, 6 min-walk distance, prior hospitalization, hypertension, peptic ulcer disease, coronary artery disease and peripheral vascular disease at registry, and bone disease and hypertension at follow-up. The remaining relevant variables were grouped in the following categories: demographics (age, gender, race [white and non-white], education level [greater or lower than high-school], working status and BMI); co-existent conditions (diabetes mellitus, malignancy, creatinine at transplantation, and cerebrovascular accident [CVA]); acuity of lung disease (% predicted forced expiratory volume and forced vital capacity, LAS and ventilator support at transplantation); transplantation diagnosis (LAS group and disease specific) and LT procedure type (single lung transplantation [SLT] vs. bilateral lung transplantation [BLT]). We derived a center volume variable using the encrypted institution identifiers in the UNOS dataset. Based on their mean annual volume of adult LT, centers were categorized as large (≥20 cases) or small (1–19 cases) volume centers. The cut-off of 20 was chosen because it has been shown to predict 30-day post-transplantation survival (19).
The primary endpoint was rate of change in functional status from year one to five post-transplantation. Physical function was measured by Karnofsky Performance score (KPS), a clinician-rated measure developed in 1948 for oncology patients. The score is an estimate of the patient’s ability to carry out his/her normal life activities and work, or to accomplish self-care with none, some or complete assistance. KPS increases by 10 points from 0 to 100 as the level of independence improves and the symptoms of disease resolve. The description of each score and a suggested comparison to the Eastern Cooperative Group is shown in table 1. The KPS questionnaire has been validated across different population settings including older adults with chronic diseases. In these individuals, a score of 60 or less is a cut-point associated with a higher risk for hospitalizations, repeated clinic visits, functional impairment, institutionalization, and death(20).
Table 1.
Conversion Table Eastern Cooperative Group to Karnofsky Performance Score.
| EASTERN COOPERATIVE GROUP PERFORMANCE SCORE (ECOG) | KARNOFSKY PERFORMANCE SCORE (KPS) |
|---|---|
| 0: Able to carry all pre-disease performance without restriction. | 100: Normal no complaints; no evidence of disease. |
| 1: Restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, e.g., light house work, office work. | 90: Able to carry on normal activity; minor signs or symptoms of disease. |
| 80: Normal activity with effort; some signs or symptoms of disease. | |
| 2: Ambulatory and capable of all self-care but unable to carry out any work activities. Up and about more than 50% of waking hours | 70: Cares for self; unable to carry on normal activity or to do active work. |
| 60: Requires occasional assistance, but is able to care for most of his personal needs. | |
| 3: Capable of only limited self-care, confined to bed or chair more than 50% of waking hours | 50: Requires considerable assistance and frequent medical care. |
| 40: Disabled; requires special care and assistance. | |
| 4: Completely disabled. Cannot carry on any self-care. Totally confined to bed or chair | 30: Severely disabled; hospital admission is indicated although death not imminent |
| 20: Very sick; hospital admission necessary; active supportive treatment necessary. | |
| 10: Moribund; fatal processes progressing rapidly. | |
| 5: Dead | 0: Dead |
Modified from: Oken, M.M. et al. AJCO 1982 (1) and Ma, C. et al. EJC 2010(2). Both ECOG and KPS are clinician-rated instruments that measure functional status. In older adults with chronic diseases a KPS of 60 is associated with a greater risk for hospitalizations, nursing home placement and death (3).
Secondary endpoints included: survival, cause of death, indicators of short-term (<90 days) post-surgical complications (acute kidney injury on hemodyalisis, acute rejection) and long-term (≥1 year) outcomes (diabetes mellitus, end-stage renal disease on hemodyalisis, CVA, and bronchiolitis obliterans syndrome [BO]).
Statistical Analyses
To depict the cohort, descriptive statistics for continuous variables were summarized as medians (25%, 75%) and for categorical variables as number (%) with the trait.
Kaplan-Meier estimates were used to describe the survival distribution conditional on having survived to 11-months post-transplantation. Recipients still alive at their last clinic visit were censored at that follow-up date. The probability (95% CI) of survival post-transplantation was estimated at 12-month intervals starting at 11-months post-transplantation, up to 60 months. Estimates were obtained for the two age group strata and the log-rank test was used to test for the statistical significance between the survival curve distributions.
For the primary analysis we were interested in characterizing the trend of KPS over time for the two age groups beginning at 11-months post-transplantation. As described before, we chose 11-months as the starting point to minimize bias from perioperative complications. To evaluate the relationship between the age group trajectories and to obtain estimates of predicted KPS means over time, we used a random coefficient linear mixed model. The mixed effects model included time since transplantation, an indicator for age group, and KPS at transplantation (tKPS). We also controlled for center volume, LT procedure type (SLT or BLT), gender, race, LAS at transplantation and LAS diagnosis group. An age group by time interaction variable was originally added to the model to determine if the pattern of change in the mean KPS over time was the same across age groups. Interactions involving tKPS, center volume and LT procedure type were also added since they were considered potential moderators. Ultimately, the only interaction found to be significant and maintained in the final model was between center volume and time.
The model allowed intercepts and slopes to vary by patient by including these as random effects. We also included a facility-level random intercept to account for possible correlation among patients in the same transplantation center. A graphical representation of functional status over time and its relationship with age group and tKPS was obtained by displaying population lines using the parameter estimates obtained from a simplified model containing age group, tKPS and time only. We constructed lines for three clinically relevant levels of tKPS: 10 = near death, rapidly progressive disease; 60 = score associated with higher risk for hospitalizations, nursing home placement and death; 100 = no symptoms of disease.
Similar to the primary analysis, a subgroup analysis was performed comparing functional status over time between recipients aged 65–69 and those 70 and older. The same methodology and covariates were used. Different from the main model where the center volume by time interaction was significant, in the subgroup analysis model the only interaction that maintained statistical significance was center volume by tKPS. A similar graph was also created, only now comparing the older (age 65–69) versus oldest (age ≥70) cohorts.
Analyses were conducted with SAS software version 9.2 (Cary, NC); p value ≤ 0.05 indicated statistical significance.
RESULTS
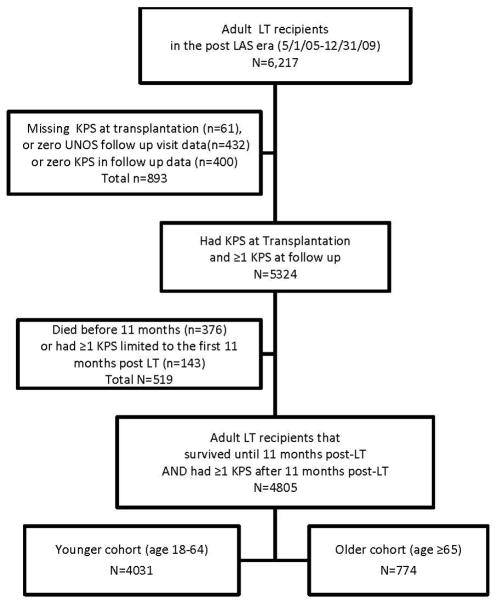
There were 6217 adults that received their first LT during the study period. See figure 1. We excluded recipients missing all UNOS follow-up files (n=400), or missing tKPS (n=61) or follow-up KPS (total n=575; 432 with zero follow-up KPS measurements and 143 whose follow-up KPS measurements occurred only before 11-months post-transplantation). Additionally, we excluded recipients that died before 11-months post-transplantation (n=376). The recipients with missing functional status data (n=1036) differed from the final study sample (n=4805) in age (median [interquartile range] for excluded = 58 [15] vs. final cohort = 57 [15], p=0.008), LAS at transplantation (median [interquartile range] for excluded = 39.8 [15.3] vs. final cohort = 37.8 [11.5], p<0.0001), and LAS diagnosis group (percentage [number] in each diagnosis group for the excluded vs. final cohort were: A= 36.2% [375] vs. 39.9% [1918], B= 4.7% [49] vs. 4% [192], C= 11.4% [118] vs. 12.9% [618], D= 43.7% [453] vs. 40.5% [1946] and Other= 4% [41] vs. 7% [131] respectively, p=0.016). The recipients who died before 11-months differed from the final cohort only in age (excluded = 61 [12] vs. final cohort = 57 ([15], p<0.0001).
Figure 1. Consort diagram for sample selection using data from the United Network for Organ Sharing registry.
Abbreviations: Lung transplantation (LT), Karnofsky Performance Score (KPS), United Network for Organ Sharing (UNOS)
Baseline characteristics and perioperative complications
The proportion of older recipients increased over time from 11% in 2006 to 23% in 2009. See table 2 for the characteristics at transplantation for all recipients stratified by age group. Older recipients were mostly white-males transplanted for IPF. The percentage (number) of African Americans in the older group was 3.4% (26) vs. 10.0% (405) in the younger group. Hispanics comprised 4% (31) of older recipients and 5% (202) of younger recipients. Both cohorts had similar proportions of co-morbid diseases except for malignancy which was higher in the older group. The acuity of lung disease differed only by a higher proportion of younger recipients needing ventilator support at transplantation. Five of every six recipients needed assistance with self-care (KPS 10–70). The younger group spent double the time on wait-list than the older group. The median (25%, 75%) days spent on wait-list by age group and diagnosis were: 29 (12, 108) for older IPF, 53 (15, 161) younger IPF, 69 (28,232) older COPD and 113 (34, 340) younger COPD.
Table 2.
Baseline Characteristics of Younger (Age 18–64) and Older (Age ≥65) Adult Lung Transplantation Recipients
| VARIABLE | YOUNGER COHORT (n=4031) | OLDER COHORT (n=774) | P value |
|---|---|---|---|
| Age (years) | 55.0 (45.0,60.0) | 67.0 (65.0,69.0) | <0.0001 |
| Female | 1758 (43.6) | 246 (31.8) | <0.0001 |
| White | 3363 (83.4) | 695 (89.8) | <0.0001 |
| Greater than high school education (N miss=652) | 1816 (45.1) | 386 (49.9) | 0.0467 |
| Working for income | 705 (17.5) | 100 (12.9) | <0.0001 |
| LAS diagnosis group | |||
| Group A (obstructive lung disease) | 1627 (40.4) | 291 (37.6) | <0.0001 |
| Group B (pulmonary vascular disease) | 172 (4.3) | 20 (2.6) | |
| Group C (CF or immunodeficiency) | 617 (15.3) | 1 (0.1) | |
| Group D (restrictive lung disease) | 1495 (37.1) | 451 (58.3) | |
| Other | 120 (3.0) | 11 (1.4) | |
| Primary disease specific diagnosis | |||
| COPD/emphysema | 1209 (30.0) | 270 (34.9) | <0.0001 |
| Idiopathic pulmonary fibrosis | 1156 (28.7) | 419 (54.1) | |
| Other | 1666 (41.3) | 85 (11.0) | |
| %Predicted FEV, median | 29.0 (19.0,48.0) | 45.0 (27.0,62.0) | <0.0001 |
| %Predicted FVC, median | 45.0 (35.0,58.0) | 53.0 (41.0,65.0) | <0.0001 |
| Type of Lung Transplantation | |||
| Single | 1227 (30.4) | 486 (62.8) | <0.0001 |
| Double | 2804 (69.6) | 288 (37.2) | |
| Disability level (KPS at transplantation) | |||
| No assistance self-care (KPS 80–100) | 652 (16.2) | 127 (16.4) | 0.0149 |
| Minimal assistance self-care (KPS 50–70) | 2553 (63.3) | 523 (67.6) | |
| Full assistance self-care (KPS 10–40) | 826 (20.5) | 124 (16.0) | |
| BMI | 24.7 (20.8,28.3) | 26.1 (23.0,28.9) | <0.0001 |
| LAS at transplantation | 37.7 (33.7,45.0) | 39.0 (33.9,47.1) | 0.0138 |
| Days on waiting list | 87.0 (26.0,270.0) | 45.0 (16.0,135.0) | <0.0001 |
| Time to last follow-up or death (years) | 2.7 (1.7,3.9) | 2.0 (1.1,3.0) | <0.0001 |
Values are summarized as number (percent) or median (25th, 75th percentile) and P values were obtained using Wilcoxon Rank Sums (continuous) and chi square (categorical) tests.
Abbreviations: Lung Transplantation (LT), Cystic fibrosis (CF), Lung allocation Score (LAS), Chronic Obstructive Pulmonary Disease (COPD), Forced Vital Capacity (FVC), Forced Expiratory Volume (FEV), Karnofsky Performance Score (KPS).
These recipients survived to 11 months after Lung Transplantation and had available Karnofsky Performance Score reported thereafter.
Six of every ten candidates in the older group had a SLT and seven of every ten candidates in the younger group had a BLT. The rates of complications prior to discharge for the older and younger cohorts were: graft rejection 5.9% and 9.7 %; acute kidney injury on hemodyalisis 0.9% and 2.5%; CVA 1.0% and 1.4%.
Trajectory of Functional Status from 1-Year Post-transplantation
There were 4805 recipients included in the main model (age ≥65 [n=774], and age 18–64 [n=4031]). Figures 2–3 depict the observed mean values of KPS over time by groups of age and level of function at transplantation. The mean KPS at one-year post-transplantation was better than at transplantation for all types of recipients. Table 3 describes the final linear model for the prediction of post-transplantation KPS using baseline characteristics. If we apply this model to a hypothetical case of a 65 year-old white-female with COPD (LAS group A), a tKPS of 10 and LAS of 30 who received a SLT at a small-volume center and survived to 5-years post-transplantation, we estimate that at 5-years, her KPS will be 60 (59.078). If we apply the model to a 55 year-old non-white male with IPF (LAS group D), a tKPS of 80 and LAS of 30, who received a BLT from a large-volume center, we estimate he will have a KPS of 80 (79.991) at 5-years. Figure 4 depicts unadjusted functional status trajectories for older and younger recipients by levels of tKPS.
Figure 2. Boxplot Kamofsky Performance Score (mean ± standard deviation) overtime for Adult Lung Transplantation Recipients by level of Function at Transplantation.
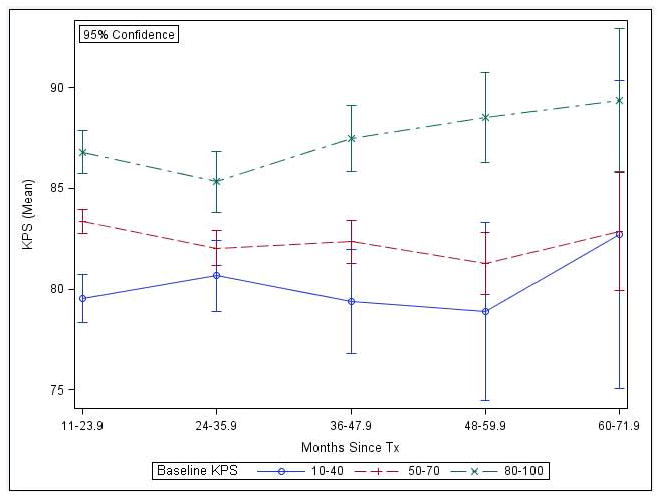
The levels of function represented are: 1) full assistance with self-care = KPS 10–40; 2) minimal assistance with self-care = KPS 50–70; 3) No assistance with self-care = 80–100. The groups did not reach ad KPS ≤ 60 at 48 months post-transplantation. The confidence intervals are wider for the group requiring full assistance with care at transplantation (KPS 10–40) and for all groups after 48 months. Abbreviations: Karnofsky Performance Score (KPS), lung transplantation (LT).
Figure 3. Boxplot of Karnofsky Performance Score (mean ± standard deviation) overtime for Younger (Age 18–64) and Older (Age ≥65) Adult Lung Transplantation Recipients.
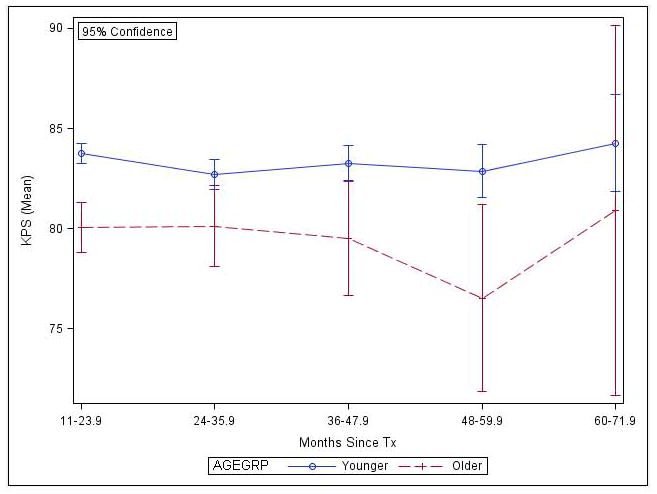
Younger and older Lung Transplantation recipients rarely reached a KPS ≤60 at 48 months post-transplantation. The confidence intervals for the older group widen over time, especially after 48 months.
Table 3.
Multivariable Linear Mixed Model for prediction of long-term Functional Status as measured by Karnofsky Performance Score
| KPS = 75.711 − 2.081 (a) + 0.128 (b) + 0.825 (c) + 2.6 (p) − 3.217 (t) + 1.178(c)(t) − 0.682 (g) + 0.039 (r) + 0.027 (I) + 0.086 (d_a) + 0.810 (d_b) + 2.378 (d_c) −0.824 (d_o). |
| a = age (0 for 18–64, 1 for ≥65), b = KPS at transplantation, c = center volume (0 for 1–19 LT per year, 1 for ≥20 LT per year), p = LT procedure type (0 for SLT, 1 for BLT), t = years after transplantation, g = gender (0 for male, 1 for female), r = race (0 for non-white, 1 for white), I = LAS at transplantation, d = LAS diagnosis group (0 for d_d, 1 for d_a, b or c). |
We tested several interactions including age group, time after transplantation, KPS at transplantation, center volume and LT procedure type but kept only the interaction found to be significant (p <0.05) in the final model, center volume by time interaction. The model allowed random effects for the intercepts and slopes by patient and facility level to account for possible correlation among patients in the same transplantation center.
Abbreviations: Karnofsky Performance Score (KPS), Lung transplantation (LT), Single LT (SLT), bilateral LT (BLT), Lung allocation score (LAS).
Figure 4. Long-term Functional Trajectory of Younger (age 18–64) and Older (age ≥65) Lung Transplantation Recipients by level of Function at Transplantation.
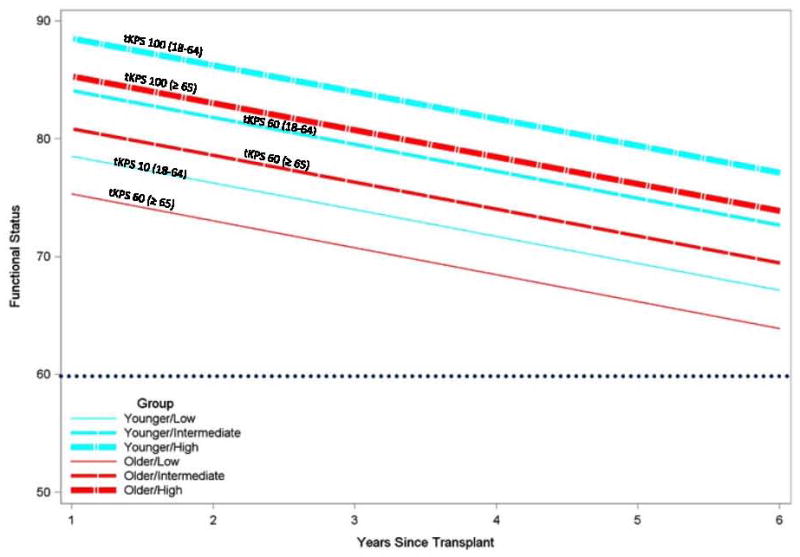
Functional status (y axis) was measured using Karnofsky Performance Score (KPS). The dotted line represents a clinically predictive cut off for higher risk for hospitalization, nursing home placement and death in older adults. Levels of functional status at transplantation (tKPS) are: Low = tKPS 10, intermediate = tKPS 60 and high = tKPS 100. This model used age group as main independent variable and time and tKPS as covariates.
On average, the post-transplantation KPS was 2.081 points higher for younger than older recipients (p=0.0020), 2.6 points higher for BLT than SLT recipients (p<0.0001); and 1.28 points higher with every 10 points higher tKPS (p<0.0001). In the subsequent years, the mean KPS declined by 3.217 points each year (p<0.0001) for both older and younger recipients, independent of tKPS, LAS, LT procedure type, gender, race or LAS diagnosis group. On average, recipients at large-volume centers had a slower decline in KPS over time (p=0.0026). Gender, race, LAS and LAS diagnosis group did not predict KPS post-transplantation.
The subgroup analysis of recipients aged 65 to 69 (n=634) and 70 and older (n=140) showed no significant difference in the rate of decline in KPS post-transplantation while controlling for tKPS, LAS, LT procedure type, LAS diagnosis group, gender and race. On average, the post-transplantation KPS was 3.854 points lower for recipients aged70 or older than those aged 65–69 (p=0.0177) and 3.462 points higher for BLT compared to SLT recipients (p=0.0157). A higher tKPS was associated with a slower decline in post-transplantation KPS for recipients of large-volume centers (p=0.0028). Figure 5 illustrates unadjusted functional status trajectories for recipients aged 65–69 and 70 or older by level of tKPS.
Figure 5. Long-term Functional Status Trajectories for the Older (age 64–69) and the Oldest (age ≥70) Lung Transplantation Recipients by level of Function at Transplantation.
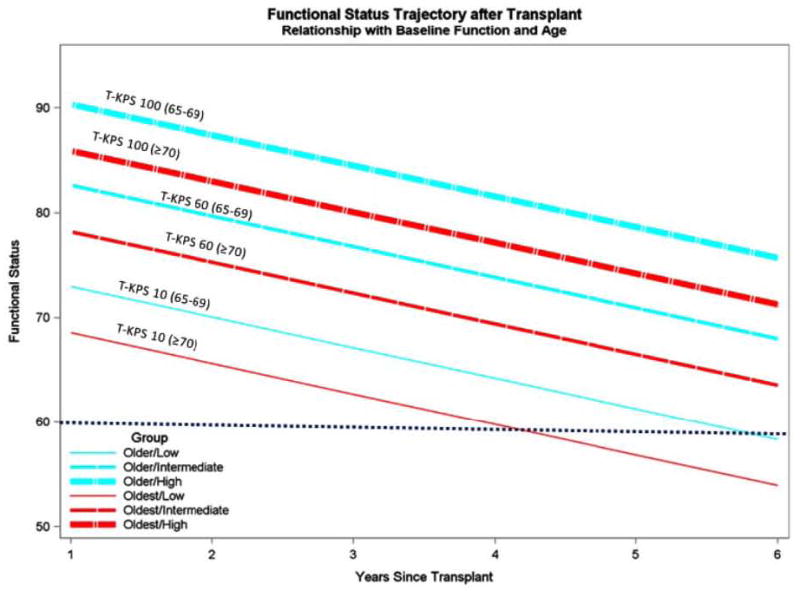
Functional status (y axis) is measured by Karnofsky Performance Score (KPS). The dotted line represents a clinically predictive cut off for higher risk for hospitalization, nursing home placement and death in older adults. The levels of functional status at transplantation are: Low = tKPS 10, intermediate = tKPS 60 and high = tKPS 100. The model used age group as main independent variable and time and tKPS as covariates.
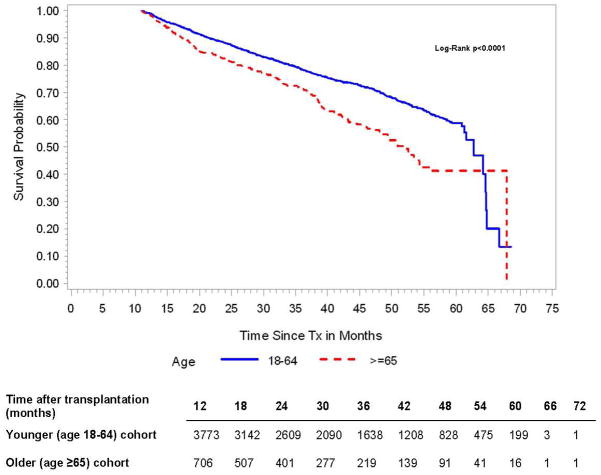
Survival
Our cohort, which includes only recipients surviving to 11-months post-transplantation with complete functional status data thereafter, had 1063 (22.12%) deaths during the follow-up period: 193 (18.2%) in the older group and 870 (81.8%) in the younger group. The median time-to-death conditional on having survived the first year post-transplantation was 52 months in the older group and 63 months in the younger group (log rank p<0.0001). Figure 6 and Table 4 show the predicted survival probabilities. The most common cause of death among older recipients was infection and among younger recipients graft rejection.
Figure 6. Predicted Survival over time for Younger (age 18–64) and Older (age ≥65) Lung Transplantation Recipients conditional on being alive at 11 months.
These are the number of recipients alive at different months after lung transplantation for each age group.
Table 4.
Predicted Survival Probabilities over time by Age Groups
| Time after transplantation (months) | 11 | 12 | 24 | 36 | 48 | 60 |
|---|---|---|---|---|---|---|
|
|
||||||
| Younger (age 18–64) cohort | 1.0 (1.0, 1.0) | 0.99 (0.99, 0.99) | 0.88 (0.87, 0.89) | 0.78 (0.77, 0.80) | 0.70 (0.68, 0.72) | 0.59 (0.56, 0.62) |
| Older (age ≥65) cohort | 1.0 (1.0, 1.0) | 0.99 (0.98, 0.99) | 0.83 (0.79, 0.85) | 0.72 (0.68, 0.76) | 0.56 (0.50, 0.62) | 0.41 (0.33, 0.49) |
These are lung transplantation recipients that survived to 11 months after transplantation and had functional status data thereafter.
Long-term complications in Older vs. Younger Recipients
Approximately 58% of recipients experienced graft rejection at some point during the follow-up period; this rate was lower in the older (50.6%) compared to the younger (59.0%) cohort. Older recipients were also less likely than younger to develop BO (22% vs. 28.3%), end-stage renal disease on hemodyalisis (3.2% vs. 4.6%), or diabetes (38.1% vs. 44.2%). The rate of CVA was similar between age groups (1.0% vs. 1.4%).
DISCUSSION
In this analysis of data from all adults who received Lung Transplantation in the U.S. in the post LAS era (5/1/2009–12/31/2009), more than 90% of older and younger recipients survived the first year post-transplantation, and the average KPS at that point was higher than at transplantation. In the subsequent years, older and younger recipients had a similar rate of decline in physical function of about 3 points per year. Considering that 10 points constitutes a clinically significant difference on this instrument, this rate of decline may not be clinically relevant for several years. On average, a high functional status at transplantation, younger age, a BLT as opposed to SLT, and transplantation at a large-volume center were associated with a modestly higher KPS post-transplantation. Recipients who underwent transplantation at a large-volume center had a statistically yet not clinically significant slower rate of decline in KPS over time. Even older SLT recipients with the lowest functional status at transplantation (tKPS=10) rarely reached the level of disability predictive of worse outcomes (KPS ≤60) within 5 years post-transplantation.
A second major finding of this study was that for recipients aged 70 and higher who survived the first year post-transplantation the rate of functional decline was not significantly different from recipients aged 65–69, though their overall mean functional status was slightly lower. Recipients 70 and older with the lowest functional status at transplantation were likely to reach the cut off for significant disability (KPS ≥60) at 48 months post-transplantation. There is controversy regarding the benefits of LT for these patients because they have a substantially increased short-term mortality risk (30-day HR=2.9 [95% CI, 1.2 to 7.1] p=0.02; 90-day HR= 3.0 [1.5 to 5.9] p<0.001); 1-year HR=2.2 [1.2 to 3.9] p=0.008) when compared to those younger than 70(2), but our data suggest that those who do survive the first year post-transplantation can expect to experience relatively good function for some years after that.
To our knowledge this is the first large-scale report of functional status trajectory after LT in older adults. A report using UNOS data from the pre LAS describes up to 27% of recipients older than 70 reverting to “normal function” at last follow-up (24±2 months). However, these authors did not define the instrument used to measure physical function or its cut off for “normal function” and did not follow repeated measures over time (2). Our study results show that LT had a positive and durable effect in the long-term physical function of adult-recipients including those aged 70 or older, in spite of their shorter survival.
On average, younger recipients lived longer than their older counterparts. The survival probabilities for both older and younger recipients were similar to previous report by the International Society of Heart and Lung Transplantation (ISHLT)(1, 5).
A third major finding was that older recipients differed from younger recipients in their patterns of long-term complications in the years following transplantation. Similar to previous reports (1, 2, 5), older recipients were less likely to experience acute or chronic graft rejection (including BO) and to enroll on hemodialysis (perhaps due to patient preferences or quality of life considerations). For all recipients, the rate of CVA post-operative and long-term was low and the rate of end-stage renal disease on hemodyalisis and diabetes increased at follow-up. These findings are consistent with prior literature (21, 22).
This study provides the first large scale, multi-institutional description of the characteristics of older recipients in the post LAS era. Older recipients had a lower proportion of females and non-White race than the younger. In the pre LAS era women made up a slightly higher proportion of older recipients (38–41.5%), whereas non-white made up a slightly lower proportion (6.5%) (2, 23). Potential reasons for these persistent ethnic and gender disparities include: physician referral bias, cultural preferences, insufficient social and financial support, higher prevalence of co-morbidities and disability and a lower prevalence of end-stage lung diseases in older females and African Americans (24, 25). Older females have a higher prevalence of morbidity and disability then older males which can preclude them from transplantation (26). IPF, which is the number one indication for transplantation in older adults, has a 2:1 predilection for females after age 65. In contrast, the worldwide prevalence of COPD in older females has reached that of older males during the last decade(25). Lastly, poverty is higher in older females from ethnic minorities and can influence the patients’ decision to accept referral for transplantation evaluation. The median annual income for older Americans in 2009 was USD$19,167(27). The estimated cost for a LT ranges from USD$450,400–657,800 added to the cost of long-term immunosuppressive medications (USD$20,500–22,800). Although Medicare covers most of the expenses, for some patients the co-pays and premiums by themselves can be prohibitive (28).
In the post LAS era, IPF surpassed COPD and became the main indication for transplantation in older adults. In the pre LAS the proportion of patients transplanted for COPD was 44% and for IPF was 15% (UNOS 2000)(3). Although, the prevalence of IPF increases after age 65 (29–88/100,000), it remains significantly lower than COPD (9.5% of older U.S population). Several factors serve to increase the proportion of LT performed for IPF. First, in comparison to COPD, IPF has a steeper and more unpredictable decline curve which leads to delayed referral (29) and contributes to a higher LAS(30). Second, there is no curative alternate treatment which further increases the urgency for transplantation. In our study IPF patients had half the wait-list time compared to those with COPD. Despite similar LAS in both age groups, older recipients had half the wait-list time of younger irrespective of diagnosis.
Sixty three percent of the older group received a SLT, while 70% of younger received a BLT. The best choice of procedure in older LT recipients is controversial. According to UNOS data (1994–2000), in older recipients with IPF there was no difference in survival between SLT and BLT up to 3 years post-transplantation. Contrarily in COPD (ISHLT 1999–1997), survival is significantly better for BLT than SLT until age 60, after which BLT has worse survival. More recent analysis (UNOS 1998–2004) showed no difference in survival between procedure types for older recipients irrespective of disease. It has been suggested that SLT is preferred in some older patients because of lower perioperative morbidity and faster recovery in frail patients (23, 31–33). In this study, BLT recipients had higher functional status post-transplantation but similar rate of decline in function when compared to SLT recipients. We caution the interpretation of these differences as they may be confounded by factors we did not control for which inform the decision to perform BLT vs. SLT (i.e. co-morbidities, provider preference, characteristics of the donor lung, etc.)
This study has several limitations which are inherent to secondary analysis of clinical data and may affect the interpretation of results. First, the UNOS data are entered by staff with different training background and some of the variables are non-mandatory to report which may bias data towards better outcomes. For example, our sample excluded 1036 recipients (17% of all adults receiving first LT in the U.S. during the post LAS era) who had missing data and could have experienced worse outcomes. Second, long-term outcomes, particularly morbidities, may be less accurate because of the complexity in diagnosis and reporting (recall bias). Third, the primary outcome is a clinician rated score, which may be subject to inter-observer variability. Lastly, the accuracy of the estimated rate of change in functional status over time and survival probabilities is lower after 48-months post-transplantation because the number of observations per month decreased beyond this point, as illustrated in figures 2–3.
Our study provides a first look into long-term functional outcomes in older lung transplantation recipients. Our principle finding was that older and younger recipients have similar rates of decline in physical function 1–5 years after transplantation. Also, among recipients who survived the first year post-transplantation (90%), even older patients who had very severe functional debility at transplantation will rarely become disabled by 48 months post-transplantation, despite having an overall lower KPS post-transplantation. These findings may assist clinicians when discussing the option of transplantation with older adults, particularly when considering outcomes other than survival. Additionally, these results should inform policy decisions and discourage the use of age alone to preclude a candidate from this life-saving procedure. Further research is needed to determine whether these findings impact the quality of life of these recipients, and the cost effectiveness of transplantation for older adults.
Supplementary Material
Acknowledgments
This work was in part supported by Health Resources and Services Administration contract 234-2005-370011C. The content is responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
List of Non-Standardized Abbreviations
- LT
Lung transplantation
- U.S
United States
- LAS
Lung Allocation Score
- IPF
Idiopathic pulmonary fibrosis
- COPD
Chronic Obstructive Pulmonary Disease
- UNOS, United Network for Organ Sharing
is a private nonprofit membership organization that has operated the Organ Procurement and Transplantation Network under contract with the Health Resources and Services Administration, part of the United States Department of Health and Human Services, since 1986
- CVA
Cerebrovascular Accident
- SLT
Single lung transplantation
- BLT
Bilateral lung transplantation
- KPS
Karnofsky Performance score
- BO
Bronchiolitis obliterans syndrome
- tKPS
Karnofsky Performance score at transplantation
- ISHLT
International Society for Heart and Lung Transplantation
Footnotes
Disclosures:
The authors Heather Whitson, Linda Sanders, and David Zaas have no conflicts of interest to disclose as described by the American Journal of Transplantation.
Liza Genao was supported partially by the National Institute on Aging Grant T32 AG00029 Kenneth E. Schmader has received grants from Merck for zoster vaccine studies.
References
- 1.Health Resources and Services Administration US. Organ Procurement and Transplantation Network. Available from: http://optn.transplant.hrsa.gov/latestData/step2.asp.
- 2.Weiss ES, Merlo CA, Shah AS. Impact of advanced age in lung transplantation: an analysis of United Network for Organ Sharing data. Journal of the American College of Surgeons. 2009 Mar;208(3):400–9. doi: 10.1016/j.jamcollsurg.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 3.Organ Procurement and Transplantation Network O. National Annual Data Reports. Available from: http://optn.transplant.hrsa.gov/latestData/
- 4.The International Society of Heart and Lung Transplantation I. Quarterly Data Report Lung in North America. 2012 Available from: http://www.ishlt.org/registries/quarterlyDataReport/
- 5.Christie JD, Edwards LB, Kucheryavaya AY, Benden C, Dobbels F, Kirk R, et al. The Registry of the International Society for Heart and Lung Transplantation: Twenty-eighth Adult Lung and Heart-Lung Transplant Report—2011. The Journal of Heart and Lung Transplantation. 2011;30(10):1104–22. doi: 10.1016/j.healun.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Mold JW, Looney SW, Viviani NJ, Quiggins PA. Predicting the health-related values and preferences of geriatric patients. The Journal of Family Practice. 1994 [PubMed] [Google Scholar]
- 7.Gibson DM. Interaction and well-being in old age: Is it quantity or quality that counts? The International Journal of Aging and Human Development. 1986;24(1):29–40. doi: 10.2190/ndu9-2175-hgd4-j9wl. [DOI] [PubMed] [Google Scholar]
- 8.Ann Bowling ZG, Banister David, Sutton Stephen. Go Findings 2002. Published by ESRC Growing Older Programme; Apr, 2002. Adding Quality to Quantity: older people’s views on their quality of life and its enhancement. [Google Scholar]
- 9.Kniepeiss D, Wagner D, Pienaar S, Thaler HW, Porubsky C, Tscheliessnigg KH, et al. Solid organ transplantation: Technical progress meets human dignity a review of the literature considering elderly patients’ health related quality of life following transplantation. Ageing research reviews. 2011 Jul 1; doi: 10.1016/j.arr.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Castriotta RJ, Eldadah BA, Foster WM, Halter JB, Hazzard WR, Kiley JP, et al. Workshop on Idiopathic Pulmonary Fibrosis in Older Adults. Chest. 2010;138(3):693–703. doi: 10.1378/chest.09-3006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kizer JR, Zisman DA, Blumenthal NP, Kotloff RM, Kimmel SE, Strieter RM, et al. Association between pulmonary fibrosis and coronary artery disease. Archives of internal medicine. 2004 Mar 8;164(5):551–6. doi: 10.1001/archinte.164.5.551. [DOI] [PubMed] [Google Scholar]
- 12.Jiayun X, Adeboyejo O, Wagley E, Aubrecht J, Mi-Kyung S, Thiry L, et al. Daily burdens of recipients and family caregivers after lung transplant. Progress in Transplantation. 2012;22(1):41–8. doi: 10.7182/pit2012815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henri C, Giraldeau G, Dorais M, Cloutier AS, Girard F, Noiseux N, et al. Atrial fibrillation after pulmonary transplantation: incidence, impact on mortality, treatment effectiveness, and risk factors. Circulation: Arrhythmia & Electrophysiology. 2012;5(1):61–7. doi: 10.1161/CIRCEP.111.964569. [DOI] [PubMed] [Google Scholar]
- 14.Langer D, Burtin C, Schepers L, Ivanova A, Verleden G, Decramer M, et al. Exercise training after lung transplantation improves participation in daily activity: a randomized controlled trial. American journal of transplantation: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2012 Jun;12(6):1584–92. doi: 10.1111/j.1600-6143.2012.04000.x. [DOI] [PubMed] [Google Scholar]
- 15.Langer D, Gosselink R, Pitta F, Burtin C, Verleden G, Dupont L, et al. Physical activity in daily life 1 year after lung transplantation. The Journal of heart and lung transplantation: the official publication of the International Society for Heart Transplantation. 2009 Jun;28(6):572–8. doi: 10.1016/j.healun.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Maury G, Langer D, Verleden G, Dupont L, Gosselink R, Decramer M, et al. Skeletal Muscle Force and Functional Exercise Tolerance Before and After Lung Transplantation: A Cohort Study. American Journal of Transplantation. 2008;8(6):1275–81. doi: 10.1111/j.1600-6143.2008.02209.x. [DOI] [PubMed] [Google Scholar]
- 17.Sager JS, Kotloff RM, Ahya VN, Hadjiliadis D, Simcox R, Blumenthal NP, et al. Association of Clinical Risk Factors with Functional Status Following Lung Transplantation. American Journal of Transplantation. 2006;6(9):2191–201. doi: 10.1111/j.1600-6143.2006.01437.x. [DOI] [PubMed] [Google Scholar]
- 18.Reinsma GD, ten Hacken NHT, Grevink RG, van der Bij W, Koëter GH, van Weert E. Limiting Factors of Exercise Performance 1 Year After Lung Transplantation. The Journal of Heart and Lung Transplantation. 2006;25(11):1310–6. doi: 10.1016/j.healun.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Weiss ES, Allen JG, Meguid RA, Patel ND, Merlo CA, Orens JB, et al. The impact of center volume on survival in lung transplantation: an analysis of more than 10,000 cases. The Annals of thoracic surgery. 2009 Oct;88(4):1062–70. doi: 10.1016/j.athoracsur.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 20.Crooks V, Waller S, Smith T, Hahn TJ. The use of the Karnofsky Performance Scale in determining outcomes and risk in geriatric outpatients. J Gerontol. 1991 Jul;46(4):M139–44. doi: 10.1093/geronj/46.4.m139. [DOI] [PubMed] [Google Scholar]
- 21.Mateen FJ, Dierkhising RA, Rabinstein AA, van de Beek D, Wijdicks EF. Neurological complications following adult lung transplantation. American journal of transplantation: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2010 Apr;10(4):908–14. doi: 10.1111/j.1600-6143.2009.02998.x. [DOI] [PubMed] [Google Scholar]
- 22.Christie JD, Edwards LB, Kucheryavaya AY, Aurora P, Dobbels F, Kirk R, et al. The Registry of the International Society for Heart and Lung Transplantation: Twenty-seventh official adult lung and heart-lung transplant report—2010. The Journal of Heart and Lung Transplantation. 2010;29(10):1104–18. doi: 10.1016/j.healun.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 23.Nwakanma LU, Simpkins CE, Williams JA, Chang DC, Borja MC, Conte JV, et al. Impact of bilateral versus single lung transplantation on survival in recipients 60 years of age and older: analysis of United Network for Organ Sharing database. The Journal of thoracic and cardiovascular surgery. 2007 Feb;133(2):541–7. doi: 10.1016/j.jtcvs.2006.09.062. [DOI] [PubMed] [Google Scholar]
- 24.Raghu G. Incidence and Prevalence of Idiopathic Pulmonary Fibrosis. American journal of respiratory and critical care medicine. 2006;174(7):810–6. doi: 10.1164/rccm.200602-163OC. [DOI] [PubMed] [Google Scholar]
- 25.Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, et al. International variation in the prevalence of COPD (The BOLD Study): a population-based prevalence study. The Lancet. 2007;370(9589):741–50. doi: 10.1016/S0140-6736(07)61377-4. [DOI] [PubMed] [Google Scholar]
- 26.von Strauss E, Aguero-Torres H, Kareholt I, Winblad B, Fratiglioni L. Women are more disabled in basic activities of daily living than men only in very advanced ages: a study on disability, morbidity, and mortality from the Kungsholmen Project. Journal of clinical epidemiology. 2003 Jul;56(7):669–77. doi: 10.1016/s0895-4356(03)00089-1. [DOI] [PubMed] [Google Scholar]
- 27.Department of Human and Heath Services US. A profile of Older Americans. 2010 Available from: http://www.aoa.gov/aoaroot/aging_statistics/Profile/2010/docs/2010profile.pdf.
- 28.Milliman iRH. Milliman Research Report for UNOS/OPTN. 2008. 2008 U.S. organ and tissue transplant cost estimates and discussion. [Google Scholar]
- 29.Martinez FJ, Safrin S, Weycker D, Starko KM, Bradford WZ, King TE, Jr, et al. The clinical course of patients with idiopathic pulmonary fibrosis. Annals of internal medicine. 2005 Jun 21;142(12 Pt 1):963–7. doi: 10.7326/0003-4819-142-12_part_1-200506210-00005. [DOI] [PubMed] [Google Scholar]
- 30.Liu V, Zamora MR, Dhillon GS, Weill D. Increasing lung allocation scorespredict worsened survival among lung transplant recipients. American journal of transplantation: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2010 Apr;10(4):915–20. doi: 10.1111/j.1600-6143.2009.03003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Minambres E, Llorca J, Suberviola B, Naranjo S, Zurbano F, Gonzalez-Castro A. Early outcome after single vs bilateral lung transplantation in older recipients. Transplant Proc. 2008 Nov;40(9):3088–9. doi: 10.1016/j.transproceed.2008.08.119. [DOI] [PubMed] [Google Scholar]
- 32.Meyer DM, Edwards LB, Torres F, Jessen ME, Novick RJ. Impact of recipientage and procedure type on survival after lung transplantation for pulmonary fibrosis. The Annals of thoracic surgery. 2005 Mar;79(3):950–7. doi: 10.1016/j.athoracsur.2004.08.076. discussion 7–8. [DOI] [PubMed] [Google Scholar]
- 33.Meyer DM, Bennett LE, Novick RJ, Hosenpud JD. Single vs bilateral, sequential lung transplantation for end-stage emphysema: influence of recipient age on survival and secondary endpoints. The Journal of heart and lung transplantation: the official publication of the International Society for Heart Transplantation. 2001 Sep;20(9):935–41. doi: 10.1016/s1053-2498(01)00295-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.