Abstract
Poor breastfeeding outcomes among late preterm infants (LPIs) have been attributed to inadequate breast milk transfer stemming from physiological immaturities. However, breastfeeding is more than a biological phenomenon, and it is unclear how mothers of LPIs manage other factors that may also impact the breastfeeding course. Using grounded theory methods and incorporating serial post‐partum interviews with several novel data collection techniques, we examined breastfeeding establishment over a 6–8‐week‐period among 10 late preterm mother‐infant dyads recruited from a maternity hospital in Pittsburgh, Pennsylvania, USA. We found that breastfeeding in the LPI population was a fluctuating, cascade‐like progression of trial and error, influenced by a host of contextual factors and events and culminating with breastfeeding continuation (with or without future caveats for duration or exclusivity of breastfeeding) or cessation. The trajectory was explained by the basic psychosocial process Weighing Worth against Uncertain Work, which encompassed the tension among breastfeeding motivation, the intensity of breastfeeding work and the ambiguity surrounding infant behaviour and feeding cues. Several sub‐processes were also identified: Playing the Game, Letting Him be the Judge vs. Accommodating Both of Us and Questioning Worth vs. Holding out Hope. If valid, our theoretical model indicates a need for earlier, more extensive and more qualified breastfeeding support for mothers of LPIs that emphasizes the connection between prematurity and observed feeding behaviours.
Keywords: late preterm, premature infant, breastfeeding, lactation, theoretical models, qualitative research
Introduction
The research documenting the nutritional, immunological and developmental advantages of breastfeeding, particularly among infants born prematurely, is significant and compelling (Callen & Pinelli 2005; Ip et al. 2007). It is concerning, then, that infants born in the late preterm period (34 0/7–36 6/7 weeks gestation) experience suboptimal breastfeeding rates and a high incidence of breastfeeding‐associated morbidity, presumably related to insufficient breast milk intake (Radtke 2011). Considering that late preterm infants (LPIs) comprise ∼70% of preterm births in the USA, their breastfeeding issues should also constitute a public health concern (Martin et al. 2010).
Unrecognised or poorly managed physiological immaturities, which often belie a ‘term’ appearance, have been implicated in LPI breastfeeding difficulties. These immaturities are often manifested in poor regulation of sleep–wake states, uncoordinated sucking and latching, and decreased oro‐motor tone, all of which contribute to non‐sustained at‐breast feeds and insufficient breast milk transfer (Meier et al. 2007; Wight et al. 2008). Current evidence‐based late preterm guidelines, based mostly on clinical experience and expert opinion, address breastfeeding mainly from a physiological standpoint (Association of Women's Health, Obstetric, and Neonatal Nurses 2010; The Academy of Breastfeeding Medicine 2011). Yet breastfeeding remains an extremely complex psychosocial, as well as a biological process, mutually influenced by mother and infant. In order to design interventions with practical relevance and improve LPI breastfeeding outcomes, exploration of maternal perspectives, contexts and individual idiosyncrasies influencing the LPI breastfeeding course is necessary.
Key messages
Breastfeeding establishment among late preterm mother–infant dyads was a complex, tenuous process in flux, complicated by the existence of preterm obstacles within a “term”‐oriented environment.
The core process, Weighing Worth against Uncertain Work, entailed how participants managed the tension between the ascribed value and effort of breastfeeding an LPI, while reliable signs of milk transfer and infant satiety remained elusive.
Our theoretical model indicates that health care providers and mothers of LPIs should be educated on the relationship between physiological prematurity and the potential for breastfeeding issues, basic breastfeeding interventions and availability of qualified breastfeeding support resources.
Materials and methods
Design
The purpose of this study was to describe the process of breastfeeding establishment among late preterm mother–infant dyads. Our philosophical orientation and methodological processes were informed by constructivist grounded theory, which posits theory development as a context‐dependent co‐creation of reality between participants and researcher (Charmaz 2004).
Setting and sample
After Institutional Review Board approval, participant recruitment occurred in the maternity wards and NICU in a tertiary care maternity hospital in Pittsburgh, Pennsylvania, USA over a one‐year period from 2011 to 2012. The hospital typically delivers over 10 000 infants per year, accounting for 45% of the births in the county. During the data collection period, the hospital was actively working on attaining Baby‐Friendly status, a prestigious designation indicating a hospital's commitment to supporting breastfeeding mothers (Baby‐Friendly USA 2010). The hospital's 2011 rate of breastfeeding initiation was 72%, below the national rate of 74.6% during the same year (Centers for Disease Control and Prevention 2011).
Post‐partum women were eligible for study participation if they were English‐speaking, at least 18 years, had delivered an infant between 34 0/7 and 36 6/7 weeks of gestation, intended to breastfeed or provide breast milk to their infant(s) and had no conditions anticipated to preclude or significantly complicate breastfeeding (e.g. HIV‐positive status, major congenital anomalies). Medical records of patients admitted to the maternity ward were screened for eligibility, and potential participants were approached for enrollment by the first author, who also worked as a staff nurse on the maternity unit but did not care for any study patients. Two patients out of 12 approached declined study participation (83% approach‐to‐consent ratio). For patients interested in the study, the informed consent process consisted of a conversation and verbalised understanding by each participant regarding the study's purpose (‘to learn more about breastfeeding and the relationship between mothers and their infants who were born slightly premature’) procedures, risks and benefits. Initially, mothers were purposefully selected for variability in age, parity, race and infant gestational age. As the study progressed, the developing theory dictated more specific recruitment based on variability in infant neonatal intensive care unit (NICU) admission, prior breastfeeding experience and early breastfeeding management.
The final study sample included 10 maternal participants and their 12 infants. Retention of enrolled participants to study completion was 100%. Six infants were born between 36 and 37 weeks gestation, three between 35 and 36 weeks and one <35 weeks. Birth weights ranged from 2210 to 3440 g, and four infants were <2500 g. There were eight male and four female infants and two sets of twins. Two infants were admitted to the NICU (not twins) during the birth hospitalization. All infants experienced one or more complications of prematurity, including hyperbilirubinaemia, hypoglycaemia, respiratory distress or infection, bradycardia and/or reflux. Three infants, including a set of twins, were re‐hospitalised with viral respiratory illnesses several weeks post‐birth.
Mothers ranged in age from 21 to 41, with a mean age of 31. There were two non‐Hispanic black women; the remaining participants were Caucasian. Seven were married, and seven were college‐educated. Two were WIC recipients. Five mothers were primiparas. Participants with other children had at least three months breastfeeding experience, and three mothers had previously breastfed a preterm infant. Four mothers had a caesarean birth, and several had pregnancy‐ or other health‐related complications, including gestational diabetes, type II diabetes and hypertension.
Data collection
Serial, semi‐structured interviews were the main source of study data. An interview guide, consisting of open‐ended questions and probes about the breastfeeding experience (e.g. management, decision processes, ascribed value, progression of issues), was created through study team discussions of the relevant breastfeeding literature and piloted with a breastfeeding mother not part of the study sample. The guide was continually revised as data collection progressed and new categories were identified. It was utilised to begin or re‐focus interviews, though priority was given to topics broached by participants. Table 1 lists examples of questions included in the guide. Interviews were conducted by the first author and occurred during the post‐partum hospitalization (1–2 days post‐birth) and at participants' homes at 1 week, 2 weeks and 6–8 weeks post‐partum. A follow‐up 1‐week interview was conducted in the NICU for a mother whose infant remained hospitalised for 13 days. Thirty‐nine total interviews were conducted and ranged from 10–65 min in length, with a mean duration of 35 min.
Table 1.
A sampling of items included in the interview guide
| Initial interview |
| Tell me about how you came to the decision to breastfeed or to provide breast milk for your new baby. |
| Tell me about the first few times you tried breastfeeding or pumping. |
| How has breastfeeding so far been different from, or similar to: (1) your expectations? (2) any prior breastfeeding experiences? |
| Describe how breastfeeding has progressed since the first feed. |
| What has breastfeeding assistance in the hospital been like? |
| How does your experience with breastfeeding so far compare with your picture of motherhood or being a mom? |
| Subsequent interviews |
| What do you think are the reason(s) that you have continued to breastfeed? |
| How does breastfeeding in the hospital compare with breastfeeding at home? |
| How have you balanced other obligations and activities with breastfeeding? |
| Describe a typical day breastfeeding. |
| Have you sought assistance or advice regarding breastfeeding? If so, how has this impacted breastfeeding? |
| What do you expect in terms of any changes in the future that will impact your ability to breastfeed? |
| Describe how breastfeeding fits into your idea of mothering or caring for your baby at this point. |
Participants were invited to participate in several additional, exploratory forms of data collection as a means to achieve methodological triangulation. These optional methods included breastfeeding e‐mail or audio ‘diaries’ and video recording with stimulated‐recall interviewing. The latter method, designed to elicit participant self‐review and reflection (Busse & Ferri 2003), encompassed participants' audio‐recorded reactions and responses to interview questions as their video‐recorded breastfeeding footage from the preceding interview was viewed. While no participants attempted audio diaries, five completed one or more e‐mail diaries (21 total entries), and two took part in video reviews (3 total video reviews). These supplemental data sources were analysed similar to interview data and served to enrich, confirm and clarify participants' thoughts and emergent themes. Data collection ceased with participant #10 when redundancy in categories and concepts was confirmed, and newly gathered data did not add significantly to the developing theoretical framework.
Data analysis
Data analysis, led by the first author, proceeded concurrently with data collection. All data were professionally transcribed and reviewed for accuracy. Transcripts were first ‘open coded’, which consisted of a detailed segment‐by‐segment analysis of salient processes and concepts and assignment of a label as close to participants' actual words as possible. Initial coding progressed to focused coding, which synthesised similar, frequently used initial codes. Naturally and simultaneously, we organised codes into more abstract categories by considering the fit of concepts into the developing theoretical framework. Certain categories held particular explanatory power and connectedness to other categories and were interwoven, along with theoretical memos, into a framework that included participants' thoughts and words, as well as the authors' interpretations. As a final step, the theoretical framework was refined and differentiated from extant theories and concepts in the literature. The process was an abductive endeavour, relying heavily on the technique of constant comparison (Charmaz 2000, 2006; Morse et al. 2009). To ensure analytic rigor and protect against bias, the first author recorded detailed field notes and kept a reflexive journal. In addition, we utilised multiple qualitative analysis techniques (e.g. matrix development, diagramming, interview summaries) during model development, and analysis decisions were discussed and validated in weekly meetings with senior authors (SMC and MBH) and a qualitative analysis workgroup.
Findings
Breastfeeding establishment among late preterm mother–infant dyads was a complex, tenuous process in flux. It was characterised by a bifurcated, cascade‐like progression of infant physiological issues and maternal reactions, initial and continued management strategies, secondary issues dependent upon management and, finally, breastfeeding cessation or continuation. For some participants, continued breastfeeding came with caveats impacting the exclusivity or long‐term duration of nursing (e.g. return to work). All participants followed one of three general paths (see Fig. 1) determined by the facilitative or detrimental nature of initial and continued breastfeeding management strategies. Women who could not, or did not, compensate for poor early breastfeeding management were those who ceased breastfeeding during or shortly after study participation. A constellation of contextual factors and events were pivotal to the entire trajectory and major determinants in management decisions.
Figure 1.
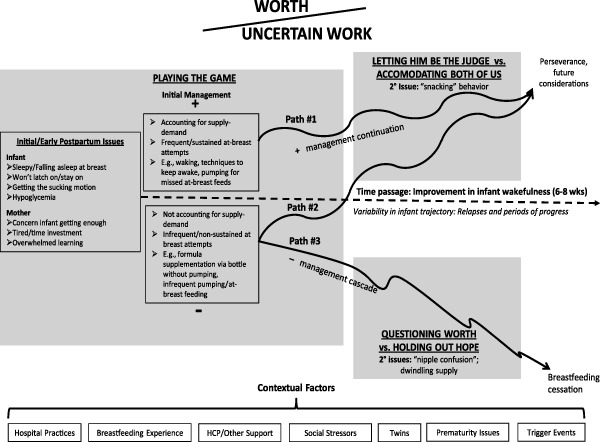
Theoretical model of late preterm breastfeeding establishment.
Late preterm breastfeeding establishment was not simple or straightforward. Participants who ultimately stopped breastfeeding (n = 3) experienced an emotional ‘rollercoaster’, involving brief periods of hope, in which their milk supply or at‐breast feeds seemed to improve, amidst a downward spiral of ineffective breastfeeding, formula supplementation, decreasing milk supply, more formula supplementation and insufficient time and energy to incorporate breastfeeding activities into daily life. Likewise, mothers who eventually achieved success in breastfeeding also experienced multiple setbacks in their breastfeeding journey, including periods when their infants were supplemented with formula against their desires and ‘getting’ breastfeeding took longer than expected.
A core social–psychological process was identified from the data: Weighing Worth against Uncertain Work. This explanatory process entailed how participants managed the tension between the value they placed on breastfeeding and the perceived mental and physical stamina necessary for breastfeeding success, while definitive or consistent signs of milk availability and transfer, as well as infant feeding and satiety cues remained elusive. Three sub‐processes in the trajectory, entailing how mothers thought about and dealt with breastfeeding over time, were also delineated: (1) ‘Playing the game’; (2) ‘Letting him be the judge vs. accommodating both of us’; and (3) ‘Questioning worth vs. holding out hope.’
Worth
‘Worth’ encompassed a mother's motivation to breastfeed or provide breast milk to her infant. For almost all participants, this was a relatively enduring concept, influenced by cumulative life experiences and therefore often established prior to the birth. Although most participants cited awareness of a wide range of breastfeeding benefits, two distinct groups of women emerged. The large majority of participants were those who identified breastfeeding as central to their role as a mother. For these women, breastfeeding ‘wasn't even a question’. It was seen as a ‘responsibility’ to one's children and ‘what being a mom is all about’. These mothers cited infant immunologic, cognitive and developmental benefits, as well as bonding, or connection to their babies, as primary reasons they chose and continued to breastfeed.
A second group of women was motivated to breastfeed by convenience, guilt and/or maternal benefits. In general, mothers of the second type exhibited a laid‐back attitude toward breastfeeding success and goals.
For me, I think it's just because I did with the other two. It's not like I ever planned on, with any of them, it was just … I did with my first, and so once you do it with one, I think you feel you should with all of them.
Uncertain work
Uncertain work was conceptualised as the non‐reciprocal effort put forth by the mother to achieve breastfeeding success, while her infant was ‘not willing to work’, ‘not trying’, ‘lazy’, ‘not interested’ or wouldn't ‘contribute’. Work was time and energy‐intensive, often consisting of multiple strategies to encourage the infant to nurse at breast, for example using nipple shields or dripping formula onto the breast, followed by formula supplementation and/or breast pumping.
It feels like I'm non‐stop moving. And, a lot of the time it is with feeding him. It's like, it'll take about an hour just between getting everything [e.g., breast pump, formula supplement] ready and [breast]feeding him on top of it.
[Pumping is] the last thing on my mind after trying to get him to eat for an hour. I don't want to spend like another 15 minutes having to pump.
The work was characterised as uncertain, as infant behaviour, particularly related to decreased responsiveness, made determination of milk transfer and identification of satiety and feeding cues difficult.
Keeping her interested in the breastfeeding and making sure she is getting enough milk [is a challenge], because she falls asleep sometimes halfway through feedings and I have to keep waking her up … my main concern is that she needs to get enough.
It is definitely easier with the formula just because [the twins] have been eating about two ounces or so with the formula … [with breastfeeding], I mean I still kind of question: like, are you really done? Was that really enough? Did you really get enough? Maybe … And if I'm really not sure sometimes I will still get a bottle out and do some formula just to make sure that their bellies are full.
Mothers also worried about whether their infant's behaviour was a sign of a more serious problem.
I guess I just wasn't prepared for [infant's sleepiness], and everyone's like, ‘Oh, be thankful,’ and I'm like, I'm only thankful if it's normal and it's OK. If that's dangerous for him to be sleeping … [or] if it's a sign of like – I don't know why I was thinking ‘brain'‐is his brain not developed? Like why in the world is he just sleeping so much?
Weighing worth against uncertain work
Over time, participants' ideals in caring for their infants (worth) were tempered by the reality of day‐to‐day breastfeeding under less than ideal circumstances (work). This balance was in almost constant fluctuation, as circumstances changed, infants matured and management strategies evolved. In general, when difficulties continued without abatement, the worth of breastfeeding was called into question. Participants with prior breastfeeding experience, however, were able to justify the initial uncertainty, time investment and lack of enjoyment derived from early nursing as temporary.
It's like a process, with everything that I have to do to nurse. I kinda see it as, ‘This is what it takes to do what I need to do,’ … It's only probably going to be temporary, so let's work through this so that we can accomplish our goal, which is getting him to latch on and not having to take so many bottles … I don't think that this is gonna be a permanent situation. He can only get better with time, so I'm just patiently waiting for him to make the adjustment. He's getting there … I mean I think it's definitely rewarding to breastfeed. It's a lot of hard work, but I just see it as … in a few short months everything is going to be changed, so, I try not to let what's going on right now affect me.
Women who were highly motivated to breastfeed and considered breastfeeding integral to their maternal identity were willing to go to great lengths to make breastfeeding successful. For example, despite stalled or slow progress with infants latching or staying on breast, some participants diligently continued at‐breast attempts each feeding, followed by formula bottles and pumping to increase or maintain milk supply. However, negative management strategies, often implemented by primiparas early to save time or energy (e.g. pumping less frequently), were corrected late, and these mothers experienced disappointment and frustration as milk supply dropped and their infants continued to have difficulty nursing.
And then when I was still pumping for 40 minutes and got half an ounce, or not even enough to cover the bottom of the bottle, I was just hopeless. It was hard for me to stop, because I was thinking, ‘I've ruined everything.’ But it was so little milk, it was frustrating. … So I did stop at about the end of August.
Alternatively, mothers who were motivated to breastfeed by convenience or guilt were willing to put in breastfeeding ‘work’ initially but were more amenable to modifying breastfeeding goals as secondary issues or contextual factors became more evident and problematic.
I mean, I'm going to [breastfeed] as long as I can, but there have been some changes just as far as family things that are going on, and my life's going to get much more complicated in the next few days … [my nieces] will be [living with me], and [they] will be able to help me more if the babies are bottle‐fed … the more time that I'll need for [my nieces], but less time with the feedings …
Playing the game
Playing the game comprised the guesswork that went into managing early breastfeeding. At this stage, which generally lasted until 39–40 weeks corrected gestational age, all mothers perceived their infants to have one or more issues that complicated sustained at‐breast feeds, including decreased wakefulness, difficulty latching/staying on breast, inability to coordinate sucking, or hypoglycaemia that required formula supplementation. These issues led to concern over whether infants were ‘getting enough’ breast milk, especially as some participants experienced delayed lactogenesis II (i.e. onset of copious milk production 2–3 days post‐birth). At the same time, primiparas and mothers of twins felt overwhelmed with the time demands and ‘learning’ associated with breastfeeding. Participants exuded anxiety, fear and frustration as they struggled to make sense of their infant's behaviour and establish successful breastfeeding.
At first, it was one of the most frustrating things … I'm like, ‘I don't know why they told us we had to feed you when you're not eating. What's going on?’
I mean, it was borderline scary for me because I'm like, ‘Hello, are you alive!? Like, I have cold rags on you, I have no clothes on you, and you are not responding to me!’ … Those first two weeks were probably the most challenging. And I think having a newborn, those are your challenging weeks anyhow, but that was, like, a different challenge for me because it was, like, just everything from scary to frustrating to, ‘How do I do this?’ Like, you know, he needs to eat. I know he needs to gain weight, but he's not waking up, you know? … It was new to me.
Breastfeeding was described as a ‘trial‐and‐error’ process or ‘game’; and infants’ behaviours related to physiologic immaturity (e.g. overstimulation and shut down behaviour after difficulty at breast) were often misinterpreted as intentional acts, personality traits or simply part of the ‘individual’ breastfeeding experience. At the extreme, some mothers did not acknowledge the infant's prematurity status at all, citing the infant's ‘term’ weight or negligible proximity to 37 weeks. Infants were described as ‘faking it’ and ‘tricking’ their mothers, as they acted hungry or ‘interested,’ but fell asleep or ‘refused’ to stay on breast.
He'll fake like he's asleep. He'll get so mad that he just lays there and acts like he's asleep, and then after a few minutes, he's like, ‘Okay, I know that she's gonna give me the bottle any minute now,’ and then he'll wake up and he'll just start crying all over again because he's hungry. He's so smart that it's just like, ‘Wow, I can't believe this is happening.’ It's weird.
I mean, it's still day‐by‐day with the whole bottle, like, after I breastfeed for the 20 minutes. I don't know what's gonna make me feel more comfortable knowing how much he's getting from me. I don't know. I guess it's just a game that you're gonna have to play, a time game. Maybe have to start breastfeeding longer to see if he'll get more that way, drink less bottle … all trial and error.
He always latches on very well. He just doesn't stay awake … he just kind of hangs out [on the breast]. We call it the baby bar, and it's like happy hour. He's just kind of hanging on and not really doing much of anything.
For some, the expected bonding or connection to their infant through breastfeeding in this period was delayed as a result of decreased infant responsiveness and interaction during nursing.
[The connection between breastfeeding and bonding] is different since he's not in that sleepy mode. Before I don't even know if I saw it more as, like, nurturing. I'm just like, ‘This is just what I'm to do. He just needs to be held.’ He was supposed to still be inside of me, so of course I loved holding him then, but now I feel like it's more of like a bonding … In the beginning, you're like, ‘I'm just trying to nurse this thing to life.’ I feel like it's dead, and I am trying to nurse it to life.
I know a lot of women enjoy breastfeeding because it bonds them and things like that. I can't say that I am doing it for that reason or not, because it really hasn't been a bonding experience. Because he's really not … he's sleeping.
These early issues were dealt with in a manner detrimental or protective to breastfeeding success, marked by accounting for the supply–demand principle of breast milk production (e.g. milk expression at regular intervals) and continued determination and attempts of at‐breast feeds. Techniques to keep the infant awake at breast (e.g. undressing, touching infant's chin, feet) were employed with mixed results. Some mothers began to wake the infant ahead of time to fit in more frequent feedings; while some started feeding diaries, used breast compressions to increase milk transfer during feedings or used nipple shields to attain a sustained latch. In the absence of definitive signs of satiety, infant weight gain was the ultimate barometer against which these at‐breast efforts were measured (which, dependent upon outcome, provided relief or further angst). Some mothers remained uncomfortable or impatient with at‐breast feeds and gravitated towards strategies that minimised time and energy demands, while permitting visual confirmation of the volume of milk ingested (e.g. bottle‐feeding with formula, expressed breast milk or a combination of the two).
[Bottle‐feeding is] a lot faster and easier … it's better for him, too. I mean, I don't know. Probably a breast would be better – a little bit more connection or something, but this way it's faster and [he] still gets breast milk at least, yeah … So I'm really happy. At least he gets what he needs instead of formula.
[I give him bottles rather than breastfeed] just so that it could be as fast and efficient as possible so that I can get a solid few hours of sleep [before going into work] … whenever I attempt to breast feed him and then bottle feed him and then change his diaper it's a good 45‐minute process. So in the middle of the night, if it's three o'clock in the morning, and I can narrow that down to like 15 minutes between a bottle‐feeding and a diaper change, that would be a lot better … it's just easier for everybody I think, unless he's doing well on the breast. If he's doing well and can eat in 15 minutes then that's ideal but if he keeps up with this napping on the breast it's tough.
Primiparas without prior breastfeeding experience and knowledge sometimes employed ‘shortcuts’. This preserved the goal to breastfeed only temporarily, as breast milk supply eventually dropped.
So [pumping] a couple times a day, it's perfect, you know? Even if he's not eating from [the] nipple, just [breast milk] from the bottle, I'm happy with that. Better than nothing at all … Because I have [enough breast milk] for like three bottles, so I can pump like every six hours.
Questioning worth vs. holding out hope
When poor breastfeeding management continued, participants experienced secondary issues including ‘nipple confusion’ (latch difficulties, presumably due to the infant ‘getting used to’ bottle nipples or flow) and difficulty maintaining their milk supplies. Typically at this point – when the success of breastfeeding was threatened – help was sought in earnest and mothers who were highly motivated to breastfeed were willing to go to extremes to preserve the breastfeeding relationship. They sought help from multiple sources (including paediatricians, friends and lactation consultants), accessed the Internet to find causes of and solutions to their breastfeeding difficulties and devoted additional time to breastfeeding. However, the effort was often too late. While participants had brief periods of hope with improved latching or small increases in milk supply, the trajectory followed a downward trend. Mothers became weary seeing little improvement in milk output and had increasing difficulty justifying the work of breastfeeding. Remarkably, two participants continued to vacillate between stopping breastfeeding and hope for eventual success until their milk supplies were nearly gone.
It doesn't help encourage me to continue to pump as frequently, because I'm not getting enough to make it‐not that it doesn't make a difference, ‘cause I know it does. I know any [breast milk] is good, but … yeah, sometimes it's not even half an ounce. Last night [I pumped] half an ounce from one side, and maybe a quarter of an ounce from the other side. And it's just, ‘Okay, well I'll give them what I can,’ but … it's just … not really picking up … Everybody keeps telling me a lot of that is just ‘cause they're not directly nursing, and that would help with production, but I can't get them to directly nurse. I mean, I still really want it to work, but I think just ‘cause I know it's what's best for them. I really want them to‐even if they're not doing it maybe the most efficient way [at breast], but it means that they're at least getting something … So I'm really hoping that now that it's past six weeks that … I haven't completely failed with it. That there still is some kind of hope to make it work.
Like, yesterday was a half ounce when I was pumping altogether. It's just frustrating. I don't even know if was worth it to do it … But I have to [continue], because I want to give him that. You know, it's still good … What I get, I give it to him because it's still there … even if it's a little bit. Still good for his body or something …
One participant, who initially identified breastfeeding as central to her identity as a mother, ceased breastfeeding at 2 1/2 weeks. Her statements and general demeanor signified defeat and denial of the original worth she attached to breastfeeding.
Pumping became too much of a hassle. I mean he wasn't latching on, and I didn't think he would … It sucks that he didn't really latch on and I didn't really produce much, but … like I said before, with the whole bonding thing … it seems the same to me whether it's breastfeeding or bottle‐feeding because he's still, you know, in your arms and … he's still close to you and everything like that. I don't see the difference. And that was one of the main reasons why I wanted [to breastfeed].
Letting him be the judge vs. accommodating both of us
As initial infant wakefulness issues resolved, mothers with positive continued breastfeeding management wrestled with the dialectic relationship between their needs and the breastfeeding demands of the infant. At this stage, infants were feeding often, but inefficiently, at the same time other life responsibilities began to consume more time and attention. Mothers described infants as ‘constantly’ breastfeeding or ‘hanging out’ on the breast for extended periods doing ‘mini‐feeds’. Although they desired more predictable feeding schedules and considered imposing feeding ‘limits’ on their babies, the threat of ‘going back to square one’ with breastfeeding difficulties loomed large. Ultimately, those who perceived breastfeeding as central to their maternal identity and had once experienced a major threat to breastfeeding success resolved to let their infants' control the nursing relationship for the foreseeable future.
But again I'm probably lax on [a feeding schedule] right now just because it's like, ‘Okay, you want to eat? I'll still continue to put weight on you right now,’ but eventually, hopefully, gradually getting out of that.
I think, right now, with her size, I'm going to let her eat when she wants to, but probably within the next week or so I'm gonna try to put her on a schedule … so I've been trying to let her be the judge of it, and once she gets used to eating … and she already has started to … I think I will definitely put her on a schedule, cause I'm gonna have to [think about] the other children's’ schedules.
I had to do so much to get her to want to breastfeed. And now she's doing so great at it, but now she's like eating too much, and the schedule part [is] the most challenging. To get her on a routine. So it could accommodate both of us.
Typically by the last interview at 6–8 weeks, these mothers reported improved infant efficiency in breastfeeding but continued to experience conflict between other responsibilities and the time demands inherent in breastfeeding; this was particularly troublesome during ‘the overnight’, when infants were perceived to be more alert and active. For some, especially among mothers in whom breastfeeding was not part of their maternal identity, these issues led to the consideration of formula supplementation and limitations on long‐term breastfeeding.
Contextual factors
A plethora of external events, individual circumstances and views shaped by personal experience became major influences on the late preterm breastfeeding process. These contextual factors impacted how mothers thought about breastfeeding, managed issues and ultimately, whether breastfeeding continued. Factors included: (1) hospital practices (e.g. time of delivery and availability of staff to assist in breastfeeding, hypoglycaemia and supplementation protocols, unit cultural differences); (2) prior breastfeeding experience; (3) breastfeeding support from health care providers (HCPs) and others; (4) social stressors (e.g. relationships, employment, additional child care responsibilities); (5) special circumstances inherent in breastfeeding twins (e.g. exhaustion, coordination of feedings); (6) prematurity issues (e.g. unpreparedness for delivery and breastfeeding, lack of conscious connection between prematurity status and infant behaviour); and (7) trigger events perceived to mark the beginning of breastfeeding difficulties (e.g. circumcision, in‐hospital formula supplementation for hypoglycemia).
In terms of hospital practices, the impact of unit cultural differences on the LPI breastfeeding course was noteworthy. In comparison with the well‐baby nursery, NICU breastfeeding schedules were more tightly regulated with an emphasis on product (quantity of pumped breast milk) over process (establishing at‐breast feeds) – perhaps leading to the palpable discomfort NICU mothers felt in transitioning to all at‐breast feedings. Conversely, NICU nursing staff was perceived to be more knowledgeable and supportive of breastfeeding than the nurses in the well‐baby nursery. NICU nurses also reinforced maternal confidence in breastfeeding through their comparisons of LPIs with more premature infants, positing LPIs as the breastfeeding ‘stars’ of the NICU.
I was surprised … with how well he's learning how to latch on and everything like that. [He's] a fast learner … Just like all the nurses say, he's feisty, very feisty. They said that the premature babies are usually just tired, just laying there, not really doing much. With this one, he was just active.
The most influential contextual factors impacting the LPI breastfeeding process were HCP support and a mother's prior breastfeeding experience. The availability, accessibility, perceived interest and provision of accurate information among HCPs (including paediatricians, lactation consultants, nurses and obstetricians) was highly variable, but figured prominently in how mothers viewed and managed breastfeeding. After hospital discharge, remarkably few mothers were aware of which practitioners they could consult for help. Most often, these mothers became self‐reliant, accessing information on the Internet or reaching out to trusted family or friends who had breastfed. Rarely were mothers given ‘warning signs’ of what to expect with breastfeeding a premature infant, and routine breastfeeding follow‐up post‐discharge was virtually nonexistent. At some point, most participants did consult the pediatrician about breastfeeding, who was perceived as available and convenient, but whose breastfeeding knowledge was often questionable.
Well [the pediatrician] asked me if she was still breastfeeding, and I told him, ‘Yeah.’ He's like, ‘Well keep doing it,’ I guess ‘cause she had gained enough weight. At this point, if I were to get any type of lactation support, it would be because I went out and got it … It's not like they're gonna come knock on my door and be like, ‘Hey, how's she doing?’ So I haven't tried to get any help.
Prior breastfeeding experience conferred an advantage in that mothers were aware of the temporary nature of breastfeeding issues, understood the concept of supply and demand and took early measures to protect their milk supplies. Experienced mothers were also more aware of breastfeeding resources and were less overwhelmed with learning the basics of infant care and breastfeeding, in addition to breastfeeding a less‐responsive infant. In fact, all of the mothers who stopped breastfeeding during the study period were first‐time mothers. The importance of experience in breastfeeding perseverance was voiced by almost all multiparas.
I just think that with [my oldest son] and [middle son], just how different they were … So I don't get as frustrated as I think I would if I didn't have the other ones … to know that, ok, so maybe this isn't just me, and eventually she'll catch on, kind of thing. So I think that's been helpful, just having other experiences, and not just her.
Discussion
We found breastfeeding within the late preterm population to be a volatile and labor‐intensive process, characterised by the coexistence of preterm obstacles and a ‘term'‐oriented environment. The misalignment between breastfeeding expectations and experiences led to anxiety, fatigue and mismanagement of issues. Mothers struggled to balance life responsibilities, while dealing with more typical ‘preterm’ concerns related to uncertain breastfeeding progress, muted feeding cues and lack of reciprocity within the breastfeeding relationship (Bernaix et al. 2006; Flacking et al. 2007). Unlike the more transient nature of breastfeeding issues noted in term dyads (Brandon et al. 2011) and more intensive, structured breastfeeding guidance typical within preterm NICU populations (Lupton & Fenwick 2001; Aagaard & Hall 2008), our work suggests that the LPI breastfeeding trajectory follows a less tightly regulated, more convoluted path, commencing in the hospital and evolving continuously during the post‐partum period.
The multifaceted social, psychological and biological nature of breastfeeding, coupled with the unique circumstances among late preterm mother–infant dyads, defied easy classification of our findings into existing theoretical models, such as the Theory of Planned Behaviour, Self‐Efficacy Theory or the Sense of Coherence Theory (Thomson & Dykes 2011). Perhaps most closely aligned with our model, both Wight (2003) and Meier et al. (2007) depict breastfeeding risk in the late preterm population as a negative cascade involving infant physiological issues, delayed lactogenesis II (associated with pregnancy or delivery complications), decreasing milk supply and increasing formula supplementation, which compromise breastfeeding success. Our model expands upon these representations by offering insight into maternal thought processes, individual variations, timing and circumstances leading to both success and failure scenarios.
The concepts of uncertainty, work and worth in breastfeeding are not new. The literature is rife with accounts describing the emotional fall‐out, guilt and despair when women's expectations and motivation to breastfeed based on the ‘naturalness’ of breastfeeding, the desire to ‘be a good mother’ or to ‘do what's best for the baby’ clash with the unmanageable and ‘surprising’ demands, intensity and ‘workload’ that breastfeeding entails (Schmied & Barclay 1999; Larsen et al. 2008; Burns et al. 2009). Uncertainty in these accounts encompasses the unsettling nature of at‐breast feeding when milk transfer is not readily visible. For mothers of preterm infants, uncertainty also centers around perception of inadequate milk supply and the infant's prognosis (Bernaix et al. 2006; Flacking et al. 2006). Burns et al. (2009) describes a scientific discourse of breastfeeding to which women are subjected, prescribing a ‘right way’ that breastfeeding mechanics and outcomes (e.g. weight gain) should be measured. This reinforces women's distrust of their bodies and discomfort with relying on infant satiety cues to ensure adequate nourishment, often leading to formula supplementation and early breastfeeding cessation (Kirkland & Fein 2003). In our sample, the tension among uncertainty, motivation and breastfeeding work seemed to be amplified, as LPI mothers operated under the auspices of a ‘normal’ breastfeeding experience, including lack of forewarning of potential issues by medical personnel and abbreviated breastfeeding support, while managing seemingly inexplicable infant breastfeeding behaviour related to prematurity. HCPs, particularly nurses and pediatricians, were disturbingly complicit in the process, as most participants encountered outdated, incorrect, and conflicting breastfeeding advice, as well as perceived lack of interest in ‘troubleshooting’ breastfeeding issues.
The lack of consistency in infant trajectory by gestational week, but fairly uniform improvement in wakefulness by 38–39 weeks of corrected gestation, was striking. These findings concur with literature noting attainment of neurological maturity around 39 weeks (Kinney 2006). Thus, our findings support the movement toward no elective deliveries before 39 weeks and the need to investigate ‘early term’ (37–38 weeks gestation) breastfeeding establishment, as well.
Our theoretical model indicates several areas for possible intervention, which should ideally commence in‐hospital, prior to the onset of the negative breastfeeding management cascade and irrevocable loss of milk supply. Both LPI mothers and HCPs should be educated on expected infant behaviour, basic breastfeeding interventions and available breastfeeding support resources. It is crucial that HCPs make repeated and sincere attempts to solidify the connection among infant behaviour, physiological prematurity and the high likelihood for problems compromising milk supply, especially for mothers who may have ‘term’ expectations based on infant weight or gestational age approaching 37 weeks. For care providers uncomfortable or unqualified to provide breastfeeding support for this population, referrals should be made to skilled lactation consultants with experience supporting mothers of premature infants. Considering the decreased suction pressures exerted by LPIs at breast, limiting their capacity to transfer adequate milk volumes and maintain an adequate maternal milk supply (Medoff‐Cooper et al. 2000), early breast milk expression should also be considered for all LPI mothers, regardless of how breastfeeding seems to be progressing.
LPI mothers and HCPs should be particularly cognizant of the risk–benefit ratio of formula supplementation. Research has shown that even small amounts of formula can drastically alter the normal gastrointestinal flora of an infant (Bullen et al. 1977), posing a substantial threat to the premature immune system. In addition, supplementation via bottle may be particularly problematic in the neurologically immature LPI population in terms of ‘imprinting’ a suck style or higher milk flow expectation that impedes the transition to at‐breast feeds (Neifert et al. 1995; Abouelfettoh et al. 2008). Indeed, participants in our study had prolonged struggles with ‘nipple confusion.’
The balance between work and worth should also be considered in LPI breastfeeding support. Our results indicate that mothers who are extremely committed to breastfeeding may be amenable to more intensive interventions – for example, providing formula via supplemental nursing systems1 to reduce the risk of later nipple confusion. First‐time LPI mothers, potentially at greater risk for breastfeeding failure, may benefit from more intensive breastfeeding support, including ‘the basics’ left uncovered before an unexpected delivery. The greater satisfaction we observed with regard to breastfeeding in the NICU certainly indicates a need for more thorough, extended LPI breastfeeding support.
Limitations
Because our sample was recruited from a single hospital system in one region, it is possible that our findings may not be applicable within other settings. The NICU culture, health care system characteristics and available breastfeeding support are likely to differ considerably in different places at different times. Although our sample is representative of the geographical area, the patient population available during data collection and the demographics most likely to breastfeed, our findings may not reflect the experiences of less educated, minority women and infants younger than 35 gestational weeks.
Our multiple data collection methods revealed some discrepancies between maternal memory and real‐time interview data. Though a natural reflection of how information is processed over time and represented to others (Sandelowski 1993), these inconsistencies required some form of resolution. When they occurred, clarification was sought, which sometimes led to even deeper reflection and understanding. When the discrepancy persisted, real‐time event data were considered ‘correct.’
A final limitation involved the duration of follow‐up. At the final interview (6–8 weeks post‐partum), several participants anticipated modifying breastfeeding based on return to work, familial demands or new information received from HCPs. Therefore, participants were re‐contacted via mail at 4–6 months, after IRB approval, to ascertain breastfeeding outcome. To date, nine mothers have been contacted, and six have provided responses. We recommend that future studies consider extended follow‐up periods, reliant on interviews or other methods convenient to participants, rather than non‐incentivised mailed questionnaires.
Source of funding
This work was funded by the National Institute of Nursing Research (F31NR011562) and additionally supported by Sigma Theta Tau International, Eta Chapter.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
JRD collected, analysed and interpreted the data and wrote the initial draft of the manuscript. All co‐authors assisted in the design of the study, interpretation of results and critical review of all sections of the text for important intellectual content. In addition, MBH and SMC provided regular consultation with JRD regarding study progress, analysis and sampling decisions.
Acknowledgements
We would like to thank Karen Wickersham, who provided thoughtful insight throughout the study process, and the study participants, who generously shared their time and breastfeeding experiences with us.
Footnotes
Device consisting of a bottle or container attached to a thin tube, opening onto the nipple of the breast. Often utilised to encourage at‐breast feeding or deliver supplemental nourishment without an artificial teat.
References
- Aagaard H. & Hall E. (2008) Mothers’ experiences of having a preterm infant in the neonatal care unit: a meta‐synthesis. Journal of Pediatric Nursing 23, e26–e36. [DOI] [PubMed] [Google Scholar]
- Abouelfettoh A., Dowling D., Dabash S., Elguindy S. & Seoud I. (2008) Cup versus bottle feeding for hospitalized late preterm infants in Egypt: a quasi‐experimental study. International Breastfeeding Journal 3, doi: 10.1186/1746-4358-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association of Women's Health, Obstetric, and Neonatal Nurses (2010) Assessment and Care of the Late Preterm Infant: Evidence‐Based Clinical Practice Guideline. AWHONN: Washington, DC. [Google Scholar]
- Baby‐Friendly USA (2010) BFHI USA . Available at: http://www.babyfriendlyusa.org/eng/index.html (Accessed 23 March 2011).
- Bernaix L., Schmidt C., Jamerson P., Seiter L. & Smith J. (2006) The NICU experience of lactation and its relationship to family management style. MCN. The American Journal of Maternal Child Nursing 31, 95–100. [DOI] [PubMed] [Google Scholar]
- Brandon D., Tully K., Silva S., Malcolm W., Murtha A., Turner B. et al (2011) Emotional responses of mothers of late‐preterm and term infants. Journal of Obstetric, Gynecologic, & Neonatal Nursing 40, 719–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullen C., Tearle P. & Stewart M. (1977) The effect of ‘humanised’ milks and supplemented breast feeding on the faecal flora of infants. Journal of Medical Microbiology 10, 403–413. [DOI] [PubMed] [Google Scholar]
- Burns E., Schmied V., Sheehan A. & Fenwick J. (2009) A meta‐ethnographic synthesis of women's experience of breastfeeding. Maternal & Child Nutrition 6, 201–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busse A. & Ferri R. (2003) Methodological reflections on a three‐step‐design combining observation, stimulated recall and interview. ZDM 35, 257–264. [Google Scholar]
- Callen J. & Pinelli J. (2005) A review of the literature examining the benefits and challenges, incidence and duration, and barriers to breastfeeding in preterm infants. Advances in Neonatal Care 5, 72–88. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2011) Breastfeeding report card‐United States, 2011 . Available at: http://www.cdc.gov/breastfeeding/pdf/2011BreastfeedingReportCard.pdf (Accessed 9 February 2012).
- Charmaz K. (2000) Grounded theory objectivist and constructivist methods In: Handbook of Qualitative Research (eds Denzin N.K. & Lincoln Y.S.), 2nd edn, pp 509–535. Sage Publications: Thousand Oaks, CA. [Google Scholar]
- Charmaz K. (2004) Premises, principles, and practices in qualitative research: revisiting the foundations. Qualitative Health Research 14, 976–993. [DOI] [PubMed] [Google Scholar]
- Charmaz K. (2006) Constructing Grounded Theory A Practical Guide through Qualitative Analysis. Sage: Los Angeles, CA. [Google Scholar]
- Flacking R., Ewald U., Nyqvist K. & Starrin B. (2006) Trustful bonds: a key to ‘becoming a mother’ and to reciprocal breastfeeding. Stories of mothers of very preterm infants at a neonatal unit. Social Science & Medicine 62, 70–80. [DOI] [PubMed] [Google Scholar]
- Flacking R., Ewald U. & Starrin B. (2007) ‘I wanted to do a good job’: experiences of ‘becoming a mother’ and breastfeeding in mothers of very preterm infants after discharge from a neonatal unit. Social Science & Medicine 64, 2405–2416. [DOI] [PubMed] [Google Scholar]
- Ip S., Chung M., Raman G., Chew P., Magula N., DeVine D. et al (2007) Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries . Evidence Report/Technology Assessment, No. 153. (AHRQ Publication No. 07‐E007). Agency for Healthcare Research and Quality: Rockville. [PMC free article] [PubMed]
- Kinney H. (2006) The near‐term (late preterm) human brain and risk for periventricular leukomalacia: a review. Seminars in Perinatology 30, 81–88. [DOI] [PubMed] [Google Scholar]
- Kirkland V. & Fein S. (2003) Characterizing reasons for breastfeeding cessation throughout the first year postpartum using the construct of thriving. Journal of Human Lactation 19, 278–285. [DOI] [PubMed] [Google Scholar]
- Larsen J., Hall E. & Aagaard H. (2008) Shattered expectations: when mothers' confidence in breastfeeding is undermined‐a metasynthesis. Scandinavian Journal of Caring Sciences 22, 653–661. [DOI] [PubMed] [Google Scholar]
- Lupton D. & Fenwick J. (2001) ‘They've forgotten that I'm the mum’: constructing and practising motherhood in special care nurseries. Social Science & Medicine 53, 1011–1021. [DOI] [PubMed] [Google Scholar]
- Martin J., Hamilton B., Sutton P., Ventura S., Mathews T., Kirmeyer S. et al (2010) Births: final data for 2007. National Vital Statistics Reports 58, 1–125. [PubMed] [Google Scholar]
- Medoff‐Cooper B., McGrath J. & Bilker W. (2000) Nutritive sucking and neurobehavioral development in preterm infants from 34 weeks PCA to term. MCN. The American Journal of Maternal Child Nursing 25, 64–70. [DOI] [PubMed] [Google Scholar]
- Meier P., Furman L. & Degenhardt M. (2007) Increased lactation risk for late preterm infants and mothers: evidence and management strategies to protect breastfeeding. Journal of Midwifery & Women's Health 52, 579–587. [DOI] [PubMed] [Google Scholar]
- Morse J., Stern P., Corbin J., Bowers B., Charmaz K. & Clarke A. (2009) Developing Grounded Theory the Second Generation. Left Coast Press: Walnut Creek. [Google Scholar]
- Neifert M., Lawrence R. & Seacat J. (1995) Nipple confusion: toward a formal definition. The Journal of Pediatrics 126, S125–S129. [DOI] [PubMed] [Google Scholar]
- Radtke J. (2011) The paradox of breastfeeding‐associated morbidity among late preterm infants. Journal of Obstetric, Gynecologic, & Neonatal Nursing 40, 9–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandelowski M. (1993) Rigor or rigor mortis: the problem of rigor in qualitative research revisited. ANS. Advances in Nursing Science 16, 1–8. [DOI] [PubMed] [Google Scholar]
- Schmied V. & Barclay L. (1999) Connection and pleasure, disruption and distress: women's experience of breastfeeding. Journal of Human Lactation 15, 325–334. [DOI] [PubMed] [Google Scholar]
- The Academy of Breastfeeding Medicine (2011) ABM clinical protocol #10: breastfeeding the late preterm infant (34 /07 to 36 6/7 weeks gestation). Breastfeeding Medicine 6, 151–156. [DOI] [PubMed] [Google Scholar]
- Thomson G. & Dykes F. (2011) Women's sense of coherence related to their infant feeding experiences. Maternal and Child Nutrition 7, 160–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wight N. (2003) Breastfeeding the borderline (near‐term) preterm infant. Pediatric Annals 32, 329–336. [DOI] [PubMed] [Google Scholar]
- Wight N., Morton J. & Kim J. (2008) Best Medicine: Human Milk in the NICU. Hale Publishing: Amarillo, TX. [Google Scholar]


