Abstract
Cardiovascular risk factors are known to be associated with intervertebral disc degeneration, but the underlying mechanism is still unclear. ApoE knockout (KO) mouse is a well-established model for arthrosclerosis. We hypothesize that ApoE may involve in maintaining disc health and ApoE KO mouse develops early disc degeneration. Discs of ApoE KO and wild-type (WT) mice were characterized with histological/immunological, biochemical, and real time RT-PCR assays. A comparison of the extracellular matrix production was also performed in disc cells. We demonstrated that ApoE was highly expressed in the endplates of WT discs and ectopic bone formed in the endplates of ApoE KO discs. Glycosaminoglycan content was decreased in both ApoE KO annulus fibrosus (AF) and nucleus pulpsous (NP) cells. Collagen levels were increased in AF and decreased in NP cells. Matrix metalloproteinases-3, 9, and 13 expression was increased which may partially explain the impaired matrix production. We also found increased collagen I, II, aggrecan and biglycan mRNA expressions in AF cells but decreased in NP cells. Apoptosis was increased in the ApoE KO NP tissue. These results suggest early disc degeneration changes in ApoE KO mice. ApoE, plus its importance to cardiovascular disease, may play a critical role in disc integrity and function.
Keywords: intervertebral disc, ApoE, disc degeneration, apoptosis, extracellular matrix
1. Introduction
Chronic low back pain (LBP) is one of the leading causes of disability in developed countries. A vast majority of the population (up to 80%) experiences chronic LBP over the course of their lives. Although the precise cause of chronic LBP has yet to be determined, intervertebral disc degeneration disease (DDD) appears to be a major factor contributing to pain and disability[1]. The development of DDD is a physiologically complex and poorly understood process involving both environmental and genetic factors[2].
Previous studies have suggested that certain risk factors involved in the pathogenesis of cardiovascular diseases are also associated with the development of DDD. Jhawar et al[3] reported that lumbar disc herniation associated with cardiovascular diseases such as high cholesterol, hypertension, and myocardial infarction before age 60. The Hangai group [4] found 57–60% of the aging Japanese population experienced DDD, as diagnosed by MRI and its close association with cardiovascular risk factors, including aging, greater body mass index, and higher low density lipoprotein (LDL).
Apolipoprotein E (ApoE) is a ligand of the LDL receptor and structural component of several lipoprotein classes (HDL, VLDL, chylomicrons, and their remnants), involves in lipoprotein metabolism and atherosclerosis. ApoE knockout (KO) mouse develops severe hyperlipidemia, spontaneous atherosclerotic lesions, and is one of the established animal models for atherosclerosis. In ApoE KO mice, aortic lesions were detected as early as 10 weeks with chow diet and 8 weeks with high fat diet [5]. Atheroma was found to increase in size in direct relation to increasing age of the animal. In aging ApoE KO mice, calcification, a process of mineralization akin to bone formation, occurs consistently and reproducibly in advanced atherosclerotic lesions [6]. Osteogenic cells along with the regulatory proteins involved in the [12–14], while on a high fat diet, the bone volume was decreased [14, 15]. However, to the best of our knowledge, the potential role of ApoE in the development of DDD is not reported so far.
As accumulating studies have shown that atherosclerosis and cardiovascular risk factors are associated with intervertebral disc degeneration [3,4], we hypothesized that ApoE deficiency may alter the integrity of the intervertebral disc causing impairment of the nutrition supply to the disc thereby leading to DDD. In this study, we demonstrate that absence of the ApoE gene results in abnormal bone formation within the endplate leading to imbalance of extracellular matrix, and triggering apoptotic pathways. These findings provide insights linking the pathogenesis of DDD with cardiovascular diseases.
2. Materials and Methods
2.1 Animals
Wild type C57BL/6J (WT) and ApoE KO female mice were purchased from the Jackson laboratory, and were fed with a regular chow diet. Euthanasia was performed at age 5, 10 and 15 weeks, and lumbar spine specimens were harvested from WT and ApoE KO mice. All procedures were performed according to prior approval by the Institutional Animal Care and Use Committee at the University of Virginia.
2.2 Radiographic analyses
The radiograph was captured using a low energy X-ray (Faxitron, Hewlett Packard, Model 43805N, McMinnville, OR) with an exposure time of 30 s (30 kV) on animals while under general anesthesia using a 2% isoflurane/oxygen mixture during the procedure.
2.3 Histology and Immunohistochemistry
Lumbar discs were fixed with 4% paraformaldehyde followed by 0.25M EDTA decalcification for 2 weeks. Six μm thick sections were stained with Safranin-O and fast green for detection of proteoglycan as described previously [16]. The sections were prepared and stained with antibodies for Type-II collagen (Chondrex, WA), Osteocalcin (OCN, SC-30045), ApoE (SC-6384), or Aggrecan (SC-25674) (Santa Cruz Biotechnology, CA). The detection of Type-II collagen was performed as previously described [17]. For the other remaining antibodies, the sections were deparaffinized, rehydrated and treated with 3% hydrogen peroxide in methanol for 30 min for blockade of endogenous peroxidase. Antigen retrieval was performed by boiling samples in 10 mM citrate buffer (pH6.0) for 30 min followed by incubation with the following polyclonal antibodies: ApoE (1:300), OCN (1:200), and Aggrecan (1:200) overnight at 4°C. Six mice from both WT and ApoE KO groups for each time points (5, 10 and 15 weeks) were examined in this experiment.
2.4 Cell Culture
The discs were dissected under sterile conditions as reported previously [18, 19] and the annulus fibrosus (AF) and nucleus pulposus (NP) tissues were harvested from lumbar discs (L1–L4) of 4 individuals from both ApoE WT and KO mice at age 15 week immediately after euthanasia. Cells were cultured in DMEM/F-12 media with 10% fetal bovine serum (Invitrogen), 1% penicillin/streptomycin, and 1% ascorbate at 37 °C, and media were changed every other day. Cells were maintained at sub-confluent and passaged with trypsin-EDTA (Invitrogen, CA). Passage 2–3 cells were used for experiments. Cells were pooled from 4 mice of each genotype for each single experiment and each experiment was performed in triplicates
2.5 Biochemical Assay
Disc cells from 4 WT and ApoE KO mice, respectively, were used for biochemical assay. Amino sugars and hydroxyproline (Hypro), as indicators of glycosaminoglycan (GAG) and collagen, respectively, were measured as reported [18]. The GAG and Hypro concentrations were normalized to DNA concentration.
2.6 Real- time PCR
Total RNA was isolated with the RNeasy Kit (Qiagen, CA) following manufacturer's instruction. cDNA was synthesized with 0.5 μg total RNA by iScript cDNA Synthesis kit (Bio-Rad, CA ). Real-time PCR was performed with iQ SYBR Green Supermix Kit (Bio-Rad, CA) using specific primers (table 1). Gene expression was calculated using the ΔΔCt method according to ABI (2001) and normalized to 18s, and expressed as fold change. Cells isolated from 4 mice of each genotype were used for real time RT-PCR analysis.
Table 1.
The primers sequences
| Target gene | Forward primer (5'-3') | Reverse primer (5'-3') |
|---|---|---|
| ApoE | TGTTTCGGAAGGAGCTGACT | TGTGTGACTTGGGAGCTCTG |
| Runx2 | AGTCCCAACTTCCTGTG | GGTGAAACTCTTGCCTCGTC |
| OCN | AAGCAGGAGGGCAATAAG | AGGACAGGGAGGATCAAG |
| ALP | ACGAGATGCCACCAGAGG | AGTTCAGTGCGGTTCCAG |
| Col I | TTGTTCTCCTGGTAAAGATGGT | CAGTA CACCAGGTTCACCTTTC |
| Col II | TCCAGGATCTGCACTGAATG | TCTGCCCAGTTCAGGTCTCT |
| Agg | CAGCAGCACCATCACAGAGT | TTTCTGCTGTCTGGGTCTCC |
| Bgn | GAACAACTGCCACCGCCATTG | CAAGCAGAGCCCAGGAGAGC |
| MMP-3 | ATGAAA ATGAAGGGTCTTCCGG | GCAGAAGCTCCATACCAGCA |
| MMP-9 | AATCTCTTCTAGAGACTGGGAAGGAG | AGCTGATTGACTAAAGTAGCTGGA |
| MMP-13 | AAGGAGCATGGCGACTTCT | TGGCCCAGGAGGAAAAGC |
| 18S | CGGCGACGACCCATTCGAAC | GAATCGAACCCTGATTCCCCGTC |
2.7 TUNEL Assay
Visualization of apoptotic cells with terminal deoxynucleotidyltranferase-mediated dUTP-biotin nick end labeling (TUNEL) was performed using paraffin-embedded sections analyzed with the In Situ Cell Death Detection POD Kit (Roche, Germany) [19]. The disc sections from 5 WT and ApoE KO mice at age 15 weeks were used for TUNEL assay. The apoptotic cells were counted at 5 visual fields with FluoView software.
2.7 Statistical analysis
Statistical significance among the differences in the means of biochemistry assay and gene expression data was analyzed by the Student's t-test. All data are presented as mean ± standard deviation. A p value of < 0.05 was considered statistically significant. Each experiment was performed in triplicates.
3.RESULTS
3.1 High expression of ApoE in lumbar disc endplate
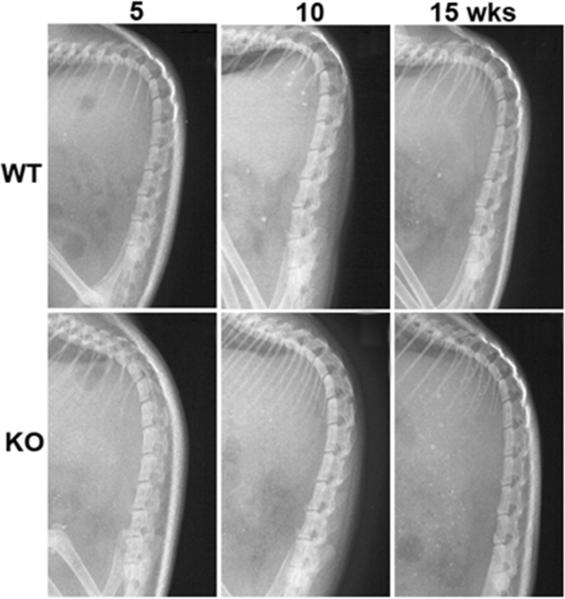
ApoE was observed in a variety of tissues including liver, intestine, spleen, kidney, adrenal gland, brain, and bone [20]. In the present study, ApoE expression was also observed within disc cells by RT-PCR method (Fig. 1A). Using X-ray imaging, no obvious spinal structural defects were found in ApoE KO mice when compared to WT mice (Fig. 1). The presence of ApoE was also detected within intervertebral disc using in situ immunohistochemistry. Surprisingly, as shown in Fig. 2B, ApoE was highly expressed in the WT endplates at 5- (Fig. 2C) and 15- (Fig. 2D) week old mice. Both NP and AF cells showed positive signals for ApoE though with lesser abundance than the endplate region. ApoE was also present in the adjacent vertebral bone tissue. The expression of ApoE was similar for the ages of mice evaluated (5–15 weeks). As expected, ApoE was not detected in any of the ApoE KO mice (Fig. 2B). IgG was used as a negative control.
Fig.1.
Radiographs show little spinal changes in ApoE KO mice compared with WT mice at the ages of 5 wks, 10 wks and 15 wks.
Fig. 2.
ApoE is highly expressed in the endplates of intervertebral discs. A: Total RNA was isolated from tissues of WT and ApoE KO mice (4 mouse of each genotype) at 15 W. The ApoE mRNA was detected by RT-PCR assay with specific primers. 18s rRNA was used as an internal loading control. B–D: representative images showing ApoE is highly expressed in the endplates of WT discs by immunohistochemistry method. The discs were fixed and embedded for sectioning. Frontal sections were stained with ApoE antibody and biotinylated IgG. The signals were developed with 3,3'-Diaminobenzidine and photographed on an Axioskop 2 Zeiss microscope. Scale bar = 200 μm. Arrow shows the positive signal of ApoE. Six mice of each genotype were used for the experiment.
3.2 Ectopic bone formation within intervertebral disc of ApoE KO mice
The role of ApoE in the discs was investigated in both WT and ApoE KO mice by analyzing and comparing any abnormalities in spinal structure microscopically. Histological analysis of ApoE KO mice endplates indicated significant amount of ectopic bone formation (Fig. 3A) at age 10 and 15 weeks. Approximately 75–80% of ApoE KO discs showed ectopic bone formation. Bone formation was not apparent in the discs of 5 week ApoE KO mice. Bone formation was confirmed with immunostaining for Osteocalcin, a specific bone formation marker. As depicted in Fig. 3B, Osteocalcin stained positively in the endplates of ApoE KO discs. In isolated AF cells, mRNA expression of osteoblast transcription factor runt-related transcription factor 2 (Runx2), alkaline phosphatase (ALP, a bone marker) and Osteocalcin were also elevated (Fig. 3C).
Fig. 3.
Ectopic bone is formed in the endplates of ApoE KO discs. A: Representative images show ectopic bone formation in endplates of ApoE KO discs by histological assay. The discs at age 5-, 10-, and 15-week were fixed, decalcified, and the sections were stained with Safranin-O. B: Osteocalcin protein present in the endplates where ectopic bone formed region of ApoE KO mice but not WT mice. The vertical sections of discs were stained with Osteocalcin antibody. Scale bar = 200 μm. Arrow head: bone formation area. C: Bone specific marker genes elevated in the cultured ApoE KO AF cells. The AF cells were isolated from 15-week-old WT and ApoE KO mice. The total RNA was isolated, and the expression of Osteocalcin (OCN), Runx2, and alkaline phosphate (ALP) were quantified by real time RT-PCR. mRNA was normalized to 18s. Cells from 4 mice of each genotype were pooled and each experiment was triplicated. *p < 0.05
3.3 Extracellular matrix of ApoE KO intervertebral discs
Collagen and proteoglycan are the two major extracellular matrix components of intervertebral discs and demonstrated to play critical roles in normal disc function. In ApoE KO AF cells, GAG (reflects proteoglycan) content had no significant changes while hydroxyproline (reflects collagen) was found to be significantly increased. In contrast, both GAG and hydroxyproline were decreased in ApoE KO NP cells (Fig. 4A). The expression of extracellular matrix genes was also evaluated with real time PCR. As shown in Fig. 4B, the expression of collagen I, II, aggrecan, and biglycan was significantly higher in ApoE KO AF cells but decreased in ApoE KO NP cells when compared to WT cells. We further evaluated in situ expression of collagen II and aggrecan in the intervertebral disc sections by immunohistochemistry assay. As demonstrated in Fig. 5, there was no noticeable change in both collagen II and aggrecan expression in discs of ApoE KO mice at age 15 weeks compared to WT.
Fig. 4.
The extracellular matrix profile of ApoE KO discs. A: The contents of GAG is significantly decreased in NP cells of ApoE KO mice, while the hydroxyproline is increased in AF cells and decreased in the NP cells. The AF and NP cells were isolated from WT and ApoE KO discs at age 15 weeks. The contents of GAG and hydroxyproline were measured by biochemical assays. Data was normalized to the content of DNA. B: The expression of collagen I, II, aggrecan, and biglycan genes is decreased and increased in the NP and AF cells, respectively. Total RNA was isolated and gene expression was measured by real time RT-PCR. mRNA was normalized to 18s. Cells from 4 mice of each genotype were pooled and each experiment was triplicated. *p < 0.05
Fig. 5.
There are no noticeable changes in both Collagen II and aggrecan expression in the discs of ApoE KO and WT mice. The discs from 15–week-old mice were fixed and stained with collagen II and aggrecan antibodies. Representative images are shown. Scale bar = 200μm. Six mice from each genotype were used.
3.4 MMP expression was increased in intervertebral discs of ApoE KO mice
Central to the pathophysiology of DDD is an imbalance of matrix synthesis and degradation. Matrix metalloproteinase (MMPs) play a major role in extracellular matrix degradation within the discs [21, 22]. In the present study, the expression of MMPs was measured in isolated AF cells. As indicated in Fig. 6, the expressions of MMP-3, -9, and -13 were significantly increased (1.5–2.2 fold) in ApoE KO disc cells as compared with WT cells. This suggests that MMPs may potentially play a major role in the early stage of DDD in ApoE KO mice.
Fig. 6.

The expression of MMPs is increased in the ApoE KO discs. Subconfluent cultured AF cells were harvested and followed by total RNA extraction. The expression of MMP-3, -9, and -13 was evaluated by RT-PCR with specific primers. mRNA was normalized to 18s. Cells from 4 mice of each genotype were pooled and each experiment was triplicated. *p < 0.05
3.5 Deletion of ApoE induces apoptosis in the intervertebral discs
Thus far, all the evidence suggests that ApoE KO mice display early stages of DDD pathophysiology. The next step was to determine whether apoptotic pathways played a role in the pathogenesis of DDD in ApoE null mice. To address this question, the in situ cell deaths were measured with the TUNEL assay. As shown in Fig. 7A and 7B, more NP cells underwent apoptosis in ApoE KO mice than WT mice at age 15 weeks. No appreciable change in apoptosis was found between WT and KO mice AF cells. Gene expression also revealed the increased mRNA expression of Fas gene in disc cells of ApoE KO mice (Fig. 7C)
Fig. 7.
Apoptosis is induced in the discs of ApoE KO mice. A: The discs from 15-week-old mice were fixed. The sections were stained with an in situ cell death kit. The apoptotic cells were stained in green color and the nucleus were counterstained with Topro (red signal). B: Bar graph shows the quantitation of the positive apoptotic cell number. Five mice of each genotype were used, * p < 0.05. C: The expression of Fas gene is evaluated by real time RT-PCR with specific primers. mRNA was normalized to 18s. Cells from 4 mice of each genotype were pooled and each experiment was triplicated. *p < 0.05
4. Discussion
DDD is a common disease with the majority of any population experiencing disc degeneration of some extent after age 70 [23]. The health and economic consequences of those suffering from back pain are remarkable. The clear etiology and pathogenesis of the disease, however, is still unclear. Cardiovascular risk factors began drawing the attention of DDD research in last few years. An array of cardiovascular risk factors such as age, smoking, hypertension, high cholesterol, and diabetes has been reported to be related to DDD and back pain [24–26]. In the present study, we found ectopic bone formation in the endplate region of the discs in ApoE KO mice, a well defined atherosclerosis animal model. The structural change in the disc was accompanied with altered extracellular matrix production, up-regulated MMP levels, and increased apoptosis.
A rising number of studies have shown that inflammatory and pro-inflammatory mediators such as macrophage infiltration, prostaglandins, and cytokine production involved in the progression of DDD. Interleukin-6, -8, -17, prostaglandin E2, nitric oxide, TNF-alpha, IFN-gamma, and intercellular adhesion molecule-1 have been shown to be produced or released in herniated discs or degenerative disc tissues [27–31]. The Weissleder group has shown that atherosclerotic inflammation precedes osteogenic activity and promotes vascular wall ossification in ApoE deficient mice [32]. We have previously shown that AF cells are capable of differentiating to osteoblasts in the osteogenic conditions [33]. A new report showed that mesenchymal stem cells existed in the degenerative human intervertebral disc cartilage endplate [34]. Therefore, one of the possible mechanisms for ectopic bone formation in the endplates of ApoE KO mice may be mediated at least in part through osteogenic differentiation of AF cells and/or endplate cells stimulated by pro-inflammatory mediators. In addition to the ectopic bone formation in the endplate region, we found abundant expression of ApoE in the vertebral endplate, which suggested that ApoE may play a critical role in the endplate. The cartilaginous endplates are normally avascular and aneural in the healthy adult [35]. Pathological conditions such as bony sclerosis, compromised blood flow, or endplate ossification can significantly block the efficient transport of nutrients into the discs as shown in Figure 8. By this effect, ectopic bone formation within the endplate region will negatively affect disc cell metabolism. Previous studies also showed that bone mineral density was increased in ApoE null mice when fed on a chow diet [13], and that high bone marrow density in the vertebra associated with severe adjacent disc degeneration [36]. We did not detect significant changes in spinal column structure with X-ray in 15-week ApoE KO mice, and this may due to young age of mice and insensitivity of X-ray method.
Fig.8.
Scheme illustrating pathogenesis of intervertebral disc degeneration in ApoE KO mice: Ectopic bone formation in the endplates defers the nutrition supplies to intervertebral disc.
The composition and organization of the extracellular matrix govern the mechanical responses and therefore maintain the mechanical functions of intervertebral discs. In the progression of DDD, the delicate balance between extracellular matrix synthesis and degradation is disturbed. In general, the disc degeneration process starts with proteoglycan breakdown and loss of cellular matrix, leading to diminished water retaining capacity and disc dehydration [37]. Accumulation of protein degradation products serve as an early marker of degenerative changes in discs. In cultured NP cells of ApoE KO mice, the content of GAG was decreased. With regards to collagen content, there was an increase in AF cells and a decrease in NP cells of ApoE KO mice. Gene expression profiles were different from NP and AF cells as the mRNA level of collagen, aggrecan, and biglycan was increased in the AF cells while decreased in the NP cells of ApoE KO mice. These data are consistent with previous reports that NP is more vulnerable than AF towards many pathological factors and responds with a progressive decline in both proteoglycan and collagens. AF on the other hand first responds with increased extracellular matrix gene expression and protein production, seen most markedly with collagens [38]. However, as the degeneration progresses, AF is not able to match much needed production of extracellular matrix to maintain the balance between demand and supply as shown by declined proteoglycan production with relatively increased collagen production along with a typical phenotype changes. We did not observe a significant change in both type II collagen and aggrecan expression at protein level by immunohistochemical method (Fig. 5). The remodeling of extracellular matrix in both normal and pathological conditions is regulated by MMPs, which is significantly increased as shown in Fig 6. Therefore, although the gene expression level of type II collagen and aggrecan is increased in Fig 4, no significant difference of Col II and aggrecan expression at the protein level is found (Fig 5). It is possible that the compensatory response of AF cells to increase the synthesis of type II collagen and aggrecan in the beginning of DDD reflected by Fig 4A is counteracted by the increase of MMPs. Besides, the discordant result in present study may be caused by the method not being sensitive enough to detect all the proteins, or that the antibodies are specific for only certain fragments of the proteins. Moreover, the turnover of the extracellular matrix proteins within the disc is very slow, which would be expected to induce changes on the order of months rather than weeks.
Consistent with previous reports[21, 22, 39], we found that mRNA expression of MMP-3, -9, and -13 was significantly increased in isolated ApoE null disc cells compared to WT. The atherosclerotic plaques from ApoE KO mice have exhibited a higher MMPs expression. The increased MMPs activities in cardiovascular disease are considered to be caused by up-regulation of reactive oxygen species in ApoE KO mice, which is manifested by increased oxidized low density lipoprotein and nitric oxide [40–42]. The reasons of increased MMPs in intervertebral disc cells deserve a detailed study.
Another important pathway for initiation and progression of DDD is apoptosis [43]. Apoptotic-cell surface proteins, including those from the Fas/Fas ligand system, have been identified in disc cells. The Fas receptor was found to be expressed only after the onset of induced degeneration, suggesting its active role in the apoptotic process. Park et al [43] previously demonstrated that apoptosis occurred in herniated lumbar discs, and found a positive relationship between the degree of apoptosis and disc degeneration. In the present study, in NP region of ApoE KO disc, more number of NP cells were following apoptotic change compared to WT disc (Fig. 7). Meanwhile, the Fas gene was significantly increased in ApoE KO cultured disc cells (Fig 7C). Thus, one of the mechanisms of apoptotic processes in ApoE KO discs may be mediated through the Fas/Fas ligand pathway. The enhanced apoptotic process may also mediate through the p53 pathway as suggested by Nakamura group in osteoblasts [15].
In conclusion, we demonstrate that ApoE protein is highly expressed in the endplates of WT mice and that disc degeneration occurs in the ApoE KO mice model. The results from the studies provide a better understanding of the underlying pathogenesis mediating disc degeneration. This study also begins to link the pathophysiology mediating two highly prevalent cardiovascular and disc degeneration diseases. Additional studies are needed to further elucidate the pathophysiology of ApoE deficiency induced disc degeneration, and how mechanisms underlying disc degeneration and cardiovascular diseases are correlated.
Acknowledgement
The work was supported by AO Foundation and NIH R03 AR053653.
Abbreviations
- DDD
(intervertebral disc degeneration disease)
- GAG
(glycosaminoglycan)
- MMP
(matrix metalloproteinase)
- WT
(wild type)
- KO
(knockout)
- ApoE
(apolipoprotein E)
- LBP
(low back pain)
Footnotes
The authors have no conflict of interests.
References
- [1].Battie MC, Videman T, Levalahti E, Gill K, Kaprio J. Heritability of low back pain and the role of disc degeneration. Pain. 2007;131:272–80. doi: 10.1016/j.pain.2007.01.010. [DOI] [PubMed] [Google Scholar]
- [2].Anderson DG, Tannoury C. Molecular pathogenic factors in symptomatic disc degeneration. Spine J. 2005;5:260S–266S. doi: 10.1016/j.spinee.2005.02.010. [DOI] [PubMed] [Google Scholar]
- [3].Jhawar BS, Fuchs CS, Colditz GA, Stampfer MJ. Cardiovascular risk factors for physician-diagnosed lumbar disc herniation. Spine J. 2006;6:684–91. doi: 10.1016/j.spinee.2006.04.016. [DOI] [PubMed] [Google Scholar]
- [4].Hangai M, Kaneoka K, Kuno S, Hinotsu S, Sakane M, Mamizuka N, Sakai S, Ochiai N. Factors associated with lumbar intervertebral disc degeneration in the elderly. Spine J. 2008;8:732–40. doi: 10.1016/j.spinee.2007.07.392. [DOI] [PubMed] [Google Scholar]
- [5].Nakashima Y, Plump AS, Raines EW, Breslow JL, Ross R. ApoE-deficient mice develop lesions of all phases of atherosclerosis throughout the arterial tree. Arterioscler Thromb. 1994;14:133–40. doi: 10.1161/01.atv.14.1.133. [DOI] [PubMed] [Google Scholar]
- [6].Bostrom K, Watson KE, Stanford WP, Demer LL. Atherosclerotic calcification: relation to developmental osteogenesis. Am J Cardiol. 1995;75:88B–91B. doi: 10.1016/0002-9149(95)80020-s. [DOI] [PubMed] [Google Scholar]
- [7].Duer MJ, Friscic T, Proudfoot D, Reid DG, Schoppet M, Shanahan CM, Skepper JN, Wise ER. Mineral surface in calcified plaque is like that of bone: further evidence for regulated mineralization. Arterioscler Thromb Vasc Biol. 2008;28:2030–4. doi: 10.1161/ATVBAHA.108.172387. [DOI] [PubMed] [Google Scholar]
- [8].Shiraki M, Shiraki Y, Aoki C, Hosoi T, Inoue S, Kaneki M, Ouchi Y. Association of bone mineral density with apolipoprotein E phenotype. J Bone Miner Res. 1997;12:1438–45. doi: 10.1359/jbmr.1997.12.9.1438. [DOI] [PubMed] [Google Scholar]
- [9].Cauley JA, Zmuda JM, Yaffe K, Kuller LH, Ferrell RE, Wisniewski SR, Cummings SR. Apolipoprotein E polymorphism: A new genetic marker of hip fracture risk--The Study of Osteoporotic Fractures. J Bone Miner Res. 1999;14:1175–81. doi: 10.1359/jbmr.1999.14.7.1175. [DOI] [PubMed] [Google Scholar]
- [10].Pluijm SM, Dik MG, Jonker C, Deeg DJ, van Kamp GJ, Lips P. Effects of gender and age on the association of apolipoprotein E epsilon4 with bone mineral density, bone turnover and the risk of fractures in older people. Osteoporos Int. 2002;13:701–9. doi: 10.1007/s001980200096. [DOI] [PubMed] [Google Scholar]
- [11].Niemeier A, Schinke T, Heeren J, Amling M. The role of apolipoprotein E in bone metabolism. Bone. 2012;50:518–24. doi: 10.1016/j.bone.2011.07.015. [DOI] [PubMed] [Google Scholar]
- [12].Nikolov IG, Joki N, Nguyen-Khoa T, Ivanovski O, Phan O, Lacour B, Drueke TB, Massy ZA, Dos Reis LM, Jorgetti V, Lafage-Proust MH. Chronic kidney disease bone and mineral disorder (CKD-MBD) in apolipoprotein E-deficient mice with chronic renal failure. Bone. 2010;47:156–63. doi: 10.1016/j.bone.2010.04.600. [DOI] [PubMed] [Google Scholar]
- [13].Schilling AF, Schinke T, Munch C, Gebauer M, Niemeier A, Priemel M, Streichert T, Rueger JM, Amling M. Increased bone formation in mice lacking apolipoprotein E. J Bone Miner Res. 2005;20:274–82. doi: 10.1359/JBMR.041101. [DOI] [PubMed] [Google Scholar]
- [14].Bartelt A, Beil FT, Schinke T, Roeser K, Ruether W, Heeren J, Niemeier A. Apolipoprotein E-dependent inverse regulation of vertebral bone and adipose tissue mass in C57Bl/6 mice: modulation by diet-induced obesity. Bone. 2010;47:736–45. doi: 10.1016/j.bone.2010.07.002. [DOI] [PubMed] [Google Scholar]
- [15].Hirasawa H, Tanaka S, Sakai A, Tsutsui M, Shimokawa H, Miyata H, Moriwaki S, Niida S, Ito M, Nakamura T. ApoE gene deficiency enhances the reduction of bone formation induced by a high-fat diet through the stimulation of p53-mediated apoptosis in osteoblastic cells. J Bone Miner Res. 2007;22:1020–30. doi: 10.1359/jbmr.070330. [DOI] [PubMed] [Google Scholar]
- [16].Li X, Jin L, Balian G, Laurencin CT, Greg Anderson D. Demineralized bone matrix gelatin as scaffold for osteochondral tissue engineering. Biomaterials. 2006;27:2426–33. doi: 10.1016/j.biomaterials.2005.11.040. [DOI] [PubMed] [Google Scholar]
- [17].Feng G, Yang X, Shang H, Marks IW, Shen FH, Katz A, Arlet V, Laurencin CT, Li X. Multipotential differentiation of human anulus fibrosus cells: an in vitro study. J Bone Joint Surg Am. 2010;92:675–85. doi: 10.2106/JBJS.H.01672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cui M, Wan Y, Anderson DG, Shen FH, Leo BM, Laurencin CT, Balian G, Li X. Mouse growth and differentiation factor-5 protein and DNA therapy potentiates intervertebral disc cell aggregation and chondrogenic gene expression. Spine J. 2008;8:287–95. doi: 10.1016/j.spinee.2007.05.012. [DOI] [PubMed] [Google Scholar]
- [19].Feng G, Wan Y, Shen FH, Li X. Nucleus pulposus explant culture model. J Orthop Res. 2009;27:814–9. doi: 10.1002/jor.20803. [DOI] [PubMed] [Google Scholar]
- [20].Lin-Lee YC, Kao FT, Cheung P, Chan L. Apolipoprotein E gene mapping and expression: localization of the structural gene to human chromosome 19 and expression of ApoE mRNA in lipoprotein- and non-lipoprotein-producing tissues. Biochemistry. 1985;24:3751–6. doi: 10.1021/bi00335a050. [DOI] [PubMed] [Google Scholar]
- [21].Weiler C, Nerlich AG, Zipperer J, Bachmeier BE, Boos N. 2002 SSE Award Competition in Basic Science: expression of major matrix metalloproteinases is associated with intervertebral disc degradation and resorption. Eur Spine J. 2002;11:308–20. doi: 10.1007/s00586-002-0472-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Le Maitre CL, Pockert A, Buttle DJ, Freemont AJ, Hoyland JA. Matrix synthesis and degradation in human intervertebral disc degeneration. Biochem Soc Trans. 2007;35:652–5. doi: 10.1042/BST0350652. [DOI] [PubMed] [Google Scholar]
- [23].Luoma K, Riihimaki H, Luukkonen R, Raininko R, Viikari-Juntura E, Lamminen A. Low back pain in relation to lumbar disc degeneration. Spine (Phila Pa 1976) 2000;25:487–92. doi: 10.1097/00007632-200002150-00016. [DOI] [PubMed] [Google Scholar]
- [24].Kauppila LI. Atherosclerosis and disc degeneration/low-back pain--a systematic review. Eur J Vasc Endovasc Surg. 2009;37:661–70. doi: 10.1016/j.ejvs.2009.02.006. [DOI] [PubMed] [Google Scholar]
- [25].Viikari-Juntura E, Shiri R, Solovieva S, Karppinen J, Leino-Arjas P, Varonen H, Kalso E, Ukkola O. Risk factors of atherosclerosis and shoulder pain--is there an association? A systematic review. Eur J Pain. 2008;12:412–26. doi: 10.1016/j.ejpain.2007.08.006. [DOI] [PubMed] [Google Scholar]
- [26].Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Varonen H, Kalso E, Ukkola O, Viikari-Juntura E. Cardiovascular and lifestyle risk factors in lumbar radicular pain or clinically defined sciatica: a systematic review. Eur Spine J. 2007;16:2043–54. doi: 10.1007/s00586-007-0362-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Weiler C, Nerlich AG, Bachmeier BE, Boos N. Expression and distribution of tumor necrosis factor alpha in human lumbar intervertebral discs: a study in surgical specimen and autopsy controls. Spine (Phila Pa 1976) 2005;30:44–53. doi: 10.1097/01.brs.0000149186.63457.20. discussion 54. [DOI] [PubMed] [Google Scholar]
- [28].Le Maitre CL, Freemont AJ, Hoyland JA. The role of interleukin-1 in the pathogenesis of human intervertebral disc degeneration. Arthritis Res Ther. 2005;7:R732–45. doi: 10.1186/ar1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Gronblad M, Virri J, Tolonen J, Seitsalo S, Kaapa E, Kankare J, Myllynen P, Karaharju EO. A controlled immunohistochemical study of inflammatory cells in disc herniation tissue. Spine (Phila Pa 1976) 1994;19:2744–51. doi: 10.1097/00007632-199412150-00002. [DOI] [PubMed] [Google Scholar]
- [30].Gabr MA, Jing L, Helbling AR, Sinclair SM, Allen KD, Shamji MF, Richardson WJ, Fitch RD, Setton LA, Chen J. Interleukin-17 synergizes with IFNgamma or TNFalpha to promote inflammatory mediator release and intercellular adhesion molecule-1 (ICAM-1) expression in human intervertebral disc cells. J Orthop Res. 2011;29:1–7. doi: 10.1002/jor.21206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Shamji MF, Setton LA, Jarvis W, So S, Chen J, Jing L, Bullock R, Isaacs RE, Brown C, Richardson WJ. Proinflammatory cytokine expression profile in degenerated and herniated human intervertebral disc tissues. Arthritis Rheum. 2010;62:1974–82. doi: 10.1002/art.27444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Aikawa E, Nahrendorf M, Figueiredo JL, Swirski FK, Shtatland T, Kohler RH, Jaffer FA, Aikawa M, Weissleder R. Osteogenesis associates with inflammation in early-stage atherosclerosis evaluated by molecular imaging in vivo. Circulation. 2007;116:2841–50. doi: 10.1161/CIRCULATIONAHA.107.732867. [DOI] [PubMed] [Google Scholar]
- [33].Feng G, Yang X, Shang H, Marks IW, Shen FH, Katz A, Arlet V, Laurencin CT, Li X. Multipotential differentiation of human anulus fibrosus cells: an in vitro study. J Bone Joint Surg Am. 2010;92:675–85. doi: 10.2106/JBJS.H.01672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Galbusera F, Mietsch A, Schmidt H, Wilke HJ, Neidlinger-Wilke C. Effect of intervertebral disc degeneration on disc cell viability: a numerical investigation. Comput Methods Biomech Biomed Engin. 2011 Oct 4; doi: 10.1080/10255842.2011.619184. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [35].Holm S, Maroudas A, Urban JP, Selstam G, Nachemson A. Nutrition of the intervertebral disc: solute transport and metabolism. Connect Tissue Res. 1981;8:101–19. doi: 10.3109/03008208109152130. [DOI] [PubMed] [Google Scholar]
- [36].Wang Y, Boyd SK, Battie MC, Yasui Y, Videman T. Is greater lumbar vertebral BMD associated with more disk degeneration? A study using microCT and discography. J Bone Miner Res. 2011;26:2785–91. doi: 10.1002/jbmr.476. [DOI] [PubMed] [Google Scholar]
- [37].Bibby SR, Jones DA, Lee RB, Yu J, Urban JPG. The pathophysiology of the intervertebral disc. Joint Bone Spine. 2001;68:537–42. doi: 10.1016/s1297-319x(01)00332-3. [DOI] [PubMed] [Google Scholar]
- [38].Cs-Szabo G, Ragasa-San Juan D, Turumella V, Masuda K, Thonar EJ, An HS. Changes in mRNA and protein levels of proteoglycans of the anulus fibrosus and nucleus pulposus during intervertebral disc degeneration. Spine (Phila Pa 1976) 2002;27:2212–9. doi: 10.1097/00007632-200210150-00006. [DOI] [PubMed] [Google Scholar]
- [39].Tallantyre EC, Bo L, Al-Rawashdeh O, Owens T, Polman CH, Lowe J, Evangelou N. Greater loss of axons in primary progressive multiple sclerosis plaques compared to secondary progressive disease. Brain. 2009;132:1190–9. doi: 10.1093/brain/awp106. [DOI] [PubMed] [Google Scholar]
- [40].Jeng AY, Chou M, Sawyer WK, Caplan SL, Von Linden-Reed J, Jeune M, Prescott MF. Enhanced expression of matrix metalloproteinase-3, -12, and -13 mRNAs in the aortas of apolipoprotein E- deficient mice with advanced atherosclerosis. Ann N Y Acad Sci. 1999;878:555–8. doi: 10.1111/j.1749-6632.1999.tb07725.x. [DOI] [PubMed] [Google Scholar]
- [41].Nakano D, Hayashi T, Tazawa N, Yamashita C, Inamoto S, Okuda N, Mori T, Sohmiya K, Kitaura Y, Okada Y, Matsumura Y. Chronic hypoxia accelerates the progression of atherosclerosis in apolipoprotein E-knockout mice. Hypertens Res. 2005;28:837–45. doi: 10.1291/hypres.28.837. [DOI] [PubMed] [Google Scholar]
- [42].Chen Y, Aratani Y, Osawa T, Fukuyama N, Tsuji C, Nakazawa H. Activation of inducible nitric oxide synthase increases MMP-2 and MMP-9 levels in ApoE-knockout mice. Tokai J Exp Clin Med. 2008;33:28–34. [PubMed] [Google Scholar]
- [43].Park JB, Lee JK, Park EY, Riew KD. Fas/FasL interaction of nucleus pulposus and cancer cells with the activation of caspases. Int Orthop. 2008;32:835–40. doi: 10.1007/s00264-007-0410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]