Abstract
Context
Sleep is a significant problem in breast cancer survivors (BCS) and measured frequently using the Pittsburgh Sleep Quality Index (PSQI). Thus, it is important to evaluate its factor structure. The two-process model of sleep regulation was the theoretical framework for this study.
Objectives
To perform a confirmatory factor analysis of the PSQI in BCS and compare results between African-American and Caucasian BCS.
Methods
This was a secondary analysis of cross-sectional data using local and regional health care facilities and Eastern Cooperative Oncology Group referrals. The study included 1174 non-depressed BCS (90% Caucasian), with a mean age of 57 years and median PSQI global scores at the cut-off for poor sleep (median = 6.00, interquartile range = 4.00–9.00). Measurements included self-reported demographics, medical history, depression, and sleep.
Results
Acceptable fit was not reached for the traditional one-factor model that would be consistent with current PSQI scoring or for alternative models in published literature from other populations. A new two-factor model (i.e., sleep efficiency and perceived sleep quality) best fit the data but nested-model comparisons by race showed different relationships by race for 1) sleep quality–sleep latency, and 2) sleep efficiency–sleep quality.
Conclusion
Results were inconsistent with current PSQI scoring that assumes a single global factor and with previously published literature. Although a new two-factor model best fit the data, further quantitative and qualitative analyses are warranted to validate our results in other populations before revising PSQI scoring recommendations. Additional recommendations for research are described.
Keywords: Sleep, breast cancer survivor, measurement of sleep, factor analysis
Introduction
Current evidence suggests that 48%–65% of breast cancer survivors (BCS) report poor sleep,1,2 a higher incidence in BCS compared with age-matched mid-life women.1,3,4 Significant correlates of sleep disturbances in BCS include estrogen depletion, poor physical functioning, depression, and/or distress.1 Additionally, racial disparities exist, with African-American BCS being three times more likely to report poor sleep.1 Sleep disturbances are important to address because, if left untreated, they can negatively affect quality of life.
Most evidence about sleep in BCS has been based on the Pittsburgh Sleep Quality Index (PSQI) questionnaire that captures both clinical and behavioral information about sleep through a single global score,5,6 which is typically the outcome variable reported. The PSQI is widely accepted because of its established psychometrics in BCS and other populations.6
It remains unclear if the PSQI captures all attributes of sleep. Within the past five years, several studies have shown that multifactor models for the PSQI might be more accurate.7–9 Cole et al. conducted exploratory and confirmatory factor analysis of the PSQI in a sample of depressed and non-depressed men (45%) and women (55%) ages 60 years or older.9 Their exploratory factor analysis (EFA) showed that a two-factor model (i.e., sleep efficiency and perceived sleep quality) best fit the data. In contrast, their confirmatory factor analysis (CFA) found that a three-factor model of sleep efficiency, perceived sleep quality, and daily disturbances best fit the data.9 The authors recommended the use of a three-factor structure to better reflect sleep disturbances. This three-factor structure was supported in two additional studies; one used principal components analysis of data from 520 Nigerian university students7 and the other was done in 135 post-renal transplant patients.8 These studies were based on relatively small samples (n=135 and 520) that included both men and women, with a wide range of ages.
Evaluating the factor structure of the PSQI has important implications for its use in descriptive and intervention research. If the global score is not the most accurate depiction of sleep, scoring for the questionnaire might need to be revised to capture essential attributes of sleep and treatment efficacy.7–9
The current scoring of the PSQI produces a single summed score that does not reflect the multiple dimensions of poor sleep as suggested by the two-process model of sleep regulation.10 This model postulates that there are multiple physiological processes that drive sleep and wakefulness; if one process is disrupted, sleep and/or wakefulness are affected. Because sleep is a significant problem in BCS and frequently measured using the PSQI, it is important to evaluate its factor structure to determine which of the commonly used or previously reported factor structures (one-, two-, or three-factor model) is most relevant for this population and in line with the theoretical framework.
The previously reported one-, two-, and three-factor models are the driving construct and basis for this study. In addition, because sleep in BCS varies by race,1 it is important to know if the factor structure is different between African-American BCS and Caucasian BCS. This information would maximize knowledge of sleep disturbances in both Caucasian and African-American BCS. Therefore, the purpose of this study was to 1) perform a CFA of the PSQI in a large sample of BCS, and 2) compare the factor structure between African-American and Caucasian BCS. The corresponding research questions were 1) will the CFA of the PSQI in a large sample of BCS support the use of a one-, two-, or three-factor model, and 2) is the resulting factor structure consistent between the African-American and Caucasian BCS? The hypothesis was that the factor structure will differ from previous research, which did not include women with cancer. It also was hypothesized that the factor structure should be similar between African-American and Caucasian BCS.
Methods
Procedures
PSQI responses from two separate cross-sectional, descriptive, comparative, parent studies were evaluated. Data were collected at a single point in time for both studies. Subjects who completed the PSQI and other questionnaires were included in the analyses. The parent studies were reviewed and approved by the university institutional review board and the cancer center scientific review committee. Both studies used similar local recruitment strategies by trained research assistants. One of the two parent studies used regional referrals from the Eastern Cooperative Oncology Group (ECOG) and a southeastern university. Eligible and willing BCS who signed consents were given a questionnaire packet in person or through the mail. The eligibility criteria for each of the two studies were similar and included women who were at least 18 years of age; stage I-III at diagnosis; cancer-free at time of study enrollment; no history of other cancers; able to read, write, and speak English; and at least two years but no more than 10 years post-completion of surgery, radiation, and/or chemotherapy. A total of 1174 BCS was identified from the two studies (study 1, n=130; study 2, n=1044) for this analysis.
Measures
Demographic and other comparative variables were assessed. Variables that are thought to impact sleep were evaluated, such as age, body mass index (BMI), marital status, years of education, menopausal status, and hot flashes. Sample characteristics were collected using an adapted multi-item questionnaire11 that captured race, age, marital status, educational and income level, employment status, height, and weight. Information about breast cancer and treatment was obtained from abstracting medical records using a standardized form. Data included date and stage at diagnosis, types and dates of treatment (surgery, chemotherapy, radiation), and endocrine therapy. Frequency and severity of menopausal symptoms such as hot flash frequency were measured using a generic 14-item questionnaire.
Depressive symptoms were assessed using the Center for Epidemiologic Studies-Depression Scale (CES-D), a 20-item self-report instrument assessing the presence and severity of depressive symptoms occurring over the past week. 12 Scores of 16 or greater are indicative of high depressive symptoms, but are not considered a diagnosis of clinical depression.13,14 This cut-off point of 16 has been used extensively in other studies, including studies of BCS.6 Internal consistency reliability has been shown to be adequate in cancer and non-cancer populations, with Cronbach’s alpha coefficients of >0.85. 15
Sleep disturbances were assessed using the PSQI,5 a 19-item scale producing a global sleep quality index score based on seven component scores: sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medications, and daytime dysfunction. Global scores range from 0–21 and scores above 5 reflect poor global sleep quality.5 Psychometrics of the PSQI have been supported in a variety of populations,16,17 including non-cancer populations (n=52; α=0. 83)5 and BCS (n=102; α=0. 80).6 Construct validity also has been demonstrated.6
Statistical Analysis
Frequency and descriptive statistics were used to analyze demographic variables using the Statistical Package for the Social Sciences (SPSS) (v. 17.0, SPSS, Inc., Chicago, IL). Chi-square and t-tests were used to examine potential differences between African-American and Caucasian BCS on the following variables: age, marital status, years of education, cancer treatment received (e.g., chemotherapy), use of hormone modulators, number of hot flashes in the past month, sleep disturbance (PSQI global score), and depressive symptoms (CESD).
Responses to the PSQI were scored into seven components5 and 95.7% of the sample had complete data on all composite scores. The greatest missingness was for habitual sleep efficiency, with 3.52% of the sample missing data on this item. Because of the small proportion of missing data, PRELIS 2.818 (Scientific Software International, Inc., Chicago, IL) was used to impute missing values by matching with other variables on the scale.19 Listwise deletion was used to eliminate cases for which missing values could not be imputed, resulting in a final sample size of 1172.
A CFA using LISREL 8.818 (Scientific Software International, Inc., Chicago, IL) was conducted. Because the single global score of the PSQI is frequently used in the literature, we examined the fit of a one-factor model. Also, because the recent Cole et al. 9 study found support for both a two-factor model (in their EFA) and a three-factor model (in their CFA) of the PSQI, we decided to examine the fit of both these models in the present sample. Given that parsimonious models are preferred to more complex ones, we examined these models in order of increasing complexity.
The data from the PSQI are ordinal rather than continuous and should not be analyzed using methods that assume they have metric properties.19 Therefore, PRELIS 2.818 was used to estimate the polychoric correlations among the indicators and their asymptotic covariance matrix.19 This matrix was then used to estimate factor models using weighted least squares.
Several indices to evaluate model fit were used: 1) Chi-square corrected for non-normality (non-normal χ2); 2) standardized root mean squared residual (SRMR); 3) root mean square error of approximation (RMSEA); and 4) comparative fit index (CFI). The non-normal χ2 and the SRMR are indices of absolute fit. A non-significant χ2 is evidence of acceptable fit. Smaller values of SRMR indicate better model fit, with values ≤ 0.08 indicating acceptable fit.20 The RMSEA is a commonly used parsimonious index, with values ≤ 0.06 indicating acceptable fit.20 The CFI is an incremental fit index, with values ≥ 0.95 indicating acceptable fit.20 Models are identified according to the authors of origin to provide clarification.
Results
Sample Characteristics
The majority of BCS were non-Hispanic (98%), Caucasian (90%), partnered (73%), well-educated (39% some college), and post-menopausal (85%). Most had had some type of cancer surgery (99%), chemotherapy (96%), radiotherapy (93%), hot flashes in the past month (52%), and 35% were taking hormone modulators. Mean (standard deviation [SD]) age was 57 (11.42) years (range 28–79 years) and mean (SD) BMI was 28.32 (6.08). BCS were not depressed (CESD scores mean [SD] 9.74 [8.92]), but the median PSQI global score was at the cut-off for poor sleep (median 6.00; interquartile range [IQR] 9.00-4.00; mean [SD] 6.46 [3.75]). African-American BCS had significantly higher BMI (mean 31.42 vs. 27.97), were significantly more depressed (mean 14.42 vs. 9.18), reported significantly poorer sleep (mean 8.25 vs. 6.26; medians 8.00 vs. 6.00; IQRs 12.00-5.00 vs. 9.00-3.00), and were not partnered (34% vs. 77%) compared with Caucasian BCS. The correlation matrix and descriptive statistics for the PSQI indicators are shown in Table 1.
Table 1.
Correlation Matrix and Descriptive Statistics of PSQI Indicators
| Correlations | |||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| 1. Subjective Sleep Quality | ---- | 0.50 | 0.39 | 0.44 | 0.45 | 0.29 | 0.39 |
| 2. Sleep Latency | ---- | 0.25 | 0.45 | 0.36 | 0.34 | 0.21 | |
| 3. Sleep Duration | ---- | 0.51 | 0.21 | 0.07 | 0.20 | ||
| 4. Habitual Sleep Efficiency | ---- | 0.29 | 0.26 | 0.25 | |||
| 5. Sleep Disturbances | ---- | 0.20 | 0.32 | ||||
| 6. Sleep Medication Use | ---- | 0.18 | |||||
| 7. Daytime Dysfunction | ---- | ||||||
| Mean | 0.97 | 1.14 | 0.87 | 0.62 | 1.38 | 0.75 | 0.84 |
| Standard Deviation | 0.75 | 1.02 | 0.77 | 0.94 | 0.58 | 1.16 | 0.74 |
| Median | 1.00 | 1.00 | 1.00 | 0.00 | 1.00 | 0.00 | 1.00 |
| Interquartile Range (75%ile – 25%ile) | 1.00 | 2.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
Note: All correlations are significant at P < 0.05. Data were based on final imputed data set. N = 1172.
Confirmatory Factor Analysis
First, the one-factor model fit was tested (global score). This single-factor model did not show acceptable fit, non-normal χ2 (df = 14) = 199.88, P < 0.05, SRMR = 0.071, RMSEA = 0.105, CFI = 0.96. Second, a two-factor model was tested consistent with the EFA results of Cole et al.9 This model did not show acceptable fit to the data, non-normal χ2 (df = 13) = 89.70, P < 0.05, SRMR = 0.0048, RMSEA = 0.075, CFI = 0.98. Third, we tested the fit of the Cole et al. three-factor model consisting of sleep efficiency, perceived sleep quality, and daily disturbances. This model did not show acceptable fit, non-normal χ2 (df = 11) = 80.32, p < 0.05, SRMR = 0.0044, RMSEA = 0.076, CFI = 0.98.
Next, modification indices were examined to determine how acceptable model fit might be reached. Based on the modification indices, the error terms were correlated among the following pairs of indicators: 1) sleep duration-subjective sleep quality; 2) sleep duration-sleep medication use; 3) sleep latency-habitual sleep efficiency; 4) sleep latency-sleep medication use; and 5) sleep latency-daytime dysfunction. The resulting Otte et al. three-factor model (sleep efficiency, perceived sleep quality, and daily disturbances) showed acceptable fit to the data, non-normal χ2 (df = 6) = 3.34, P = 0.76, SRMR = 0.012, RMSEA = 0.000, CFI = 1.00.
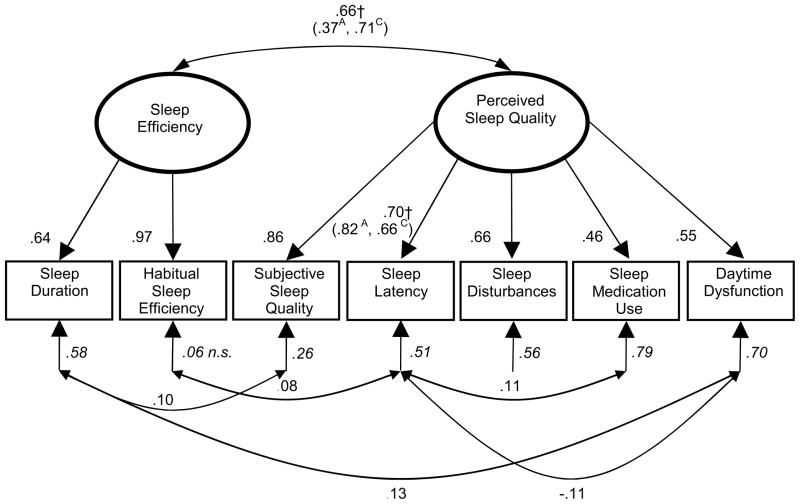
There was a high correlation between daily disturbances and perceived sleep quality (r = 0.93). Hence, we conducted a nested-model comparison with this correlation fixed to 1.0 to see if a new Otte et al. two-factor solution fit the data as well as the Otte et al. three-factor model. This nested-model comparison showed no significant decrement in model fit, Δχ2 (df = 1) = 1.13, P = 0.29. Therefore, we examined the overall fit of the new Otte et al. two-factor model with the correlated error terms. This model showed acceptable fit, non-normal χ2 (df = 8) = 8.85, P = 0.36, SRMR = 0.019, RMSEA = 0.016, CFI = 1.00. Hence, the Otte et al. two-factor model (sleep efficiency and perceived sleep quality) best fit the data among BCS (Fig. 1). A one-factor model with the correlated error terms did not show acceptable fit to the data, χ2 (df = 10) = 127.72, P < 0.001, SRMR = 0.058, RMSEA = 0.110, CFI = 0.97.
Fig. 1.
Otte et al. two-factor model of PSQI sleep quality in BCS.
All coefficients are standardized and significant at P < 0.05, unless otherwise noted. Ovals = latent variables. Rectangles = measured variables. Single-headed arrows = factor loadings. Double-headed arrows = correlations; Italicized coefficients are error terms, representing the proportion of variation in the variable not accounted for by the model; † = parameters were found to differ significantly between African-American and Caucasian subsamples. A = parameter estimate for African-American subsample; C = parameter estimate for Caucasian subsample.
To test whether the same factor structure was constant between African-American and Caucasian subsamples, several two-group comparisons were conducted. First, all parameters were constrained to be equal across both groups. This model showed mixed evidence for fit, non-normal χ2 (df = 37) = 68.03, P = 0.003, SRMR = 0.027, RMSEA = 0.039, CFI = 0.99. Next, the factor loadings were freed, and the model showed significantly improved fit, Δ non-normal χ2 (df = 7) = 14.42, P = 0.04, indicating that the factor loadings differed between African-American and Caucasian BCS.
A series of nested-model comparisons was conducted freeing individual factor loadings to determine which ones significantly differed between African-American and Caucasian BCS (Table 2). The factor loading of perceived sleep quality onto sleep latency differed significantly, with a factor loading of 0.82 among African-American BCS and 0.66 for Caucasian BCS (Fig. 1) indicating that the time required to fall asleep is a stronger indicator of perceived sleep quality among African-American BCS compared with Caucasian BCS.
Table 2.
Chi-Square Difference Tests Comparing Factor Loadings on PSQI Indicators in African-American versus Caucasian Breast Cancer Survivors
| Factor | Indicator | λA | λC | Δχ2 | df | P |
|---|---|---|---|---|---|---|
| Sleep Efficiency | ||||||
| Sleep Duration | 0.57 | 0.62 | 0.09 | 1 | 0.764 | |
| Habitual Sleep Efficiency | 0.99 | 0.96 | 0.68 | 1 | 0.410 | |
|
| ||||||
| Perceived Sleep Quality | ||||||
| Subjective Sleep Quality | 0.83 | 0.87 | 0.01 | 1 | 0.920 | |
| Sleep Latency | 0.82 | 0.66 | 7.00 | 1 | 0.008 | |
| Sleep Disturbances | 0.73 | 0.63 | 0.43 | 1 | 0.512 | |
| Sleep Medication Use | 0.53 | 0.46 | 1.76 | 1 | 0.185 | |
| Daytime Dysfunction | 0.66 | 0.53 | 2.32 | 1 | 0.128 | |
Note: λA = factor loading in African-American subsample; λC = factor loading in Caucasian subsample.
Next, the correlation between sleep efficiency and sleep quality was freed to vary between groups, and the model showed significantly improved fit, Δ non-normal χ2 (df = 1) = 6.64, P = 0.0099, indicating that the relationship between sleep efficiency and sleep quality differed between African-American and Caucasian BCS. The relationship between sleep efficiency and perceived sleep quality was more modest among African-American BCS (r = 0.37) than among Caucasian BCS (r = 0.71) (Fig. 1).
Finally, the correlations among residuals were freed to vary across the two groups. This did not result in improved model fit, Δ non-normal χ2 (df = 5) = 9.91, P = 0.078. Hence, the correlated residuals were held invariant across groups. The final Otte et al. two-group model with the factor loading from perceived sleep quality to sleep latency freed and the correlation between sleep efficiency and perceived sleep quality freed showed good fit to the data, non-normal χ2 (df = 35) = 51.25, P = 0.037, SRMR = 0.028, RMSEA = 0.026, CFI = 1.00.
Discussion
Three important findings emerged. First, the study supports previous results that the PSQI single global score derived by the seven components may not be consistent with the factor structure of this questionnaire. This finding is supported by the theoretical framework since sleep is not a unidimensional problem. The single-factor model from this study produced an average standardized loading of 0.56 for each the component scores, which was lower when compared to previous studies.8,9
Second, Cole et al.’s three-factor model fit the data of BCS better than a single-factor model, but the correlation between the latent variables of perceived sleep quality and daily disturbances was 0.93, which is higher compared with two previous studies (r=0.75–0.81).8,9 Because a correlation this strong between two variables suggests a single factor, the Otte et al. two-factor model of sleep efficiency and perceived sleep quality fit the data as well as the Otte et al. three-factor model. These findings suggest that, before altering PSQI scoring, further exploration of the factor structure is needed to determine if the factor structure varies by the gender, race, or other characteristics of various populations.
Third, the overall factor models were consistent between African-American and Caucasian BCS with two important differences. First, there was a weaker relationship between the latent variables of sleep efficiency and perceived sleep quality in African-American BCS. Second, sleep latency was a stronger indicator of perceived sleep quality among African-American BCS than among Caucasian BCS. It has been noted in previous studies that African-American BCS perceive aspects of survivorship and quality of life differently than Caucasian BCS.21 This difference in perception has been reflected in how African-American BCS respond to questionnaire items. African-American BCS could be answering PSQI items based on a different understanding of the meaning of “time in bed” or “time to fall asleep.” For example, African-American BCS might spend time in bed relaxing before falling asleep. This might result in calculations of sleep efficiency and sleep latency that do not match perceptions of sleep quality among Caucasian BCS. It is also important to note that African-American BCS reported more depressive symptoms in this study, which could have influenced question responses.
In science, parsimony is desirable; the Otte et al. two-factor model was used for the second part of the study comparing the factor structure of African-American BCS and Caucasian BCS. The sample size of African-American BCS was smaller than Caucasian BCS. However, because African-American BCS are at higher risk than Caucasian BCS for sleep problems and there were similar numbers of African-American BCS subjects compared with previous studies, the benefit of this information would outweigh the limitation of the smaller African-American BCS sample size and we proceeded with caution in testing racial differences in the factor structure.
Limitations of the study include: 1) this was a cross-sectional study; 2) BCS might differ from newly diagnosed, in treatment, or completing treatment BCS; 3) this was a heterogeneous sample of BCS; and 4) results could be related to being female or having a history of breast cancer, limiting generalization of findings to males or other cancer survivors.
In sum, this study provides new information about the factor structure of the PSQI in BCS with results that do not match previously published results and do not reflect the multidimensionality of sleep problems as suggested in the two-process model of sleep regulation. Further quantitative and qualitative analyses are needed of individual sleep items within the questionnaire to examine the existing factor structure of the PSQI. Alternative scoring would include revisiting the content of each item and match with the specific construct of sleep problems, revise the scoring to reduce the complexity and subscales produced, and perform additional reliability and validity to ensure the overall measure is reflective of poor sleep.
Acknowledgments
The authors would like to thank Dr. Phyllis Dexter for her editorial support.
Footnotes
Disclosures
Funding was provided by the American Cancer Society grant #RSGPB-04-089-01-PBP (Champion), NIH/NCI #R03CA97737 (Russell), and the Walther Cancer Institute Foundation (Russell). One of the parent studies (Champion) was conducted by the Eastern Cooperative Oncology Group (Robert L. Comis, MD) and supported in part by Public Health Service Grants CA21115, CA37604 and funding from the National Cancer Institute Division of Cancer Prevention, National Institutes of Health and the Department of Health and Human Services. Study contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute. The authors have no disclosures to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Otte JL, Carpenter JS, Russell KM, Bigatti S, Champion VL. Prevalence, severity, and correlates of sleep-wake disturbances in long-term breast cancer survivors. J Pain Symptom Manage. 2010;39(3):535–547. doi: 10.1016/j.jpainsymman.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carpenter JS, Andrykowski MA. Menopausal symptoms in breast cancer survivors. Oncol Nurs Forum. 1999;26(8):1311–1317. [PubMed] [Google Scholar]
- 3.Owens JF, Matthews KA. Sleep disturbance in healthy middle-aged women. Maturitas. 1998;30(1):41–50. doi: 10.1016/s0378-5122(98)00039-5. [DOI] [PubMed] [Google Scholar]
- 4.Owen DC, Parker KP, McGuire DB. Comparison of subjective sleep quality in patients with cancer and healthy subjects. Oncol Nurs Forum. 1999;26(10):1649–1651. [PubMed] [Google Scholar]
- 5.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 6.Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45(1):5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- 7.Aloba OO, Adewuya AO, Ola BA, Mapayi BM. Validity of the Pittsburgh Sleep Quality Index (PSQI) among Nigerian university students. Sleep Med. 2007;8(3):266–270. doi: 10.1016/j.sleep.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Burkhalter H, Sereika SM, Engberg S, et al. Structure validity of the Pittsburgh Sleep Quality Index in renal transplant recipients: a confirmatory factor analysis. Sleep and Biological Rhythms 2010. 2010;8(4):274–281. [Google Scholar]
- 9.Cole JC, Motivala SJ, Buysse DJ, et al. Validation of a 3-factor scoring model for the Pittsburgh sleep quality index in older adults. Sleep. 2006;29(1):112–116. doi: 10.1093/sleep/29.1.112. [DOI] [PubMed] [Google Scholar]
- 10.Borbely AA. A two process model of sleep regulation. Hum Neurobiol. 1982;1(3):195–204. [PubMed] [Google Scholar]
- 11.Giesler RB, Given B, Given CW, et al. Improving the quality of life of patients with prostate carcinoma: a randomized trial testing the efficacy of a nurse-driven intervention. Cancer. 2005;104(4):752–762. doi: 10.1002/cncr.21231. [DOI] [PubMed] [Google Scholar]
- 12.Radloff LS. The CES-D Scale: a self-report depression scale for research in general population. Applied and Psychological Measures. 1977;1(1):385–401. [Google Scholar]
- 13.Comstock GW, Helsing KJ. Symptoms of depression in two communities. Psychol Med. 1976;6(4):551–563. doi: 10.1017/s0033291700018171. [DOI] [PubMed] [Google Scholar]
- 14.Berkman LF, Berkman CS, Kasl S, et al. Depressive symptoms in relation to physical health and functioning in the elderly. Am J Epidemiol. 1986;124(3):372–388. doi: 10.1093/oxfordjournals.aje.a114408. [DOI] [PubMed] [Google Scholar]
- 15.Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) J Psychosom Res. 1999;46(5):437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- 16.Tiffin P, Ashton H, Marsh R, Kamali F. Pharmacokinetic and pharmacodynamic responses to caffeine in poor and normal sleepers. Psychopharmacology (Berl) 1995;121(4):494–502. doi: 10.1007/BF02246500. [DOI] [PubMed] [Google Scholar]
- 17.Gentili A, Weiner DK, Kuchibhatla M, Edinger JD. Test-retest reliability of the Pittsburgh Sleep Quality Index in nursing home residents. J Am Geriatr Soc. 1995;43(11):1317–1318. doi: 10.1111/j.1532-5415.1995.tb07415.x. [DOI] [PubMed] [Google Scholar]
- 18.Joreskog KG, Sorbom D. LISREL (Version 8.8) [computer software] Chicago: Scientific Software International; 2006. [Google Scholar]
- 19.Joreskog K. Structural equation with ordinal variables using LISREL. Chicago: Scientific Software International; 2005. pp. 1–77. [Google Scholar]
- 20.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 21.Kooken WC, Haase JE, Russell KM. “I’ve been through something”: poetic explorations of African American women’s cancer survivorship. West J Nurs Res. 2007;29(7):896–919. doi: 10.1177/0193945907302968. discussion 920-899. [DOI] [PubMed] [Google Scholar]