Abstract
Background To date little has been published about epidemiology and public health capacity (training, research, funding, human resources) in WHO/AFRO to help guide future planning by various stakeholders.
Methods A bibliometric analysis was performed to identify published epidemiological research. Information about epidemiology and public health training, current research and challenges was collected from key informants using a standardized questionnaire.
Results From 1991 to 2010, epidemiology and public health research output in the WHO/AFRO region increased from 172 to 1086 peer-reviewed articles per annum [annual percentage change (APC) = 10.1%, P for trend < 0.001]. The most common topics were HIV/AIDS (11.3%), malaria (8.6%) and tuberculosis (7.1%). Similarly, numbers of first authors (APC = 7.3%, P for trend < 0.001), corresponding authors (APC = 8.4%, P for trend < 0.001) and last authors (APC = 8.5%, P for trend < 0.001) from Africa increased during the same period. However, an overwhelming majority of respondents (>90%) reported that this increase is only rarely linked to regional post-graduate training programmes in epidemiology. South Africa leads in publications (1978/8835, 22.4%), followed by Kenya (851/8835, 9.6%), Nigeria (758/8835, 8.6%), Tanzania (549/8835, 6.2%) and Uganda (428/8835, 4.8%) (P < 0.001, each vs South Africa). Independent predictors of relevant research productivity were ‘in-country numbers of epidemiology or public health programmes’ [incidence rate ratio (IRR) = 3.41; 95% confidence interval (CI) 1.90–6.11; P = 0.03] and ‘number of HIV/AIDS patients’ (IRR = 1.30; 95% CI 1.02–1.66; P < 0.001).
Conclusions Since 1991, there has been increasing epidemiological research productivity in WHO/AFRO that is associated with the number of epidemiology programmes and burden of HIV/AIDS cases. More capacity building and training initiatives in epidemiology are required to promote research and address the public health challenges facing the continent.
Keywords: Epidemiology, public health, training, Africa, capacity building, retention, research, WHO/AFRO
Introduction
Purpose and objectives
This is the first article commissioned for each of the six WHO regions by the International Epidemiological Association to provide an overview of epidemiology capacity—defined as training, research, funding and human resources—and to make recommendations to address current challenges. Information gathered will support strategic planning by the International Epidemiological Association, governments and non-government organizations involved in public health and epidemiological training and research.
Definition of WHO/AFRO
The WHO is the specialized United Nations agency for global health matters. Its presence in the sub-Saharan region of Africa consists of the WHO Regional Office for Africa (WHO/AFRO), a Secretariat for the African region, three inter-country support teams and WHO Country and Liaison Offices located in each of the 46 member states of WHO/AFRO. Eight other African countries (Morocco, Libya, Egypt, Tunisia, Sudan, South Sudan, Djibouti, Eritrea and Somalia) are included the WHO’s Eastern Mediterranean Regional Office. This article considers only countries in WHO/AFRO.
Epidemiology vs public health research and training
‘Epidemiology’ as used in this manuscript is defined as the study of the occurrence and distribution of health-related states or events in specified populations, including the study of the determinants influencing such states, and the application of this knowledge to control health problems.1 In high-income countries, the emphasis of epidemiological research is often on finding and elucidating causal relationships. In Africa, however, the application of epidemiology ‘to control health problems’ appears to be of primary interest. In this sense, ‘epidemiological research’ is often used synonymously with ‘public health research’. This use is somewhat misleading, however, because public health research as a branch of investigation generally uses a wider range of approaches than traditional epidemiological research alone. Epidemiology in African settings often still focuses on communicable disease conditions, but this focus will widen alongside the growing interest in non-communicable diseases. However, whether epidemiological research will ever include, complement or overlap with social science research remains to be seen. These fields are currently very separate—taught and practised in separate compartments of science and health—but a re-focusing on chronic disease, coupled with a renewed interest in the social determinants of health, may well cause a convergence of epidemiology, public health research and social science research methods to describe health-related states and health impact. Although others have reviewed medical education2 and biostatistics resources and research strengthening in sub-Saharan Africa,3 to our knowledge, no review focusing on epidemiological training and research output in WHO/AFRO has been published previously.
Burden of disease and risk factors in WHO/AFRO
Eleven million deaths, including 5.78 million in males (∼52%), were estimated to occur in Africa in 2007, representing about one-sixth of the world’s deaths that year. Forty-one percent of deaths in Africa in 2007 occurred in children aged 0–4 years, mainly associated with infectious diseases including diarrhoeal diseases, malaria and lower respiratory infections, as well as adverse perinatal conditions. The high rate of childhood deaths largely explains the low median life expectancy of 54 years in this region, considerably lower than that in other regions.4
Communicable diseases, mainly HIV/AIDS, tuberculosis (TB) and malaria, continue to be associated with the highest proportion of documented deaths in Africa through ages 0–5 years, peaking again in adults aged 30–44 years. Of all deaths due to communicable diseases in the AFRO region, 68% are associated with HIV/AIDS.5 Mortality associated with HIV/AIDS at any age was 14.7% in the AFRO region, compared with 3.5% globally. Global HIV incidence fell by >25% between 2001 and 2009 in 33 countries surveyed, 22 of which are in sub-Saharan Africa.6 During the past 2 decades, the number of new TB cases has tripled in high HIV prevalence countries. In 2008, there were an estimated 1.4 million HIV-positive TB patients globally, roughly 80% of whom lived in the AFRO region.7 The global number of malaria cases increased from 223 million in 2000 to 244 million in 2005, but decreased to 225 million in 2009. Although decreased malaria burden has been documented in other WHO regions, the largest absolute decrease in malaria deaths occurred in the AFRO region.8
The region also has a rapidly increasing burden of non-communicable conditions including high blood pressure, diabetes and cancer in certain countries, which leads to widening health gaps between and within countries.3 Southern countries share a relatively higher burden of both HIV/AIDS and non-communicable diseases.9–14 Recent estimates for South Africa are concerning: WHO estimates its burden from non-communicable diseases to be two to three times higher than of developed countries.15 Non-communicable diseases appear to be increasing in rural parts of South Africa and are driving increased demand for chronic medical care.16,17 Also in South Africa, violence and trauma contribute to total disease burden, especially among the poor,15 but the distribution and pattern of morbidity and mortality are shaped by the major intermediate risk factor of malnutrition, which also causes marked height disparities between higher and lower socio-economic groups. Other determinants of disease burden include a lack of food security, poor access to safe sanitation, prevalence of indoor pollutants and high unemployment.18
Although HIV prevalence is high in the WHO/AFRO on average, it ranges from single digits in west, central and east Africa to double digits in southern Africa. This heterogeneity has been the subject of numerous studies. Among its causes are variability among these countries with regard to behavioural and socio-cultural factors, high population mobility, inequalities of wealth, gender inequality, intergenerational sex, gender and sexual violence, stigma, multiple concurrent partnerships and levels of male circumcision.19,20 Unsafe sex, defined as sex with an infected person without any measures to prevent HIV infection, accounts for 13.5% of disability-adjusted life-years lost in Africa, compared with <3% in any other region in the world.3
Although communicable diseases together with perinatal and maternal conditions are still a grave threat and non-communicable diseases and non-intentional injuries growing threats, much about contemporary morbidity and mortality in African countries is unclear owing to lack of consistent, reliable and updated data. Essential health information in the region is often based on ‘studies’ and ‘surveys’ that may have local and regional biases rather than using well-functioning national registries.21,22
Materials and methods
Key informants
Information about epidemiology training models, current research and challenges was collected from a convenience sample of 10 key informant expert epidemiologists attending the Africa Regional Meeting at the 2011 International Epidemiological Association Conference, August 7–9, 2011, Edinburgh, UK, using a standardized questionnaire that was also sent to and completed by 11 of the 14 authors of this manuscript.
Bibliometric analysis
We also conducted a bibliometric analysis using the online version of the Science Citation Index Expanded (SCI-Expanded), the Social Science Citation Index (SSCI) and the Thomson Reuters Web of Science. All original articles and papers from conference proceedings published from 1991 through 2010 that include the keywords epidemiology, epidemiological, epidemiologic, epidemiologist, epidemiologists, epidemiology, ‘public health’, ‘public healthcare’ and ‘public healthy’ in the title, abstract, author keywords or Keywords Plus and had at least one author whose address was in a WHO/AFRO country were selected. Records were downloaded into Microsoft Excel 2007, and additional coding was done manually to obtain frequency distributions and proportions. All words in the article title and keywords reported by authors and assigned by Web of Science were identified and divided into 5-year intervals (1991–95, 1996–2000, 2001–05 and 2006–10), after which they were ranked and frequencies calculated. Type of research collaboration depended on author addresses. ‘Single country article’ was assigned if researchers’ addresses were all from the same country. ‘Internationally collaborative article’ applies to articles co-authored by researchers from more than one country or territory.23 The impact factor of a journal was determined for each document as reported in the Journal Citation Reports 2010.
Statistical analyses
To allow weighted comparisons, the ratios of the number of publications from countries to their population, gross domestic product and health expenditure were calculated. Pearson’s correlation analysis was used to examine the association between national population, gross domestic product, health expenditure and research productivity. Poisson regression models were used to estimate the time trends in the number of indexed articles. Results of trend analyses are reported as average annual percentage change (APC). To estimate the APC, the following regression model was used:
where log (puby) is the natural log of publication in year y, b0 is the intercept and b1 is trend.24 The APC was first computed for all WHO/AFRO countries together and then by region (central, east, north, west and southern Africa). Univariate and multivariate negative binomial regression models were used to explore factors associated with variation in research productivity. Negative binomial regression, using a robust method, has been shown to address the failure of the Poisson regression model in the presence of statistical over dispersion by adding a parameter that reflects unobserved heterogeneity among observations (i.e. greater variability in the number of indexed articles than might be expected).25,26 Univariate (unadjusted) negative binomial regression analyses were used to investigate the bivariate relationship between each country-level factor (listed earlier in the text) and total research productivity. Multivariate (adjusted) negative binomial regression analyses were carried out to determine which country-level factors were independently associated with total research productivity. Only factors associated with the research productivity at the univariate level were included in the multivariate model. Results were presented as incidence rate ratio (IRR) with 95% confidence intervals (CIs) and percentage change. Exponents of coefficients negative binomial regression models were equal to the IRR. For correlation analysis and negative binomial regression, country-level indicators were log transformed to linearize these associations. Data were processed and analysed with Stata 11 software (Stata Corp., College Station, TX, USA).
Epidemiology and public health training
Academic institutions/graduate-level training in epidemiology or public health
Sub-Saharan Africa faces considerable public health challenges that require a well-trained and robust workforce. During the past decade, epidemiological training in Africa has grown, but much more is needed. In 2007, AfriHealth estimated that roughly 50 academic institutions in the AFRO region were providing graduate-level training in public health.27 Supplementary Table S1 (available as Supplementary data at IJE online) lists the main academic public health and/or epidemiology training programmes offered through African universities. Of note, doctoral programmes or other higher-level training in epidemiology are scarce.
South Africa and Nigeria have the most academic institutions offering post-graduate training in public health and/or epidemiology. The University of Cape Town has offered Masters-level training in epidemiological methods since the mid-1990s, and today runs a Master of Public Health (MPH) programme, which offers specializations in epidemiology and biostatistics or clinical epidemiology. The University of Zimbabwe is one of the oldest public health educational programmes in the AFRO region, having started a Master of Public Health (MPH) training in the early 1990s. Although enrolment criteria initially favoured doctors already working in public health or aspiring to do so, they now include other health professionals. The programme aimed at and succeeded in providing epidemiologically competent public health specialists. Since 2010, the MPH programme has been complemented by a Master of Sciences (MSc) in Clinical Epidemiology offered by the University of Zimbabwe College of Health Sciences.28
The University of the Western Cape in South Africa and the Makerere University School of Public Health in Uganda reported that by 2007, >600 graduates had earned certificates or diplomas in public health through their distance learning options.29 A recent resource to strengthen academic public health training through universities is the ‘Higher Education Alliance for Leadership Through Health’.30 This alliance of East African Schools of Public Health (Makerere University School of Public Health, Uganda; Muhimbili University of Health and Allied Sciences, Tanzania; National University Rwanda School of Public Health; Jimma University, Ethiopia; and University of Nairobi College Community Health and Moi University School of Public Health, both in Kenya).
Another resource for public health training is the One Health Central and Eastern Africa (OHCEA)32 consortium. OHCEA is a network of 14 Schools of Public Health and Veterinary Medicine in six central and eastern African countries (Uganda, Tanzania, Ethiopia, Rwanda, Kenya and Democratic Republic of Congo). One Health Central and Eastern Africa is supported by the US Agency for International Development (USAID). Its mission is to drive transformational change for continuous improvement of health and well-being of humans, animals and ecosystems. In addition, the East African Public Health Association holds annual conferences in collaboration with the Tanzania Public Health Association. From 1985–95, the Epidemiological Society of Southern Africa existed in South Africa, but this has been integrated into the Public Health Association of South Africa, which holds annual meetings with public health and epidemiological research features on the agenda and capacity-building sessions on particular issues in public health research methods. At the continental level, it is also worth mentioning the Association of Schools of Public Health in Africa, which was established in 2010 to foster the practice of public health in Africa, including advocacy for public health policy, research, training and technical collaboration, such as development of curricula and modules.33
Epidemiological modelling training has been provided since 2006 by the South African Centre for Epidemiological Modeling and Analysis (SACEMA)34 based at Stellenbosch University. This centre is conducting a variety of major research projects concentrated on TB and HIV and has greatly contributed to the understanding of transmission, surveillance and control for both diseases. Additionally, SACEMA is the leading institute on computational epidemiological modelling in Africa and hosts multiple training courses. SACEMA also provides scholarships for African nationals to train in multi-disciplinary research at the centre, helping to build capacity for modelling activities in Africa.
Field epidemiology training
Field epidemiology training is offered through various cooperative efforts. One major contributor is the African Field Epidemiology Network (AFENET),35 with funding from the Division of Global Public Health Capacity Development of the US Centers for Disease Control and Prevention (CDC), USAID, WHO/AFRO and WHO Lyon, the Task Force for Child Survival and Development, the Emory University School of Medicine, the Merck Foundation and Health Systems 20/20, a USAID-funded project.36 AFENET is a non-profit organization and networking alliance dedicated to helping Ministries of Health in Africa build strong, effective, sustainable programmes and capacity to improve public health systems on the African continent. AFENET is based in Uganda and currently operates in 11 member countries (Ethiopia, Kenya, Tanzania, South Africa, Zimbabwe, Niger, Nigeria, Ghana, Mali, Burkina Faso, Togo). South Sudan is an associate member, and several other AFRO countries (Democratic Republic of Congo, Central Africa Republic, Cameroon, Mozambique) are likely future members. AFENET offers two residency-based programmes in applied epidemiology: Field Epidemiology Training Programs and Field Epidemiology and Laboratory Training Programs. The programmes’ combination of classroom-based instruction, mentored practical work and laboratory practice (in Field Epidemiology and Laboratory Training Programs) provides hands-on multi-disciplinary training in public health surveillance, outbreak investigation, laboratory management, programme evaluation and other aspects of epidemiology research and methods.
The International Clinical Epidemiology Network (INCLEN), initially created by the Rockefeller Foundation and now an independent organization whose coordinating office is in New Delhi (India), is an association of 82 clinical epidemiology institutes around the world, nine of which are in Africa. INCLEN-Africa is the network of clinical epidemiology units based in Uganda, Ethiopia, Zimbabwe, South Africa, Kenya, Tanzania, Ghana, Nigeria and Zambia. Each clinical epidemiology unit consists of a number of social scientists, biostatisticians and clinicians from different disciplines based in a leading teaching medical institution and who have been trained at the Masters degree or Doctor of Philosophy (PhD) level in Clinical Epidemiology. The mission of INCLEN-Africa is to improve quality and equity of health services for the people of Africa by promoting quality research, practice of evidence-based health care, research capacity building and creation of strategic partnerships.37
The International Epidemiologic Database to Evaluate AIDS (IeDEA) is a network of regional consortia at 11 regional sites around the world funded by the US National Institutes of Health. The East African region is the major IeDEA site in the WHO/AFRO region and includes Kenya, Uganda and Tanzania. The database in East Africa follows ∼120 000 HIV-infected adults and children. In addition to data analysis, IeDEA augments capacity building by providing field training in Epidemiology, Biostatistics and Data Management.38 For example, the Southern African region includes sites across South Africa, Zambia, Malawi and Botswana, and features a Data Management Centre at the University of Cape Town that links post-graduate training (including MPH and PhD students) to research opportunities in epidemiology.
The International Network for the Demographic Evaluation of Populations and their Health (INDEPTH) is a network of 42 health and demographic surveillance system sites based in low-income countries in Africa and Asia, with headquarters in Accra, Ghana.39 INDEPTH was set up by its members to increase their research productivity, amount, quality and impact by sharing experience and skills and mounting multi-site field research projects. To do this, INDEPTH and its members collect and analyse high-quality health and demographic surveillance data and make standardized data series and data sets available to the wider scientific community. The INDEPTH Network aims to build scientific leadership in member sites through Masters programmes of the University of the Witwatersrand in Johannesburg, South Africa, and is now considering adding PhD programmes. As of 2011, there were 35 MSc in population-based field epidemiology students from low- and middle-income countries enrolled and 14 who already graduated.39
Training in epidemiology and public health offered by institutions outside Africa, including online training
Numerous universities with Schools of Public Health in high-income countries (North America, Europe Union, UK, Australia, etc.) offer short-, medium- (Masters), or long-term (PhD) training in Epidemiology to students from the WHO/AFRO region. Funding to access such training programmes has been provided during the past decades by the French Agence Nationale de la Recherche Scientifique,40 the Fogarty International Center (FIC) of the US National Institutes of Health and from research training programmes such as AIDS Training and Research Program (AITRP),3,41 the UK-based Wellcome Trust and the European Developing Countries Clinical Trial Partnership42 to cite just few. To date, the National Institutes of Health (NIH)/FIC-funded AITRP programme has invested in African investigators who have been trained in the USA and returned home to make significant contributions to groundbreaking studies on microbicides to prevent HIV in South Africa,43 male circumcision in Rakai district, Uganda,44 prevention of mother-to-child transmission of HIV in Kenya,45 Malawi,46 HIV treatment as prevention47 or evaluation of novel regimens for prevention of TB in HIV-infected adults.48 In addition, the John McGoldrick Programme initiated in 2008 at the Harvard School of Public Health offers a 6-month training in Biostatistics and Epidemiology in Boston and is targeted at physicians from Africa who show promise in clinical/epidemiological research and dedication to applying the acquired knowledge in conducting high quality AIDS research back in Africa.49 Online educational programmes from foreign institutions are also available. For example, Supercourse is a repository of lectures on epidemiology and global health available on the internet free of charge through the Department of Epidemiology at University of Pittsburgh Graduate School of Public Health.50 Online programmes can provide an important educational and training option in areas where local programmes are not available. However, it is necessary to understand better what proportion of epidemiologists and public health degree holders are trained outside Africa as opposed to in Africa. This information is essential to judge and plan for training capacity needs, for reasons of sustainability, to ensure that Africans get the training relevant to public health in Africa and to begin planning and building Africa’s own alumni network that will further support epidemiology and public health training capacity for the continent.
Linking training and research
Although availability of local and foreign programmes is a substantial improvement for the AFRO region, researchers in epidemiology and public health remain scarce.26 Furthermore, most local and foreign educational programmes offer insufficient research experience, and most graduates require further on-the-job training in epidemiology practice and research.51 Unfortunately, even though graduates’ home institutions often have ongoing externally funded epidemiological studies coordinated by expatriates and older expert academicians, these studies are usually separated from the institution’s educational programmes, and graduates often cannot access them for training.26,52,53
Epidemiology and public health research output
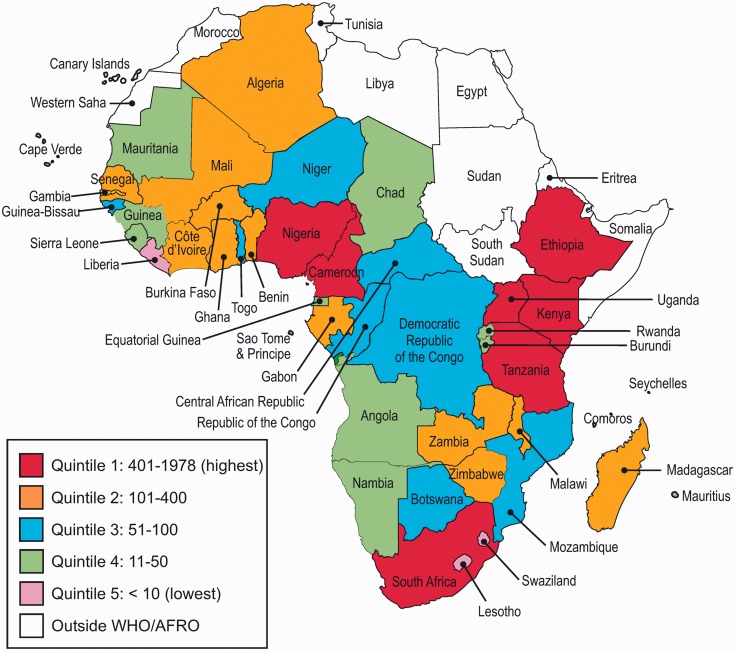
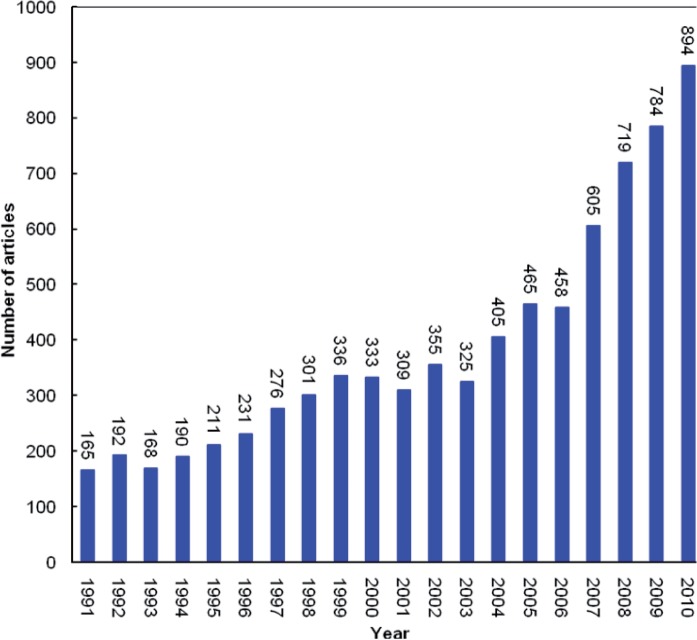
An estimated 8835 indexed epidemiology and public health articles were published by authors from the WHO/AFRO region between 1991 and 2010 (Figure 1). Seven countries (South Africa, Kenya, Nigeria, Tanzania, Uganda, Ethiopia and Cameroon) are in the highest quintile with a total of 401–1978 indexed articles. Thirteen, eight and twelve countries belong to second quintile (101–400 articles), third quintile (51–100 articles) and fourth quintile (11–50 articles), respectively, whereas six countries, Cape Verde, Sao Tome and Principle, Liberia, Comoros, Lesotho and Swaziland, fall in the lowest quintile and produced <10 indexed articles. From 1991 to 2010, epidemiology or public health research output in the WHO/AFRO region increased from 172 to 1086 peer-reviewed articles (APC = 10.1%, P for trend <0.001) (Figure 2). Most articles concerned HIV/AIDS (11.3%), malaria (8.6%) and TB (7.1%). Similarly, the number of first authors (APC = 7.3%, P for trend < 0.001), corresponding authors (APC = 8.4%, P for trend < 0.001) and last authors (APC = 8.5%, P for trend < 0.001) from Africa increased during this period.
Figure 1.
Map representing WHO/AFRO public health and epidemiology publications indexed by SCI (1991–2010)
Figure 2.
Trends in public health and epidemiology articles output by WHO/AFRO researchers as first, last or corresponding authors indexed by SCI (1991–2010)
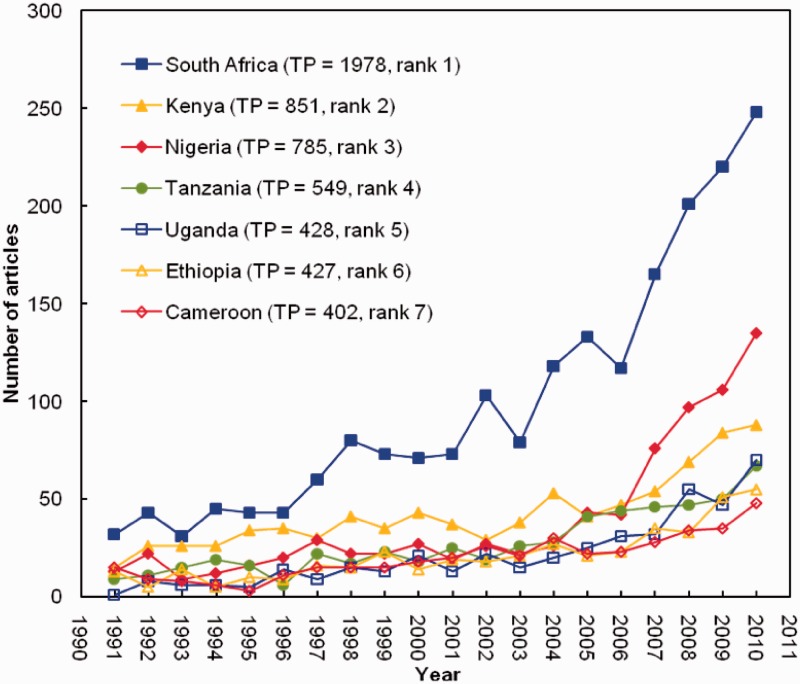
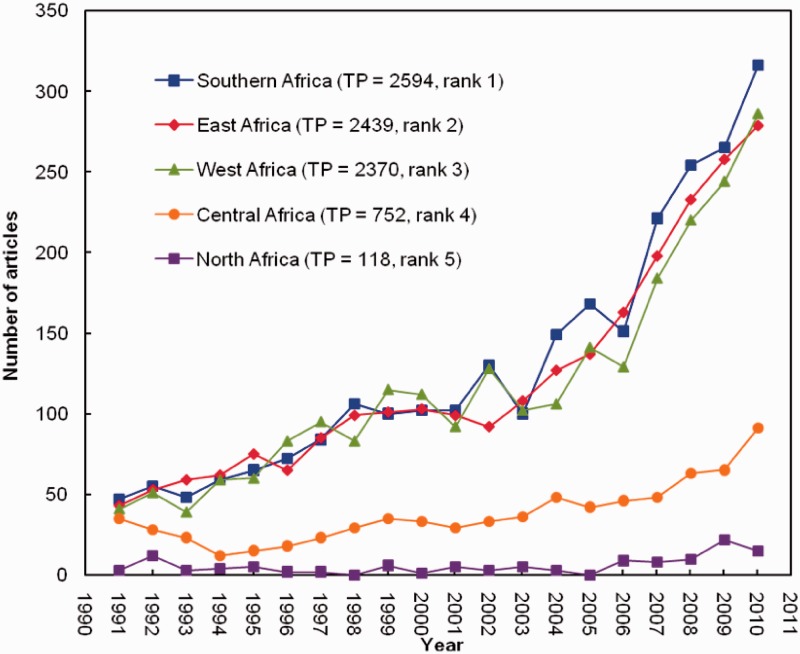
In absolute numbers, authors from the top seven countries combined produced almost two-thirds (61.4%) of the total indexed articles (Figure 3). Authors from South Africa (22.4%) produced the highest number of articles, followed by authors from Kenya (9.6%) and Nigeria (8.9%) (P < 0.001, comparing each country with South Africa). Regionally, authors from Southern Africa (2739 articles; APC = 10.9%, P for trend < 0.001) produced the highest number of articles, followed by authors from East Africa (2597 articles; APC = 10.2%, P for trend < 0.001) and closely followed by authors from West Africa (2564 articles; APC = 10.1%, P for trend < 0.001) (P < 0.001, comparing each country with South Africa) (Figure 4). Overall, French-speaking parts of Africa produced many fewer publications (2260/8835, 25.6%) than a English-speaking areas (6575/8835, 74.4%) (P < 0.001). The top 20 journals publishing the articles are shown in Table 1. The top three are Tropical Medicine and International Health (3.1%), American Journal of Tropical Medicine and Hygiene (2.9%) and Transactions of the Royal Society of Tropical Medicine and Hygiene (2.4%).
Figure 3.
Top seven countries (highest quintile) and trends in epidemiology and public health articles output indexed by SCI (1991–2010). TP, total published articles
Figure 4.
Trends in WHO/AFRO sub-regional epidemiology and public health articles output indexed by SCI (1991–2010). Note: The apparent contrast in North African showing little rise in published output for 2 decades need to take account of the fact that our bibliometric analysis covers only WHO/AFRO region, which include Algeria as the only North Africa country. Four other North African countries (Morocco, Libya, Egypt, Tunisia) are included the WHO’s Eastern Mediterranean Regional Office (WHO/EMRO). TP, total published articles
Table 1.
Top 20 journals and their impact factors with WHO/AFRO researchers as first, senior or corresponding authors
| Journal | TPa | % | 2010 IFa |
|---|---|---|---|
| Tropical Medicine and International Health | 243 | 3.1 | 2.841 |
| American Journal of Tropical Medicine and Hygiene | 227 | 2.9 | 2.446 |
| Transactions of the Royal Society of Tropical Medicine and Hygiene | 188 | 2.4 | 2.832 |
| Malaria Journal | 143 | 1.9 | 3.489 |
| AIDS | 141 | 1.8 | 6.348 |
| Acta Tropica | 132 | 1.7 | 2.262 |
| East African Medical Journal | 128 | 1.7 | N/A |
| Bulletin de la Société de Pathologie Exotique | 127 | 1.6 | N/A |
| Journal of Clinical Microbiology | 124 | 1.6 | 4.22 |
| Bulletin of the World Health Organization | 122 | 1.6 | 5.459 |
| South African Medical Journal | 112 | 1.5 | 1.676 |
| Journal of Infectious Diseases | 102 | 1.3 | 6.288 |
| Lancet | 93 | 1.2 | 33.633 |
| International Journal of Tuberculosis and Lung Disease | 91 | 1.2 | 2.557 |
| Veterinary Parasitology | 87 | 1.1 | 2.331 |
| Annals of Tropical Medicine and Parasitology | 81 | 1.0 | 1.288 |
| BMC Public Health | 81 | 1.0 | 2.364 |
| Journal of Medical Virology | 80 | 1.0 | 2.895 |
| Onderstepoort Journal of Veterinary Research | 79 | 1.0 | 0.302 |
| Tropical Animal Health and Production | 77 | 1.0 | 1.003 |
aTP, total productivity (total number of articles indexed in SCI between 1991 and 2010); IF, impact factor.
Small countries like the Seychelles, Gambia and Gabon had the highest research output per million inhabitants. However, when total published research manuscripts were adjusted for gross domestic product (GDP), Gambia, Guinea Bissau and Zimbabwe were the most productive countries. Gambia, Guinea Bissau and the Seychelles had the highest number of publications per 1 million US dollars of health expenditure.
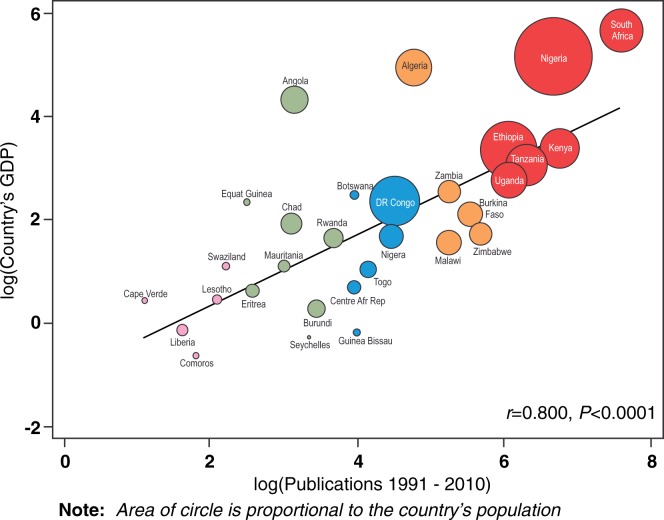
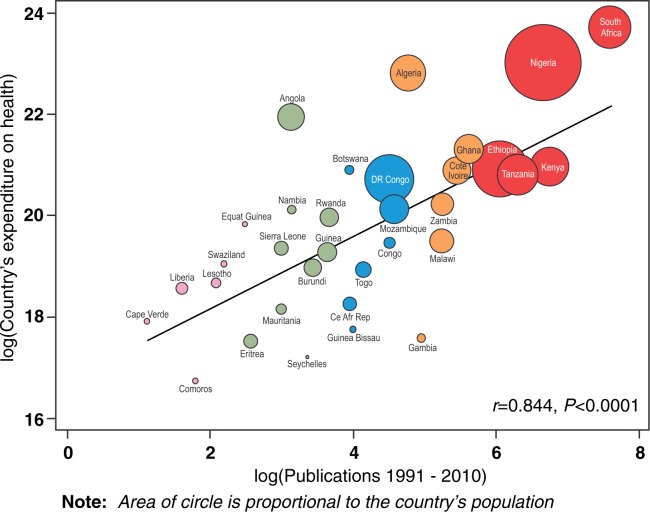
A moderately positive correlation exists between total numbers of published articles and population size of countries (r = 0.556, P = 0.001). A stronger positive correlation was also seen between total numbers of published articles and national GDP (r = 0.800, P < 0.001) (Figure 5). There also was a positive correlation between the total numbers of published article and health expenditure (r = 0.844, P < 0.001) (Figure 6).
Figure 5.
Scatter plot showing association between total publications and country’s GDP. Note: Gross domestic product, 2009 United Nations Development Programme estimates
Figure 6.
Scatter plot showing association between total publications and country’s expenditure on health. Note: Expenditure on health (as % of GDP), 2009 United Nations Development Programme estimates
Population size, language, GDP, number of public health training institutions, health expenditure, research and development expenditure and number of HIV patients were statistically associated with research productivity (Table 2). For every 1 million increase in a country’s population size, the expected research productivity increases by 92% (IRR = 1.92; 95% CI 1.66–2.22). Compared with French-speaking countries, English-speaking countries were 124% more likely to have indexed articles (IRR = 2.24; 95% CI 1.08–6.64). Research productivity increased by 96% per one US$ billion increase in country’s GDP (IRR = 1.96; 95% CI 1.64–2.34). For every one additional increase in the number of public health training institutions in a country, research productivity increased by 298% (IRR = 3.98; 95% CI 2.68–5.89). Similarly, for every 1% increase in GDP spent on health expenditure (IRR = 1.92; 95% CI 1.61–2.30) and research and development expenditure (IRR = 1.92; 95% CI 1.56–2.36), research productivity increased by 92%. Countries’ research productivity increased by 47% per 1000 increase in the number of HIV patients (IRR = 1.64; 95% CI 1.42–1.90). There was no association between adult literacy rate, number of physicians, prevalence of TB, malaria cases and research productivity. In multivariate analysis (Table 2), only the number of public health training institutions (IRR = 3.41; 95% CI 1.90–6.11) and number of HIV patients (IRR = 1.30; 95% CI 1.02–1.66) remained associated with research productivity.
Table 2.
Factors associated with public health and epidemiology research productivity in WHO/AFRO, identified by univariable and multivariable negative binomial regressions
| Indicatora | Univariable (unadjusted) |
Multivariable (adjusted) |
||||
|---|---|---|---|---|---|---|
| IRR (95% CI) | P-value | Percentage Change | IRR (95% CI) | P-value | Percentage Change | |
| Country’s population (in millions) | 1.92 (1.66–2.22) | 0.000 | 92.0 | 1.21 (0.80–1.84) | 0.372 | |
| English (vs French) speaking | 2.24 (1.08–6.64) | 0.030 | 123.8 | 0.66 (0.35–1.23) | 0.188 | |
| Adult literacy rate (% of people ≥15 years) | 1.74 (0.64–4.71) | 0.278 | N/A | N/A | N/A | N/A |
| GDP (in US$ billion) | 1.96 (1.64–2.34) | 0.000 | 95.8 | 1.67 (0.59–4.71) | 0.332 | |
| Physicians (per 100 000 people) | 1.24 (0.91–1.69) | 0.176 | N/A | N/A | N/A | N/A |
| Public health training institutes | 3.98 (2.68–5.89) | 0.000 | 297.5 | 3.41 (1.90–6.11) | 0.000 | 241.2 |
| Expenditure | ||||||
| Health expenditure (as % of GDP) | 1.92 (1.61–2.30) | 0.000 | 92.4 | 0.87 (0.35–2.16) | 0.762 | |
| Research and development (as % of GDP) | 1.92 (1.56–2.36) | 0.000 | 91.9 | 0.61 (0.33–1.13) | 0.116 | |
| Burden of disease | ||||||
| Number of HIV patients | 1.64 (1.42–1.90) | 0.000 | 63.9 | 1.30 (1.02–1.66) | 0.034 | 30.0 |
| TB prevalence (per 100 000 people) | 1.73 (0.99–3.02) | 0.053 | N/A | N/A | N/A | |
| Malaria cases | 0.99 (0.88–1.11) | 0.855 | N/A | N/A | N/A | N/A |
IRR, incidence rate ratio; CI, confidence interval; GDP, gross domestic product; N/A, not applicable.
aIndicators were log transformed.
National and state/provincial epidemiology or public health institutes
Many national health research institutes in the AFRO region operate under direction of a Ministry of Health or other national ministry, e.g. the National Institute of Medical Research in Tanzania,54 the National Institute of Health Research of Zimbabwe,55 the Kenya Medical Research Institute (KEMRI)56 and the Uganda Virus Research Institute.57 However, the South African Medical Research Council is independently established under an act of Parliament. Members of the Board are appointed by the Minister of Health—to whom they are thus accountable.58 The South African Medical Research Council has played a major role for decades in advancing medical research through its various cooperative responsibilities. The Medical Research Council (MRC)’s role in developing skills of future health researchers is apparent in its support for epidemiology and public health programmes in South African universities. The Nigerian Institute of Medical Research was established in 1977 and tasked with research in human medicine by the Nigeria Ministry of Health. The Nigerian Institute of Medical Research has made modest contributions to local research efforts but does not have applied epidemiology or national surveillance capabilities.59
Non-governmental research capacity-building centres or organizations
Significant challenges remain for African countries to establish a common framework for sustainable research capacity strengthening. One rapidly growing approach is establishment of regional or national centres of research excellence. These institutions tend to be research-focused centres that link to epidemiology training programmes within countries or internationally. Selected models of well-functioning research and research support centres that support epidemiology and population health research capacity building in sub-Saharan Africa with support from various funding agencies to include WHO/TDR,60 the Ifakara Health Institute in Tanzania,61 Kintampo Health Research Centre in Kintampo, Ghana,62 KEMRI-Wellcome Trust Research Programme in Kilifi, Kenya,63 the Manhiça Health Research Centre in Maputo, Mozambique,64 the Infectious Diseases Institute of Makerere University in Kampala, Uganda,65,66 the Rakai Health Sciences Programme in Rakai, Uganda,67 the Malaria Research and Training Centre, University of Bamako, Mali,68 the Research Support Centre of the College of Medicine in Malawi69 and the Centre for the AIDS Programme of Research in South Africa.70
The Council on Health Research for Development (COHRED) network concentrates on strengthening national and institutional governance of research and innovation for health, equity and development in low- and middle-income countries worldwide and has a strong presence in sub-Saharan Africa.71 COHRED supports national governance by creating and maintaining Health Research Web72 knowledge platforms that operate in a ‘wiki-type’ mode to enable countries and institutions to provide high-quality information on national health-research systems, funders’ strategies and activities related to health research. It extends into ethical review of health research through a separate platform.73 In addition, the Initiative to Strengthen Health Research Capacity in Africa (ISHReCA)74 is an African-led WHO/TDR-supported network of scientists aimed at advocacy and building capacity for health research in Africa and improving health systems at the same time.75
The African Network for Drugs and Diagnostics Innovation (ANDI), started in 2008, receives funding from the European Union. Its main current activity is encouraging African institutions ‘to be recognized as centres of excellence’, which brings ‘the opportunity to become future ANDI centres for health innovation and further capacity development in Africa’. These centres will be expected to participate both in the implementation of ANDI projects, which will be linked to capacity building, and stimulation of intra-African collaboration and networking.76
Major recent international medical education initiatives that include substantial epidemiology and public health research capacity-building include programmes from the USA and Canada. In 2008, the US President’s Emergency Plan for AIDS Relief provided leadership to support the fight against HIV/AIDS, TB and malaria and was instrumental in the dramatic increase of access to antiretroviral therapy in low-income countries. However, by October 2010, President’s Emergency Plan for AIDS Relief recognized the need to build strong health worker infrastructure and health systems to sustain initial achievements. To do so, it provided a $130 million grant to expand medical education and research capabilities, including epidemiology, through 13 African academic institutions to increase the number of health care staff trained and education quality during the next 5 years.77,78 The Health Research Capacity Strengthening Initiative partnership between the UK Department for International Development, the International Development and Research Center, Canada, and the Wellcome Trust has lent support to develop nationally available research grant funding, awarded and administered locally, in Kenya and Malawi. The Wellcome Trust has recently launched an African Institutions Initiative, which aims to build a critical mass of sustainable local research capacity across Africa by strengthening African universities and research institutions.79
Funding for epidemiological and public health training or research
Most of the funding for epidemiological research in the AFRO region comes from grants and collaborative research projects funded by external sources such as NIH, CDC, USAID, Department for International Development, Australian Agency for International Development, professional societies, private organizations and universities. Charitable organizations such as the Wellcome Trust, the Bill & Melinda Gates Foundation and private industry (i.e. pharmaceutical companies) also provide financial support for research throughout the region—directly or through large programmes they fund. Inevitably, most such externally funded research focuses on the three big conditions only—HIV/AIDS, TB and malaria—but there is a growing interest in addressing the need to cover epidemiology and public health research training and practice relevant to other conditions such as non-communicable diseases (including the emerging burden of disease linked to mental health and trauma/violence) or health systems with the support of the Alliance for Health Systems and Policy Research and the Doris Duke Foundation’s African initiative.80
Many private organizations offer scholarships for students from developing nations to attend universities or training sessions overseas. Professional societies also frequently offer financial support to bring researchers from low-income countries to their conferences to encourage sharing of results and collaboration. Unfortunately, with too few exceptions—such as South Africa funding the South African Medical Research Council, Kenya funding its KEMRI, Tanzania funding its National Institute for Medical Research and a few others—there is minimal public funding from national and local governments for epidemiological research and little, if any, from local private organizations within the countries of the AFRO region. A comparative analysis of the selected epidemiological and/or public health research capacity-building initiatives of >5 years in existence (AFENET, INCLEN, COHRED, ISHReCA, NIH/FIC-AITRP) demonstrate clear achievements and key challenges such as long-term sustainability, which is threatened by dependence on foreign funding (Supplementary Table S2, available as Supplementary data at IJE online).
Human resources in epidemiology
There is a global shortage of health care workers in general and particularly of personnel that are appropriately trained.81,86 In addition, there are limited opportunities and resources for more advanced epidemiology training in Africa and mostly a lack of attention to continuous professional development as well as support staff, hardware, software and speedy internet connectivity. Funding shortfalls and lack of career prospects lead to the loss of talented individuals (from both clinical and public health disciplines) to pursue academic or employment opportunities elsewhere. Those who remain in Africa may find work in the non-governmental sector or private sector without using their epidemiology training. Of those that leave Africa for training, many will not return to their home countries to work or teach. Although numbers are difficult to estimate, the collective effect is both an ‘internal’ and an ‘external’ ‘brain-drain’ in Africa. Furthermore, additional hurdles exist to creating a large and well-trained workforce in epidemiology in Africa, including poor recognition in Africa of epidemiology as a distinct and valuable discipline, restriction of epidemiology education to doctors in many regions, few funding opportunities for epidemiological research and surveillance and poor support for epidemiologists once trained.
However, a clearer picture is emerging of what the ideal epidemiology workforce in the AFRO region would look like. According to our survey respondents, it should include both field epidemiologists working in surveillance and health-related non-governmental organizations and clinical and academic epidemiologists working to advance epidemiological training and research in academic institutions, health care settings and research organizations. In addition, the workforce should include health professionals from public and private institutions and with a range of backgrounds, including medical and veterinary doctors, environmental health professionals, nurses, laboratory scientists, social scientists and others. Ideally, each district should have a health professional trained in epidemiology to provide support for field epidemiology projects and other efforts to identify and address issues at the district level. A Masters degree in public health or epidemiology should be the minimum desired credential, with PhDs in epidemiology expected for those serving as trainers or supervisors. Although our survey respondents are not a representative global sample and may have selection bias, their collected opinions regarding a future vision for epidemiology training and research in the region provide a valuable foundation for planning.
Discussion
A key finding of this study is that during the past 2 decades, the amount of research carried out in the AFRO region has increased dramatically, whether conducted by Africans alone or in collaboration with partners from high-income countries. In parallel, the number and quality of publications also have increased, with particular increases in publications in high impact journals. The findings from our multivariable regression model corroborate this by showing that epidemiology and public health research productivity was associated with number of HIV patients independent of other factors. This association and factors such as increasing North–South collaborations are likely to account for the rapid acceleration in output in recent years seen in South Africa, Nigeria and the eastern Africa region.
Given the growing global interest and the regional impact of non-communicable diseases (including maternal, neonatal and child health) and climate change, such areas of research and training emphasis—disease epidemiology through the life course and climate change/environmental epidemiology—need to move much higher on the agenda in Africa.87 This is especially true in sub-Saharan Africa, where epidemiology training has mostly served control of communicable diseases in general and control of HIV/AIDS, TB and malaria in particular. Additionally, to comprehensively and efficiently address the full burden of diseases in WHO/AFRO, the next decade must see increases in regional epidemiological expertise to identify and elucidate causes of illness rather than just to control communicable diseases and outbreaks.
As national training curricula need to run ahead of national disease burden changes, it is urgent that African and external training programmes include a much more substantial part of public health and epidemiology training in non-communicable disease epidemiology. With the current global interest in non-communicable diseases (NCDs) on the increase, there is a key opportunity to resource African-based epidemiology training programmes (e.g. using existing structures and leveraging on successful programmes on infectious disease research) to be able to deal effectively with NCDs. This can take many forms, including offering PhD scholarships, twinning with successful NCD programmes outside Africa, upgrading of expertise of current academic staff and inclusion of distance learning modules into current African programmes. This list is not exhaustive.
We found that collaboration in public health and epidemiological research in WHO/AFRO happens mostly with researchers in western Europe and the USA and to a far lesser extent with researchers within Africa or Asia. There are many fewer collaborations involving Latin America, but we are aware that Brazil is taking an active interest in building public health research capacity in lusophone countries in Africa, specifically Mozambique and Angola. Whenever collaborative research is in place, it is often not linked to post-graduate training programmes in epidemiology, thus missing major opportunities for experiential training of high quality epidemiologists. Features that seemed to support more successful partnerships include a strong capacity development component, mutual respect of partners, research priorities driven by local needs, involvement of all the key players (including policy makers) and diversity of funding mechanisms (including by local governments).
Centres of epidemiology or public health research excellence or field epidemiological training programmes—often linked to one or more high-income country donor or research institution—are gaining popularity as a tool for research capacity building in epidemiology and public health, and the number of such centres in increasing. However, Masters-level training in public health and epidemiology should be available to all countries—using internet-based resources to supplement areas where capacity lacks. More specialized epidemiology training should be developed in African institutions or centres of excellence where there is already proven capacity—and where additional resources can be used to increase the reach of these institutions.
In addition, even though African countries pay for most local salaries and institutions, external funding influences the research topics being addressed. Priorities from external countries and agencies and those from African countries or from the continent as a whole do not necessarily correlate closely.82,83 Thus, for Africa to take charge of its own research agenda, it will have to start investing in its own research—epidemiological and public health research included.84,85 Indeed, as shown in our comparative analysis of existing epidemiological and public health capacity building initiatives in WHO/AFRO, one of the major challenges is sustainability of such efforts, as they are threatened by dependence on foreign funding, and this need to be addressed urgently.
There are still major shortfalls in continental training capacity in epidemiology and public health, but possibly also in job specifications and career opportunities that require graduate epidemiology training. Training opportunities and demand for epidemiologists should be high, given the health needs of the region. However, human resources for epidemiological and public health research are still limited and are insufficient to meet the demand and expertise needed. Futhermore, although public health training is offered by a number of institutions, post-graduate epidemiology training is not yet as common.
Lastly, although this article focused on WHO/AFRO, there are excellent training epidemiology programmes in north African countries, which are not under WHO/AFRO such as Tunisia, Morocco and Egypt. These are often less expensive than programmes in English-speaking Africa and are often in French, which can supplement lack of capacity in French-speaking regions.88,89 Taking a Pan-African view, this is an option well worth pursuing.
Conclusions and recommendations
Epidemiological research, capacity and expertise in Africa are increasing, but they can have a greater impact on health if the following recommendations are implemented. Human resources planning for public health and epidemiology will need the same level of attention from local and global actors as human resources for personal health services. Without an adequate epidemiology workforce, public health cannot take off—and without public health, disease prevention and health promotion will remain stunted. In short, planning for ‘human resources for health’ without a grand strategy for epidemiology and epidemiologists is self-defeating. In addition, African governments must invest in epidemiology and public health research if they want to take charge of the research agenda and sustain existing capacity building efforts, which are mostly foreign funded. To do this, investments in more graduate and post-graduate training programmes in epidemiology and public health are needed across the continent. They should not only aim for Masters level (with introductory and intermediate epidemiology), but some—in academia and centres of excellence—should target doctoral programme level and the creation of tenure track positions for epidemiologists with advanced analysis skills.
Foreign-funded epidemiology and public health research programmes must maximize the potential for epidemiological research capacity building by linking to national graduate institutions in public health. Ideally, all international collaborative health research programmes with public health characteristics should be linked to at least one African School of Public Health or similar institution that provides graduate degrees in epidemiology or public health. The recently created Association of Schools of Public Health in Africa should have a major focus on advocacy, standardization, collaborative fundraising for research and training activities and holding governments and international collaborators accountable to address all of Africa’s priority public health problems with relevant research and funding. This could perhaps be built into existing groupings, like ISHReCA, or grow out of existing regional or sub-regional epidemiological and public health associations to cover regional economic (and language) communities such as the Community Market of Eastern and Southern Africa, the Economic Community of West African States and the Economic Communities of Central African States as first targets.
Supplementary Data
Supplementary Data are available at IJE online.
Funding
This manuscript was supported by the International Epidemiological Association (IEA) as well as the U.S. President's Emergency Plan for AIDS Relief (PEPFAR), through The Health Resources and Services Administration (HRSA) and via the Stellenbosch University Rural Medical Education Partnership Initiative (SURMEPI). J.B.N. is supported by the United States National Institutes for Allergy and Infectious Disease (NIAID-NIH), Division of AIDS (DAIDS): K23 AI 068582-01; the US PEPFAR Grant Award, T84HA21652-01-00 for Medical Education Partnership Initiative (MEPI); the European Developing Countries Clinical Trial Partnership (EDCTP) Senior Fellowship Award: TA-08-40200-021 and the Wellcome Trust Southern Africa Consortium for Research Excellence (SACORE), WT087537MA. J.B.N. is a 2009 John McGoldrick Fellow, Center for Biostatistics in AIDS Research at Harvard School of Public Health, Boston, MA, USA. C.A. was a 2006 to 2011 double Sommer Scholar at the Department of Epidemiology at the Johns Hopkins Bloomberg School of Public Health and a Fogarty AITRP Fellow/Post-doctoral Fellow with the Institute of Human Virology of the University of Maryland School of Medicine from 2008 to 2011.
Supplementary Material
Acknowledgements
The authors wish to thank Joanna Downer, PhD at Duke University, USA, and Professor Rodney Erlhich, MBChB, PhD and Associate Professor Landon Myer at University of Cape Town, South Africa, as well as Professor Jimmy Volmink at Stellenbosch University, Cape Town, South Africa, for critical reading of this manuscript and constructive suggestions, Mrs. Debbie Harrison, BA, for administrative support. J.B.N. led the setting of overall article structure and drafting. M.L. undertook preliminary information searches, liaisons with co-authors and informants, adaptation of the questionnaire and initial drafting of selected sections of the article. All authors contributed to data interpretation, and writing of the paper, as well as approval of the final version. J.B.N. and C.I. were responsible for the major final edit.
Conflict of interest: None declared.
KEY MESSAGES.
Epidemiology and public health research productivity is skewed in the 46-member WHO/AFRO region: South Africa, Kenya and Nigeria make up a striking 40% of the total number of articles indexed by PubMed between 1991 and 2010.
To increase epidemiology research productivity in the region, more high-quality intermediate and advanced levels epidemiology education and training programmes are needed, as is increased recognition of the ability of epidemiology to identify causes of disease.
The primary emphasis for growth should be on Masters level training, with some doctoral and post-doctoral training opportunities in academia and centres of excellence, to ensure that Africa becomes self-sufficient in epidemiological research and education.
In sub-Saharan Africa, epidemiology training has mostly served control of communicable diseases in general and control of HIV/AIDS, TB and malaria in particular. However, to comprehensively and efficiently address the full burden of diseases in WHO/AFRO—which includes an increasing impact of non-communicable diseases, maternal and child health conditions and injury—regional epidemiological expertise will be needed that can identify emerging health concerns and elucidate determinants of population burden of disease, rather than just control communicable diseases and outbreaks.
Comparative analysis of the various epidemiological and/or public health training and research capacity-building initiatives of >5 years in existence (AFENET, INCLEN, COHRED, ISHReCA, NIH/FIC-AITRP) demonstrate clear achievements, but sustainability of such efforts is threatened by dependence on foreign funding, and this need to be addressed urgently.
References
- 1.Porta M. A Dictionary of Epidemiology. 5th edn. Oxford University Press; 2008. [Google Scholar]
- 2.Greysen SR, Dovlo D, Olapade-Olaopa EO, Jacobs M, Sewankambo N, Mullan F. Medical education in sub-Saharan Africa: a literature review. Med Educ. 2011;45:973–86. doi: 10.1111/j.1365-2923.2011.04039.x. [DOI] [PubMed] [Google Scholar]
- 3.Gezmu M, DeGruttola V, Dixon D, et al. Strengthening biostatistics resources in sub-Saharan Africa: research collaborations through U.S. partnerships. Stat Med. 2011;30:695–708. doi: 10.1002/sim.4144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. Geneva: World Health Organization, 2009. http://www.who.int/healthinfo/global_burden_disease/risk_factors/en/index.html (26 June 2011, date last accessed)
- 5.Ezzati M, Lopez A, Rodgers A, et al. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 6.UNAIDS 2010. UNAIDS report on the Global AIDS Epidemic 2010. http://www.unaids.org/globalreport/documents/20101123_GlobalReport_full_en.pdf (26 June 2011, date last accessed)
- 7.World Health Organization. TB/HIV Facts 2009. http://www.who.int/tb/challenges/hiv/factsheet_hivtb_2009update.pdf (26 June 2011, date last accessed)
- 8.World Health Organization. World Malaria Report 2010. http://www.who.int/malaria/world_malaria_report_2010/worldmalariareport2010.pdf (26 June 2011, date last accessed)
- 9.WHO 2009. Cooperation Strategy at a Glance: Nigeria. http://reliefweb.int/node/344389 (26 October 2011, date last accessed)
- 10.WHO 2009. Cooperation Strategy at a Glance: Liberia. http://reliefweb.int/node/333668 (26 October 2011, date last accessed)
- 11.WHO 2009. Cooperation Strategy at a Glance: Uganda. http://reliefweb.int/node/344383 (26 October 2011, date last accessed)
- 12.WHO 2009. Cooperation Strategy at a Glance: Malawi. http://reliefweb.int/node/333709 (26 October 2011, date last accessed)
- 13.WHO 2009. Cooperation Strategy at a Glance: Zambia. http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_zmb_en.pdf (26 October 2011, date last accessed)
- 14.WHO 2009. Cooperation Strategy at a Glance: South Africa. http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_zaf_en.pdf (26 October 2011, date last accessed)
- 15.Mayosi BM, Flisher AJ, Lalloo UG, et al. Health in South Africa 4. The burden of non-communicable diseases in South Africa. Lancet. 2009;374:934–47. doi: 10.1016/S0140-6736(09)61087-4. [DOI] [PubMed] [Google Scholar]
- 16.Tollman SM, Kahn K, Sartorius B, et al. Implications of mortality transition for primary health care in rural South Africa: a population-based surveillance study. Lancet. 2008;372:893–901. doi: 10.1016/S0140-6736(08)61399-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Groenewald P, Bradshaw D, Daniels J, et al. Cause of Death and Premature Mortality in Cape Town, 2001–2006. Cape Town: South African Medical Research Council; 2008. [Google Scholar]
- 18.Sanders D, Chopra M. Key challenges to achieving health for all in an inequitable society: The case of South Africa. Am J Public Health. 2006;96:73–78. doi: 10.2105/AJPH.2005.062679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shisana O, Rehle LC, Simbayi L, et al. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2008: A Turning Tide Among Teenagers? Cape Town: HSRC Press. http://www.hsrcpress.ac.za/product.php?productid=2264&freedownload=1. (26 June 2011, date last accessed)
- 20.The World Bank. Southern Africa HIV/AIDS and Tuberculosis Plan of Action. 2010–2011. http://siteresources.worldbank.org/extafrregtophivaids/Resources/SACU-Action-Plan.pdf (11 October 2011, date last accessed)
- 21.Kalua F, Awotedu A, Kamwanja L, et al. The New Partnership for Africa’s Development (NEPAD). Science, Technology and Innovation for Public Health in Africa, 2009 http://www.nepadst.org/doclibrary/pdfs/stipha_mar2009.pdf (25 November 2012, date last accessed) [Google Scholar]
- 22.Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–57. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 23.Li JF, Zhang YH, Wang XS, et al. Bibliometric analysis of atmospheric simulation trends in meteorology and atmospheric science journals. Croat Chem Acta. 2009;82:695–705. [Google Scholar]
- 24.Clegg LX, Hankey BF, Tiwari R, et al. Estimating average annual percent change in trend analysis. Stat Med. 2009;28:3670–82. doi: 10.1002/sim.3733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lloyd-Smith JO. Maximum likelihood estimation of the negative binomial dispersion parameter for highly overdispersed data, with applications to infectious diseases. PLoS One. 2007;2:e180. doi: 10.1371/journal.pone.0000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Binet FE. Fitting the negative binomial-distribution. Biometrics. 1986;42:989–92. [PubMed] [Google Scholar]
- 27.IJsselmuiden CB, Nchinda TC, Duale S, et al. Mapping Africa’s advanced public health education capacity: the AfriHealth project. Bull World Health Organ. 2007;85:914–22. doi: 10.2471/BLT.07.045526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thomson Reuters. Global Research Report 2010. http://thomsonreuters.com/content/corporate/docs/globalresearchreport-africa.pdf (20 June 2011, date last accessed)
- 29.Sanders D, Guwatudde D, Alexander L. Accessible public-health education: A potential growth area? Bull World Health Organ. 2008;86:577–656. doi: 10.2471/BLT.08.051334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The Higher Education Alliance for Leadership through Health (HEALTH) http://musph.mak.ac.ug/index.php?option=com_content&view=article&id=74:the-higher-education-alliance-for-leadership-through-health-health&catid=17&Itemid=339. (20 September 2012, date last accessed)
- 31.The Leadership Initiative for Public Health in East Africa (LIPHEA) project. http://liphea.halliance.org/ (11 October 2011, date last accessed)
- 32.One Health Central and Eastern Africa consortium (OHCEA) http://foodsystemsleadership.org/Archives/Archive.aspx?ArID=34 (11 October 2011, date last accessed)
- 33. Public Health Association of South Africa. Association of Schools of Public Health in Africa (ASPHA). http://www.phasa.org.za/public-health-news/association-of-schools-of-public-health-in-africa-aspha.html/ (19 September 2012, date last accessed)
- 34.The South African Centre for Epidemiological Modelling and Analysis (SACEMA) http://www.sacema.com/ (19 October 2011, date last accessed)
- 35.The African Field Epidemiology Network. http://www.afenet.net (19 October 2011, date last accessed)
- 36.Mukanga D, Namusisi O, Gitta S, et al. Field epidemiology training programmes in Africa—where are the graduates? Hum Res Health. 2010;8:18. doi: 10.1186/1478-4491-8-18. http://www.human-resources-health.com/content/8/1/18/. (19 October 2011, date last accessed) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.The International Clinical Epidemiology Network (INCLEN) http://www.inclen.org/ (19 October 2011, date last accessed)
- 38.International Epidemiologic Database to Evaluate AIDS (IeDEA) http://www.nichd.nih.gov/research/supported/iedea.cfm/ (10 October 2010, date last accessed)
- 39.Kinyanjui S, Timæus IM. The International Network for the Demographic Evaluation of Populations and their Health (INDEPTH), the importance of core support. Sida Rev 2010:11. http://www.sidaresearch.se/media/5221/sida%20rewiew%20of%20indepth.pdf/ (19 October 2011, date last accessed)
- 40.Agence Nationale de Recherches sur le SIDA et les Hepatites Virales (ANRS) http://www.anrs.fr/ (22 September 2012, date last accessed)
- 41.National Institutes of Health. http://www.fic.nih.gov (19 September 2012, date last accessed)
- 42.The European & Developing Countries Clinical Trials Partnership (EDCTP) http://www.edctp.org (20 November 2011, date last accessed) [DOI] [PMC free article] [PubMed]
- 43.Abdool Karim Q, Abdool Karim SS, Frohlich JA, et al. CAPRISA004 Trial Group. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329:1168–74. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–66. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 45.Nduati R, John G, Mbori-Ngacha D, et al. Effect of breastfeeding and formula feeding on transmission of HIV-1: a randomized clinical trial. JAMA. 2000;283:1167–74. doi: 10.1001/jama.283.9.1167. [DOI] [PubMed] [Google Scholar]
- 46.Chasela CS, Hudgens MG, Jamieson DJ, et al. Maternal or infant antiretroviral drugs to reduce HIV-1 transmission. N Engl J Med. 2010;362:2271–81. doi: 10.1056/NEJMoa0911486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cohen MS, Chen YQ, McCauley M, et al. HPTN 052 Study Team. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martinson NA, Barnes GL, Moulton LH, et al. New regimens to prevent tuberculosis in adults with HIV infection. N Engl J Med. 2011;365:11–20. doi: 10.1056/NEJMoa1005136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harvard University, School of Public Health. The John L. McGoldrick Fellowship in Biostatistics in AIDS Research. http://www.hsph.harvard.edu/biostats/mcgoldrick/ (19 September 2012, date last accessed) [Google Scholar]
- 50.Pittsburgh University Department of Epidemiology. Supercourse: Epidemiology the internet and Global Health. http://www.pitt.edu/∼super1/ (19 September 2012, date last accessed) [Google Scholar]
- 51.Eisemon TO, Davis CH. Can the quality of scientific training and research in Africa be improved? Minerva. 1991;29:1–26. [Google Scholar]
- 52.Meek VL, Teichler U, Kearney ML. Higher education, research and innovation: changing dynamics. Report on the UNESCO Forum on Higher Education, Research and Knowledge 2001–2009. http://www.uni-kassel.de/incher/v_pub/UNESCO_RR_09.pdf (19 September 2011, date last accessed)
- 53.Edejer TTT. North-South research partnerships: the ethics of carrying out research in developing countries. BMJ. 1999;319:438–41. doi: 10.1136/bmj.319.7207.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.National Institute for Medical Research, Tanzania. http://www.nimr.or.tz/ (19 September 2012, date last accessed)
- 55.The National Institute of Health Research, Zimbabwe. Blair Research Laboratory renamed. http://www.thezimbabwean.co.uk/news/zimbabwe/55270/blair-research-laboratory-renamed.html (30 November 2012, date last accessed)
- 56.Kenya Medical Research Institute. http://www.kemri.org/ (10 October 2011, date last accessed)
- 57.Uganda Virus Research Institute (UVRI) and Medical Research Council (MRC) Collaboration. http://www.mrcuganda.org/Collaboration2.html (10 October 2011, date last accessed)
- 58.South African Medical Research Council. http://www.mrc.ac.za/ (10 October 2011, date last accessed)
- 59.Nigeria Institute of Medical Research. http://www.nimr-ng.org/ (10 October 2011, date last accessed)
- 60.The Special Programme for Research and Training in Tropical Diseases. http://www.who.int/tdr/about/en/ (30 November 2012, date last accessed)
- 61.Ifakara Health Institute. Excellence in science. Profiles of research institutions in developing countries. http://www.ihi.or.tz (19 September 2012, date last accessed)
- 62.Kintampo Health Research Centre, Ghana. http://www.kintampo-hrc.org/ (19 September 2012, date last accessed)
- 63.Kenya Medical Research Institute (KEMRI)-Wellcome Trust Research Programme. http://www.kemri-wellcome.org/ (19 September 2012, date last accessed)
- 64.The Manhiça Health Research Centre, Mozambique. http://www.manhica.org/eng (19 September 2012, date last accessed)
- 65.Makerere University Infectious Diseases Research Institute. http://idi-makerere.com/ (19 September 2012, date last accessed)
- 66.Ronald A, Kamya M, Katabira E, et al. The Infectious Diseases Institute at Makerere University, Kampala, Uganda. Infect Dis Clin North Am. 2011;25:369–83. doi: 10.1016/j.idc.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 67.Rakai Health Sciences Program. http://www.rhsp.org/content/rakai-health-sciences-program (19 September 2012, date last accessed)
- 68.MalariaGen. Malaria Research and Training Centre, University of Bamako, Bamako, Mali. http://www.malariagen.net/node/197 (19 September 2012, date last accessed)
- 69.University of Malawi College of Medicine. Research Support Centre. http://www.medcol.mw/rsc/index.htm (19 September 2012, date last accessed)
- 70.Center for the AIDS Programme of Research in South Africa. http://www.caprisa.org/SitePages/Home.aspx (19 September 2012, date last accessed)
- 71.IJsselmuiden CB, Duale S, Nchinda TC. Principles of Good Partnerships for Strengthening Public Health Education Capacity in Africa. Washington, DC: Council on Health Research for Development and the Academy for Educational Development; 2004. [Google Scholar]
- 72.Health Research Web. www.healthresearchweb.org (10 October 2011, date last accessed)
- 73.Research Ethics Web. Mapin African Research Ethics Review Capacity. www.researchethicsweb.org (10 October 2011, date last accessed)
- 74.ISHReCA. http://ishreca.org/ (19 September 2012, date last accessed)
- 75.Whitworth JA, Kokwaro G, Kinyanjui S, et al. Strengthening capacity for health research in Africa. Lancet. 2008;372:1590–93. doi: 10.1016/S0140-6736(08)61660-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.The African Network for Drugs and Diagnostics Innovation. http://www.andi-africa.org/ (10 October 2011, date last accessed) [DOI] [PubMed]
- 77.National Institutes of Health/Fogarty International Center (NIH/FIC). HHS Agencies Partner with PEPFAR to Transform African Medical Education in the MEPI Program (Medical Education Partnership Initiative) http://www.nih.gov/news/health/oct2010/fic-07.htm (8 October 2011, date last accessed)
- 78.National Institutes of Health/Fogarty International Center (NIH/FIC). NIH Partners with PEPFAR to Strengthen Medical Education in Africa. http://www.nih.gov/news/health/mar2010/fic-15.htm (8 October 2011, date last accessed)
- 79.The Wellcome Trust African Institutions Initiative. African institutions lead international consortia in £30 million initiative. Available from: http://www.wellcome.ac.uk/News/Media-office/Press-releases/2009/WTX055742.htm (27 November 2011, date last accessed)
- 80.IJsselmuiden CB, Kennedy AK. COHRED Statement. Responsible Vertical Programming: How Global Health Research can Deliver Essential Research, Achieve Impact and Build National Systems. Geneva: COHRED, 2007. ISBN 92-9226-024-3. (available from www.cohred.org)
- 81.World Health Organization. The World Health Report 2006 - working together for health. http://www.who.int/whr/2006/en/index.html (29 November 2012, date last accessed)
- 82.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31:285–93. [PubMed] [Google Scholar]
- 83.Esser DE, Keating Bench K. Does global health funding respond to recipients’ needs? Comparing public and private donors’ allocations in 2005–2007. World Develop. 2011;39:1271–80. [Google Scholar]
- 84.Sato J, Shiga H, Kobayashi T, Kondoh H. “Emerging donors” from a recipient perspective: an institutional analysis of foreign aid in Cambodia. World Develop. 2011;39:2091–104. [Google Scholar]
- 85.Swingler GH, Pillay V, Pienaar ED, Ioannidis JP. International collaboration, funding and association with burden of disease in randomized controlled trials in Africa. Bull World Health Organ. 2005;83:511–17. [PMC free article] [PubMed] [Google Scholar]
- 86.IJsselmuiden C, Marais DL, Becerra-Posada F, Ghannem H. Africa’s neglected area of human resources for health research—the way forward. S Afr Med J. 2012;102:236–41. [PubMed] [Google Scholar]
- 87.Mayosi BM, Mekwa JN, Blackburn J, et al. Strengthening research for health, innovation and development in South Africa. Proceedings and Recommendations of the 2011 National Health Research Summit. Pretoria: National Health Research Committee, 2012. http://www.doh.gov.za/docs/reports/2012/summitreport.pdf (22 August 2012, date last accessed)
- 88.Jabbour S, Giacaman R, Khawaja M, Nuwayhid I. Public Health in the Arab World. Cambridge: Cambridge University Press, 2012.
- 89.Zurayk H, Giacaman R, Mandil A. Graduate education in public health: toward a multidisciplinary model. http://www.aub.edu.lb/fhs/phaw/about/Documents/phaw_web-appendix_Ch-33.pdf (22 August 2012, date last accessed)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.