Abstract
Bacillus anthracis is the causative agent of anthrax, and its spores have been developed into lethal bioweapons. To mitigate an onslaught from airborne anthrax spores that are maliciously disseminated, it is of paramount importance to develop a rapid-response anthrax vaccine that can be mass administered by nonmedical personnel during a crisis. We report here that intranasal instillation of a nonreplicating adenovirus vector encoding B. anthracis protective antigen could confer rapid and sustained protection against inhalation anthrax in mice in a single-dose regimen in the presence of preexisting adenovirus immunity. The potency of the vaccine was greatly enhanced when codons of the antigen gene were optimized to match the tRNA pool found in human cells. In addition, an adenovirus vector encoding lethal factor can confer partial protection against inhalation anthrax and might be coadministered with a protective antigen-based vaccine.
INTRODUCTION
Anthrax is a naturally occurring bacterial disease caused by Bacillus anthracis infection, manifested in cutaneous, gastrointestinal, or inhalational form (1). Malicious dissemination of anthrax spores as an airborne bioweapon is a major biodefense concern since inhalation of anthrax spores is highly lethal (2). The harmful impact of anthrax on health is attributed to the production of a poly-gamma-d-glutamic acid (PGA) capsule, which confers resistance to phagocytosis postinfection (3), and the production of a tripartite exotoxin consisting of protective antigen (PA), lethal factor (LF), and edema factor (EF) (4). Although antibiotic therapy is effective against anthrax, latent spores may germinate many weeks postexposure, requiring prolonged administration of the antibiotic for full therapeutic effect (5, 6). Vaccination is the most effective medical intervention against anthrax, either as a preventative or in conjunction with antibiotic treatment for conferring postexposure prophylaxis (1).
The currently licensed human anthrax vaccine in the United States is anthrax vaccine adsorbed (AVA; BioThrax), which is produced by adsorbing cell-free filtrates of microaerophilic cultures of the B. anthracis V770-NP1-R strain onto aluminum hydroxide (1). The principal antigenic component of AVA is PA with undefined amounts of LF and EF (7). AVA requires five intramuscular injections over 18 months plus annual boosters to maintain the level of protection (8). The administration of AVA is associated with ∼1% local, as well as systemic, adverse reactions (8). Although vaccination by injection of AVA confers complete protection against inhalation anthrax in animal models (9), it is unclear how well AVA can protect humans against inhalation anthrax (2). A variety of next-generation anthrax vaccines designed to address these issues are currently in development. Ideally, a new anthrax vaccine should be suitable to rapid mass manufacturing, mass administration by nonmedical personnel with minimal side effects, and preferably effective in a single-dose regimen.
Nasal administration of nonreplicating human adenovirus serotype 5 (Ad5)-vectored vaccines mimic a route of natural infection and stimulate both humoral and cellular immunity systemically and on mucosal surfaces (10–12). These features make them ideal for the purpose of intranasal (i.n.) vaccination against pathogens.
We have shown previously that mice are protected against tetanus by i.n. immunizations with an Ad5 vector encoding tetanus toxin C fragment (13). We have shown that in the presence of strong preexisting anti-Ad5 immunity humans can be safely and effectively immunized with an Ad5-vectored nasal influenza vaccine (14). We provide in the present study experimental data that demonstrate that A/J mice with preexisting immunity to Ad5 can be immunized and protected by a single i.n. administration with an Ad5-vectored anthrax vaccine (AdVAV) encoding a codon-optimized PA gene. In addition, i.n. administration of an Ad5 vector expressing LF induces limited protection against spore infection and might be used in conjunction with a PA-based vaccine.
MATERIALS AND METHODS
Cell culture, medium, and reagents.
PER.C6 cells were provided by CruCell (Netherlands) and cultured in Dulbecco modified Eagle medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and 10 mM MgCl2. Contaminant-free human embryonic kidney 293 (HEK293) cells (Medicine BioServices, Inc., La Jolla, CA) were maintained in RPMI 1640 supplemented with 10% FBS. RAW 264.7 mouse macrophage cells were purchased from the American Type Culture Collection (ATCC; Manassas, VA) and cultured in DMEM supplemented with 10% FBS. The cells were incubated at 37°C in 10% CO2. Cell culture media and reagents were purchased from Mediatech, Inc. (Herndon, VA), and FBS was purchased from Serologicals Corp. (Norcross, GA).
Construction and production of adenoviral vectors. (i) Construction of adenoviral vectors encoding non-codon-optimized gene sequences: AdPAD4, AdPA63, AdPA83, AdLFn, and AdmLF7.
The full-length non-codon-optimized PA gene encoding PA83 and its signal peptide sequence was PCR amplified with template DNA prepared from a Sterne strain (34F2) of B. anthracis by using the specific primers 5′-GGATTCGGTACCACCATGAAAAAACGAAAAGTGTTAATACCA-3′ and 5′-GAATTCTCTAGACCTTATCCTATCTCATAGCCTTTTTTAGAA-3′ and cloned into a pAdApt shuttle vector to generate a pAdApt/PA83 construct. pAdApt/PAD4 (encoding domain 4 of PA which includes C-terminal last 139 amino acids of the PA) was provided by Charles Turnbough (University of Alabama, Birmingham, AL). pAdApt/PA63 (encoding a 63-kDa active form of PA that includes amino acids 175 to 764 of the PA), pAdApt/LFn (encoding amino acids 10 to 254 of LF, a truncated version of LF that retained the N-terminal PA-binding domain without the catalytic domain of LF [15]), and pAdApt/mLF7 (encoding the full-length but atoxic B. anthracis LF, which has the E687C substitution [16]) were provided by Darrell Galloway (Ohio State University, Columbus, OH). The AdPAD4, AdPA63, AdPA83, AdLFn, and AdmLF7 viral vector seeds were created by cotransfection of the pAdApt/PAD4, pAdApt/PA63, pAdApt/PA83, pAdAptLFn, and pAdApt/mLF7 with an Ad5 backbone plasmid pAdeasy-1 into the PER.C6 packaging cells (17).
(ii) Construction of adenoviral vector encoding codon-optimized gene sequences, AdtPA83hu, AdtLFnhu, and AdPA83hu.
The tPA83hu fragment, an amino-terminal human tissue plasminogen activator (tPA) leader sequence, followed with a codon-optimized B. anthracis PA83 gene (without the PA signal peptide sequence), and the tLFnhu fragment, the tPA leader sequence followed by a codon-optimized fusion gene of the LFn fragment (encoding amino acids 1 to 254) and Yersinia V fragment were amplified by using a forward primer 5′-TAAGGGAAGCTTGCTAGCCACCATGGATGCAATGAAGAGA-3′ and a reverse primer 5′-ATGGCTGTTAACTAGAAGGCACAGCAGATCTTCA-3′, which incorporate the HindIII, NheI, and HpaI cleavage sites, with VR1020/humanizedPA83 and VR1020/humanizedLCRvLFn plasmids as DNA templates, respectively. The PCR generated tPA83hu fragment was digested with HindIII and HpaI and cloned into the HindIII and HpaI sites of a pAd shuttle vector, and the PCR-generated tLFnhu fragment was digested with NheI and HpaI and cloned into the NheI and HpaI sites of a pAd shuttle vector to construct pAdtPA83hu and pAdtLFnhu, respectively. A codon-optimized PA83 gene with its signal peptide sequence (but not the tPA leader sequence) was synthesized and cloned into HindIII and XbaI sites of the pAd shuttle vector to generate a pAdPA83hu. The pAdtPA83hu, pAdtLFnhu, and pAdPA83hu plasmids were used for generation of AdtPA83hu, AdtLFnhu, and AdPA83hu vectors as described previously (18).
(iii) Production of adenoviral vectors.
All Ad5 vectors were propagated on PER.C6 cells and purified by ultracentrifugation over a cesium chloride gradient as described previously (13). The purified Ad5 vectors were sterilized by 0.22-μm-pore-size filtration and stored at 4°C or −20°C in A195 adenoviral storage buffer (19). Ad5 vector titers were determined by using an Adeno-X rapid titer kit (Clontech, Mountain View, CA) on HEK293 cells. All of the insertions of above Ad5 vectors were checked by partial DNA sequencing (The Genomics Core Facility of the Heflin Center for Human Genetics, University of Alabama at Birmingham).
Animal experiments.
The B. anthracis Sterne 34F2 strain (Colorado Serum Co., Denver, CO) is nonencapsulated (pXO2−) but toxigenic (pXO1+) with PA and LF expressed from the pXO1 plasmid. Live B. anthracis Sterne spores were mass produced and purified through gradients of Renografin-60 (Bracco Diagnostic, Princeton, NJ) as described previously (20). A/J mouse vaccinations with adenoviral constructs, followed by B. anthracis Sterne spore challenge, were performed at the Battelle Memorial Institute (Columbus, OH; studies 613-G005625, 649-G005625, and 675-G005625) and at the University of Alabama at Birmingham (Birmingham, AL), respectively. Briefly, young (2- to 3-month-old) female A/J mice (Jackson Laboratory, Bar Harbor, ME) were immunized by i.n. inoculation of 30 to 50 μl of Ad5 vectors into one of the nostrils of an anesthetized mouse. Blood samples were collected pre- and postvaccination and stored at −20°C until analyzed. Bronchoalveolar lavage (BAL) was taken by flushing the lungs with 1.0 ml of phosphate-buffered saline (PBS) and stored at −20°C until analyzed. Immunized A/J mice were challenged by i.n. instillation of 5 × 105 CFU of B. anthracis Sterne spores (∼50 × the 50% lethal dose [LD50]) in a volume of 10 μl as previously described (20). Animals were maintained in the animal facility at the Battelle Memorial Institute and University of Alabama at Birmingham. Daily care was provided by trained technicians at Battelle Memorial Institute and University of Alabama at Birmingham Animal Resource Center. Challenge studies were performed in designed challenge rooms. All experiments in mice were performed according to institutional guidelines.
Anti-PA and anti-LF IgG and IgA antibody titers.
Anti-PA and anti-LF immunoglobulin G (IgG) titers in mouse serum samples were determined by enzyme-linked immunosorbent assay (ELISA) using purified PA or LF protein (List Biological Laboratories, Campbell, CA) as the capture antigen. Briefly, 96-well plates were coated with 100 ng of purified PA or LF protein/well dissolved in PBS at 4°C overnight. Plates were washed with Tris-buffered saline (TBS; 50 mM Tris-HCl, 0.15 M NaCl [pH 7.3]) and blocked with 1% bovine serum albumin in TBS. The serum samples and horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG (Promega Corp., Madison, WI) were incubated sequentially on the plates with extensive washing between incubations. All incubations were carried out at 37°C for 1 h. The presence of bound antibody was detected after 10 min of incubation in the presence of α-phenylenediamine substrate (Sigma), and the absorbance was read at 490 nm using a Molecular Devices model Precision microplate reader. The endpoint was determined as the dilution of serum producing the same optical density at 490 nm as a 1/100 dilution of preimmune serum. Sera negative at the lowest dilution tested were assigned endpoint titers of 1. Titers of anti-PA and anti-LF IgA in mouse BAL samples were measured by ELISA as described above. The second antibody used was HRP-conjugated goat anti-mouse IgA (Southern Biotech, Birmingham, AL).
Anti-Letx neutralizing antibody titers.
Serum samples were analyzed for anti-lethal toxin (anti-Letx) neutralizing antibodies as described for a toxin neutralization assay (21) with modifications. RAW 264.7 mouse macrophage cells were placed in flat-bottom 96-well microtiter plates at a concentration of 5 × 104 cells/well in culture medium incubated for 24 h at 37°C. Serum samples from each mouse were serially diluted and incubated with an equal volume of Letx (200 ng of PA/ml plus 200 ng of LF/ml in cell culture medium) for 1 h at room temperature to allow neutralization to occur. Media from the cells in 96-well plates were aspirated and replaced with the serum-Letx mixture at 100 μl/well. Cells in control wells were incubated with 100 μl of medium only or Letx without mouse serum. After ∼20 h of incubation at 37°C, the cell viability was measured by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenylterazolium bromide (MTT) assay as described previously (20). Samples in duplicate were read on a Precision microplate reader (Molecular Devices) at 490 nm. The survival of control cells without exposure to Letx was arbitrarily defined as 100% protection, and the reading of the Letx-only wells was defined as 0% protection. The neutralization titer was determined as the reciprocal of the highest serum dilution resulting in 50% protection of the cells.
Anti-Ad5 neutralizing antibody assay.
Anti-Ad5 neutralizing antibody titers were measured by incubating diluted serum samples with wild-type (wt) Ad5 as described previously (13). Briefly, 293 cells were placed in flat-bottom 96-well microtiter plates at a concentration of 2.5 × 104 cells/well in culture medium incubated for 24 h at 37°C. Serum samples from each mouse were serially diluted in serum-free culture medium. Then, 60 μl of each dilution was mixed with 1.7 × 104 infectious units (IFU) of wt Ad5 in 60 μl of medium containing 2% FBS with antibiotic for 1 h at room temperature to allow neutralization to occur. Media from the cells in 96-well plates were aspirated and replaced with 100 μl of serum-Ad5 mixture/well. The cells in control wells were incubated with 100 μl of medium only or wt Ad5 without mouse serum. After 2 h of incubation at 37°C, the serum-Ad5 mixture was replaced with cell culture medium. Cell viability at 4 days postinfection was determined by MTT assay. The survival of control cells without exposure to Ad5 was arbitrarily defined as 100% protection, and the readings of the Ad5-only wells were defined as 0% protection. Neutralization titer was determined as the reciprocal of the highest serum dilution resulting in 50% protection of the cells.
Statistical analysis.
All statistical analysis was performed using GraphPad Prism version 5.04 (GraphPad Software, San Diego, CA). Log-rank (Mantel-Cox) tests were performed for comparing survival curves and the mean times to death (MTD) in challenged animals. One-way analysis of variance with Tukey's multiple-comparison post tests were performed to compare anti-Letx neutralizing antibody titers and anti-PA and anti-LF IgG ELISA titers. Statistical significance was set at P < 0.05.
RESULTS
Codon-optimized Ad5-vectored anthrax vaccines offer better protection against anthrax spore challenges than their cognate counterparts.
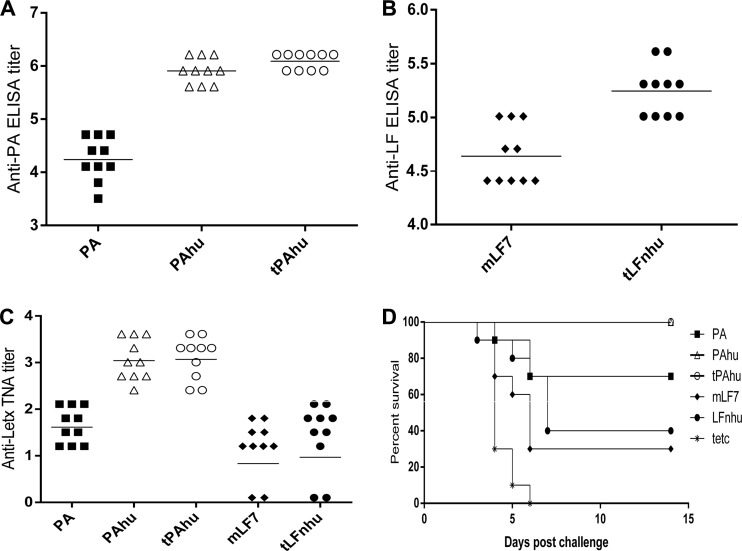
In developing the Ad5-vectored anthrax vaccines, five Ad5 vectors—AdPAD4, AdPA63, AdPA83, AdLFn, and AdmLF7—encoding non-codon-optimized DNA sequence for subdomains and full length of PA or LF proteins were constructed. Animal experiments indicated that the Ad5 vectors encoding full-length PA or LF were able to achieve higher levels of serum antigen-specific IgG antibodies, stronger anti-Letx neutralizing antibody responses, and better protection against lethal anthrax spore challenges than their truncated counterparts. However, only partial protection was afforded against a 5 × 105 CFU B. anthracis Sterne spore (∼50 × the LD50) challenge after a single i.n. immunization with 107 IFU of AdPA83, the most immunogenic vaccine construct, per mouse (Vaxin, Inc., unpublished data). To improve the potency of Ad5-vectored anthrax vaccines, codon optimization of PA and LF genes and fusion of the tPA leader sequence approaches were applied to generate AdtPA83hu, AdtLFnhu, and AdPA83hu. The relative immunogenicities among these Ad5 vectors encoding codon-optimized and non-codon-optimized PA and LF were then assessed by i.n. vaccination of groups A/J mice (10 mice per group) with 107 IFU of AdPA83, AdPA83hu, AdtPA83hu, AdmLF7, and AdtLFnhu, respectively, per mouse. A recombinant Ad5 vector (Adtetc encoding tetanus C fragment) served as an Ad5 vector control. Analysis of the sera by ELISA showed that the geometric mean titers of anti-PA IgG antibody induced by AdPA83hu and AdtPA83hu were 45.3 and 68.6 times that induced by AdPA83 (P < 0.001 for both AdPA83hu versus AdPA83 and AdtPA83hu versus AdPA83; P > 0.05 for AdtPA83hu versus AdPA83hu) (Fig. 1A). The geometric mean titers of anti-LF IgG antibody stimulated by AdtLFnhu were 4.0 times that induced by AdmLF7 after 4 weeks with a single i.n. administration (Fig. 1B). To determine the functionality of antibodies to PA and LF elicited by the immunization, the abilities of sera to protect mouse macrophage cells from Letx mediated lysis were measured. As shown in Fig. 1C, the highest anti-Letx antibody titers were detected in mice immunized with AdtPA83hu. Both AdtPA83hu and AdPA83hu could induce significantly higher anti-Letx antibody titers than did AdPA83 (P < 0.001 for both AdPA83hu versus AdPA83 and AdtPA83hu versus AdPA83; P > 0.05 AdtPA83hu versus AdPA83hu). Furthermore, the anti-LF antibodies elicited by both AdtLFnhu and AdmLF7 were able to inhibit the cytotoxic effects of Letx (Fig. 1C). To test the effectiveness of Ad5-vectored anthrax vaccines with regard to protection against anthrax infection, immunized mice were challenged with 50× LD50 B. anthracis Sterne spores after 4 weeks vaccination (Fig. 1D). All mice receiving the control Adtetc died within 6 days, and 100% of the mice vaccinated with AdPA83hu and AdtPA83hu survived the spore challenge. Protection was also achieved in 70, 30, and 40% of the mice vaccinated with AdPA83, AdmLF7, and AdtLFnhu, respectively (P > 0.05 for both AdPA83hu versus AdPA83 and AdtPA83hu versus AdPA83; P < 0.001 for both AdPA83 versus Adtetc and AdtLFnhu versus Adtetc; P < 0.05 AdmLF7 versus Adtetc). These results indicate that optimization of codon usage improved the protection potency of an AdVAV and fusion with the tPA leader sequence may further enhance its immunogenicity.
Fig 1.
Comparison of immune responses in A/J mice induced by Ad5 vectors encode codon-optimized and non-codon-optimized PA or LF genes. (A to C) Anti-PA IgG ELISA titer (A), anti-LF IgG ELISA titer (B), and anti-Letx neutralizing antibody titer (C) in mouse serum were compared 4 weeks after a single i.n. immunization with AdPA83 (PA), AdPA83hu (PAhu), AdtPA83hu (tPAhu), AdmLF7 (mLF7), and AdtLFnhu (tLFnhu) at a dose of 107 IFU per vector. All mice immunized with Adtetc control vectors and all preimmune sera had anti-PA or anti-LF IgG ELISA titers of ≤100 and had anti-Letx neutralizing antibody titers of <8. (D) Survival of vaccinated A/J mice against a 50× LD50 B. anthracis Sterne spore challenge. The results of anti-PA and anti-LF IgG ELISAs and anti-Letx neutralizing assays are plotted as the log10 titers. Bars are geometric mean of the anti-PA and anti-LF ELISA titers or the anti-Letx neutralizing antibody titers.
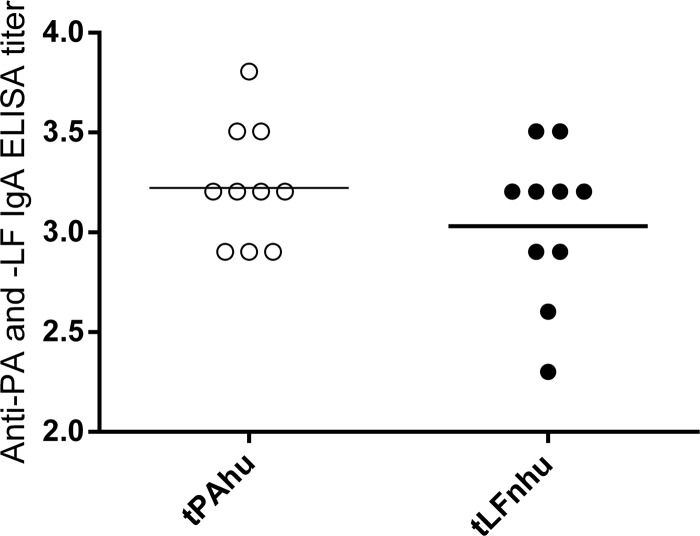
Intranasal vaccination with Ad5-vectored anthrax vaccines induces secretory IgA antibodies.
Intranasal vaccination is an effective approach for optimal protection of mucosal surfaces by inducing mucosal and systemic immunity. To test the feasibility of AdVAVs for induction of mucosal immunity, groups of A/J mice (10 mice per group) were immunized with 107 IFU of AdtPA83hu, AdtLFnhu, or Adtetc/mouse. Mouse BAL samples from immunized mice were collected at 4 weeks postvaccination and assessed by ELISA. As shown in Fig. 2, strong anti-PA and anti-LF secretory IgA antibodies were induced by AdtPA83hu and AdtLFnhu, respectively (Fig. 2).
Fig 2.
Anti-PA and anti-LF IgA ELISA titers in the BAL fluid were measured 4 weeks after a single i.n. immunization with AdtPA83hu (tPAhu) or AdtLFnhu (tLFnhu) at a dose of 107 IFU per vector. All mice immunized with Adtetc vector controls and all preimmune sera had anti-PA and anti-LF IgA ELISA titers of ≤100. The results of anti-PA and anti-LF IgA ELISAs are plotted as the log10 titers. Bars are geometric means of the anti-PA or anti-LF ELISA titers.
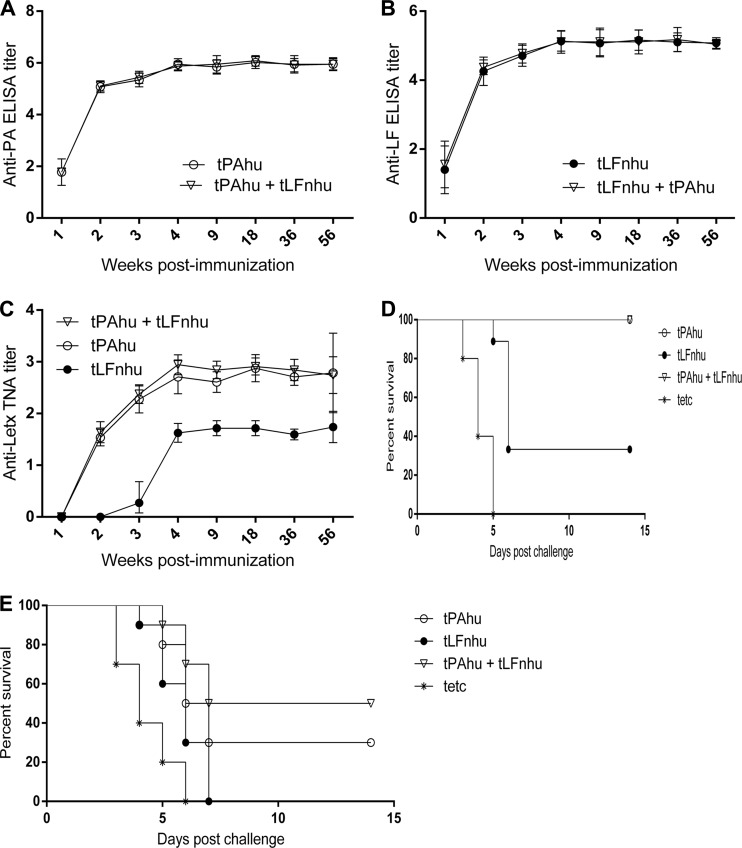
Intranasal immunization of Ad-vectored anthrax vaccines elicits partial protective immunity within 2 weeks, and the robust immunity lasts at least 1 year.
To determine the kinetics and durability of the immune response, groups of A/J mice (10 mice per group) with a single i.n. administration of 107 IFU of AdtPA83hu, AdtLFnhu, or both/mouse were evaluated. Significant levels of anti-PA IgG antibody (Fig. 3A), anti-LF IgG antibody (Fig. 3B), and anti-Letx antibody (Fig. 3C) were detected after 2 weeks immunization, and the antibody titers increased and peaked around week 4 and remained unchanged to the time of spore challenge at week 56 (P > 0.05 for the anti-Letx antibody titers at 4 weeks postvaccination versus the anti-Letx antibody titers at 56 weeks postvaccination in animals immunized with AdtPA83hu, AdtLFnhu, or both). All animals vaccinated with AdtPA83hu and AdtPA83hu+AdtLFnhu and three of nine mice immunized only with AdtLFnhu survived the challenge (Fig. 3D). To determine the onset of protective immunity, groups of A/J mice were challenged 2 weeks after vaccination (Fig. 3E). Thirty percent in the AdtPA83hu-immunized group and 50% in the AdtPA83hu+AdtLFnhu-vaccinated group survived (P < 0.001 for both AdtPA83hu versus Adtetc and AdtPA83hu+AdtLFnhu versus Adtetc). All mice receiving Adtetc or AdtLFnhu alone died after spore challenge. However, the mean time to death (MTD) was 4.8 days for mice immunized with AdtLFnhu, while the MTD for Adtetc-immunized control mice was 3.3 days (P < 0.05). Our findings demonstrate that a single i.n. vaccination with an AdVAV can provide rapid and long-term protection against a lethal challenge of B. anthracis spores. The anti-LF immune responses induced by AdtLFnhu increase the anti-Letx antibody titers minimally and enhanced the protective immunity induced by AdtPA83hu (Fig. 3C and E), although the differences between AdtLFnhu+AdtPA83hu and AdtPA83hu alone were not statistically significant.
Fig 3.
Kinetics of immune responses in A/J mice. (A to C) The anti-PA IgG ELISA titer (A), anti-LF IgG ELISA titer (B), and anti-Letx neutralizing antibody titer (C) in mouse serum were measured at the indicated time points after a single i.n. immunization with 107 IFU of AdtPA83hu (tPAhu), 107 IFU of AdtLFnhu (tLFnhu), or 107 IFU of AdtPA83hu plus 107 IFU of AdtLF4hu (tPAhu+tLFnhu). All mice immunized with 107 IFU of Adtetc vectors and all preimmune sera had anti-PA and anti-LF IgG ELISA titers of ≤100 and had anti-Letx neutralizing antibody titers of <8. The results of anti-PA and anti-LF IgG ELISAs and anti-Letx neutralizing assays are plotted as the log10 titers. All of the data are shown as geometric means with 95% confidence intervals of 8 to 10 mice per group. (D and E) Protection of A/J mice against a 50× LD50 B. anthracis Sterne spore challenge at 2 weeks (E) and 56 weeks (D) postimmunization.
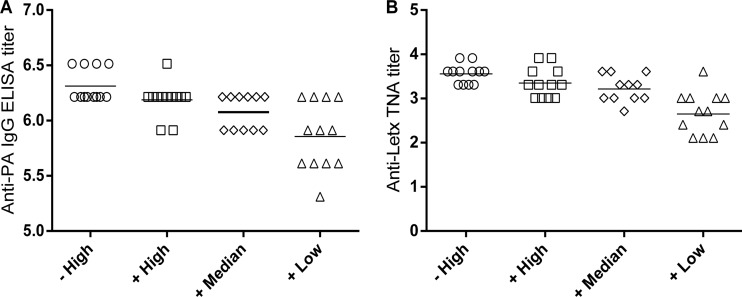
Preexisting immunity to Ad5 did not impair the potency of an Ad-vectored nasal anthrax vaccine.
To determine the effect of preexisting anti-Ad5 immunity on i.n. vaccination of an AdVAV, A/J mice (12 animals per group) were primed by i.n. installation with 107 IFU of wt Ad5/mouse or control buffer on day 0. On day 14, serum anti-Ad5 neutralizing antibody titers ranging from 1:32 to 1:256 (with a geometric mean at 1:57) were detected in mice primed with wt Ad5 on day 0. These mice were i.n. immunized with 108 IFU of AdtPA83hu/mouse plus 5.4 × 106 IFU of AdmInhAhu/mouse (an Ad5 vector encoding B. anthracis immune inhibitor A gene) (high dose), 107 IFU of AdtPA83hu/mouse plus 5.4 × 105 IFU of AdmInhAhu/mouse (median dose), 106 IFU of AdtPA83hu/mouse plus 5.4 × 104 IFU of AdmInhAhu/mouse (low dose) on day 14. One group of mice without wt Ad5 priming were immunized with 108 IFU of AdtPA83hu plus 5.4 × 106 IFU of AdmInhAhu (high dose) as controls. Although vaccination of mice without wt Ad5 priming produced slightly higher anti-PA IgG and anti-Letx antibody titers, the differences between two groups (high dose) were not statistically significant (P > 0.05 for both anti-PA IgG and anti-Letx antibody titers) (Fig. 4). All of the mice immunized with AdthuPA83 plus AdmInhAhu with or without wt Ad5 priming were protected against a 50× LD50 B. anthracis Sterne spore challenge. All animals in control groups succumbed to the anthrax spore challenge (Table 1). These results demonstrated that animals possessing high levels of antibodies against Ad5 can be effectively vaccinated against anthrax with an i.n. AdVAV.
Fig 4.
Immunogenicity of Ad-vectored nasal anthrax vaccines in the presence of preexisting anti-Ad5 vector immunity. The A/J mice were first i.n. inoculated with 107 IFU of wt Ad5 per mouse and then after 2 weeks were i.n. immunized with 108 IFU of AdtPA83hu plus 5.4 × 106 IFU of AdmInhAhu (+High), 107 IFU of AdtPA83hu plus 5.4 × 105 IFU of AdmInhAhu (+Median), or 106 IFU of AdtPA83hu plus 5.4 × 104 IFU of AdmInhAhu (+Low). One group of mice without Ad5 priming were immunized with108 IFU of AdtPA83hu plus 5.4 × 106 IFU of AdmInhAhu (−High) as controls. Anti-PA IgG ELISA titers (A) and anti-Letx neutralizing antibody titers (B) were determined at 4 weeks postimmunization. The results of the anti-PA IgG ELISAs and anti-Letx neutralizing assays are plotted as log10 titers. Bars indicate geometric means of the anti-PA ELISA titers or anti-Letx neutralizing antibody titers.
Table 1.
Protection of immunized mice with or without wt Ad5 priming against a lethal-dose anthrax spore challengea
| Group | No. of animals/group | Vector/buffer | Dose/animal | Ad5 priming | No. of survivors/no. of animals tested |
|---|---|---|---|---|---|
| 1 | 12 | AdtPA83hu + AdmInhAhu | High dose | – | 12/12 |
| 2 | 12 | A195 buffer | None | – | 0/12 |
| 3 | 12 | AdtPA83hu + AdmInhAhu | High dose | + | 12/12 |
| 4 | 11b | AdtPA83hu + AdmInhAhu | Median dose | + | 11/11 |
| 5 | 12 | AdtPA83hu + AdmInhAhu | Low dose | + | 12/12 |
| 6 | 12 | AdmInhAhu | 108 IFU | – | 0/12 |
| 7 | 12 | A195 buffer | None | + | 0/12 |
| 8 | 12 | Naive control | None | – | 0/12 |
High dose, 108 IFU of AdtPA83hu/mouse plus 5.4 × 106 IFU of AdmInhAhu/mouse; median dose, 107 IFU of AdtPA83hu/mouse plus 5.4 × 105 IFU of AdmInhAhu/mouse; low dose, 106 IFU of AdtPA83hu/mouse plus 5.4 × 105 IFU of AdmInhAhu/mouse; none, no AdtPA83hu and AdmInhAhu treatment.
Lost one animal without replacement.
DISCUSSION
To develop the next generation of safe and effective anthrax vaccines, it is crucial that the vaccine can induce rapid and sustained protective immunity in a single-dose regimen with no adverse side effects. Manufacturing, distribution, and administration must be rapid, easy, and economical. To address these requirements, several AdVAVs expressing PA or LF proteins were tested. Certain attributes of Ad5 vectors make them attractive for use as nasal vaccine platforms. (i) Replication-competent adenovirus (RCA)-free Ad5-vectored vaccines can be manufactured in PER.C6 cells quickly using disposable manufacturing technologies (17, 18, 22). (ii) Novel formulations allow Ad5-vectored vaccines to be stored in liquid buffer (19) or as lyophilized dry powder (23) at 4°C for at least a year and newly developed thermostabilization techniques allow Ad5 vectors to be stored at room temperature up to 45°C for 6 months with minimal declining infectivity (24). (iii) Ad5-vectored vaccines may be self-administered with a spray in an emergency event.
In research for new anthrax vaccines, numerous DNA constructs and viral vectors encoding codon-optimized or non-codon-optimized anthrax immunogens have been tested in anthrax vaccine studies, but the protective efficacies as vaccine candidates have not been compared in a same system. In the present study, we compared the relative levels of serum antigen-specific antibody titers and anti-Letx neutralizing antibody titers, as well as the strength of protective immunity induced by Ad5 vectors encoding codon-optimized or non-codon-optimized PA and LF genes in the A/J mouse model. Our results suggest that codon optimization of anthrax immunogens can enhance the humoral immune response of an AdVAV (Fig. 1), although the levels of protection against a lethal spore challenge among the AdPA83, AdPA83hu, and AdtPA83hu groups were not statistically significant in this particular experiment (Fig. 1D).
We demonstrated here that 100% of A/J mice can be protected from a lethal anthrax spore challenge after a single-dose i.n. vaccination with AdtPA83hu vectors (Fig. 1D and 3D). The duration of immunity with AdtPA83hu and/or AdtLFnhu has been measured in mice with demonstrable high serum anti-Letx antibody titers and antigen specific IgG titers that persist for at least 1 year (Fig. 3A to C). Moreover, partial protective immune responses can be rapidly generated within 2 weeks (Fig. 3E). These results are consistent with previous reports that Ad5-vectored vaccines could provide rapid and sustained protective immunity (11, 12, 25–28).
There is compelling evidence that the upper respiratory tract and other mucosal tissues are early targets of inhalational anthrax spore infection (29–31). A nasal anthrax vaccine that potentially induces both systemic and respiratory mucosal immune responses may be a favorable candidate against inhalational anthrax (32–34). Nasal delivery of an Ad5-vectored human immunodeficiency virus vaccine induced stronger mucosal immunity (35), and a nasal Ad5-vectored vaccine provided better protection against airway Mycobacterium tuberculosis than intramuscularly injected Ad5-vectored vaccines (36). In contrast to vaccines requiring artificial adjuvants and multiple immunizations for inducing sufficient mucosal immunity, an AdVAV can provide self-adjuvanting activity (37) capable of eliciting high titers of secreted IgA in animals after single-dose administration (Fig. 2). In addition, i.n. Ad5-vectored vaccines can also induce strong cell-mediated immunity (38, 39). It would be interesting to test whether an AdVAV can elicit cellular immune responses that may be beneficial in combating early infection when spores are engulfed by pulmonary phagocytes.
Studies by us and others indicate that administration of Ad5-vectored vaccines via the i.n. route might overcome preexisting immunity against the Ad5 vector (14, 40–42). In the present study, we demonstrated that an AdVAV, administered i.n. 2 weeks after priming with wt Ad5, could effectively immunize A/J mice (Fig. 4). Additional nonclinical and clinical information is needed to clarify the influence of the preexisting Ad5 immunity and to confirm the suitability of an i.n. AdVAV for human use.
Anthrax vaccines that can induce immune responses against both PA and an additional component such as PGA (43), LF (21), or Bacillus collagen-like protein of anthracis (BclA) (44) may be more effective against anthrax than the vaccines based on PA alone. Consistent with previous reports (21, 45), we observed that immune responses to LF alone could provide partial protection against a lethal anthrax spore challenge (Fig. 1D and 3D). Our study also suggested that multivalent AdVAVs could be mixed and delivered simultaneously (Fig. 3C and E). Additional testing to determine whether Ad5-vectored anthrax vaccines encoding PA and additional components would provide better protection against anthrax by targeting the early stages of spore infection as well as the toxins produced by the vegetative bacilli is warranted.
In summary, the data presented here show that (i) i.n. AdVAV can induce both systemic and mucosa immunity responses, (ii) i.n. immunization with AdtPA83hu provides full protection in vaccinated A/J mice against a lethal anthrax spore challenge, (iii) a single dose of AdVAV can elicit rapid and sustained protective immunity, (iv) AdVAV can effectively immunize A/J mice in the presence of preexisting immunity to Ad5, and (v) AdVAV has merit for further studies in the search a new and improved vaccine against aerosolized anthrax spores.
ACKNOWLEDGMENTS
This study was supported in part by the National Institutes of Health (1-UC1-AI067198-01).
We thank Megan Lallier and Robert Davenport for their outstanding technical assistance, Darrell Galloway and Charles Turnbough for providing plasmids, and Bo Andersen and Vyjayanthi Krishnan for critical review of the manuscript. We also thank the Battelle Memorial Institute and University of Alabama at Birmingham for providing facilities for animal testing, as well as Crucell Holland BV for providing the PER.C6 cell line, and Medicine BioServices, Inc., for providing contaminant-free HEK293 cells.
Footnotes
Published ahead of print 24 October 2012
REFERENCES
- 1. Baillie LW. 2009. Is new always better than old?: the development of human vaccines for anthrax. Hum. Vaccin. 5:806–812 [DOI] [PubMed] [Google Scholar]
- 2. Inglesby TV, O'Toole T, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Friedlander AM, Gerberding J, Hauer J, Hughes J, McDade J, Osterholm MT, Parker G, Perl TM, Russell PK, Tonat K, Working Group on Civilian Biodefense. 2002. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA 287:2236–2252 [DOI] [PubMed] [Google Scholar]
- 3. Green BD, Battisti L, Koehler TM, Thorne CB, Ivins BE. 1985. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 49:291–297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moayeri M, Leppla SH. 2009. Cellular and systemic effects of anthrax lethal toxin and edema toxin. Mol. Aspects Med. 30:439–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Friedlander AM, Welkos SL, Pitt ML, Ezzell JW, Worsham PL, Rose KJ, Ivins BE, Lowe JR, Howe GB, Mikesell P, Lawrence WB. 1993. Postexposure prophylaxis against experimental inhalation anthrax. J. Infect. Dis. 167:1239–1243 [DOI] [PubMed] [Google Scholar]
- 6. Henderson DW, Peacock S, Belton FC. 1956. Observations on the prophylaxis of experimental pulmonary anthrax in the monkey. J. Hyg. (Lond.) 54:28–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Little S. 2005. Anthrax vaccines: a development update. BioDrugs 19:233–245 [DOI] [PubMed] [Google Scholar]
- 8. Wright JG, Quinn CP, Shadomy S, Messonnier N, Centers for Disease Control and Prevention. 2010. Use of anthrax vaccine in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR Recomm. Rep. 59:1–30 [PubMed] [Google Scholar]
- 9. Fellows PF, Linscott MK, Ivins BE, Pitt ML, Rossi CA, Gibbs PH, Friedlander AM. 2001. Efficacy of a human anthrax vaccine in guinea pigs, rabbits, and rhesus macaques against challenge by Bacillus anthracis isolates of diverse geographical origin. Vaccine 19:3241–3247 [DOI] [PubMed] [Google Scholar]
- 10. Langley WA, Bradley KC, Li ZN, Smith ME, Schnell MJ, Steinhauer DA. 2010. Induction of neutralizing antibody responses to anthrax protective antigen by using influenza virus vectors: implications for disparate immune system priming pathways. J. Virol. 84:8300–8307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McConnell MJ, Hanna PC, Imperiale MJ. 2007. Adenovirus-based prime-boost immunization for rapid vaccination against anthrax. Mol. Ther. 15:203–210 [DOI] [PubMed] [Google Scholar]
- 12. Santra S, Seaman MS, Xu L, Barouch DH, Lord CI, Lifton MA, Gorgone DA, Beaudry KR, Svehla K, Welcher B, Chakrabarti BK, Huang Y, Yang ZY, Mascola JR, Nabel GJ, Letvin NL. 2005. Replication-defective adenovirus serotype 5 vectors elicit durable cellular and humoral immune responses in nonhuman primates. J. Virol. 79:6512–6522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shi Z, Zeng M, Yang G, Siegel F, Cain LJ, van Kampen KR, Elmets CA, Tang DC. 2001. Protection against tetanus by needle-free inoculation of adenovirus-vectored nasal and epicutaneous vaccines. J. Virol. 75:11474–11482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Van Kampen KR, Shi Z, Gao P, Zhang J, Foster KW, Chen DT, Marks D, Elmets CA, Tang DC. 2005. Safety and immunogenicity of adenovirus-vectored nasal and epicutaneous influenza vaccines in humans. Vaccine 23:1029–1036 [DOI] [PubMed] [Google Scholar]
- 15. Arora N, Klimpel KR, Singh Y, Leppla SH. 1992. Fusions of anthrax toxin lethal factor to the ADP-ribosylation domain of Pseudomonas exotoxin A are potent cytotoxins which are translocated to the cytosol of mammalian cells. J. Biol. Chem. 267:15542–15548 [PubMed] [Google Scholar]
- 16. Klimpel KR, Arora N, Leppla SH. 1994. Anthrax toxin lethal factor contains a zinc metalloprotease consensus sequence which is required for lethal toxin activity. Mol. Microbiol. 13:1093–1100 [DOI] [PubMed] [Google Scholar]
- 17. Fallaux FJ, Bout A, van der Velde I, van den Wollenberg DJ, Hehir KM, Keegan J, Auger C, Cramer SJ, van Ormondt H, van der Eb AJ, Valerio D, Hoeben RC. 1998. New helper cells and matched early region 1-deleted adenovirus vectors prevent generation of replication-competent adenoviruses. Hum. Gene Ther. 9:1909–1917 [DOI] [PubMed] [Google Scholar]
- 18. Tang DC, Zhang J, Toro H, Shi Z, Van Kampen KR. 2009. Adenovirus as a carrier for the development of influenza virus-free avian influenza vaccines. Expert Rev. Vaccines 8:469–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Evans RK, Nawrocki DK, Isopi LA, Williams DM, Casimiro DR, Chin S, Chen M, Zhu DM, Shiver JW, Volkin DB. 2004. Development of stable liquid formulations for adenovirus-based vaccines. J. Pharm. Sci. 93:2458–2475 [DOI] [PubMed] [Google Scholar]
- 20. Zhang J, Shi Z, Kong FK, Jex E, Huang Z, Watt JM, Van Kampen KR, Tang DC. 2006. Topical application of Escherichia coli-vectored vaccine as a simple method for eliciting protective immunity. 2006. Topical application of Escherichia coli-vectored vaccine as a simple method for eliciting protective immunity. Infect Immun. 174:3607–3617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Price BM, Liner AL, Park S, Leppla SH, Mateczun A, Galloway DR. 2001. Protection against anthrax lethal toxin challenge by genetic immunization with a plasmid encoding the lethal factor protein. Infect. Immun. 69:4509–4515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Berdichevsky M, Gentile MP, Hughes B, Meis P, Peltier J, Blumentals I, Auniņs J, Altaras NE. 2008. Establishment of higher passage PER.C6 cells for adenovirus manufacture. Biotechnol. Prog. 24:158–165 [DOI] [PubMed] [Google Scholar]
- 23. Croyle MA, Cheng X, Wilson JM. 2001. Development of formulations that enhance physical stability of viral vectors for gene therapy. Gene Ther. 8:1281–1290 [DOI] [PubMed] [Google Scholar]
- 24. Alcock R, Cottingham MG, Rollier CS, Furze J, De Costa SD, Hanlon M, Spencer AJ, Honeycutt JD, Wyllie DH, Gilbert SC, Bregu M, Hill AV. 2010. Long-term thermostabilization of live poxviral and adenoviral vaccine vectors at supraphysiological temperatures in carbohydrate glass. Sci. Transl. Med. 2:19ra12. [DOI] [PubMed] [Google Scholar]
- 25. Fernández E, Toledo JR, Chiong M, Parra F, Rodríguez E, Montero C, Méndez L, Capucci L, Farnós O. 2011. Single dose adenovirus vectored vaccine induces a potent and long-lasting immune response against rabbit hemorrhagic disease virus after parenteral or mucosal administration. Vet. Immunol. Immunopathol. 142:179–188 [DOI] [PubMed] [Google Scholar]
- 26. Holst PJ, Bartholdy C, Stryhn A, Thomsen AR, Christensen JP. 2007. Rapid and sustained CD4+ T-cell-independent immunity from adenovirus-encoded vaccine antigens. J. Gen. Virol. 88:1708–1716 [DOI] [PubMed] [Google Scholar]
- 27. Hu RL, Liu Y, Zhang SF, Zhang F, Fooks AR. 2007. Experimental immunization of cats with a recombinant rabies-canine adenovirus vaccine elicits a long-lasting neutralizing antibody response against rabies. Vaccine 25:5301–5307 [DOI] [PubMed] [Google Scholar]
- 28. Tan Y, Hackett NR, Boyer JL, Crystal RG. 2003. Protective immunity evoked against anthrax lethal toxin after a single intramuscular administration of an adenovirus-based vaccine encoding humanized protective antigen. Hum. Gene Ther. 14:1673–1682 [DOI] [PubMed] [Google Scholar]
- 29. Cleret A, Quesnel-Hellmann A, Vallon-Eberhard A, Verrier B, Jung S, Vidal D, Mathieu J, Tournier JN. 2007. Lung dendritic cells rapidly mediate anthrax spore entry through the pulmonary route. J. Immunol. 178:7994–8001 [DOI] [PubMed] [Google Scholar]
- 30. Glomski IJ, Piris-Gimenez A, Huerre M, Mock M, Goossens PL. 2007. Primary involvement of pharynx and Peyer's patch in inhalational and intestinal anthrax. PLoS Pathog. 3:e76 doi:10.1371/journal.ppat.0030076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Russell BH, Vasan R, Keene DR, Koehler TM, Xu Y. 2008. Potential dissemination of Bacillus anthracis utilizing human lung epithelial cells. Cell Microbiol. 10:945–957 [DOI] [PubMed] [Google Scholar]
- 32. Flick-Smith HC, Eyles JE, Hebdon R, Waters EL, Beedham RJ, Stagg TJ, Miller J, Alpar HO, Baillie LW, Williamson ED. 2002. Mucosal or parenteral administration of microsphere-associated Bacillus anthracis protective antigen protects against anthrax infection in mice. Infect. Immun. 70:2022–2028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Huang J, Mikszta JA, Ferriter MS, Jiang G, Harvey NG, Dyas B, Roy CJ, Ulrich RG, Sullivan VJ. 2007. Intranasal administration of dry powder anthrax vaccine provides protection against lethal aerosol spore challenge. Hum. Vaccin. 3:90–93 [DOI] [PubMed] [Google Scholar]
- 34. Mikszta JA, Sullivan VJ, Dean C, Waterston AM, Alarcon JB, Dekker JP, 3rd, Brittingham JM, Huang J, Hwang CR, Ferriter M, Jiang G, Mar K, Saikh KU, Stiles BG, Roy CJ, Ulrich RG, Harvey NG. 2005. Protective immunization against inhalational anthrax: a comparison of minimally invasive delivery platforms. J. Infect. Dis. 191:278–288 [DOI] [PubMed] [Google Scholar]
- 35. Lemiale F, Kong WP, Akyürek LM, Ling X, Huang Y, Chakrabarti BK, Eckhaus M, Nabel GJ. 2003. Enhanced mucosal immunoglobulin A response of intranasal adenoviral vector human immunodeficiency virus vaccine and localization in the central nervous system. J. Virol. 77:10078–10087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wang J, Thorson L, Stokes RW, Santosuosso M, Huygen K, Zganiacz A, Hitt M, Xing Z. 2004. Single mucosal, but not parenteral, immunization with recombinant adenoviral-based vaccine provides potent protection from pulmonary tuberculosis. J. Immunol. 173:6357–6365 [DOI] [PubMed] [Google Scholar]
- 37. Molinier-Frenkel V, Lengagne R, Gaden F, Hong SS, Choppin J, Gahery-Ségard H, Boulanger P, Guillet JG. 2002. Adenovirus hexon protein is a potent adjuvant for activation of a cellular immune response. J. Virol. 76:127–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jones FR, Gabitzsch ES, Xu Y, Balint JP, Borisevich V, Smith J, Smith J, Peng BH, Walker A, Salazar M, Paessler S. 2011. Prevention of influenza virus shedding and protection from lethal H1N1 challenge using a consensus 2009 H1N1 HA and NA adenovirus vector vaccine. Vaccine 29:7020–7026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Patel A, Zhang Y, Croyle M, Tran K, Gray M, Strong J, Feldmann H, Wilson JM, Kobinger GP. 2007. Mucosal delivery of adenovirus-based vaccine protects against Ebola virus infection in mice. J. Infect. Dis. 2:S413–420 [DOI] [PubMed] [Google Scholar]
- 40. Croyle MA, Patel A, Tran KN, Gray M, Zhang Y, Strong JE, Feldmann H, Kobinger GP. 2008. Nasal delivery of an adenovirus-based vaccine bypasses preexisting immunity to the vaccine carrier and improves the immune response in mice. PLoS One 3:e3548 doi:10.1371/journal.pone.0003548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Xu Q, Pichichero ME, Simpson LL, Elias M, Smith LA, Zeng M. 2009. An adenoviral vector-based mucosal vaccine is effective in protection against botulism. Gene Ther. 16:367–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Yu JR, Kim S, Lee JB, Chang J. 2008. Single intranasal immunization with recombinant adenovirus-based vaccine induces protective immunity against respiratory syncytial virus infection. J. Virol. 82:2350–2357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rhie GE, Roehrl MH, Mourez M, Collier RJ, Mekalanos JJ, Wang JY. 2003. A dually active anthrax vaccine that confers protection against both bacilli and toxins. Proc. Natl. Acad. Sci. U. S. A. 100:10925–10930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hahn UK, Boehm R, Beyer W. 2006. DNA vaccination against anthrax in mice-combination of anti-spore and anti-toxin components. Vaccine 24:4569–4571 [DOI] [PubMed] [Google Scholar]
- 45. Hermanson G, Whitlow V, Parker S, Tonsky K, Rusalov D, Ferrari M, Lalor P, Komai M, Mere R, Bell M, Brenneman K, Mateczun A, Evans T, Kaslow D, Galloway D, Hobart P. 2004. A cationic lipid-formulated plasmid DNA vaccine confers sustained antibody-mediated protection against aerosolized anthrax spores. Proc. Natl. Acad. Sci. U. S. A. 101:13601–13606 [DOI] [PMC free article] [PubMed] [Google Scholar]