Abstract
In an effort to develop a sustainable platform for manufacturing protein-based vaccine candidates, we expressed a triple mutant of staphylococcal enterotoxin B carrying the L45R, Y89A, and Y94A modifications in transgenic soybean seeds (soy-mSEB). Soy-mSEB possessed no detectable superantigen activity in vitro. We found that this soybean-derived, nontoxic mutant of SEB could be stably expressed, stored in seeds for extended periods at room temperature without degradation, and easily purified from contaminating soy proteins. Vaccination of pigs with purified soy-mSEB, or the identical triple mutant expressed in Escherichia coli (E. coli-mSEB), resulted in high antibody titers against the native toxin in immunized animals. In fact, titers were indistinguishable regardless of the immunogen used, demonstrating the equivalence of soy-mSEB and E. coli-mSEB vaccinations. Antisera from either immunized group were able to block native SEB superantigen activity in an in vitro neutralization assay. Similar results were obtained when immunized animals were challenged with a sublethal dose of native toxin. Significant reductions in toxin-induced serum cytokine levels were observed in soy-mSEB- and E. coli-mSEB-immunized pigs compared to control animals. The reductions in SEB-induced cytokine responses were similar regardless of the immunogen used for vaccination. Surprisingly, however, some clinical symptoms, such as prostration, lethargy, emesis, and/or diarrhea, were still observed in all immunized animals. These studies demonstrate the potential for soybean-derived proteins as a platform technology for sustainable vaccine manufacturing and the usefulness of a sublethal challenge model in pigs for evaluating the efficacy of potential SEB vaccine candidates.
INTRODUCTION
Staphylococcal enterotoxin B (SEB) is among the most potent of the Staphylococcus aureus exotoxins (1). This superantigen-like toxin mediates its pathological effects by linking major histocompatibility complex (MHC) class II molecules with T cell receptors outside the antigen binding site (2, 3). One result of this toxin-induced T lymphocyte activation is the overproduction of certain cytokines which contribute to the clinical symptoms of SEB-induced toxicity and shock (4). Such symptoms include anorexia, nausea, vomiting, and diarrhea, which may present with hypotension, tachycardia, and hyperperistalsis. The most common natural exposure to SEB is through ingestion of contaminated foods (5).
The ability of ingested SEB to survive passage through the gastrointestinal tract and cause disease demonstrates the inherent stability of this protein's structure (3). Two tightly compacted domains contribute to SEB's durability as a native or recombinant protein (3, 6). Unfortunately, the potency of this toxin, coupled with its stable structure, makes it a prime candidate for possible use as an agent of biowarfare (7, 8) or bioterrorism (9). Successful weaponization of SEB as an aerosolized biological warfare agent was achieved in the 1960s (7, 8, 10). Militarily, weaponized SEB was considered an incapacitating agent, with mild exposure resulting in shortness of breath, chest pain, and some tachycardia (8, 10, 11). More extensive exposure could result in significant pulmonary edema, neurological symptoms, and a respiratory distress-like syndrome. With supportive medical intervention, death following inhalation was not very common. However, symptoms could linger for up to 2 weeks following exposure, in keeping with the goal of incapacitation (8, 10). For these reasons, SEB has been characterized as one of the “two most important toxin threats on the battlefield or in bioterrorism” (9). Therefore, the availability of an efficacious anti-SEB treatment for use by the military or other at-risk populations would represent a significant deterrent for those considering the use of SEB to induce injury.
Unfortunately, prophylactic or therapeutic treatments for this potential threat have yet to be developed. Monoclonal antibodies against SEB have been generated, and they demonstrate protection in mouse models of toxin-induced death (12–15). However, passive administration of such antibodies in human subjects would need to occur before or soon after toxin exposure, since the effects of inhaled SEB can be felt within minutes to hours (8, 11). Active immunization against modified or mutant SEB proteins has also been attempted. Toxoid-based formalin-inactivated SEB vaccination was not reproducibly protective (16). More recently, engineered, nontoxic mutant forms of SEB have been investigated for the ability to induce protective immune responses (17–19). In particular, a triple mutant carrying L45R, Y89A, and Y94A modifications was expressed as a recombinant protein in Escherichia coli (E. coli-mSEB) (19). This nontoxic mutant was subsequently shown to induce immunity in mice (18, 19) and nonhuman primates (17, 19) and to protect these animals from death after challenge with wild-type SEB. Phase I clinical trials for this potential vaccine candidate, designated STEBVax, are pending.
In an effort to develop a sustainable platform for manufacturing protein-based vaccine candidates, we expressed the same triple mutant (19) carrying L45R, Y89A, and Y94A modifications in transgenic soybean seeds. We found that this soybean-derived, nontoxic mutant of SEB (soy-mSEB) could be stably expressed, stored in seeds for extended periods at room temperature, and purified from contaminating soy proteins in rapid fashion.
To test the efficacy of vaccination with soy-mSEB, we developed a sublethal challenge model in pigs. Weaponized SEB is an incapacitating agent, yet animal models (17–19) have routinely relied on death as an endpoint following exposure to extremely high doses of toxin. Since native SEB functions as a superantigen in pigs, it was possible to define an SEB dose which induced incapacitation, but not death, as a more sensitive endpoint for evaluating soy-mSEB and E. coli-mSEB as candidate vaccines. Following vaccination of pigs with these immunogens, high anti-SEB antibody titers and a reduction in the SEB-induced cytokine response were observed following challenge with a sublethal dose of toxin. Antibody titers and reductions in the SEB-induced cytokine response mediated by soy-mSEB vaccination in pigs were indistinguishable from those observed following vaccination with E. coli-mSEB. Taken together, these studies demonstrate the potential for soybean-derived proteins as a platform technology for sustainable vaccine manufacturing and show that the sublethal challenge model in pigs is useful for evaluating the efficacy of potential SEB vaccine candidates.
MATERIALS AND METHODS
Animals.
All animal procedures were approved by the Institutional Animal Care and Use Committee at North Carolina State University. Sixteen male crossbred piglets (18 days of age) were obtained from the North Carolina State University Swine Education Unit and group housed (n = 8/pen) in 1.8-m by 1.8-m pens. Pigs were maintained under controlled lighting (15-hour light and 9-hour dark cycle) and temperature (20.5 ± 0.75°C) conditions. Pigs had ad libitum access to water and a typical nursery pig diet that met or exceeded their nutrient requirements (20). Pigs were allowed to adjust to their new surroundings for 1 week and then were randomly assigned to one of three immunization groups (n = 4 to 6 pigs/group). Body weights were recorded on days 0, 1, 2, 3, 7, 8, 9, 10, 14, 15, 16, 17, 25, and 36. Piglets were fed a milk replacer liquid diet (Milk Specialties Company, Carpentersville, IL) each morning, afternoon, and evening for the 30 days. Feed amounts and feed weigh-back amounts were recorded at each feeding. After the final vaccination, piglets were switched to a dry pelleted feed (Ralco Nutrition, Marshall, MN) and had access to feed and water ad libitum.
Expression of mutant SEB (L45R/Y89A/Y94A) in transgenic soybean seeds (soy-mSEB).
A plant codon-optimized mutant SEB sequence was used to create a binary vector, using methods similar to those previously described (21–24). The encoded nontoxic form of SEB carried a triple mutation (L45R/Y89A/Y94A) which has previously been shown to have no toxicity in a variety of assay systems (19, 25–27).
Agrobacterium-mediated soybean transformations were performed as described previously (21–24). Putative transgenic events were taken to maturity, and T1 seeds were collected. Genomic DNAs were prepared from individual cot chips and used in PCR to screen for the presence of the transgene. Seed proteins were also extracted from individual cot chips and used in Western analyses and enzyme-linked immunosorbent assay (ELISAs) to screen and quantify transgenic mSEB. Based on results from these assays, select seeds were germinated and propagated over several generations.
Storage of transgenic seeds expressing soy-mSEB.
Transgenic seeds (20 seeds per lot) were stored in brown envelopes under ambient laboratory conditions (35% relative humidity, 21 to 24°C) from August 2009 until their use at the indicated times following harvest (July 2012).
Purification of mutant SEB (L45R/Y89A/Y94A) from soybean seeds (soy-mSEB).
Transgenic soybean seeds containing mSEB were ground to a fine powder in a generic coffee grinder. Seed protein was extracted by sonication in 50 mM Tris-HCl (pH 7.8) at a ratio of ∼20 ml buffer to 1 g dry seed powder. The sonicated protein mixture was clarified by centrifugation, and endogenous acidic proteins were precipitated by lowering the pH to 4.5. Insoluble proteins were removed by centrifugation, and the pH of the soluble extract was raised to 8.0 prior to passage over DEAE-cellulose. The DEAE flowthrough fraction was collected, dialyzed against 50 mM MES (morpholineethanesulfonic acid; pH 6.0), and then passed over carboxymethyl cellulose (CM-cellulose). Proteins bound to the CM-cellulose resin were eluted using a 0 to 250 mM NaCl step gradient. Western analysis was used to monitor soy-mSEB in protein fractions throughout the purification procedure. Purified mSEB was quantified using the Bradford reagent (with bovine serum albumin [BSA] as a standard), and purity was determined by Coomassie blue staining of SDS-PAGE gels.
Expression and purification of mutant SEB (L45R/Y89A/Y94A) from E. coli (E. coli-mSEB).
The soybean codon-optimized mSEB open reading frame was cloned into a pET expression vector and transformed into E. coli. Following selection and molecular verification, bacterial cultures containing the expression plasmid were grown to stationary phase in terrific broth at 37°C for 16 h. IPTG (isopropyl-β-d-thiogalactopyranoside) was not needed to induce expression of mSEB. Cells were harvested by centrifugation, and the cell paste was resuspended in 50 mM phosphate buffer (pH 6.3) and sonicated on ice. Soluble and insoluble protein fractions were separated by centrifugation, and nickel resin was used to bind protein from the soluble fraction. Recombinant protein was eluted with 50 mM phosphate buffer containing 400 mM imidazole. Western analysis was used to monitor mSEB throughout the purification procedure. Eluted E. coli mSEB was quantified using the Bradford reagent (with BSA as a standard), and purity was determined by Coomassie blue staining of SDS-PAGE gels.
Protease digestion.
Protease (Sigma-Aldrich, St. Louis, MO) was added to four tubes containing 10 μg of recombinant mSEB at increasing concentrations (0.0003, 0.0006, 0.0012, and 0.0025 units) and incubated at 37°C for 10 min. Samples were removed, mixed with SDS-PAGE loading buffer, boiled for 10 min, and subjected to SDS-PAGE and Western blot analysis.
Western blot analysis.
Proteins were separated by SDS-PAGE and transferred in CAPS (N-cyclohexyl-3-aminopropanesulfonic acid) buffer (pH 11) to Immobilon-P membranes (Millipore, Bedford, MA). Membranes were blocked overnight at 4°C with 5% nonfat milk in phosphate-buffered saline (PBS), incubated with rabbit anti-SEB serum (1:5,000) for 1 h at 23°C, and washed three times (for 10 min each) with PBS containing 0.05% Tween. Membranes were then incubated with horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG (Santa Cruz Biotechnology, Santa Cruz, CA) for 30 min at 23°C and washed as described above. Detection was carried out using a SuperSignal West Pico substrate kit (Thermo Scientific, Rockford, IL).
Induction of cytokine production by native SEB and soy-mSEB.
To assess the ability of native SEB and soy-mSEB to function as a superantigen, mononuclear leukocytes were isolated from healthy pig spleen tissue. Following aseptic removal of spleens, single-cell suspensions were made by pressing tissue through 30-gauge wire mesh screens, followed by passage over nylon wool to remove cellular debris. Cells were then pelleted, and mononuclear leukocytes were isolated by centrifugation on Histopaque 1077 density medium (Sigma-Aldrich). After washing, cells were counted, plated at 500,000 per well (Corning, Corning, NY), and incubated in RPMI 1640 (Mediatech, Manassas, VA) supplemented with 10% fetal calf serum (Atlanta Biologicals, Atlanta, GA).
Various concentrations of native SEB (1.0 to 10 μg/ml; Sigma-Aldrich) or purified soy-mSEB (1.0 to 10 μg/ml) were added to wells in triplicate, as indicated. Culture supernates were harvested 48 h later, and gamma interferon (IFN-γ) production was quantified using an ELISA (R&D Systems, Minneapolis, MN) following the instructions supplied by the manufacturer.
Immunization of pigs.
Groups of 25-day-old piglets (n = 4 to 6) were immunized intramuscularly (day 0) and then boosted 14 and 28 days later with 250 μg of E. coli-mSEB or soy-mSEB. Both immunogens were suspended in Alhydrogel (Sigma-Aldrich) as an adjuvant. Control animals received an equal volume of buffer containing Alhydrogel. Injection sites were visually inspected for inflammation at 12, 24, and 36 h postvaccination.
Blood collection and in vivo challenge with native SEB.
Blood was collected by jugular venipuncture from each pig on days 0, 14, and 28 just prior to immunization in coagulation tubes. Serum was extracted from each blood sample for use in determining antibody titers using the ELISA described below.
On days 36 to 38 postimmunization, pigs had intravenous catheters surgically implanted to facilitate toxin administration and to allow rapid and frequent blood collection. Specifically, an 18-gauge central venous catheter (Arrow International, Inc., Reading, PA) was placed in the jugular vein approximately 10 cm proximal to the heart. On days 38 to 40 postimmunization, pigs (n = 3 to 5) were challenged intravenously with a sublethal dose of native SEB (25 μg/kg of body weight). This sublethal dose was defined in prior, developmental studies to be one which induced incapacitation, as defined by prostration, lethargy, emesis, and/or diarrhea, but not death (data not shown). Further, control animals receiving intravenous injection of saline without native SEB had no discernible clinical effects and no significant alterations in the cytokines measured (data not shown). Blood was taken at the indicated hours postchallenge for determining antibody titers and for cytokine quantification using ELISAs as described below.
ELISA to determine anti-SEB antibody titers.
To determine the anti-SEB titers in sera of immunized animals, microtiter plates were coated with 200 ng/well of native SEB (Toxin Technology, Sarasota, FL) in 100 μl of carbonate buffer overnight at 4°C. Wells were then blocked with 1% BSA in PBS. After washing, serial dilutions of sera were incubated in wells for 2 h at room temperature. After unbound material was washed off, a horseradish peroxidase-conjugated goat anti-swine IgG (Southern Biotech, Birmingham, AL) was added for 2 h. Following washing, plates were incubated with 3,3′,5,5′-tetramethylbenzidine (TMB) substrate (BioFX) at room temperature. The enzymatic reactions were stopped by addition of 1 M sulfuric acid, and absorbances were read at 405 nm. The endpoint titer was defined as the last serum dilution with an absorbance double that of animals immunized in a similar manner with an irrelevant immunogen.
In vitro antibody neutralization assay.
To assess the ability of antibodies from immunized pigs to inactivate native SEB, an in vitro neutralization assay was performed. Sera isolated from individual pigs were dialyzed against RPMI 1640 medium and filtered (0.2 μm) prior to use. Various dilutions of each serum antibody sample (0 to 1 mg) were incubated with 10 μg/ml of native SEB in a total of 100 μl for 30 min in microtiter plates prior to the addition of pig splenic leukocytes. Pig splenic leukocytes were isolated as described above and incubated in RPMI 1640 (Mediatech) supplemented with 10% fetal calf serum (Atlanta Biologicals). Cell cultures were incubated at 37°C for 48 h. Culture supernates were harvested, and gamma interferon production was quantified using an ELISA (R&D Systems) and the instructions supplied by the manufacturer.
ELISA to quantify serum cytokine levels.
On days 38 to 40 postimmunization, pigs (n = 3 to 5) were challenged intravenously with a sublethal dose of native SEB (25 μg/kg). Blood was taken at the indicated hours postchallenge, and sera were extracted for quantification of interleukin-1β (IL-1β), IL-6, IL-8, IL-12p40, IFN-γ, and tumor necrosis factor alpha (TNF-α) by use of ELISAs (R&D Systems) and the instructions supplied by the manufacturer.
Statistical analysis.
For analysis of growth performance, data were analyzed using the MIXED procedure of the statistical analysis system SAS 9.1 (SAS, Cary, NC). Significance was declared when the P value was <0.05. Data are presented as least-squares means with the pooled standard error of the mean (SEM).
For analysis of immune responses in pigs, one-way analysis of variance (ANOVA) was performed, followed by the post hoc Tukey-Kramer test, using Graph Pad Prism 4.0 software (Innotech, Schönaich, Germany). Statistical significance was declared when the P value was <0.05, and data are presented as means ± standard errors.
RESULTS
Characterization, quantification, and stability of soy-mSEB.
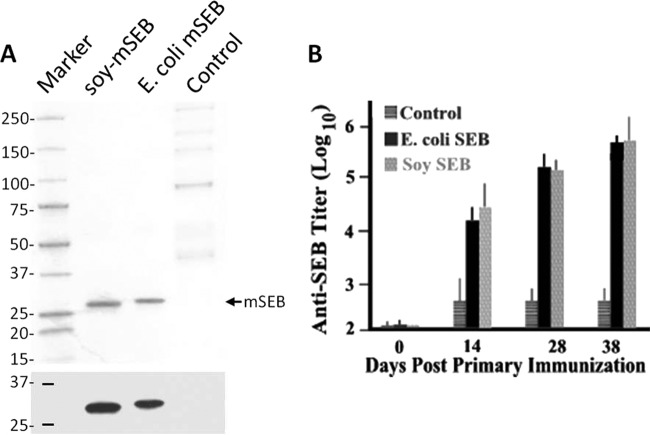
To test the safety and immunogenicity of soy-mSEB, this mutant form of the toxin was purified from transgenic seeds and quantified prior to its use. Following affinity chromatography, a single band migrating at approximately 28 kDa in Coomassie-stained SDS-PAGE gels was observed (Fig. 1A). Western blot analyses demonstrated the identity of this protein band by its being immunoreactive with anti-SEB antibodies (Fig. 1B). Quantification of purified soy-mSEB, prior to its use in vitro and in vivo, was performed using Bradford protein assays and a capture ELISA specific for native SEB (data not shown), along with coelectrophoresis of known quantities of recombinant mSEB by Western blot analysis (Fig. 1C).
Fig 1.
Purification, quantification, and stability of soy-mSEB. Soybean-derived mSEB (soy-mSEB) was expressed in transgenic soybean seeds and purified by affinity chromatography as outlined in Materials and Methods. (A) Representative Coomassie blue-stained SDS-PAGE gel. (B) Representative Western blot of crude soybean extract (10 μg) next to purified extract (1 μg), each demonstrating a single band of soy-mSEB at approximately 28 kDa. (C) Representative Western blot used for quantification of soy-mSEB purified from seed extracts relative to recombinant SEB standards. (D) (Left) Western blot analysis of soymilk protein (10 μg) extracted from T1 seeds expressing mSEB. Seeds were harvested in 2009 and stored for 3 years at ambient temperature. (Right) Digestion of recombinant mSEB (2 μg) with increasing amounts of protease. The migration of molecular size standard proteins is shown in kilodaltons in all panels.
To demonstrate the stability of soy-mSEB, transgenic seeds were harvested from plants and stored at ambient temperature for as long as 3 years. Western blot analyses were performed using antibodies against SEB to demonstrate the presence of intact soy-mSEB. Figure 1D (left panel) shows a representative Western blot of soy-mSEB at the predicted size of 28 kDa for seeds that were stored for 3 years at ambient temperature. In our routine seed screening, we saw no evidence of detectable smaller fragments which would be indicative of mSEB degradation, regardless of the storage time. Figure 1D (right panel) shows that when recombinant mSEB was treated with trypsin, degraded mSEB fragments could be detected using this Western blotting assay, which utilized a polyclonal anti-SEB antibody. The fact that we never detected such fragmentation, even with seeds stored for 3 years at ambient temperature, demonstrates the stability of soy-mSEB.
Soy-mSEB lacks superantigen activity in pig lymphocytes.
Previous works have demonstrated a lack of superantigen activity for E. coli-mSEB, using human, primate, or pig leukocyte cultures (17, 19, 28). Figure 2 demonstrates that while pig leukocytes are quite responsive to native SEB, soy-mSEB induced no detectable secretion of cytokines. Therefore, soy-mSEB was similar to E. coli-mSEB in its inability to activate cultured leukocytes, even at high concentrations (17, 19, 28). These in vitro studies suggested that soy-mSEB used in subunit vaccine formulations would be nontoxic to piglets.
Fig 2.
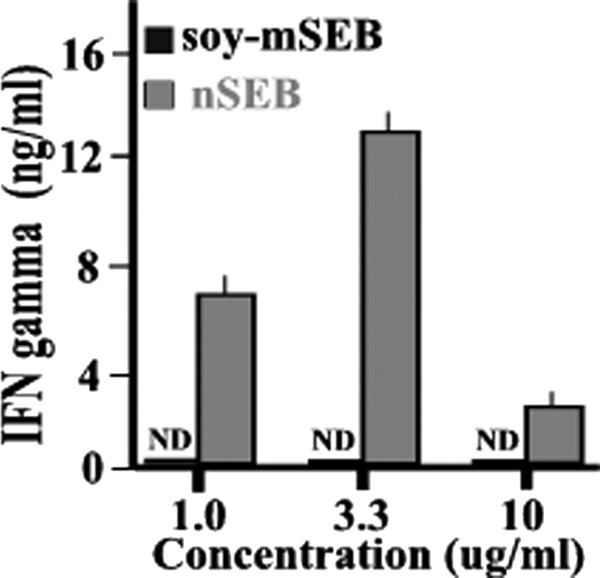
Soy-mSEB lacks superantigen activity in pig lymphocytes. Pig splenic leukocytes were isolated and then cultured in the presence of the indicated concentrations of native SEB (nSEB) or soy-mSEB. After 48 h of culture, culture supernates were taken and porcine IFN-γ secretion determined using an ELISA. Results are presented as mean values (plus SEM) for triplicate determinations. Levels of gamma interferon that were below the 50-pg/ml detection limit for this ELISA were designated nondetectable (ND).
Intramuscular vaccination with alum-adjuvanted soy-mSEB has no significant effect on piglet weight.
The in vitro results from Fig. 2 suggested that soy-mSEB would be nontoxic to pigs, even when injected intramuscularly with alum as an adjuvant. To demonstrate the safety of such vaccine formulations, groups of pigs received an immunization regimen with soy-mSEB, E. coli-mSEB, or buffer containing adjuvant. Each animal was monitored during this course of treatment for food consumption and body weight. There was no significant difference in weight gain in comparing the three groups of piglets throughout the immunization regimen (data not shown).
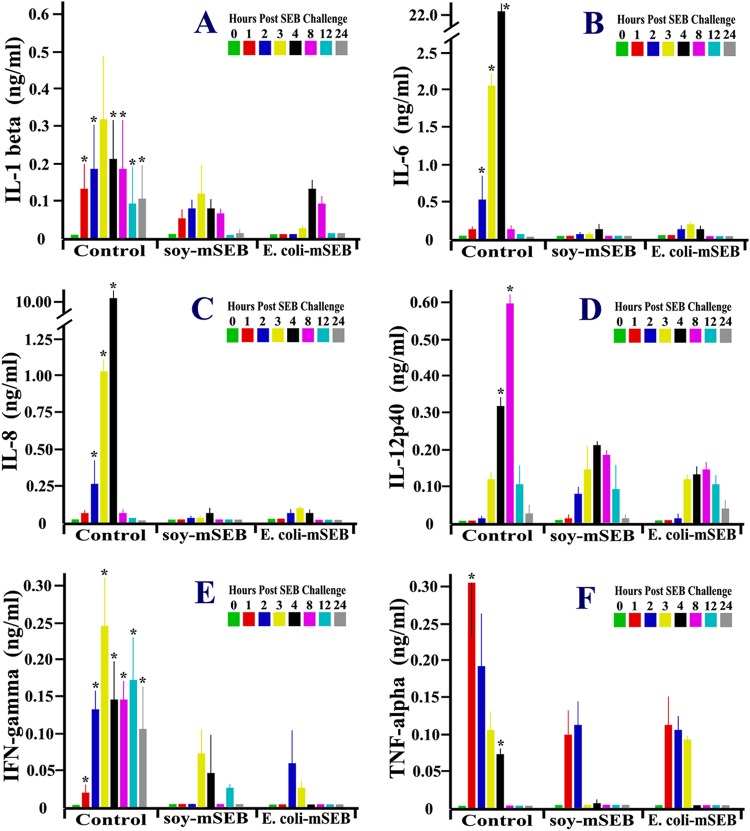
Immunization of pigs with soy-mSEB or E. coli-mSEB results in similar anti-SEB antibody responses.
To demonstrate that immunization with soy-mSEB or E. coli-mSEB could induce similar antibody responses, groups of pigs received intramuscular injections of either purified vaccine or buffer (Fig. 3A) in alum adjuvant on days 0, 14, and 28. Blood was taken from each animal prior to immunization on the indicated days, and serum antibodies against native SEB were detected by ELISA. Figure 3B shows that as early as day 14 following a single immunization, significant levels of IgG anti-SEB antibodies could be detected in the sera of pigs immunized with either soy-mSEB or E. coli-mSEB compared to sera from control animals. Antibody titers continued to increase on days 28 and 38 following booster vaccinations. Pigs immunized with soy-mSEB had titers that were indistinguishable from those of pigs immunized with E. coli-mSEB (Fig. 3B). Taken together, these studies demonstrated that either vaccine candidate was effective in inducing antibodies which recognized native SEB, regardless of the protein expression system used for production.
Fig 3.
Immunization of pigs with soy-mSEB and E. coli-mSEB results in high antitoxin serum titers. Groups of 25-day-old pigs (n = 5) were immunized intramuscularly (day 0) and then boosted on days 14 and 28 with E. coli-mSEB or soy-mSEB in alum. Control pigs were immunized with an equal amount of buffer containing alum. (A) Representative Coomassie blue-stained SDS-PAGE gel and accompanying Western blot, demonstrating the purity of each immunogen. Each animal was bled just prior to immunization on days 0, 14, 28, and 38. (B) ELISAs were performed to determine serum IgG anti-native SEB reactivity. These data are presented as mean anti-native SEB titers (plus SEM).
In vitro anti-soy-mSEB antibody neutralization of native SEB.
To begin to assess the ability of antibodies from immunized pigs to inactivate native SEB, an in vitro neutralization assay was performed. Antisera from individual pigs were mixed with native SEB prior to adding the mixture to cultured pig leukocytes. The ability of the antibodies to bind native SEB and neutralize its toxic effects was assayed by detecting a reduction in toxin-induced gamma interferon production. Figure 4 shows that dilutions of antisera from pigs immunized with soy-mSEB or E. coli-mSEB had similar abilities to limit native SEB-induced gamma interferon production in vitro compared to antisera from control animals. These results demonstrated that the antagonistic antibodies induced by either vaccine were indistinguishable in their ability to neutralize native SEB toxicity in vitro.
Fig 4.
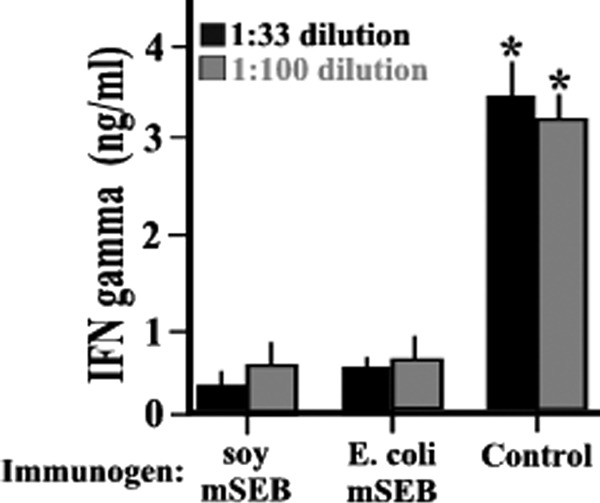
Antibodies from pigs immunized with soy-mSEB and E. coli-mSEB effectively neutralized native SEB activity in vitro. Sera collected at day 38 postimmunization were used in an in vitro neutralization assay to demonstrate the ability to limit native SEB-induced cytokine responses. Dilutions (1:33 or 1:100) of sera from soy-mSEB-immunized, E. coli-mSEB-immunized, or control animals were mixed with 0.5 μg/ml of native SEB for 30 min prior to the addition of the mixtures to cultures of pig splenic leukocytes. Forty-eight hours after coincubation, culture supernates were taken and porcine IFN-γ secretion determined using an ELISA. Results are presented as mean values (plus SEM) for triplicate determinations for each immunogen group (n = 3 or 4). Asterisks indicate statistically significant differences (P < 0.01) compared to control animals.
In vivo challenge of immunized pigs with a sublethal dose of native SEB.
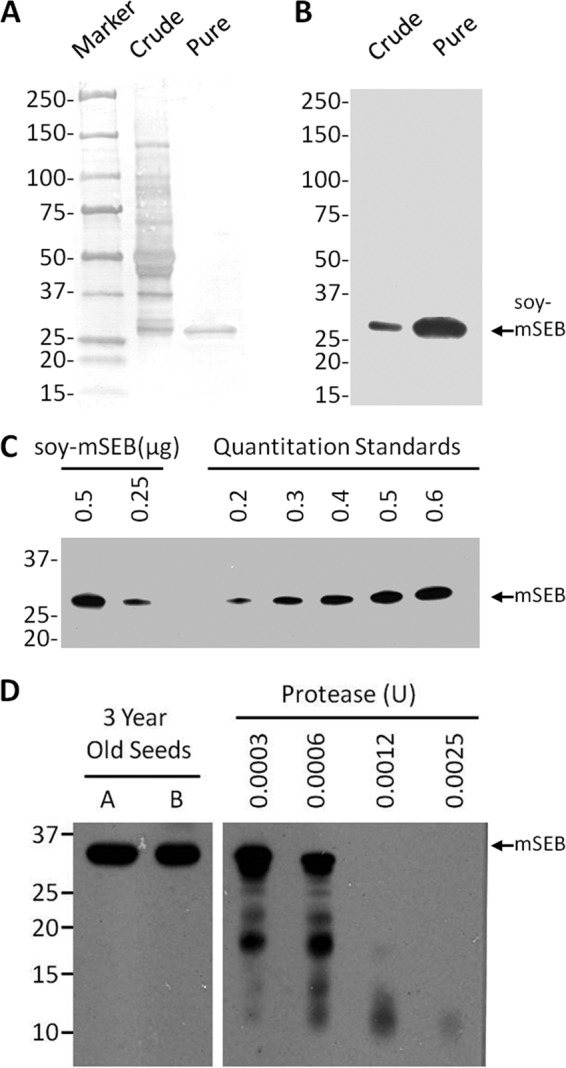
As a final test of vaccine efficacy, pigs were challenged in vivo with native SEB. On days 36 to 38 postimmunization, pigs had intravenous catheters surgically implanted to facilitate toxin administration and to allow rapid and frequent blood collection. Our preliminary studies had demonstrated that sublethal doses of native SEB given intravenously stimulated a rapid and dramatic cytokine cascade in pigs (data not shown). We utilized this sublethal model to follow the magnitude and duration of this cytokine response. Pigs were challenged with 25 μg/kg of native SEB, and blood was taken at 0, 1, 2, 3, 4, 8, 12, and 24 h postchallenge. The acute IL-1β (Fig. 5A), IL-6 (Fig. 5B), IL-8 (Fig. 5C), IL-12p40 (Fig. 5D), IFN-γ (Fig. 5E), and TNF-α (Fig. 5F) responses were followed in each pig immunized with soy-mSEB or E. coli-mSEB and in control animals. Each of these mediators was significantly increased at multiple times following challenge of control pigs compared to preadministration levels (0 h), indicating toxin-induced cytokine induction (Fig. 5).
Fig 5.
Reduced cytokine responses in pigs immunized with soy-mSEB and E. coli-mSEB following challenge with a sublethal dose of native SEB. At 36 to 38 days postimmunization, pigs had intravenous catheters surgically implanted to facilitate toxin administration and to allow for rapid and frequent blood collection. At days 38 to 40 postimmunization, pigs (n = 3 to 5) were challenged intravenously with a sublethal dose of native SEB (25 μg/kg). Blood was taken at the indicated hours postchallenge for quantification of IL-1β (A), IL-6 (B), IL-8 (C), IL-12p40 (D), IFN-γ (E), and TNF-α (F). For each time postchallenge (0, 1, 2, 3, 4, 8, 12, and 24 h), cytokines in sera (ng/ml) are presented as mean levels (plus SEM) for each group (n = 3 to 5) of immunized pigs. Asterisks indicate P values of <0.05 for comparing control values to values obtained for soy-mSEB- or E. coli-mSEB-immunized animals.
Overall, pigs immunized with soy-mSEB showed significantly reduced cytokine responses following native SEB challenge compared to controls (Fig. 5). The most dramatic reductions in the cytokine response included those of IL-6 (Fig. 5B), IL-8 (Fig. 5C), IFN-γ (Fig. 5E), and TNF-α (Fig. 5F). More modest overall decreases in IL-1β (Fig. 5A) and IL-12p40 (Fig. 5D) were also observed.
Similar results were observed in pigs immunized with E. coli-mSEB (Fig. 5). In total, the reductions in toxin-induced cytokine production in these vaccinated pigs mirrored those observed in pigs immunized with soy-mSEB. We concluded from these results that immunization with either vaccine candidate induced immunity that was substantially equivalent as assayed by the ability to reduce a native SEB-induced cytokine cascade following in vivo challenge.
Clinical observations of pigs challenged with a sublethal dose of SEB.
Despite the fact that pigs immunized with soy-mSEB or E. coli-mSEB had significantly reduced cytokine responses following challenge with native SEB, this did not completely alleviate all clinical symptoms of toxicity. All pigs in each group experienced some level of incapacitation, regardless of the immunization. Clinical symptoms for each pig included at least one of the following: emesis, prostration, and lethargy. Clinical symptoms began within 1 to 2 h following native toxin challenge.
DISCUSSION
SEB was originally weaponized as an incapacitating agent (8, 10). Such biological weapons debilitate victims for days to weeks following exposure, requiring medical personnel and treatment facilities to provide supportive care during recovery. The considerable infrastructure required to recover from widespread SEB exposure likely heightens the attractiveness of this toxin for weaponization (7) as well as bioterrorism (9). Mortality from weaponized SEB was not the primary objective, since there are more efficient methods for achieving battlefield fatalities (29). In fact, exposure to SEB in contaminated foodstuffs (5) or following accidental aerosolization (8, 11) rarely results in death.
Therefore, the goal of therapeutic interventions targeting SEB toxicity should focus on eliminating the ability of this agent to incapacitate. Likely, this will be a more difficult milestone to achieve than merely reducing any modest mortality that might have occurred following weaponized or bioterrorism-delivered SEB. This rationale directed our efforts to develop an incapacitating pig model using sublethal toxin exposure. Such a model more closely mimics what would occur within populations and provides much more sensitive efficacy endpoints (Fig. 5) than models which rely on death following exposure to extreme dosages of native toxin (17, 19, 30, 31).
While it is generally accepted that a cytokine cascade rapidly initiates clinical symptomology following exposure to SEB in humans (5), defining which combination of cytokines is responsible for incapacitation remains unclear. This fact makes a comparison of the acute cytokine response in humans versus pigs following a sublethal SEB exposure difficult. Since SEB functions as a superantigen in pigs (Fig. 2), it is logical to assume that this animal's response could mirror the human condition. If this assumption is accurate, then the data reported here represent some of the first to quantify the kinetics and magnitude of an acute cytokine response following an incapacitating, sublethal dose of SEB that might be relevant to humans (Fig. 5).
Unfortunately, other animal models provide little insight into understanding the SEB-induced cytokine cascade in humans. It is not surprising that mouse models of SEB toxicity which require lipopolysaccharide (LPS) potentiation (17–19, 26) do not induce cytokine responses that are similar in kinetics or magnitude to those observed here (Fig. 5). SEB does not function as a superantigen in normal mice (17–19, 26), and the potentiator LPS can influence the cytokine response by itself. Attempts to genetically manipulate mice by expressing HLA class II increased the responsiveness of these animals to SEB (32, 33). However, the cytokine responses reported for these animals (32, 33) do not mimic the cytokine responses observed here (Fig. 5). It seems logical to assume that the cytokine response in pigs, for which SEB functions as a superantigen (Fig. 2), would be more representative of the human response than that of normal or genetically manipulated mice. In addition, complicating much of the mouse model literature is the use of supralethal doses of SEB, SEB plus LPS, or SEB plus other potentiating agents (e.g., d-galactosamine [32]). While such large amounts of toxin may be useful for evaluating the conditions responsible for SEB-induced mortality in rodents, they likely have little relevance for sublethal human exposures, as noted above.
SEB-induced lethality models have also been developed in pigs and primates. An SEB dose of 150 μg/kg was lethal to 100% of piglets (27, 30), suggesting that this dose represented more than 5 times the 50% lethal dose (LD50). Analyses of serum cytokine responses following this lethal injection were quite modest (30) compared to those observed here (Fig. 5). For example, the IL-6 and IL-8 responses following lethal injection (150 μg/kg) did not exceed 15 and 35 pg/ml, respectively (30). For comparison, we observed IL-6 and IL-8 serum levels of approximately 22,000 and 10,000 pg/ml, respectively, at peak times following injection with sublethal SEB (25 μg/ml). Whether these differences were due to SEB dosages, the age of pigs at toxin challenge, or some other factor is presently unclear. Similar difficulties arise in attempting to evaluate the role of cytokines in SEB-induced death in primates (34). In some cases, in vivo cytokine responses were not reported (17), or the reported values (31, 34) are very different from the results obtained here (Fig. 5). For example, no significant TNF-α responses were reported in the first 24 h following exposure, and it took 24 h for significant increases in IL-6 to be observed (31). Each of these primate studies utilized lethal doses of SEB (75 LD50s and 150 μg/kg) given by aerosol (17, 34) or endotracheal tube (31). The only study to use a nonlethal dose of SEB found somewhat elevated IL-2 and IL-6 levels but no significant TNF-α or IFN-γ production following exposure of primates to aerosolized SEB (35). These results (35) are difficult to reconcile with the activity of SEB as a superantigen (5). In contrast, the data reported here represent some of the first to quantify the kinetics and magnitude of the cytokine response following an incapacitating, sublethal dose of SEB (Fig. 5). Pigs clearly recognize this toxin as a superantigen (Fig. 2), and the resulting cytokine response is rapid and dramatic (Fig. 5). As toxin is cleared and pigs begin to recover, the cytokine response abates. Additional studies will be required to define which particular cytokines make the greatest contribution to the pathophysiology associated with exposure to sublethal doses of SEB.
No efficacious therapy currently exists for treating or preventing SEB toxicity. Passive administration of anti-SEB antibodies (12–15) suffers from the therapeutic challenge of competing with the rapidity of toxin action. It is not clear how prophylactic use of such antibodies could be implemented. Active immunization against modified or mutant SEB proteins seems promising; however, it is difficult to assess the efficacy of such efforts. One SEB mutant (with the L45R, Y89A, and Y94A mutations) has shown the promise of being nontoxic (17, 19, 28) as well as stimulating antibodies which neutralize native toxin (Fig. 4) (17, 19, 28). Vaccination studies using formulations with alum-based adjuvants demonstrated its ability to reduce mortality in primates following exposure to lethal doses of aerosolized toxin (17). It was not clear from this study whether the immunized macaques that survived still experienced significant incapacitation (17). Regardless, phase I clinical trials for this potential vaccine candidate, designated STEBVax, are pending. However, results from the studies presented here question the extent of protection of such mutant SEB vaccine formulations. While high titers against native SEB were achieved using soy-mSEB or E. coli-mSEB (Fig. 3B), and toxin-induced cytokine responses were reduced (Fig. 5), immunized pigs still experienced some level of incapacitation. These symptoms included emesis, prostration, and/or lethargy, and at least one of these symptoms was observed in each pig. A reduction in primate mortality (17) and a reduction in the cytokine cascade following toxin exposure (Fig. 5) may not be sufficient to effectively limit the incapacitating effects of weaponized or bioterrorism-delivered SEB. Formulations which include more efficacious adjuvants (36) or which stimulate mucosal and systemic antibody responses may be required to achieve such a high level of resistance to toxin exposure. For example, one formulation that promoted immunity and long-term memory to protein antigens was discovered (37). For these studies, virus-sized nanoparticles were used to encapsulate protein antigens alongside encapsulated Toll-like receptor 4 (TLR-4) and TLR-7 agonists. Following immunization, not only did the vaccinations produce high titers of antibody and T cell responses, but memory responses were persistent. Nanoparticle-mediated delivery to antigen-presenting cells coupled with the stimulating effects of Toll-like receptor danger signals resulted in efficacious immunization against the protein antigen. Such studies suggest that the future of biodefense vaccines may lie in customized formulations of one or more subunit proteins presented as particles while being adjuvanted by one or more danger signals.
While questions still remain regarding the efficacy of mSEB vaccinations using alum adjuvants, there are other hurdles to overcome in attempting to manufacture biodefense vaccines. The sustainability of producing, purifying, and stockpiling sufficient quantities of biodefense vaccines is a daunting task (38–40). Major factors limiting the perpetual maintenance of vaccine stocks include the cost of production, cost of purification, limited shelf life, and cold storage requirements for many of these biologics. Continually destroying entire lots of outdated vaccines not only is costly but also wastes valuable resources while affecting the environment. It cannot be assumed that biodefense funds will always be available for maintaining stockpiles of biodefense vaccines using current manufacturing processes and current storage requirements. Developing platforms for vaccine production and processing and rapid-response manufacturing, as well as defining formulations with an extended shelf life that require no cold chain are therefore worthy goals.
The preclinical biodefense vaccine candidate selected for this study was a triple mutant of SEB (17–19), designated STEBVax. A detailed purification scheme for this E. coli-derived mutant toxin has already been published (41) and serves as a comparison for considering expression of the identical mutant toxin expressed in soybean seeds. Specifically, Table 1 shows the previously reported figures for E. coli-derived vaccine production (41) and our laboratory findings and theoretical projections for manufacturing the equivalent, soy-derived protein. The differences are dramatic and reflect the biology of these two very distinct protein expression platforms.
Table 1.
Comparison of E. coli- and soybean-derived mSEB starting materials and yields
| Expression systema | Vol of starting material (liters)b | Starting biomassc | Total soluble protein from biomassd | Recoverable yield of vaccine (g)e |
|---|---|---|---|---|
| E. coli cell culture | 56.5 (from fermentor) | 2,543 g of bacterial cell pellet | 28.127 g | 8.297 |
| Transgenic soybean seeds | 1.0 (soy powder) | 800 g of soy powder per liter | 320.000 g of protein per liter (theoretical) | 12.800 (theoretical) |
E. coli-derived mutant SEB (L45R/Y89A/Y94A) was produced as described previously (6). Soy-mSEB was produced as described in Materials and Methods.
The volume of E. coli cell culture was taken from a previous report (41). One liter of soy powder made by grinding transgenic seeds expressing soy-mSEB is used as a theoretical comparison.
The starting biomass of E. coli-mSEB required medium filtration and concentration of the cell pellet. The size of the pellet mass was taken from a previous report (41). One liter of soy powder equals approximately 800 g and required no additional concentration or manipulation.
The total soluble protein extracted from the E. coli cell pellet was taken from a previous report (41). Theoretically, 320 g of protein can be extracted from 800 g of soy powder, since approximately 40% of the total mass is protein (42). This number assumes minimal loss of protein during the extraction procedure.
The stability of E. coli-derived SEB was stated to be 1 year at −70°C (41). This result implies that every year, this expensive, laborious production and purification scheme must be repeated if there is to be a ready available stock of vaccine for use in response to a bioterrorism threat that may or may not occur. Alternatively, soy powder made from transgenic seeds expressing soy-mSEB was found to be stable over many years at ambient storage temperatures (Fig. 1D). The implications of this finding are that vaccine production can be a separate event, with purification occurring later if desired. Stated simply, it should be possible to store soy powder expressing soy-mSEB for years, until it is needed, without the need for refrigeration or freezing. This ability to separate protein production, in time and geography, from its purification has the potential to add unprecedented flexibility and cost savings to the logistics of supplying recombinant proteins as needed with minimal waste.
The practicality of maintaining a perpetual stockpile of biodefense vaccines rests in the successes of future endeavors to reduce costs, increase shelf life, eliminate cold storage, and simplify the manufacturing process. Here we compared the efficacies of soy-mSEB and E. coli-mSEB as vaccines in a pig model and found the two immunogens to be substantially equivalent. These studies not only demonstrate the ability of transgenic soybean seeds to function as a platform technology for expressing proteins but also highlight the unique advantages of this manufacturing system.
ACKNOWLEDGMENT
This work was supported by Public Health Service grant R42 AI72777 from the National Institute of Allergy and Infectious Diseases.
Footnotes
Published ahead of print 31 October 2012
REFERENCES
- 1. Dinges MM, Orwin PM, Schlievert PM. 2000. Exotoxins of Staphylococcus aureus. Clin. Microbiol. Rev. 13:16–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Herman A, Kappler JW, Marrack P, Pullen AM. 1991. Superantigens: mechanism of T-cell stimulation and role in immune responses. Annu. Rev. Immunol. 9:745–772 [DOI] [PubMed] [Google Scholar]
- 3. Papageorgiou AC, Tranter HS, Acharya KR. 1998. Crystal structure of microbial superantigen staphylococcal enterotoxin B at 1.5 A resolution: implications for superantigen recognition by MHC class II molecules and T-cell receptors. J. Mol. Biol. 277:61–79 [DOI] [PubMed] [Google Scholar]
- 4. Drake CG, Kotzin BL. 1992. Superantigens: biology, immunology, and potential role in disease. J. Clin. Immunol. 12:149–162 [DOI] [PubMed] [Google Scholar]
- 5. Marrack P, Kappler J. 1990. The staphylococcal enterotoxins and their relatives. Science 248:705–711 [DOI] [PubMed] [Google Scholar]
- 6. Swaminathan S, Furey W, Pletcher J, Sax M. 1992. Crystal structure of staphylococcal enterotoxin B, a superantigen. Nature 359:801–806 [DOI] [PubMed] [Google Scholar]
- 7. Christopher GW, Cieslak TJ, Pavlin JA, Eitzen EM., Jr 1997. Biological warfare. A historical perspective. JAMA 278:412–417 [PubMed] [Google Scholar]
- 8. Ulrich RG, Sidell S, Taylor TJ. 1997. Staphylococcal enterotoxin B and related pyogenic toxins, p 621–631 In Sidell FR, Takafuji ET, Franz DR. (ed), Textbook of military medicine. Part 1. Warfare, weaponry and the casualty. Office of the Surgeon General, Department of the Army, Washington, DC [Google Scholar]
- 9. Madsen JM. 2001. Toxins as weapons of mass destruction. A comparison and contrast with biological-warfare and chemical-warfare agents. Clin. Lab. Med. 21:593–605 [PubMed] [Google Scholar]
- 10. Dembek ZF. 2007. Medical aspects of biological warfare, p. xxiii Office of the Surgeon General, United States Army Medical Department Center and School, Washington, DC [Google Scholar]
- 11. Rusnak JM, Kortepeter M, Ulrich R, Poli M, Boudreau E. 2004. Laboratory exposures to staphylococcal enterotoxin B. Emerg. Infect. Dis. 10:1544–1549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Karauzum H, Chen G, Abaandou L, Mahmoudieh M, Boroun AR, Shulenin S, Devi VS, Stavale E, Warfield KL, Zeitlin L, Roy CJ, Sidhu SS, Aman MJ. 2012. Synthetic human monoclonal antibodies towards staphylococcal enterotoxin B (SEB) protective against toxic shock syndrome. J. Biol. Chem. 287:25203–25215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Larkin EA, Stiles BG, Ulrich RG. 2010. Inhibition of toxic shock by human monoclonal antibodies against staphylococcal enterotoxin B. PLoS One 5:e13253 doi:10.1371/journal.pone.0013253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tilahun ME, Kwan A, Natarajan K, Quinn M, Tilahun AY, Xie C, Margulies DH, Osborne BA, Goldsby RA, Rajagopalan G. 2011. Chimeric anti-staphylococcal enterotoxin B antibodies and lovastatin act synergistically to provide in vivo protection against lethal doses of SEB. PLoS One 6:e27203 doi:10.1371/journal.pone.0027203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Varshney AK, Wang X, Cook E, Dutta K, Scharff MD, Goger MJ, Fries BC. 2011. Generation, characterization, and epitope mapping of neutralizing and protective monoclonal antibodies against staphylococcal enterotoxin B-induced lethal shock. J. Biol. Chem. 286:9737–9747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tseng J, Komisar JL, Trout RN, Hunt RE, Chen JY, Johnson AJ, Pitt L, Ruble DL. 1995. Humoral immunity to aerosolized staphylococcal enterotoxin B (SEB), a superantigen, in monkeys vaccinated with SEB toxoid-containing microspheres. Infect. Immun. 63:2880–2885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Boles JW, Pitt ML, LeClaire RD, Gibbs PH, Torres E, Dyas B, Ulrich RG, Bavari S. 2003. Generation of protective immunity by inactivated recombinant staphylococcal enterotoxin B vaccine in nonhuman primates and identification of correlates of immunity. Clin. Immunol. 108:51–59 [DOI] [PubMed] [Google Scholar]
- 18. Stiles BG, Garza AR, Ulrich RG, Boles JW. 2001. Mucosal vaccination with recombinantly attenuated staphylococcal enterotoxin B and protection in a murine model. Infect. Immun. 69:2031–2036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ulrich RG, Olson MA, Bavari S. 1998. Development of engineered vaccines effective against structurally related bacterial superantigens. Vaccine 16:1857–1864 [DOI] [PubMed] [Google Scholar]
- 20. National Research Council 1998. Nutrient requirements of swine, 10th ed National Academies Press, Washington, DC [Google Scholar]
- 21. Garg R, Tolbert M, Oakes JL, Clemente TE, Bost KL, Piller KJ. 2007. Chloroplast targeting of FanC, the major antigenic subunit of Escherichia coli K99 fimbriae, in transgenic soybean. Plant Cell Rep. 26:1011–1023 [DOI] [PubMed] [Google Scholar]
- 22. Hudson L, Bost KL, Piller KJ. 2011. Optimizing recombinant protein expression in soybean seeds, p 19–42 In Sudaric A. (ed), Soybean: molecular aspects of breeding. InTech, Rijeka, Croatia [Google Scholar]
- 23. Piller KJ, Clemente TE, Jun SM, Petty CC, Sato S, Pascual DW, Bost KL. 2005. Expression and immunogenicity of an Escherichia coli K99 fimbriae subunit antigen in soybean. Planta 222:6–18 [DOI] [PubMed] [Google Scholar]
- 24. Powell R, Hudson LC, Lambirth KC, Luth D, Wang K, Bost KL, Piller KJ. 2011. Recombinant expression of homodimeric 660 kDa human thyroglobulin in soybean seeds: an alternative source of human thyroglobulin. Plant Cell Rep. 30:1327–1338 [DOI] [PubMed] [Google Scholar]
- 25. Mateu de Antonio E, Husmann RJ, Hansen R, Lunney JK, Strom D, Martin S, Zuckermann FA. 1998. Quantitative detection of porcine interferon-gamma in response to mitogen, superantigen and recall viral antigen. Vet. Immunol. Immunopathol. 61:265–277 [DOI] [PubMed] [Google Scholar]
- 26. Stiles BG, Bavari S, Krakauer T, Ulrich RG. 1993. Toxicity of staphylococcal enterotoxins potentiated by lipopolysaccharide: major histocompatibility complex class II molecule dependency and cytokine release. Infect. Immun. 61:5333–5338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van Gessel YA, Mani S, Bi S, Hammamieh R, Shupp JW, Das R, Coleman GD, Jett M. 2004. Functional piglet model for the clinical syndrome and postmortem findings induced by staphylococcal enterotoxin B. Exp. Biol. Med. 229:1061–1071 [DOI] [PubMed] [Google Scholar]
- 28. Inskeep TK, Stahl C, Odle J, Oakes J, Hudson L, Bost KL, Piller KJ. 2010. Oral vaccine formulations stimulate mucosal and systemic antibody responses against staphylococcal enterotoxin B in a piglet model. Clin. Vaccine Immunol. 17:1163–1169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Richardson JG. 2004. The bane of “inhumane” weapons and overkill: an overview of increasingly lethal arms and the inadequacy of regulatory controls. Sci. Eng. Ethics 10:667–692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bi S, Das R, Zelazowska E, Mani S, Neill R, Coleman GD, Yang DC, Hammamieh R, Shupp JW, Jett M. 2009. The cellular and molecular immune response of the weanling piglet to staphylococcal enterotoxin B. Exp. Biol. Med. (Maywood) 234:1305–1315 [DOI] [PubMed] [Google Scholar]
- 31. Komisar JL, Weng CF, Oyejide A, Hunt RE, Briscoe C, Tseng J. 2001. Cellular and cytokine responses in the circulation and tissue reactions in the lung of rhesus monkeys (Macaca mulatta) pretreated with cyclosporin A and challenged with staphylococcal enterotoxin B. Toxicol. Pathol. 29:369–378 [DOI] [PubMed] [Google Scholar]
- 32. Faulkner L, Cooper A, Fantino C, Altmann DM, Sriskandan S. 2005. The mechanism of superantigen-mediated toxic shock: not a simple Th1 cytokine storm. J. Immunol. 175:6870–6877 [DOI] [PubMed] [Google Scholar]
- 33. Roy CJ, Warfield KL, Welcher BC, Gonzales RF, Larsen T, Hanson J, David CS, Krakauer T, Bavari S. 2005. Human leukocyte antigen-DQ8 transgenic mice: a model to examine the toxicity of aerosolized staphylococcal enterotoxin B. Infect. Immun. 73:2452–2460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Weng CF, Komisar JL, Hunt RE, Johnson AJ, Pitt ML, Ruble DL, Tseng J. 1997. Immediate responses of leukocytes, cytokines and glucocorticoid hormones in the blood circulation of monkeys following challenge with aerosolized staphylococcal enterotoxin B. Int. Immunol. 9:1825–1836 [DOI] [PubMed] [Google Scholar]
- 35. Krakauer T, Pitt L, Hunt RE. 1997. Detection of interleukin-6 and interleukin-2 in serum of rhesus monkeys exposed to a nonlethal dose of staphylococcal enterotoxin B. Mil. Med. 162:612–615 [PubMed] [Google Scholar]
- 36. O'Hagan DT, De Gregorio E. 2009. The path to a successful vaccine adjuvant—‘the long and winding road.' Drug Discov. Today 14:541–551 [DOI] [PubMed] [Google Scholar]
- 37. Kasturi SP, Skountzou I, Albrecht RA, Koutsonanos D, Hua T, Nakaya HI, Ravindran R, Stewart S, Alam M, Kwissa M, Villinger F, Murthy N, Steel J, Jacob J, Hogan RJ, Garcia-Sastre A, Compans R, Pulendran B. 2011. Programming the magnitude and persistence of antibody responses with innate immunity. Nature 470:543–547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Barrett AD, Beasley DW. 2009. Development pathway for biodefense vaccines. Vaccine 27(Suppl 4):D2–D7 [DOI] [PubMed] [Google Scholar]
- 39. Matheny J, Mair M, Smith B. 2008. Cost/success projections for US biodefense countermeasure development. Nat. Biotechnol. 26:981–983 [DOI] [PubMed] [Google Scholar]
- 40. Poland GA, Jacobson RM, Tilburt J, Nichol K. 2009. The social, political, ethical, and economic aspects of biodefense vaccines. Vaccine 27(Suppl 4):D23–D27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Coffman JD, Zhu J, Roach JM, Bavari S, Ulrich RG, Giardina SL. 2002. Production and purification of a recombinant staphylococcal enterotoxin B vaccine candidate expressed in Escherichia coli. Protein Expr. Purif. 24:302–312 [DOI] [PubMed] [Google Scholar]
- 42. Bost KL, Piller KJ. 2011. Protein expression systems: why soybean seeds?, p 3–18 In Sudaric A. (ed), Soybean: molecular aspects of breeding. InTech, Rijeka, Croatia [Google Scholar]